Introduction
Acute exacerbation is a common event for chronic
obstructive pulmonary disease (COPD), the third leading cause of
death worldwide, and is characterized by worsened dyspnea, cough
and sputum within 14 days, which is often related to elevated
pulmonary and systemic inflammation (1). Due to ethnic and lifestyle
differences, patients with acute exacerbation of COPD (AECOPD) at
high altitude (HA) may exhibit distinct disease patterns. Previous
studies showed that in highlands of Peru and China, the disease
burden in patients with COPD was mainly attributed to the use of
biomass fuels rather than smoking (2,3),
with a confirmed genetic association between the Tibetans and
susceptibility to COPD (4),
indicating that environmental and genetic factors may uniquely
affect AECOPD progression in HA populations.
Furthermore, when exposed to the hypobaric and
hypoxic environment at HA, AECOPD patients not only experience
exacerbated gas exchange and hypoxia with subsequent higher rates
of complications such as pulmonary hypertension (PH) (5-7),
but also exhibit increased inflammation and oxidative stress
(8,9), which may further result in prolonged
hospitalization, increased medical costs and higher mortality
risks. However, demographic and clinical features of patients with
AECOPD at HA have not been well elucidated.
The present study aimed to systematically compare
the demographics, cardiopulmonary comorbidities and laboratory data
of patients with AECOPD residing at HA and low altitude (LA), and
identify factors associated with prolonged length of hospital stay
(LOHS) in patients with AECOPD at HA to offer insights for the
evaluation and prognosis of these patients.
Patients and methods
Subjects
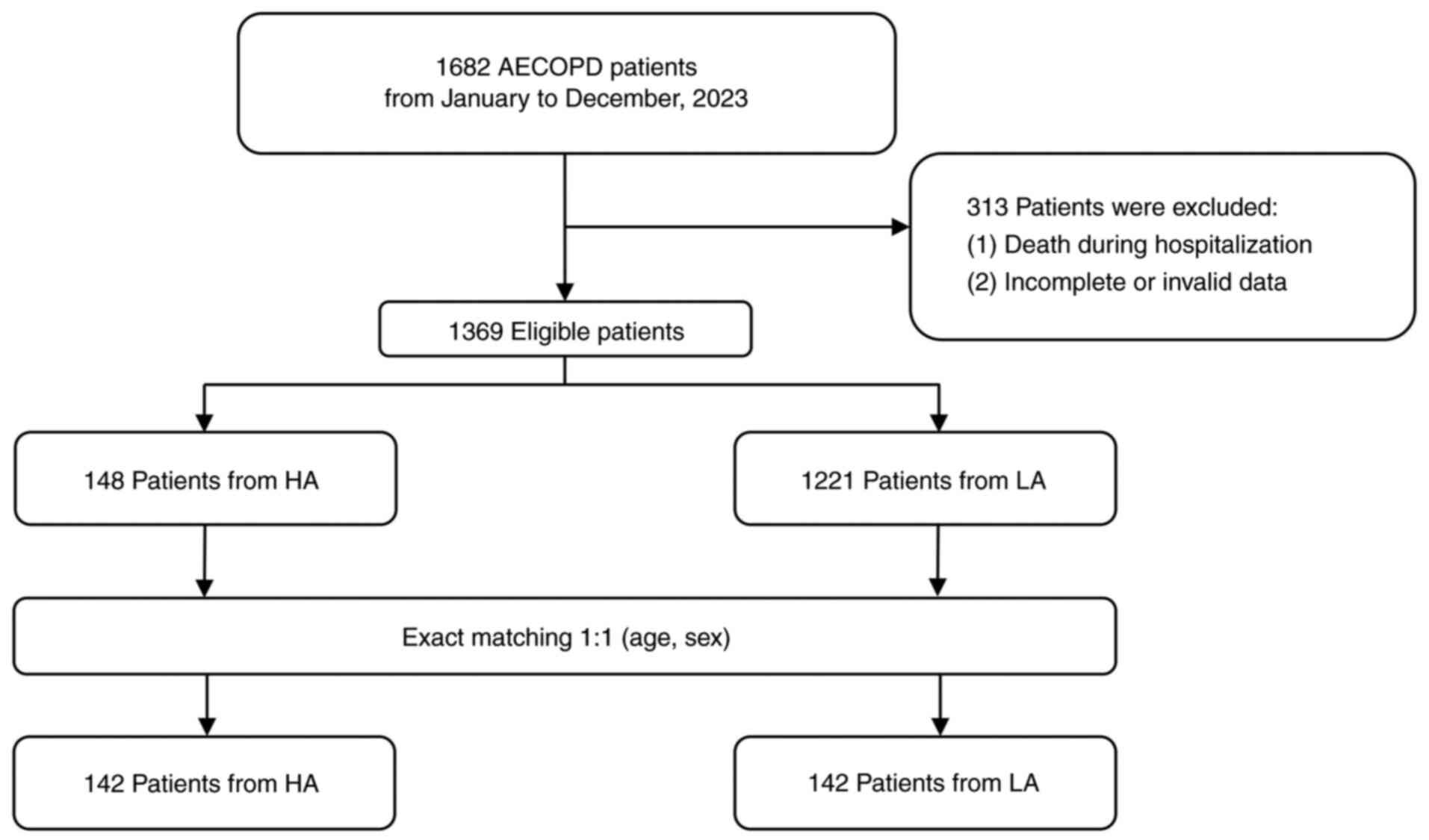
A total of 142 patients with AECOPD at HA [>2,500
meters (m)] who were hospitalized in West China Hospital of Sichuan
University (Chengdu, China) between January 1, 2023 and December
31, 2023 and comprised of 102 males and 40 females with a median
age of 68.25 years and an age range of 46 to 93 years, were
retrospectively recruited. These patients were natives and
long-term (>10 years) immigrants in Qinghai-Tibet Plateau. For
each patient, an age- and sex-matched control from LA (<500 m)
who was hospitalized during the same period, selected through
simple random sampling when multiple candidates met the criteria,
was identified (Fig. 1). The
inclusion criteria were: i) A discharge diagnosis of AECOPD,
characterized by increased dyspnea and/or cough and sputum within
14 days, based on the Global Initiative for Chronic Obstructive
Lung Disease (GOLD) 2024 Report (10); ii) patients aged ≥40 years at
admission; and iii) availability of complete baseline and clinical
data. The exclusion criteria were: i) Patients not hospitalized for
the first time due to AECOPD at West China Hospital of Sichuan
University; ii) patients whose respiratory difficulties were
primarily caused by factors other than AECOPD, such as
pneumothorax, pleural effusion, acute coronary syndrome or
pulmonary embolism; iii) patients who died during hospitalization
or were discharged against medical advice; and iv) patients with
incomplete baseline or clinical data. All of the patients included
in the study were consecutive and hospitalized patients. Data for
this study was collected through a retrospective search of the
hospital's electronic system between February 9, 2024 and May 17,
2024.
The study was approved by the Ethics Committee of
West China Hospital of Sichuan University (Chengdu, China; approval
no. 2024-85) and conducted following the Helsinki Declaration.
Data collection
Baseline information, including age, sex, smoking
status and ethnicity, as well as cardiopulmonary comorbidities,
laboratory data and LOHS, which was defined as the period from
admission to discharge, were collected. Considering the impact of
chronic hypoxia at HA on blood, immune and metabolic functions
(11), laboratory data mainly
encompassed blood routine tests [hemoglobin (Hb), platelets (PLT),
white blood cells (WBC), neutrophils (NEU), eosinophils (EOS) and
lymphocytes (LYM)], liver function [total bilirubin (TB), direct
bilirubin (DB), indirect bilirubin (IB), aspartate transaminase
(AST), alanine transaminase (ALT), gamma-glutamyl transferase
(GGT), lactate dehydrogenase (LDH)], kidney function [urea,
creatinine (Cr), uric acid (UA)] and metabolic indicators [glucose
(Glu), total cholesterol (TC), triglycerides (TG) and low-density
lipoprotein (LDL)]. These laboratory data were collected upon
admission and all measurements complied with standard methods and
technical requirements. Furthermore, cardiopulmonary comorbidities
were investigated, including hypertension, pulmonary heart disease
(PHD), PH, respiratory failure, pneumonia, pulmonary tuberculosis,
coronary heart disease (CHD) and bronchiectasis.
Statistical analysis
SPSS software version 29 (IBM Corp.) was used for
all statistical analyses. Normally distributed data were expressed
as the mean ± standard deviation, while skewed data were reported
as the median (interquartile range). The independent-sample t-test
(two-tailed) and the Mann-Whitney U test were employed for
comparing normally and skewed distributed data, respectively.
Chi-square tests were used to compare categorical variables.
Fisher's exact test was used to compare categorical variables with
frequencies of <5, such as ethnicity. Furthermore, since there
is no standardized definition for prolonged LOHS in patients with
AECOPD and previous research emphasized the heterogeneity of LOHS
among patients from different hospitals (12), the 75th percentile was predefined
as the cut-off for prolonged LOHS, referencing established
methodologies (13). Accordingly,
prolonged LOHS was defined as >18 inpatient days for patients
from HA (Table I). Univariate and
multivariate binary logistic regression analyses were performed
using the binary logistic regression model to identify factors
related to prolonged LOHS in patients from HA. Receiver operating
characteristic (ROC) curve analysis was used to identify the
cut-off values of variables for logistic regression analysis.
P<0.05 was considered to indicate statistical significance.
 | Table IDemographics and length of hospital
stay of patients with acute exacerbation of chronic obstructive
pulmonary disease at HA and LA. |
Table I
Demographics and length of hospital
stay of patients with acute exacerbation of chronic obstructive
pulmonary disease at HA and LA.
| Characteristic | HA (n=142) | LA (n=142) | P-value |
|---|
| Age, years | 68.25±9.36 | 68.25±9.36 | >0.999 |
| Sex | | | >0.999 |
|
Male | 102 (71.8) | 102 (71.8) | |
|
Female | 40 (28.2) | 40 (28.2) | |
| Smoking | | | 0.015 |
|
Yes | 77 (54.2) | 97 (68.3) | |
|
No | 65 (45.8) | 45 (31.7) | |
| Ethnicity | | | <0.001 |
|
Han | 39 (27.5) | 141 (99.3) | |
|
Tibetan | 101 (71.1) | 0 (0) | |
|
Other | 2 (1.4) | 1 (0.7) | |
| LOHS, days | 13.00 (9.00,
18.00) | 11.00 (9.00,
16.00) | 0.259 |
Results
Demographics and cardiopulmonary
comorbidities compared between patients with AECOPD at HA and
LA
The age in each of the two groups was 68.25±9.36
years, with the same gender distribution of 102 males (71.8%) and
40 females (28.2%). In the LA group, there were 141 Han individuals
(99.3%) and 97 smokers (68.3%). Compared to patients at LA,
patients at HA had a higher percentage of Tibetans (n=101, 71.1%)
and non-smokers (n=65, 45.8%). Furthermore, the prevalences of
cardiopulmonary comorbidities differed between the two groups. In
the patients at HA, the most prevalent cardiopulmonary
comorbidities were hypertension (40.85%), PHD (35.21%) and PH
(28.90%). Respiratory failure was observed in 25.35% of patients
and pneumonia was found in 23.24%. Another two notable
comorbidities, pulmonary tuberculosis and CHD, affected 11.27% of
the patients, respectively. In the LA group, PHD was the most
common comorbidity, affecting 57.04% of patients, followed by
respiratory failure in 54.93%. Hypertension was observed in 23.94%
of patients and PH in 21.80%. Pneumonia was present in 18.31%,
while bronchiectasis was found in 11.27% and CHD was observed in
5.63%. Demographics of the two groups are shown in Table I, while the cardiopulmonary
comorbidities are listed in Table
II.
 | Table IICardiopulmonary comorbidities of
patients with acute exacerbation of chronic obstructive pulmonary
disease at HA and LA. |
Table II
Cardiopulmonary comorbidities of
patients with acute exacerbation of chronic obstructive pulmonary
disease at HA and LA.
| Comorbidity | HA (n=142) | LA (n=142) |
|---|
| Hypertension | 58 (40.85) | 34 (23.94) |
| Pulmonary heart
disease | 50 (35.21) | 81 (57.04) |
| Pulmonary
hypertension | 41 (28.90) | 31 (21.80) |
| Respiratory
failure | 36 (25.35) | 78 (54.93) |
| Pneumonia | 33 (23.24) | 26 (18.31) |
| Pulmonary
tuberculosis | 16 (11.27) | 0 (0.00) |
| Bronchiectasis | 0 (0.00) | 16 (11.27) |
| Coronary heart
disease | 16 (11.27) | 8 (5.63) |
Laboratory data of patients with
AECOPD at HA and LA
Significant differences in laboratory indicators
were observed between the two groups (Table III). The HA group exhibited
significantly elevated levels of Hb at 145.92±34.50 g/l compared to
129.00 (118.50, 143.00) g/l in the LA group (P<0.001), with a
higher EOS count at 0.14 (0.06, 0.24) x109/l in
comparison to 0.06 (0.00, 0.18) x109/l in the LA group
(P<0.001). Furthermore, lower counts of WBC (P<0.001) and NEU
(P<0.001) were also observed in the patients at HA. In terms of
liver and kidney function, the HA group demonstrated higher levels
of TB (P<0.001), DB (P<0.001), IB (P<0.001), AST
(P=0.023), ALT (P=0.001) and GGT (P<0.001), along with lower
levels of urea (P=0.015) and Cr (P=0.034). Regarding metabolic
indicators, TG (P=0.050) was higher, but Glu (P=0.002) and TC
(P<0.001) were notably lower in the HA group.
 | Table IIILaboratory data of patients with acute
exacerbation of chronic obstructive pulmonary disease at HA and
LA. |
Table III
Laboratory data of patients with acute
exacerbation of chronic obstructive pulmonary disease at HA and
LA.
| Parameter | Normal range | HA (n=142) | LA (n=142) | P-value |
|---|
| Blood routine | | | | |
|
Hb, g/l | 115.00-150.00 | 145.92±34.50 | 129.00 (118.50,
143.00) | <0.001 |
|
PLT,
x109/l | 100.00-300.00 | 165.00 (127.75,
226.75) | 167.50 (123,00,
231.50) | 0.935 |
|
WBC,
x109/l | 3.50-9.50 | 5.90 (4.78,
7.31) | 6.76 (5.50,
9.18) | <0.001 |
|
NEU,
x109/l | 1.80-6.30 | 3.95 (3.09,
5.52) | 4.94 (3.75,
7.35) | <0.001 |
|
EOS,
x109/l | 0.02-0.52 | 0.14 (0.06,
0.24) | 0.06 (0.00,
0.18) | <0.001 |
|
LYM,
x109/l | 1.10-3.20 | 1.04 (0.76,
1.45) | 1.13±0.60 | 0.779 |
| Liver function | | | | |
|
TB,
µmol/l | 3.20-20.50 | 13.50 (9.88,
19.10) | 9.65 (7.30,
14.18) | <0.001 |
|
DB,
µmol/l | <6.80 | 5.45 (3.50,
8.00) | 3.65 (2.60,
5.53) | <0.001 |
|
IB,
µmol/l | <20.00 | 7.45 (5.30,
11.70) | 5.75 (4.28,
8.93) | <0.001 |
|
AST,
IU/l | <35.00 | 25.50 (18.75,
36.00) | 22.00 (17.00,
28.25) | 0.023 |
|
ALT,
IU/l | <40.00 | 24.00 (15.00,
37.00) | 17.00 (12.00,
29.25) | 0.001 |
|
GGT,
IU/l | <45.00 | 52.00 (25.75,
92.25) | 23.50 (14.00,
41.75) | <0.001 |
|
LDH,
µmol/l | 120.00-250.00 | 205.00 (164.00,
278.75) | 196.00 (170.25,
249.75) | 0.664 |
| Kidney
function | | | | |
|
Urea,
µmol/l | 2.60-7.50 | 4.77 (3.60,
6.51) | 5.48 (4.03,
7.63) | 0.015 |
|
Cr,
µmol/l | 48.00-79.00 | 67.50 (51.90,
80.18) | 71.75 (57.45,
87.00) | 0.034 |
|
UA,
µmol/l | 155.00-357.00 | 296.50 (210.35,
361.25) | 258.50 (189.50,
338.75) | 0.079 |
| Metabolic
indicators | | | | |
|
Glu,
mmol/l | 3.90-6.10 | 4.98 (4.36,
6.30) | 5.70 (4.75,
7.23) | 0.002 |
|
TC,
mmol/l | 2.80-5.17 | 3.76±1.02 | 4.20 (3.46,
5.03) | <0.001 |
|
TG,
mmol/l | 0.29-1.70 | 1.00 (0.76,
1.28) | 0.91 (0.69,
1.20) | 0.050 |
|
LDL,
mmol/l | <3.40 | 2.16±0.80 | 2.29±0.82 | 0.159 |
Factors associated with prolonged LOHS
in patients with AECOPD at HA
An increased median LOHS was revealed in the HA
group (13 days) vs. the LA group (11 days), although the difference
did not reach any statistical significance (P=0.259) (Table I). Of note, markedly higher Hb
levels and EOS count were observed in patients at HA compared with
those at LA, which were identified as the two key factors
influencing prolonged LOHS at HA by univariate and multivariate
binary logistic regression analyses. The results of the univariate
binary logistic regression analyses presented in Table IV indicated that patients with
AECOPD at HA with prolonged LOHS had a lower Hb level (P=0.027) and
EOS count (P=0.027). ROC curve analysis was used to identify the
cut-off values of variables for logistic regression analysis
(Fig. 2). Consequently, 157.5 g/l
was determined as the cut-off for Hb [area under curve (AUC)=0.633;
sensitivity, 40.7%; specificity, 82.4%], while the cut-off for EOS
was determined to be 0.075x109/l (AUC=0.628;
sensitivity, 73.1%; specificity, 50.0%). Based on these findings,
Hb and EOS were included as covariates in the multivariate logistic
regression model. Continuous variables were converted into
categorical variables according to the established cut-off values.
The results indicated that Hb <157.5 g/l [odds ratio (OR):
3.356, 95% confidence interval (CI): 1.257-8.964] and EOS
<0.075x109/l (OR: 2.849, 95% CI: 1.255-6.467) were
significantly associated with prolonged LOHS in patients with
AECOPD at HA, as shown in Table
V.
 | Table IVDemographics and laboratory data of
patients with acute exacerbation of chronic obstructive pulmonary
disease at HA with non-prolonged and prolonged LOHS. |
Table IV
Demographics and laboratory data of
patients with acute exacerbation of chronic obstructive pulmonary
disease at HA with non-prolonged and prolonged LOHS.
| Variables | Non-prolonged LOHS
(n=108) | Prolonged LOHS
(n=34) | OR (95% CI) | P-value |
|---|
| Demographics | | | | |
|
Age,
years | 68.00±8.94 | 69.06±10.76 | 1.012
(0.971-1.055) | 0.565 |
| Sex | | | 0.894
(0.375-2.131) | 0.801 |
|
Male | 77 (71.3) | 25 (73.5) | | |
|
Female | 31 (28.7) | 9 (26.5) | | |
| Smoking | | | 0.934
(0.431-2.023) | 0.863 |
|
No | 49 (45.4) | 16 (47.1) | | |
|
Yes | 59 (54.6) | 18 (52.9) | | |
| Blood routine | | | | |
|
Hb, g/l | 149.56±34.41 | 134.35±32.62 | 0.987
(0.975-0.999) | 0.027 |
|
PLT,
x109/l | 165.50 (129.25,
221.50) | 182.53±100.48 | 1.000
(0.996-1.005) | 0.914 |
|
WBC,
x109/l | 5.93 (4.98,
7.29) | 5.49 (4.43,
8.18) | 1.007
(0.883-1.149) | 0.917 |
|
NEU,
x109/l | 3.95 (3.05,
5.15) | 3.88 (3.12,
6.87) | 1.087
(0.954-1.239) | 0.210 |
|
EOS,
x109/l | 0.14 (0.06,
0.28) | 0.08 (0.03,
0.17) | 0.032
(0.002-0.671) | 0.027 |
|
LYM,
x109/l | 1.19±0.50 | 0.89 (0.63,
1.20) | 0.506
(0.225-1.137) | 0.099 |
| Liver function | | | | |
|
TB,
µmol/l | 13.40 (10.10,
19.78) | 13.95 (8.78,
18.33) | 1.001
(971-1.033) | 0.928 |
|
DB,
µmol/l | 5.45 (3.50,
7.90) | 5.45 (3.88,
8.15) | 1.023
(0.983-1.065) | 0.267 |
|
IB,
µmol/l | 8.05 (5.45,
11.85) | 7.86±4.46 | 0.945
(0.873-1.023) | 0.163 |
|
AST,
IU/l | 26.00 (19.00,
37.50) | 24.00 (14.75,
31.50) | 0.994
(0.977-1.011) | 0.503 |
|
ALT,
IU/l | 23.50 (17.25,
37.75) | 24.00 (13.75,
37.00) | 0.992
(0.974-1.010) | 0.367 |
|
GGT,
IU/l | 49.00 (26.25,
91.25) | 55.50 (21.75,
103.50) | 1.000
(0.996-1.005) | 0.929 |
|
LDH,
µmol/l | 205.00 (165.25,
278.75) | 225.94±85.33 | 0.999
(0.995-1.002) | 0.551 |
| Kidney
function | | | | |
|
Urea,
µmol/l | 4.94 (3.83,
6.52) | 4.40 (3.28,
6.62) | 1.035
(0.971-1.104) | 0.292 |
|
Cr,
µmol/l | 69.10 (57.25,
79.80) | 58.25 (47.00,
88.58) | 1.000
(0.996-1.004) | 0.878 |
|
UA,
µmol/l | 303.59±108.67 | 248.00 (170.00,
336.00) | 1.000
(0.997-1.003) | 0.753 |
| Metabolic
indicators | | | | |
|
Glu,
mmol/l | 4.93 (4.27,
6.29) | 5.18 (4.47,
6.26) | 1.008
(0.873-1.164) | 0.916 |
|
TC,
mmol/l | 3.83±1.02 | 3.53±0.99 | 0.743
(0.499-1.105) | 0.142 |
|
TG,
mmol/l | 1.00 (0.78,
1.33) | 1.06±0.41 | 0.728
(0.319-1.664) | 0.452 |
|
LDL,
mmol/l | 2.22±0.81 | 1.97±0.75 | 0.671
(0.404-1.116) | 0.125 |
 | Table VFactors associated with patients with
acute exacerbation of chronic obstructive pulmonary disease at HA
with prolonged length of hospital stay based on univariate and
multivariate binary logistic regression analysis. |
Table V
Factors associated with patients with
acute exacerbation of chronic obstructive pulmonary disease at HA
with prolonged length of hospital stay based on univariate and
multivariate binary logistic regression analysis.
| Variables | Univariate OR (95%
CI) | P-value | Multivariate OR
(95% CI) | P-value |
|---|
| Hb <157.5
g/l | 3.208
(1.226-8.393) | 0.018 | 3.356
(1.257-8.964) | 0.016 |
| EOS <0.075
x109/l | 2.724
(1.229-6.036) | 0.014 | 2.849
(1.255-6.467) | 0.012 |
Discussion
In the present study, patients with AECOPD residing
at HA and LA were compared, highlighting the heterogeneity of
AECOPD in the two different groups. Compared to the LA group,
patients with AECOPD at HA had a higher proportion of Tibetans and
non-smokers, and exhibited different prevalences of cardiopulmonary
comorbidities, with more hypertension, PH, pneumonia and CHD, and
fewer cases of respiratory failure and PHD, as well as different
indicators in the blood routine and biochemical tests, particularly
higher Hb levels and EOS counts, which were negatively associated
with the LOHS.
Compared with patients at LA, patients with AECOPD
at HA exhibited significantly higher Hb levels, reflecting the
physiological adaptation to chronic hypoxia, achieved by an
increased production of red blood cells to enhance the
oxygen-carrying capacity (14). Hb
<157.5 g/l indicated a lack of adequate compensatory mechanisms,
which may impair oxygen delivery efficiency, thereby complicating
disease management and leading to prolonged LOHS. However,
excessively high Hb levels can pose certain health risks. As
demonstrated in the present study, more hypertension and CHD
overlapped with AECOPD at HA. Besides a different lifestyle in
highlands, a significantly higher median Hb level might facilitate
hypertension and increase blood viscosity, ultimately leading to
CHD (15-18).
Regarding inflammatory status, it was observed that
WBC and NEU counts were significantly lower in the patients at HA,
reflecting suppressed inflammation due to chronic hypoxia, which
could act as a protective adaptation to alleviate inflammatory
damage on cells and tissues (19).
As a result, patients with AECOPD at HA may lack typical
inflammatory responses to infections, such as significant increases
in WBC and NEU, making early identification of infections more
challenging. In the present study, pneumonia and pulmonary
tuberculosis were the main cardiopulmonary infectious comorbidities
for AECOPD at HA, different from those at LA, which were pneumonia
and bronchiectasis, possibly related to significantly lower median
NEU in blood at HA than those at LA. On the contrary, a higher
median EOS count in the blood at HA was noticeably revealed,
present in the majority of Tibetan non-smokers at HA, which
indicated, except smoking, other exposures, such as biomass and
dust, which may take an important part in AECOPD at HA (20). In addition, the elevation of EOS in
patients from HA may indicate an eosinophil-dominated chronic
airway inflammation, which, combined with relatively mild pulmonary
infection, may contribute to a lower prevalence of respiratory
failure and PHD (21,22). Due to a poorer ability to combat
infections (23), a relatively
lower EOS count (<0.075x109/l) in patients may
contribute to prolonged LOHS. Thus, EOS may serve as a potential
biomarker for predicting inhaled corticosteroids responsiveness or
hospitalization duration in patients with AECOPD at HA (24,25).
In addition, PH and PHD were the most important
cardiopulmonary comorbidities in both groups. PH was more prevalent
in patients at HA than LA, mainly owing to the hypoxic environment
in highlands, which likely exaggerated pulmonary vasoconstriction
and thus remodeling at the inflammatory basis of AECOPD. However,
compared to LA, a relatively lower prevalence of PHD was revealed
at HA. In fact, in addition to PH, decompensated PHD is dependent
on several risk factors, particularly pulmonary infection, which is
the most common trigger for AECOPD (26,27).
Furthermore, the HA group showed elevated levels of
liver enzymes and bilirubin, while Glu, TC, urea and Cr were lower
than those in the LA group, indicating metabolic adaptations to
highlands, including increased oxygen consumption, higher basal
metabolic rate, regulation of lipid storage and adjustments of
renal tubular function (28,29).
Although most indicators remained within the normal range, they may
indicate potential risks of cardiovascular, metabolic or renal
diseases.
There are certain limitations to the present study.
The retrospective design limited the completeness of data,
particularly the inability to assess long-term follow-up in
patients with AECOPD in highlands. Potential confounding factors,
such as socioeconomic status, environmental pollution and genetic
differences, were not fully controlled, which may have influenced
the observed associations and introduced bias. Additionally, the
single-center design also restricted the generalizability of the
results, necessitating multi-center studies for validation. Lastly,
the AUC values for Hb and EOS were moderate with limited predictive
ability. By combining multiple symptoms, such as dyspnea, cough and
fever, along with imaging studies and other biomarkers, Hb and EOS
can offer a more comprehensive assessment of patients with AECOPD
at HA, helping physicians develop individualized treatment
plans.
In conclusion, patients with AECOPD at HA,
regardless of sex and age, exhibit unique demographic and clinical
characteristics compared to those at LA, including a higher
proportion of Tibetans and non-smokers, along with differences in
the prevalences of cardiopulmonary comorbidities, and variations in
blood routine and biochemical markers, particularly higher levels
of Hb and blood EOS count, and relatively low Hb levels and EOS
count in patients at HA may increase the risk of prolonged LOHS.
These findings emphasize the significance of these differences in
the evaluation and prognosis of AECOPD at HA, highlighting the
importance of focusing on them to accurately assess and optimize
management strategies, such as improving oxygen therapy,
strengthening infection prevention and enhancing management of
cardiopulmonary comorbidities. Future studies should investigate
the mechanisms underlying these differences and explore novel
interventions to improve clinical outcomes for patients with AECOPD
at HA.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the Key Research and
Development Program of Sichuan Province (grant no.
2024YFFK0084).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YT, BR, and FC made substantial contributions to the
conception and design of the study, acquisition, analysis, and
interpretation of data, as well as manuscript writing. LL and LC
conceived the study, supervised the research, critically reviewed
the manuscript for important intellectual content, and confirmed
the authenticity of the raw data. All authors have read and
approved the final version of the manuscript and agreed to be
accountable for all aspects of the work, ensuring that any
questions related to the accuracy or integrity of any part of the
work were appropriately investigated and resolved.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
West China Hospital of Sichuan University (approval no. 2024-85)
and conducted following the Declaration of Helsinki.
Patient consent for publication
Not applicable.
Competing interests
All the authors declare that they have no competing
interests.
References
|
1
|
Wedzicha JAECC, Miravitlles M, Hurst JR,
Calverley PM, Albert RK, Anzueto A, Criner GJ, Papi A, Rabe KF,
Rigau D, et al: Management of COPD exacerbations: A European
respiratory society/American thoracic society guideline. Eur Respir
J. 49(1600791)2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jaganath D, Miranda JJ, Gilman RH, Wise
RA, Diette GB, Miele CH, Bernabe-Ortiz A and Checkley W: CRONICAS
Cohort Study Group. Prevalence of chronic obstructive pulmonary
disease and variation in risk factors across four geographically
diverse resource-limited settings in Peru. Respir Res.
16(40)2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chenxia G, Qiongda B, Yanping N, Ning S,
Chun C and Yipeng D: Clinical characteristics and management
strategies of chronic obstructive pulmonary disease in
high-altitude areas. Chin J Health Manag. 18:48–53. 2024.(In
Chinese).
|
|
4
|
Xiao J, Han J, Wang X, Hua D, Su D, Bao Y
and Lv F: Association of ADAM33 gene with susceptibility to COPD in
Tibetan population of China. Mol Biol Rep. 38:4941–4945.
2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gonzalez-Garcia M, Barrero M and Maldonado
D: Exercise capacity, ventilatory response, and gas exchange in
COPD patients with mild to severe obstruction residing at high
altitude. Front Physiol. 12(668144)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Aguirre-Franco C, Torres-Duque CA, Salazar
G, Casas A, Jaramillo C and Gonzalez-Garcia M: Prevalence of
pulmonary hypertension in COPD patients living at high altitude.
Pulmonology. 30:247–253. 2024.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yang C, Tuo Y, Shi X, Duo J, Liu X, Zhang
F and Feng X: Prevalence, risk factors, and clinical
characteristics of pulmonary embolism in patients with acute
exacerbation of COPD in Plateau regions: A prospective cohort
study. BMC Pulm Med. 24(102)2024.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Pham K, Parikh K and Heinrich EC: Hypoxia
and inflammation: Insights from high-altitude physiology. Front
Physiol. 12(676782)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Pena E, El Alam S, Siques P and Brito J:
Oxidative stress and diseases associated with high-altitude
exposure. Antioxidants (Basel). 11(267)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Global Initiative for Chronic Obstructive
Lung Disease: Global Strategy for Prevention, Diagnosis and
Management of Copd: 2024 Report, 2023.
|
|
11
|
Zhao Q, Hao D, Wang S, Chen S, Zhou C, Fan
C, Su Q, Huang W, Liu J, Kong Q, et al: Exposure to high altitude
leads to disturbances in host metabolic homeostasis: Study of the
effects of hypoxia-reoxygenation and the associations between the
microbiome and metabolome. mSystems. 10(e0134724)2025.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Quintana JM, Unzurrunzaga A,
Garcia-Gutierrez S, Gonzalez N, Lafuente I, Bare M, de Larrea NF,
Rivas F and Esteban C: IRYSS-COPD Group. Predictors of hospital
length of stay in patients with exacerbations of COPD: A cohort
study. J Gen Intern Med. 30:824–831. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wang Y, Stavem K, Dahl FA, Humerfelt S and
Haugen T: Factors associated with a prolonged length of stay after
acute exacerbation of chronic obstructive pulmonary disease
(AECOPD). Int J Chron Obstruct Pulmon Dis. 9:99–105.
2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Akunov A, Sydykov A, Toktash T, Doolotova
A and Sarybaev A: Hemoglobin changes after long-term intermittent
work at high altitude. Front Physiol. 9(1552)2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Braekkan SK, Mathiesen EB, Njølstad I,
Wilsgaard T and Hansen JB: Hematocrit and risk of venous
thromboembolism in a general population. The Tromso study.
Haematologica. 95:270–275. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Bilo G, Caravita S, Torlasco C and Parati
G: Blood pressure at high altitude: Physiology and clinical
implications. Kardiol Pol. 77:596–603. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Narvaez-Guerra O, Herrera-Enriquez K,
Medina-Lezama J and Chirinos JA: Systemic hypertension at high
altitude. Hypertension. 72:567–578. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
He Z, Chen Z, Wang Y, Qin H, Wu W, Fu P,
Chen S, Wu S and Chen Y: Individual and joint effects of red blood
cell traits on hypertension: A longitudinal analysis. Eur J Prev
Cardiol: Feb 21, 2025 (Epub ahead of print).
|
|
19
|
Malacrida S, Giannella A, Ceolotto G,
Reggiani C, Vezzoli A, Mrakic-Sposta S, Moretti S, Turner R, Falla
M, Brugger H and Strapazzon G: Transcription factors regulation in
human peripheral white blood cells during hypobaric hypoxia
exposure: An in-vivo experimental study. Sci Rep.
9(9901)2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Brakema EA, Tabyshova A, Kasteleyn MJ,
Molendijk E, van der Kleij RMJJ, van Boven JFM, Emilov B,
Akmatalieva M, Mademilov M, Numans ME, et al: High COPD prevalence
at high altitude: Does household air pollution play a role? Eur
Respir J. 53(1801193)2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Pavord ID, Lettis S, Anzueto A and Barnes
N: Blood eosinophil count and pneumonia risk in patients with
chronic obstructive pulmonary disease: A patient-level
meta-analysis. Lancet Respir Med. 4:731–741. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ruiying W, Zhaoyun and Jianying X:
Clinical features and three-year prognosis of AECOPD patients with
different levels of blood eosinophils. Heart Lung. 56:29–39.
2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Shaaban H, Daniel S, Sison R, Slim J and
Perez G: Eosinopenia: Is it a good marker of sepsis in comparison
to procalcitonin and C-reactive protein levels for patients
admitted to a critical care unit in an urban hospital? J Crit Care.
25:570–575. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Cheng SL: Blood eosinophils and inhaled
corticosteroids in patients with COPD: Systematic review and
meta-analysis. Int J Chron Obstruct Pulmon Dis. 13:2775–2784.
2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Viniol C and Vogelmeier CF: Exacerbations
of COPD. Eur Respir Rev. 27(170103)2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Humbert M, Kovacs G, Hoeper MM,
Badagliacca R, Berger RMF, Brida M, Carlsen J, Coats AJS,
Escribano-Subias P, Ferrari P, et al: 2022 ESC/ERS guidelines for
the diagnosis and treatment of pulmonary hypertension. Eur Respir
J. 61(2200879)2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
You L, Niu H, Huang K, Dong F, Yang T and
Wang C: Clinical features and outcomes of acute exacerbation in
chronic obstructive pulmonary disease patients with pulmonary heart
disease: A multicenter observational study. Int J Chron Obstruct
Pulmon Dis. 16:2901–2910. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Wang SY, Gao J and Zhao JH: Effects of
high altitude on renal physiology and kidney diseases. Front
Physiol. 13(969456)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Yuan Z, Zou Y, Liu X, Wang L and Chen C:
Longitudinal study on blood and biochemical indexes of Tibetan and
Han in high altitude area. Front Public Health.
11(1282051)2023.PubMed/NCBI View Article : Google Scholar
|