Introduction
Postoperative delirium (POD) is a prevalent acute
central nervous system disorder in elderly patients following
surgery, typically manifesting 24-72 h post-operation (1,2). POD
contributes to a range of adverse outcomes, including increased
postoperative complications, such as pneumonia, deep venous
thrombosis and accidental injury, extended hospital stays, higher
medical costs and elevated readmission rates (1,2).
Inouye et al (3) reported
that POD affects 11-51% of surgical patients, with the incidence
notably higher in older adults undergoing joint replacement
procedures. With an aging population, the number of elderly
patients undergoing surgery has risen, with a study suggesting that
up to 46% of these patients experience POD (3). Furthermore, previous research has
indicated that delirium or POD may increase the long-term risk of
developing dementia and mortality due to neuroinflammation and
neuronal damage (4). In addition
to its high morbidity, POD escalates treatment costs and hospital
stay durations, placing a substantial financial burden on the
healthcare system. In the United States, >2.6 million adults
aged ≥65 years old experience delirium annually, resulting in an
estimated $164 billion in healthcare expenses each year (4). Addressing the prevention and
reduction of POD during the perioperative period is therefore of
critical importance. However, the precise pathophysiological
mechanisms of delirium remain unclear, complicating diagnosis and
leading to frequent misdiagnosis or oversight. Currently, no
specific medications are available for the treatment or prevention
of delirium (2).
Remimazolam, a novel ultrashort-acting
benzodiazepine, has gained notable attention for its potential in
preventing and managing POD. It has been suggested that remimazolam
may perioperatively reduce the incidence of POD (5). A retrospective observational study
found that elderly patients receiving remimazolam for maintenance
anesthesia experienced markedly lower POD rates compared with those
receiving alternative anesthetics, with remimazolam being
independently associated with a reduced incidence of POD (6). Xue et al (7) similarly reported that perioperative
administration of remimazolam notably decreased the occurrence of
POD. A meta-analysis of 11 trials involving 1,985 participants
indicated that remimazolam decreased the likelihood of POD after
non-cardiac surgery than saline, although it was not superior to
dexmedetomidine or propofol; however, remimazolam was associated
with reduced intraoperative hypotension (5). On the other hand, another systematic
review and meta-analysis indicated that the perioperative use of
remimazolam did not markedly increase POD incidence but it was
linked to a lower rate of intraoperative hypotension (8). Supporting this, in a prospective
randomized controlled trial comparing remimazolam and propofol in
orthopedic surgery for elderly patients, no significant difference
was found in POD incidence between the two groups. However, the
remimazolam group experienced longer postoperative extubation times
and longer stays in the post-anesthesia care unit, although they
had a lower incidence of postoperative hypotension (9). A prospective cohort study in
cardiovascular surgery showed that remimazolam did not markedly
increase POD incidence compared with other anesthetics, suggesting
that it may be a safe option in cardiovascular procedures (10). Furthermore, Glumac et al
(11) reported that preoperative
corticosteroid administration can mitigate the inflammatory
response induced by surgery, reducing the incidence and severity of
cognitive impairment. Given that remimazolam also markedly
alleviates the inflammatory response during the perioperative
period, its potential to reduce POD is promising (12). However, its effects across various
surgical types and patient populations require further
investigation through large-scale trials. Notably, to the best of
our knowledge, no large-scale study has yet examined the impact of
remimazolam on delirium following hip fracture surgery.
Additionally, previous studies did not involve continuous
remimazolam infusion during hip fracture surgery (11,12).
Therefore, the present study aimed to evaluate the
clinical efficacy of continuous remimazolam infusion during hip
fracture surgery with subarachnoid block in elderly patients at
risk for POD. A large sample of data from a single center were
used, which to the best of our knowledge is rarely reported.
Additionally, the study aimed to specifically investigate the role
of remimazolam in the high-risk, vulnerable and understudied hip
fracture population, where polypharmacy, frailty and specific
surgical stressors might modulate drug effects differently.
Patients and methods
Study design and participant
selection
A retrospective study involving 405 elderly patients
who underwent elective hip fracture surgery under subarachnoid
block was conducted at The 904th Hospital of the Joint Logistics
Support Force (Wuxi, China) from January 2019 to December 2023.
Participants were patients of both sexes, aged ≥65 years, with a
BMI of 18.5-31.0 kg/m2 and American Society of
Anesthesiologists (ASA) (13)
grades I-II. The median age was 68 years (range, 65-86) in the
observation group and 69 years (range, 65-87) in the control group.
The present study included 109 male and 71 female patients in the
observation group, and 128 male and 97 female patients in the
control group. Surgical procedures included hip replacement and
femoral neck internal fixation. The study protocol was approved by
the Ethics Committee of The 904th Hospital of the Joint Logistics
Support Force, People's Liberation Army of China (approval no.
2024-002). All participants provided written informed consent.
Exclusion criteria included: i) An inability to complete the
Mini-Mental State Examination (14) or scoring below the minimum
threshold for their educational level [<24 points (less than
postsecondary education), <23 points (less than secondary
education) or <20 points (less than primary education)]; ii)
preoperative central nervous system disorders (such as dementia,
Parkinson's disease or severe sequelae of cerebrovascular events);
iii) prior use of antianxiety or antidepressant medications; iv) a
history of drug or alcohol dependence; v) significant visual or
hearing impairment; vi) pulmonary, hepatic or renal insufficiency;
and vii) contraindications to spinal anesthesia (including the use
of anticoagulants, coagulation disorders, spinal cord diseases or
refusal of spinal anesthesia). Patients were also excluded due to
the following reasons: Converted to general anesthesia during
surgery, intraoperative blood loss of >400 ml, unplanned
transfer to the intensive care unit (ICU) and lost to follow-up
post-operation.
Specific anesthesia protocol
All patients were instructed to fast and abstain
from drinking for ≥8 h prior to surgery. Upon arrival in the
operating room, patients were administered oxygen via a mask at a
flow rate of 4 l/min and peripheral venous access was established.
Standard monitoring included an electrocardiogram and peripheral
oxygen saturation (SpO2) measurements. Radial artery
puncture and catheterization were performed to monitor invasive
blood pressure. Compound sodium acetate was infused at a rate of
5-7 ml/kg/h. Spinal anesthesia was performed with the patient in
the knee-chest position with the affected side facing upward. After
disinfection and draping, the L3-L4 or L2-L3 intervertebral space
was selected for subarachnoid puncture. Once cerebrospinal fluid
was aspirated, 2.0-2.5 ml heavy bupivacaine (1 ml 10% glucose + 2
ml 0.75% bupivacaine) was injected, with the upper limit of
anesthesia targeted at T10-T12.
In the remimazolam group, an initial dose of 0.1
mg/kg remimazolam (diluted to 1 mg/ml and administered over 1 min)
was followed by a continuous intravenous infusion at a rate of 0.2
mg/kg/h to maintain a modified observer's assessment of
alertness/sedation (MOAA/S) score of 1 or 2. If the MOAA/S score
was >2, a supplementary dose of remimazolam (0.05 mg/kg) was
administered, with a minimum interval of 3 min between dose s until
the MOAA/S score dropped to <2. The remimazolam infusion was
discontinued after surgery. For intraoperative management, the
following interventions were used if needed: 8 µg norepinephrine
for hypotension [systolic blood pressure (SBP) <80% of
baseline]; 0.2 mg nicardipine for hypertension (SBP >120% of
baseline); 0.5 mg atropine for bradycardia (heart rate <45
beats/min); and jaw lifting or oxygen administration through a mask
with pressure for hypoxemia (SpO2 <90%), with
oropharyngeal airway or laryngeal mask placement as necessary. The
analgesic pump formula consisted of 1.5 µg/kg sufentanil, 0.25 mg
palonosetron and 100 ml normal saline, with an infusion rate of 2
ml/h, a single press dose of 0.5 ml and a maximum infusion of 15
min. If the visual analogue scale (VAS) pain score was >3 points
postoperatively and unrelieved by the analgesic pump, 50 mg
flurbiprofen axetil was administered intravenously for rescue
analgesia (15). In the control
group, conventional sedation with propofol and analgesia was used
without remimazolam. The initial propofol dosage was 1.0-1.5 mg/kg,
followed by continuous intravenous infusion at a rate of 4-12
mg/kg/h to maintain a MOAA/S score of 1 or 2. Neither group
received sedatives after surgery.
Observation indicators
Intraoperative blood loss, fluid infusion, operation
time, anesthesia time and postoperative hospital stay were
recorded. The Confusion Assessment Method-Chinese Revision (CAM-CR)
was administered between 1 and 7 days after surgery by an
experienced evaluator blinded to the intervention (16). POD occurrence was assessed twice
daily, at 8:00-10:00 a.m. and 4:00-8:00 p.m. A POD diagnosis was
made if the CAM-CR score was >22 at any point. The number of POD
cases, the onset time (from the end of the operation to POD
diagnosis) and the duration (from POD diagnosis to a CAM-CR score
of ≤22 points) were documented. The number of patients who
experienced POD was documented, with POD diagnosis indicating a
positive case. The duration of POD was recorded during the entire
7-day period and the time when POD symptoms occurred was also
documented. Anxiety scores were recorded 1 day before surgery and 1
day post-surgery. The State Anxiety Inventory (17) was used to assess anxiety 1 day
before surgery, whereas the 7-item Generalized Anxiety Disorder
scale (18) was used to evaluate
anxiety 1 day post-surgery. VAS pain scores and the need for rescue
analgesia on days 1-3 post-surgery were also collected.
Additionally, incidences of intraoperative hypertension,
hypotension, bradycardia, hypoxemia, and postoperative nausea and
vomiting were monitored and recorded.
Statistical analysis
Statistical analyses were performed using SPSS
software (version 20.0; IBM Corp) and GraphPad Prism 6.0
(Dotmatics). All data were verified by the data committee of the
hospital. Data were first assessed for normality using the
Shapiro-Wilk test. Continuous variables and data following a normal
distribution are presented as the mean ± standard deviation.
Quantitative data were analyzed using independent sample t-tests,
while categorical data were compared using the χ2 test
or Fisher's exact test. Categorical scores are presented as median
(IQR) and were analyzed using Mann-Whitney U test. A two-sided
P-value <0.05 was considered to indicate a statistically
significant difference. As the results of the univariate analysis
did not fall <0.05, there was no need to conduct a multivariate
analysis.
Results
Patient enrollment and baseline
characteristics
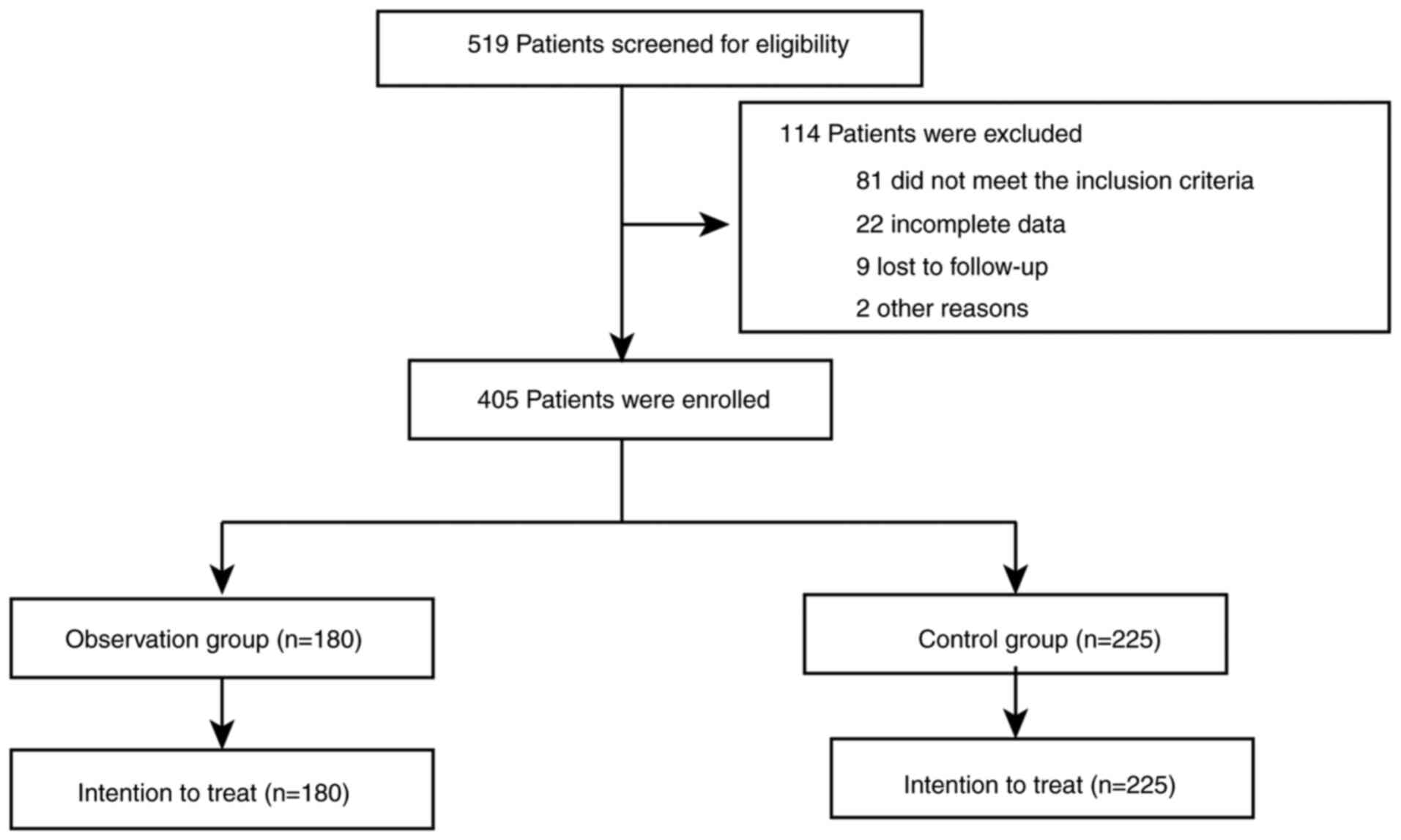
After an initial assessment of 519 patients, 405
patients were enrolled in the study, with 180 in the observation
group and 225 in the control group (Fig. 1). All patients were analyzed using
the intention-to-treat approach. No statistically significant
differences were found between the two groups regarding demographic
characteristics, including sex, age, weight, BMI, ASA
classification, educational level, comorbidities, intraoperative
blood loss, intraoperative fluid infusion volume, operation time,
anesthesia time or postoperative hospital stay (Table I).
 | Table IComparison of baseline data. |
Table I
Comparison of baseline data.
| Characteristic | Observation group
(n=180) | Control group
(n=225) | P-value |
|---|
| Age, years | 68.29±7.15 | 69.06±7.46 | 0.294 |
| Sex, n (%) | | | 0.457 |
|
Male | 109 (60.56) | 128 (56.89) | |
|
Female | 71 (39.44) | 97 (43.11) | |
| BMI,
kg/m2 | 23.12±1.98 | 22.94±1.91 | 0.354 |
| ASA physical
classification status, n (%) | | | 0.184 |
|
I,
Healthy | 7 (3.89) | 15 (6.67) | |
|
II, Mild
systemic disease | 128 (71.11) | 163 (72.44) | |
|
III, Severe
systemic disease | 44 (24.44) | 46 (20.44) | |
|
IV, Severe,
life-threatening disease | 1 (0.56) | 1 (0.44) | |
| Educational level,
n (%) | | | 0.805 |
|
<Elementary
school | 113 (62.78) | 145 (64.44) | |
|
Elementary
school | 45 (25.00) | 51 (22.67) | |
|
≥Secondary
school | 22 (12.22) | 29 (12.89) | |
| Median
MMSEa (IQR) | 20 (17, 24) | 20 (16, 25) | 0.865 |
| Preexisting
dementia, n (%) | 66 (36.67) | 84 (37.33) | 0.890 |
| Preoperative
delirium, n (%) | 1 (0.56) | 2 (0.89) | >0.999 |
| Type of fracture, n
(%) | | | - |
|
Femoral
neck | 104 (57.78) | 131 (58.22) | 0.928 |
|
Intertrochanteric | 68 (37.78) | 87 (38.67) | 0.855 |
|
Subtrochanteric | 6 (3.33) | 6 (2.67) | 0.694 |
|
Femoral
head | 2 (1.11) | 1 (0.44) | 0.587 |
| Risk factors | | | |
|
Smoking
history, n (%) | 57 (31.67) | 74 (32.89) | 0.794 |
|
Hypertension,
n (%) | 119 (66.11) | 154 (68.44) | 0.619 |
|
Hyperlipidemia,
n (%) | 104 (57.78) | 122 (54.22) | 0.474 |
|
Diabetes, n
(%) | 51 (28.33) | 66 (29.33) | 0.825 |
|
Atrial
fibrillation, n (%) | 78 (43.33) | 91 (40.44) | 0.558 |
| Living environment,
n (%) | | | 0.840 |
|
Town | 75 (41.67) | 96 (42.67) | |
|
Countryside | 105 (58.33) | 129 (57.33) | |
| Intraoperative
blood loss, ml | 110.54±21.04 | 108.61±20.86 | 0.357 |
| Intraoperative
fluid infusion volume, ml | 950.76±65.43 | 938.27±67.29 | 0.20 |
| Operation time,
min | 62.18±15.63 | 65.44±14.09 | 0.395 |
| Anesthesia time,
min | 98.07±18.95 | 97.72±19.87 | 0.857 |
| Postoperative
hospital stay, days | 9.29±2.05 | 9.17±1.92 | 0.546 |
Comparison of POD
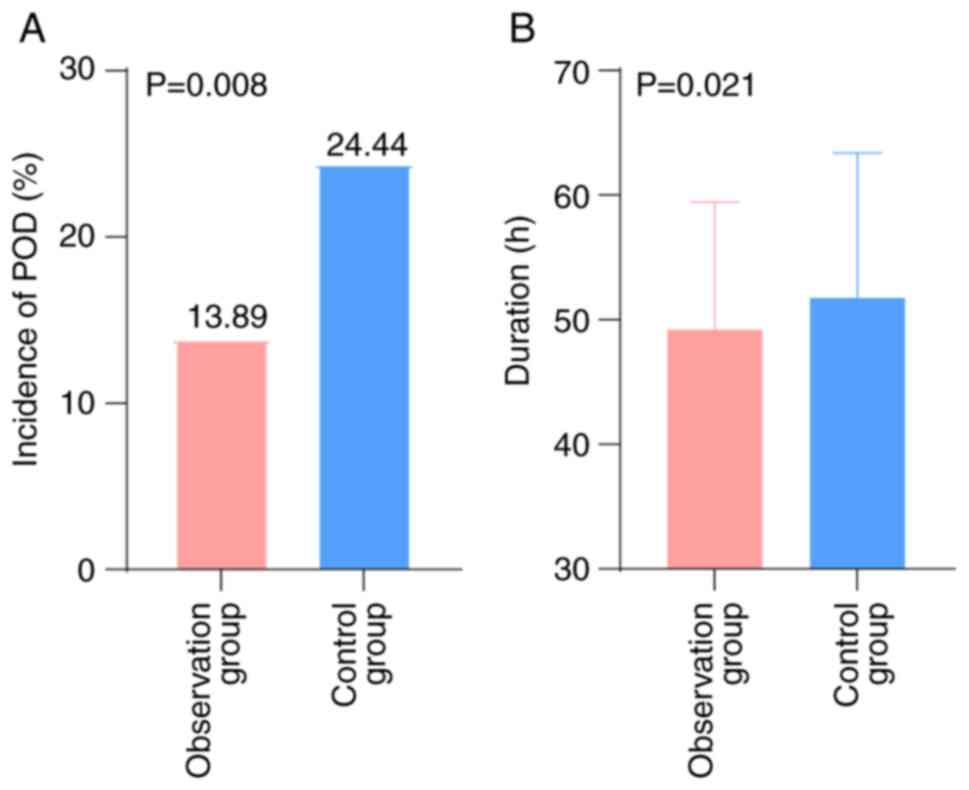
The overall clinical efficacy of remimazolam
measured by the incidence of POD was compared between the two
groups. The total incidence of POD in the observation group was
significantly lower than that in the control group (13.89% vs.
24.44%; P=0.008) (Table II;
Fig. 2), and the duration of POD
was also significantly shorter (49.17±10.28 h vs. 51.74±11.65 h;
P=0.021). However, no statistically significant difference was
observed in the onset time of POD between the groups (Table II).
 | Table IIComparison of the incidence of
POD. |
Table II
Comparison of the incidence of
POD.
| POD | Observation group
(n=180) | Control group
(n=225) | P-value |
|---|
| Incidence, n
(%) | 25 (13.89) | 55 (24.44) | 0.008 |
| Onset time, h | 25.19±8.11 | 26.11±8.47 | 0.269 |
| Duration time,
h | 49.17±10.28 | 51.74±1.65 | 0.021 |
Comparison of anxiety
After follow-up, anxiety scores were found to be
similar between the two groups (Table III). However, the anxiety score 1
day post-surgery was significantly lower in the observation group
(P=0.015) (Table III).
 | Table IIIComparison of anxiety. |
Table III
Comparison of anxiety.
| Anxiety | Observation group
(n=180) | Control group
(n=225) | P-value |
|---|
| 1 day before
operationa | 35 (26, 45) | 36 (25, 47) | 0.670 |
| 1 day after
operationb | 6 (5, 9) | 5 (7, 10) | 0.015 |
Comparison of VAS scores and pain
Regarding pain management, no significant
differences were found in the VAS pain scores 1 or 3 days
post-surgery, nor in the incidence of rescue analgesia between the
groups (Table IV). By contrast, 2
days post-surgery the VAS pain score was significantly lower in the
observation group than in the control group (P=0.046).
 | Table IVComparison of VAS scores and
pain. |
Table IV
Comparison of VAS scores and
pain.
| Variable | Observation group
(n=180) | Control group
(n=225) | P-value |
|---|
| VAS 1 day after
operation | 4 (2, 6) | 4 (2, 6) | 0.442 |
| VAS 2 days after
operation | 2 (1, 3) | 2 (1, 5) | 0.046 |
| VAS 3 days after
operation | 3 (2, 4) | 3 (2, 4) | 0.339 |
| Remedial analgesia,
n (%) | 31 (17.22) | 47 (20.89) | 0.352 |
Comparison of complications
To evaluate the safety of remimazolam, the incidence
of perioperative complications was compared. The observation group
exhibited a significantly lower incidence of intraoperative
hypertension (P<0.05). No significant differences were found in
the incidences of intraoperative hypotension, bradycardia,
hypoxemia, or postoperative nausea and vomiting between the two
groups (Table V).
 | Table VComparison of complications. |
Table V
Comparison of complications.
| Complication | Observation group
(n=180) | Control group
(n=225) | P-value |
|---|
| Hypertension | 11 (6.11) | 30 (13.33) | 0.017 |
| Hypotension | 19 (10.56) | 34 (15.11) | 0.177 |
| Bradycardia | 16 (8.89) | 17 (7.56) | 0.626 |
| Hypoxemia | 6 (3.33) | 10 (4.44) | 0.568 |
| Nausea | 13 (7.22) | 19 (8.44) | 0.650 |
| Vomiting | 9 (5.00) | 12 (5.33) | 0.881 |
Discussion
In the present study, it was observed that the
incidence of POD was significantly lower in elderly patients with
hip fractures under subarachnoid block in the remimazolam group
compared with that in the control group. However, there were no
significant differences between the two groups regarding the onset
time of POD. The anxiety scores on the 1st postoperative day and
the incidence of intraoperative hypertension were also
significantly reduced in the remimazolam group compared with those
in the control group. No significant differences were noted in the
incidence of intraoperative hypotension, bradycardia, hypoxemia, or
postoperative nausea and vomiting between the two groups.
POD is a common complication in elderly patients
with hip fractures undergoing subarachnoid block, particularly
those undergoing hip replacement surgery (19-21).
A previous study reported that the incidence of POD in elderly
patients ranges from 4-53%, making POD one of the most prevalent
surgical complications in this age group (22). Consistent with these findings, the
present study revealed a high incidence of POD in elderly patients
undergoing geriatric hip surgery. Elderly individuals face a
notably increased risk of POD after hip surgery; however, the
specific reason is unknown. Notably, POD can have profound
implications for long-term prognosis, such as an increased
incidence of dementia (2,23). The onset of POD is influenced by
various factors, including advanced age, hip fracture surgery (as
compared with elective hip surgery) (24,25),
and preoperative cognitive impairment or delirium (19). POD not only impacts short-term
recovery but can also contribute to long-term cognitive decline and
other complications (26), such as
urinary tract infections. Research has indicated that POD is
associated with extended hospital stays, increased medical
complications and poorer short-term functional outcomes, such as
psychological well-being (22).
Therefore, effective management of POD should emphasize prevention
and early detection. While the efficacy of medical preventive
interventions is limited, a multidisciplinary approach, including
adequate hydration, optimized analgesia, minimizing polypharmacy,
active physical therapy and early identification of delirium
symptoms, has been shown to effectively reduce the incidence of POD
(22).
Progress has been made in the treatment and
pharmacological management of POD in elderly patients undergoing
hip surgery (27,28). Multidisciplinary comprehensive care
is widely regarded as one of the most effective strategies for
preventing and treating POD. By predicting perioperative risks,
avoiding certain medications and providing integrated geriatric
care, the incidence of POD can be substantially reduced (29). Early identification and
intervention are critical for improving patient outcomes; therefore
employing validated, user-friendly bedside diagnostic tools, such
as the CAM-CR scale, to screen for POD allows healthcare
professionals to promptly detect and manage delirium (30). Research into pharmacological
prophylaxis is also advancing; among pharmacological interventions,
dexmedetomidine and multimodal analgesia have shown potential in
managing POD; however, the adverse effects of antipsychotic drugs
must be considered (29). While
routine drug use for prevention is not yet recommended, the
effectiveness of multicomponent preventive strategies has been well
established and should be incorporated into clinical practice
(30). Despite evidence from
numerous clinical studies demonstrating that drugs such as
dexmedetomidine reduce POD, some studies have found them
ineffective or even associated with an increased incidence of
complications, such as hypotension and bradycardia (31-33).
A randomized clinical trial examining dexmedetomidine use in
elderly patients undergoing major elective noncardiac surgery found
no notable reduction in POD with its intraoperative use (31). This study suggested that while
dexmedetomidine was linked to lower delirium rates in ICUs, its use
during surgery did not yield the same benefits, indicating that the
timing of administration may be a key factor in determining its
efficacy. Similarly, a study on oral and maxillofacial surgery
demonstrated that perioperative dexmedetomidine use did not notably
impact the incidence of POD (29).
Although dexmedetomidine was associated with reduced postoperative
pain and improved sleep quality, it did not markedly prevent
delirium. Therefore, identifying new anti-delirium agents and
establishing evidence-based clinical guidelines remains
critical.
Remimazolam, a novel ultrashort-acting
benzodiazepine, primarily induces rapid sedation and anesthesia by
selectively binding to GABAA receptors. Compared with traditional
benzodiazepines, remimazolam offers a faster onset and shorter
recovery time, providing clinical advantages (34,35).
The pharmacological properties of remimazolam make it suitable for
a range of clinical applications, including as a sedative and
anti-epileptic medication. Remimazolam provides effective sedation
without prolonging its duration of action, facilitating quicker
recovery and earlier discharge of patients (35). In patients undergoing cardiac
surgery, remimazolam has been shown to ensure good hemodynamic
stability, with minimal impact on recovery and extubation times
postoperatively (36). Wang et
al (37) conducted a
meta-analysis of randomized controlled trials, and the results
suggested that remimazolam may be safer for elderly patients than
other sedatives, as the risk of POD following general anesthesia or
sedation was not increased, and it may improve cognitive function
after surgery. A recent randomized controlled trial also
demonstrated that remimazolam, used in surgeries for lower
extremity fractures in older adults, may increase the power
spectrum density of the α band in frontal brain waves, thus
improving postoperative cognitive function compared with midazolam
(38). Furthermore, compared with
other anesthetic agents such as propofol, remimazolam poses a lower
risk of cardiovascular and respiratory depression (39).
In the present study, remimazolam significantly
reduced anxiety scores, which may be attributed to its superior
ability to alleviate pain and reduce inflammatory responses
(40). Mao et al (41) similarly found that preoperative
administration of remimazolam and estazolam, whether used
individually or in combination, effectively eased preoperative
anxiety during laparoscopic cholecystectomy. In the present study,
the difference in anxiety scores between the two groups may be
related to the differences in analgesic effects of different drugs.
Patients with anxiety have a higher risk of developing POD after
surgery (42). Gu et al
(43) reported that the
perioperative sleep quality of patients with preoperative anxiety
was worse than that of patients without preoperative anxiety.
Furthermore, high preoperative anxiety is related to more severe
postoperative pain and an increased requirement for analgesia.
Shimony et al (44)
reported that perioperative use of twice-daily 150 mg pregabalin
attenuated preoperative anxiety, improved sleep quality, and
reduced postoperative pain scores and analgesic usage without
increasing the rate of adverse effects, and indicated that anxiety
may reduce the occurrence of POD. Ren et al (45) reported that preoperative anxiety
may help to predict the risk of POD in elderly patients undergoing
elective orthopedic surgery; therefore relieving preoperative
anxiety could be a new target for preventive interventions to
reduce POD. Given that the pharmacological profile of remimazolam
reduces the likelihood of sedative-induced POD, this warrants
attention for the potential of remimazolam in preventing and
treating POD and postoperative anxiety.
Remimazolam has potential advantages in reducing the
incidence of POD. Firstly, its effectiveness in preventing POD has
been preliminarily established; a previous study comparing
remimazolam to other anesthetic drugs, including propofol, in
elderly patients found that the incidence of POD was significantly
lower in those receiving remimazolam (6). Additionally, remimazolam has been
shown to improve postoperative cognitive dysfunction, likely due to
its anti-inflammatory and neuroprotective effects (46). Secondly, the pharmacological
mechanism of remimazolam provides further theoretical support for
its application in delirium prevention; research has indicated that
remimazolam protects the nervous system by modulating
neuroinflammatory responses and reducing the release of
inflammatory factors, such as IL-6, IL-1β and tumor necrosis
factor-α (46). Furthermore,
remimazolam has been found to improve sleep patterns and reduce the
incidence of postoperative sleep disorders, which are critical
factors in preventing delirium (47). Finally, the safety and efficacy of
remimazolam have been validated in clinical use. Compared with
traditional anesthetics, remimazolam provides better hemodynamic
stability and a lower incidence of adverse reactions (8). These characteristics position it as a
promising agent for preventing delirium. Therefore, remimazolam
holds considerable potential for POD prevention through mechanisms
such as regulating neuroinflammation and improving sleep rhythms.
However, further large-scale clinical trials are necessary to
confirm its efficacy and safety.
The present study does have several limitations. It
was a retrospective, single-center study, which inherently carries
the risk of selection bias. Due to the substantial differences in
treatment and sedation regimens in the control group, which could
impact the results, future studies should aim for a uniform
treatment regimen. Additionally, larger sample sizes are required
to study POD more comprehensively, and large-scale, multi-center
randomized controlled trials with expanded sample sizes are crucial
for validation. We are currently registering and conducting a large
sample size, multi-center randomized controlled trial study.
In conclusion, continuous intraoperative infusion of
remimazolam may reduce the incidence of POD in elderly patients
undergoing hip fracture surgery with subarachnoid block, likely due
to its ability to alleviate intraoperative anxiety. Furthermore,
remimazolam did not increase the incidence of perioperative
complications; therefore, the clinical effects of remimazolam in
preventing delirium are both safe and effective. However, further
extensive multicenter randomized controlled trials are essential to
substantiate these findings.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
QZ, LZ and BS contributed to the conception and
design of the study. QZ and LZ were responsible for data collection
and statistical analysis. QZ and BS wrote the initial draft of the
manuscript. QZ revised the manuscript, managed the project,
coordinated the study and provided final approval for the version
to be published. All authors confirm the authenticity of all the
raw data, contributed to manuscript revision, and read and approved
the final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by The Ethics
Committee of the 904th Hospital of the Joint Logistics Support
Force, People's Liberation Army of China (approval no. 2024-002)
and was conducted in accordance with the principles set forth in
The Declaration of Helsinki. Written informed consent was obtained
from patients or their immediate family members.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Goldberg TE, Chen C, Wang Y, Jung E,
Swanson A, Ing C, Garcia PS, Whittington RA and Moitra V:
Association of delirium with long-term cognitive decline: A
meta-analysis. JAMA Neurol. 77:1373–1381. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chen J, Wang Y, Hu X, Li M, Xiong K, Zhang
Z and Chen Q: The role of statins in the management of delirium:
Recent advances. CNS Neurol Disord Drug Targets. 20:203–215.
2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Saczynski JS, Marcantonio ER, Quach L,
Fong TG, Gross A, Inouye SK and Jones RN: Cognitive trajectories
after postoperative delirium. N Engl J Med. 367:30–39.
2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Redelmeier DA, Manzoor F and Thiruchelvam
D: Association between statin use and risk of dementia after a
concussion. JAMA Neurol. 76:887–896. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wang M, Liu J, Liu W, Zhang X, Zhang G,
Sun L, Bi Y, Wang H and Dong R: Effectiveness of perioperative
remimazolam in preventing postoperative delirium: A systematic
review and meta-analysis. Eur J Med Res. 30(122)2025.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Fujimoto D, Obata N and Mizobuchi S:
Effectiveness of remimazolam in preventing postoperative delirium
in elderly patients with proximal femoral fractures. J Anesth.
38:475–482. 2024.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Xue X, Ma X, Zhao B, Liu B, Zhang J, Li Z,
Li H, Liu X and Zhao S: The impact of remimazolam compared to
propofol on postoperative delirium: A systematic review and
meta-analysis. Minerva Anestesiol. 91:70–79. 2025.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Suga M, Yasuhara J, Watanabe A, Takagi H,
Kuno T, Nishimura T, Ijuin S, Taira T, Inoue A, Ishihara S, et al:
Postoperative delirium under general anaesthesia by remimazolam
versus propofol: A systematic review and meta-analysis of
randomised controlled trials. J Clin Anesth.
101(111735)2025.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yang JJ, Lei L, Qiu D, Chen S, Xing LK,
Zhao JW, Mao YY and Yang JJ: Effect of remimazolam on postoperative
delirium in older adult patients undergoing orthopedic surgery: A
Prospective randomized controlled clinical trial. Drug Des Devel
Ther. 17:143–153. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Aoki Y, Kurita T, Nakajima M, Imai R,
Suzuki Y, Makino H, Kinoshita H, Doi M and Nakajima Y: Association
between remimazolam and postoperative delirium in older adults
undergoing elective cardiovascular surgery: A prospective cohort
study. J Anesth. 37:13–22. 2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Glumac S, Kardum G, Sodic L, Supe-Domic D
and Karanovic N: Effects of dexamethasone on early cognitive
decline after cardiac surgery: A randomised controlled trial. Eur J
Anaesthesiol. 34:776–784. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lee H, Kim K and Lee C: Remimazolam-based
anesthesia and systemic inflammatory biomarkers in relation to
postoperative delirium in elderly patients: A retrospective cohort
study. Medicina (Kaunas). 61(1023)2025.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kanatas A, Gorton H, Smith AB, Mannion C,
Ong TK and Mitchell D: ASA grade and disease-free mortality in head
and neck cancer patients: A prospective study. Br J Oral Maxillofac
Surg. 48:591–593. 2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kim M, Heo D, Kim S, Lee Y, Kim YS, Sung W
and Kim HJ: Cognitive impairment screening test in Korea as a
screening tool for dementia: The correlation study of subtest
scores with Korean version of the mini mental state examination 2nd
edition. Dement Neurocogn Disord. 24:126–134. 2025.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gould D, Kelly D, Goldstone L and Gammon
J: Examining the validity of pressure ulcer risk assessment scales:
Developing and using illustrated patient simulations to collect the
data. J Clin Nurs. 10:697–706. 2001.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Wong CL, Holroyd-Leduc J, Simel DL and
Straus SE: Does this patient have delirium?: Value of bedside
instruments. JAMA. 304:779–786. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Guillén-Riquelme A and Buela-Casal G:
Meta-analysis of group comparison and meta-analysis of reliability
generalization of the state-trait anxiety inventory questionnaire
(STAI). Rev Esp Salud Publica. 88:101–112. 2014.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
18
|
Pachana NA, Byrne GJ, Siddle H, Koloski N,
Harley E and Arnold E: Development and validation of the geriatric
anxiety inventory. Int Psychogeriatr. 19:103–114. 2007.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lee SJ, Jung SH, Lee SU, Lim JY, Yoon KS
and Lee SY: Postoperative delirium after hip surgery is a potential
risk factor for incident dementia: A systematic review and
meta-analysis of prospective studies. Arch Gerontol Geriatr.
87(103977)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kappenschneider T, Maderbacher G, Weber M,
Greimel F, Holzapfel D, Parik L, Schwarz T, Leiss F, Knebl M,
Reinhard J, et al: Special orthopaedic geriatrics (SOG)-a new
multiprofessional care model for elderly patients in elective
orthopaedic surgery: A study protocol for a prospective randomized
controlled trial of a multimodal intervention in frail patients
with hip and knee replacement. BMC Musculoskelet Disord.
23(1079)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
HIP ATTACK Investigators. Accelerated
surgery versus standard care in hip fracture (HIP ATTACK): An
international, randomised, controlled trial. Lancet. 395:698–708.
2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Rizk P, Morris W, Oladeji P and Huo M:
Review of postoperative delirium in geriatric patients undergoing
hip surgery. Geriatr Orthop Surg Rehabil. 7:100–105.
2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Krzych ŁJ, Pluta MP, Putowski Z and Czok
M: Investigating association between intraoperative hypotension and
postoperative neurocognitive disorders in non-cardiac surgery: A
comprehensive review. J Clin Med. 9(3183)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sieber FE, Mears S, Lee H and Gottschalk
A: Postoperative opioid consumption and its relationship to
cognitive function in older adults with hip fracture. J Am Geriatr
Soc. 59:2256–2262. 2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kalisvaart KJ, Vreeswijk R, de Jonghe JF,
van der Ploeg T, van Gool WA and Eikelenboom P: Risk factors and
prediction of postoperative delirium in elderly hip-surgery
patients: Implementation and validation of a medical risk factor
model. J Am Geriatr Soc. 54:817–822. 2006.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Olofsson B, Lundström M, Borssén B, Nyberg
L and Gustafson Y: Delirium is associated with poor rehabilitation
outcome in elderly patients treated for femoral neck fractures.
Scand J Caring Sci. 19:119–127. 2005.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chen Z, Liu YY, Hu Q, Wang JS, Cao RY, Yu
ST, Lu F, Zhong ML, Liang WD and Wang L: Effect of ciprofol on
postoperative delirium in elderly patients undergoing hip surgery:
A randomized controlled trial. Drug Des Devel Ther. 19:6207–6218.
2025.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Geng P, Shang Z, Cheng F, Zhang Y, Deng X,
Chen X, Zhan L, Zheng L and Liu X: Preoperative low-dose
dexmedetomidine reduces postoperative delirium in elderly patients
with hip fracture under spinal anesthesia: A randomized, double
blind, controlled clinical study. J Clin Anesth.
105(111897)2025.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Chen Y, Liang S, Wu H, Deng S, Wang F,
Lunzhu C and Li J: Postoperative delirium in geriatric patients
with hip fractures. Front Aging Neurosci.
14(1068278)2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Popp J and Arlt S: Prevention and
treatment options for postoperative delirium in the elderly. Curr
Opin Psychiatry. 25:515–521. 2012.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Deiner S, Luo X, Lin HM, Sessler DI,
Saager L, Sieber FE, Lee HB and Sano M: and the Dexlirium Writing
Group. Jankowski C, et al: Intraoperative infusion of
dexmedetomidine for prevention of postoperative delirium and
cognitive dysfunction in elderly patients undergoing major elective
noncardiac surgery: A randomized clinical trial. JAMA Surg.
152(e171505)2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Liu T, Tuo J, Wei Q, Sun X, Zhao H, Zhao X
and Qu M: Effect of perioperative dexmedetomidine infusion on
postoperative delirium in elderly patients undergoing oral and
maxillofacial surgery: A randomized controlled clinical trial. Int
J Gen Med. 15:6105–6113. 2022.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Halpin E, Inch H and O'Neill M:
Dexmedetomidine's relationship to delirium in patients undergoing
cardiac surgery: A systematic review. Crit Care Nurs Q. 43:28–38.
2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kilpatrick GJ: Remimazolam: Non-clinical
and clinical profile of a new sedative/anesthetic agent. Front
Pharmacol. 12(690875)2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Paton DM: Remimazolam: A short-acting
benzodiazepine for procedural sedation. Drugs Today (Barc).
57:337–346. 2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Muncan B and Bennett-Guerrero E:
Remimazolam use in cardiac anesthesia: A narrative review. J
Cardiothorac Vasc Anesth. 38:3179–3187. 2024.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Wang Y, Gou ZH, Wang GM, Ye LH, Chen L and
Wang Q: Association of remimazolam with delirium and cognitive
function in elderly patients undergoing general anesthesia or
procedural sedation: A meta-analysis of randomized controlled
trials. Front Med (Lausanne). 12(1567794)2025.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Wu H, Tian S, Ma H, Zhou W, Feng S, Meng
L, Ou J, Xu F and Zhang Z: Effects of remimazolam on intraoperative
frontal alpha band power spectrum density and postoperative
cognitive function in older adults undergoing lower extremity
fractures surgeries: A randomized controlled trial. Clin Interv
Aging. 19:2195–2205. 2024.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Zhang H, Li H, Zhao S and Bao F:
Remimazolam in general anesthesia: A comprehensive review of its
applications and clinical efficacy. Drug Des Devel Ther.
18:3487–3498. 2024.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Li S, Sana S and Wang D: Remimazolam
mitigates oxidative stress response in patients undergoing one-lung
ventilation. Front Surg. 12(1456827)2025.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Mao S, Gao R, Huang Y, He H, Yao J and
Feng J: Effect of remimazolam combined with estazolam on anxiety
levels and postoperative gastrointestinal function recovery in
patients undergoing laparoscopic cholecystectomy surgery. Eur J Med
Res. 30(118)2025.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Li CW, Xue FS and Hou HJ: In reference to
effects of preoperative anxiety on postoperative delirium in
elderly patients [letter]. Clin Interv Aging. 16:799–800.
2021.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Gu X, Zhang Y, Wei W and Zhu J: Effects of
preoperative anxiety on postoperative outcomes and sleep quality in
patients undergoing laparoscopic gynecological surgery. J Clin Med.
12(1835)2023.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Shimony N, Amit U, Minz B, Grossman R,
Dany MA, Gonen L, Kandov K, Ram Z and Weinbroum AA: Perioperative
pregabalin for reducing pain, analgesic consumption, and anxiety
and enhancing sleep quality in elective neurosurgical patients: A
prospective, randomized, double-blind, and controlled clinical
study. J Neurosurg. 125:1513–1522. 2016.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Ren A, Zhang N, Zhu H, Zhou K, Cao Y and
Liu J: Effects of preoperative anxiety on postoperative delirium in
elderly patients undergoing elective orthopedic surgery: A
prospective observational cohort study. Clin Interv Aging.
16:549–557. 2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Zhou L, Shi H, Xiao M, Liu W, Wang L, Zhou
S, Chen S, Wang Y and Liu C: Remimazolam attenuates
lipopolysaccharide-induced neuroinflammation and cognitive
dysfunction. Behav Brain Res. 476(115268)2025.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Yaqiu L, Heng Z, Ruimin W and Xuri W:
Effects of remimazolam and propofol on sleep rhythm and delirium
after spinal surgery in elderly patients. Perioper Med (Lond).
14(18)2025.PubMed/NCBI View Article : Google Scholar
|