Introduction
Acute coronary syndrome (ACS) refers to cardiac
acute ischemic syndrome, caused by thrombosis, resulting from the
rupture or erosion of unstable atheromatous plaques in the coronary
arteries (1). It is classified
into non-ST-segment elevation myocardial infarction (NSTEMI), STEMI
and unstable angina pectoris (UA) (1,2). In
clinical settings, UA and NSTEMI present with similar clinical
manifestations and electrocardiographic (ECG) features, such as
ST-segment depressions and T-wave inversion, and are thus together
considered as non-ST-segment-elevation (NSTE)-ACS (3). Both STEMI and NSTEMI are
characterized by myocardial injury or necrosis, typically indicated
by significantly elevated levels of cardiac biomarkers, such as
troponin I (TnI) and troponin T (TnT) (4,5).
Compared with patients with NSTEMI, patients with STEMI more
frequently exhibit complete occlusion of the culprit artery, a
higher incidence of transmural ischemia, a larger infarcted
myocardial area and worse short-term diagnosis compared with
patients with NSTEMI (2).
Globally, STEMI is the single most common cause of
sudden death (4,6). It accounts for 1.8 million deaths
annually (20% of all deaths) in Europe alone, with a decreasing
trend in its relative incidence and a concomitant rise in the
incidence of NSTE-ACS (4).
According to published data, the incidence of ACS varies by age and
sex. In individuals younger than 60 years, ACS occurs 3 to 4 times
more frequently in males than in females, whereas females
constitute the majority of patients over the age of 75(4). The risk of myocardial infarction (MI)
has been extensively studied and numerous factors, including
increased body-mass index, low-density lipoproteins, C-reactive
protein (CRP), diabetes, hypertension, smoking and hyperlipidemia
are regarded as being associated with increased susceptibility to
MI (7,8). Patients typically present with
symptoms such as chest pain, epigastric pain, radiating pain to the
neck or shoulder, and shortness of breath (6,9,10).
Acute myocardial infarction (AMI) has the highest mortality rate
within hours of onset, and early diagnosis and treatment initiation
are key interventions for patients with ACS (6). Notably, the 12-lead ECG and cardiac
troponins (cTn) are the primary diagnostic tools for AMI (6,11).
However, only 5% of patients who present with acute chest pain and
undergo ECG are diagnosed with STEMI (6). In addition, troponin is used to
evaluate NSTE-ACS in patients with chest pain without pre-hospital
ST-segment elevation. Most of these patients are found to have
negative troponin levels and are subsequently diagnosed with
unstable angina, indicating that troponin may not be an optimal
biomarker for NSTE-ACS (6,12).
In clinical practice, patients with suspected ACS
are often directly admitted to emergency departments (EDs). Yet,
the majority of these patients are not ultimately diagnosed with
ACS and could be managed at general care centers to avoid
unnecessary ED congestion, costs and time delays (5,13).
To solve this problem, numerous biomarkers, such as
high-sensitivity cTn (hs-cTn), N-terminal prohormone of brain
natriuretic peptide (NT-proBNP), hsCRP and D-dimer, have been
clinically applied for risk stratification based on major adverse
cardiac events (MACE), enabling appropriate treatment decisions and
timely, safe discharge (9-12).
In addition, numerous studies have evaluated the diagnostic and
prognostic value of emerging biomarkers, including soluble
suppression of tumorigenicity 2 protein (sST2), which is a
biomarker for cellular stress and injury (14-16),
hs-cTnT, a biomarker of MI (5,9,13)
and lipoprotein-associated phospholipase A2 (Lp-PLA2), a biomarker
of plaque inflammation (8,10,17),
in the classification and risk stratification of ACS. Elevated
serum levels of sST2 have been shown to independently predict
future heart failure, cardiovascular events and mortality (18), while increased hs-cTnT levels are
associated with a higher risk of MACE (9). Lp-PLA2 has demonstrated limited
utility as a standalone biomarker for cardiovascular events, but it
could offer additional prognostic information when assessed at a
time-point significantly distant from the acute coronary event
(8).
The diagnosis of STEMI and NSTE-ACS determines the
choice and timing of ACS treatment and management (17). However, the diagnostic, prognostic
and classificatory value of reported biomarkers in ACS remains
largely undetermined. Published studies reported inconsistent
results for various kinds of biomarkers in ACS classification. A
total of 11 biomarkers, such as ST2 protein and fibroblast growth
factor, have been reported to exhibit elevated concentrations in
STEMI and NSTEMI, respectively, and may effectively differentiate
between these two MI types. However, these findings lack clinical
reliability due to their reliance on registry data (2). Patients with NSTE-ACS with high sST2
levels had a ~3-fold higher risk of cardiovascular disease (CVD)
and heart failure (HF) compared to patients with STEMI within the
following year (15). The upper
reference limits, as well as age and sex-based thresholds for these
11 biomarkers and other biomarkers in ACS classification is still
uncertain (15,19). Therefore, assessing the performance
of these biomarkers for distinguishing STEMI and NSTEMI is most
important in the management of patients with ACS. Of them, the
hs-cTnT, sST2 and Lp-PLA2 biomarkers are most focused on in
clinical practice; therefore, the present study investigated the
role of these three emerging biomarkers in the classification of
ACS.
Patients and methods
Patients
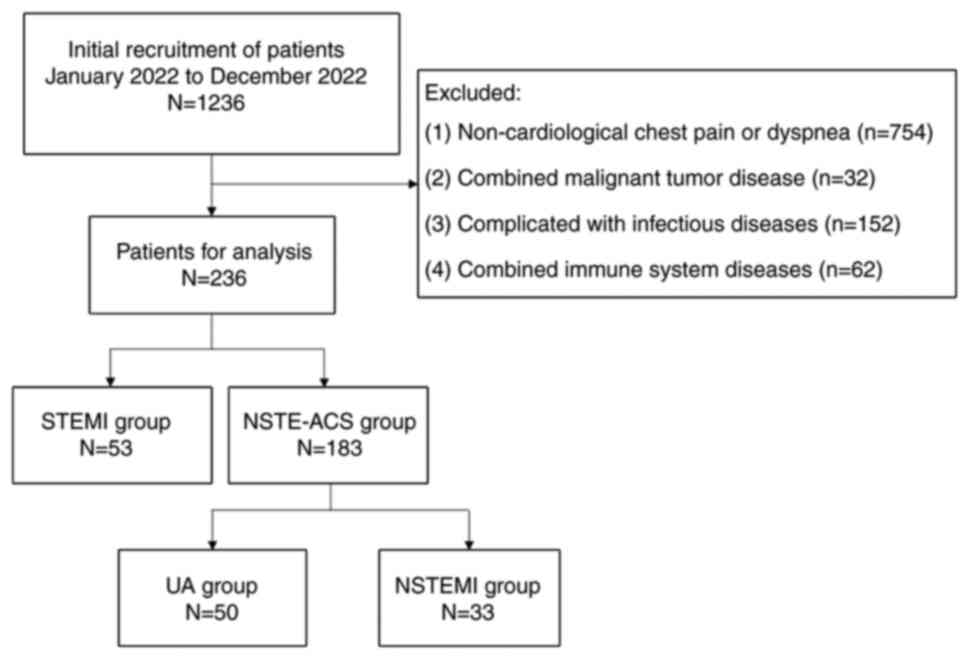
A total of 1,236 patients with suspected ACS
encountered at Nanjing First Hospital (Nanjing, China) between
January 2022 and December 2022 were enrolled in the present study.
Eligible patients were identified according to the following
inclusion and exclusion criteria. The inclusion criterion was
patients suspected of having ACS by clinical doctors based on their
clinical symptoms, such as chest pain and dyspnea. The exclusion
criteria were as follows: i) Non-cardiological chest pain or
dyspnea; ii) combined malignant tumor disease; iii) cases
complicated with infectious diseases; and iv) coexisting immune
system diseases. All coronary angiograms (CAG) were independently
reviewed by two cardiologists and a diagnosis of ACS was
established based on a combination of clinical symptoms, ECG
changes, cardiac biomarkers and CAG findings indicating significant
stenosis (≥50%) in one or more coronary arteries, following the
diagnostic criteria recommended by the European Society of
Cardiology guidelines (20-22).
This retrospective study was approved by the Institutional Review
Board of Nanjing First Hospital (approval no. KY20250714-KS-01),
which waived the requirement for individual patient consent.
Finally, a total of 183 patients (150 with UA and 33 with NSTEMI)
were diagnosed as having NSTE-ACS, and 53 patients were diagnosed
with STEMI. The patient inclusion flow-chart is shown in Fig. 1. Among the 263 patients included,
175 (74.15%) were male and 61 (25.85%) were female. The median age
was 59 years (range, 31-91 years).
Instruments and reagents
Heparin-anticoagulated peripheral blood and serum
samples were collected for hs-cTnT detection, which was detected
with an electrochemiluminescence analyzer (Cobas e411; Roche
Diagnostics) and non-anticoagulated samples were used to obtain
serum for the detection of sST2 and Lp-PLA2 via chemiluminescence
analyzers (CL2000; Beijing Leadman; and 411; Nanjing Norman,
respectively).
Statistical analysis
All statistical analyses were performed using SPSS
20.0 software (IBM Corp.). The Kolmogorov-Smirnov test was used to
assess the normality of the measurement data. The measurement data
in accordance with the normal distribution were presented as the
mean ± standard deviation. Student's t-test was used to compare the
groups. Non-normally distributed measurement data were expressed as
the median (interquartile range) and the Mann-Whitney U-test was
used to analyze differences between groups. Enumeration data were
expressed as n (%) and the χ2 test was used for
intergroup comparison. Univariate logistic regression model was
conducted to evaluate the impact of individual factors on ACS
classification. The Hosmer-Lemeshow test was performed to evaluate
the fit of the regression model. Receiver operating characteristic
(ROC) curves were plotted to calculate the diagnostic value of
individual and combined biomarkers for ACS classification.
Furthermore, the DeLong test (23)
was applied to compare the AUCs of different biomarkers. A
two-sided P<0.05 was considered to indicate statistical
significance.
Results
Characteristics of patients
There was a significant difference in gender
distribution between STEMI (males/females=46:7) and NSTE-ACS
(males/females=129:54) cases (χ2=5.697, P=0.017), as
shown in Table I. However, no
significant difference was observed in age between the two groups
(STEMI: 63.60±12.90 years vs. NSTE-ACS: 65.25±11.39 years,
P=0.369). The levels of hs-cTnT [STEMI: median 1,641.00 ng/l
(interquartile range 288.15-4193.50 ng/l) vs. NSTE-ACS: median
17.08 ng/l (interquartile range 9.62-166.10 ng/l), P<0.001;
cut-off value 524 ng/l) and sST2 [STEMI: median 53.17 ng/ml
(interquartile range 28.47-154.87 ng/ml) vs. NSTE-ACS: median 16.92
ng/ml (interquartile range 12.50-25.01), P<0.001; cut-off value
29.27 ng/ml) were significantly higher in the STEMI group compared
to the NSTE-ACS group; however, no significant difference was found
in Lp-PLA2 levels between the two groups [STEMI: median 194.48
ng/ml (interquartile range 141.36-276.59 ng/ml) vs. NSTE-ACS:
median 184.26 ng/ml (interquartile range132.05-259.92), P=0.470],
as shown in Table I.
 | Table IComparison of clinical data between
NSTE-ACS group and STEMI group. |
Table I
Comparison of clinical data between
NSTE-ACS group and STEMI group.
| Group | NSTE-ACS | STEMI |
t/χ2 | P-value |
|---|
| Sex
(male/female) | 129/54 | 46/7 | 5.697 | 0.017 |
| Age, years | 65.25±11.39 | 63.60±12.90 | 0.234 | 0.369 |
| hs-cTnT, ng/l | 17.08
(9.62-166.10) | 1641.00
(288.15-4193.50) | -7.989 | <0.001 |
| sST2, ng/ml | 16.92
(12.50-25.01) | 53.17
(28.47-154.87) | -7.369 | <0.001 |
| Lp-PLA2, ng/ml | 184.26
(132.05-259.92) | 194.48
(141.36-276.59) | -0.723 | 0.470 |
Predictive value of hs-cTnT and sST2
in patients with ACS
A univariate logistic regression analysis of the
factors influencing the likelihood that the patient had NSTE-ACS or
STEMI was conducted, with the presence or absence of STEMI as the
dependent variable, and gender, age, hs-cTnT, sST2 and Lp-PLA2 as
the independent variables. The results showed that hs-cTnT [odds
ratio (OR)=1.010, 95% CI: 1.007-1.014] and sST2 (OR=1.022, 95% CI:
1.011-1.033) were predictors of STEMI, as shown in Table II. The Hosmer-Lemeshow test was
performed to evaluate the fit of the regression model and the
result (χ2=11.158, P=0.193) showed no significant
difference between the predicted and observed values, suggesting
that the model fits the data well for classifying the two ACS
groups.
 | Table IIResults of a univariate logistic
regression analysis of the factors associated with the risk of
ST-segment elevation myocardial infarction as opposed to
non-ST-segment-elevation acute coronary syndrome. |
Table II
Results of a univariate logistic
regression analysis of the factors associated with the risk of
ST-segment elevation myocardial infarction as opposed to
non-ST-segment-elevation acute coronary syndrome.
| Factor | β | P-value | OR | 95% CI |
|---|
| Sex
(male/female) | 0.242 | 0.675 | 1.273 | 0.412-3.937 |
| Agea | -0.038 | 0.050 | 0.963 | 0.928-1.000 |
|
hs-cTnTa | 0.001 | <0.001 | 1.010 | 1.007-1.014 |
| sST2a | 0.021 | <0.001 | 1.022 | 1.011-1.033 |
|
Lp-PLA2a | -0.002 | 0.312 | 0.998 | 0.995-1.002 |
Diagnostic value of hs-cTnT and sST2
in patients with ACS
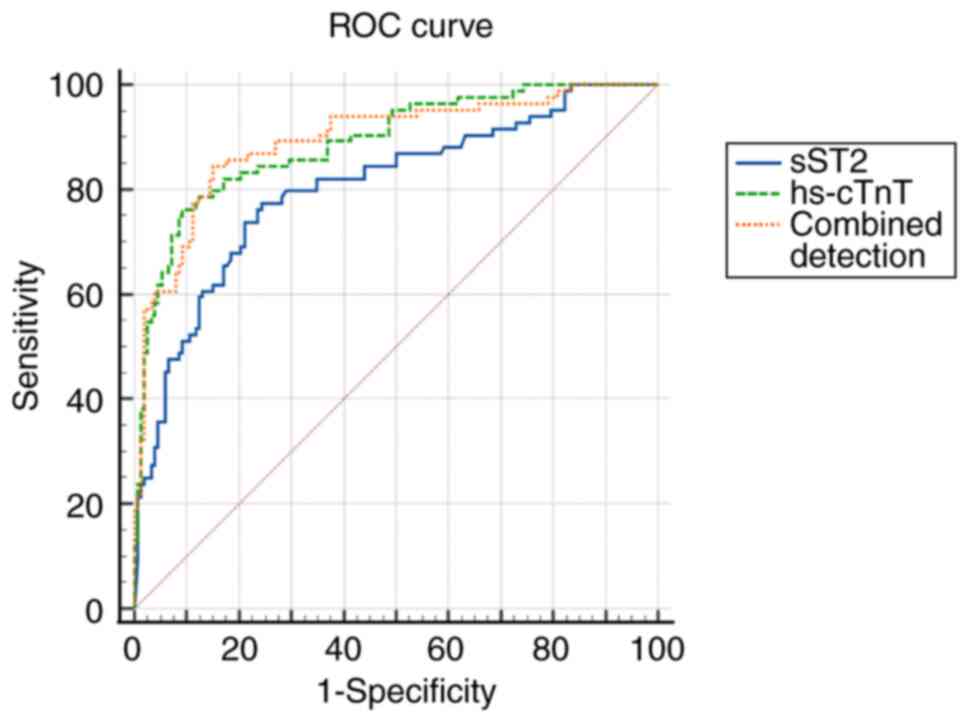
To further assess the diagnostic value of hs-cTnT
and sST2 in distinguishing STEMI from NSTE-ACS, the predictive
values for hs-cTnT and sST2 alone and in combination for
classification of the two ACS groups were assessed, and the results
revealed that hs-cTnT (AUC=0.861, cut-off value=524 ng/l, 95% CI:
0.810-0.902; specificity: 88.52%; sensitivity: 71.70%), sST2
(AUC=0.833, cut-off value=29.27 ng/ml, 95% CI: 0.779-0.878;
specificity: 83.06%, sensitivity: 75.47%) and their combination
(AUC=0.863, 95% CI: 0.812-0.904; specificity: 91.80%, sensitivity:
71.70%) could serve as diagnostic biomarkers for STEMI, as shown in
Table III and Fig. 2. Additionally, the diagnostic
efficacy of hs-cTnT (AUC=0.861, P=0.0017) and the combination of
hs-cTnT and sST2 (AUC=0.863, P<0.005) was higher than that of
sST2 alone (AUC=0.833).
 | Table IIIDiagnostic value of combined
detection of hs-cTnT and sST2 to distinguish ST-segment elevation
myocardial infarction from non-ST-segment-elevation acute coronary
syndrome. |
Table III
Diagnostic value of combined
detection of hs-cTnT and sST2 to distinguish ST-segment elevation
myocardial infarction from non-ST-segment-elevation acute coronary
syndrome.
| Variable | Cut-off value | Youden index | Sensitivity, % | Specificity, % | AUC | 95% CI | AUC P |
|---|
| hs-cTnT | 524 ng/l | 0.6022 | 71.70 | 88.52 | 0.861 | 0.810-0.902 | 0.0017 |
| sST2 | 29.27 ng/ml | 0.5853 | 75.47 | 83.06 | 0.833 | 0.779-0.878 | - |
| Combined
detection | - | 0.6350 | 71.70 | 91.80 | 0.863 | 0.812-0.904 | <0.005 |
Discussion
The present retrospective study indicated that both
sST2 and hs-cTnT demonstrated significant utility in
differentiating between STEMI and NSTE-ACS, while Lp-PLA2 was not a
valuable biomarker for the classification of the two types of MI.
We observed that the circulating levels of hs-cTnT were 96-fold
higher in STEMI than that in NSTE-ACS, providing a cut-off value of
524 ng/l to discriminate between the types of MIs. Moreover, the
serum levels of sST2 were 3-fold higher in STEMI than in NSTE-ACS,
and it could accurately classify the two types of ACS with a
cut-off value of 29.27 ng/ml. Of note, hs-cTnT and its combination
with sST2 outperformed sST2 alone in terms of diagnostic efficiency
in patients with ACS and combined detection of the two markers did
not improve the biomarkers' ability to distinguish between the two
types of ACS as compared to hs-cTnT alone.
Over decades of standardized cardiovascular disease
prevention in developed countries, the incidence of STEMI has
decreased significantly, while China has shown a rapid growth trend
(24,25). Similar to the present findings,
numerous studies have reported higher cases of STEMI in males
(63-67%) than in females (30-37%) (26,27).
This difference may be due to risk factors such as smoking,
diabetes, dyslipidemia, abdominal obesity and hypertension, which
are more prevalent in males (28).
In addition, estrogen hormone in females offers a temporary
premenopausal vascular protection, delaying the onset and severity
of atherosclerosis in women contrary to men, though this protection
declines post-menopause, allowing for the later onset of ACS events
in women. In contrast to the present results, NSTE-ACS has been
reported to be predominantly higher in females (29,30),
likely due to a higher incidence of diffuse coronary artery
disease, microvascular dysfunction and older age at ACS
presentation, factors less frequently associated with STEMI's
characteristic vessel occlusion (31). These sex-based epidemiological
patterns underscore the necessity of gender-tailored strategies for
ACS prevention, diagnosis and management.
Various guidelines and expert consensus affirm the
diagnostic and therapeutic value of myocardial markers, including
creatine kinase isoenzyme and myoglobin (CK-MB), cTnT, cTnI,
heart-type fatty acid binding protein, myosin binding protein C and
NT-proBNP, in ACS pathophysiology and guiding risk stratification
(5,14,32).
Despite the critical need to accurately and safely rule out STEMI
in patients with NSTE-ACS, the discriminative value of these
biomarkers is still unclear. The present study focused on
evaluating hs-cTnT, sST2 and Lp-PLA2 for ACS classification. The
results indicated that both hs-cTnT and sST2, individually and in
combination, effectively predicted STEMI, whereas Lp-PLA2 showed no
utility in ACS classification.
Stimulation expression gene 2 (ST2), a member of the
interleukin (IL)-1 receptor family, interacts specifically with and
IL-33 (15,16,18).
It exists mainly in 2 isoforms: ST2 and ST2L, which is divided into
transmembrane forms, and sST2 (14,18).
sST2 is a marker of stress and injury of cardiomyocytes (14,15),
whose high expression in serum has been reported to independently
predict HF, CVD events and death in both STEMI and NSTE-ACS
(14,16,18).
Numerous studies suggest that sST2, as a marker reflecting
myocardial fibrosis, inflammation and oxidative stress, is helpful
for risk stratification and prognostic evaluation of patients with
HF (33,34). For the application of sST2 in the
diagnosis of ACS, the present study established that the biomarker
had 3-fold higher expression in STEMI than NSTE-ACS, which is
similar to the findings reported by Hjort et al (2). This higher level of sST2 in STEMI is
attributed to the greater degree of myocardial damage and
dysfunction compared to NSTE-ACS (2,15).
However, Hjort et al (2)'s
conclusions were based on registry data and non-quantitative assays
with no absolute concentration measurements, limiting direct
comparison with the clinically applied cut-offs. Importantly, the
present study was conducted using clinical patient's results taken
from the hospital's database, enabling for sST2 clinical comparison
and STEMI prediction with a cut-off value of 29.27 ng/ml
(sensitivity: 75.47%, specificity: 83.06%).
cTnI and -T are proteins that are implicated in
actin-myosin interaction, produced and released by cardiomyocytes
due to stress or necrosis (35);
their elevated levels in peripheral blood indicate cardiomyocyte
damage (12,36) and are reported to be more sensitive
and specific markers of cardiomyocyte injury than CK, its CK-MB and
myoglobin, which was once considered the gold standard for
myocardial injury (19). However,
conventional cTn assays have the drawback of delayed elevation and
require serial sampling over 6-9 h, limiting their sensitivity at
AMI presentation (19,25). hs-cTn assays were developed to
detect low cTn concentrations at or below concentrations
corresponding to the 99th percentile value of a normal reference
population to enable the diagnosis of an ongoing myocardial injury
in stable patients and even seemingly healthy populations (19). Giannitsis et al (7) also found that the evaluation of
hs-cTnT was a more accurate approach for troponin detection in
patients with NSTE-ACS than the conventional cTnT or -I assay. In
the present study, a 96-fold higher median value of hs-cTnT in
STEMI than in NSTE-ACS was observed, which can be associated with
the higher incidence of transmural ischemia and a larger area of
infarction in STEMI that increase cardiomyocyte stress, producing
more hs-cTnT in response than in patients with NSTE-ACS (2,35,37).
hs-cTnT, when used alone and in combination with sST2 showed higher
potential to discriminate STEMI compared with sST2 alone. Although
the combined model yielded a numerically higher AUC than hs-cTnT
alone (0.863 vs. 0.861), DeLong's test showed no statistically
significant difference (P=0.849). The estimated ΔAUC (0.002)
indicates that any incremental discrimination, if present, is
likely very small. Detecting such a modest effect generally
requires substantially larger sample sizes and event counts than
those yielded in the present study. Accordingly, the current
analysis may be underpowered and the absence of statistical
significance should not be overinterpreted as evidence of no
effect. Future work with larger cohorts and/or external validation
is warranted to clarify whether the addition of variables to
hs-cTnT provides statistically and clinically meaningful
improvement.
Lp-PLA2 is a biomarker of plaque inflammation whose
circulating levels are associated with changes in coronary plaque
volume (10,17). It has been shown that there is a
link between Lp-PLA2 levels and the severity of coronary artery
disease (38). Zhao et al
(39) concluded that a higher
serum Lp-PLA2 activity level is associated with a more severe
degree of coronary artery disease. Similarly, a study by Möckel
et al (12) revealed that
Lp-PLA2 is an effective independent marker for risk stratification,
which proved to be superior to CRP and the Thrombolysis in
Myocardial Infarction (TIMI) risk score (12). Lp-PLA2 was reportedly higher in
NSTE-ACS than STEMI (40), but its
sensitivity and specificity in differentiating between the two ACS
subtypes was relatively low (41).
Similarly, in the present study, there was no significant
difference in Lp-PLA2 serum levels between STEMI and NSTE-ACS,
showing low discriminative power. These findings indicate that
Lp-LPA2 is only a biomarker of atherosclerotic burden and chronic
vascular inflammation rather than acute plaque rupture or
myocardial injury, which are critical in distinguishing between
STEMI and NSTE-ACS (40,41); hence, it is not an applicable
marker in ACS classification.
To the best of our knowledge, the present study is
the first retrospective cohort study demonstrating the potential of
hs-cTnT and sST2 to discriminate between STEMI and NSTE-ACS, both
independently and in combination. However, despite these remarkable
findings, the present study has certain limitations. As a
single-center retrospective study, it may be subject to inherent
biases and limited external validity. No adjustments were made for
sociodemographic factors, clinical characteristics or medication
use, which may affect the absolute diagnostic power. Notably, this
study focused solely on the etiologic classification of ACS and the
findings were independent of disease severity. Although NSTE-ACS is
clinically diagnosed, the severity of individual cases may vary
depending on baseline health conditions. Hence, treatment
strategies should be tailored according to risk stratification,
which can be guided by established risk scoring systems, such as
the Global Registry of Acute Coronary Events risk score and the
TIMI risk score (42,43). In addition, a larger sample size or
an external validation cohort would be required to confirm whether
the observed modest incremental value is statistically significant.
Therefore, multicenter studies with larger sample sizes may be
recommended to validate the present findings, with or without
adjustments for potential confounding factors.
In conclusion, the present findings indicate that
cardiac biomarkers, including hs-cTnT and sST2, either individually
or in combination, can effectively distinguish patients with STEMI
from those with NSTE-ACS.
Acknowledgements
Not applicable.
Funding
Funding: This work was supported by the Jiangsu Provincial
Medical Key Discipline Cultivation Unit (grant no. JSDW202239) and
Nanjing Medical Key Laboratory of Laboratory Diagnostics.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YW was responsible for software, data collection and
writing the manuscript. NL participated in data curation and
manuscript writing. CS contributed to data collection and
manuscript writing. BH participated in conception, design, and
critical review of the manuscript. YPM performed formal analysis
and acquired funding. HP designed the study and revised the
manuscript. HP and YPM confirmed the authenticity of the raw data.
All authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The Ethics Committee of Nanjing First Hospital
(Nanjing, China) approved this study (approval no.
KY20250714-KS-01).
Patient consent for publication
As this was a retrospective study, patient consent
for inclusion was waived.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rubini Gimenez M, Thiele H and Pöss J:
Management of acute coronary syndrome without ST-segment elevation.
Herz. 47:381–392. 2022.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
2
|
Hjort M, Eggers KM, Lindhagen L, Baron T,
Erlinge D, Jernberg T, Marko-Varga G, Rezeli M, Spaak J and Lindahl
B: Differences in biomarker concentrations and predictions of
long-term outcome in patients with ST-elevation and
non-ST-elevation myocardial infarction. Clin Biochem. 98:17–23.
2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Braunwald E and Morrow DA: Unstable
angina: Is it time for a requiem? Circulation. 127:2452–2457.
2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ibanez B, James S, Agewall S, Antunes MJ,
Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA,
Halvorsen S, et al: 2017 ESC Guidelines for the management of acute
myocardial infarction in patients presenting with ST-segment
elevation: The Task Force for the management of acute myocardial
infarction in patients presenting with ST-segment elevation of the
European society of cardiology (ESC). Eur Heart J. 39:119–177.
2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sandeman D, Syed MBJ, Kimenai DM, Lee KK,
Anand A, Joshi SS, Dinnel L, Wenham PR, Campbell K, Jarvie M, et
al: Implementation of an early rule-out pathway for myocardial
infarction using a high-sensitivity cardiac troponin T assay. Open
Heart. 8(e001769)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ishak M, Ali D, Fokkert MJ, Slingerland
RJ, Dikkeschei B, Tolsma RT, Lichtveld RA, Bruins W, Boomars R,
Bruheim K, et al: Fast assessment and management of chest pain
without ST-elevation in the pre-hospital gateway: rationale and
design. Eur Heart J Acute Cardiovasc Care. 4:129–136.
2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Giannitsis E, Garfias-Veitl T, Slagman A,
Searle J, Müller C, Blankenberg S, von Haehling S, Katus HA, Hamm
CW, Huber K, et al: Biomarkers-in-cardiology 8
RE-VISITED-consistent safety of early discharge with a dual marker
strategy combining a normal hs-cTnT with a normal copeptin in
low-to-intermediate risk patients with suspected acute coronary
syndrome-A secondary analysis of the randomized
biomarkers-in-cardiology 8 trial. Cells. 11(211)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
O'Donoghue M, Morrow DA, Sabatine MS,
Murphy SA, McCabe CH, Cannon CP and Braunwald E:
Lipoprotein-associated phospholipase A2 and its association with
cardiovascular outcomes in patients with acute coronary syndromes
in the PROVE IT-TIMI 22 (PRavastatin Or atorVastatin evaluation and
infection therapy-thrombolysis in myocardial infarction) trial.
Circulation. 113:1745–1752. 2006.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Inoue K, Chieh JTW, Yeh LC, Chiang SJ,
Phrommintikul A, Suwanasom P, Kasim S, Ahmad B, Idrose AM, Salleh
FM, et al: An international, stepped wedge, cluster-randomized
trial investigating the 0/1-h algorithm in suspected acute coronary
syndrome in Asia: The rational of the DROP-Asian ACS study. Trials.
23(986)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Möckel M, Danne O, Müller R, Vollert JO,
Müller C, Lueders C, Störk T, Frei U, Koenig W, Dietz R and Jaffe
AS: Development of an optimized multimarker strategy for early risk
assessment of patients with acute coronary syndromes. Clin Chim
Acta. 393:103–109. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Morawiec B, Kawecki D, Przywara-Chowaniec
B, Opara M, Muzyk P, Ho L, Tat LC, Gabrysiak A, Muller O and
Nowalany-Kozielska E: Copeptin as a prognostic marker in acute
chest pain and suspected acute coronary syndrome. Dis Markers.
2018(6597387)2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Möckel M, Müller R, Vollert J, Müller C,
Danne O, Gareis R, Störk T, Dietz R and Koenig W:
Lipoprotein-associated phospholipase A2 for early risk
stratification in patients with suspected acute coronary syndrome:
A multi-marker approach: The North Wuerttemberg and Berlin
infarction study-II (NOBIS-II). Clin Res Cardiol. 96:604–612.
2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
van Cauteren YJM, Smulders MW, Theunissen
RALJ, Gerretsen SC, Adriaans BP, Bijvoet GP, Mingels AMA, van Kuijk
SMJ, Schalla S, Crijns HJGM, et al: Cardiovascular magnetic
resonance accurately detects obstructive coronary artery disease in
suspected non-ST elevation myocardial infarction: A sub-analysis of
the CARMENTA trial. J Cardiovasc Magn Reson. 23(40)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Dhillon OS, Narayan HK, Khan SQ, Kelly D,
Quinn PA, Squire IB, Davies JE and Ng LL: Pre-discharge risk
stratification in unselected STEMI: is there a role for ST2 or its
natural ligand IL-33 when compared with contemporary risk markers?
Int J Cardiol. 167:2182–2188. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kohli P, Bonaca MP, Kakkar R, Kudinova AY,
Scirica BM, Sabatine MS, Murphy SA, Braunwald E, Lee RT and Morrow
DA: Role of ST2 in non-ST-elevation acute coronary syndrome in the
MERLIN-TIMI 36 trial. Clin Chem. 58:257–266. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sabatine MS, Morrow DA, Higgins LJ,
MacGillivray C, Guo W, Bode C, Rifai N, Cannon CP, Gerszten RE and
Lee RT: Complementary roles for biomarkers of biomechanical strain
ST2 and N-terminal prohormone B-type natriuretic peptide in
patients with ST-elevation myocardial infarction. Circulation.
117:1936–1944. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Dohi T, Miyauchi K, Okazaki S, Yokoyama T,
Ohkawa R, Nakamura K, Yanagisawa N, Tsuboi S, Ogita M, Yokoyama K,
et al: Decreased circulating lipoprotein-associated phospholipase
A2 levels are associated with coronary plaque regression in
patients with acute coronary syndrome. Atherosclerosis.
219:907–912. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Januzzi JL Jr: ST2 as a cardiovascular
risk biomarker: From the bench to the bedside. J Cardiovasc Transl
Res. 6:493–500. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang J, Tan GJ, Han LN, Bai YY, He M and
Liu HB: Novel biomarkers for cardiovascular risk prediction. J
Geriatr Cardiol. 14:135–150. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
McDonagh TA, Metra M, Adamo M, Gardner RS,
Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, et
al: 2021 ESC guidelines for the diagnosis and treatment of acute
and chronic heart failure. Eur Heart J. 42:3599–3726.
2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Visseren FLJ, Mach F, Smulders YM,
Carballo D, Koskinas KC, Bäck M, Benetos A, Biffi A, Boavida JM,
Capodanno D, et al: 2021 ESC guidelines on cardiovascular disease
prevention in clinical practice: Developed by the Task Force for
cardiovascular disease prevention in clinical practice with
representatives of the European society of cardiology and 12
medical societies with the special contribution of the European
association of preventive cardiology (EAPC). Rev Esp Cardiol (Engl
Ed). 75(429)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lapostolle F, Loyeau A, Bataille S, Boche
T, Le Bail G, Weisslinger L, Juliard JM and Lambert Y: New European
society of cardiology guidelines for the management of patients
with ST-elevation myocardial infarction: Effect on physician's
compliance and patient's outcome. Eur J Emerg Med. 26:380–381.
2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
DeLong ER, DeLong DM and Clarke-Pearson
DL: Comparing the areas under two or more correlated receiver
operating characteristic curves: A nonparametric approach.
Biometrics. 44:837–845. 1988.PubMed/NCBI
|
|
24
|
Du X, Patel A, Anderson CS, Dong J and Ma
C: Epidemiology of cardiovascular disease in China and
opportunities for improvement: JACC international. J Am Coll
Cardiol. 73:3135–3147. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Dalal JJ, Ponde CK, Pinto B, Srinivas CN,
Thomas J, Modi SK, Mehta S, Shetty S, Manimarane and Desai
B: Time to shift from contemporary to high-sensitivity cardiac
troponin in diagnosis of acute coronary syndromes. Indian Heart J.
68:851–855. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Duraes AR, Bitar YS, Freitas ACT, Filho
IM, Freitas BC and Fernandez AM: Gender differences in ST-elevation
myocardial infarction (STEMI) time delays: Experience of a public
health service in Salvador-Brazil. Am J Cardiovasc Dis. 7:102–107.
2017.PubMed/NCBI
|
|
27
|
Kuehnemund L, Koeppe J, Feld J, Wiederhold
A, Illner J, Makowski L, Gerß J, Reinecke H and Freisinger E:
Gender differences in acute myocardial infarction-A nationwide
German real-life analysis from 2014 to 2017. Clin Cardiol.
44:890–898. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Akbar H and Mountfort S: Acute ST-segment
elevation myocardial infarction (STEMI). In: StatPearls. StatPearls
Publishing LLC. Treasure Island, FL, 2025.
|
|
29
|
Al-Assadi MY, Aljaber NN, Al-Habeet A, Al
Nono O and Al-Motarreb A: Sex-related differences in acute coronary
syndrome: Insights from an observational study in a Yemeni cohort.
Front Cardiovasc Med. 12(1481917)2025.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Soeiro AM, Silva PGMBE, Roque EAC, Bossa
AS, Biselli B, Leal TCAT, Soeiro MCFA, Pitta FG, Serrano CV Jr and
Oliveira MT Jr: Prognostic differences between men and women with
acute coronary syndrome. Data from a Brazilian registry. Arq Bras
Cardiol. 111:648–653. 2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sári C, Heesch CM, Kovács AJ and Andréka
P: Sex-related differences in care and prognosis in acute coronary
syndrome. Prev Med Rep. 55(103131)2025.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Kavsak PA, Shortt C, Ma J, Clayton N,
Sherbino J, Hill SA, McQueen M, Mehta SR, Devereaux PJ and Worster
A: A laboratory score at presentation to rule-out serious cardiac
outcomes or death in patients presenting with symptoms suggestive
of acute coronary syndrome. Clin Chim Acta. 469:69–74.
2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Aimo A, Januzzi JL Jr, Bayes-Genis A,
Vergaro G, Sciarrone P, Passino C and Emdin M: Clinical and
prognostic significance of sST2 in heart failure: JACC review topic
of the week. J Am Coll Cardiol. 74:2193–2203. 2019.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Sanada S, Hakuno D, Higgins LJ, Schreiter
ER, McKenzie AN and Lee RT: IL-33 and ST2 comprise a critical
biomechanically induced and cardioprotective signaling system. J
Clin Invest. 117:1538–1549. 2007.PubMed/NCBI View
Article : Google Scholar
|
|
35
|
Stătescu C, Anghel L, Tudurachi BS, Leonte
A, Benchea LC and Sascău RA: From classic to modern prognostic
biomarkers in patients with acute myocardial infarction. Int J Mol
Sci. 23(9168)2022.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Badimon L, Romero JC, Cubedo J and
Borrell-Pagès M: Circulating biomarkers. Thromb Res. 130 (Suppl
1):S12–S15. 2012.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Smulders MW, Kietselaer BLJH, Wildberger
JE, Dagnelie PC, Brunner-La Rocca HP, Mingels AMA, van Cauteren
YJM, Theunissen RALJ, Post MJ, Schalla S, et al: Initial
imaging-guided strategy versus routine care in patients with
non-ST-segment elevation myocardial infarction. J Am Coll Cardiol.
74:2466–2477. 2019.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Zhang H, Gao Y, Wu D and Zhang D: The
relationship of lipoprotein-associated phospholipase A2 activity
with the seriousness of coronary artery disease. BMC Cardiovasc
Disord. 20(296)2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Zhao SQ, Chang H and Zhang L: Correlation
between the level of lipoprotein-associated phospholipase A2
activity in serum, the degree of coronary artery ste-nosis and
major adverse cardiovascular events in patients with coronary heart
disease. Chin J Lab Diagn. 1:1621–1624. 2021.
|
|
40
|
Verdoia M, Rolla R, Gioscia R, Rognoni A
and De Luca G: Novara Atherosclerosis Study Group (NAS).
Lipoprotein associated-phospholipase A2 in STEMI vs NSTE-ACS
patients: a marker of cardiovascular atherosclerotic risk rather
than thrombosis. J Thromb Thrombolysis. 56:37–44. 2023.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Chung H, Kwon HM, Kim JY, Yoon YW, Rhee J,
Choi EY, Min PK, Hong BK, Rim SJ, Yoon JH, et al:
Lipoprotein-associated phospholipase A2 is related to
plaque stability and is a potential biomarker for acute coronary
syndrome. Yonsei Med J. 55:1507–1515. 2014.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Gale CP, Stocken DD, Aktaa S, Reynolds C,
Gilberts R, Brieger D, Carruthers K, Chew DP, Goodman SG, Fernandez
C, et al: Effectiveness of GRACE risk score in patients admitted to
hospital with non-ST elevation acute coronary syndrome (UKGRIS):
Parallel group cluster randomised controlled trial. BMJ.
381(e073843)2023.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Neumann FJ and Sousa-Uva M: ‘Ten
commandments’ for the 2018 ESC/EACTS guidelines on myocardial
revascularization. Eur Heart J. 40:79–80. 2019.PubMed/NCBI View Article : Google Scholar
|