Introduction
Bronchogenic cysts (BCs) are rare congenital benign
tumors that arise during early embryonic foregut development. The
pathogenesis is hypothesized to be a result of the abnormal
detachment and displacement of primitive tracheobronchial tree buds
(1). These cysts can be found in
any organ derived from the embryonic primitive foregut and,
according to the site of occurrence, can be classified into the
intrapulmonary type, mediastinal type and ectopic type. Over 80% of
cases occur in the lungs and posterior mediastinum. Clinically, BCs
located outside of the thoracic cavity are referred to as ectopic
BCs (EBCs). EBCs, although rare, can also be found in various
locations, including the neck, brain, meninges and abdominal
cavity, with retroperitoneal occurrences being uncommon and
accounting for only 0.03% of retroperitoneal tumors (2). The first report of an EBC was made by
Miller et al (3) in 1953.
Due to their common growth locations within body cavities, BCs are
typically asymptomatic and are often discovered incidentally during
routine imaging. Preoperative definitive diagnosis is relatively
challenging and final confirmation still relies on
histopathological analysis. The present case report describes a
patient with an ectopic retroperitoneal BC (ERBC), successfully
treated through laparoscopic excision after cyst puncture and
drainage. A literature review is also included to update the
clinical features of this rare disease in adult patients, in order
to provide a reference for the diagnosis and treatment of patients
with ERBC.
Case report
A 53-year-old male patient presented at The Second
Affiliated Hospital of Zunyi Medical University (Zunyi, China) in
August 2023 with a 2-week history of recurrent lower back pain and
a fever of 38.8˚C. Despite these symptoms, the patient's mental and
physical health were good, and there was no history of trauma. A
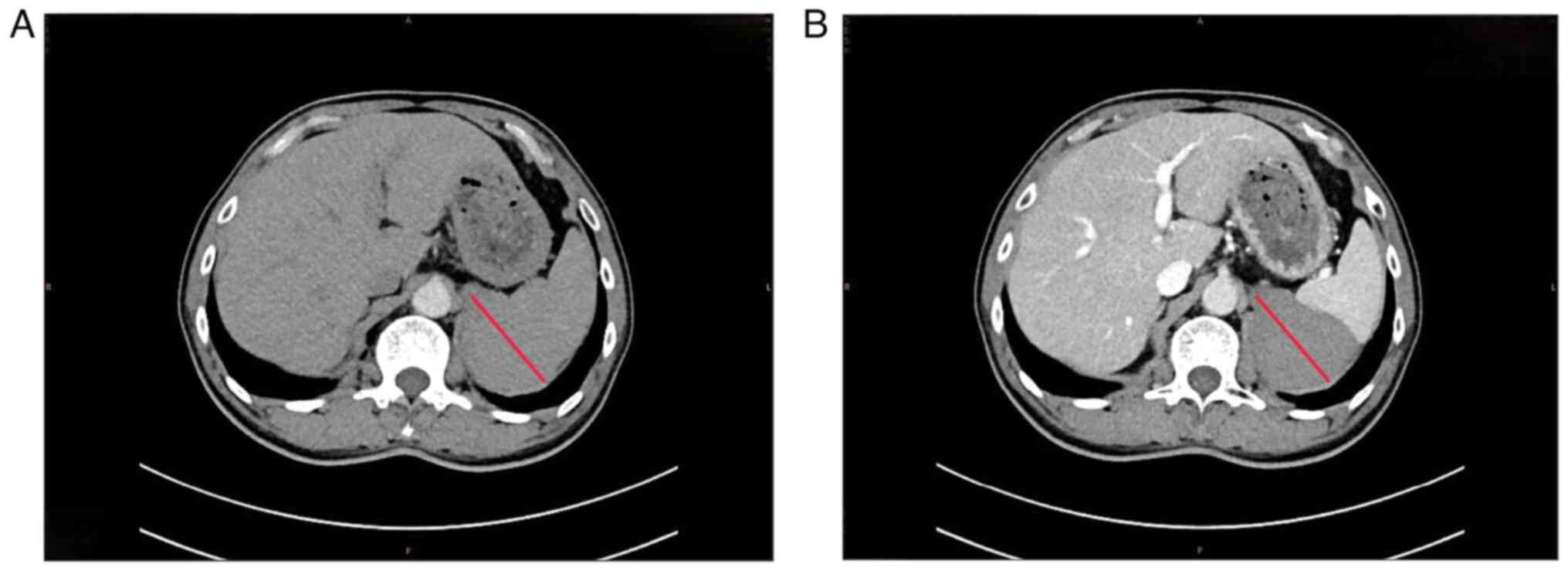
computed tomography (CT) scan revealed a cystic lesion in the left
retroperitoneum, suspected to be an adrenal cyst complicated by
hemorrhage and infection (Fig. 1).
Upon admission, the patient denied any significant history of
infectious or chronic diseases, except for a previous kidney stone
surgery, which was performed in May 2020. No mass was detected in
the upper abdomen and CT findings confirmed a left adrenal cyst
with hemorrhage and infection. Given the fever and infection, a
provisional diagnosis of a left adrenal cyst with hemorrhage and
infection was made. A CT-guided aspiration of the left perinephric
fluid yielded brown purulent fluid. Routine analysis of the
aspirate showed red blood cells (+) and white blood cells (++), and
a bacterial smear revealed white blood cells (+), Gram-positive
cocci (+) and Gram-negative rods (-). Although bacterial cultures
showed no growth after 48 h, likely due to prior antibiotic
treatment, the puncture drainage was ineffective, prompting
laparoscopic resection of the retroperitoneal cyst after 1 week of
antibiotic treatment, and exclusion of any surgical
contraindications.
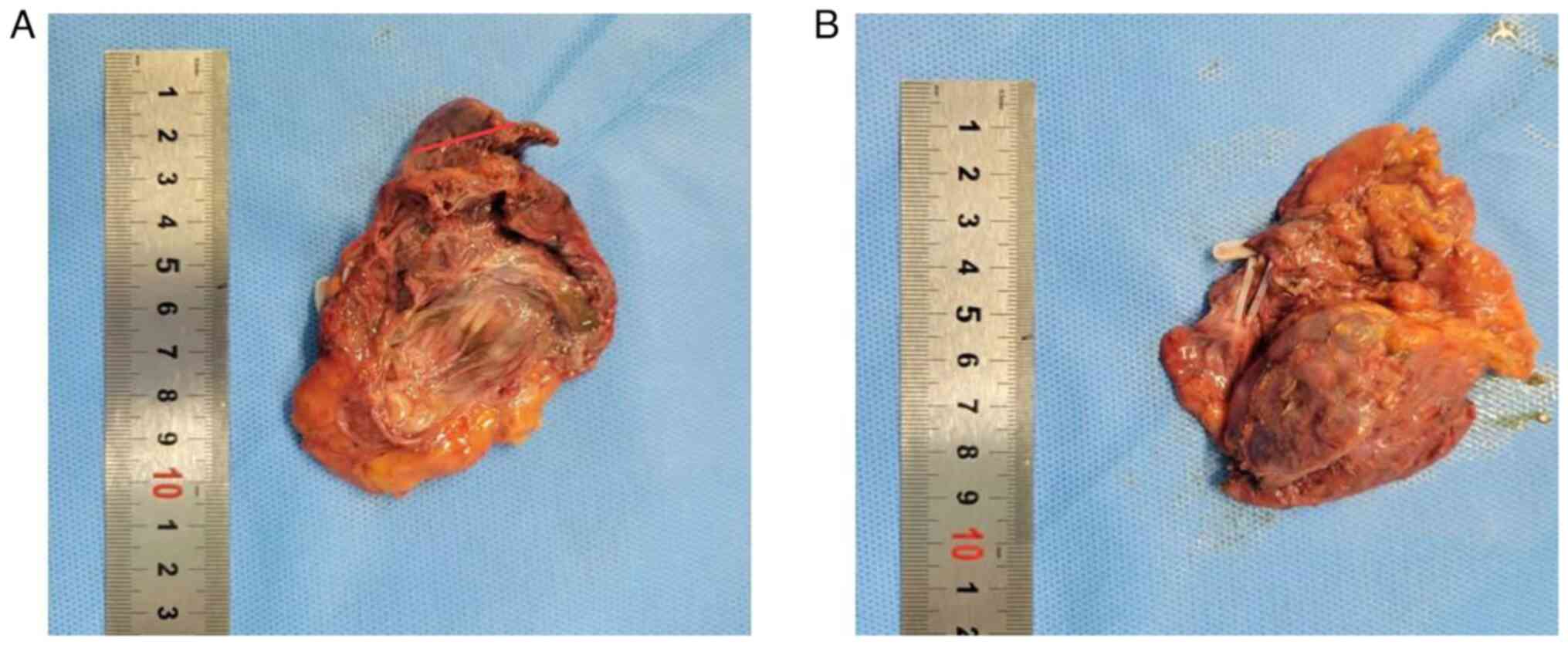
Intraoperatively, the left adrenal gland was located
above the psoas major muscle, with a cystic mass ~10 cm in diameter
and a smooth surface (Fig. 2). The
excised mass measured 7.4x5.1x5.5 cm and had a multi-segmented
cystic structure, with localized solid areas (~1.5x0.7 cm) from
which 80 ml of grayish-brown viscous fluid was discharged.
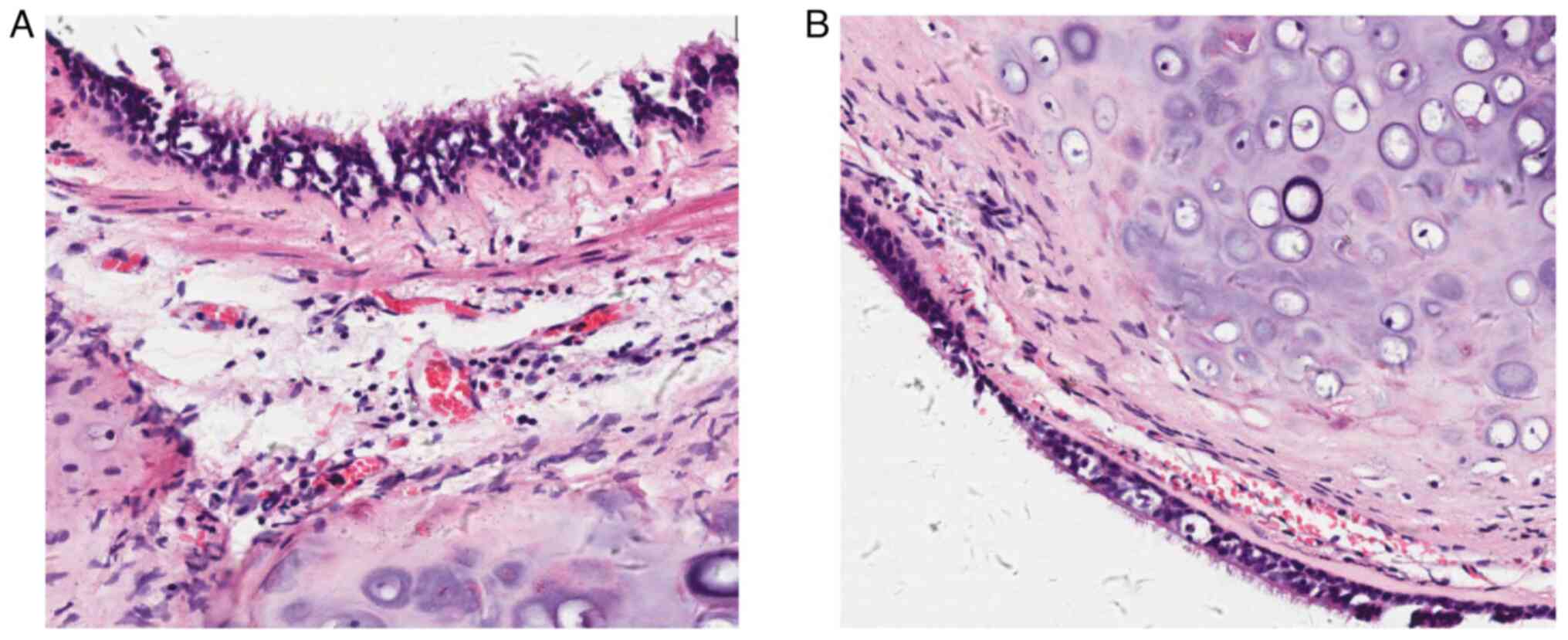
Pathological examination (H&E staining; Data S1) of the resected mass revealed
that the cyst wall was lined with ciliated columnar epithelium,
with fibrous connective tissue beneath. Irregular cartilage
fragments were observed within the cyst wall and mucus was present
inside the cyst (Fig. 3). Based on
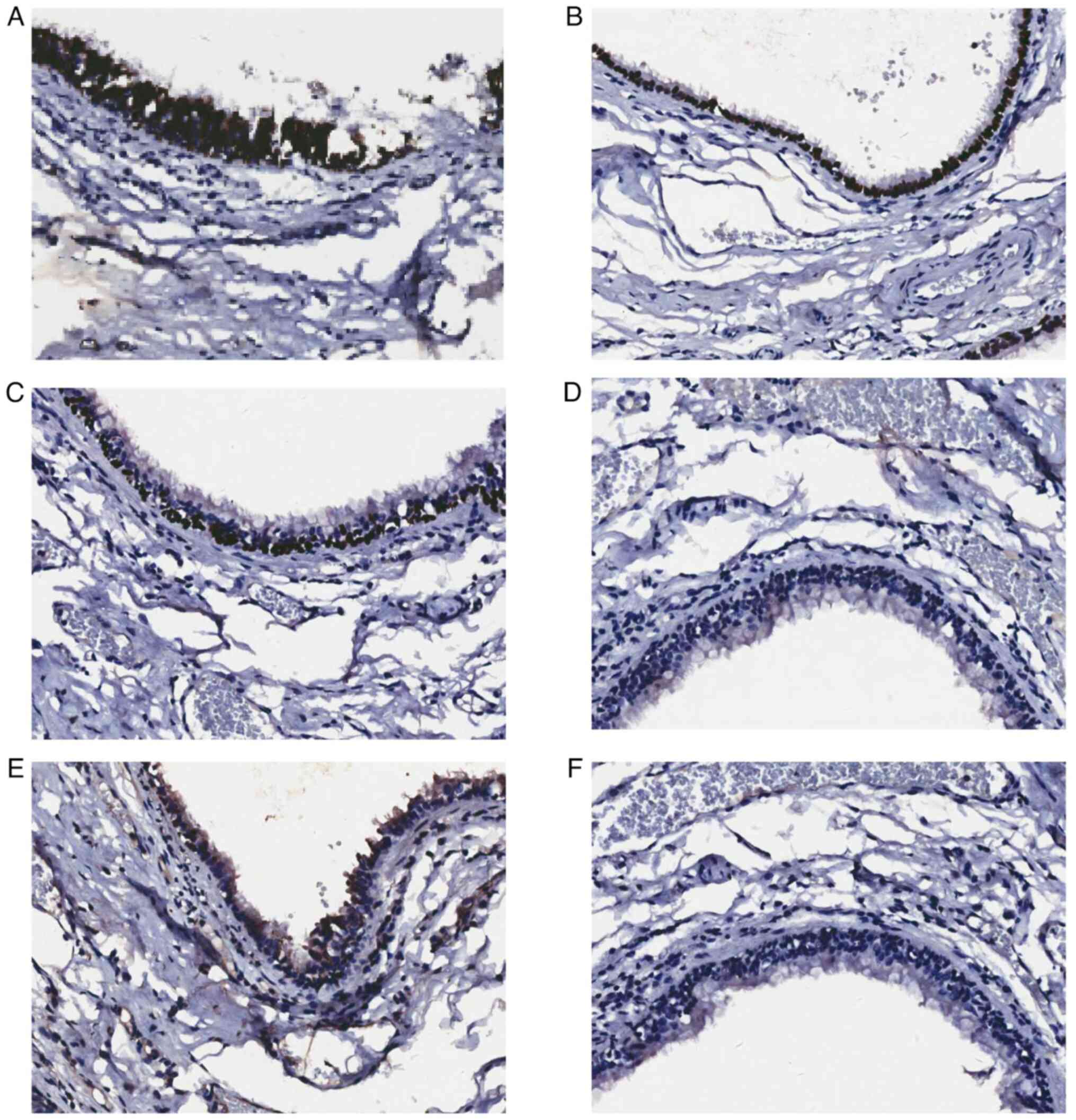
surgical and pathological findings (Fig. 4) the final diagnosis was a left
adrenal BC. The patient has been followed up regularly
postoperatively, with ultrasound examinations performed at 3 and 12
months after surgery, and no medications or other treatments were
administered postoperatively. As of 12 months post-surgery, no
recurrence has been observed. At the time of manuscript submission,
the patient reported a satisfactory recovery with no signs of
recurrence.
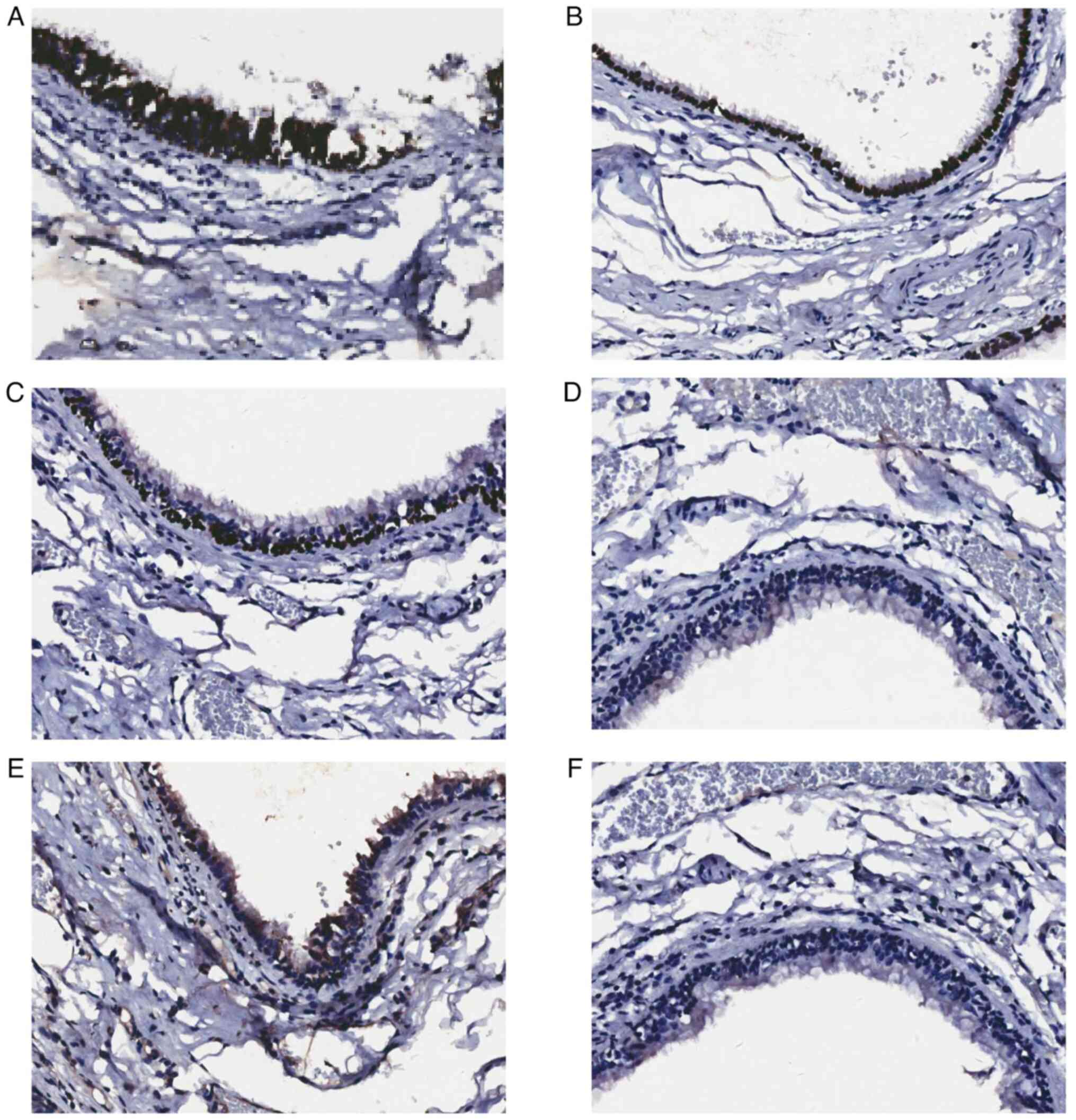 | Figure 4Postoperative immunohistochemical
analysis of the bronchogenic cyst revealed positive expression of
(A) CK7, (B) TTF-1 and (C) p63 in the epithelial cells, while (D)
Napsin A, (E) Pax8 and (F) ER were negative. CK7 and Napsin A
showed cytoplasmic localization, whereas TTF-1, P63, Pax8 and ER
were localized in the nucleus (magnification, x400). CK,
cytokeratin; TTF-1, thyroid transcription factor 1; ER, estrogen
receptor; Pax8, paired box 8. |
Discussion
BCs are developmental anomalies originating from the
early embryonic foregut, predominantly found in the lungs and
mediastinum, with RBCs occurring rarely (2). In recent years, only a few cases have
been reported in the literature, most of them in case reports. ERBC
can occur at any age, with similar incidence rates in men and
women. The cysts are generally <5 cm in diameter and are mostly
unilateral and unilocular (3).
These cysts are characterized by pseudostratified columnar
epithelium, resembling bronchioles, and may be accompanied by
cartilage, smooth muscle or glandular tissue (4). Due to their unusual location,
variable cystic content and non-specific imaging features, RBCs are
frequently misdiagnosed as cystic teratomas, adrenal tumors or
other benign or malignant retroperitoneal masses (5).
The exact pathogenesis of RBCs remains elusive.
Currently, the most widely accepted hypothesis is the germ bud
detachment and displacement theory (6). Based on embryological evidence, it is
proposed that during the 4-6th week of embryonic development, the
ventral wall of the foregut forms the laryngotracheal diverticulum,
which gradually develops into the bronchial tree. During cellular
migration, some primitive bronchial bud cells abnormally detach and
remain in the posterior mediastinum or more distant locations such
as the retroperitoneum. From a molecular biology perspective, the
formation of RBCs may be associated with abnormalities in embryonic
developmental signaling pathways and imbalances in the cellular
microenvironment (7). This mainly
involves abnormal activation of the Wnt/β-catenin pathway, which
promotes the survival of ectopic epithelial cells and cystic
expansion, aberrant expression of homeobox (HOX) genes (such as the
HOXA/B clusters), potentially causing mislocalization of foregut
epithelial cells to the retroperitoneum, and extracellular matrix
remodeling along with TGF-β signaling regulation, which facilitates
cartilage and smooth muscle differentiation, forming the
characteristic cyst wall structure (8). As this study is a case report, there
are inherent limitations in exploring detailed mechanisms or
molecular aspects.
Clinically, ~60% of RBCs are located near the
adrenal glands. This may be attributed to the overlapping timing of
adrenal embryogenesis, derived from the neural crest and mesoderm,
and foregut differentiation, as well as the presence of loose
connective tissue in the region, which provides space for cyst
growth. Among these, the left adrenal region is most commonly
affected (6). This may be due to
the counterclockwise rotation of the caudal primitive foregut and
midgut from left to right during embryonic development. It is
hypothesized that the detached germ bud fails to follow this
rotation and remains on the left side. In the present case, the RBC
was located above the left adrenal gland, consistent with most
cases reported in the literature (9,10).
RBCs are often incidentally discovered during
imaging examinations such as upper abdominal CT or MRI. On CT,
abdominal EBCs typically appear as round or oval cystic masses with
well-defined borders and homogeneous densities, often presenting as
unilocular lesions of varying sizes (11). When these cysts are located within
tissue planes, their long axis usually aligns with surrounding
tissues, displacing adjacent structures. The cyst wall may be thin
and difficult to discern on imaging, although occasional punctate
calcifications may be visible. The CT density of BCs varies
depending on their contents, ranging from low-density, water-like
appearances to mildly hyperdense regions, with minimal enhancement
of the cyst wall on contrast-enhanced scans (12,13).
On unenhanced MRI, the cyst contents typically appear isointense to
hypointense on T1-weighted images, slightly higher than the signal
of simple fluid. On T2-weighted images, they usually show high
signal intensity, which may be attributed to the presence of
methemoglobin, mucin and other proteinaceous components (12,14).
Contrast-enhanced scans may reveal enhancement of the cyst wall,
while the cyst contents generally show no obvious enhancement.
RBCs are often asymptomatic, with clinical symptoms
emerging only when the cyst enlarges, ruptures, compresses
surrounding structures or becomes secondarily infected (15). Symptoms can include lower back
pain, abdominal discomfort, nausea, vomiting or fever, as observed
in the present case. Certain studies (15-17)
have found that when RBCs are located in the adrenal region,
patients may exhibit pheochromocytoma-like clinical symptoms such
as palpitations, insomnia and hypertension. Mild elevations in
adrenal hormone levels may also be observed. The underlying
pathogenesis is hypothesized to involve compression of the
surrounding adrenal gland by a relatively large cyst. These
symptoms typically show notable improvement after surgical
resection and relief of the compression (18). In the present case, the BC was
located in the left adrenal region. Although it was relatively
large, the patient did not exhibit any pheochromocytoma-like
clinical manifestations. In addition, the serological examinations
revealed no elevation in adrenal hormone levels. This may be
because the cyst had already ruptured and was no longer exerting
considerable compressive effects on the adrenal gland. The majority
of patients with BC typically do not exhibit any notable
abnormalities in tumor markers such as CA19-9, CA12-5 and CEA
(19). However, in clinical
practice, routine assessment of tumor markers, such as CA19-9, CEA
and CA24-2, are still recommended, as they can aid in the
differential diagnosis from retroperitoneal tumors such as
pancreatic and adrenal tumors, thereby helping to avoid
misdiagnosis.
As the BC described in the present report was
located in the left adrenal region, distinguishing it from other
cystic adrenal lesions, such as adrenal hemorrhage or pseudocysts,
was crucial. The combination of clinical history, blood tests and
imaging studies, including CT, facilitated this differentiation.
However, a definitive diagnosis still ultimately relies on
pathological examination. The pathological features of RBC often
include a cyst wall lined with pseudostratified ciliated columnar
epithelium (20). Additionally,
the cyst wall contains cartilage, mucous glands and bronchial
smooth muscle. The presence of cartilage in the cyst wall is
considered a characteristic feature of RBC. However, further
comprehensive immunohistochemical staining for thyroid
transcription factor (TTF)-1, cytokeratin (CK)7 and p63 is also
currently recommended. These immunohistochemical stainings are
designed to form a comprehensive panel for determining the tissue
of origin, thereby elucidating the histogenesis and nature of the
cyst, aiding in differential diagnosis, and ultimately improving
the accuracy of pathological evaluation. The immunohistochemical
experiments shown in Fig. 4 were
performed for diagnostic purposes. With regard to the tumor of the
present patient, immunohistochemical analysis performed at a later
stage revealed CK7 and Napsin A with cytoplasmic positive staining
(brown coloration), whereas TTF-1, p63, paired box 8 and estrogen
receptor exhibited nuclear positive staining. In view of the benign
histological features and lack of atypia, KRAS/BRAF mutation
analysis was deemed unnecessary in the present case. Nonetheless,
in scenarios suggestive of malignant transformation, molecular
testing may provide valuable insights into tumor biology and inform
clinical management strategies.
Adrenal hemorrhagic cysts can be classified into two
types: i) Those associated with hematomas or hemorrhage within
adrenal cortical or medullary tumors; and ii) those arising from
trauma, inflammation or other causes (21). Hemorrhagic cysts often appear as
acute or subacute hemorrhages on imaging, presenting as masses with
varying densities, occasionally accompanied by calcifications but
without surrounding tissue infiltration (22). By contrast, traumatic adrenal
hemorrhage may appear on ultrasound as heterogeneous, echogenic
masses that become more mixed or hypoechoic as liquefaction
progresses (23). In the present
case, the EBC exhibited symptoms similar to those of a peri-adrenal
abscess due to infection and rupture. The pseudo complex columnar
epithelium of the cyst has secretory functions, and as
intracapsular pressure increases, the risk of rupture rises,
releasing mucus and secretions into surrounding tissues, creating a
favorable environment for bacterial colonization (2). This explains why Gram-positive cocci
were identified in the cyst fluid culture described in the present
report. However, subsequent bacterial cultures did not detect any
positive bacteria, possibly because sensitive antibiotic therapy
had already been administered prior to the aspiration
procedure.
The tissue surrounding the adrenal glands is loose
and rich in fat and lymphatic vessels, making it easy for
inflammation to spread. When a cyst ruptures, the infection may
spread through the bloodstream. Abdominal EBCs typically present as
fluid-filled lesions on CT or MRI, with no notable enhancement on
contrast imaging (24). They can
often be misdiagnosed as adrenal hematomas or other retroperitoneal
masses. This was also the reason why a prompt diagnosis was not
established for the patient described in the present case report
and laparoscopic surgery was performed. RBCs are challenging to
diagnose preoperatively. However, if an RBC is located around the
adrenal gland, it is still recommended that serum potassium,
catecholamines, 24-h urinary cortisol and serum adrenocorticotropic
hormone tests are performed to exclude adrenal pheochromocytoma and
adrenal cortical tumors. If the RBC is located around the pancreas,
it is recommended that serum amylase, lipase and CA-19-9 levels are
measured to differentiate it from pancreatic pseudocysts,
pancreatic cancer and other diseases. Current literature suggests
that retroperitoneal cysts <6 cm can be managed conservatively,
but surgical resection is required when they exhibit mass effect,
cause hydronephrosis or when malignancy cannot be excluded. Due to
their deep location and proximity to critical structures such as
the adrenal glands and spleen, complete excision may be difficult
in certain cases (25). However,
laparoscopic resection is the preferred treatment due to its
minimal invasiveness, high success rate and low complication rate.
In the present case, complete laparoscopic resection was safe and
effective, with no recurrence observed during follow-up.
Although bronchogenic cysts have been reported
previously, the present case is unique in presenting a rare
retroperitoneal location combined with hemorrhagic and infectious
complications, which is exceptionally uncommon (26-28).
Furthermore, based on this case, we propose a diagnostic approach
to aid in differentiating retroperitoneal cystic lesions, including
consideration of bronchogenic cysts when the adrenal origin is
uncertain. In the patient of the present study, the diagnostic
confusion primarily resulted in a prolonged diagnostic and
therapeutic process. The main reason for the misdiagnosis was
insufficient awareness of this rare condition, leading to its
exclusion from the initial preoperative differential diagnosis.
Although this delay did not cause any evident deterioration in the
patient's health condition at the time of treatment or in the
postoperative period, it underscores the importance of considering
this entity in similar clinical scenarios to avoid unnecessary
delays in management. While this is not a mechanistic study, the
rare presentation and clinical insights may offer meaningful value
to clinicians and radiologists (20,29).
In conclusion, in the present study, a case of a
retroperitoneal EBC with hemorrhage and infection on the left side
was reported. Although this type of cyst is rare and typically
benign, it poses potential risks of complications, such as
opportunistic infection and hemorrhage, as it enlarges. Therefore,
in clinical practice, for patients presenting with symptoms and
imaging features suggestive of adrenal cysts with hemorrhage and
infection, clinicians should be vigilant and consider EBCs as part
of the differential diagnosis for retroperitoneal tumors. Timely
identification and diagnosis of such cysts can help avoid delays
and misjudgments in treatment. The long-term prognosis of this
condition is favorable, with no reported recurrence in patients who
have undergone laparoscopic surgery.
Supplementary Material
Supplementary methods
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by The Guizhou Provincial
Department of Education (grant no. SJJG-2023177).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
BY and QX were the patient's urologists and
suggested a writing strategy for the manuscript. MM and YN analyzed
the patient's information and wrote the manuscript. YH, NF, CY, DW,
HL, XX and LL obtained and analyzed the patient's information and
reviewed the discussion part on the clinical diagnosis and
treatment. BY and XX were responsible for the revision of the
manuscript for important intellectual content. QX and XX confirm
the authenticity of all the raw data. All authors have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The specimens used in Fig. 4 were derived from the same
postoperative paraffin-embedded tissue of the patient described in
this case report. Additional sectioning and immunohistochemical
staining were performed on the original paraffin block at the
Department of Pathology, The Second Affiliated Hospital of Zunyi
Medical University (Zunyi, China) as part of the supplementary
diagnostic evaluation. As these procedures were conducted for the
same patient and not for a separate research project, no additional
ethics approval was required.
Patient consent for publication
Written informed consent to publish this case report
and the accompanying images was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pederiva F, Rothenberg SS, Hall N,
Ijsselstijn H, Wong KKY, von der Thüsen J, Ciet P, Achiron R, Pio
d'Adamo A and Schnater JM: Congenital lung malformations. Nat Rev
Dis Primers. 9(60)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Xie W, Huang Z, Huang Z, Chen Z, Zhang B,
Xie L, Zhu L, Lian K and Lin D: Retroperitoneal bronchogenic cyst
with fluid-fluid level: A case report and literature review. Exp
Ther Med. 25(5)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Miller RF, Graub M and Pashuck ET:
Bronchogenic cysts; anomalies resulting from maldevelopment of the
primitive foregut and midgut. Am J Roentgenol Radium Ther Nucl Med.
70:771–785. 1953.PubMed/NCBI
|
|
4
|
Weissferdt A: Non-neoplastic thoracic
cysts: A clinicopathologic study of 136 cases. Am J Surg Pathol.
47:1349–1363. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Matsumoto H, Hasegawa S, Maezawa Y,
Okauchi S, Ohara G, Iguchi K, Kawai H, Takayashiki N and Satoh H:
An atypical presentation of bronchogenic cyst. Klin Onkol.
39:463–466. 2024.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sumiyoshi K, Shimizu S, Enjoji M, Iwashita
A and Kawakami K: Bronchogenic cyst in the abdomen. Virchows Arch A
Pathol Anat Histopathol. 408:93–98. 1985.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hernandorena González M, Joudanin Seijo
JR, Sanchís García JM and Pina Pallín M: Unusual location of a
bronchogenic cyst simulating a pancreatic tumor. Radiologia.
52:465–468. 2010.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
8
|
Obando J, Merkle E and Bean SM: A
retroperitoneal bronchogenic cyst. Clin Gastroenterol Hepatol.
7:A24–e21. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Govaerts K, Van Eyken P, Verswijvel G and
Van der Speeten K: A bronchogenic cyst, presenting as a
retroperitoneal cystic mass. Rare Tumors. 4(e13)2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jiang B, Xie T, Hu J, Xu Y and Zhang H:
Retroperitoneal bronchogenic cyst: A case report and literature
review. Front Oncol. 14(1406270)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fu GS, Wang SF, Wang YN, Han FG, Xu Y, Wei
YY, Zhang F, Duan QC and Zhang J: Clinical analysis of 21 cases of
children with ectopic bronchogenic cyst. Zhonghua Er Bi Yan Hou Tou
Jing Wai Ke Za Zhi. 59:941–946. 2024.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
12
|
Gu X, Zhu L, Li Y, Yin B and Wang Z:
Imaging findings and misdiagnosis of bronchogenic cysts: A study of
83 cases. J Belg Soc Radiol. 107(81)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Topal U: Bronchogenic cysts: Radiologic
findings. Tani Girisim Radyol. 9:333–338. 2003.PubMed/NCBI(In Turkish).
|
|
14
|
Park JW, Jeong WG, Lee JE, Lee HJ, Ki SY,
Lee BC, Kim HO, Kim SK, Heo SH, Lim HS, et al: Pictorial review of
mediastinal masses with an emphasis on magnetic resonance imaging.
Korean J Radiol. 22:139–154. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gostomczyk K, Borowczak J, Zdrenka M and
Szylberg Ł: Atypical presentation of bronchogenic cyst in the
retroperitoneal space. Cureus. 16(e55029)2024.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Moez R, Ouanes Y, Sahnoun W, Mokhtar B,
Dali KM, Sellami A, Ben Rhouma S and Nouira Y: Retroperitoneal
cystic mass: A rare form of adrenal pheochromocytoma. J Surg Case
Rep. 2021(rjab169)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Mokhtari M and ZeraatianNejadDavani S:
Primary adrenal hydatid cyst presenting with arterial hypertension.
Arch Iran Med. 15:328–330. 2012.PubMed/NCBI
|
|
18
|
Cao DH, Zheng S, Lv X, Yin R, Liu LR, Yang
L, Huang Y and Wei Q: Multilocular bronchogenic cyst of the
bilateral adrenal: Report of a rare case and review of literature.
Int J Clin Exp Pathol. 7:3418–3422. 2014.PubMed/NCBI
|
|
19
|
Wang M, He X, Qiu X, Tian C, Li J and Lv
M: Retroperitoneal bronchogenic cyst resembling an adrenal tumor
with high levels of serum carbohydrate antigen 19-9: A case report.
Medicine (Baltimore). 96(e7678)2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wen Y, Chen W, Chen J and He X:
Retroperitoneal bronchogenic cyst resembling an adrenal tumor: Two
case reports and literature review. J Int Med Res.
48(300060520925673)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Elhassan YS, Ronchi CL, Wijewickrama P and
Baldeweg SE: Approach to the patient with adrenal hemorrhage. J
Clin Endocrinol Metab. 108:995–1006. 2023.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Arslan S, Sarıkaya Y, Akata D, Özmen MN,
Karçaaltıncaba M and Karaosmanoğlu AD: Imaging findings of
spontaneous intraabdominal hemorrhage: Neoplastic and
non-neoplastic causes. Abdom Radiol (NY). 47:1473–1502.
2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Piskunowicz M, Stefanowicz J, Batko T,
Hwang M, Świętoń D, Szarmach A, Back S and Kosiak W:
Contrast-enhanced ultrasound of adrenal hemorrhage: A helpful
problem solving tool. Med Ultrason. 24:284–289. 2022.PubMed/NCBI View
Article : Google Scholar
|
|
24
|
Singh AK, Neyaz Z, Verma R, Gupta A,
Mishra R and Mishra P: Diagnostic yield and safety of percutaneous
CT-guided biopsy of retroperitoneal lesions and analysis of imaging
features. Acta Radiol. 63:149–158. 2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Al-Jawad M, Yehya B, Katbi E, Abousaadah M
and Danial AK: Right-sided retroperitoneal bronchogenic cyst: A
case report. Int J Surg Case Rep. 126(110671)2025.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Yuan K, Shu M, Ma Y, Feng W, Ye J and Yuan
Y: Ectopic bronchogenic cyst in the retroperitoneal region: A case
report and literature review of adult patients. BMC Surg.
21(347)2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Murakami R, Machida M, Kobayashi Y, Ogura
J, Ichikawa T and Kumazaki T: Retroperitoneal bronchogenic cyst: CT
and MR imaging. Abdom Imaging. 25:444–447. 2000.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Qureshi M, Wawryk S and Yap Z:
Retroperitoneal bronchogenic cyst: A rare diagnosis of a
retroperitoneal mass. Cureus. 17(e76922)2025.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Runge T, Blank A, Schäfer SC, Candinas D,
Gloor B and Angst E: A retroperitoneal bronchogenic cyst mimicking
a pancreatic or adrenal mass. Case Rep Gastroenterol. 7:428–432.
2013.PubMed/NCBI View Article : Google Scholar
|