Introduction
Localized failure of tooth eruption may result from
numerous factors. Mechanical impediments, such as contact with
adjacent teeth, localized bone calcifications or odontoma
formation, and parafunctional habits, such as thumb-sucking,
commonly inhibit tooth emergence. However, once the observed
obstruction is removed, eruption often resumes. By contrast,
primary failure of eruption (PFE) denotes cessation or absence of
eruption of a tooth in the absence of any identifiable local or
systemic cause. Affected teeth neither erupt nor respond to
conventional orthodontic forces, and they often become ankylosed
when traction is applied, meaning they are directly fused to the
surrounding alveolar bone (1).
PFE is a rare, non-syndromic, hereditary condition
attributed to loss-of-function mutations in the parathyroid hormone
(PTH) receptor 1 (PTH1R) gene and dysregulation of the cyclic
adenosine monophosphate-dependent protein kinase A signalling
pathway. Notably, the aforementioned pathways are essential for
healthy tooth eruption (2-4).
At present, diagnosis remains challenging due to the condition's
low prevalence and the absence of radiographic evidence of
mechanical blockage. Therapeutic options are limited; for example,
orthodontic traction alone may be ineffective, while surgical
luxation or direct restorative procedures exhibit risks, such as
root resorption and further ankylosis (3).
The present study aimed to report the case of
isolated PFE affecting a single permanent mandibular first molar in
a 12-year-old female. Clinical and radiographic examination
revealed no mechanical obstruction and the affected molar failed to
erupt, despite available space and application of orthodontic
force. The present case highlights the requirement for heightened
clinical awareness of PFE and consideration of alternative
management strategies when conventional approaches are
unsuccessful.
Case report
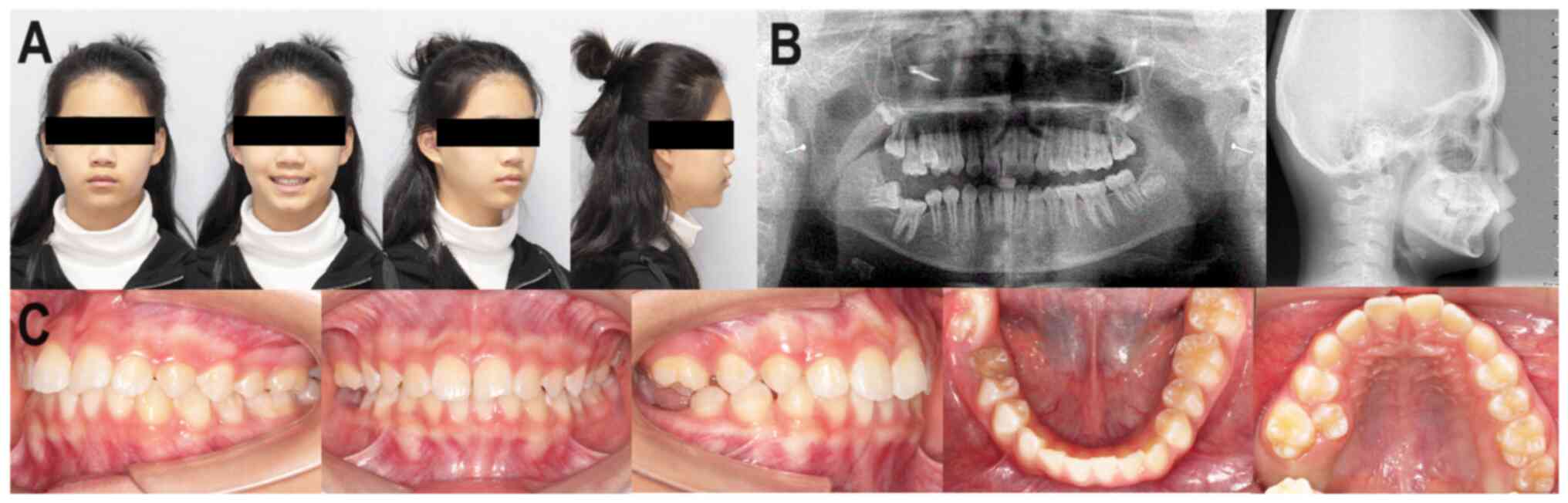
A 12-year-old female patient sought consultation at
Peking University Shenzhen Hospital (Futian, China) in January 2020
due to delayed eruption of the right mandibular first molar, an
issue that had persisted for the past six years (Fig. 1). Evaluation of the patient's
familial medical history revealed a complex and undiagnosed
treatment history in the left mandible; however, this was not
directly associated with PFE. Facial examination revealed no
notable abnormalities. Intraoral examination revealed partial
eruption of the crown of the right mandibular first molar, with
only the occlusal surface visible. By contrast, the left mandibular
first molar exhibited healthy crown development and no eruption
disturbances were observed in the remaining dentition. A Class I
(Angle's classification) (5) molar
and canine occlusion was present on the left side, whereas the
right molars displayed an open bite with no occlusal contact.
Dental cast analysis identified mild crowding in the
upper arch, while the lower arch was well-aligned. The anterior
teeth exhibited a slight deep overbite and overjet, and the curve
of Spee in the lower arch measured ~2 mm. Panoramic radiography
(Fig. 1) revealed an abnormally
low vertical position of the right mandibular first molar, with its
root apices located within the mandibular canal. There were no
obvious differences in crown or root morphology between the right
and left mandibular first molars.
Radiographic examination revealed a markedly narrow
periodontal ligament space with variable thickness. The lamina dura
surrounding the right mandibular first molar appeared poorly
defined and discontinuous compared with the left side. In addition,
a concave, pit-like defect was observed in the alveolar bone
surrounding the crown, resulting in a significantly reduced
mandibular bone height on the affected side. Notably, the right
mandibular second premolar was healthy; however, the right
mandibular second molar was horizontally impacted and the germ of
the right mandibular third molar was developing as expected.
Cephalometric analysis confirmed a Class I (Angle's classification)
(5) skeletal malocclusion.
Subsequently, the patient was preliminary diagnosed with Angle's
Class I malocclusion (5) and PFE
of the right mandibular first molar.
In the present case, the patient was provided with
the following treatment plan: i) Extraction of the bilateral
maxillary second premolar and the right mandibular first molar; ii)
alignment and retraction of the upper anterior teeth using a metal
self-ligating bracket system; iii) uprighting of the right
mandibular second molar and mesial movement to replace the missing
right mandibular first molar, thereby establishing a Class II molar
occlusion relationship (5)
bilaterally; and iv) retention and monitoring of the eruption of
the right mandibular third molar, with local correction considered,
where required, to substitute for the second molar.
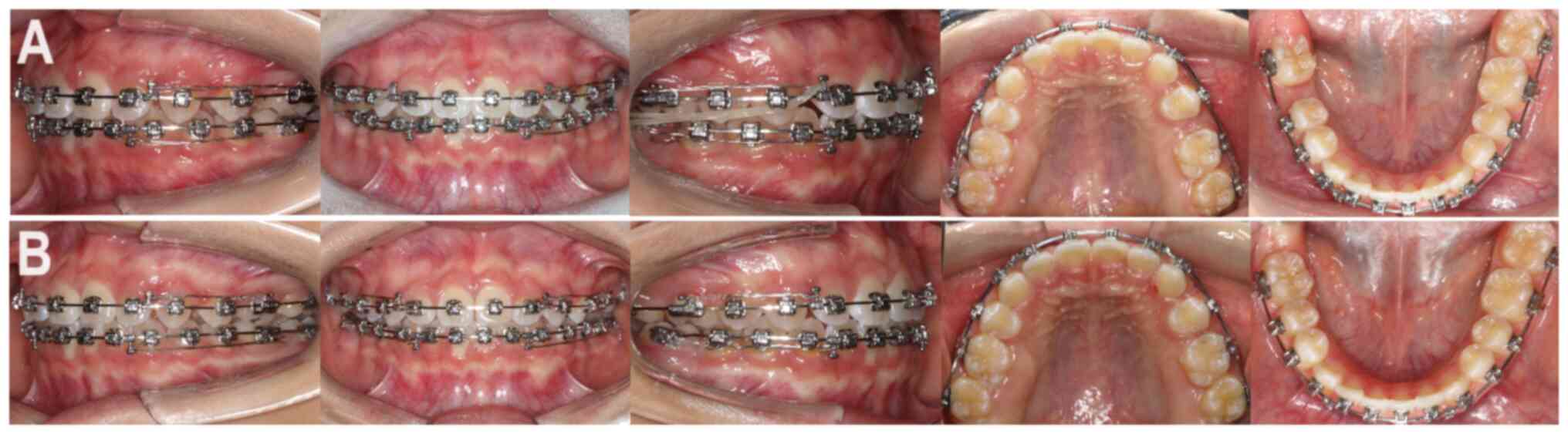
After 2 months of application of orthodontic force,
no change in the position of the molars was noticed. Therefore, it
could be confirmed that the affected tooth is a case of PFE rather
than mechanical failure of eruption. Following the extraction of
the bilateral maxillary second premolars and the right mandibular
first molar, all teeth were bonded with Damon Q self-ligating
brackets with standard torque. For aligning the teeth, round
0.014'' NiTi arch wires were used. These were subsequently replaced
by rectangular 0.014''x0.025'' NiTi arch wires, and ultimately by
rectangular 0.019''x0.025'' NiTi arch wires, implemented
sequentially for both the upper and lower dental arches (Fig. 2). To level the dental arches,
rectangular 0.018''x0.025'' stainless steel arch wires were
utilized, which ultimately facilitated the closure of spaces and
retraction of upper anterior teeth through the application of a
power chain. Final occlusal refinement marked the completion of the
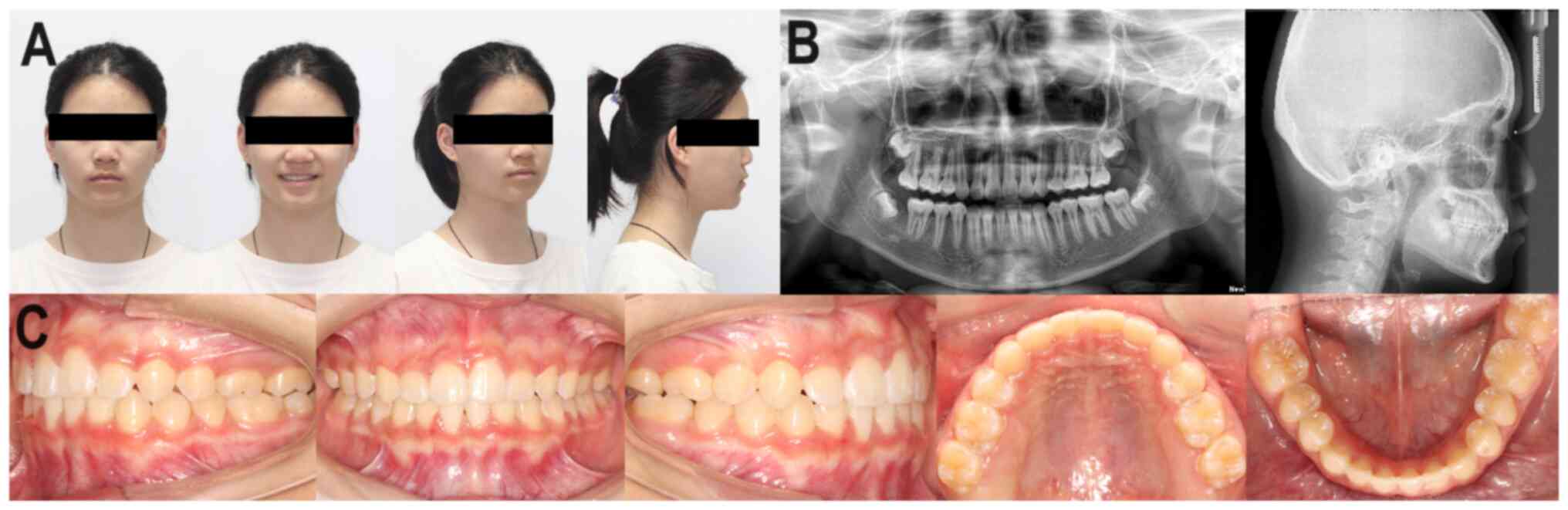
corrective treatment (Fig. 3). The
total treatment duration was 34 months. Following treatment, clear
dental retainers were provided for nocturnal wear to ensure
long-term stability (potentially lifelong).
Post-treatment evaluations demonstrated successful
repositioning of the right mandibular second molar and restoration
of alveolar bone integrity (Fig.
4). Routine follow-up examinations were scheduled
semi-annually, with oral clinical assessments serving as the
primary evaluation method, supplemented by imaging studies when
necessary. At the 1-year follow-up, the patient exhibited stable
occlusion, satisfactory anterior alignment, a favourable facial
profile and healthy development of the right mandibular third
molar.
In conclusion, early identification and intervention
in patients with PFE are critical for achieving optimal functional
and aesthetic outcomes. The present case highlights the importance
of individualized orthodontic planning and long-term follow-up.
Further research is required to better understand the mechanisms
underlying eruption disturbances and to refine treatment
strategies.
Discussion
PFE is a rare hereditary oral disease, with a
reported global prevalence of ~0.06% (1). Multiple studies confirm that PFE
exhibits familial involvement but may present with incomplete
penetrance. It is characterized by the partial or complete failure
of tooth eruption beyond the expected timeline, often resulting in
an open bite. The diagnosis excludes cases involving eruption
failure due to dentoalveolar ankylosis or other mechanical
obstructions. In PFE, bone resorption typically creates a clear
eruption pathway on the crown side of the affected tooth. However,
abnormalities within the periodontal ligament disrupt the eruption
process, preventing the tooth from reaching the occlusal plane. As
a result, the affected tooth may exhibit little or no response to
orthodontic forces, increasing the risk of developing secondary
dentoalveolar ankylosis (2).
The present study reports the case of a 12-year-old
adolescent presenting with a tooth eruption disorder confined to a
single quadrant of the mouth. The condition presented as a
localized eruption disturbance in the right mandibular quadrant,
with the first molar failing to erupt as expected, leading to an
open bite. The second molar leaned horizontally towards the first
molar and both were obstructed by the impaction of the first molar.
Consequently, occlusion on the right side could not be achieved,
resulting in compromised masticatory function.
Prior to initiating orthodontic treatment, the
patient was advised to undertake genetic testing; however, this was
declined. Thus, clinical attributes, familial medical history and
imaging results led to the diagnosis of PFE. While direct
restoration may restore occlusal function in PFE-affected teeth,
this procedure is often recommended for adult patients. This
recommendation is based on numerous factors, such as opposite tooth
elongation, low positioning of the tooth, the requirement for root
canal treatment, poorly positioned restoration margins,
insufficient resistance and fixation, and decay vulnerability.
Notably, all of the aforementioned factors may negatively impact
long-term prognosis and aesthetics (6). Considering that only a single tooth
was involved and the remaining dentition appeared as expected in
the present case, the patient chose to proceed with a treatment
plan involving extraction of the affected tooth and mesial
repositioning of the second molar as its replacement, following a
detailed discussion of the risks and benefits. This approach was
deemed more appropriate than direct restoration.
Family history may be a key factor in PFE; however,
it is not consistently present and may also exhibit incomplete
penetrance. Advances in molecular biology have suggested an
association between the pathogenic gene responsible for PFE and
PTH1R (7). This gene interacts
with PTH-related protein and PTH, both of which are essential for
healthy physiological functions. Mutations in PTH1R may disrupt the
balance between osteogenesis and osteoclastogenesis, thereby
contributing to the development of PFE. However, this genetic
mutation does not affect the Hertwig's epithelial root sheath,
which controls root development (7). Therefore, the tooth can complete its
root formation normally but lacks the cellular mechanism to
erupt.
Hendricks et al (8) identified PTH1R mutations in all
included patients with PFE, confirming an association between this
gene and the disorder. However, further research is required to
validate the potential association, clarify the underlying
molecular mechanisms and determine why these mutations selectively
affect certain teeth (8,9).
In conclusion, PFE is a tooth eruption disorder
attributed to an abnormal eruption mechanism rather than mechanical
impediments. It predominantly affects the eruption of permanent
molars and, less frequently, permanent anterior teeth. These
impacted teeth are structurally healthy and exhibit no associated
systemic symptoms. Affected teeth typically fail to respond, or
respond poorly, to orthodontic forces. Due to the impact on the
periodontal membrane, PFE may lead to dentoalveolar ankylosis.
Several studies have reported that mutations in the PTH1R gene may
precipitate PFE and early differential diagnosis can be established
via PTH1R gene screening. In the present case, the non-responsive
tooth was extracted and the second molar was repositioned to
restore occlusion. This approach corrected the mandibular
deficiency and re-established healthy masticatory function. Such a
treatment strategy may be appropriate for patients diagnosed with
PFE.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Sanming Project
of Medicine in Shenzhen (grant no. SZSM202111012) and Shenzhen Fund
for Guangdong Provincial High-level Clinical Key Specialties (grant
no. SZGSP008).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
MG contributed to writing the manuscript. WZ treated
the patient and provided critical revision of the manuscript. MG
and WZ confirm the authenticity of all the raw data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Peking University (Beijing, China) (approval no.
IRB00001053-08043).
Patient consent for publication
The guardians of the patient provided written
informed consent for the publication of the patient's medical data
and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yamaguchi T, Hosomichi K, Shirota T,
Miyamoto Y, Ono W and Ono N: Primary failure of tooth eruption:
Etiology and management. Jpn Dent Sci Rev. 58:258–267.
2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Grippaudo C, D'Apolito I, Cafiero C, Re A,
Chiurazzi P and Frazier-Bowers SA: Validating clinical
characteristic of primary failure of eruption (PFE) associated with
PTH1R variants. Prog Orthod. 22(43)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Jain U, Kallury A, Rao DD and Bharti HV:
Primary failure of eruption (PFE). BMJ Case Rep.
2015(bcr2015209703)2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Goonewardene SS, Gillatt D and Persad R: A
systematic review of PFE pre-prostatectomy. J Robot Surg.
12:397–400. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gravely JF and Johnson DB: Angle's
classification of malocclusion: An assessment of reliability. Br J
Orthod. 1:79–86. 1974.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Roulias P, Kalantzis N, Doukaki D, Pachiou
A, Karamesinis K, Damanakis G, Gizani S and Tsolakis AI: Teeth
eruption disorders: A critical review. Children (Basel).
9(771)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Stellzig-Eisenhauer A, Decker E,
Meyer-Marcotty P, Rau C, Fiebig BS, Kress W, Saar K, Rüschendorf F,
Hubner N, Grimm T, et al: Primary failure of eruption
(PFE)-clinical and molecular genetics analysis. J Orofac Orthop.
71:6–16. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hendricks HM, Bencharit S, Seaman W and
Frazier-Bowers SA: In silico and functional evaluation of PTH1R
mutations found in patients with primary failure of eruption (PFE).
Orthod Craniofac Res. 20 (Suppl 1):S57–S62. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Pilz P, Meyer-Marcotty P, Eigenthaler M,
Roth H, Weber BH and Stellzig-Eisenhauer A: Differential diagnosis
of primary failure of eruption (PFE) with and without evidence of
pathogenic mutations in the PTHR1 gene. J Orofac Orthop.
75:226–239. 2014.PubMed/NCBI View Article : Google Scholar
|