Introduction
Cervical cancer remains a major global health
burden, particularly in developing countries, with an estimated
604,000 new cases and 342,000 associated deaths worldwide in 2020,
according to the GLOBOCAN 2020 report (1). For early-stage disease, radical
hysterectomy remains a key part of curative treatment. However,
patients frequently experience substantial postoperative pain,
delayed gastrointestinal and physical recovery and an increased
rate of minor complications, all of which negatively affect their
quality of life and prolong hospitalization (2,3).
Enhanced recovery after surgery (ERAS) protocols
have gained attention for improving perioperative outcomes through
multimodal interventions. These include preoperative education,
optimized analgesia, early feeding and mobilization strategies
(4). In previous years, ERAS has
been increasingly implemented in gynecologic oncology, with studies
showing its efficacy in reducing the length of hospital stays,
opioid use and postoperative complications (5,6).
Notably, a 2023 multicenter study by Nelson et al (7) demonstrated that ERAS pathways in
gynecologic malignancies were associated with faster bowel function
recovery and improved patient satisfaction, without increasing
adverse events.
However, numerous existing ERAS studies have
emphasized surgical or anesthetic optimization, with limited
attention given to the nursing-specific implementation and
adherence of ERAS elements. Successful ERAS implementation requires
high-fidelity bedside execution of core elements, structured pain
assessment with multimodal and non-pharmacologic analgesia, early
mobilization, nutrition and patient education, a number of which
are nursing-led within perioperative workflows (8-10).
In gynecologic surgery, higher adherence to these ERAS elements is
associated with fewer complications, shorter hospital stays and
reduced readmissions, underscoring the clinical impact of
nursing-driven compliance (11).
Furthermore, the evidence supporting ERAS-based perioperative
nursing in cervical cancer surgery remains sparse, especially in
retrospective real-world settings.
Therefore, the present study aimed to evaluate the
effectiveness of ERAS-based perioperative nursing care in reducing
postoperative pain, enhancing functional recovery and lowering
complication rates in patients with cervical cancer undergoing
radical hysterectomy. We hypothesized that structured nursing-led
ERAS protocols would lead to improved early postoperative outcomes
compared with conventional nursing care.
Materials and methods
Study design
The present retrospective comparative cohort study
was performed at The Affiliated Hospital of Southwest Medical
University (Luzhou, China). The present study evaluated patients
who underwent radical hysterectomy for cervical cancer between
January 2020 and December 2023. Based on the perioperative care
pathway received, patients were divided into an ERAS group and a
control group. Clinical, surgical and nursing data were obtained
from the hospital's electronic medical record and nursing
documentation systems. The ERAS protocol was officially implemented
at the institution in February 2022, allowing for natural
allocation of patients by implementation period. A complete-case
analysis was conducted to include all eligible patients with
complete perioperative data.
Participants
Female patients who underwent elective type II or
type III radical hysterectomy for cervical cancer between January
2020 and December 2023 were screened for eligibility. The inclusion
criteria comprised: i) Histologically confirmed cervical cancer;
ii) aged between 18-75 years; iii) American Society of
Anesthesiologists (ASA) physical status classification I-III; and
iv) complete medical and nursing documentation, including
postoperative pain assessments (12). Exclusion criteria comprised: i)
History of chronic pain or psychiatric illness; ii) preoperative
opioid use; iii) emergency or palliative surgery; iv)
intraoperative conversion to an alternate procedure; and v)
readmission or reoperation within 7 days postoperatively. A
complete-case approach was used to maximize data
representativeness, resulting in a final cohort of 327 eligible
patients.
Perioperative nursing
intervention
Patients were categorized into two groups based on
the perioperative nursing protocol received. The ERAS group was
managed using a standardized institutional ERAS nursing pathway,
while the control group received conventional perioperative care.
The ERAS protocol included structured preoperative education and
counseling, shortened fasting time (clear fluids allowed up to 2 h
preoperatively), carbohydrate loading 2 h before surgery,
intraoperative normothermia maintenance, fluid restriction and
preventive multimodal analgesia with non-opioid agents.
Postoperative nursing strategies in the ERAS group focused on early
mobilization within 24 h, early oral intake, standardized pain
monitoring and non-pharmacological analgesia techniques such as
guided breathing, music therapy and psychological support. All ERAS
nurses received formal training and protocol adherence was
monitored using structured checklists, with ≥80% compliance defined
as adequate implementation. By contrast, the control group received
traditional nursing care, including prolonged preoperative fasting
(>8 h), routine opioid-based analgesia administered as needed,
delayed ambulation (>48 h postoperatively) and unstructured
patient education without standardized recovery goals.
Pain and outcome assessment
The primary outcome was postoperative pain
intensity, measured using the 10-point visual analog scale (VAS) at
6, 24 and 48 h after surgery (13). Pain assessments were part of
routine nursing care and were recorded by ward nurses. As nurses
were aware of perioperative practices (such as early mobilization
in the ERAS group), complete blinding was not feasible. However,
the use of a standardized VAS protocol helped to minimize
subjectivity. Additional pain-related outcomes included time to
first analgesia request, cumulative opioid consumption within 48 h
(converted to morphine-equivalent dose), use of patient-controlled
analgesia (PCA), use of non-opioid analgesics and application of
non-pharmacologic pain relief methods. Patient satisfaction with
pain control was assessed using a four-point Likert scale (1=very
dissatisfied; 4=very satisfied) and categorized for analysis as
‘satisfied’ (score ≥3) or ‘not satisfied’ (score <3). Secondary
outcomes included early functional recovery indicators comprising
the time to first ambulation (defined as time from arrival in the
ward to first standing or walking, assisted or unassisted), time to
first flatus, time to resume oral intake, time to urinary catheter
and analgesic pump removal and length of postoperative hospital
stay. Recovery of independent mobility was recorded as the number
of days post-surgery until walking without assistance.
Postoperative complications were recorded during hospitalization
and classified using the Clavien-Dindo grading system (14). Complication subtypes (fever,
urinary retention or wound infection) and 30-day hospital
readmissions were also recorded.
Data collection
Detailed demographic, surgical and clinical
variables were extracted from institutional electronic records,
including age, BMI, ASA physical status, International Federation
of Gynecology and Obstetrics (FIGO) stage, surgical method
(laparoscopic vs. open), surgical type (type II or III), operative
time and estimated blood loss. Comorbidities such as hypertension,
diabetes mellitus and cardiopulmonary disease were recorded, as
were lifestyle-related factors (such as smoking or alcohol use).
Laboratory parameters included preoperative hemoglobin and serum
albumin levels. Postoperative nursing records were used to capture
pain scores, analgesia use, recovery milestones (time to
ambulation, oral intake or catheter removal), complications and
discharge-related outcomes.
Statistical analysis
Data analysis was performed using SPSS version 26.0
(IBM Corp.). Normality of continuous variables was tested using the
Kolmogorov-Smirnov test. Normally distributed variables were
presented as mean ± SD and compared using independent-sample
t-tests. Non-normally distributed variables were reported as median
and interquartile range and analyzed using Mann-Whitney U tests.
Categorical variables were summarized as counts and percentages and
compared using χ2 or Fisher's exact tests, as
appropriate. To identify independent predictors of pain intensity
at 24 h, a multivariable linear regression model was constructed.
Candidate variables included ERAS care, laparoscopic surgery, use
of PCA, use of non-pharmacologic analgesia, BMI, age, ASA class,
operative time, estimated blood loss and preoperative VAS pain
score. Prior to model fitting, collinearity diagnostics were
performed using variance inflation factor (VIF) and no variables
exceeded the conventional threshold (VIF <2 for all predictors).
The model's goodness of fit was evaluated using adjusted
R2 and the F-statistic. Two-tailed P<0.05 was
considered to indicate a statistically significant difference.
Results
Baseline characteristics of the
present study population
A total of 327 patients undergoing radical surgery
for cervical cancer were included in the present analysis, with 162
assigned to the ERAS group and 165 to the control group (Table I). The two groups were well
balanced with regard to baseline demographic and clinical
characteristics. The mean age was 49.8±8.3 years in the ERAS group
and 50.5±8.1 years in the control group (P=0.368). BMI was
comparable between groups (23.4±3.2 vs. 23.1±3.4 kg/m², P=0.422).
Distribution of education level (P=0.289), ASA physical status
(P=0.733) and FIGO stage (P=0.648) showed no statistically
significant differences between groups. Laparoscopic surgery was
performed in 59.3% of patients in the ERAS group and 55.2% in the
control group (P=0.518), and the proportion of type III radical
hysterectomy was similar (27.8 vs. 29.1%; P=0.782). Operative time
(P=0.117), estimated blood loss (P=0.212), preoperative VAS pain
score (P=0.296), and the prevalence of comorbidities such as
hypertension (P=0.691) and diabetes mellitus (P=0.765) were
comparable. No significant differences were observed in smoking
(P=0.799), alcohol use (P=0.384), or laboratory parameters
including preoperative albumin (P=0.561) and hemoglobin (P=0.472).
Overall, there were no statistically significant differences in any
baseline characteristics between the two groups, indicating good
comparability prior to intervention.
 | Table IBaseline characteristics of patients
with cervical cancer undergoing surgery in the ERAS and control
groups. |
Table I
Baseline characteristics of patients
with cervical cancer undergoing surgery in the ERAS and control
groups.
| Variable | ERAS group
(n=162) | Control group
(n=165) | P-value |
|---|
| Age, years | 49.8±8.3 | 50.5±8.1 | 0.368 |
| BMI,
kg/m2 | 23.4±3.2 | 23.1±3.4 | 0.422 |
| Education level | | | 0.289 |
|
Primary or
below | 18 (11.1) | 22 (13.3) | |
|
Secondary | 84 (51.9) | 90 (54.5) | |
|
Tertiary or
above | 60 (37.0) | 53 (32.1) | |
| ASA physical
status | | | 0.733 |
|
I | 68 (42.0) | 65 (39.4) | |
|
II | 81 (50.0) | 86 (52.1) | |
|
III | 13 (8.0) | 14 (8.5) | |
| FIGO stage | | | 0.648 |
|
IA-IB | 108 (66.7) | 104 (63.0) | |
|
IIA-IIB | 54 (33.3) | 61 (37.0) | |
| Surgical
approach | | | 0.518 |
|
Laparoscopic | 96 (59.3) | 91 (55.2) | |
|
Open | 66 (40.7) | 74 (44.8) | |
| Surgical type
III | 45 (27.8) | 48 (29.1) | 0.782 |
| Operative time,
min | 184.6±31.2 | 179.8±34.1 | 0.117 |
| Median estimated
blood loss, ml (IQR) | 200 (150-300) | 220 (160-320) | 0.212 |
| Preoperative VAS pain
score | 1.2±0.8 | 1.3±0.9 | 0.296 |
| Hypertension | 24 (14.8) | 27 (16.4) | 0.691 |
| Diabetes
mellitus | 16 (9.9) | 18 (10.9) | 0.765 |
| Cardiopulmonary
disease | 9 (5.6) | 13 (7.9) | 0.419 |
| Smoking history | 19 (11.7) | 21 (12.7) | 0.799 |
| Alcohol use | 17 (10.5) | 23 (13.9) | 0.384 |
| Preoperative albumin,
g/l | 42.1±3.8 | 41.9±3.5 | 0.561 |
| Hemoglobin, g/l | 125.2±10.9 | 124.5±11.3 | 0.472 |
Postoperative pain and analgesia
outcomes
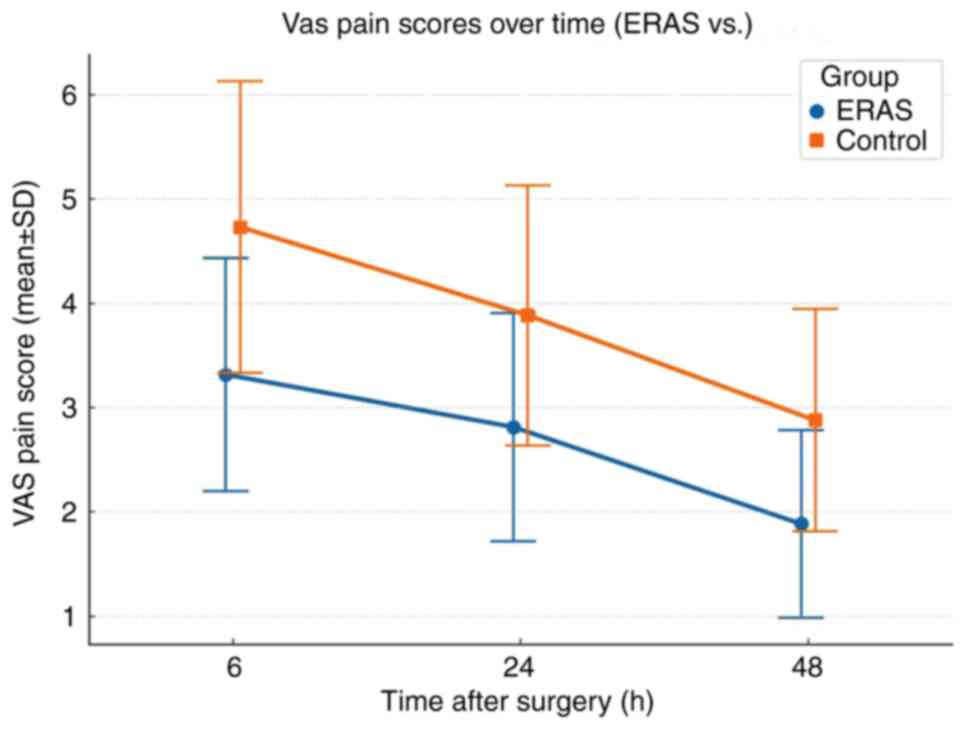
Postoperative pain intensity was significantly lower
in the ERAS group compared with the control group at all
postoperative time points (Table
II). At 6 h after surgery, the mean VAS score was 3.4±1.2 in
the ERAS group and 4.8±1.4 in the control group (P<0.001). This
difference remained significant at 24 h (2.7±1.1 vs. 3.9±1.3;
P<0.001) and 48 h (1.9±0.9 vs. 2.7±1.1; P<0.001). Although
both groups showed reductions in pain from 6 to 48 h
postoperatively, the magnitude of reduction was smaller in the ERAS
group (1.5±0.7 vs. 2.1±0.9; P=0.002), suggesting improved early
pain control. As shown in Table
II, patients in the ERAS group required significantly lower
cumulative opioid doses within the first 48 h postoperatively
(14.2±5.6 vs. 20.6±6.3 mg morphine equivalents; P<0.001).
Additionally, the proportion of patients requiring PCA was
significantly lower in the ERAS group (31.5%) compared with the
control group (58.8%; P<0.001). The use of non-opioid analgesics
(72.8 vs. 58.2%; P=0.005) and application of multimodal analgesia
strategies (51.9 vs. 28.5%; P<0.001) were significantly more
common among patients receiving ERAS-based care. Non-pharmacologic
interventions were also more frequently implemented in the ERAS
group, as summarized in Table II.
Methods such as guided breathing and music therapy were employed
with 42.6% of patients in the ERAS group compared with only 17.0%
in the control group (P<0.001). Furthermore, the time to first
analgesia request was longer in the ERAS group (3.9±1.4 h) compared
with in the control group (2.6±1.2 h; P<0.001), suggesting
improved pain tolerance. Notably, patient satisfaction with
postoperative pain management was significantly higher in the ERAS
group (82.7 vs. 58.2%; P<0.001). Together these results
indicated that the ERAS-based nursing pathway markedly improved
pain control, reduced reliance on opioids, encouraged multimodal
and non-pharmacologic pain strategies and enhanced patient
satisfaction during the early postoperative period in patients with
cervical cancer (Table II and
Fig. 1). In the present study, the
overall adherence rate to the ERAS nursing protocol was
approximately 86.4%, with no notable differences in compliance
across individual ERAS elements. Core components such as
preoperative counseling, shortened fasting, multimodal analgesia,
early mobilization, and early oral intake all demonstrated
adherence rates above 80%, indicating consistent application of key
protocol elements.
 | Table IIComparison of postoperative
pain-related outcomes between ERAS and control groups. |
Table II
Comparison of postoperative
pain-related outcomes between ERAS and control groups.
| A, VAS pain scores
and dynamics |
|---|
| Variable | ERAS group
(n=162) | Control group
(n=165) | P-value |
|---|
| VAS score at 6
h | 3.4±1.2; [3
(3-4)] | 4.8±1.4; [5
(4-6)] | 0.000001 |
| VAS score at 24
h | 2.7±1.1; [3
(2-3)] | 3.9±1.3; [4
(3-5)] | 0.000003 |
| VAS score at 48
h | 1.9±0.9; [2
(1-2)] | 2.7±1.1; [3
(2-3)] | 0.000024 |
| VAS reduction 6-48
h | 1.5±0.7; [2
(1-2)] | 2.1±0.9; [2
(2-3)] | 0.002 |
| B, Analgesic use
and methods |
| Variable | ERAS group | Control group | P-value |
| Cumulative opioid
dose, mg | 14.2±5.6; [14
(10-18)] | 20.6±6.3; [20
(16-25)] | 0.000001 |
| Use of PCA
devices, | 51 (31.5) | 97 (58.8) | 0.000015 |
| Non-opioid
analgesics used | 118 (72.8) | 96 (58.2) | 0.005 |
| Multimodal
analgesia applied | 84 (51.9) | 47 (28.5) | 0.000038 |
| C,
Non-pharmacologic and satisfaction outcomes |
| Variable | ERAS group | Control group | P-value |
| Use of
non-pharmacological pain relief | 69 (42.6) | 28 (17.0) | 0.000004 |
| Time to first
request for analgesia, h | 3.9±1.4; [4
(3-5)] | 2.6±1.2; [3
(2-3)] | 0.000009 |
| Patient
satisfaction with pain management | 134 (82.7) | 96 (58.2) | 0.000003 |
Postoperative recovery and
complications
Patients in the ERAS group demonstrated
significantly faster postoperative recovery across multiple
indicators compared with those in the control group (Table III). The median time to first
ambulation was 18 h in the ERAS group compared with 27 h in the
control group (P<0.001), while time to first flatus and oral
intake were also reduced in the ERAS group (30 vs. 40 h and 17 vs.
31 h, respectively; both P<0.001). The removal of urinary
catheters and analgesic pumps occurred earlier in the ERAS group
(30.6±5.7 and 41.3±6.5 h) compared with the control group (39.1±6.2
and 53.8±8.4 h; both P<0.001). Overall, functional recovery was
improved in the ERAS group. The average time to independent walking
was 1.8±0.7 days in the ERAS group compared with 2.5±0.9 days in
the control group (P<0.001). Additionally, a higher proportion
of patients in the ERAS group were discharged without assistance
(88.9 vs. 71.5%; P<0.001). The median postoperative hospital
stay was significantly shorter in the ERAS group [5 (4-6)
days] compared with in the control group [7 (6-9)
days; P<0.001]. The overall incidence of postoperative
complications was lower in the ERAS group (8.0%) compared with the
control group (17.6%; P=0.009). Minor complications (Clavien-Dindo
grades I-II) were significantly reduced in the ERAS group (5.6 vs.
12.7%; P=0.031). There was no significant difference in the rate of
major complications (Clavien-Dindo grades III-IV) between groups
(P=0.283). Specific complications such as fever (P=0.065), urinary
retention (P=0.163) and wound infection (P=0.337) occurred less
frequently in the ERAS group, although the differences were not
statistically significant. The 30-day readmission rate was also
lower in the ERAS group (2.5 vs. 4.8%), but the difference did not
reach statistical significance (P=0.283). These findings suggested
that ERAS-based perioperative nursing markedly improved
postoperative functional recovery and reduced minor complications
in patients with cervical cancer undergoing surgery.
 | Table IIIPostoperative recovery and
complications between ERAS and control groups. |
Table III
Postoperative recovery and
complications between ERAS and control groups.
| A, Early recovery
indicators |
|---|
| Variable | ERAS group
(n=162) | Control group
(n=165) | P-value |
|---|
| Time to first
ambulation, h | 18 (15-22) | 27 (23-34) | 0.000002 |
| Time to first
flatus, h | 30 (26-35) | 40 (34-46) | 0.000004 |
| Time to resume oral
intake, h | 17 (14-20) | 31 (25-36) | 0.000001 |
| Time to remove
urinary catheter, h | 30.6±5.7 | 39.1±6.2 | 0.000003 |
| Time to stop
analgesic pump, h | 41.3±6.5 | 53.8±8.4 | 0.000002 |
| B, Overall recovery
and discharge |
| Variable | ERAS group
(n=162) | Control group
(n=165) | P-value |
| Postoperative
hospital stay, days | 5 (4-6) | 7 (6-9) | 0.000001 |
| Time to independent
walking, days | 1.8±0.7 | 2.5±0.9 | 0.000006 |
| Discharged without
assistance, n (%) | 144 (88.9) | 118 (71.5) | 0.000013 |
| C, Postoperative
complications |
| Variable | ERAS group
(n=162) | Control group
(n=165) | P-value |
| Any complication, n
(%) | 13 (8.0) | 29 (17.6) | 0.009 |
| Clavien-Dindo grade
I-II, n (%) | 9 (5.6) | 21 (12.7) | 0.031 |
| Clavien-Dindo grade
III-IV, n (%) | 4 (2.5) | 8 (4.8) | 0.283 |
| Fever (>38.5˚C),
n (%) | 6 (3.7) | 14 (8.5) | 0.065 |
| Urinary retention,
n (%) | 4 (2.5) | 9 (5.5) | 0.163 |
| Wound infection, n
(%) | 3 (1.9%) | 6 (3.6) | 0.337 |
| 30-day readmission,
n (%) | 4 (2.5) | 8 (4.8) | 0.283 |
Factors associated with postoperative
pain at 24 h
Multivariate linear regression analysis identified
several independent predictors of VAS pain score at 24 h
postoperatively (Table IV).
ERAS-based nursing care was significantly associated with lower
pain scores (β=-1.05; 95%CI: -1.34 to -0.76; P<0.001). The use
of non-pharmacological analgesia methods also contributed to
reduced pain (β=-0.39; P=0.010), while the use of PCA was
associated with higher reported pain scores (β=0.51; P<0.001),
perhaps reflecting more severe discomfort requiring intervention.
Higher preoperative VAS scores (β=0.18; P=0.017), greater blood
loss (β=0.09 per 100 ml; P=0.032) and longer operative times
(β=0.05 per 10 min; P=0.021) were also positively associated with
increased postoperative pain. Laparoscopic surgery was
independently associated with lower pain scores compared with open
surgery (β=-0.46; P=0.006). Higher BMI was significantly associated
with increased pain scores (β=0.06; P=0.031), whereas age and ASA
class showed no significant associations. The overall model
demonstrated good fit and explanatory power (F=8.41; P<0.001;
adjusted R2=0.37), indicating that ERAS nursing and
intraoperative factors together accounted for a meaningful
proportion of variance in early postoperative pain. Collinearity
diagnostics confirmed no evidence of multicollinearity among
predictors (all VIF <2).
 | Table IVMultivariate linear regression
analysis of factors associated with VAS pain score at 24 h
postoperatively (n=327). |
Table IV
Multivariate linear regression
analysis of factors associated with VAS pain score at 24 h
postoperatively (n=327).
| Variable | β coefficient | 95% CI | P-value |
|---|
| ERAS nursing care
(yes vs. no) | -1.05 | -1.34 to -0.76 | 0.000002 |
| Preoperative VAS
pain score | 0.18 | 0.03 to 0.33 | 0.017 |
| Use of PCA (yes vs.
no) | 0.51 | 0.23 to 0.80 | 0.000004 |
| Use of
non-pharmacological analgesia (yes vs. no) | -0.39 | -0.68 to -0.09 | 0.010 |
| Laparoscopic
surgery (vs. open) | -0.46 | -0.80 to -0.13 | 0.006 |
| Age (per 1 year
increase) | 0.01 | -0.01 to 0.03 | 0.264 |
| BMI, kg/m2 | 0.06 | 0.01 to 0.11 | 0.031 |
| ASA class III (vs.
I-II) | 0.28 | -0.02 to 0.58 | 0.069 |
| Operative time (per
10 min increase) | 0.05 | 0.01 to 0.10 | 0.021 |
| Estimated blood
loss (per 100 ml increase) | 0.09 | 0.01 to 0.18 | 0.032 |
Discussion
The present retrospective cohort study provided
evidence to support the effectiveness of ERAS-based perioperative
nursing in enhancing postoperative outcomes among patients with
cervical cancer undergoing radical hysterectomy. Compared with
conventional care, patients managed under ERAS nursing protocols
reported significantly lower pain scores, faster recovery, reduced
opioid usage and fewer minor complications, all without increased
rates of major adverse events or readmission.
Effective pain management is a key part of
successful postoperative recovery. The present findings showed that
ERAS care significantly reduced pain intensity at 6, 24 and 48 h
postoperatively, aligning with previous ERAS studies in gynecologic
malignancies (15-17).
This improvement may be attributed to the integrated use of
multimodal analgesia, reduced opioid dependence and the increased
adoption of non-pharmacologic interventions, such as guided
breathing and music therapy. Multivariate regression analysis
confirmed ERAS nursing as an independent predictor of reduced VAS
pain score at 24 h. These findings highlight the key influence of
structured nursing-led protocols in optimizing early postoperative
pain trajectories.
In addition to superior pain control, patients in
the ERAS group achieved earlier mobilization, faster return of
gastrointestinal function and shorter hospitalization, objectives
that are key to ERAS (18,19). The present findings revealed that
patients in the ERAS group achieved earlier ambulation (median, 18
vs. 27 h) and oral intake (17 vs. 31 h), and a higher proportion
(88.9 vs. 71.5%) were discharged without assistance, reflecting
superior early functional recovery. This finding aligns with recent
prospective studies indicating that early ambulation after
abdominal or pelvic cancer surgery is associated with a reduced
risk of postoperative venous thromboembolism and paralytic ileus
(20,21). These benefits are plausibly
mediated by ERAS nursing components that promote early mobilization
and multimodal, opioid-sparing analgesia, which together reduce
opioid-related gastrointestinal hypomotility and facilitate earlier
activity and feeding (18-21).
Preoperative counseling and goal-setting may enhance patient
participation and adherence, supporting earlier independent
ambulation and discharge.
Notably, ERAS care was associated with a lower
incidence of Clavien-Dindo grade I-II complications. While the
reduction in major complications and readmission was not
statistically significant, the observed trends suggest a positive
clinical trajectory (22-24).
Consistent implementation of nursing-led elements, such as
optimized fluid management, active temperature maintenance and
structured postoperative monitoring, has been linked to fewer minor
infections and urinary complications in ERAS pathways, which is
concordant with the present study findings (8,11,22).
A key strength of the present study lies in its
nursing-centered focus. Numerous ERAS studies emphasize surgical
techniques or anesthetic interventions yet overlook the operational
role of nursing staff (25,26).
The present findings reinforced that the quality and consistency of
nursing practice were central to ERAS success. Trained nurses were
responsible not only for implementing daily care interventions, but
also for promoting patient education, protocol adherence and
recovery assessment, all factors shown to influence ERAS outcomes
across specialties (27).
However, several limitations warrant consideration.
First, the retrospective design inherently carries risks of
information and selection bias, even with statistical adjustments.
Second, the present study was conducted at a single academic
institution, which may limit generalizability, particularly in
settings lacking dedicated ERAS training programs. Third,
postoperative pain scores were documented by ward nurses as part of
routine clinical care. As the nurses were aware of perioperative
practices (including earlier ambulation and oral intake in the ERAS
group), true blinding was not feasible. This limitation raised the
possibility of detection bias, although the standardized use of the
VAS scale aimed to minimize subjectivity. Fourth, as allocation was
purely time-based (2020-2021 for conventional care and February
2022 onwards for ERAS) potential temporal confounding factors, such
as gradual refinements in surgical practice, evolving hospital
protocols and the impact of the COVID-19 pandemic cannot be
completely excluded. This may have introduced a degree of detection
bias, although standardized use of the VAS scale was applied to
mitigate subjectivity. With this, patient-level factors such as
anxiety, depression and cultural attitudes toward pain, which are
known to influence postoperative outcomes, were not captured in
this analysis. Fifth, nursing compliance rates or ERAS fidelity
scores were not quantified, both of which are key metrics in ERAS
implementation science. Lastly, long-term functional outcomes,
patient-reported quality of life and cost-effectiveness were not
evaluated in the present study but remain important targets for
future prospective research.
In conclusion, the present study demonstrated that
ERAS-based perioperative nursing was associated with improved pain
management, faster recovery and lower minor complication rates in
cervical cancer surgery. These findings support the integration of
standardized nursing protocols within ERAS frameworks and
underscore the need for scalable, nurse-led ERAS models in
gynecologic oncology.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
LM contributed to the study design, data collection
and manuscript drafting. RL participated in data curation,
statistical analysis and interpretation of results. XW assisted
with patient screening, clinical data extraction and literature
review. ZX was responsible for coordinating clinical procedures and
quality control of perioperative data. ZW contributed to the
implementation of the ERAS nursing protocol and provided key
revisions to the manuscript. LC contributed to the conception and
design of the study, critically reviewed all data analyses for
methodological accuracy, guided the interpretation of findings and
revised the manuscript for important intellectual content. LM and
RL confirm the authenticity of all the raw data. All authors have
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study was conducted in accordance with
the Declaration of Helsinki and was approved by the Ethics
Committee of The Affiliated Hospital of Southwest Medical
University (approval no. KY2025317). Due to the retrospective
nature of the present study and the use of anonymized patient data,
the requirement for informed consent was waived by the
committee.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Li DL, Li W and Chen ZJ: Enhanced recovery
after surgery in the perioperative period promotes recovery of
cervical cancer patients undergoing transabdominal radical
resection. Am J Transl Res. 17:230–238. 2025.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Benlolo S, Hanlon JG, Shirreff L, Lefebvre
G, Husslein H and Shore EM: Predictors of persistent postsurgical
pain after hysterectomy-A prospective cohort study. J Minim
Invasive Gynecol. 28:2036–2046.e1. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ljungqvist O, Scott M and Fearon KC:
Enhanced recovery after surgery: A review. JAMA Surg. 152:292–298.
2017.
|
|
5
|
Bhandoria GP, Bhandarkar P, Ahuja V,
Maheshwari A, Sekhon RK, Gultekin M, Ayhan A, Demirkiran F,
Kahramanoglu I, Wan YL, et al: Enhanced recovery after surgery
(ERAS) in gynecologic oncology: An international survey of
peri-operative practice. Int J Gynecol Cancer. 30:1471–1478.
2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bisch SP, Jago CA, Kalogera E, Ganshorn H,
Meyer LA, Ramirez PT, Dowdy SC and Nelson G: Outcomes of enhanced
recovery after surgery (ERAS) in gynecologic oncology-A systematic
review and meta-analysis. Gynecol Oncol. 161:46–55. 2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Nelson G, Fotopoulou C, Taylor J, Glaser
G, Bakkum-Gamez J, Meyer LA, Stone R, Mena G, Elias KM, Altman AD,
et al: Enhanced recovery after surgery (ERAS®) society
guidelines for gynecologic oncology: Addressing implementation
challenges-2023 update. Gynecol Oncol. 173:58–67. 2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Balfour A, Amery J, Burch J and
Smid-Nanninga H: Enhanced recovery after surgery (ERAS): Barriers
and solutions for nurses. Asia Pac J Oncol Nurs.
9(100040)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Brown D and Xhaja A: Nursing perspectives
on enhanced recovery after surgery. Surg Clin North Am.
98:1211–1221. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Akbuğa GA and Yılmaz K: Obstacles to
compliance and implementation of ERAS protocol from nursing
perspective: A qualitative study. J Perianesth Nurs. 40:331–336.
2025.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hayek J, Zorrilla-Vaca A, Meyer LA, Mena
G, Lasala J, Iniesta MD, Suki T, Huepenbecker S, Cain K,
Garcia-Lopez J and Ramirez PT: Patient outcomes and adherence to an
enhanced recovery pathway for open gynecologic surgery: A 6-year
single-center experience. Int J Gynecol Cancer. 32:1443–1449.
2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mayhew D, Mendonca V and Murthy BVS: A
review of ASA physical status-historical perspectives and modern
developments. Anaesthesia. 74:373–379. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Myles PS, Myles DB, Galagher W, Boyd D,
Chew C, MacDonald N and Dennis A: Measuring acute postoperative
pain using the visual analog scale: The minimal clinically
important difference and patient acceptable symptom state. Br J
Anaesth. 118:424–429. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Clavien PA, Barkun J, de Oliveira ML,
Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J,
Slankamenac K, Bassi C, et al: The Clavien-Dindo classification of
surgical complications: Five-year experience. Ann Surg.
250:187–196. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chao L, Lin E and Kho K: Enhanced recovery
after surgery in minimally invasive gynecologic surgery. Obstet
Gynecol Clin North Am. 49:381–395. 2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Asklid D, Ljungqvist O, Xu Y and
Gustafsson UO: Short-term outcome in robotic vs. laparoscopic and
open rectal tumor surgery within an ERAS protocol: A retrospective
cohort study from the Swedish ERAS database. Surg Endosc.
36:2006–2017. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bogani G, Sarpietro G, Ferrandina G,
Gallotta V, DI Donato V, Ditto A, Pinelli C, Casarin J, Ghezzi F,
Scambia G and Raspagliesi F: Enhanced recovery after surgery (ERAS)
in gynecology oncology. Eur J Surg Oncol. 47:952–959.
2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Nelson G: Enhanced recovery in gynecologic
oncology surgery-state of the science. Curr Oncol Rep.
25:1097–1104. 2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ding Y, Zhang X, Qiu J, Zhang J and Hua K:
Assessment of ESGO quality indicators in cervical cancer surgery: A
real-world study in a high-volume chinese hospital. Front Oncol.
12(802433)2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Porserud A, Aly M, Nygren-Bonnier M and
Hagströmer M: Association between early mobilisation after
abdominal cancer surgery and postoperative complications. Eur J
Surg Oncol. 49(106943)2023.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Egger EK, Merker F, Ralser DJ, Marinova M,
Vilz TO, Matthaei H, Hilbert T and Mustea A: Postoperative
paralytic ileus following debulking surgery in ovarian cancer
patients. Front Surg. 9(976497)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tazreean R, Nelson G and Twomey R: Early
mobilization in enhanced recovery after surgery pathways: Current
evidence and recent advancements. J Comp Eff Res. 11:121–129.
2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Shen Y, Lv F, Min S, Wu G, Jin J, Gong Y,
Yu J, Qin P and Zhang Y: Impact of enhanced recovery after surgery
protocol compliance on patients' outcome in benign hysterectomy and
establishment of a predictive nomogram model. BMC Anesthesiol.
21(289)2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chen Y, Wan J, Zhu Z, Su C and Mei Z:
Embedding evidence of early postoperative off-bed activities and
rehabilitation in a real clinical setting in China: An interrupted
time-series study. BMC Nurs. 21(98)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wainwright TW, Jakobsen DH and Kehlet H:
The current and future role of nurses within enhanced recovery
after surgery pathways. Br J Nurs. 31:656–659. 2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Peña CG: What makes a nurse a good ERAS
nurse? Asia Pac J Oncol Nurs. 9(100034)2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Francis NK, Walker T, Carter F, Hübner M,
Balfour A, Jakobsen DH, Burch J, Wasylak T, Demartines N, Lobo DN,
et al: Consensus on training and implementation of enhanced
recovery after surgery: A delphi study. World J Surg. 42:1919–1928.
2018.PubMed/NCBI View Article : Google Scholar
|