|
1
|
Abdulkareem AA, Al-Taweel FB, Al-Sharqi
AJB, Gul SS, Sha A and Chapple ILC: Current concepts in the
pathogenesis of periodontitis: From symbiosis to dysbiosis. J Oral
Microbiol. 15(2197779)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Meyle J and Chapple I: Molecular aspects
of the pathogenesis of periodontitis. Periodontol 2000. 69:7–17.
2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hajishengallis G and Chavakis T: Local and
systemic mechanisms linking periodontal disease and inflammatory
comorbidities. Nat Rev Immunol. 21:426–440. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tonetti MS, Greenwell H and Kornman KS:
Staging and grading of periodontitis: Framework and proposal of a
new classification and case definition. J Clin Periodontol 45
Suppl. 20:S149–S161. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kwon T, Lamster IB and Levin L: Current
concepts in the management of periodontitis. Int Dent J.
71:462–476. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Graziani F, Karapetsa D, Alonso B and
Herrera D: Nonsurgical and surgical treatment of periodontitis: How
many options for one disease? Periodontol 2000. 75:152–188.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Slots J: Periodontitis: Facts, fallacies
and the future. Periodontol 2000. 75:7–23. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Haque MM, Yerex K, Kelekis-Cholakis A and
Duan K: Advances in novel therapeutic approaches for periodontal
diseases. BMC Oral Health. 22(492)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Preshaw PM and Bissett SM: Periodontitis
and diabetes. Br Dent J. 227:577–584. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Zhou N, Zou F, Cheng X, Huang Y, Zou H,
Niu Q, Qiu Y, Shan F, Luo A, Teng W and Sun J: Porphyromonas
gingivalis induces periodontitis, causes immune imbalance, and
promotes rheumatoid arthritis. J Leukoc Biol. 110:461–473.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Cardoso EM, Reis C and Manzanares-Céspedes
MC: Chronic periodontitis, inflammatory cytokines, and
interrelationship with other chronic diseases. Postgrad Med.
130:98–104. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Persson GR: Periodontal complications with
age. Periodontol 2000. 78:185–194. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Napimoga MH, Nametala C, da Silva FL,
Miranda TS, Bossonaro JP, Demasi AP and Duarte PM: Involvement of
the Wnt-β-catenin signalling antagonists, sclerostin and
dickkopf-related protein 1, in chronic periodontitis. J Clin
Periodontol. 41:550–557. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mihara A, Yukata K, Seki T, Iwanaga R,
Nishida N, Fujii K, Nagao Y and Sakai T: Effects of sclerostin
antibody on bone healing. World J Orthop. 12:651–659.
2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jacobsen CM: Application of
anti-Sclerostin therapy in non-osteoporosis disease models. Bone.
96:18–23. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kitaura H, Marahleh A, Ohori F, Noguchi T,
Shen WR, Qi J, Nara Y, Pramusita A, Kinjo R and Mizoguchi I:
Osteocyte-related cytokines regulate osteoclast formation and bone
resorption. Int J Mol Sci. 21(5169)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Liao C, Liang S, Wang Y, Zhong T and Liu
X: Sclerostin is a promising therapeutic target for oral
inflammation and regenerative dentistry. J Transl Med.
20(221)2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chatzopoulos GS, Costalonga M, Mansky KC
and Wolff LF: WNT-5a and SOST levels in gingival crevicular fluid
depend on the inflammatory and osteoclastogenic activities of
periodontal tissues. Medicina (Kaunas). 57(788)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yakar N, Guncu GN, Akman AC, Pınar A,
Karabulut E and Nohutcu RM: Evaluation of gingival crevicular fluid
and peri-implant crevicular fluid levels of sclerostin, TWEAK,
RANKL and OPG. Cytokine. 113:433–439. 2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chatzopoulos GS, Koidou VP and Wolff LF:
Expression of Wnt signaling agonists and antagonists in
periodontitis and healthy subjects, before and after non-surgical
periodontal treatment: A systematic review. J Periodontal Res.
57:698–710. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chatzopoulos GS, Mansky KC, Lunos S,
Costalonga M and Wolff LF: Sclerostin and WNT-5a gingival protein
levels in chronic periodontitis and health. J Periodontal Res.
54:555–565. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ozden FO, Demir E, Lutfioglu M, Acarel EE,
Bilgici B and Atmaca A: Effects of periodontal and bisphosphonate
treatment on the gingival crevicular levels of sclerostin and
dickkopf-1 in postmenopausal osteoporosis with and without
periodontitis. J Periodontal Res. 57:849–858. 2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Delgado-Calle J, Sato AY and Bellido T:
Role and mechanism of action of sclerostin in bone. Bone. 96:29–37.
2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Iwamoto R, Koide M, Udagawa N and
Kobayashi Y: Positive and negative regulators of sclerostin
expression. Int J Mol Sci. 23(4895)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Tanaka S and Matsumoto T: Sclerostin: From
bench to bedside. J Bone Miner Metab. 39:332–340. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Cosman F, Crittenden DB, Adachi JD,
Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki
EM, Miyauchi A, et al: Romosozumab treatment in postmenopausal
women with osteoporosis. N Engl J Med. 375:1532–1543.
2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Martiniakova M, Babikova M and Omelka R:
Pharmacological agents and natural compounds: Available treatments
for osteoporosis. J Physiol Pharmacol. 71:2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tinsley BA, Dukas A, Pensak MJ, Adams DJ,
Tang AH, Ominsky MS, Ke HZ and Lieberman JR: Systemic
administration of sclerostin antibody enhances bone morphogenetic
protein-induced femoral defect repair in a rat model. J Bone Joint
Surg Am. 97:1852–1859. 2015.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Korn P, Kramer I, Schlottig F, Tödtman N,
Eckelt U, Bürki A, Ferguson SJ, Kautz A, Schnabelrauch M, Range U,
et al: Systemic sclerostin antibody treatment increases
osseointegration and biomechanical competence of
zoledronic-acid-coated dental implants in a rat osteoporosis model.
Eur Cell Mater. 37:333–346. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Virdi AS, Irish J, Sena K, Liu M, Ke HZ,
McNulty MA and Sumner DR: Sclerostin antibody treatment improves
implant fixation in a model of severe osteoporosis. J Bone Joint
Surg Am. 97:133–140. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Li X, Ominsky MS, Villasenor KS, Niu QT,
Asuncion FJ, Xia X, Grisanti M, Wronski TJ, Simonet WS and Ke HZ:
Sclerostin antibody reverses bone loss by increasing bone formation
and decreasing bone resorption in a rat model of male osteoporosis.
Endocrinology. 159:260–271. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Cumpston M, Li T, Page MJ, Chandler J,
Welch VA, Higgins JP and Thomas J: Updated guidance for trusted
systematic reviews: A new edition of the cochrane handbook for
systematic reviews of interventions. Cochrane Database Syst Rev.
10(ED000142)2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Drevon D, Fursa SR and Malcolm AL:
Intercoder reliability and validity of WebPlotDigitizer in
extracting graphed data. Behav Modif. 41:323–339. 2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Hooijmans CR, Rovers MM, de Vries RB,
Leenaars M, Ritskes-Hoitinga M and Langendam MW: SYRCLE's risk of
bias tool for animal studies. BMC Med Res Methodol.
14(43)2014.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Higgins JPT and Green S: Cochrane handbook
for systematic reviews of interventions. Version 5.1.0. The
Cochrane Collaboration, London, 2011. www.handbook.cochrane.org.
|
|
37
|
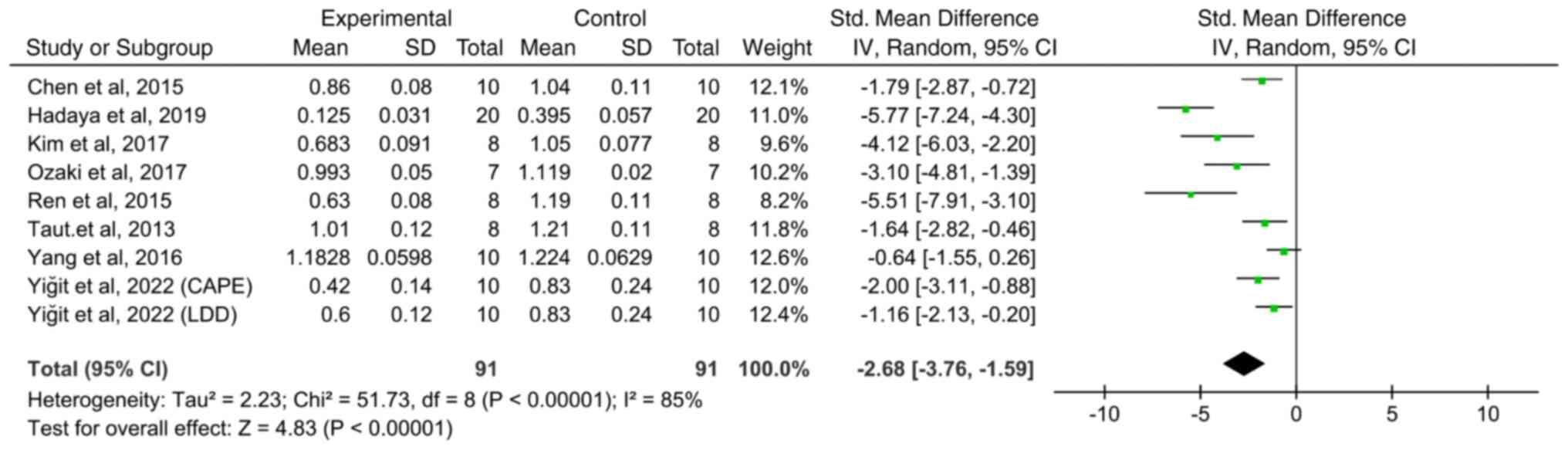
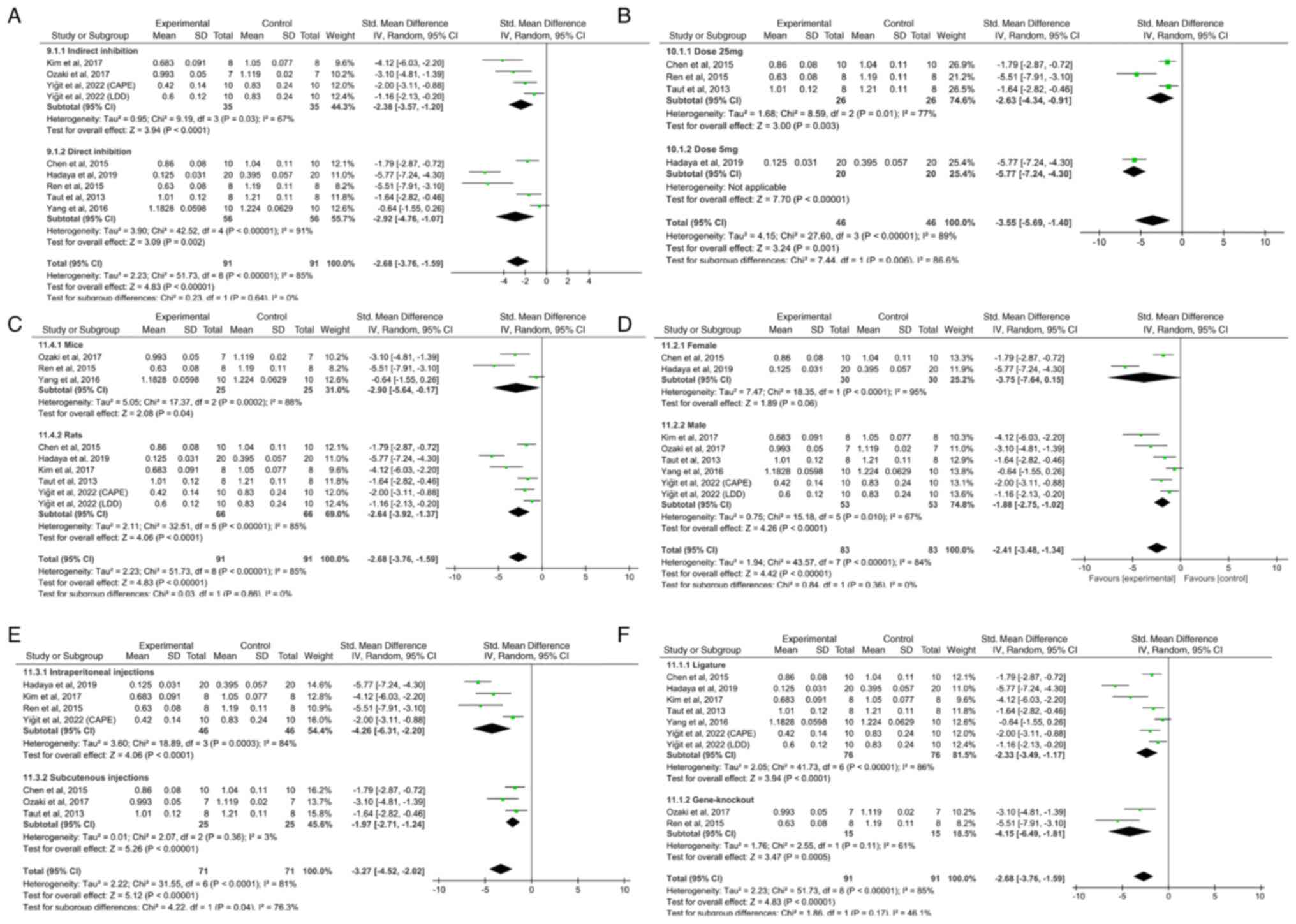
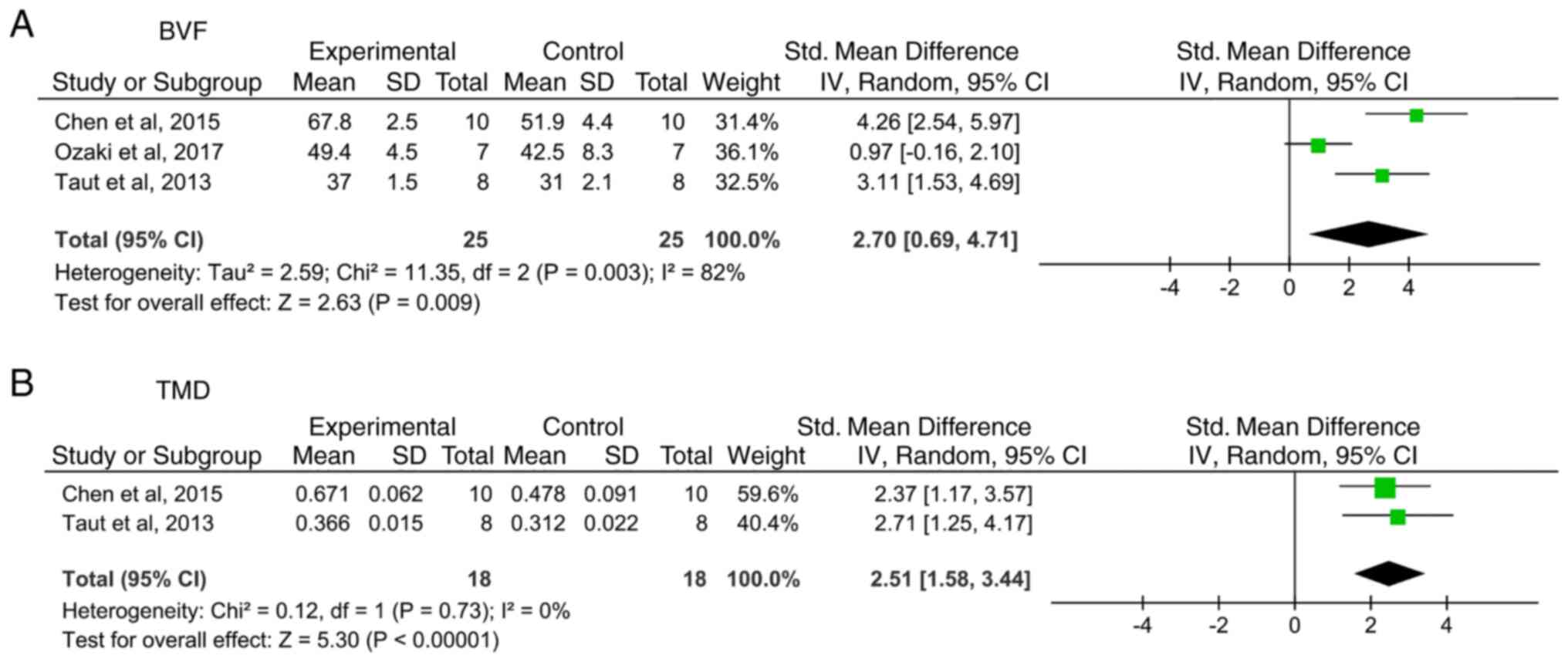
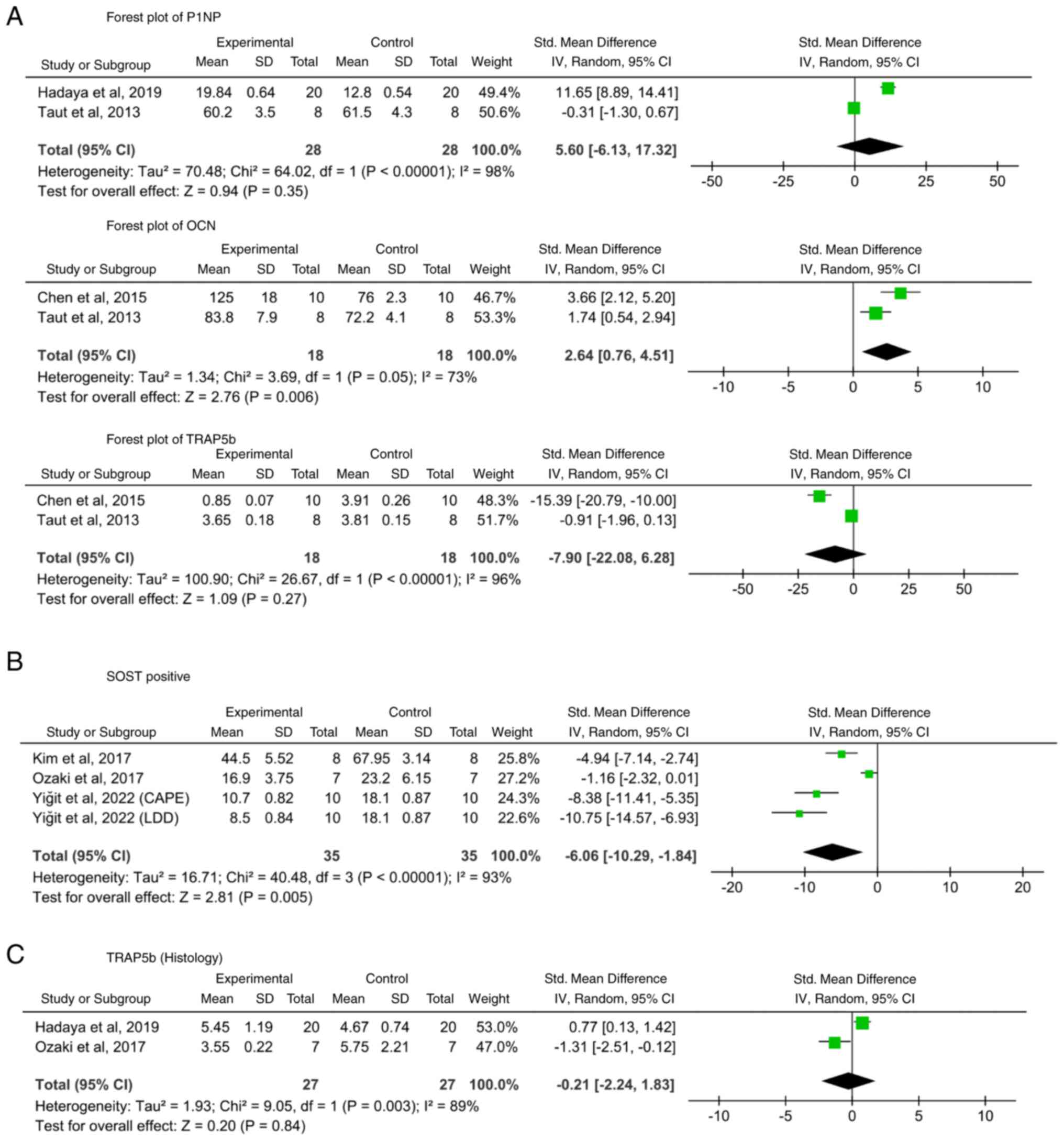
Chen H, Xu X, Liu M, Zhang W, Ke HZ, Qin
A, Tang T and Lu E: Sclerostin antibody treatment causes greater
alveolar crest height and bone mass in an ovariectomized rat model
of localized periodontitis. Bone. 76:141–148. 2015.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Hadaya D, Gkouveris I, Soundia A,
Bezouglaia O, Boyce RW, Stolina M, Dwyer D, Dry SM, Pirih FQ,
Aghaloo TL and Tetradis S: Clinically relevant doses of sclerostin
antibody do not induce osteonecrosis of the jaw (ONJ) in rats with
experimental periodontitis. J Bone Miner Res. 34:171–181.
2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kim JH, Kim AR, Choi YH, Jang S, Woo GH,
Cha JH, Bak EJ and Yoo YJ: Tumor necrosis factor-α antagonist
diminishes osteocytic RANKL and sclerostin expression in diabetes
rats with periodontitis. PLoS One. 12(e0189702)2017.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ozaki Y, Koide M, Furuya Y, Ninomiya T,
Yasuda H, Nakamura M, Kobayashi Y, Takahashi N, Yoshinari N and
Udagawa N: Treatment of OPG-deficient mice with WP9QY, a
RANKL-binding peptide, recovers alveolar bone loss by suppressing
osteoclastogenesis and enhancing osteoblastogenesis. PLoS One.
12(e0184904)2017.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Ren Y, Han X, Ho SP, Harris SE, Cao Z,
Economides AN, Qin C, Ke H, Liu M and Feng JQ: Removal of SOST or
blocking its product sclerostin rescues defects in the
periodontitis mouse model. FASEB J. 29:2702–2711. 2015.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Taut AD, Jin Q, Chung JH, Galindo-Moreno
P, Yi ES, Sugai JV, Ke HZ, Liu M and Giannobile WV: Sclerostin
antibody stimulates bone regeneration after experimental
periodontitis. J Bone Miner Res. 28:2347–2356. 2013.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Yang X, Han X, Shu R, Jiang F, Xu L, Xue
C, Chen T and Bai D: Effect of sclerostin removal in vivo on
experimental periodontitis in mice. J Oral Sci. 58:271–276.
2016.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Yiğit U, Kırzıoğlu FY and Özmen Ö: Effects
of low dose doxycycline and caffeic acid phenethyl ester on
sclerostin and bone morphogenic protein-2 expressions in
experimental periodontitis. Biotech Histochem. 97:567–575.
2022.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Ominsky MS, Boyce RW, Li X and Ke HZ:
Effects of sclerostin antibodies in animal models of osteoporosis.
Bone. 96:63–75. 2017.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Ashifa N, Viswanathan K, Sundaram R and
Srinivasan S: Sclerostin and its role as a bone modifying agent in
periodontal disease. J Oral Biosci. 63:104–110. 2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
de Vries TJ and Huesa C: The osteocyte as
a novel key player in understanding periodontitis through its
expression of RANKL and sclerostin: A review. Curr Osteoporos Rep.
17:116–121. 2019.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Sapir-Koren R and Livshits G: Osteocyte
control of bone remodeling: Is sclerostin a key molecular
coordinator of the balanced bone resorption-formation cycles?
Osteoporos Int. 25:2685–2700. 2014.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Li X, Niu QT, Warmington KS, Asuncion FJ,
Dwyer D, Grisanti M, Han CY, Stolina M, Eschenberg MJ, Kostenuik
PJ, et al: Progressive increases in bone mass and bone strength in
an ovariectomized rat model of osteoporosis after 26 weeks of
treatment with a sclerostin antibody. Endocrinology. 155:4785–4797.
2014.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Percie du Sert N, Hurst V, Ahluwalia A,
Alam S, Avey MT, Baker M, Browne WJ, Clark A, Cuthill IC, Dirnagl
U, et al: The ARRIVE guidelines 2.0: Updated guidelines for
reporting animal research. PLoS Biol. 18(e3000410)2020.PubMed/NCBI View Article : Google Scholar
|