Introduction
Synovitis, acne, pustulosis, hyperostosis and
osteitis (SAPHO) syndrome is a rare, heterogeneous autoinflammatory
condition involving osteoarticular and dermatological
manifestations. It is estimated to affect <1 in 10,000
individuals, with an onset typically in early adulthood (1). The pathogenesis involves a complex
interplay between innate immune activation, cytokine dysregulation
(notably TNF-α, IL-1β and IL-17), and genetic susceptibility, with
occasional associations to Propionibacterium acnes as a
triggering antigen (2).
Therapeutic strategies include non-steroidal anti-inflammatory
drugs (NSAIDs), corticosteroids, conventional disease-modifying
anti-rheumatic drugs (DMARDs) (methotrexate, sulfasalazine,
cyclosporine) and biologics (TNF inhibitors, IL-1 and IL-17
blockers) (3,4). Leflunomide, a pyrimidine synthesis
inhibitor, offers an oral, cost-effective alternative with
immunomodulatory effects on T-cell proliferation, supported mainly
by case reports and small series (5,6).
Case report
A 60-year-old Caucasian female from Southern Italy,
a homemaker and non-smoker, with no significant comorbidities or
concurrent use of medications for major conditions, was diagnosed
with SAPHO syndrome in early 2015 at the Madonna delle Grazie
Hospital (Matera, Italy). The diagnosis was based on palmoplantar
pustulosis (PPP) and severe, painful swelling of the
manubriosternal joint. Thoracic pain was intense enough to require
high-dose opioid analgesics (buprenorphine transdermal patch 20
µg/h) with modest benefit.
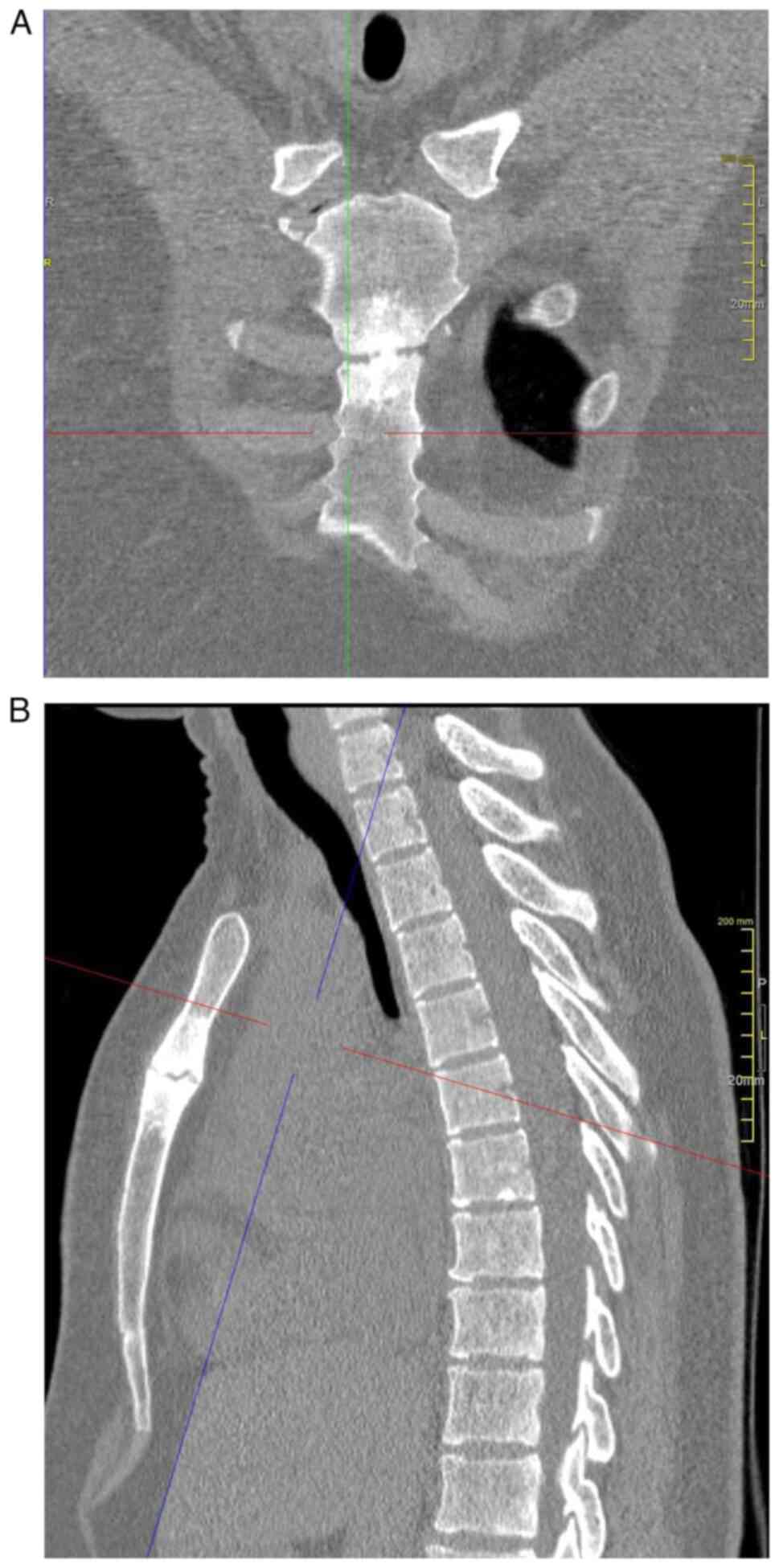
Baseline inflammatory markers were elevated
[C-reactive protein (CRP) 18 mg/l (normal, <5 mg/l), erythrocyte
sedimentation rate (ESR) 48 mm/h (normal, <20 mm/h)]. Imaging
studies (Fig. 1A and B), including plain radiography and
high-resolution computed tomography (CT), demonstrated structural
joint pathology characterized by erosive changes and marked
subchondral sclerosis at the manubriosternal articulation. Human
leukocyte antigen (HLA) genotyping, performed according to the
manufacturer's standard Luminex-based protocol (One Lambda; Thermo
Fisher Scientific, Inc.), revealed no alleles of known clinical
significance (specifically negative for HLA-B27, HLA-B51 and
HLA-Cw6). Rheumatoid factor, comprehensive thyroid function tests,
serum calcium, parathyroid hormone, alkaline phosphatase and other
relevant biochemical parameters, together with an extended panel of
immunological assays (including antinuclear antibodies and
anti-cyclic citrullinated peptide antibodies), were all within
normal limits or negative.
Initial treatment with NSAIDs, corticosteroids and
methotrexate (150 mg/day diclofenac and 10 mg/day prednisone,
together with 15 mg/week methotrexate) for 4 months yielded only
partial improvement, as indicated by a reduction in pain and a mild
decrease in inflammatory markers. After 5 months, leflunomide was
initiated at 20 mg daily, resulting in gradual but complete
resolution of both cutaneous and skeletal symptoms over 3 years.
Within four months, CRP and ESR normalized and remained stable.
In the past 2 years, the leflunomide dose was
tapered to 20 mg on alternate days, with sustained remission. The
patient was clinically reviewed every 6 months, and CT scans
performed during follow-up examinations every 2 years were reported
as unchanged compared to baseline, with no new erosions or
extension of sclerosis.
No adverse events occurred during the 10-year
treatment period, with normal liver function tests and blood counts
on regular monitoring every 2 months.
Discussion
The present case confirms leflunomide's potential
for durable remission in SAPHO syndrome, even at reduced dosing.
Its efficacy likely relates to sustained T-cell suppression via
dihydroorotate dehydrogenase inhibition. The absence of adverse
effects over prolonged therapy further supports its safety in
selected patients.
Table I provides a
comparison between the present case and previously published
reports of leflunomide for treating SAPHO syndrome. The present
case demonstrates several advantages compared to previously
reported leflunomide use in SAPHO syndrome. Scarpato and Tirri
(5) reported symptom resolution in
two patients treated with leflunomide 20 mg/day for 6-12 months,
with ~1 year of follow-up and no reported adverse events. Li et
al (6) described nail and
joint improvement in one patient receiving leflunomide 20 mg/day
for 12 months, also without adverse events. By contrast, the
present case represents the longest documented remission on
leflunomide therapy (~5 years), with the additional benefit of
successful dose reduction to alternate-day administration while
maintaining clinical remission. Furthermore, the patient of the
present study achieved complete normalization of inflammatory
markers (CRP and ESR) within four months and demonstrated stable
imaging findings throughout follow-up, indicating not only
symptomatic improvement but also control of the underlying
inflammatory process. The ability to maintain remission on reduced
dosing (20 mg alternate days) represents a significant advantage in
terms of long-term safety and cost-effectiveness, which was not
reported in previous cases.
 | Table IPublished reports on leflunomide for
Synovitis, Acne, Pustulosis, Hyperostosis, Osteitis syndrome and
present case. |
Table I
Published reports on leflunomide for
Synovitis, Acne, Pustulosis, Hyperostosis, Osteitis syndrome and
present case.
| First author,
year | Patients, n | Dose and
duration | Outcomes | Follow-up | Adverse events | (Refs.) |
|---|
| Scarpato, 2005 | 2 | Leflunomide 20
mg/day; 6-12 months | Symptom
resolution | ~1 year | None reported | (5) |
| Li, 2023 | 1 | Leflunomide 20
mg/day; 12 months | Nail and joint
improvement | 12 months | None reported | (6) |
| Present case | 1 | Leflunomide 20 mg/day
→ alternate days (maintenance) | Full remission | ~5 years | None reported | - |
Regarding comparative efficacy and safety of
treatment options, NSAIDs and short courses of systemic
corticosteroids remain the first-line therapy for pain control and
reduction of inflammation, with a generally favorable safety
profile but limited disease-modifying potential, and carry
gastrointestinal, cardiovascular and metabolic risks with prolonged
use (7). Conventional DMARDs show
a variable benefit: Methotrexate offers a benefit for peripheral
arthritis but shows limited efficacy for axial bone lesions and may
cause hepatotoxicity, cytopenia or gastrointestinal intolerance.
Sulfasalazine can improve peripheral synovitis, though its impact
on osteitis is modest; adverse effects include gastrointestinal
upset, rash and, rarely, agranulocytosis. Cyclosporine is
occasionally used for refractory cases but is hampered by
nephrotoxicity and hypertension risk. Bisphosphonates (e.g.,
pamidronate) have demonstrated consistent analgesic effects and
radiologic improvement of osteitis in observational series, with
acute-phase reactions and hypocalcaemia as the main adverse events
(7). Among biologic agents, TNF
inhibitors are highly effective in severe, refractory SAPHO,
providing substantial improvement in both osteoarticular and
cutaneous manifestations, yet are associated with variable
cutaneous responses, but infection risk and secondary loss of
response are concerns (8,9). IL-17 inhibitors
(secukinumab/brodalumab) appear effective for osteitis and severe
skin disease in emerging reports, with mucocutaneous candidiasis
and neutropenia as recognized risks (10). IL-1 blockade (anakinra) is a
reasonable option for refractory pustulosis/osteitis with a
favourable safety profile dominated by injection-site reactions
(11). Targeted synthetic agents
(e.g., JAK inhibitors) have only anecdotal support and require
caution due to infection, haematologic and cardiovascular signals
(12). Overall, the choice should
be individualized to the dominant phenotype (axial osteitis vs.
peripheral synovitis vs. PPP) and comorbidities, balancing efficacy
with toxicity and access.
The rarity of SAPHO, combined with heterogeneous
presentation and course, complicates the establishment of standard
treatment algorithms. The review of the literature performed in the
present study [conducted in PubMed (https://pubmed.ncbi.nlm.nih.gov/) and Scopus
(https://www.scopus.com/) and limited to
English-language articles published in the past 10 years)
highlights leflunomide as an underutilized but promising option,
particularly when biologics are contraindicated or unavailable.
Importantly, early initiation in the patient of the present study
may have contributed to rapid normalization of inflammatory markers
and prevention of structural progression, as evidenced by stable CT
findings during follow-up.
In conclusion, low-dose leflunomide can maintain
long-term remission in SAPHO syndrome with an excellent safety
profile. While data remain limited, this case report and literature
review supports its consideration as part of individualized
treatment strategies, particularly for patients achieving remission
on full-dose therapy and suitable for tapering. Larger studies are
needed to confirm these findings.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AN performed study conceptualization, data
collection, clinical management, literature review, manuscript
drafting and final approval. AN confirms the authenticity of all
the raw data. AN has read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report.
Competing interests
The author declares that they have no competing
interests.
References
|
1
|
Kahn MF and Khan MA: The SAPHO syndrome.
Baillieres Clin Rheumatol. 8:333–362. 1994.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Furer V, Kishimoto M, Tomita T, Elkayam O
and Helliwell PS: Current and future advances in practice: SAPHO
syndrome and chronic non-bacterial osteitis (CNO). Rheumatol Adv
Pract. 8(rkae114)2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ferraioli M, Levani J, De Luca R,
Matucci-Cerinic C, Gattorno M, Guiducci S, Bellando Randone S and
Chimenti MS: What is new and what is next for SAPHO syndrome
management: A narrative review. J Clin Med. 14(1366)2025.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Benhamou CL, Chamot AM and Kahn MF:
Synovitis-acne-pustulosis hyperostosis-osteomyelitis syndrome
(SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp
Rheumatol. 6:109–112. 1988.PubMed/NCBI
|
|
5
|
Scarpato S and Tirri E: Successful
treatment of SAPHO syndrome with leflunomide. Report of two cases.
Clin Exp Rheumatol. 23(731)2005.PubMed/NCBI
|
|
6
|
Li Z, Liu S, Liu Y, Ma M, Li L and Li C:
Successful treatment of nail involvement using leflunomide in a
patient with synovitis, acne, pustulosis, hyperostosis and osteitis
(SAPHO) syndrome. Australas J Dermatol. 64:156–157. 2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Li SWS, Roberts E and Hedrich CM:
Treatment and monitoring of SAPHO syndrome: A systematic review.
RMD Open. 9(e003688)2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cheng W, Li F, Tian J, Xie X, Chen JW,
Peng XF, Tang Q and Ge Y: New insights in the treatment of SAPHO
syndrome and medication recommendations. J Inflamm Res.
15:2365–2380. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wang Y, Gu M, Zheng Z, Jiang H, Han L,
Huang H, Wu Y and Li C: Therapeutic approaches for SAPHO syndrome
from the perspective of pathogenesis: A review of the literature.
Front Immunol. 16(1560398)2025.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chen L, Liang Q, Chen S and Cheng H: Case
report: Successful treatment of refractory synovitis, acne,
pustulosis, hyperostosis, and osteitis syndrome and palmoplantar
pustulosis with ustekinumab. Front Immunol.
16(1628279)2025.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Rossi-Semerano L, Fautrel B, Wendling D,
Hachulla E, Galeotti C, Semerano L, Touitou I and Koné-Paut I:
MAIL1 (Maladies Auto-inflammatoires et Anti-IL-1) study Group on
behalf of CRI (Club Rhumatisme et Inflammation). Tolerance and
efficacy of off-label anti-interleukin-1 treatments in France: A
nationwide survey. Orphanet J Rare Dis. 10(19)2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yang Q, Zhao Y, Li C, Luo Y, Hao W and
Zhang W: Case report: Successful treatment of refractory SAPHO
syndrome with the JAK inhibitor tofacitinib. Medicine (Baltimore).
97(e11149)2018.PubMed/NCBI View Article : Google Scholar
|