|
1
|
Anthwal N and Thompson H: The development
of the mammalian outer and middle ear. J Anat. 228:217–232.
2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pfaff C, Schultz JA and Schellhorn R: The
vertebrate middle and inner ear: A short overview. J Morphol.
280:1098–1105. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Anthwal N, Joshi L and Tucker AS:
Evolution of the mammalian middle ear and jaw: Adaptations and
novel structures. J Anat. 222:147–160. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
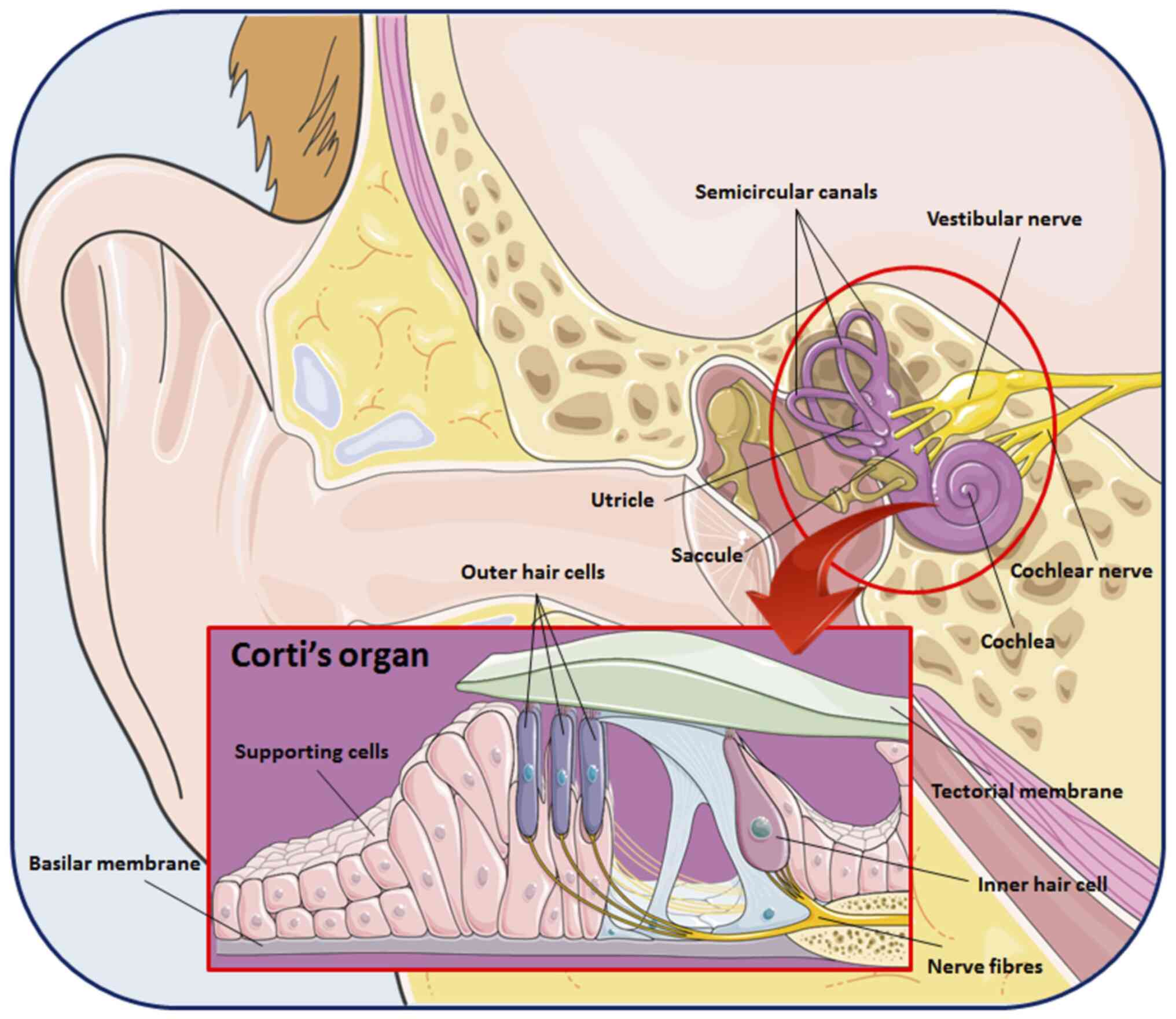
Goutman JD, Elgoyhen AB and Gómez-Casati
ME: Cochlear hair cells: The sound-sensing machines. FEBS Lett.
589:3354–3361. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Driver EC and Kelley MW: Development of
the cochlea. Development. 147(dev162263)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Fuchs JC and Tucker AS: Development and
integration of the ear. Curr Top Dev Biol. 115:213–232.
2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Szmuilowicz J and Young R: Infections of
the Ear. Emerg Med Clin North Am. 37:1–9. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sone M: Inner ear disturbances related to
middle ear inflammation. Nagoya J Med Sci. 79:1–7. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Uchida Y, Sugiura S, Nishita Y, Saji N,
Sone M and Ueda H: Age-related hearing loss and cognitive
decline-The potential mechanisms linking the two. Auris Nasus
Larynx. 46:1–9. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Themann CL and Masterson EA: Occupational
noise exposure: A review of its effects, epidemiology, and impact
with recommendations for reducing its burden. J Acoust Soc Am.
146(3879)2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ohgami N, Iida M, Yajima I, Tamura H,
Ohgami K and Kato M: Hearing impairments caused by genetic and
environmental factors. Environ Health Prev Med. 18:10–15.
2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Provenzano MJ and Domann FE: A role for
epigenetics in hearing: Establishment and maintenance of auditory
specific gene expression patterns. Hear Res. 233:1–13.
2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Giambò F, Leone GM, Gattuso G, Rizzo R,
Cosentino A, Cinà D, Teodoro M, Costa C, Tsatsakis A, Fenga C and
Falzone L: Genetic and epigenetic alterations induced by pesticide
exposure: Integrated analysis of gene expression, microRNA
expression, and DNA methylation datasets. Int J Environ Res Public
Health. 18(8697)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Filetti V, Loreto C, Falzone L, Lombardo
C, Cannizzaro E, Castorina S, Ledda C and Rapisarda V: Diagnostic
and prognostic value of three microRNAs in environmental
asbestiform fibers-associated malignant mesothelioma. J Pers Med.
11(1205)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Filetti V, Falzone L, Rapisarda V,
Caltabiano R, Eleonora Graziano AC, Ledda C and Loreto C:
Modulation of microRNA expression levels after naturally occurring
asbestiform fibers exposure as a diagnostic biomarker of
mesothelial neoplastic transformation. Ecotoxicol Environ Saf.
198(110640)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
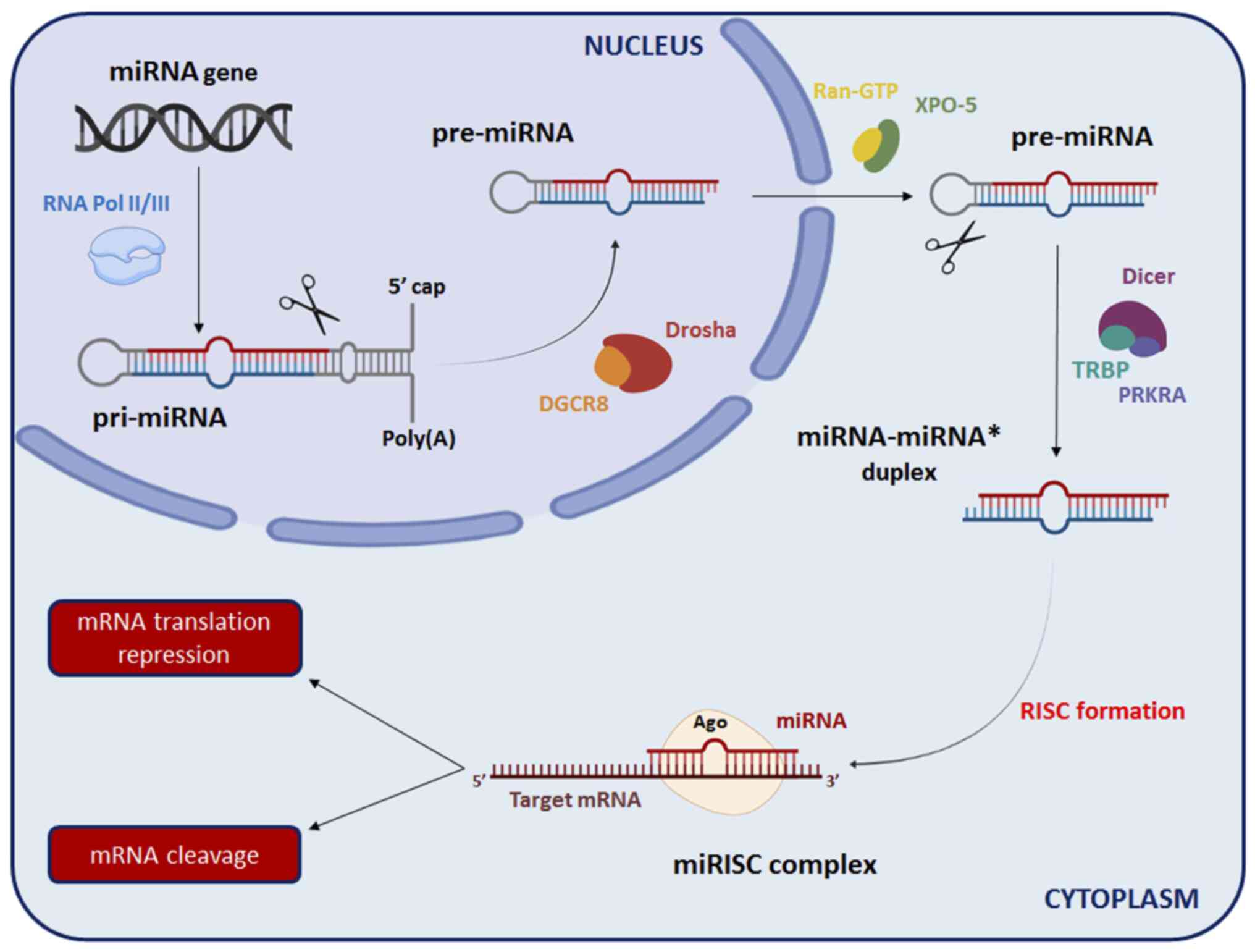
Macfarlane LA and Murphy PR: MicroRNA:
Biogenesis, function and role in cancer. Curr Genomics. 11:537–561.
2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hammond SM: An overview of microRNAs. Adv
Drug Deliv Rev. 87:3–14. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Faller M and Guo F: MicroRNA biogenesis:
There's more than one way to skin a cat. Biochim Biophys Acta.
1779:663–667. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lee Y, Kim M, Han J, Yeom KH, Lee S, Baek
SH and Kim VN: MicroRNA genes are transcribed by RNA polymerase II.
EMBO J. 23:4051–4060. 2004.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kwon SC, Nguyen TA, Choi YG, Jo MH, Hohng
S, Kim VN and Woo JS: Structure of Human DROSHA. Cell. 164:81–90.
2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yi R, Qin Y, Macara IG and Cullen BR:
Exportin-5 mediates the nuclear export of pre-microRNAs and short
hairpin RNAs. Genes Dev. 17:3011–3016. 2003.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wu K, He J, Pu W and Peng Y: The role of
exportin-5 in MicroRNA biogenesis and cancer. Genomics Proteomics
Bioinformatics. 16:120–126. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Koscianska E, Starega-Roslan J and
Krzyzosiak WJ: The role of Dicer protein partners in the processing
of microRNA precursors. PLoS One. 6(e28548)2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kobayashi H and Tomari Y: RISC assembly:
Coordination between small RNAs and Argonaute proteins. Biochim
Biophys Acta. 1859:71–81. 2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sarshad AA, Juan AH, Muler AIC,
Anastasakis DG, Wang X, Genzor P, Feng X, Tsai PF, Sun HW, Haase
AD, et al: Argonaute-miRNA complexes silence target mRNAs in the
nucleus of mammalian stem cells. Mol Cell. 71:1040–1050.e8.
2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Behm-Ansmant I, Rehwinkel J and Izaurralde
E: MicroRNAs silence gene expression by repressing protein
expression and/or by promoting mRNA decay. Cold Spring Harb Symp
Quant Biol. 71:523–530. 2006.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Fabian MR and Sonenberg N: The mechanics
of miRNA-mediated gene silencing: A look under the hood of miRISC.
Nat Struct Mol Biol. 19:586–593. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Crimi S, Falzone L, Gattuso G, Grillo CM,
Candido S, Bianchi A and Libra M: Droplet Digital PCR analysis of
liquid biopsy samples unveils the diagnostic role of
hsa-miR-133a-3p and hsa-miR-375-3p in oral cancer. Biology (Basel).
9(379)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Falzone L, Grimaldi M, Celentano E,
Augustin LSA and Libra M: Identification of modulated MicroRNAs
associated with breast cancer, diet, and physical activity. Cancers
(Basel). 12(2555)2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Candido S, Lupo G, Pennisi M, Basile MS,
Anfuso CD, Petralia MC, Gattuso G, Vivarelli S, Spandidos DA, Libra
M and Falzone L: The analysis of miRNA expression profiling
datasets reveals inverse microRNA patterns in glioblastoma and
Alzheimer's disease. Oncol Rep. 42:911–922. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Yeh CH, Moles R and Nicot C: Clinical
significance of microRNAs in chronic and acute human leukemia. Mol
Cancer. 15(37)2016.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Mahmoodian Sani MR,
Hashemzadeh-Chaleshtori M, Saidijam M, Jami MS and Ghasemi-Dehkordi
P: MicroRNA-183 family in inner ear: Hair cell development and
deafness. J Audiol Otol. 20:131–138. 2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Sekine K, Matsumura T, Takizawa T, Kimura
Y, Saito S, Shiiba K, Shindo S, Okubo K and Ikezono T: Expression
profiling of MicroRNAs in the inner ear of elderly people by
real-time PCR quantification. Audiol Neurootol. 22:135–145.
2017.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Van den Ackerveken P, Mounier A, Huyghe A,
Sacheli R, Vanlerberghe PB, Volvert ML, Delacroix L, Nguyen L and
Malgrange B: The miR-183/ItgA3 axis is a key regulator of
prosensory area during early inner ear development. Cell Death
Differ. 24:2054–2065. 2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Cao H, Shi J, Du J, Chen K, Dong C, Jiang
D and Jiang H: MicroRNA-194 regulates the development and
differentiation of sensory patches and statoacoustic ganglion of
inner ear by Fgf4. Med Sci Monit. 24:1712–1723. 2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Khan S and Chang R: Anatomy of the
vestibular system: A review. NeuroRehabilitation. 32:437–443.
2013.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Ekdale EG: Form and function of the
mammalian inner ear. J Anat. 228:324–337. 2016.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Hudspeth AJ: Integrating the active
process of hair cells with cochlear function. Nat Rev Neurosci.
15:600–614. 2014.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kopecky BJ, Jahan I and Fritzsch B:
Correct timing of proliferation and differentiation is necessary
for normal inner ear development and auditory hair cell viability.
Dev Dyn. 242:132–147. 2013.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Zhong C, Fu Y, Pan W, Yu J and Wang J:
Atoh1 and other related key regulators in the development of
auditory sensory epithelium in the mammalian inner ear: Function
and interplay. Dev Biol. 446:133–141. 2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Elliott KL, Pavlínková G, Chizhikov VV,
Yamoah EN and Fritzsch B: Development in the mammalian auditory
system depends on transcription factors. Int J Mol Sci.
22(4189)2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Shin JO, Ankamreddy H, Jakka NM, Lee S,
Kim UK and Bok J: Temporal and spatial expression patterns of
Hedgehog receptors in the developing inner and middle ear. Int J
Dev Biol. 61:557–563. 2017.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Żak M, Klis SF and Grolman W: The Wnt and
Notch signalling pathways in the developing cochlea: Formation of
hair cells and induction of regenerative potential. Int J Dev
Neurosci. 47:247–258. 2015.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Jiang D, Du J, Zhang X, Zhou W, Zong L,
Dong C, Chen K, Chen Y, Chen X and Jiang H: miR-124 promotes the
neuronal differentiation of mouse inner ear neural stem cells. Int
J Mol Med. 38:1367–1376. 2016.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Du J, Zhang X, Cao H, Jiang D, Wang X,
Zhou W, Chen K, Zhou J, Jiang H and Ba L: MiR-194 is involved in
morphogenesis of spiral ganglion neurons in inner ear by
rearranging actin cytoskeleton via targeting RhoB. Int J Dev
Neurosci. 63:16–26. 2017.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Geng R, Furness DN, Muraleedharan CK,
Zhang J, Dabdoub A, Lin V and Xu S: The microRNA-183/96/182 cluster
is essential for stereociliary bundle formation and function of
cochlear sensory hair cells. Sci Rep. 8(18022)2018.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Brown CS, Emmett SD, Robler SK and Tucci
DL: Global hearing loss prevention. Otolaryngol Clin North Am.
51:575–592. 2018.PubMed/NCBI View Article : Google Scholar
|
|
48
|
World Health Organization (WHO): Deafness
and hearing loss. WHO, Geneva, 2022. https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss.
Accessed April 1, 2022.
|
|
49
|
Edmiston R and Mitchell C: Hearing loss in
adults. BMJ. 346(f2496)2013.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Horowitz G, Ungar OJ, Levit Y, Himmelfarb
M and Handzel O: The impact of conductive hearing loss on balance.
Clin Otolaryngol. 45:106–110. 2020.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Michels TC, Duffy MT and Rogers DJ:
Hearing loss in adults: Differential diagnosis and treatment. Am
Fam Physician. 100:98–108. 2019.PubMed/NCBI
|
|
52
|
Cunningham LL and Tucci DL: Hearing loss
in adults. N Engl J Med. 377:2465–2473. 2017.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Amanipour RM, Zhu X, Duvey G, Celanire S,
Walton JP and Frisina RD: Noise-Induced hearing loss in mice:
Effects of high and low levels of noise trauma in CBA mice. Annu
Int Conf IEEE Eng Med Biol Soc. 2018:1210–1213. 2018.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Lin BM, Wang M, Stankovic KM, Eavey R,
McKenna MJ, Curhan GC and Curhan SG: Cigarette smoking, smoking
cessation, and risk of hearing loss in women. Am J Med.
133:1180–1186. 2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Haugnes HS, Stenklev NC, Brydøy M, Dahl O,
Wilsgaard T, Laukli E and Fosså SD: Hearing loss before and after
cisplatin-based chemotherapy in testicular cancer survivors: A
longitudinal study. Acta Oncol. 57:1075–1083. 2018.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Yang T, Guo L, Wang L and Yu X: Diagnosis,
intervention, and prevention of genetic hearing loss. Adv Exp Med
Biol. 1130:73–92. 2019.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Bowl MR and Dawson SJ: Age-Related hearing
loss. Cold Spring Harb Perspect Med. 9(a033217)2019.PubMed/NCBI View Article : Google Scholar
|
|
58
|
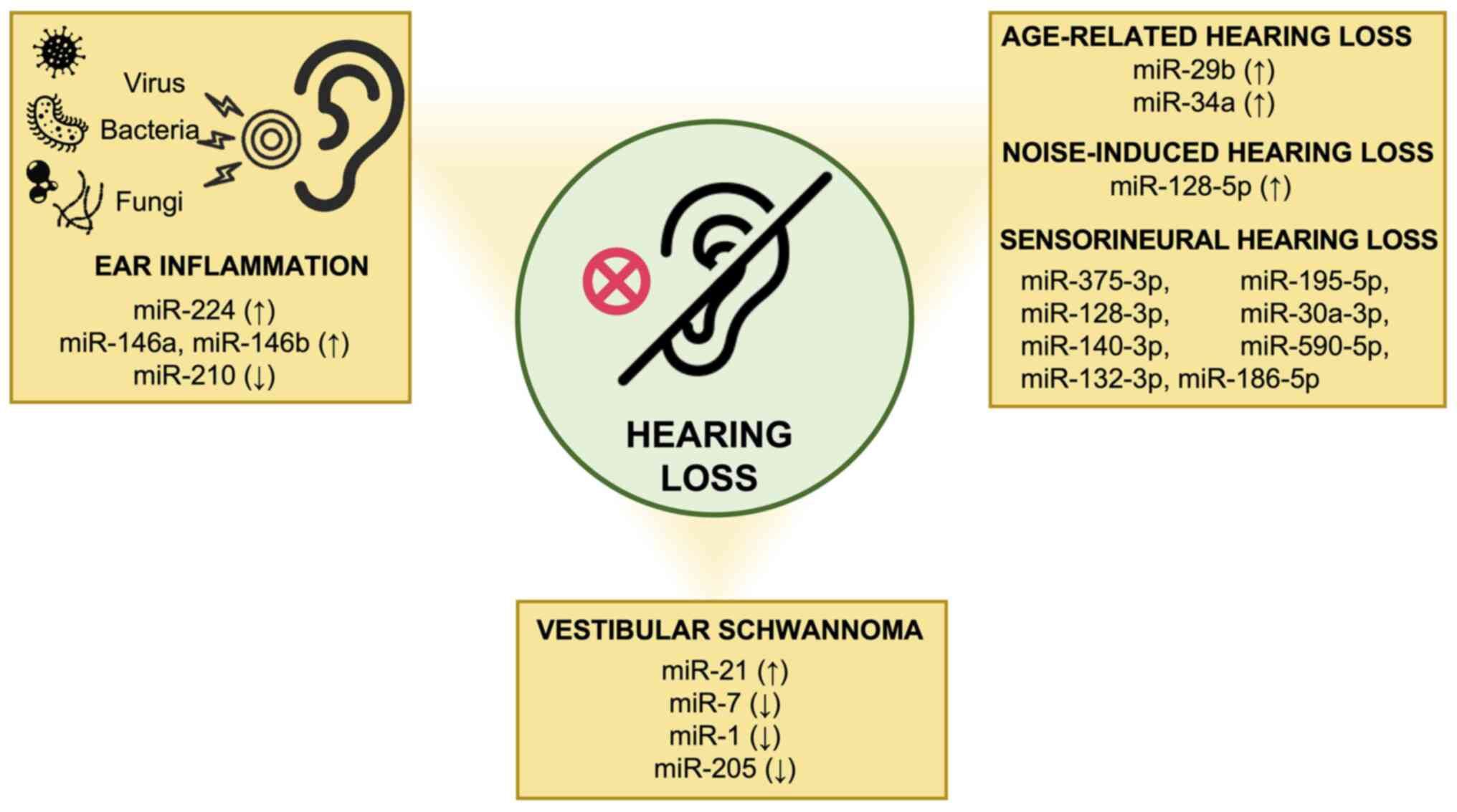
Xue T, Wei L, Zha DJ, Qiu JH, Chen FQ,
Qiao L and Qiu Y: miR-29b overexpression induces cochlear hair cell
apoptosis through the regulation of SIRT1/PGC-1α signaling:
Implications for age-related hearing loss. Int J Mol Med.
38:1387–1394. 2016.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Pang J, Xiong H, Lin P, Lai L, Yang H, Liu
Y, Huang Q, Chen S, Ye Y, Sun Y and Zheng Y: Activation of miR-34a
impairs autophagic flux and promotes cochlear cell death via
repressing ATG9A: Implications for age-related hearing loss. Cell
Death Dis. 8(e3079)2017.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Li YH, Yang Y, Yan YT, Xu LW, Ma HY, Shao
YX, Cao CJ, Wu X, Qi MJ, Wu YY, et al: Analysis of serum microRNA
expression in male workers with occupational noise-induced hearing
loss. Braz J Med Biol Res. 51(e6426)2018.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Nunez DA, Wijesinghe P, Nabi S, Yeh D and
Garnis C: microRNAs in sudden hearing loss. Laryngoscope.
130:E416–E422. 2020.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Gheorghe DC, Niculescu AG, Bîrcă AC and
Grumezescu AM: Nanoparticles for the treatment of inner ear
infections. Nanomaterials (Basel). 11(1311)2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Cohen BE, Durstenfeld A and Roehm PC:
Viral causes of hearing loss: A review for hearing health
professionals. Trends Hear. 18(2331216514541361)2014.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Palma S, Roversi MF, Bettini M, Mazzoni S,
Pietrosemoli P, Lucaccioni L, Berardi A and Genovese E: Hearing
loss in children with congenital cytomegalovirus infection: An
11-year retrospective study based on laboratory database of a
tertiary paediatric hospital. Acta Otorhinolaryngol Ital. 39:40–45.
2019.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Caroça C, Vicente V, Campelo P, Chasqueira
M, Caria H, Silva S, Paixão P and Paço J: Rubella in Sub-Saharan
Africa and sensorineural hearing loss: A case control study. BMC
Public Health. 17(146)2017.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Himmelein S, Lindemann A, Sinicina I, Horn
AKE, Brandt T, Strupp M and Hüfner K: differential involvement
during latent herpes simplex virus 1 infection of the superior and
inferior divisions of the vestibular Ganglia: Implications for
vestibular neuritis. J Virol. 91:e00331–17. 2017.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Yee KT, Neupane B, Bai F and Vetter DE:
Zika virus infection causes widespread damage to the inner ear.
Hear Res. 395(108000)2020.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Van Hoecke H, De Paepe AS, Lambert E, Van
Belleghem JD, Cools P, Van Simaey L, Deschaght P, Vaneechoutte M
and Dhooge I: Haemophilus influenzae biofilm formation in chronic
otitis media with effusion. Eur Arch Otorhinolaryngol.
273:3553–3560. 2016.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Rosenblut A, Napolitano C, Pereira A,
Moreno C, Kolhe D, Lepetic A and Ortega-Barria E: Etiology of acute
otitis media and serotype distribution of Streptococcus pneumoniae
and Haemophilus influenzae in Chilean children <5 years of age.
Medicine (Baltimore). 96(e5974)2017.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Emami A, Pirbonyeh N, Moattari A,
Bazargani A and Motamedifar M: Risk of otitis media with effusion
(OME) in children by Pseudomonas aeruginosa. Int J Pediatr
Otorhinolaryngol. 125:6–10. 2019.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Ozturk A, Cetintas İ, Bayraktar M and
İynen İ: Evaluation of microbial agents and their antibiotic
susceptibility profiles in patients with chronic suppurative otitis
media. Int J Clin Pract. 75(e14382)2021.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Sillanpää S, Oikarinen S, Sipilä M, Kramna
L, Rautiainen M, Huhtala H, Aittoniemi J, Laranne J, Hyöty H and
Cinek O: Moraxella catarrhalis might be more common than expected
in acute otitis media in young finnish children. J Clin Microbiol.
54:2373–2379. 2016.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Møller MN, Brandt C, Østergaard C and
Caye-Thomasen P: Bacterial invasion of the inner ear in association
with pneumococcal meningitis. Otol Neurotol. 35:e178–e186.
2014.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Niedzielski A, Chmielik LP and Stankiewicz
T: The formation of biofilm and bacteriology in otitis media with
effusion in children: A prospective cross-sectional study. Int J
Environ Res Public Health. 18(3555)2021.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Mofatteh MR, Shahabian Moghaddam F,
Yousefi M and Namaei MH: A study of bacterial pathogens and
antibiotic susceptibility patterns in chronic suppurative otitis
media. J Laryngol Otol. 132:41–45. 2018.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Ali K, Hamed MA, Hassan H, Esmail A and
Sheneef A: Identification of fungal pathogens in otomycosis and
their drug sensitivity: Our experience. Int Arch Otorhinolaryngol.
22:400–403. 2018.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Kiakojuri K, Mahdavi Omran S, Roodgari S,
Taghizadeh Armaki M, Hedayati MT, Shokohi T, Haghani I, Javidnia J,
Kermani F, Badali H and Abastabar M: Molecular identification and
antifungal susceptibility of yeasts and molds isolated from
patients with otomycosis. Mycopathologia. 186:245–257.
2021.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Hajioff D and MacKeith S: Otitis externa.
BMJ Clin Evid. 2015(0510)2015.PubMed/NCBI
|
|
79
|
Candido S, Tomasello BMR, Lavoro A,
Falzone L, Gattuso G and Libra M: Novel insights into epigenetic
regulation of IL6 pathway: In silico perspective on inflammation
and cancer relationship. Int J Mol Sci. 22(10172)2021.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Sonkoly E and Pivarcsi A: microRNAs in
inflammation. Int Rev Immunol. 28:535–561. 2009.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Rudnicki A, Shivatzki S, Beyer LA, Takada
Y, Raphael Y and Avraham KB: microRNA-224 regulates Pentraxin 3, a
component of the humoral arm of innate immunity, in inner ear
inflammation. Hum Mol Genet. 23:3138–3146. 2014.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Samuels TL, Yan J, Khampang P, MacKinnon
A, Hong W, Johnston N and Kerschner JE: Association of microRNA 146
with middle ear hyperplasia in pediatric otitis media. Int J
Pediatr Otorhinolaryngol. 88:104–108. 2016.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Zhang J, He J, Luo Y, Liu Y and Fan X:
miR-210 regulates the inflammation of otitis media with effusion by
inhibiting the expression of hypoxia-inducible factor (HIF)-1a.
Biochem Biophys Res Commun. 534:401–407. 2021.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Frye MD, Ryan AF and Kurabi A:
Inflammation associated with noise-induced hearing loss. J Acoust
Soc Am. 146(4020)2019.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Kociszewska D and Vlajkovic S: Age-Related
hearing loss: The link between inflammaging, immunosenescence, and
gut dysbiosis. Int J Mol Sci. 23(7348)2022.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Lassale C, Vullo P, Cadar D, Batty GD,
Steptoe A and Zaninotto P: Association of inflammatory markers with
hearing impairment: The English Longitudinal study of ageing. Brain
Behav Immun. 83:112–119. 2020.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Lanvers-Kaminsky C, Zehnhoff-Dinnesen AA,
Parfitt R and Ciarimboli G: Drug-induced ototoxicity: Mechanisms,
pharmacogenetics, and protective strategies. Clin Pharmacol Ther.
101:491–500. 2017.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Kros CJ and Steyger PS: Aminoglycoside-
and cisplatin-induced ototoxicity: Mechanisms and otoprotective
strategies. Cold Spring Harb Perspect Med.
9(a033548)2019.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Gattuso G, Falzone L, Costa C, Giambò F,
Teodoro M, Vivarelli S, Libra M and Fenga C: Chronic pesticide
exposure in farm workers is associated with the epigenetic
modulation of hsa-miR-199a-5p. Int J Environ Res Public Health.
19(7018)2022.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Gatto MP, Fioretti M, Fabrizi G, Gherardi
M, Strafella E and Santarelli L: Effects of potential neurotoxic
pesticides on hearing loss: A review. Neurotoxicology. 42:24–32.
2014.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Hoshino ACH, Pacheco-Ferreira H, Taguchi
CK, Tomita S and de Fátima Miranda M: Ototoxicity study in workers
exposed to organophosphate. Braz J Otorhinolaryngol. 74:912–918.
2008.PubMed/NCBI View Article : Google Scholar
|
|
92
|
DiSogra RM: Common aminoglycosides and
platinum-based ototoxic drugs: Cochlear/vestibular side effects and
incidence. Semin Hear. 40:104–107. 2019.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Gersten BK, Fitzgerald TS, Fernandez KA
and Cunningham LL: Ototoxicity and platinum uptake following cyclic
administration of platinum-based chemotherapeutic agents. J Assoc
Res Otolaryngol. 21:303–321. 2020.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Xie J, Talaska AE and Schacht J: New
developments in aminoglycoside therapy and ototoxicity. Hear Res.
281:28–37. 2011.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Ding D, Liu H, Qi W, Jiang H, Li Y, Wu X,
Sun H, Gross K and Salvi R: Ototoxic effects and mechanisms of loop
diuretics. J Otol. 11:145–156. 2016.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Ikeda AK, Prince AA, Chen JX, Lieu JEC and
Shin JJ: Macrolide-associated sensorineural hearing loss: A
systematic review. Laryngoscope. 128:228–236. 2018.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Altissimi G, Colizza A, Cianfrone G, de
Vincentiis M, Greco A, Taurone S, Musacchio A, Ciofalo A, Turchetta
R, Angeletti D and Ralli M: Drugs inducing hearing loss, tinnitus,
dizziness and vertigo: An updated guide. Eur Rev Med Pharmacol Sci.
24:7946–7952. 2020.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Landier W, Knight K, Wong FL, Lee J,
Thomas O, Kim H, Kreissman SG, Schmidt ML, Chen L, London WB, et
al: Ototoxicity in children with high-risk neuroblastoma:
Prevalence, risk factors, and concordance of grading scales-a
report from the Children's oncology group. J Clin Oncol.
32:527–534. 2014.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Waissbluth S, Del Valle Á, Chuang A and
Becker A: Incidence and associated risk factors for
platinum-induced ototoxicity in pediatric patients. Int J Pediatr
Otorhinolaryngol. 111:174–179. 2018.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Wei M and Yuan X: Cisplatin-induced
ototoxicity in children with solid tumor. J Pediatr Hematol Oncol.
41:e97–e100. 2019.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Landier W: Ototoxicity and cancer therapy.
Cancer. 122:1647–1658. 2016.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Ganesan P, Schmiedge J, Manchaiah V,
Swapna S, Dhandayutham S and Kothandaraman PP: Ototoxicity: A
challenge in diagnosis and treatment. J Audiol Otol. 22:59–68.
2018.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Kim CW, Han JH, Wu L and Choi JY:
microRNA-183 is essential for hair cell regeneration after neomycin
injury in zebrafish. Yonsei Med J. 59:141–147. 2018.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Lee SH, Ju HM, Choi JS, Ahn Y, Lee S and
Seo YJ: Circulating Serum miRNA-205 as a diagnostic biomarker for
ototoxicity in mice treated with aminoglycoside antibiotics. Int J
Mol Sci. 19(2836)2018.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Li J, Ling Y, Huang W, Sun L, Li Y, Wang
C, Zhang Y, Wang X, Dahlgren RA and Wang H: Regulatory mechanisms
of miR-96 and miR-184 abnormal expressions on otic vesicle
development of zebrafish following exposure to β-diketone
antibiotics. Chemosphere. 214:228–238. 2019.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Chen J, Liu Z, Yan H, Xing W, Mi W, Wang
R, Li W, Chen F, Qiu J and Zha D: miR-182 prevented ototoxic
deafness induced by co-administration of kanamycin and furosemide
in rats. Neurosci Lett. 723(134861)2020.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Stangerup SE, Caye-Thomasen P, Tos M and
Thomsen J: The natural history of vestibular schwannoma. Otol
Neurotol. 27:547–552. 2006.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Paldor I, Chen AS and Kaye AH: Growth rate
of vestibular schwannoma. J Clin Neurosci. 32:1–8. 2016.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Sughrue ME, Yang I, Aranda D, Rutkowski
MJ, Fang S, Cheung SW and Parsa AT: Beyond audiofacial morbidity
after vestibular schwannoma surgery. J Neurosurg. 114:367–374.
2011.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Halliday J, Rutherford SA, McCabe MG and
Evans DG: An update on the diagnosis and treatment of vestibular
schwannoma. Expert Rev Neurother. 18:29–39. 2018.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Yao L, Alahmari M, Temel Y and Hovinga K:
Therapy of sporadic and NF2-Related vestibular schwannoma. Cancers
(Basel). 12(835)2020.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Pandrangi VC, Han AY, Alonso JE, Peng KA
and St John MA: An update on epidemiology and management trends of
vestibular schwannomas. Otol Neurotol. 41:411–417. 2020.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Andersen JF, Nilsen KS, Vassbotn FS,
Møller P, Myrseth E, Lund-Johansen M and Goplen FK: Predictors of
vertigo in patients with untreated vestibular schwannoma. Otol
Neurotol. 36:647–652. 2015.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Kaul V and Cosetti MK: Management of
vestibular schwannoma (Including NF2): Facial nerve considerations.
Otolaryngol Clin North Am. 51:1193–1212. 2018.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Dunn IF, Bi WL, Mukundan S, Delman BN,
Parish J, Atkins T, Asher AL and Olson JJ: Congress of neurological
surgeons systematic review and evidence-based guidelines on the
role of imaging in the diagnosis and management of patients with
vestibular schwannomas. Neurosurgery. 82:E32–E34. 2018.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Goldbrunner R, Weller M, Regis J,
Lund-Johansen M, Stavrinou P, Reuss D, Evans DG, Lefranc F,
Sallabanda K, Falini A, et al: EANO guideline on the diagnosis and
treatment of vestibular schwannoma. Neuro Oncol. 22:31–45.
2020.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Cioffi JA, Yue WY, Mendolia-Loffredo S,
Hansen KR, Wackym PA and Hansen MR: MicroRNA-21 overexpression
contributes to vestibular schwannoma cell proliferation and
survival. Otol Neurotol. 31:1455–1462. 2010.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Saydam O, Senol O, Würdinger T, Mizrak A,
Ozdener GB, Stemmer-Rachamimov AO, Yi M, Stephens RM, Krichevsky
AM, Saydam N, et al: miRNA-7 attenuation in Schwannoma tumors
stimulates growth by upregulating three oncogenic signaling
pathways. Cancer Res. 71:852–861. 2011.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Mahajan K and Mahajan NP: ACK1/TNK2
tyrosine kinase: Molecular signaling and evolving role in cancers.
Oncogene. 34:4162–4167. 2015.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Li SL, Ma XH, Ji JF, Li H, Liu W, Lu FZ,
Wu ST and Zhang Y: miR-1 association with cell proliferation
inhibition and apoptosis in vestibular schwannoma by targeting
VEGFA. Genet Mol Res. 15(gmr15048923)2016.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Peng CY, Liao YW, Lu MY, Yu CH, Yu CC and
Chou MY: Downregulation of miR-1 enhances tumorigenicity and
invasiveness in oral squamous cell carcinomas. J Formos Med Assoc.
116:782–789. 2017.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Xu W, Zhang Z, Zou K, Cheng Y, Yang M,
Chen H, Wang H, Zhao J, Chen P, He L, et al: MiR-1 suppresses tumor
cell proliferation in colorectal cancer by inhibition of
Smad3-mediated tumor glycolysis. Cell Death Dis.
8(e2761)2017.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Chen C, Zhou Y, Ding P and He L: miR-1
targeted downregulation of Bcl-2 increases chemosensitivity of lung
cancer cells. Genet Test Mol Biomarkers. 25:540–545.
2021.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Yin X, Huo Z, Yan S, Wang Z, Yang T, Wu H
and Zhang Z: MiR-205 inhibits sporadic vestibular schwannoma cell
proliferation by targeting cyclin-dependent kinase 14. World
Neurosurg. 147:e25–e31. 2021.PubMed/NCBI View Article : Google Scholar
|