|
1
|
Nakaya Y and Sheng G: Epithelial to
mesenchymal transition during gastrulation: An embryological view.
Dev Growth Differ. 50:755–766. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Qin Q, Xu Y, He T, Qin C and Xu J: Normal
and disease-related biological functions of Twist1 and underlying
molecular mechanisms. Cell Res. 22:90–106. 2012. View Article : Google Scholar :
|
|
3
|
Piera-Velazquez S, Li Z and Jimenez SA:
Role of endothelial- mesenchymal transition (EndoMT) in the
pathogenesis of fibrotic disorders. Am J Pathol. 179:1074–1080.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fidler IJ: The pathogenesis of cancer
metastasis: The ‘seed and soil’ hypothesis revisited. Nat Rev
Cancer. 3:453–458. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Książkiewicz M, Markiewicz A and Zaczek
AJ: Epithelial-mesenchymal transition: A hallmark in metastasis
formation linking circulating tumor cells and cancer stem cells.
Pathobiology. 79:195–208. 2012. View Article : Google Scholar
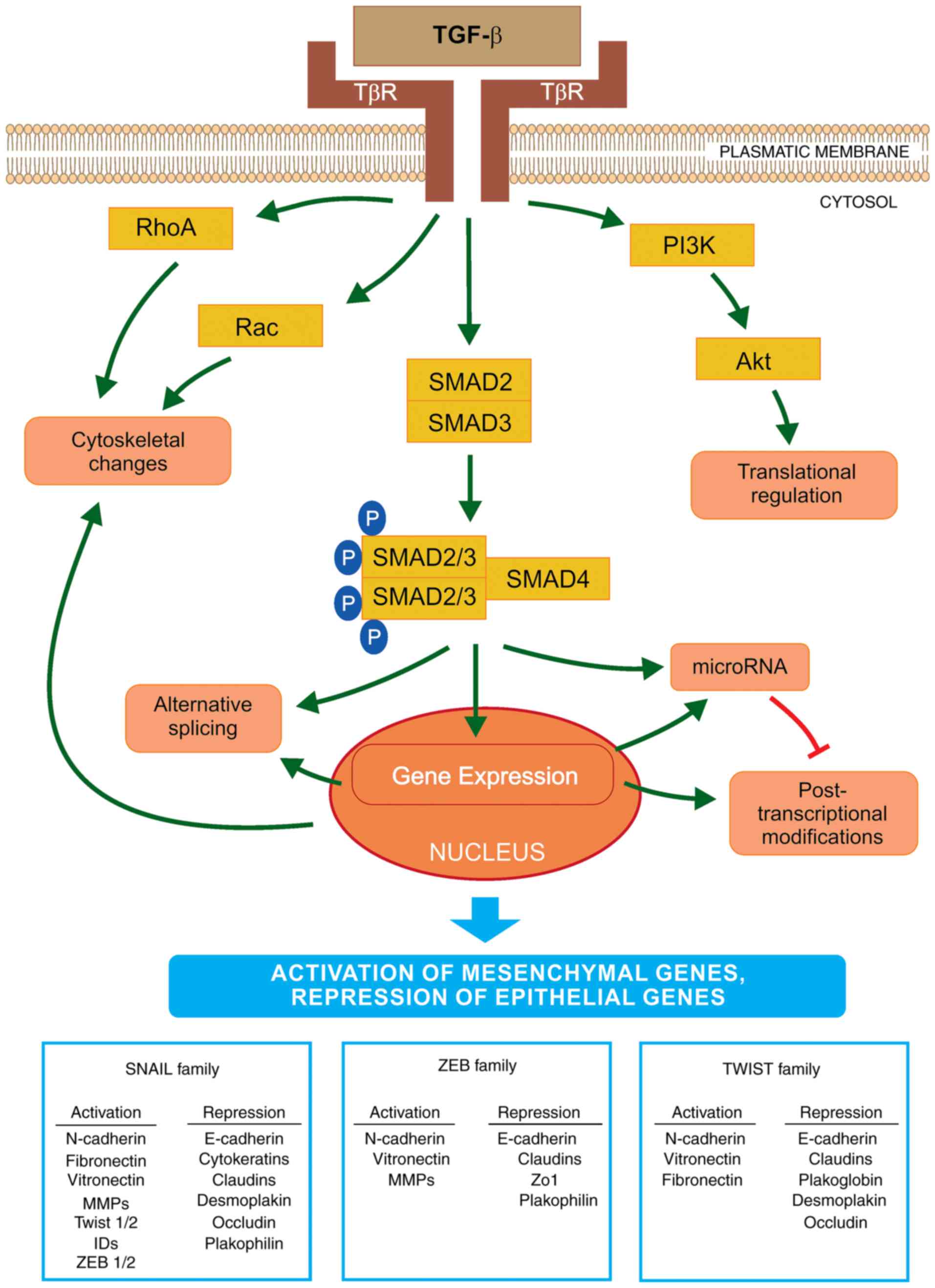
|
|
6
|
Nieto M: Epithelial plasticity: A common
theme in embryonic and cancer cells. Science. 342:12348502013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sarkar S, Horn G, Moulton K, Oza A, Byler
S, Kokolus S and Longacre M: Cancer development, progression, and
therapy: An epigenetic overview. Int J Mol Sci. 14:21087–21113.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
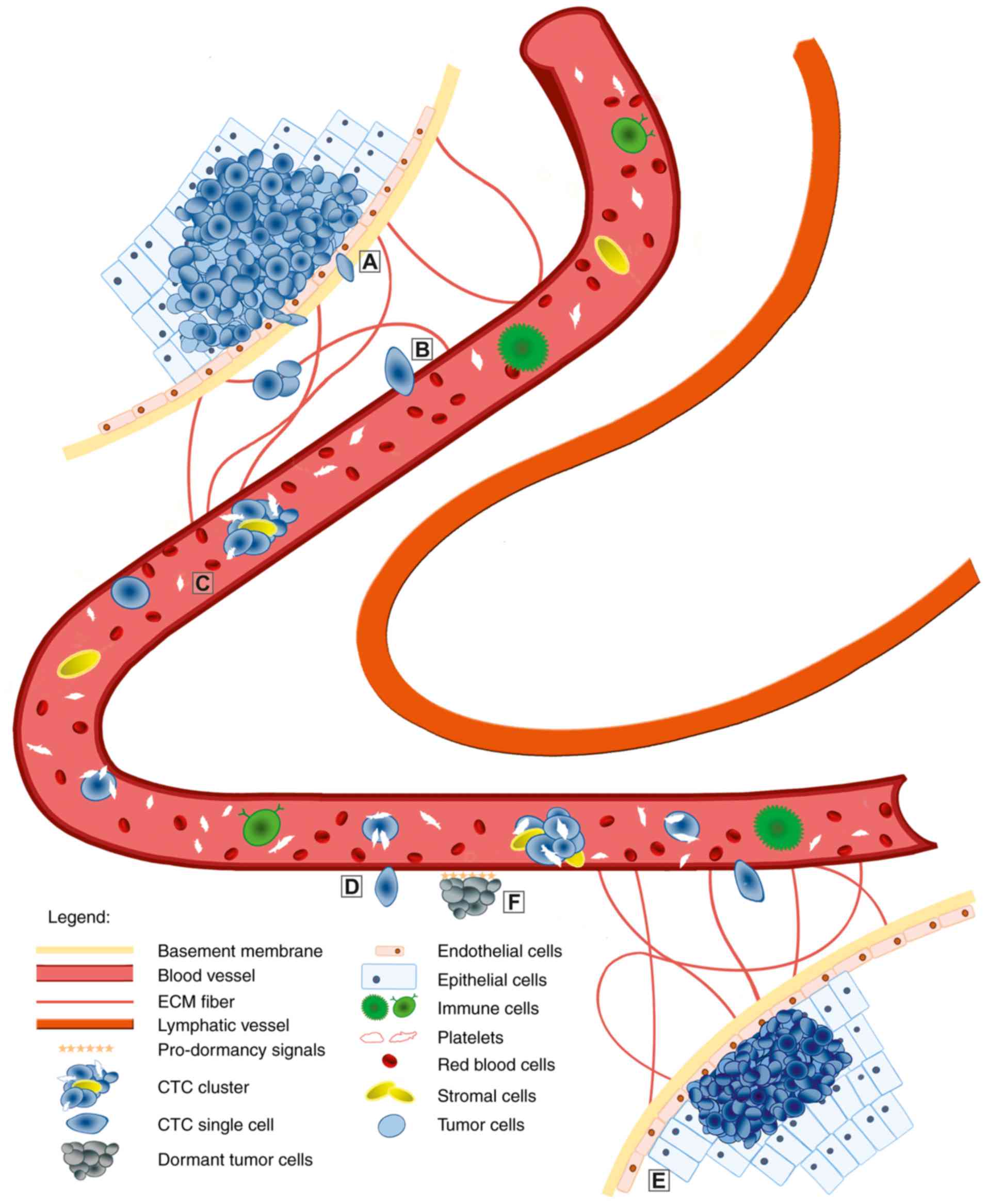
Aceto N, Bardia A, Miyamoto DT, Donaldson
MC, Wittner BS, Spencer JA, Yu M, Pely A, Engstrom A, Zhu H, et al:
Circulating tumor cell clusters are oligoclonal precursors of
breast cancer metastasis. Cell. 158:1110–1122. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hong Y, Fang F and Zhang Q: Circulating
tumor cell clusters: What we know and what we expect (Review). Int
J Oncol. 49:2206–2216. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Heerboth S, Housman G, Leary M, Longacre
M, Byler S, Lapinska K, Willbanks A and Sarkar S: EMT and tumor
metastasis. Clin Transl Med. 4:62015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim YN, Koo KH, Sung JY, Yun UJ and Kim H:
Anoikis resistance: An essential prerequisite for tumor metastasis.
Int J Cell Biol. 2012:3068792012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Iwatsuki M, Mimori K, Yokobori T, Ishi H,
Beppu T, Nakamori S, Baba H and Mori M: Epithelial-mesenchymal
transition in cancer development and its clinical significance.
Cancer Sci. 101:293–299. 2010. View Article : Google Scholar
|
|
13
|
Chaffer CL, Thompson EW and Williams ED:
Mesenchymal to epithelial transition in development and disease.
Cells Tissues Organs. 185:7–19. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yang J and Weinberg RA:
Epithelial-mesenchymal transition: At the crossroads of development
and tumor metastasis. Dev Cell. 14:818–829. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yap AS, Brieher WM and Gumbiner BM:
Molecular and functional analysis of cadherin-based adherens
junctions. Annu Rev Cell Dev Biol. 13:119–146. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nelson WJ: Remodeling epithelial cell
organization: Transitions between front-rear and apical-basal
polarity. Cold Spring Harb Perspect Biol. 1:a0005132009. View Article : Google Scholar
|
|
17
|
Greenburg G and Hay ED: Cytoskeleton and
thyroglobulin expression change during transformation of thyroid
epithelium to mesenchyme-like cells. Development. 102:605–622.
1988.PubMed/NCBI
|
|
18
|
Thiery JP, Acloque H, Huang RY and Nieto
MA: Epithelial-mesenchymal transitions in development and disease.
Cell. 139:871–890. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kiesslich T, Pichler M and Neureiter D:
Epigenetic control of epithelial-mesenchymal-transition in human
cancer. Mol Clin Oncol. 1:3–11. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Radisky DC, Kenny PA and Bissell MJ:
Fibrosis and cancer: Do myofibroblasts come also from epithelial
cells via EMT? J Cell Biochem. 10:830–839. 2007. View Article : Google Scholar
|
|
21
|
Zeisberg EM, Tarnavski O, Zeisberg M,
Dorfman AL, McMullen JR, Gustafsson E, Chandraker A, Yuan X, Pu WT,
Roberts AB, et al: Endothelial-to-mesenchymal transition
contributes to cardiac fibrosis. Nat Med. 13:952–961. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zeisberg EM, Potenta SE, Sugimoto H,
Zeisberg M and Kalluri R: Fibroblasts in kidney fibrosis emerge via
endothelial-to- mesenchymal transition. J Am Soc Nephrol.
19:2282–2287. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Strippoli R, Benedicto I, Pérez Lozano ML,
Cerezo A, López-Cabrera M and del Pozo MA:
Epithelial-to-mesenchymal transition of peritoneal mesothelial
cells is regulated by an ERK/NF-kappaB/Snail1 pathway. Dis Model
Mech. 1:264–274. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Boutet A, De Frutos CA, Maxwell PH, Mayol
MJ, Romero J and Nieto MA: Snail activation disrupts tissue
homeostasis and induces fibrosis in the adult kidney. EMBO J.
25:5603–5613. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yeung KT and Yang J:
Epithelial-mesenchymal transition in tumor metastasis. Mol Oncol.
11:28–39. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Derksen PW, Liu X, Saridin F, van der
Gulden H, Zevenhoven J, Evers B, van Beijnum JR, Griffioen AW, Vink
J, Krimpenfort P, et al: Somatic inactivation of E-cadherin and p53
in mice leads to metastatic lobular mammary carcinoma through
induction of anoikis resistance and angiogenesis. Cancer Cell.
10:437–449. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Tsai JH and Yang J: Epithelial-mesenchymal
plasticity in carcinoma metastasis. Genes Dev. 27:2192–2206. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jouppila-Mättö A, Tuhkanen H, Soini Y,
Pukkila M, Närkiö-Mäkelä M, Sironen R, Virtanen I, Mannermaa A and
Kosma VM: Transcription factor snail1 expression and poor survival
in pharyngeal squamous cell carcinoma. Histol Histopathol.
26:443–439. 2011.PubMed/NCBI
|
|
30
|
Francí C, Gallén M, Alameda F, Baró T,
Iglesias M, Virtanen I and García de Herreros A: Snail1 protein in
the stroma as a new putative prognosis marker for colon tumours.
PLoS One. 4:e55952009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bièche I, Lerebours F, Tozlu S, Espie M,
Marty M and Lidereau R: Molecular profiling of inflammatory breast
cancer: Identification of a poor-prognosis gene expression
signature. Clin Cancer Res. 10:6789–6795. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sarkar FH, Li Y, Wang Z and Kong D:
Pancreatic cancer stem cells and EMT in drug resistance and
metastasis. Minerva Chir. 64:489–500. 2009.PubMed/NCBI
|
|
33
|
van Zijl F, Zulehner G, Petz M, Schneller
D, Kornauth C, Hau M, Machat G, Grubinger M, Huber H and Mikulits
W: Epithelial-mesenchymal transition in hepatocellular carcinoma.
Future Oncol. 5:1169–1179. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Halasova E, Adamkov M, Matakova T, Kavcova
E, Poliacek I and Singliar A: Lung cancer incidence and survival in
chromium exposed individuals with respect to expression of
anti-apoptotic protein survivin and tumor suppressor P53 protein.
Eur J Med Res. 15(Suppl 2): S55–S59. 2010.
|
|
35
|
Heuberger J and Birchmeier W: Interplay of
cadherin-mediated cell adhesion and canonical Wnt signaling. Cold
Spring Harb Perspect Biol. 2:a0029152010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Katsuno Y, Lamouille S and Derynck R:
TGF-β signaling and epithelial-mesenchymal transition in cancer
progression. Curr Opin Oncol. 25:76–84. 2013. View Article : Google Scholar
|
|
37
|
Akhurst RJ and Padgett RW: Matters of
context guide future research in TGFβ superfamily signaling. Sci
Signal. 8:re102015. View Article : Google Scholar
|
|
38
|
Zavadil J and Böttinger EP: TGF-beta and
epithelial-to- mesenchymal transitions. Oncogene. 24:5764–5774.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Nawshad A, Lagamba D, Polad A and Hay ED:
Transforming growth factor-beta signaling during
epithelial-mesenchymal transformation: Implications for
embryogenesis and tumor metastasis. Cells Tissues Organs.
179:11–23. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ricciardi M, Zanotto M, Malpeli G, Bassi
G, Perbellini O, Chilosi M, Bifari F and Krampera M:
Epithelial-to-mesenchymal transition (EMT) induced by inflammatory
priming elicits mesenchymal stromal cell-like immune-modulatory
properties in cancer cells. Br J Cancer. 112:1067–1075. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wei SC, Fattet L, Tsai JH, Guo Y, Pai VH,
Majeski HE, Chen AC, Sah RL, Taylor SS, Engler AJ and Yang J:
Matrix stiffness drives epithelial-mesenchymal transition and
tumour metastasis through a TWIST1-G3BP2 mechanotransduction
pathway. Nat Cell Biol. 17:678–688. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Roberts AB and Wakefield LM: The two faces
of transforming growth factor beta in carcinogenesis. Proc Natl
Acad Sci USA. 100:8621–8623. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Cano A, Pérez-Moreno MA, Rodrigo I,
Locascio A, Blanco MJ, del Barrio MG, Portillo F and Nieto MA: The
transcription factor snail controls epithelial-mesenchymal
transitions by repressing E-cadherin expression. Nat Cell Biol.
2:76–83. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Peinado H, Olmeda D and Cano A: Snail, Zeb
and bHLH factors in tumour progression: An alliance against the
epithelial phenotype? Nat Rev Cancer. 7:415–428. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Grille SJ, Bellacosa A, Upson J,
Klein-Szanto AJ, van Roy F, Lee-Kwon W, Donowitz M, Tsichlis PN and
Larue L: The protein kinase Akt induces epithelial mesenchymal
transition and promotes enhanced motility and invasiveness of
squamous cell carcinoma lines. Cancer Res. 63:2172–2178.
2003.PubMed/NCBI
|
|
46
|
Zhang L, Huang G, Li X, Zhang Y, Jiang Y,
Shen J, Liu J, Wang Q, Zhu J, Feng X, et al: Hypoxia induces
epithelial-mesenchymal transition via activation of SNAI1 by
hypoxia-inducible factor-1α in hepatocellular carcinoma. BMC
Cancer. 13:1082013. View Article : Google Scholar
|
|
47
|
Park SM, Gaur AB, Lengyel E and Peter ME:
The miR-200 family determines the epithelial phenotype of cancer
cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes
Dev. 22:894–907. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Long J, Zuo D and Park M: Pc2-mediated
sumoylation of Smad-interacting protein 1 attenuates
transcriptional repression of E-cadherin. J Biol Chem.
280:35477–35489. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Xu J, Lamouille S and Derynck R:
TGF-beta-induced epithelial to mesenchymal transition. Cell Res.
19:156–172. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Bax NA, Pijnappels DA, van Oorschot AA,
Winter EM, de Vries AA, van Tuyn J, Braun J, Maas S, Schalij MJ,
Atsma DE, et al: Epithelial-to-mesenchymal transformation alters
electrical conductivity of human epicardial cells. J Cell Mol Med.
15:2675–2683. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lamouille S, Xu J and Derynck R: Molecular
mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell
Biol. 15:178–196. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yang MH, Hsu DS, Wang HW, Wang HJ, Lan HY,
Yang WH, Huang CH, Kao SY, Tzeng CH, Tai SK, et al: Bmi1 is
essential in Twist1-induced epithelial-mesenchymal transition. Nat
Cell Biol. 12:982–992. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Li CW, Xia W, Huo L, Lim SO, Wu Y, Hsu JL,
Chao CH, Yamaguchi H, Yang NK, Ding Q, et al:
Epithelial-mesenchymal transition induced by TNF-α requires
NF-κB-mediated transcriptional upregulation of Twist1. Cancer Res.
72:1290–1300. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Cheng GZ, Zhang WZ, Sun M, Wang Q, Coppola
D, Mansour M, Xu LM, Costanzo C, Cheng JQ and Wang LH: Twist is
transcriptionally induced by activation of STAT3 and mediates STAT3
oncogenic function. J Biol Chem. 283:14665–14673. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yang MH, Wu MZ, Chiou SH, Chen PM, Chang
SY, Liu CJ, Teng SC and Wu KJ: Direct regulation of TWIST by
HIF-1alpha promotes metastasis. Nat Cell Biol. 10:295–305. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Diepenbruck M and Christofori G:
Epithelial-mesenchymal transition (EMT) and metastasis: Yes, no,
maybe? Curr Opin Cell Biol. 43:7–13. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Porta-de-la-Riva M, Stanisavljevic J,
Curto J, Francí C, Díaz VM, García de Herreros A and Baulida J:
TFCP2c/LSF/LBP-1c is required for Snail1-induced fibronectin gene
expression. Biochem J. 435:563–568. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Kuo YC, Su CH, Liu CY, Chen TH, Chen CP
and Wang HS: Transforming growth factor-beta induces CD44 cleavage
that promotes migration of MDA-MB-435s cells through the
up-regulation of membrane type 1-matrix metalloproteinase. Int J
Cancer. 124:2568–2576. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Beaty BT and Condeelis J: Digging a little
deeper: The stages of invadopodium formation and maturation. Eur J
Cell Biol. 93:438–444. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
David JM and Rajasekaran AK: Dishonorable
discharge: The oncogenic roles of cleaved E-cadherin fragments.
Cancer Res. 72:2917–2923. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Kalluri R: EMT: When epithelial cells
decide to become mesenchymal-like cells. J Clin Invest.
119:1417–1419. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Osta WA, Chen Y, Mikhitarian K, Mitas M,
Salem M, Hannun YA, Cole DJ and Gillanders WE: EpCAM is
overexpressed in breast cancer and is a potential target for breast
cancer gene therapy. Cancer Res. 64:5818–5824. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Wu S, Liu S, Liu Z, Huang J, Pu X, Li J,
Yang D, Deng H, Yang N and Xu J: Classification of circulating
tumor cells by epithelial-mesenchymal transition markers. PLoS One.
10:e01239762015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Tam WL and Weinberg RA: The epigenetics of
epithelial- mesenchymal plasticity in cancer. Nat Med.
19:1438–1449. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Yoshikawa M, Hishikawa K, Marumo T and
Fujita T: Inhibition of histone deacetylase activity suppresses
epithelial-to- mesenchymal transition induced by TGF-beta1 in human
renal epithelial cells. J Am Soc Nephrol. 18:58–65. 2007.
View Article : Google Scholar
|
|
66
|
Bullock MD, Sayan AE, Packham GK and
Mirnezami AH: MicroRNAs: Critical regulators of epithelial to
mesenchymal (EMT) and mesenchymal to epithelial transition (MET) in
cancer progression. Biol Cell. 104:3–12. 2012. View Article : Google Scholar
|
|
67
|
Luo M, Li Z, Wang W, Zeng Y, Liu Z and Qiu
J: Long non-coding RNA H19 increases bladder cancer metastasis by
associating with EZH2 and inhibiting E-cadherin expression. Cancer
Lett. 333:213–221. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Neureiter D, Zopf S, Leu T, Dietze O,
Hauser-Kronberger C, Hahn EG, Herold C and Ocker M: Apoptosis,
proliferation and differentiation patterns are influenced by
Zebularine and SAHA in pancreatic cancer models. Scand J
Gastroenterol. 42:103–116. 2007. View Article : Google Scholar
|
|
69
|
Richterová R, Jurečeková J, Evinová A,
Kolarovszki B, Benčo M, De Riggo J, Sutovský J, Mahmood S, Račay P
and Dobrota D: Most frequent molecular and immunohistochemical
markers present in selected types of brain tumors. Gen Physiol
Biophys. 33:259–279. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Caplakova V, Babusikova E, Blahovcova E,
Balharek T, Zelieskova M and Hatok J: DNA methylation machinery in
the endometrium and endometrial cancer. Anticancer Res.
36:4407–4420. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Bolden JE, Peart MJ and Johnstone RW:
Anticancer activities of histone deacetylase inhibitors. Nat Rev
Drug Discov. 5:769–784. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Lapinska K, Housman G, Byler S, Heerboth
S, Willbanks A, Oza A and Sarkar S: The effects of histone
deacetylase inhibitor and calpain inhibitor combination therapies
on ovarian cancer cells. Anticancer Res. 36:5731–5742. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Blahovcová E, Škovierová H, Strnádel J,
Mištuna D and Halašová E: Apoptosis in cancer cells. Information
technologies in medicine. Advances in intelligent systems and
computing. Piętka E, Badura P, Kawa J and Wieclawek W: 472.
Springer; Cham: pp. 207–213. 2016
|
|
74
|
Shapiro IM, Cheng AW, Flytzanis NC,
Balsamo M, Condeelis JS, Oktay MH, Burge CB and Gertler FB: An
EMT-driven alternative splicing program occurs in human breast
cancer and modulates cellular phenotype. PLoS Genet.
7:e10022182011. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Weidmann MD, Surve CR, Eddy RJ, Chen X,
Gertler FB, Sharma VP and Condeelis JS: MenaINV dysregulates
cortactin phosphorylation to promote invadopodium maturation. Sci
Rep. 6:361422016. View Article : Google Scholar :
|
|
76
|
Brown RL, Reinke LM, Damerow MS, Perez D,
Chodosh LA, Yang J and Cheng C: CD44 splice isoform switching in
human and mouse epithelium is essential for epithelial-mesenchymal
transition and breast cancer progression. J Clin Invest.
121:1064–1074. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Stefani G and Slack FJ: Small non-coding
RNAs in animal development. Nat Rev Mol Cell Biol. 9:219–230. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Brabletz S and Brabletz T: The ZEB/miR-200
feedback loop-a motor of cellular plasticity in development and
cancer? EMBO Rep. 11:670–677. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Burk U, Schubert J, Wellner U, Schmalhofer
O, Vincan E, Spaderna S and Brabletz T: A reciprocal repression
between ZEB1 and members of the miR-200 family promotes EMT and
invasion in cancer cells. EMBO Rep. 9:582–589. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Bracken CP, Li X, Wright JA, Lawrence DM,
Pillman KA, Salmanidis M, Anderson MA, Dredge BK, Gregory PA,
Tsykin A, et al: Genome-wide identification of miR-200 targets
reveals a regulatory network controlling cell invasion. EMBO J.
33:2040–2056. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Chang CJ, Chao CH, Xia W, Yang JY, Xiong
Y, Li CW, Yu WH, Rehman SK, Hsu JL, Lee HH, et al: p53 regulates
epithelial-mesenchymal transition and stem cell properties through
modulating miRNAs. Nat Cell Biol. 13:317–323. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Brabletz S, Bajdak K, Meidhof S, Burk U,
Niedermann G, Firat E, Wellner U, Dimmler A, Faller G, Schubert J
and Brabletz T: The ZEB1/miR-200 feedback loop controls Notch
signalling in cancer cells. EMBO J. 30:770–782. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Adamkov M, Halasova E, Rajcani J, Bencat
M, Vybohova D, Rybarova S and Galbavy S: Relation between
expression pattern of p53 and survivin in cutaneous basal cell
carcinomas. Med Sci Monit. 17:BR74–BR80. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Ma L, Young J, Prabhala H, Pan E, Mestdagh
P, Muth D, Teruya-Feldstein J, Reinhardt F, Onder TT, Valastyan S,
et al: miR-9, a MYC/MYCN-activated microRNA, regulates E-cadherin
and cancer metastasis. Nat Cell Biol. 12:247–256. 2010.PubMed/NCBI
|
|
85
|
Ashworth TR: A case of cancer in which
cells similar to those in the tumors were seen in the blood after
death. Australasian Med J. 14:146–149. 1869.
|
|
86
|
Watanabe S: The metastasizability of tumor
cells. Cancer. 7:215–223. 1954. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Watson MA, Ylagan LR, Trinkaus KM,
Gillanders WE, Naughton MJ, Weilbaecher KN, Fleming TP and Aft RL:
Isolation and molecular profiling of bone marrow micrometastases
identifies TWIST1 as a marker of early tumor relapse in breast
cancer patients. Clin Cancer Res. 13:5001–5009. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Nierodzik ML, Plotkin A, Kajumo F and
Karpatkin S: Thrombin stimulates tumor-platelet adhesion in vitro
and metastasis in vivo. J Clin Invest. 87:229–236. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Kopp HG, Placke T and Salih HR:
Platelet-derived transforming growth factor-beta down-regulates
NKG2D thereby inhibiting natural killer cell antitumor reactivity.
Cancer Res. 69:7775–7783. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Dasgupta A, Lim AR and Ghajar CM:
Circulating and disseminated tumor cells: Harbingers or initiators
of metastasis? Mol Oncol. 11:40–61. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Ao Z, Shah SH, Machlin LM, Parajuli R,
Miller PC, Rawal S, Williams AJ, Cote RJ, Lippman ME, Datar RH and
El-Ashry D: Identification of cancer-associated fibroblasts in
circulating blood from patients with metastatic breast cancer.
Cancer Res. 75:4681–4687. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Upreti M, Jamshidi-Parsian A, Koonce NA,
Webber JS, Sharma SK, Asea AA, Mader MJ and Griffin RJ:
Tumor-endothelial cell three-dimensional spheroids: New aspects to
enhance radiation and drug therapeutics. Transl Oncol. 4:365–376.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Sharma D, Brummel-Ziedins KE, Bouchard BA
and Holmes CE: Platelets in tumor progression: A host factor that
offers multiple potential targets in the treatment of cancer. J
Cell Physiol. 229:1005–1015. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Cristofanilli M, Budd GT, Ellis MJ,
Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ,
Terstappen LW and Hayes DF: Circulating tumor cells, disease
progression, and survival in metastatic breast cancer. N Engl J
Med. 351:781–791. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Goldkorn A, Ely B, Quinn DI, Tangen CM,
Fink LM, Xu T, Twardowski P, Van Veldhuizen PJ, Agarwal N, Carducci
MA, et al: Circulating tumor cell counts are prognostic of overall
survival in SWOG S0421: A phase III trial of docetaxel with or
without atrasentan for metastatic castration-resistant prostate
cancer. J Clin Oncol. 32:1136–1142. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Mego M, Cierna Z, Janega P, Karaba M,
Minarik G, Benca J, Sedlácková T, Sieberova G, Gronesova P,
Manasova D, et al: Relationship between circulating tumor cells and
epithelial to mesenchymal transition in early breast cancer. BMC
Cancer. 15:5332015. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Kasimir-Bauer S, Hoffmann O, Wallwiener D,
Kimmig R and Fehm T: Expression of stem cell and
epithelial-mesenchymal transition markers in primary breast cancer
patients with circulating tumor cells. Breast Cancer Res.
14:R152012. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Weismann P, Weismanova E, Masak L, Mlada
K, Keder D, Ferancikova Z, Vizvaryova M, Konecny M, Zavodna K,
Kausitz J, et al: The detection of circulating tumor cells
expressing E6/E7 HR-HPV oncogenes in peripheral blood in cervical
cancer patients after radical hysterectomy. Neoplasma. 56:230–238.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Mego M, Gao H, Lee BN, Cohen EN, Tin S,
Giordano A, Wu Q, Liu P, Nieto Y, Champlin RE, et al: Prognostic
value of EMT-circulating tumor cells in metastatic breast cancer
patients undergoing high-dose chemotherapy with autologous
hematopoietic stem cell transplantation. J Cancer. 3:369–380. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Li YM, Xu SC, Li J, Han KQ, Pi HF, Zheng
L, Zuo GH, Huang XB, Li HY, Zhao HZ, et al: Epithelial-mesenchymal
transition markers expressed in circulating tumor cells in
hepatocellular carcinoma patients with different stages of disease.
Cell Death Dis. 4:e8312013. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Jansson S, Bendahl PO, Larsson AM,
Aaltonen KE and Rydén L: Prognostic impact of circulating tumor
cell apoptosis and clusters in serial blood samples from patients
with metastatic breast cancer in a prospective observational
cohort. BMC Cancer. 16:4332016. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Chang MC, Chang YT, Chen JY, Jeng YM, Yang
CY, Tien YW, Yang SH, Chen HL, Liang TY, Wang CF, et al: Clinical
significance of circulating tumor microemboli as a prognostic
marker in patients with pancreatic ductal adenocarcinoma. Clin
Chem. 62:505–513. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Zhao Q, Barclay M, Hilkens J, Guo X,
Barrow H, Rhodes JM and Yu LG: Interaction between circulating
galectin-3 and cancer-associated MUC1 enhances tumour cell
homotypic aggregation and prevents anoikis. Mol Cancer. 9:1542010.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Cheung KJ, Padmanaban V, Silvestri V,
Schipper K, Cohen JD, Fairchild AN, Gorin MA, Verdone JE, Pienta
KJ, Bader JS and Ewald AJ: Polyclonal breast cancer metastases
arise from collective dissemination of keratin 14-expressing tumor
cell clusters. Proc Natl Acad Sci USA. 113:E854–E863. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Au SH, Storey BD, Moore JC, Tang Q, Chen
YL, Javaid S, Sarioglu AF, Sullivan R, Madden MW, O’Keefe R, et al:
Clusters of circulating tumor cells traverse capillary-sized
vessels. Proc Natl Acad Sci USA. 113:4947–4952. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Cima I, Kong SL, Sengupta D, Tan IB, Phyo
WM, Lee D, Hu M, Iliescu C, Alexander I, Goh WL, et al:
Tumor-derived circulating endothelial cell clusters in colorectal
cancer. Sci Transl Med. 8:345ra892016. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Fabisiewicz A and Grzybowska E: CTC
clusters in cancer progression and metastasis. Med Oncol.
34:122017. View Article : Google Scholar
|
|
108
|
Punnoose EA, Atwal SK, Spoerke JM, Savage
H, Pandita A, Yeh RF, Pirzkall A, Fine BM, Amler LC, Chen DS and
Lackner MR: Molecular biomarker analyses using circulating tumor
cells. PLoS One. 5:e125172010. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Zhang L, Ridgway LD, Wetzel MD, Ngo J, Yin
W, Kumar D, Goodman JC, Groves MD and Marchetti D: The
identification and characterization of breast cancer CTCs competent
for brain metastasis. Sci Transl Med. 5:180ra482013. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Chéry L, Lam HM, Coleman I, Lakely B,
Coleman R, Larson S, Aguirre-Ghiso JA, Xia J, Gulati R, Nelson PS,
et al: Characterization of single disseminated prostate cancer
cells reveals tumor cell heterogeneity and identifies dormancy
associated pathways. Oncotarget. 5:9939–9951. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Yu M, Bardia A, Wittner BS, Stott SL, Smas
ME, Ting DT, Isakoff SJ, Ciciliano JC, Wells MN, Shah AM, et al:
Circulating breast tumor cells exhibit dynamic changes in
epithelial and mesenchymal composition. Science. 339:580–584. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Harouaka R, Kang Z, Zheng SY and Cao L:
Circulating tumor cells: Advances in isolation and analysis, and
challenges for clinical applications. Pharmacol Ther. 141:209–221.
2014. View Article : Google Scholar :
|
|
113
|
Beije N, Jager A and Sleijfer S:
Circulating tumor cell enumeration by the CellSearch system: The
clinician’s guide to breast cancer treatment? Cancer Treat Rev.
41:144–150. 2015. View Article : Google Scholar
|
|
114
|
Freidin MB, Tay A, Freydina DV, Chudasama
D, Nicholson AG, Rice A, Anikin V and Lim E: An assessment of
diagnostic performance of a filter-based antibody-independent
peripheral blood circulating tumour cell capture paired with
cytomorphologic criteria for the diagnosis of cancer. Lung Cancer.
85:182–185. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Warkiani ME, Khoo BL, Wu L, Tay AK, Bhagat
AA, Han J and Lim CT: Ultra-fast, label-free isolation of
circulating tumor cells from blood using spiral microfluidics. Nat
Protoc. 11:134–148. 2016. View Article : Google Scholar
|
|
116
|
Saucedo-Zeni N, Mewes S, Niestroj R,
Gasiorowski L, Murawa D, Nowaczyk P, Tomasi T, Weber E, Dworacki G,
Morgenthaler NG, et al: A novel method for the in vivo isolation of
circulating tumor cells from peripheral blood of cancer patients
using a functionalized and structured medical wire. Int J Oncol.
41:1241–1250. 2012.PubMed/NCBI
|
|
117
|
Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan
A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M, et al: The
epithelial-mesenchymal transition generates cells with properties
of stem cells. Cell. 133:704–715. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Jolly MK, Jia D, Boareto M, Mani SA,
Pienta KJ, Ben-Jacob E and Levine H: Coupling the modules of EMT
and stemness: A tunable ‘stemness window’ model. Oncotarget.
6:25161–25174. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Jolly MK, Tripathi SC, Jia D, Mooney SM,
Celiktas M, Hanash SM, Mani SA, Pienta KJ, Ben-Jacob E and Levine
H: Stability of the hybrid epithelial/mesenchymal phenotype.
Oncotarget. 7:27067–27084. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Damaskos C, Garmpis N, Valsami S, Kontos
M, Spartalis E, Kalampokas T, Kalampokas E, Athanasiou A, Moris D,
Daskalopoulou A, et al: Histone deacetylase inhibitors: An
attractive therapeutic strategy against breast cancer. Anticancer
Res. 37:35–46. 2017. View Article : Google Scholar
|
|
121
|
Škovierová H, Vidomanová E, Mahmood S,
Sopková J, Drgová A, Červeňová T, Halašová E and Lehotský J: The
molecular and cellular effect of homocysteine metabolism imbalance
on human health. Int J Mol Sci. 17:17332016. View Article : Google Scholar :
|
|
122
|
Stintzing S, Kemmerling R, Kiesslich T,
Alinger B, Ocker M and Neureiter D: Myelodysplastic syndrome and
histone deacetylase inhibitors: ‘To be or not to be acetylated’? J
Biomed Biotechnol. 2011:2141432011. View Article : Google Scholar
|
|
123
|
Li A, Liu Z, Li M, Zhou S, Xu Y, Xiao Y
and Yang W: HDAC5, a potential therapeutic target and prognostic
biomarker, promotes proliferation, invasion and migration in human
breast cancer. Oncotarget. 7:37966–37978. 2016.PubMed/NCBI
|
|
124
|
Stojanovic N, Hassan Z, Wirth M, Wenzel P,
Beyer M, Schäfer C, Brand P, Kroemer A, Stauber RH, Schmid RM, et
al: HDAC1 and HDAC2 integrate the expression of p53 mutants in
pancreatic cancer. Oncogene. 36:1804–1815. 2017. View Article : Google Scholar
|
|
125
|
Mann BS, Johnson JR, He K, Sridhara R,
Abraham S, Booth BP, Verbois L, Morse DE, Jee JM, Pope S, et al:
Vorinostat for treatment of cutaneous manifestations of advanced
primary cutaneous T-cell lymphoma. Clin Cancer Res. 13:2318–2322.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Marks PA: Discovery and development of
SAHA as an anticancer agent. Oncogene. 26:1351–1356. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Barbarotta L and Hurley K: Romidepsin for
the treatment of peripheral T-Cell lymphoma. J Adv Pract Oncol.
6:22–36. 2015.PubMed/NCBI
|
|
128
|
Libby EN, Becker PS, Burwick N, Green DJ,
Holmberg L and Bensinger WI: Panobinostat: A review of trial
results and future prospects in multiple myeloma. Expert Rev
Hematol. 8:9–18. 2015. View Article : Google Scholar
|
|
129
|
Ghajar CM: Metastasis prevention by
targeting the dormant niche. Nat Rev Cancer. 15:238–247. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Marcucci F, Stassi G and De Maria R:
Epithelial-mesenchymal transition: A new target in anticancer drug
discovery. Nat Rev Drug Discov. 15:311–325. 2016. View Article : Google Scholar : PubMed/NCBI
|