Introduction
Cardiovascular disease (CVD) is one of the primary
diseases currently threatening human health. In particular, acute
myocardial infarction (AMI) is a factor that primarily results in
increasing morbidity of CVD patients (1). Therefore, early, timely and accurate
diagnosis and evaluation of AMI are essential for actively
administrating effective treatment (2). Furthermore, early diagnosis may
result in timely cardiac reperfusion and reduce mortality (2). The early treatment of AMI is crucial
in the favorable prognosis of patients. At present, creatine kinase
isozyme and myoglobin are the predominant serum biomarkers used for
the clinical diagnosis of AMI (3). Notably, the aforementioned markers
have attained certain levels in sensitivity and specificity of the
early diagnosis of AMI (3).
However, researchers have continued their efforts in studying novel
serum markers with increased sensitivity and specificity (4). Serum markers reflecting the
prognosis for AMI patients are of primary research interest
(4).
It has previously een demonstrated that non-coding
microRNAs (miRNAs) are closely associated with the genesis,
development and prognosis of all diseases (5). miRNA expression demonstrates tissue
specificity and high stability in the blood (6). Therefore, myocardium specific miRNAs
have been speculated to act as ideal biomarkers for the early
diagnosis of AMI (5).
Furthermore, miRNA is important in numerous pathophysiological
processes. These include the genesis and development of Myocardial
Infarction (MI), myocardial fibrosis following MI and myocardial
remodeling (7). A previous study
suggested that miRNA is crucial in the genesis and development of
human diseases, including tumor initiation, cardiovascular disease,
diabetes, immune system and renal diseases (7). Furthermore, the effects of miRNAs
generally manifest as a complicated regulatory network formed by
multiple miRNAs during regulation of disease genesis and
development (7). Therefore, the
study of miRNA is of great importance to the understanding of
genesis and developmental mechanisms of various diseases.
Under normal physiological status, the myocardium is
energy-supplemented primarily via fat oxidation. However, in the
case of an insufficient coronary blood supply, the myocardium is
under anoxic conditions (8) and
fatty acid oxidation efficiency is low (8). Furthermore, glucose and
glycogenolysis for energy supply only account for a small part of
aerobic metabolism (9). The
persistent ischemia and hypoxia results in irreversible
mitochondrial injury and myocardial cell death (9). Cell death occurs in three ways:
Necrosis, apoptosis and autophagy (10). Apoptosis and autophagy have
previously been demonstrated to be involved in ischemia reperfusion
injury (10).
The mechanistic target of rapamycin (mTOR) signaling
pathway receives and integrates multiple signals (11). These signals include amino acids,
glucose, oxidative stress and growth factors (11). Therefore, mTOR exhibits an
important regulatory role in cell growth, proliferation, and
protein synthesis (12). mTOR
signaling has been verified to be one of the canonical autophagy
regulatory pathways (13). It is
the signaling pathway that senses the cell nutritional status
(13) and primarily exerts an
autophagy-associated inhibitory effect on cardiac cell apoptosis,
whilst stimulating cell growth and proliferation (13).
The phosphoinositide 3-kinase (PI3K)/RAC-γ
serine/threonine-protein kinase (Akt)/mTOR signaling pathway
exhibits a critical regulatory role in autophagy. A previous study
suggests that research has been successful in identifying
inhibitory drugs targeting various signaling pathways in order to
treat growth of tumors (14).
mTOR is the downstream molecule of Akt in the PI3K/Akt regulatory
pathway. It is involved in regulating protein synthesis, cell cycle
and angiogenesis. PI3K/Akt/mTOR signaling pathway is a core pathway
that promotes cell growth, movement, protein synthesis, survival,
and hormone, growth factor and nutrient metabolism (15). The present study investigated the
effects of miRNA-145 on AMI and the potential underlying
mechanism.
Materials and methods
Ethics and AMI model
Adult male Sprague-Dawley (180–220 g; n=12) rats
were maintained in cages at 21±2°C, under a 12 h light-dark cycle,
with 55±5% constant humidity, and had free access to food and
water. All rats were randomized into two groups: Control (n=10) and
AMI model groups (n=10). All animal experimentation was performed
in accordance with the NIH Guide for the Care and Use of Laboratory
Animals of Cangzhou Central Hospital, Hebei Medical University
(Cangzhou, China), and approved by the Ethics Committee of Cangzhou
Central Hospital. Rats were anesthetized with pentobarbital sodium
(35 mg/kg, i.p.) and exposed following the skin incision in the
fourth intercostal space of a left thoracotomy. A snare occlude was
used to ligate the left anterior descending coronary artery with
6-0 silk suture. Cardiac ischemia was verified by visual
observation and continuous electrocardiogram monitoring. The
coronary artery was reperfused by releasing the knot following 1 h
of occlusion. A total of 3 h following induction of AMI, cardiac
tissue was harvested.
Haematoxylin and eosin (H&E)
staining
Cardiac tissue was harvested under pentobarbital
sodium (35 mg/kg, i.p.) and washed with PBS. Cardiac tissue was
fixed with 4% paraformaldehyde for 24 h and embedded into paraffin.
Samples were cut into 4.0 µm of sections and sections were
stained with H&E for 5 min at room temperature and observed
under a LSM 780 NLO confocal microscope (Carl Zeiss AG, Oberkochen,
Germany).
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR) and gene expression
microarrays
Total RNA was extracted from tissue samples or cells
using TRIzol® kit (Invitrogen; Thermo Fisher Scientific,
Inc., Waltham, MA, USA) and total RNA (200 ng) was then reverse
transcribed to cDNA using an RT kit (Takara Biotechnology Co.,
Ltd., Dalian, China). RT-qPCR was performed using SYBR Premix Ex
TaqII (Takara Biotechnology Co., Ltd.) and amplification occurred
under the following conditions: Pre-denaturation for 10 min at
94°C; 40 cycles of 30 sec at 94°C, 30 sec at 55°C and 30 min at
72°C, followed by an extension step for 10 min at 72°C. Primers
sequences sued were as follows: miRNA-145 forward, 5′-GGT CCA GTT
TTC CCA GG-3′ and reverse 5′-CAG TGC GTG TCG TGG AGT-3′; U6
forward, 5′-AGA AGG CTG GGG CTC ATT TG-3′ and reverse 5′-AGG GGC
CAT CCA CAG TCT TC-3′. Data using RT-qPCR was quantified using the
2−∆∆Cq method (16).
A total of 500 ng total RNA was used to execute the
gene expression microarrays, and amplified using the Ovation PicoSL
WTA System V2 kit (Nugen Technologies. Inc., CA, USA). cDNA samples
were Cy3-labeled using the SureTag DNA labeling kit (Agilent
Technologies, Inc., Santa Clara, CA, USA). The scanning was
conducted using a SureScan Microarray Scanner and Feature
Extraction software, version 10.7.3.1 (Agilent Technologies,
Inc.).
Cell culture and cell transfection
The H9c2 cell line was cultured and maintained in
Dulbecco's minimum essential medium (DMEM, Thermo Fisher
Scientific, Inc.) supplemented with 10% fetal bovine serum
(HyClone; GE Healthcare Life Sciences, Logan, UT, USA) at 37°C, in
an environment containing 5% CO2. 100 ng of miRNA-145
mimics (5′-GUC CAG UUU UCC CAG GAA UCC CU-3′), 100 ng of miRNA-145
inhibitors (5′-AGG GAU UCC UGG GAA AAC UGG AC-3′) and 100 ng of
negative control (5′-CAG UAC UUU UGU GUA GUA CAA-3′) were
transfected into H9c2 cells using Lipofectamine 2000 (Thermo Fisher
Scientific, Inc) at 37°C according to the manufacturer's protocol.
After transfection for 4 h, old medium was removed and new DMEM was
added into H9c2 cells for 20, 44 or 68 h. Then, H9c2 cells were
subjected to a hypoxia/reoxygenation protocol for 2 h.
Luciferase reporter gene assay
Bioinformatics software on http://www.targetscan.org was adopted to predict the
targeted correlation between miRNA-145 and Akt3. AKT3-3′UTR-WT
plasmid and miR-145 mimics were constructed by Shanghai GenePharma,
Co., Ltd (Shanghai, China) and transfected using Lipofectamine 2000
(Thermo Fisher Scientific, Inc.). The expression of reporter gene
was presented using luminometer reading (TD20/20; Turner Designs,
Sunnyvale, CA, USA) by the activity ratio of firefly luciferase and
renilla luciferase.
Western blotting
Following cell transfection (n=3) for 48 h, cells
were washed with PBS, and total protein was extracted using
radioimmunoprecipitation assay lysis buffer (Beyotime Institute of
Biotechnology, Nanjing, China), and then quantified using a
bicinchoninic acid assay (Beyotime Institute of Biotechnology). A
total of 50 µg total protein was separated by 8–12% sodium
dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and
transferred onto a polyvinylidene fluoride membrane. The membrane
was blocked with 5% milk in Tris buffered saline Tween-20 (TBST)
and incubated with primary antibodies against B cell lymphoma 2
associated apoptosis regulator (Bax, cat. no. sc-6236; 1:500; Santa
Cruz Biotechnology; Inc., Dallas, TX, USA), p-Akt (cat. no.
sc-7985-R; 1:500; Santa Cruz Biotechnology; Inc.), p-mTOR (cat. no.
sc-101738; 1:500; Santa Cruz Biotechnology; Inc.), microtubule
associated protein 1 light chain 3 (LC3, cat. no. sc-292354; 1:500;
Santa Cruz Biotechnology; Inc.) and GAPDH (cat. no. sc-25778;
1:500; Santa Cruz Biotechnology; Inc.) at 4°C overnight. Following
this, the membrane was washed with TBST and incubated with goat
anti-rabbit IgG-horse radish peroxidase (cat. no. sc-2004; 1:5,000;
Santa Cruz Biotechnology; Inc.) for 1 h at 37°C. Protein bands were
exposed by BeyoECL Moon (Beyotime Institute of Biotechnology) and
analyzed using Bio-Rad Laboratories Quantity One software, version
3.0 (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
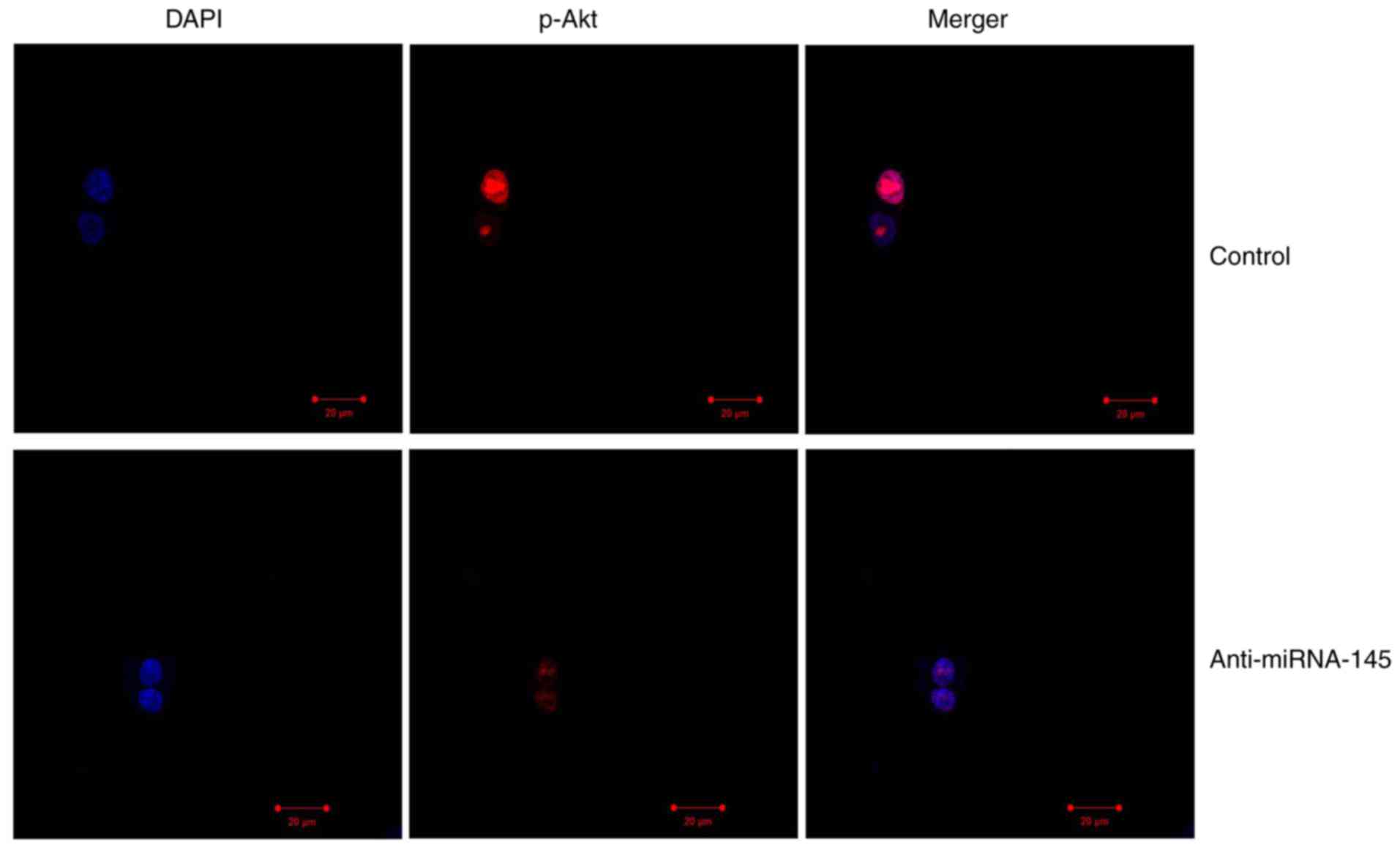
Immunofluorescence
Following cell transfection, (n=3) for 48 h, cells
were washed with PBS for 15 min and fixed with 4% paraformaldehyde
for 15 min at room temperature. Cells were incubated with 0.1%
Triton X-100 for 15 min at room temperature and blocked with 5%
bovine serum albumin (Beyotime Institute of Biotechnology) in PBS
for 1 h at room temperature and incubated with the primary antibody
against LC3 (cat. no. sc-292354; 1:100; Santa Cruz Biotechnology;
Inc.), p-Akt (cat. no. sc-7985-R; 1:100; Santa Cruz Biotechnology;
Inc.) at 4°C overnight. Following washing with PBS, cells were
incubated in a mixture of fluorescent secondary antibody (Alexa 488
anti-mouse immunoglobulin G; 1:100, cat. no. sc-516248; Santa Cruz
Biotechnology; Inc.) for 1 h at room temperature, incubated with
DAPI assay for 30 min and analyzed using a LSM 780 NLO confocal
microscope (Carl Zeiss AG, Oberkochen, Germany).
MTT assay
Following cell transfection (n=3) for 24, 48 or 72
h, cells were stained with 20 µl MTT (5 g/l, G3582; Promega
Corporation, Madison, WI, USA) for 4 h at 37°C, in an incubator in
an environment containing 5% CO2. A total of 150
µl dimethyl sulfoxide was added to cells and shaken for 10
min. Cell proliferation was measured using a microplate reader
(SpectraMax M5; Molecular Devices, LLC, Sunnyvale, CA, USA) at a
wavelength of 490 nm.
Flow cytometry
Following cell transfection (n=3) for 48 h at 37°C,
cells (1×106 cell/ml) were collected at 1,000 × g for 10
min at 4°C and washed with PBS, fixed with 4% paraformaldehyde for
15 min at room temperature and resuspended with 150 µl
binding buffer. A total of 10 µl Annexin V-FITC and 5
µl propidium iodide (BB-4101-2; BestBio Science., Shanghai,
China) staining solution were added to the cells for 15 min, in the
dark. Flow cytometry was used to detect cell apoptosis and analyzed
using Flowjo 7.6.1 (FlowJo, LLC,).
Statistical analysis
Data are presented as the mean ± standard deviation
(n=3) using SPSS software, version 17.0 (SPSS Inc., Chicago, IL,
USA), and were analyzed by one-way analysis of variance (ANOVA) or
two-way ANOVA followed by Tukey's post-hoc test. P<0.05 was
considered to indicate a statistically significant difference.
Results
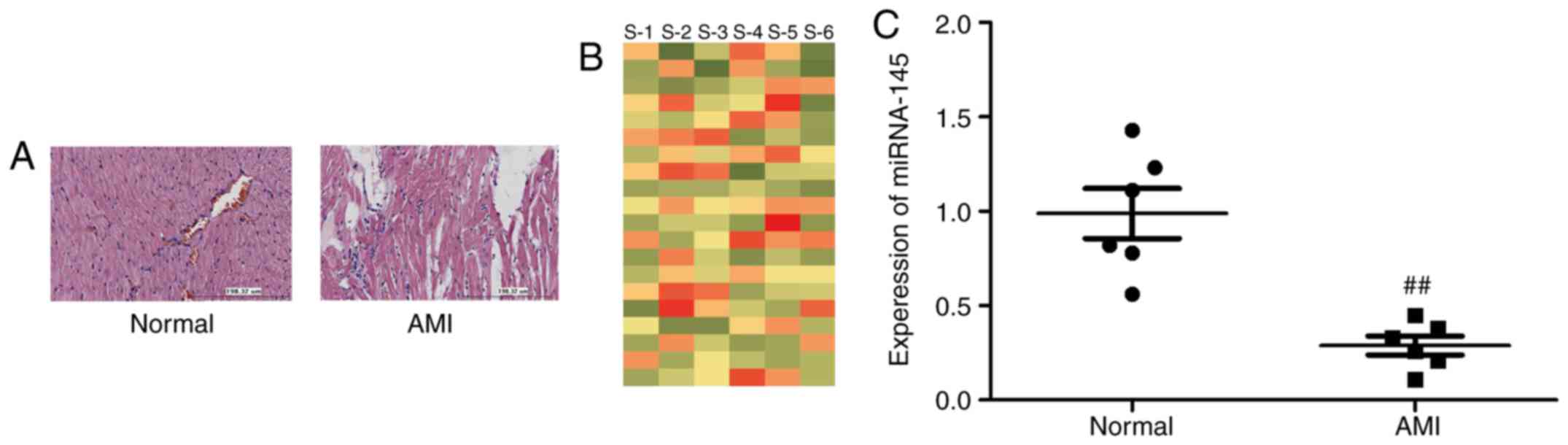
Expression of miRNA-145 in AMI in vivo
model
Firstly, the present study measured the alteration
of miRNAs in the AMI in viv model using the microarray gene
chip method. As presented in Fig.
1A, H&E staining of heart tissue indicated that there was
myocardial damage in the AMI model, compared with normal group.
miRNA-145 expression was downregulated in the AMI rat model,
compared with control group (Fig.
1B). In addition, miRNA-145 expression was analyzed using
RT-qPCR. Fig. 1C demonstrated
that miRNA-145 expression was downregulated in the AMI rat model,
compared with control group. It was therefore hypothesized that
miRNA-145 may be a regulator for AMI.
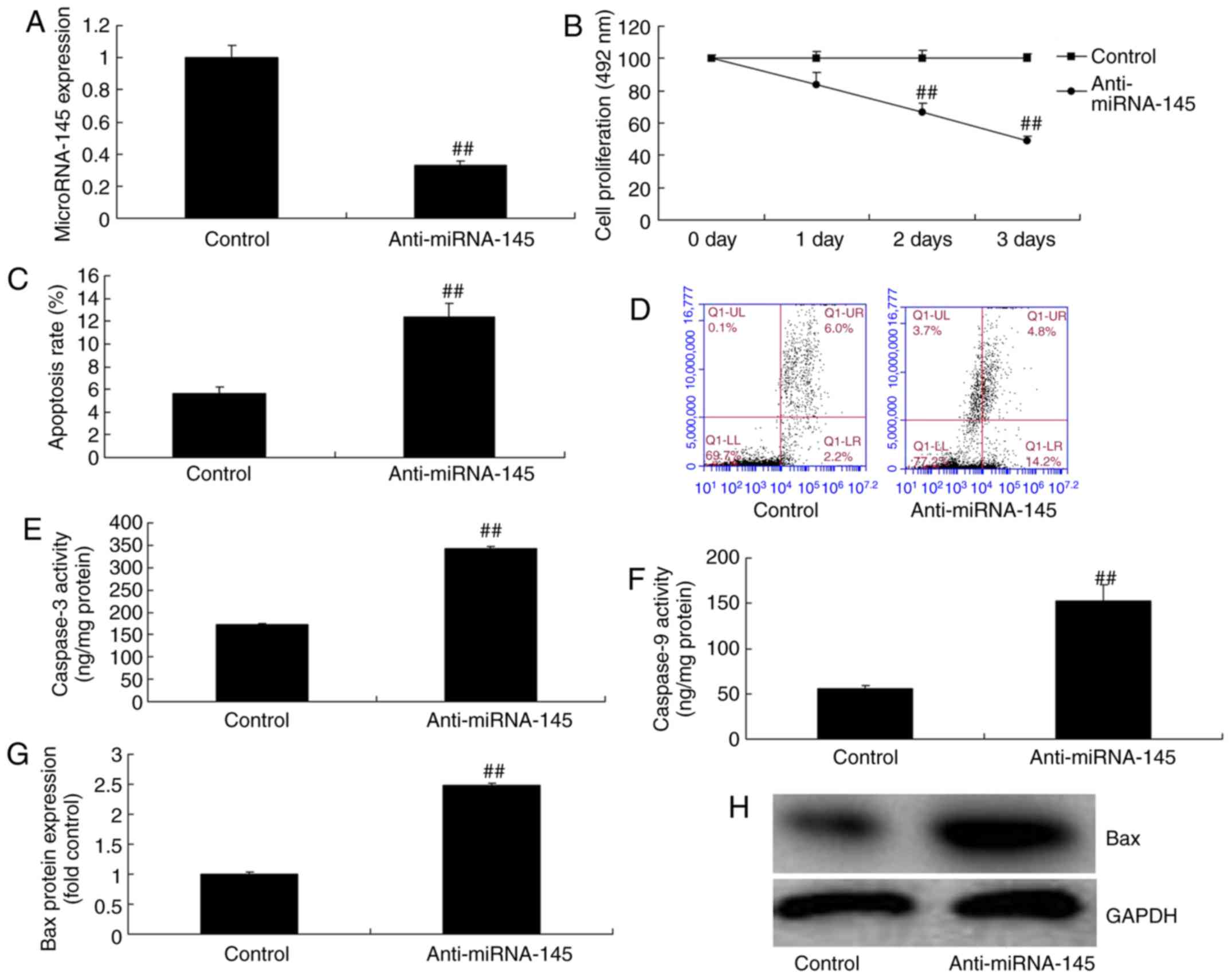
Downregulation of miRNA-145 increases
cardiac cell apoptosis in an in vitro model of AMI
To test the function of miRNA-145 in an in
vitr model of AMI, the present study downregulated miRNA-145
expression levels using anti-miRNA-145 inhibitor. As presented in
Fig. 2A, anti-miRNA-145 mimics
decreased miRNA-145 expression, compared with control group.
Downregulation of miRNA-145 inhibited cell proliferation and
increased apoptosis rate, compared with control group (Fig. 2B–D). Downregulation of miRNA-145
additionally promoted caspase-3 and -9 activities, and induced Bax
protein expression, compared with control group (Fig. 2E–H).
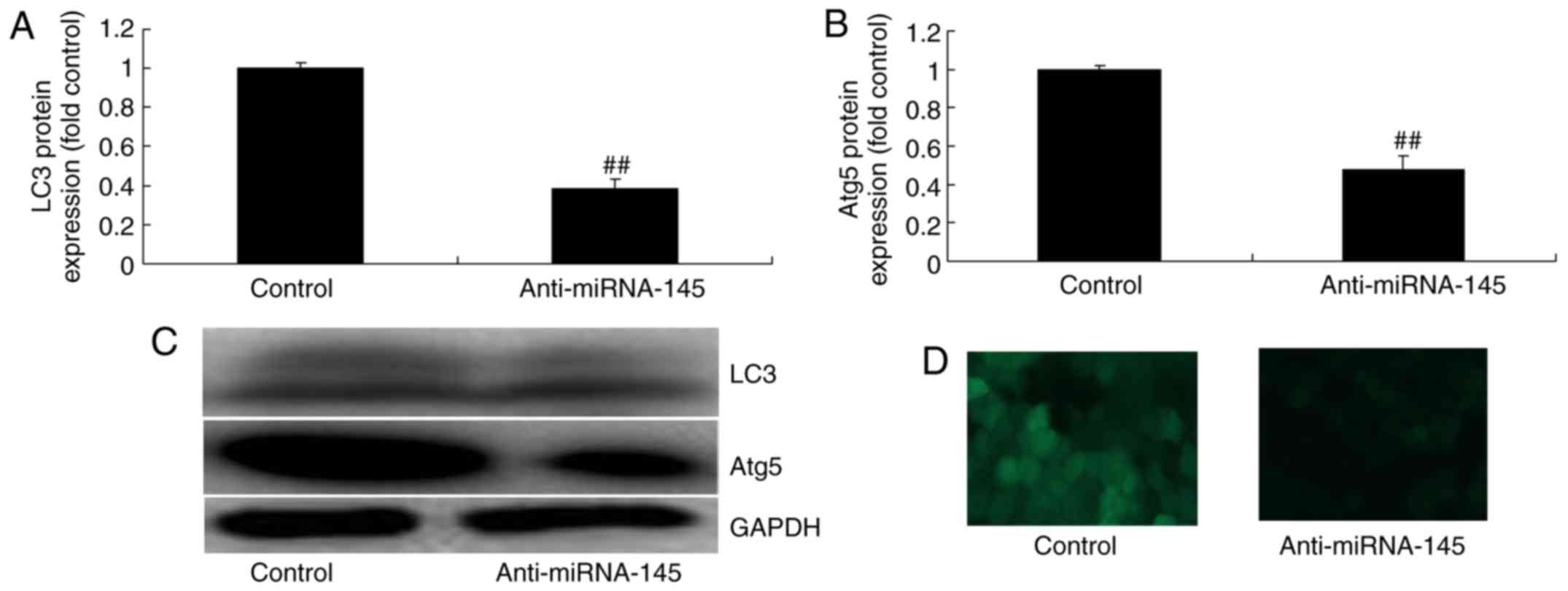
Downregulation of miRNA-145 suppresses
autophagy in an in vitro model of AMI
To validate the mechanism of miRNA-145 on apoptosis
in AMI, the present study measured the alterations of autophagy.
Downregulation of miRNA-145 suppressed LC3 and ATG5 protein
expression compared with control group (Fig. 3A–C). Immunofluorescent staining
demonstrated that downregulation of miRNA-145 suppressed LC3
protein expression compared with control group (Fig. 3D).
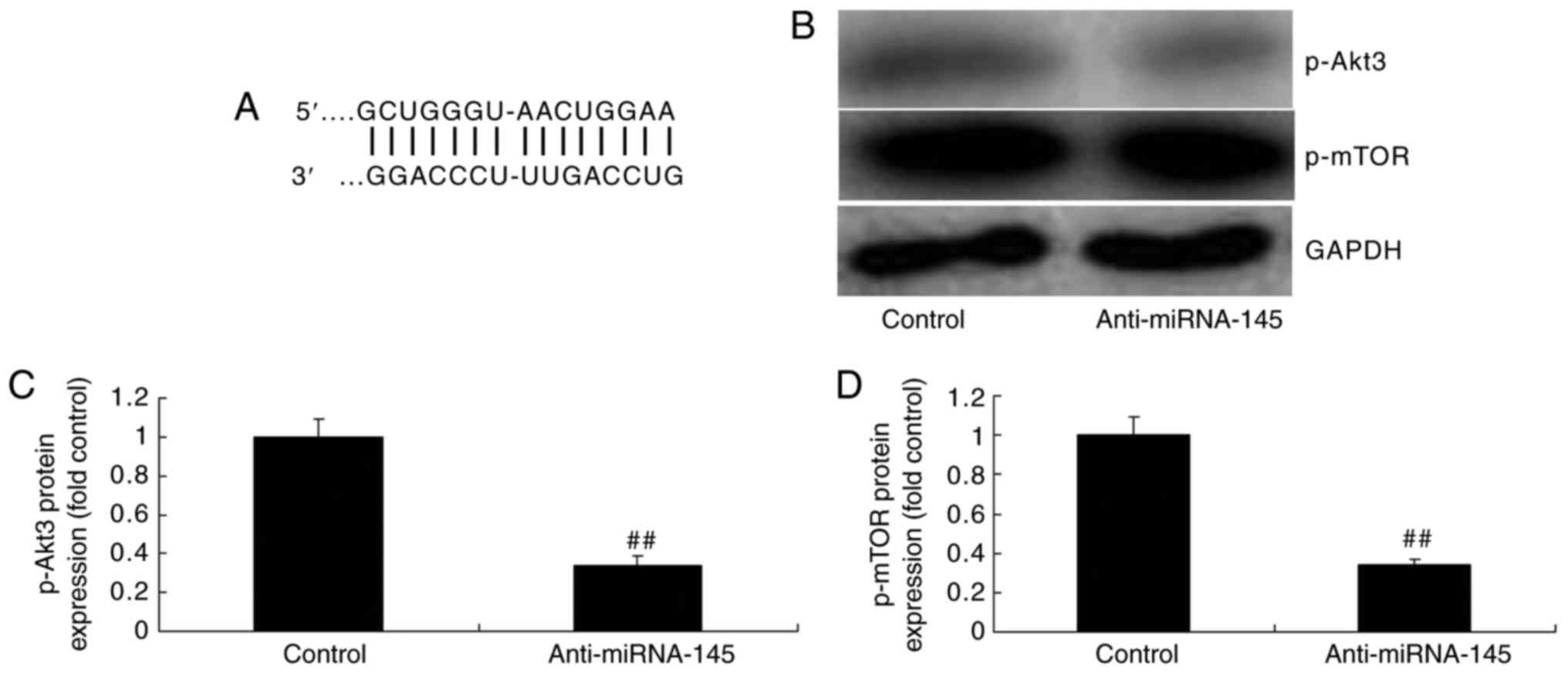
Downregulation of miRNA-145 suppresses
p-Akt3 and p-mTOR protein expression in an in vitro model of
AMI
Bioinformatics software (http://www.targetscan.org) was used to analyze the
targeted association between miRNA-145 and Akt3. As presented in
Fig. 4A, Akt3 was predicted to be
the target gene of miRNA-145. The results of the western blotting
demonstrated that downregulation of miRNA-145 suppressed p-Akt3 and
p-mTOR protein expression, compared with control group (Fig. 4B–D). The immunofluorescent
staining results presented in Fig.
5 revealed that downregulation of miRNA-145 suppressed p-Akt3
protein expression, compared with control group.
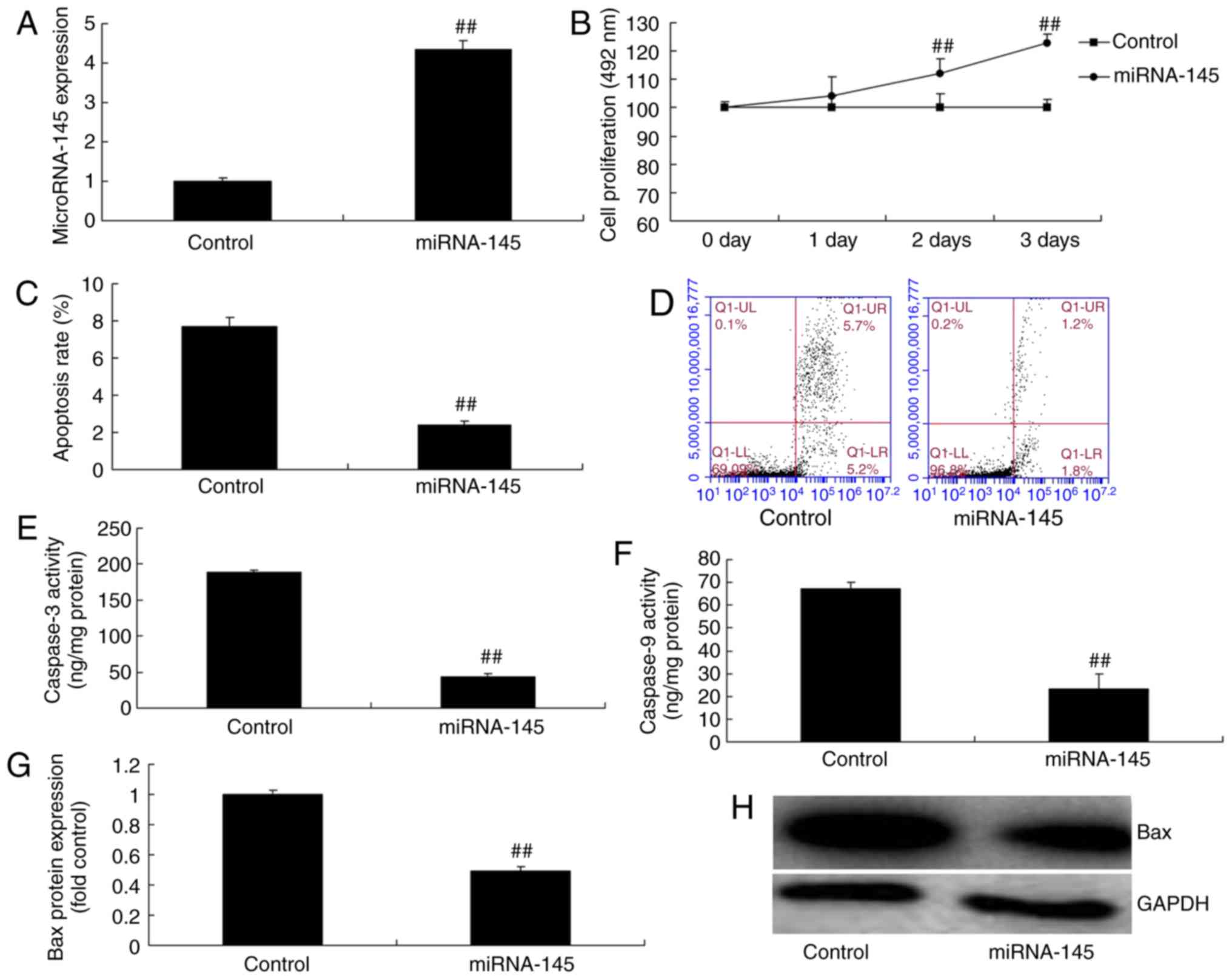
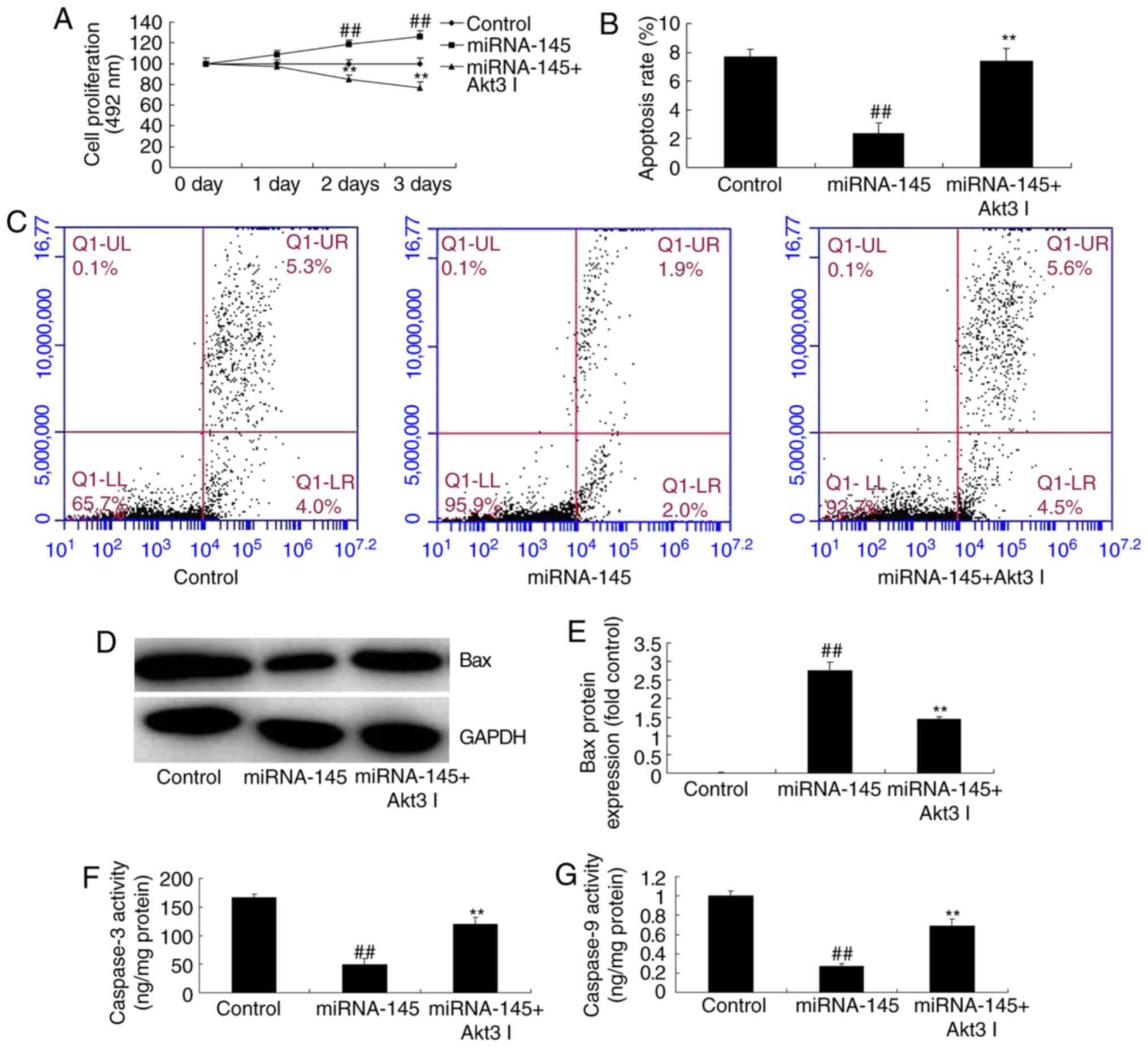
Overexpression of miRNA-145 decreases
cardiac cell apoptosis in an in vitro model of AMI
To demonstrate the function of miRNA-145 in cardiac
cell apoptosis, the present study used miRNA-145 mimics to increase
miRNA-145 expression. As presented in Fig. 6A, miRNA-145 mimics increased
miRNA-145 expression, compared with control group. Overexpression
of miRNA-145 promoted cell proliferation, and decreased cardiac
cell apoptosis, compared with control group (Fig. 6B–D). The overexpression of
miRNA-145 reduced Bax protein expression and inhibited caspase-3/9
activities compared with control group (Fig. 6E–H).
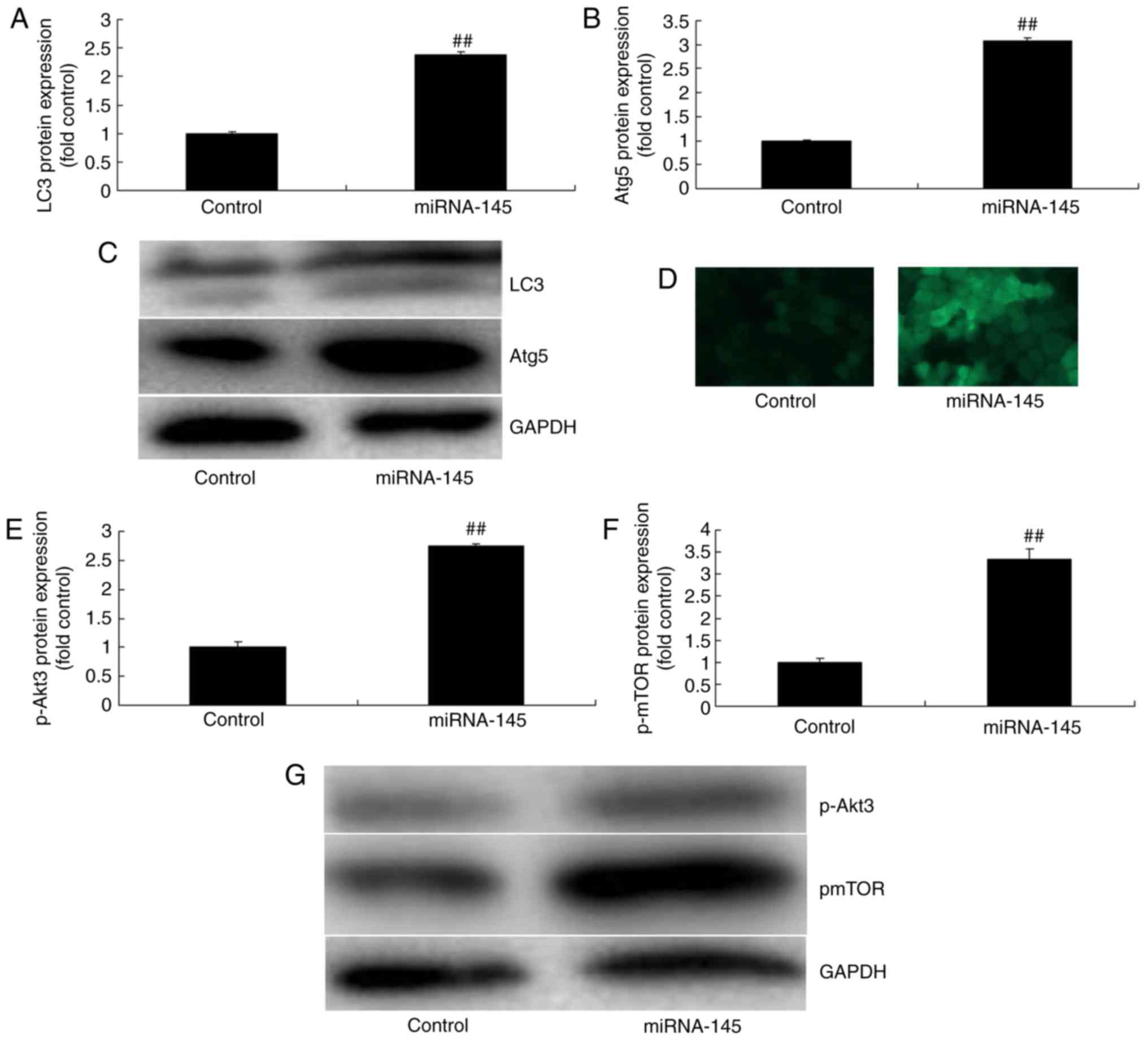
Overexpression of miRNA-145 induces
p-Akt3 and p-mTOR protein expression and promotes autophagy in an
in vitro model of AMI
The overexpression of miRNA-145 promoted LC3 and AGT
5 protein expression, compared with control group (Fig 7A–C). Immunofluorescent staining
indicated that the overexpression of miRNA-145 promoted LC3 protein
expression compared with control group (Fig. 7D). In addition, it was
demonstrated that p-Akt3 and p-mTOR protein expression levels were
increased, compared with control group (Fig. 7E–G).
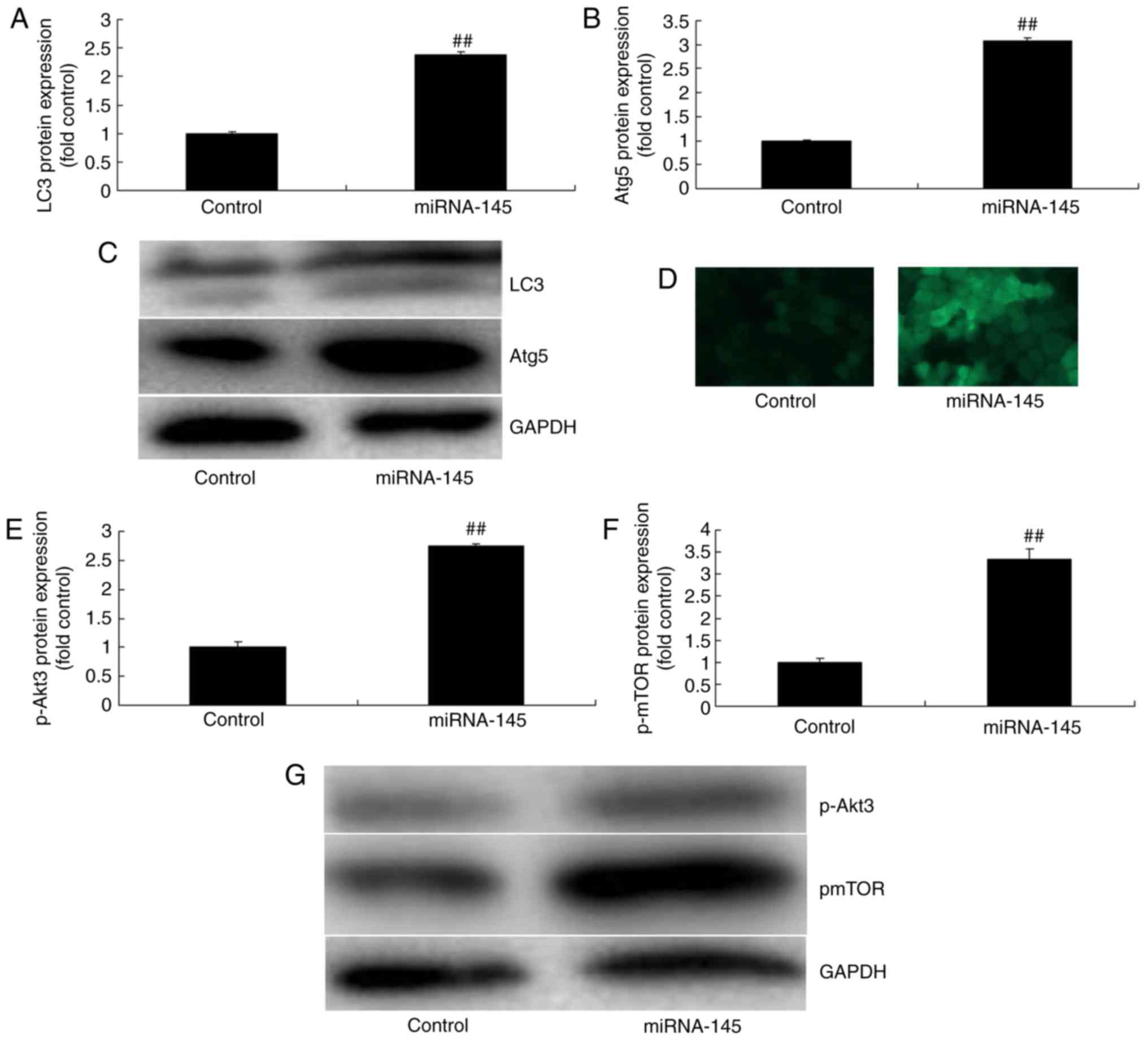 | Figure 7Overexpression of miRNA-145 induces
autophagy and increases p-Akt3 and p-mTOR protein expression in an
in vitr model of acute myocardial infarction. Quantitative
representation of (A) LC3, (B) Atg5 protein expression levels and
(C) representative image, detected via western blotting. (D)
Immunofluorescent staining for LC3 protein expression. Quantitative
analysis of (E) p-Akt3, (F) p-mTOR protein expression levels and
(G) representative image, detected via western blotting.
##P<0.01 vs. control group. miRNA, microRNA;
miRNA-145, miRNA-145 overexpression group; control, control group;
LC3, microtubule associated protein 1 light chain 3; Atg5,
autophagy protein 5; p, phosphorylated; Akt3, RAC-γ
serine/threonine-protein kinase; mTOR, mechanistic target of
rapamycin. |
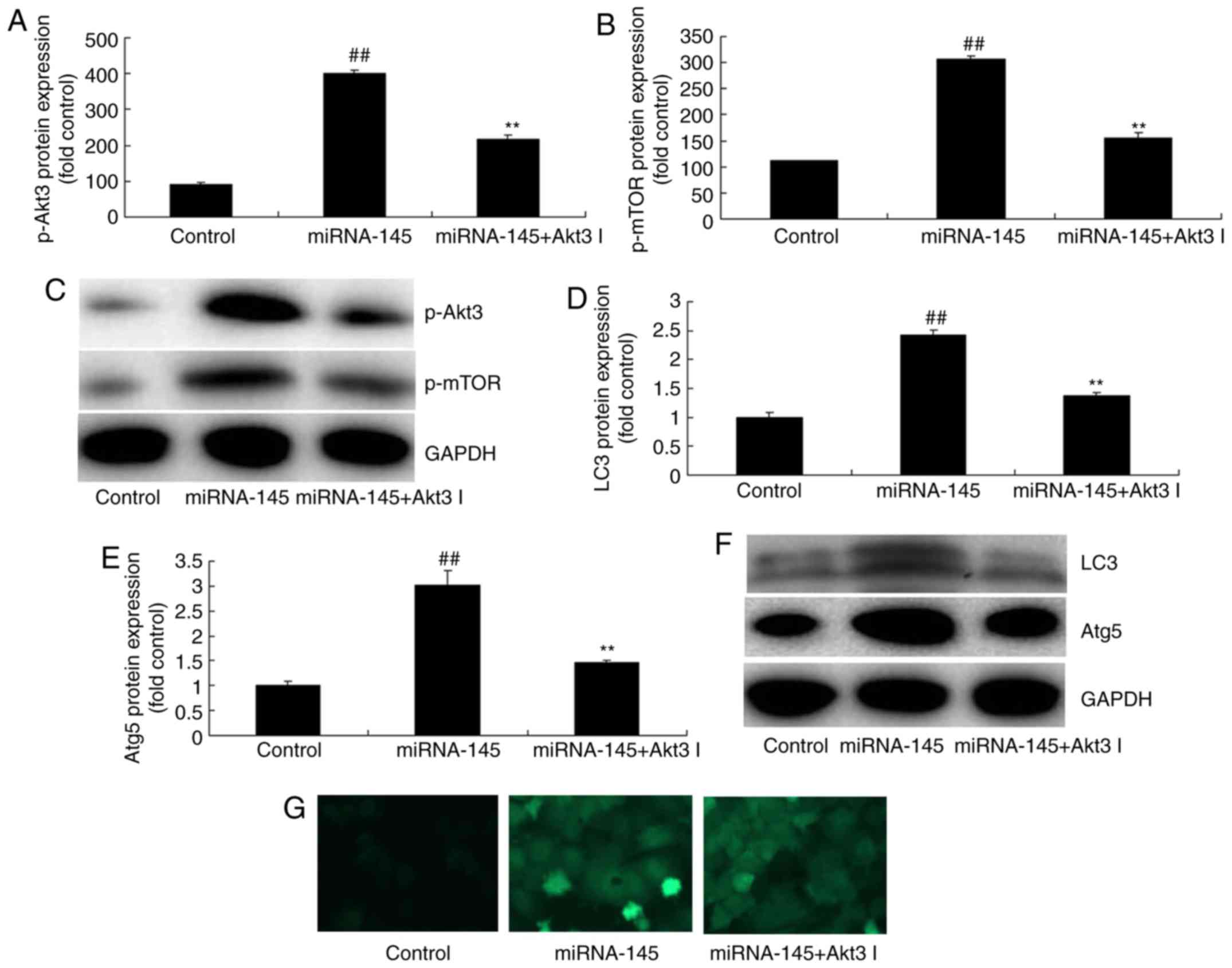
Inhibition of Akt3 suppresses the effects
of miRNA-145 upregulation on cell apoptosis in an in vitro model of
AMI
The present study next explored the function of Akt3
in the effects of miRNA-145 upregulation on cell apoptosis. As
presented in Fig. 8A–C,
administration of 1 nM Akt3 inhibitor GSK2110183 following
miRNA-145 upregulation, suppressed p-Akt3 and p-mTOR protein
expression, compared with upregulated miRNA-145 group. Furthermore,
the inhibition of Akt3 following miRNA-145 upregulation suppressed
LC3 and AGT5 protein expression, compared with upregulated
miRNA-145 group (Fig. 8D–G). The
effects of miRNA-145 upregulation on cell proliferation, cardiac
cell apoptosis and Bax protein expression, in addition to
caspase-3/9 activities, were reversed by Akt3 inhibitor, compared
with upregulated miRNA-145 group (Fig. 9).
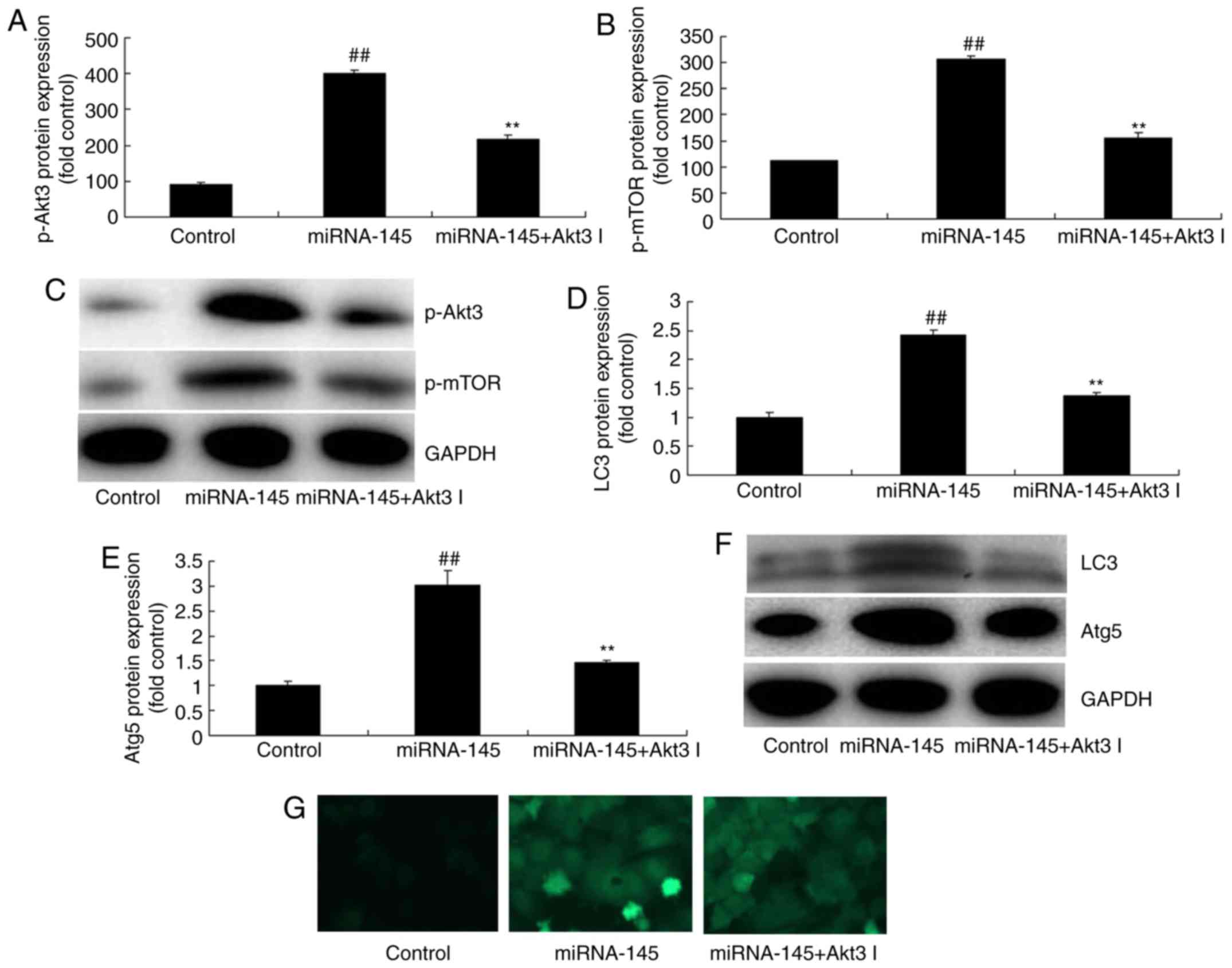 | Figure 8Inhibition of Akt3 suppresses the
effects of miRNA-145 upregulation on cell apoptosis in an in
vitr model of acute myocardial infarction. Quantification of
(A) p-Akt3, (B) p-mTOR protein expression levels and (C)
representative image, detected via western blotting. Quantification
of (D) LC3, (E) Atg5 protein expression levels and (F)
representative image, detected via western blotting. (G)
Immunofluorescent staining for LC3 protein expression levels.
##P<0.01 vs. control group; **P<0.01
vs. miRNA-145 overexpression group. miRNA, microRNA; control,
control group; miRNA-145, miRNA-145 overexpression group; miRNA-145
+ Akt3 I, miRNA-145 overexpression and Akt3 inhibitor group; LC3,
microtubule associated protein 1 light chain 3; Atg5, autophagy
protein 5; p, phosphorylated; Akt3, RAC-γ serine/threonine-protein
kinase; mTOR, mechanistic target of rapamycin. |
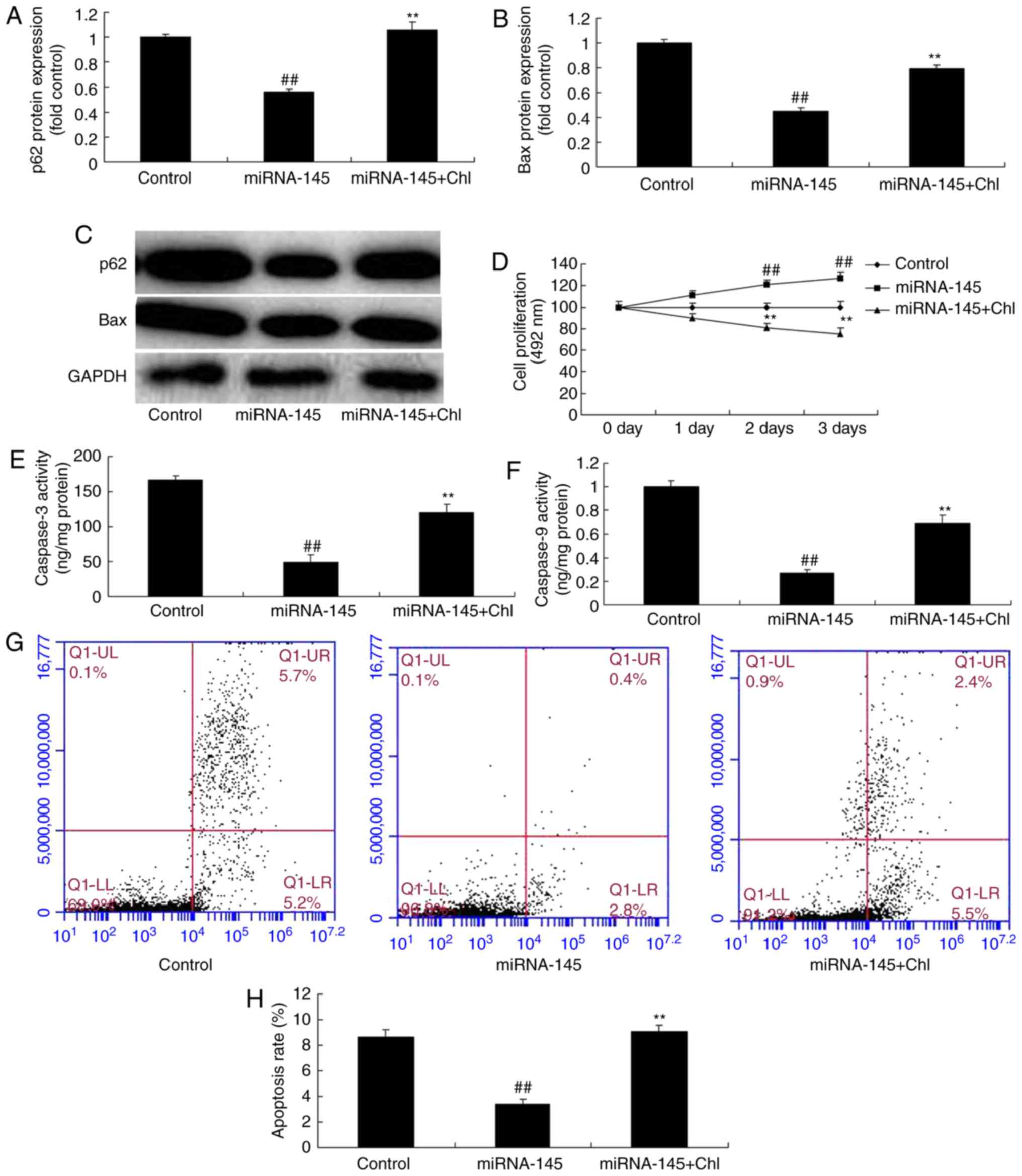
Lysosomal inhibitors inhibit the effects
of miRNA-145 upregulation on cell apoptosis in an in vitro model of
AMI
Exposure to a total of 5 µM lysosomal
inhibitor chloroquine diphosphate following miRNA-145 upregulation
increased Bax protein expression levels compared with miRNA-145
upregulated group (Fig. 10A–C).
In addition, chloroquine diphosphate reduced cell growth, increased
cardiac cell apoptosis, and promoted caspase-3 and caspase-9
activities, compared with miRNA-145 upregulated group (Fig. 10D–H).
Discussion
AMI is the primary cause of coronary heart
disease-associated mortalities (1). Early thrombolytic therapy or
percutaneous coronary intervention has been adopted to recover
blood perfusion in the ischemic site. This method effectively
rescues the injured myocardium (1) and improves myocardial ischemia and
necrosis (2). However, adverse
effects include partial myocardial cell apoptosis and loss of heart
function. These effects are termed ischemia reperfusion injury
(2). At present, the potential
cellular mechanism leading to ischemia reperfusion injury remains
to be fully elucidated (3). The
present study observed that miRNA-145 expression was downregulated
in the AMI rat model, compared with control group.
miRNA is a highly conserved small non-coding RNA
molecule (17) that regulates
mRNA gene expression through complementary base pairing with mRNA
(17). miRNA is intracellular RNA
(17) and may regulate the
post-transcription expression levels of multiple mRNAs. Therefore,
it exhibits the potential to act as a useful therapeutic target.
Numerous studies have been conducted researching the pathogenesis
of CVD (18). Furthermore, miRNA
alterations have been demonstrated to be involved in angiogenesis,
myocardial hypertrophy, heart failure and myocardial fibrosis
(18). The present study
demonstrated that the downregulation of miRNA-145 increased cardiac
cell apoptosis in an in vitr model of AMI. In accordance
with the findings, Zhang et al (19) additionally suggests that miRNA-145
levels decrease in AMI.
Autophagy is commonly seen in acute and chronic
myocardial ischemia and heart failure. It has previously been
demonstrated that autophagy is markedly upregulated in ischemia
reperfusion myocardial cells (20). Cell autophagy is the process by
which lysosomes in the eukaryote degrade the damaged substances in
the cell (21). In this process,
various damaged proteins or organelles are consumed by the
autopha-gosome with a bilayer structure (21). They are sent to the lysosome
(animal) or vacuole (yeast and plant) for degradation, or are
recycled (21). The results of
the present study revealed that downregulation of miRNA-145
suppressed autophagy in an in vitr model of AMI. Higashi
et al (22) suggests that
miRNA-145 repairs infarcted myocardium by accelerating
cardiomyocyte autophagy (21).
PI3K activates the serine/threonine Akt. Akt leads
to the phosphorylation of serine/threonine mTOR via numerous
regulators (23). mTOR is a
serine/threonine protein kinase (23), highly conserved from fungus to
mammal. The primary effect of mTOR is to regulate the cell cycle,
cell growth and proliferation (24). Therefore, mTOR in mammals
maintains a constant state of activation. This results in a dynamic
balance between cell growth and metabolism. Research has verified
that mTOR has a role as an active switch in regulatory cell
autophagy. It senses the alterations of multiple intracellular and
extracellular signals. In addition to this, it activates or
inhibits the rate of autophagy (24). Subsequently, it enhances cell
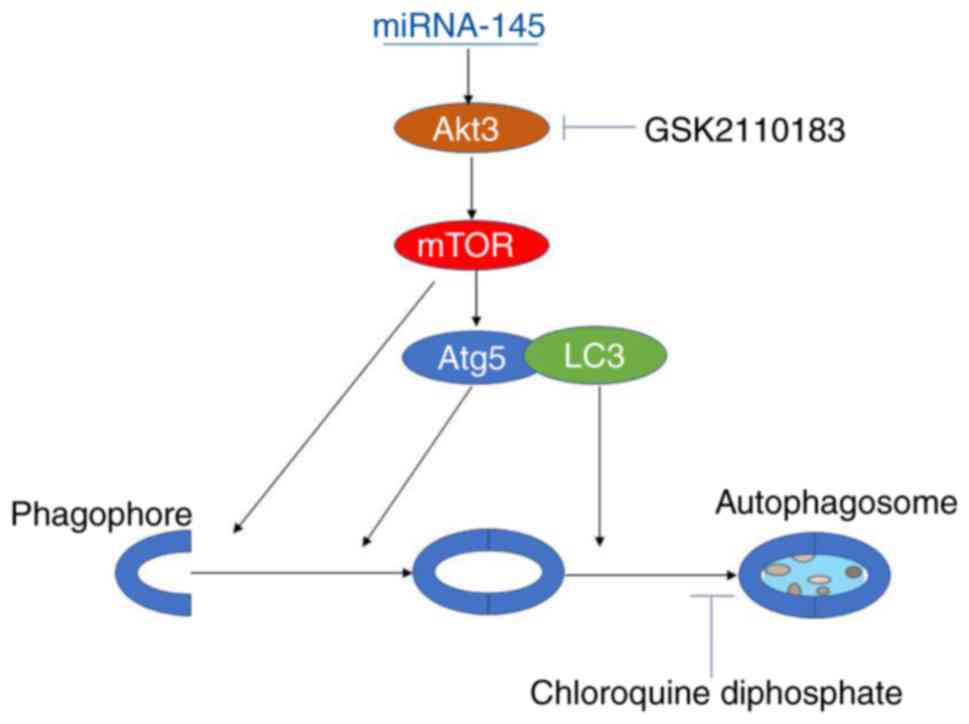
adaptability to environmental stress (24). The present study observed that the
downregulation of miRNA-145 suppressed p-Akt3 and p-mTOR protein
expression. Furthermore, the inhibition of Akt3 decreased the
effects of miRNA-145 upregulation on cell apoptosis. The lysosomal
inhibitor chloroquine diphosphate inhibited the effects of
miRNA-145 upregulation on autophagy to adjust cell apoptosis, in an
in vitr model of AMI (Fig.
11). Zhou et al (25)
reported that an increase in miRNA-145 inhibits the proliferation
and invasion of invasive pituitary adenoma cells through AKT3/mTOR
signaling pathway in viv and in vitro (25).
In conclusion, the results of the present study
demonstrated that miRNA-145 inhibited myocardial infarction-induced
apoptosis by induction of autophagy via the Akt3/mTOR signaling
pathway, in viv and in vitro. This finding increases
the understanding of miRNA in the field of molecular biology
research, and will potentially be useful for treating myocardial
infarction patients in the future. However, further analysis and
larger samples are necessary in order to validate the results.
Acknowledgments
Not applicable.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
LY designed the experiment; NG, YC, SZ, JW, FL, YW
and XC performed the experiments; LY analyzed the data and wrote
the manuscript.
Ethics approval and consent to
participate
All animal experiments were approved by the Ethics
Committee of Cangzhou Central Hospital (Cangzhou, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pöss J, Köster J, Fuernau G, Eitel I, de
Waha S, Ouarrak T, Lassus J, Harjola VP, Zeymer U, Thiele H and
Desch S: Risk stratification for patients in cardiogenic shock
after acute myocardial infarction. J Am Coll Cardiol. 69:1913–1920.
2017. View Article : Google Scholar
|
|
2
|
Myojo M, Ando J, Uehara M, Daimon M,
Watanabe M and Komuro I: Feasibility of extracorporeal shock wave
myocardial revascularization therapy for post-acute myocardial
infarction patients and refractory angina pectoris patients. Int
Heart J. 58:185–190. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yurdakul S and Aytekin S: Left atrial
mechanical functions in patients with anterior myocardial
infarction: A velocity vector imaging-based study. Kardiol Pol.
71:1266–1272. 2013. View Article : Google Scholar
|
|
4
|
Erkol A, Oduncu V, Turan B, Kılıçgedik A,
Sırma D, Gözübüyük G, Karabay CY, Guler A, Dündar C, Tigen K, et
al: The value of plasma D-dimer level on admission in predicting
no-reflow after primary percutaneous coronary intervention and
long-term prognosis in patients with acute ST segment elevation
myocardial infarction. J Thromb Thrombolysis. 38:339–347. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Liu Z, Ye P, Wang S, Wu J, Sun Y, Zhang A,
Ren L, Cheng C, Huang X, Wang K, et al: MicroRNA-150 protects the
heart from injury by inhibiting monocyte accumulation in a mouse
model of acute myocardial infarction. Circ Cardiovasc Genet.
8:11–20. 2015. View Article : Google Scholar
|
|
6
|
Boon RA and Dimmeler S: MicroRNAs in
myocardial infarction. Nat Rev Cardiol. 12:135–142. 2015.
View Article : Google Scholar
|
|
7
|
Bronze-da-Rocha E: MicroRNAs expression
profiles in cardiovascular diseases. Biomed Res Int.
2014:9854082014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guo X, Jiang H, Yang J, Chen J, Yang J,
Ding JW, Li S, Wu H and Ding HS: Radioprotective 105 kDa protein
attenuates ischemia/reperfusion-induced myocardial apoptosis and
autophagy by inhibiting the activation of the TLR4/NF-κB signaling
pathway in rats. Int J Mol Med. 38:885–893. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Xia Y, Liu Y, Xia T, Li X, Huo C, Jia X,
Wang L, Xu R, Wang N, Zhang M, et al: Activation of
volume-sensitive Cl-channel mediates autophagy-related cell death
in myocardial ischaemia/reperfusion injury. Oncotarget.
7:39345–39362. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shao H, Yang L, Wang L, Tang B, Wang J and
Li Q: MicroRNA-34a protect myocardial cells against
ischemia-reperfusion injury through inhibiting autophagy via
regulating TNFα expression. Biochem Cell Biol. 96:349–354. 2017.
View Article : Google Scholar
|
|
11
|
Buss SJ, Riffel JH, Katus HA and Hardt SE:
Augmentation of autophagy by mTOR-inhibition in myocardial
infarction: When size matters. Autophagy. 6:304–306. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hou S, Yin X, Wang Z, Zhang J, Yuan Q and
Chen Z: Cardamonin attenuates lung carcinoma and promotes autophagy
via targeting p53 and regulating mTOR. Eur J Pharmacol.
S0014-2999:304662017.
|
|
13
|
Suhara T, Baba Y, Shimada BK, Higa JK and
Matsui T: The mTOR signaling pathway in myocardial dysfunction in
type 2 diabetes mellitus. Curr Diab Rep. 17:382017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yao H and Han X and Han X: The
cardioprotection of the insulin-mediated PI3K/Akt/mTOR signaling
pathway. Am J Cardiovasc Drugs. 14:433–442. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tanaka Y, Hosoyama T, Mikamo A, Kurazumi
H, Nishimoto A, Ueno K, Shirasawa B and Hamano K: Hypoxic
preconditioning of human cardiosphere-derived cell sheets enhances
cellular functions via activation of the PI3K/Akt/mTOR/HIF-1α
pathway. Am J Transl Res. 9:664–673. 2017.
|
|
16
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
17
|
Cortez-Dias N, Costa MC, Carrilho-Ferreira
P, Silva D, Jorge C, Calisto C, Pessoa T, Robalo Martins S, de
Sousa JC and da Silva PC: Circulating miR-122-5p/miR-133b ratio is
a specific early prognostic biomarker in acute myocardial
infarction. Circ J. 81:6132017. View Article : Google Scholar
|
|
18
|
Oyama Y, Bartman CM, Gile J and Eckle T:
Circadian MicroRNAs in cardioprotection. Curr Pharm Des.
23:3723–3730. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang M, Cheng YJ, Sara JD, Liu LJ, Liu
LP, Zhao X and Gao H: Circulating MicroRNA-145 is associated with
acute myocardial infarction and heart failure. Chin Med J (Engl).
130:51–56. 2017. View Article : Google Scholar
|
|
20
|
Wang ZG, Li H, Huang Y, Li R, Wang XF, Yu
LX, Guang XQ, Li L, Zhang HY and Zhao YZ: Nerve growth
factor-induced Akt/mTOR activation protects the ischemic heart via
restoring autophagic flux and attenuating ubiquitinated protein
accumulation. Oncotarget. 8:5400–5413. 2017.
|
|
21
|
Peng YQ, Xiong D, Lin X, Cui RR, Xu F,
Zhong JY, Zhu T, Wu F, Mao MZ, Liao XB and Yuan LQ: Oestrogen
inhibits arterial calcification by promoting autophagy. Sci Rep.
7:35492017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Higashi K, Yamada Y, Minatoguchi S, Baba
S, Iwasa M, Kanamori H, Kawasaki M, Nishigaki K, Takemura G and
Kumazaki M: MicroRNA-145 repairs infarcted myocardium by
accelerating cardiomyocyte autophagy. Am J Physiol Heart Circ
Physiol. 309:H1813–H1826. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cui J, Zhang F, Wang Y, Liu J, Ming X, Hou
J, Lv B, Fang S and Yu B: Macrophage migration inhibitory factor
promotes cardiac stem cell proliferation and endothelial
differentiation through the activation of the PI3K/Akt/mTOR and
AMPK pathways. Int J Mol Med. 37:1299–1309. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wu ST, Sun GH, Cha TL, Kao CC, Chang SY,
Kuo SC and Way TD: CSC-3436 switched tamoxifen-induced autophagy to
apoptosis through the inhibition of AMPK/mTOR pathway. J Biomed
Sci. 23:602016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhou K, Fan YD, Wu PF, Duysenbi S, Feng
ZH, Du GJ and Zhang TR: MicroRNA-145 inhibits the activation of the
mTOR signaling pathway to suppress the proliferation and invasion
of invasive pituitary adenoma cells by targeting AKT3 in vivo and
in vitro. Onco Targets Ther. 10:1625–1635. 2017. View Article : Google Scholar : PubMed/NCBI
|