Introduction
Biliary atresia (BA) results from inflammatory and
fibrotic obstruction of extrahepatic bile ducts, and is a leading
cause of neonatal cholestasis. In addition, BA is the major reason
for pediatric liver transplantation worldwide (1-3).
The majority of children with BA succumb to liver failure within a
year, and surgery is the only satisfactory treatment option, which
includes Kasai surgery and liver transplantation (4). The pathogenesis of BA is currently
unclear; therefore, there is an urgent requirement for more
effective methods to reduce the risk of treatment, and improve
diagnosis and therapeutic effects. Identification of the relevant
mechanisms is conducive to the development of novel treatment
strategies, and is beneficial to reduce BA-induced hepatic injury
and improve clinical outcomes.
The Human Genome Project indicated that although 70%
of the genome is transcribed, only ≤2% of the human genome serves
as a blueprint for protein coding (5). Until recently, long non-coding RNAs
(lncRNAs) were considered a by-product of the process of
transcription without a biological function (6). However, recent studies have revealed
that lncRNAs serve an important role in several biological events,
including post-transcriptional regulation of human genes,
epigenetic regulation, cell cycle regulation and regulation of cell
differentiation (7,8). In previous studies that have focused
on liver injury, lncRNAs have received attention, and several
lncRNAs have been reported to be closely associated with the
initiation and progression of liver injury (9-14).
It has been reported that the lncRNA Annexin A2
pseudo-gene 3 (ANXA2P3) encodes Annexin A2 pseudogenes. These
pseudogene-expressed non-coding RNAs have a functional role in
regulating their protein-coding counterparts (15). It has previously been reported
that these pseudogenes can act as signaling regulators and, in most
cases, pseudogenes and parental genes exhibit positive coupling and
positive functional correlation (16). For example, octamer-binding
transcription factor 4 (Oct4) psuedogene (Oct4P1) is a pseudogene
that overexpresses Oct4, and can promote the self-renewal of
mesenchymal stem cells and inhibit cell differentiation (17). A negative correlation between the
expression of a psuedogene of B-Raf proto-oncogene,
serine/threonine kinase (BRAF) and the degree of BRAF mutation has
been detected in thyroid carcinoma; BRAF overexpression can
effectively promote the transformation of NIH3T3 cells and induce
tumorigenesis in nude mice (18).
It has previously been reported that ANXA2 pseudogenes can be used
as novel biomarkers for the diagnosis, prognosis and targeted
therapy of glioma (19). However,
to the best of our knowledge, the biological function of ANXA2P3 in
liver injury and its expression in patients with BA have yet to be
determined.
Annexin A2 (ANXA2) is a member of the connexin
family, which is involved in several biological events, including
cell proliferation and apoptosis; in previous studies, a close
association between ANXA2 and liver damage-associated diseases has
been demonstrated (20-25). Furthermore, ANXA2 is widely
recognized as a promising serum marker of liver damage or liver
fibrosis. In patients with chronic hepatitis B-associated hepatic
fibrosis, serum ANXA2 is significantly upregulated compared with
its serum levels in healthy individuals (26). Similarly, in rats with immune
liver fibrosis and alcoholic liver models, ANXA2 on the membrane
surface is significantly upregulated (27). In addition, ANXA2 promotes liver
fibrosis by mediating von Willebrand factor secretion, which can be
used to mitigate the progression of liver fibrosis (28). Hepatic overexpression of ANXA1 and
ANXA2 inhibits acetaminophen-induced expansion of liver injury
(29). However, to date, the
biological functions of ANXA2 in liver injury and its expression in
patients with BA have not been thoroughly studied.
Based on these previous findings, the present study
aimed to investigate the expression profiles of ANXA2 and ANXA2P3
in liver tissue derived from patients with BA, and to elucidate its
involvement in liver injury. The results may provide novel insight
into the biological functions of ANXA2 and ANXA2P3, and their
underlying mechanisms of action in liver injury.
Materials and methods
Patients and specimens
Liver tissue was obtained from 20 children (age 53
days-3 months old) who were diagnosed with BA and underwent Kasai
surgery at the Department of General Surgery, Fudan University
Children’s Hospital (Shanghai, China) between March 2016 and
October 2016. Paracarcinoma liver tissue was obtained from six
children (age, 2-4 years old) who were diagnosed with
hepatoblastoma. Fresh tissue was immediately snap-frozen in liquid
nitrogen and stored at −80°C for further analysis. The present
study was approved by the Ethical Review Board of Fudan University
Children’s Hospital, and written informed consent was obtained from
all the parents of all participants enrolled.
Cell culture
The L0-2 normal human liver cell line was obtained
from the Cell Bank of the Chinese Academy of Sciences (Shanghai,
China). All cells were cultured in Dulbecco’s modified Eagle’s
medium (DMEM; Gibco; Thermo Fisher Scientific, Inc., Waltham, MA,
USA) supplemented with 10% heat-inactivated fetal bovine serum
(Sigma-Aldrich: Merck KGaA, Darmstadt, Germany), 50 U/ml penicillin
and 50 µg/ml streptomycin (Gibco; Thermo Fisher Scientific,
Inc.). Cells were maintained at 37°C in a humidified atmosphere
containing 5% CO2. In the present study, cells up to
passage 10 were used.
Cell transfection
All the procedures were performed at room
temperature unless otherwise specified. ANXA2P3 small interfering
RNA (siRNA) (si-ANXA2P3), non-targeting siRNA (si-NC) and ANXA2
siRNA (si-ANXA2) were synthesized by Shanghai GenePharma Co., Ltd.
(Shanghai, China). The siRNAs and si-NC were transfected into
2×105 L0-2 cells, after mixing with
Lipofectamine® 2000 reagent (Invitrogen; Thermo Fisher
Scientific, Inc.) for 20 min, at a final concentration of 50 nM,
unless otherwise indicated. The siRNA sequences were as follows:
si-NC for ANXA2P3: NR_001446.2 [National Center for Biotechnology
Information (NCBI) reference sequence]; si-NC for ANXA2:
NM_001002858.2 (NCBI reference sequence); scrambled negative
control vector (OE-NC) for ANXA2: NM_001002858.2 (NCBI reference
sequence); OE-NC for ANXA2P3: NR_001446.2 (NCBI reference
sequence); si-ANXA2, 5′-GGA GTG AAG AGG AAA GGA ACT-3′;
si-ANXA2P3-1, 5′-GGA TGG CTC TGT CG TTG ATT A-3′; si-ANXA2P3-2,
5′-GGT CAT CAC TCT ACA CCC TCA-3′; si-ANXA2P3-3, 5′-GGA GAG AGG ATG
TTG CCT TTG-3′. In addition, pcDNA3.1 (+) expression vectors and
OE-NC vectors were purchased from Shanghai GenePharma Co., Ltd.
After culturing in antibiotic-free DMEM for 24 h, and once
confluence reached >80%, a total of 0.5×105 cells
were transfected with pcDNA vectors (multiplicity of infection, 20)
and polybrene (final concentration, 5 µg/ml), according to
the manufacturer’s protocol. A total of 48 h post-transfection, the
transfection efficacy was assessed by reverse
transcription-quantitative polymerase chain reaction (RT-qPCR).
Qualitative analysis of gene silencing was conducted by observing
cells under a fluorescence microscope (Leica DMi1; Leica
Microsystems GmbH, Wetzlar, Germany) after 48 h of
transfection.
Total RNA extraction and RT-qPCR
Total RNA was isolated from liver samples from
patients with BA and L0-2 liver cells using TRIzol®
reagent (Invitrogen; Thermo Fisher Scientific, Inc.). Subsequently,
cDNA was synthesized from 200 ng extracted total RNA using the
PrimeScript RT reagent kit (Qiagen China Co., Ltd., Shanghai,
China), according to the manufacturer’s protocol. Briefly, 1
µg total RNA mixed with nuclease-free water was used for
cDNA synthesis with the PrimeScript RT reagent kit (Takara Bio,
Inc., Otsu, Japan), according to the manufacturer’s protocol. All
RT procedures and no-template controls were run at the same time.
Following RT, qPCR was conducted to determine the expression of
ANXA2 and ANXA2P3 using SYBR Premix Ex Taq (Takara Bio, Inc.) on an
ABI-7300 instrument (Applied Biosystems; Thermo Fisher Scientific,
Inc.). According to the manufacturer’s protocol, a final 20
µl reaction mixture was amplified using the following
reaction conditions: Predenaturation at 94°C for 5 min;
amplification for 35 cycles (denaturation at 94°C for 30 sec,
annealing at 58°C for 30 sec and extension at 72°C for 30 sec);
final extension at 72°C for 5 min. The 20 µl PCR mixture
included 2 µl cDNA, 10 µl 2X QuantiTect SYBR-Green
PCR Mix, 2 µl 10X upstream primer (forward), 2 µl 10X
downstream primer (reverse) and 4 µl RNase-free water. GAPDH
served as the control gene. The 2−ΔΔCq method was used
to determine gene expression levels (30). Primer sequences were as follows:
ANXA2P3 forward, 5′-GAG AGG ATG TTG CCT TTG-3′ reverse, 5′-TAC TGA
GCA GGT GTC TTC-3′; GAPDH forward, 5′-AAT CCC ATC ACC ATC TTC-3′
and reverse, 5′-AGG CTG TTG TCA TAC TTC-3′; and ANXA2 forward,
5′-ATG GTC TCC CGC AGT GAA GTG-3′ and reverse, 5′-TCG CCC TTA GTG
TCT TGC TGG-3′.
Immunohistochemical analysis
All procedures were performed at room temperature
unless otherwise specified. Liver tissue (~20 mm) was dissected,
post-fixed in 0.1 M PBS containing 4% paraformaldehyde for 24 h at
4°C and embedded in paraffin. Paraffin-embedded liver samples were
cut longitudinally with a microtome, to obtain 4-µm
sections. Sections were rehydrated in a microwave oven at 37°C for
30 min, and sections on microscope slides were immersed in xylene
and a diluted alcohol series (95, 90, 80 and 70%) for 15 min, in
order to dewax and rehydrate paraffin-embedded sections.
Subsequently sections were immersed in 3%
H2O2 for 10 min to quench endogenous
peroxidase activity. Sections were then rinsed two times in
distilled water (5 min/wash), and antigen retrieval was performed
using 0.01 mol/l citrate buffer solution (pH 6.0) in a microwave
oven for 20 min. Once sections were cooled to room temperature,
they were rinsed a further three times in 0.1 M PBS (5 min/wash),
and were incubated with 5% bovine serum albumin blocking solution
for 20 min to block non-specific binding. Subsequently, sections
were incubated overnight with an ANXA2 antibody (1:100; cat. no.
ab41803; Abcam, Cambridge, MA, USA) at 4°C. Sections were then
rinsed a further three times in 0.1 M PBS (5 min/wash), and were
incubated with IRDye 800-conjugated immunoglobulin G secondary
antibodies (1:1,000; cat. no. ab150077; Abcam) in Tris-buffered
saline containing 0.1% Tween-20 (TBST) for 30 min at room
temperature. The slides were stained with DAB and counterstained
with hematoxylin, prior to visualization under a Leica microscope
(DFC490; Leica Microsystems GmbH). LAS AF Lite V3.6 software (Leica
Microsystems GmbH) was used to analyze the images.
Histopathological examination
Collagen deposition in the liver was evaluated by
Masson staining. All procedures were performed at room temperature
unless otherwise specified. Liver tissues were fixed with 10%
neutral formalin for 48-72 h, embedded in paraffin, continuously
sectioned at a thickness of 5 µm, and stained with Masson
stains. Briefly, slides were placed in Bouin solution (Richard
Allen Scientific; Thermo Fisher Scientific, Inc.) for 1 h at 56°C,
after which, the slides were stained with Weigert hematoxylin
(Sigma-Aldrich; Merck KGaA) for 10 min, followed by Biebrich
scarlet-acid fuchsin for 5 min, phosphomolybdic/phosphotungstic
acid solution for 10 min and aniline blue (all Sigma-Aldrich; Merck
KGaA) for 5 min. Hepatic fibrosis was graded based on the
internationally used Metavir scoring system (31).
Western blot analysis
All the procedures were performed at room
temperature unless otherwise specified. Total protein was extracted
using mammalian protein extraction reagent (Pierce; Thermo Fisher
Scientific, Inc.) supplemented with a protease inhibitor cocktail
(Sigma-Aldrich; Merck KGaA). Total protein concentration was
determined using a bicinchoninic acid assay kit. Protein samples
(50 µg) were resolved by 10% SDS-PAGE and were then
transferred onto polyvinylidene fluoride membranes (EMD Millipore,
Billerica, MA, USA). Membranes were blocked in TBST containing 5%
w/v non-fat milk at room temperature for 1 h, and were then probed
with the following antibodies overnight: Anti-ANXA2 (1:1,000;
rabbit; cat. no. ab41803) and anti-GAPDH (1:2,500; rabbit; cat. no.
ab9485; both Abcam). Subsequently, membranes were incubated for 2 h
with specific horseradish peroxidase-conjugated secondary antibody
(1:1,000; anti-rabbit immunoglobulin G; cat. no. ab150077; Abcam)
in TBST. Proteins were visualized using an enhanced
chemiluminescence kit (Pierce; Thermo Fisher Scientific, Inc.) and
densitometric analysis was conducted using ImageJ software (V1.51;
National Institutes of Health, Bethesda, MD, USA).
Cell viability assay
All the procedures were performed at room
temperature unless otherwise specified. Transfected L0-2 cells were
seeded into a 96-well plate at a density of 2,000 cells/well and
were incubated at 37°C. Proliferation was determined using a Cell
Counting kit (CCK)-8 kit (Nanjing Keygen Biotech Co., Ltd.,
Nanjing, China) at 24, 48 (optional), 72 and 96 h
post-transfection, according to the manufacturer’s protocol.
Optical density was measured at a wavelength of 450 nm using a
microtiter plate reader.
Cell cycle analysis
All the procedures were performed at room
temperature unless otherwise specified. Transfected L0-2 cells were
washed in PBS and fixed in 70% ethanol for 2 h at 4°C. DNA staining
was conducted with propidium iodide for 15 min in the dark using a
Cellular DNA Flow Cytometric Analysis kit (Roche Diagnostics). Cell
cycle profiles were generated using a FACSCalibur flow cytometer
with ModFit 3.0 software (both BD Biosciences, San Jose, CA,
USA).
Cell apoptosis assay
Transfected L0-2 cells were stained using an Annexin
V-fluorescein isothiocyanate Apoptosis Detection kit I (BD
Biosciences), according to the manufacturer’s protocol.
Subsequently, cells were analyzed using a FACSCalibur flow
cytometer equipped with CellQuest software (version 5.1; BD
Biosciences). Cells were divided into viable cells, necrotic cells,
early apoptotic cells and late apoptotic cells.
Statistical analysis
Statistical analyses were performed using SPSS
version 18.0 software (SPSS, Inc., Chicago, IL, USA) and GraphPad
Prism (version 6.01) software (GraphPad Software, Inc., La Jolla,
CA, USA). ImageJ software (National Institutes of Health) was used
for immunohistochemical analysis and densitometric analysis of
western blotting, which was normalized to the respective loading
controls. Data are presented as the means ± standard deviation of
at least three independent experiments. The statistical
significance between groups was determined using the Student’s
t-test and one-way analysis of variance followed by a post hoc
Tukey’s test for multiple comparisons. All P-values are two-sided
and P<0.05 was considered to indicate a statistically
significant difference.
Results
ANXA2 and ANXA2P3 expression is increased
in liver tissues from patients with BA
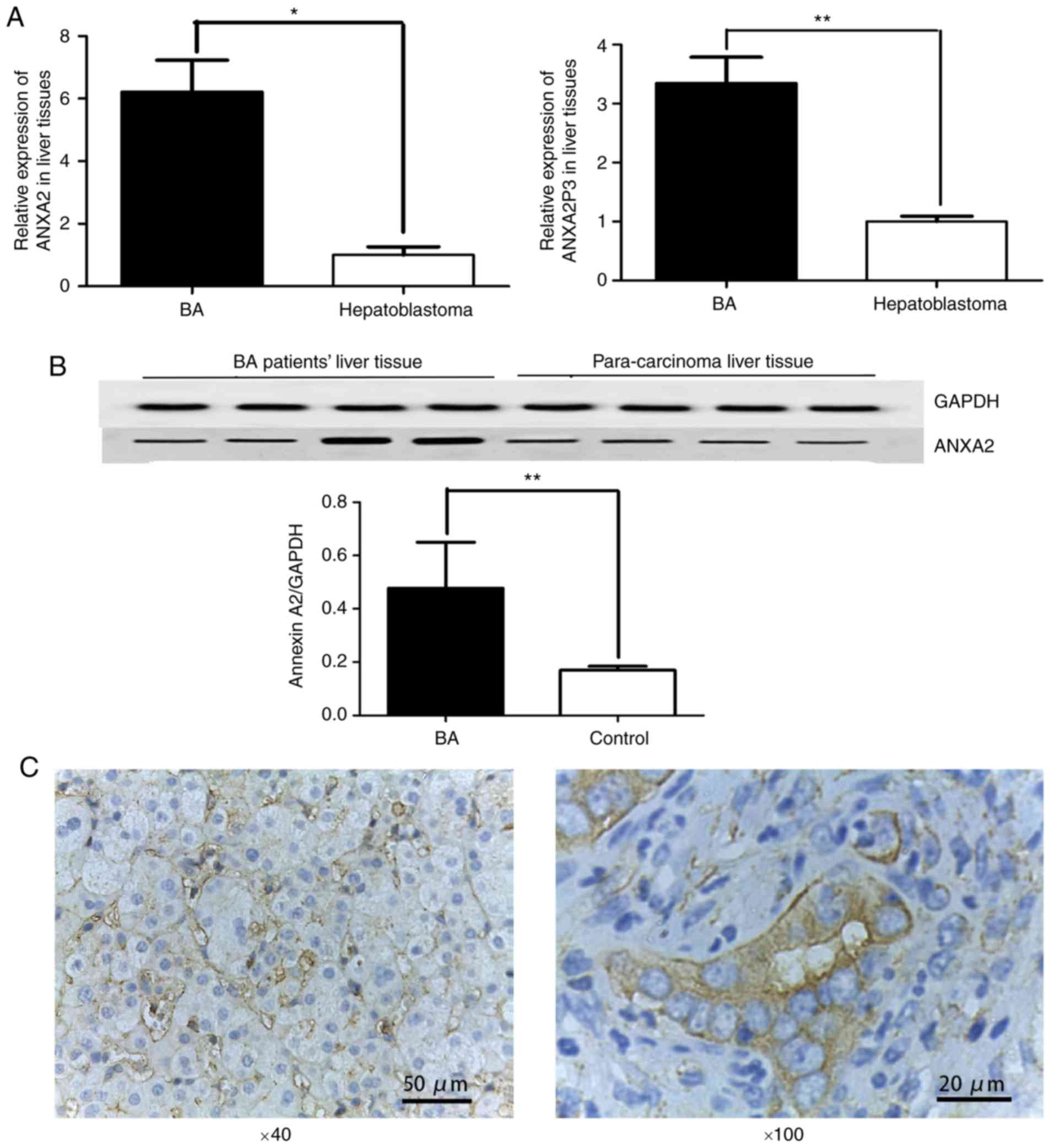
RT-qPCR was performed to determine the expression
levels of ANXA2 and ANXA2P3 in clinical samples normalized to
GAPDH. The results revealed that the expression levels of ANXA2 and
ANXA2P3 were significantly increased in liver tissues from patients
with BA compared with in paracarcinoma liver tissues from patients
with hepatoblastoma (P=0.0210 and 0.0083, respectively; Fig. 1A). Western blot analysis indicated
that ANXA2 protein expression was increased in liver tissues from
patients with BA when compared with paracarcinoma liver tissues
from patients with hepatoblastoma (Fig. 1B). Immunohistochemical staining of
liver tissues further confirmed that the protein expression levels
of ANXA2 were abundant in the cell membrane in patients with BA
(Fig. 1C). The present study also
evaluated the clinicopathological characteristics of patients with
BA, and revealed that all patients had liver fibrosis, varying
between stages 1 and 3. A total of four patients were at stage 1,
14 patients were at stage 2 and two patients were at stage 3 (data
not shown). No significant associations were determined between the
expression levels of ANXA2 and ANXA2P3 and other
clinicopathological factors, including sex and age.
ANXA2 and ANXA2P3 knockdown inhibits
liver cell proliferation, increases cell apoptosis and induces cell
cycle arrest in G1 phase in vitro
To elucidate the role of ANXA2 and ANXA2P3 in liver
injury progression, the expression levels of ANXA2 and ANXA2P3 were
downregulated via siRNA transfection and overexpressed via pcDNA3.1
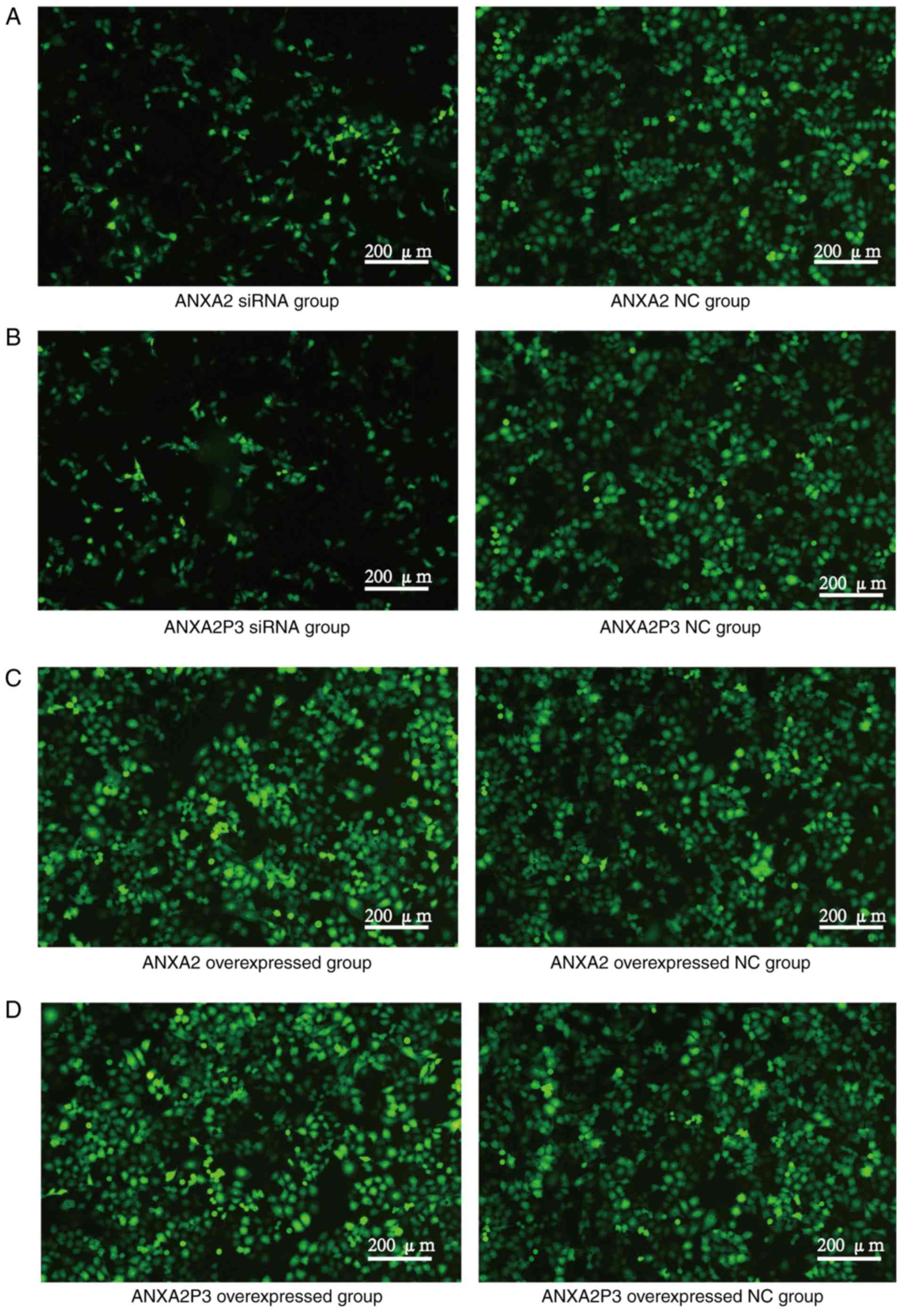
plasmid vector transfection in normal liver cells. Cells were
transfected with green fluorescent protein to detect fluorescence
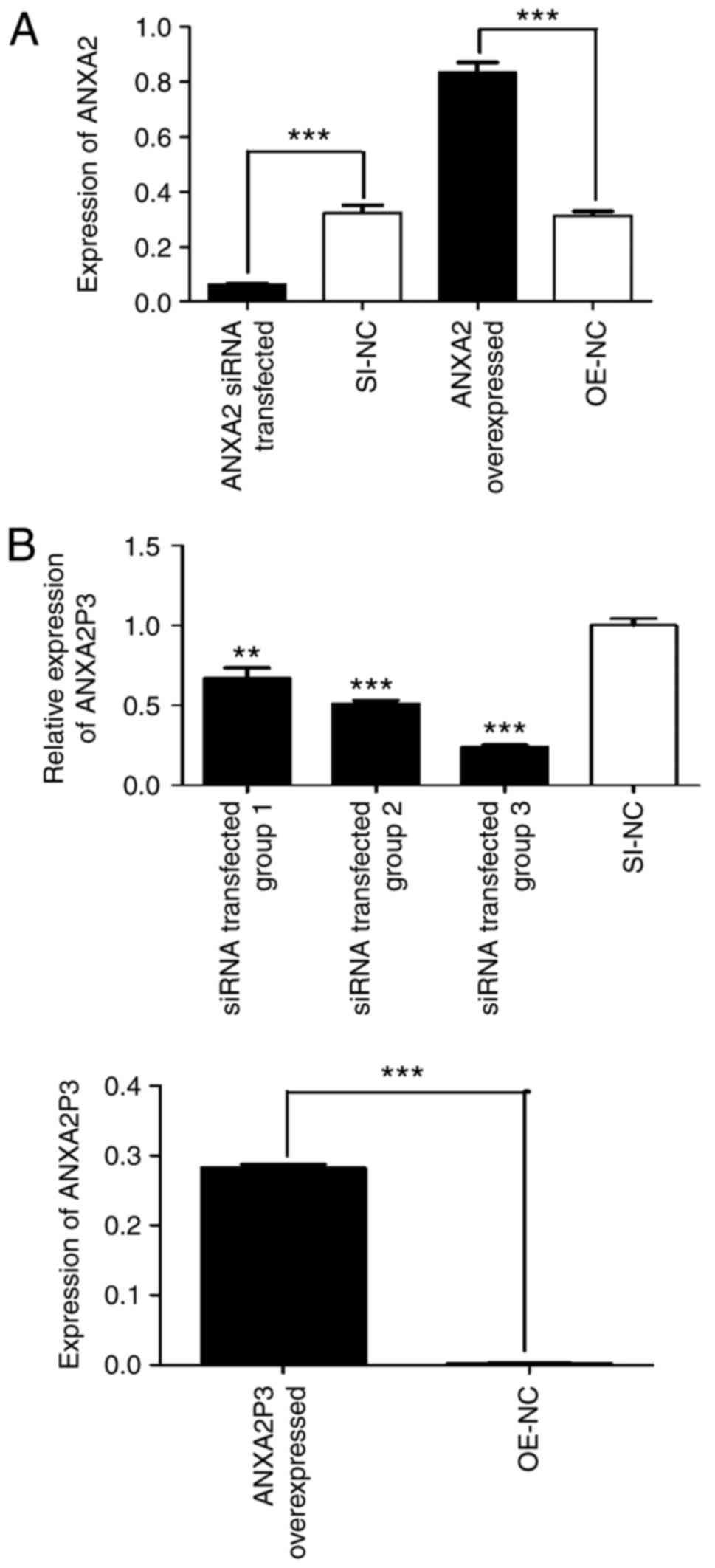
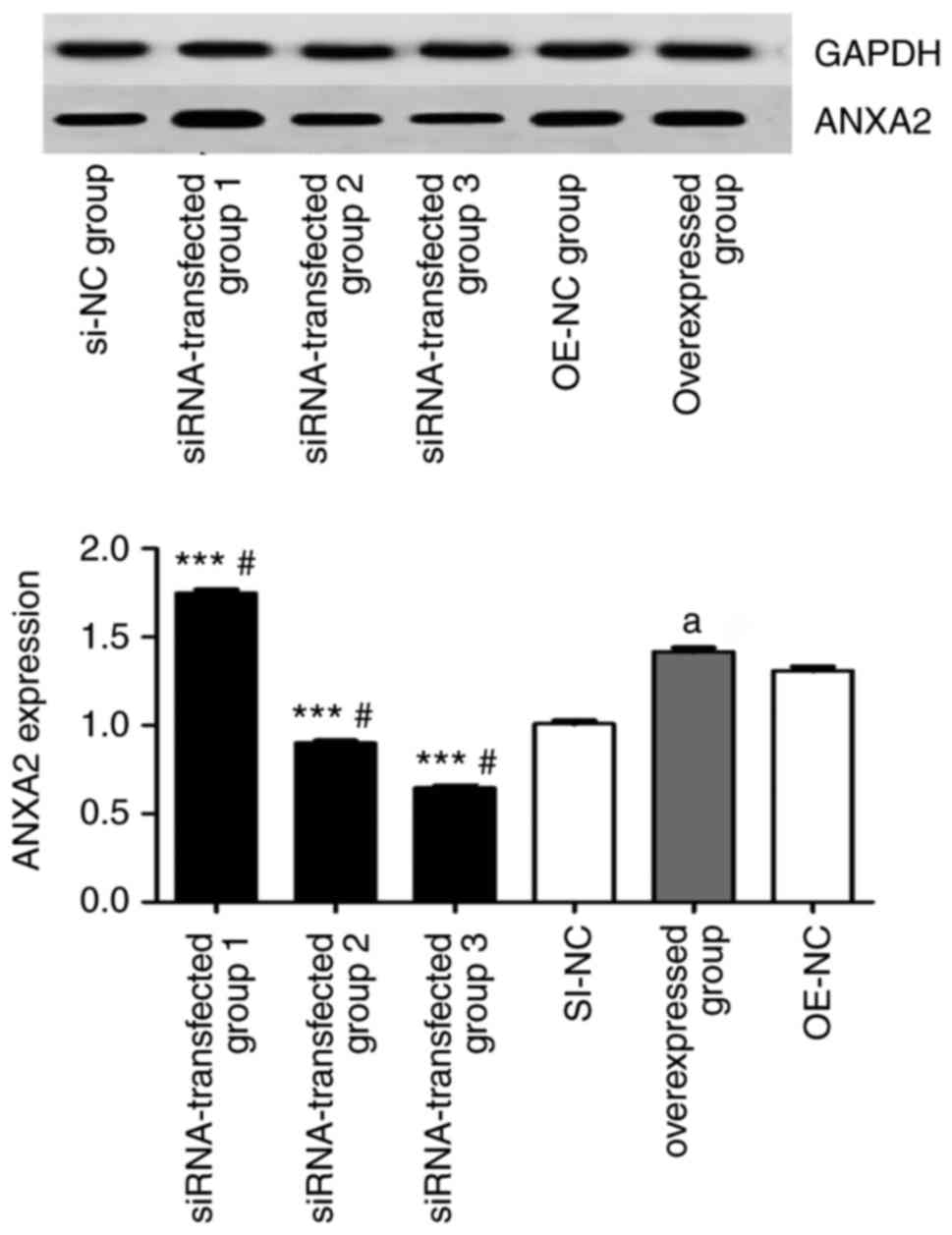
(Fig. 2). RT-qPCR results
revealed that in siRNA-transfected liver cells the expression
levels of ANXA2 and ANXA2P3 were markedly reduced compared with in
si-NC-transfected cells (Fig. 3A and
B). Conversely, in pcDNA3.1 plasmid vector-transfected liver
cells (OE-ANXA2 and OE-ANXA2P) the expression levels of ANXA2 and
ANXA2P3 were significantly increased compared with in the OE-NC
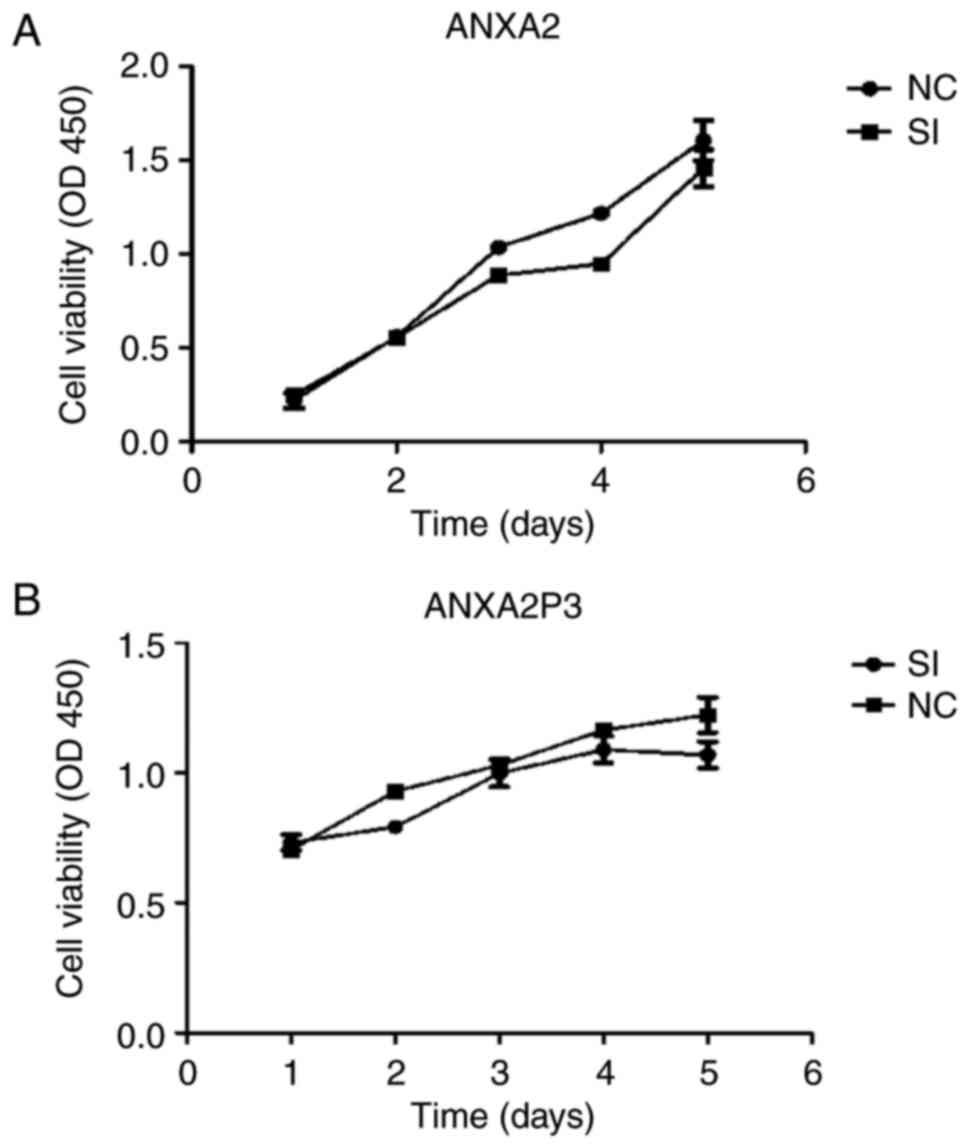
group (Fig. 3A and B). Using the
CCK-8 kit, it was revealed that knockdown of ANXA2P3 or ANXA2 in
liver cells inhibited cell proliferation; however, the results were
not significant (Fig. 4).
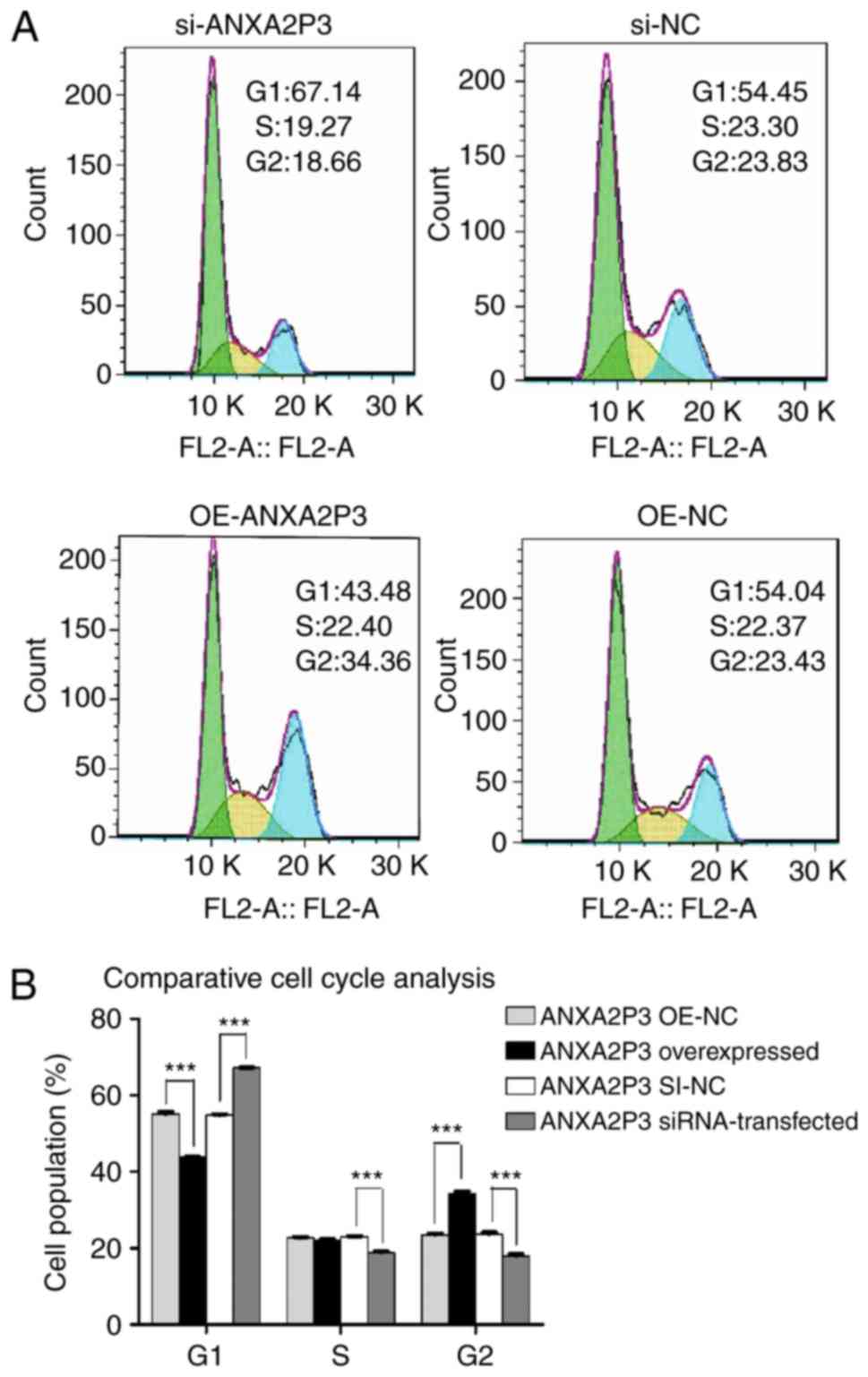
Using flow cytometry, it was revealed that
si-ANXA2P3-transfected liver cells were arrested in G1
phase compared with si-NC-transfected cells; conversely,
OE-ANXA2P3-transfected liver cells were arrested in G2
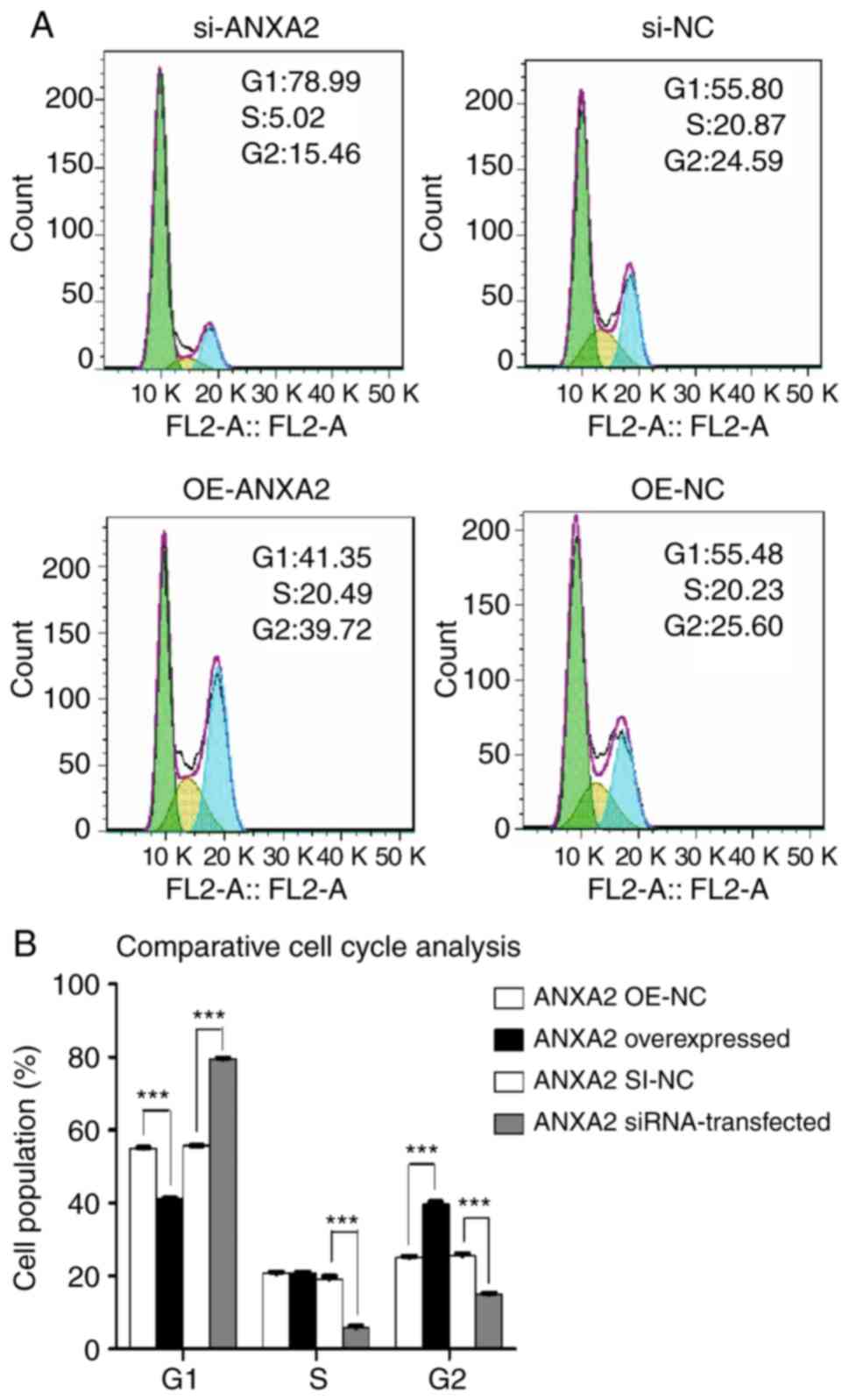
phase compared with OE-NC-transfected cells (Fig. 5). When compared with the si-NC
group, flow cytometric analysis of si-ANXA2-transfected liver cells
exhibited similar results as in the si-ANXA2P3 group; an increased
proportion of liver cells was arrested in G1 phase
compared with si-NC-transfected cells. Furthermore,
OE-ANXA2-transfected liver cells were arrested in G2
phase compared with OE-NC-transfected cells (Fig. 6). According to the results of flow
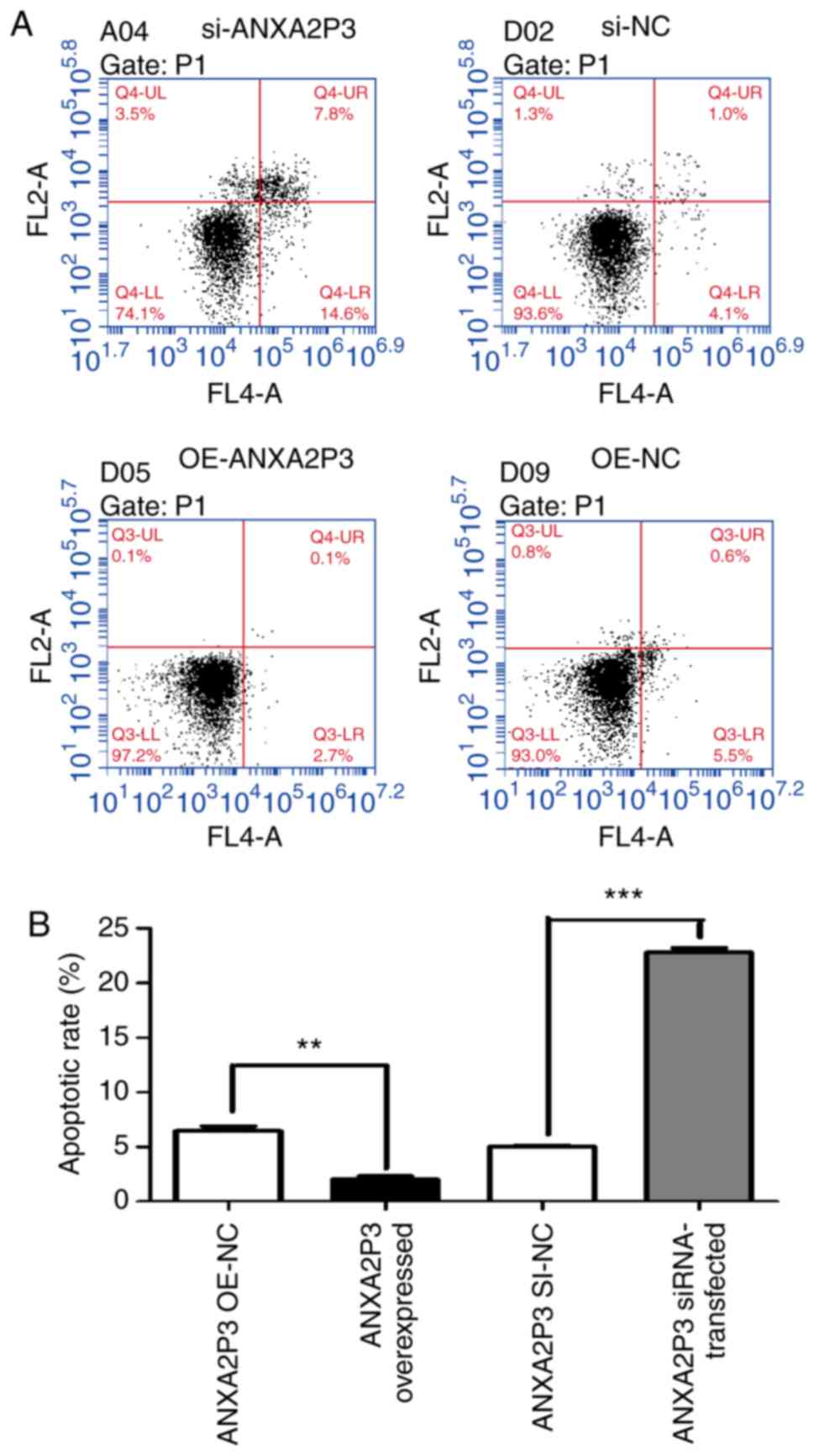
cytometric analysis, it was revealed that siANXA2P3-transfected
liver cells exhibited an increased apoptotic rate when compared
with the si-NC group, whereas opposite findings were detected in
the OE-ANXA2P3 group, in which the apoptotic rate was reduced
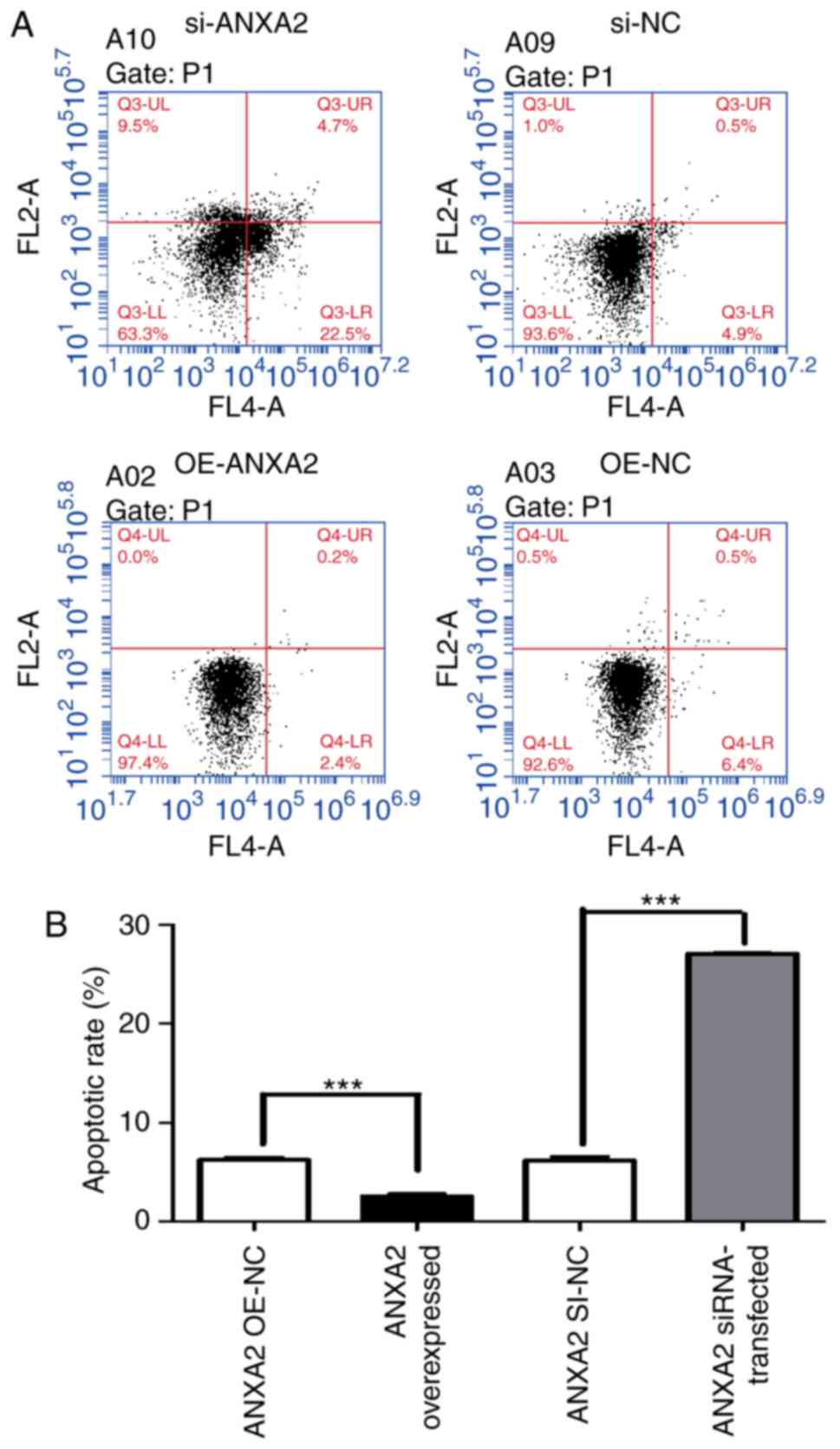
compared with in the OE-NC group (Fig. 7). Similarly, siANXA2-transfected
liver cells exhibited an increased apoptotic rate compared with the
si-NC group, whereas the OE-ANXA2 group exhibited a reduced
apoptotic rate compared with the OE-NC group (Fig. 8).
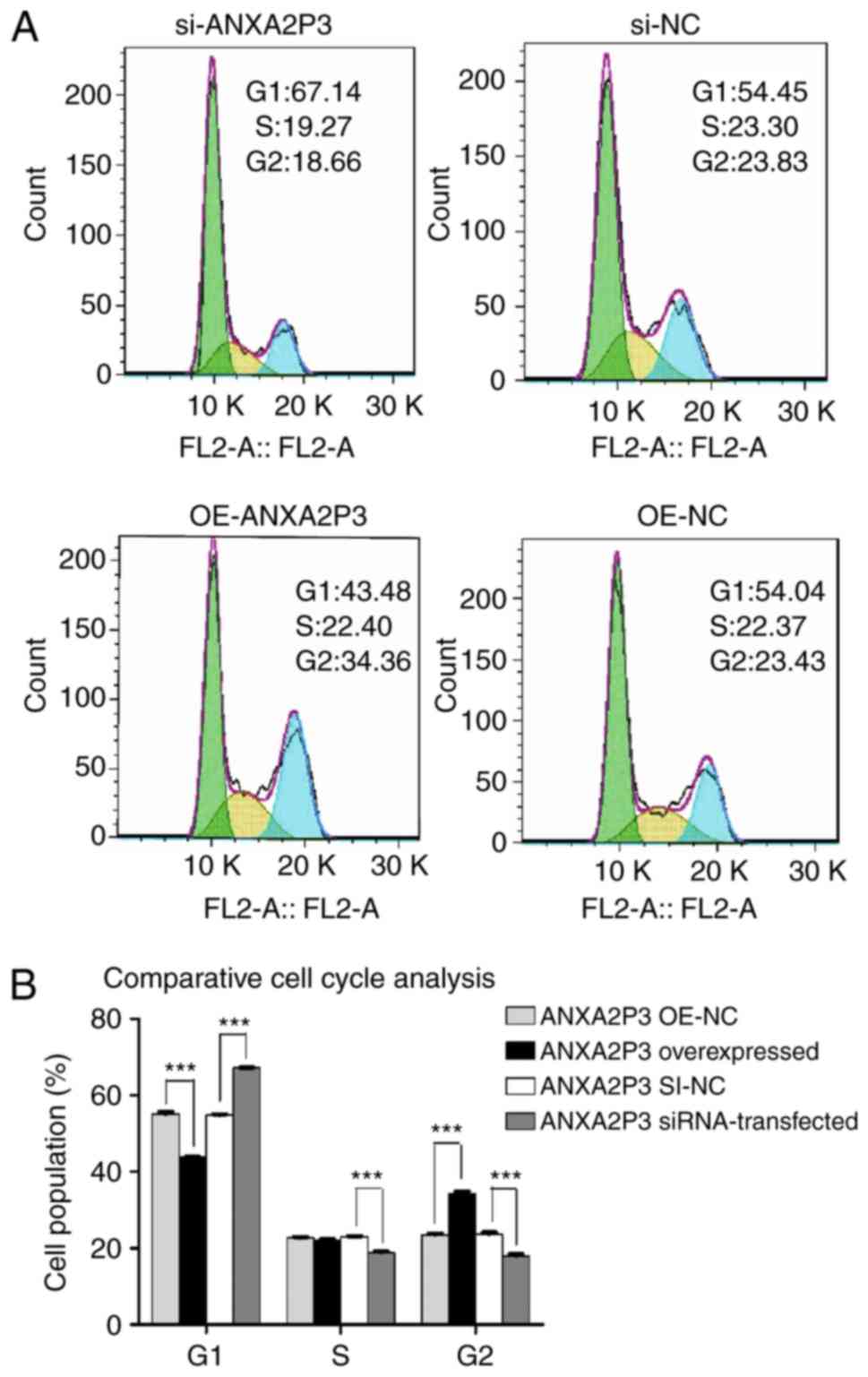 | Figure 5Results of flow cytometric analysis
of cell cycle progression. (A) si-ANXA2P3-transfected liver cells
exhibited cell cycle arrest in the G1 phase compared
with si-NC cells. si-ANXA2P3 group: 67.14% in G1 phase,
19.27% in S phase and 18.66% in G2 phase; si-NC group:
54.45, 23.3 and 23.83%, respectively. In the OE-ANXA2P3 group, the
percentage of cells in G1 phase, S phase and
G2 phase was 43.48, 22.40 and 34.36%, respectively.
Conversely, in the OE-NC group, the percentage of cells in
G1 phase, S phase and G2 phase was 54.04,
22.37 and 23.43%, respectively. (B) Summary of cell cycle
distribution in transfected liver cells. Data are presented as the
means ± standard deviation. P-values were obtained by Student’s
t-test. For all experiments, n=3. ***P<0.001.
ANXA2P3, Annexin A2 pseudogene 3; NC, negative control; OE,
overexpression; SI/siRNA, small interfering RNA. |
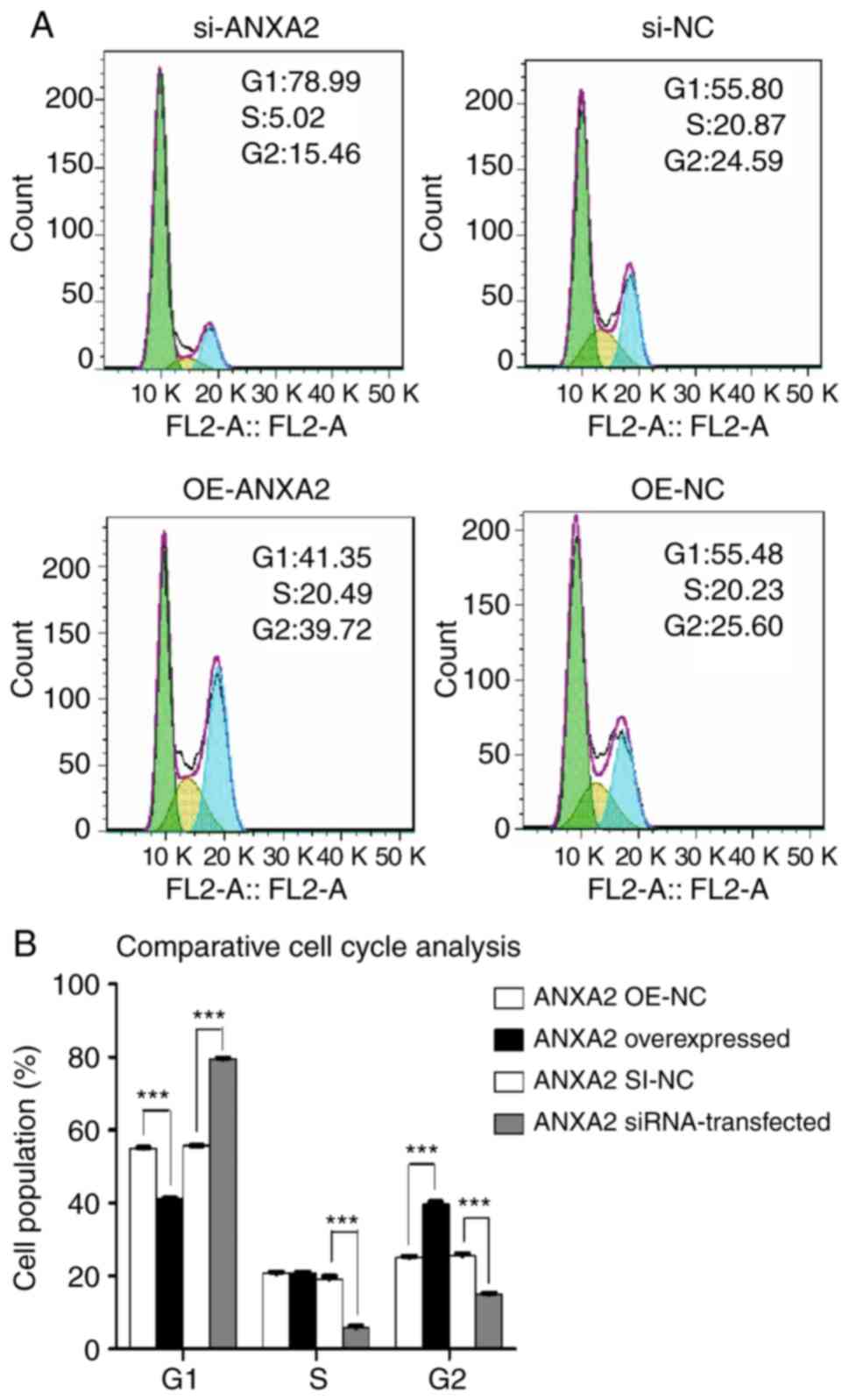 | Figure 6Results of flow cytometric analysis
of cell cycle progression. (A) Of the si-ANXA2-transfected human
liver cells, 78.99% were in G1 phase, 5.02% were in S
phase and 15.46% were in G2 phase. In the si-NC group,
55.80, 20.87 and 24.59% cells were in G1, S and
G2 phases, respectively. In the OE-ANXA2 group, the
percentage of cells in G1 phase, S phase and
G2 phase was 41.35, 20.49 and 39.72%, respectively.
Conversely, in the OE-NC group, the percentage of cells in
G1 phase, S phase and G2 phase was 55.48,
20.23 and 25.6%, respectively. (B) Summary of cell cycle
distribution in transfected liver cells. Data are presented as the
means ± standard deviation. P-values were obtained by Student’s
t-test. For all experiments, n=3. ***P<0.001. ANXA2,
Annexin A2; NC, negative control; OE, overexpression; SI/siRNA,
small interfering RNA. |
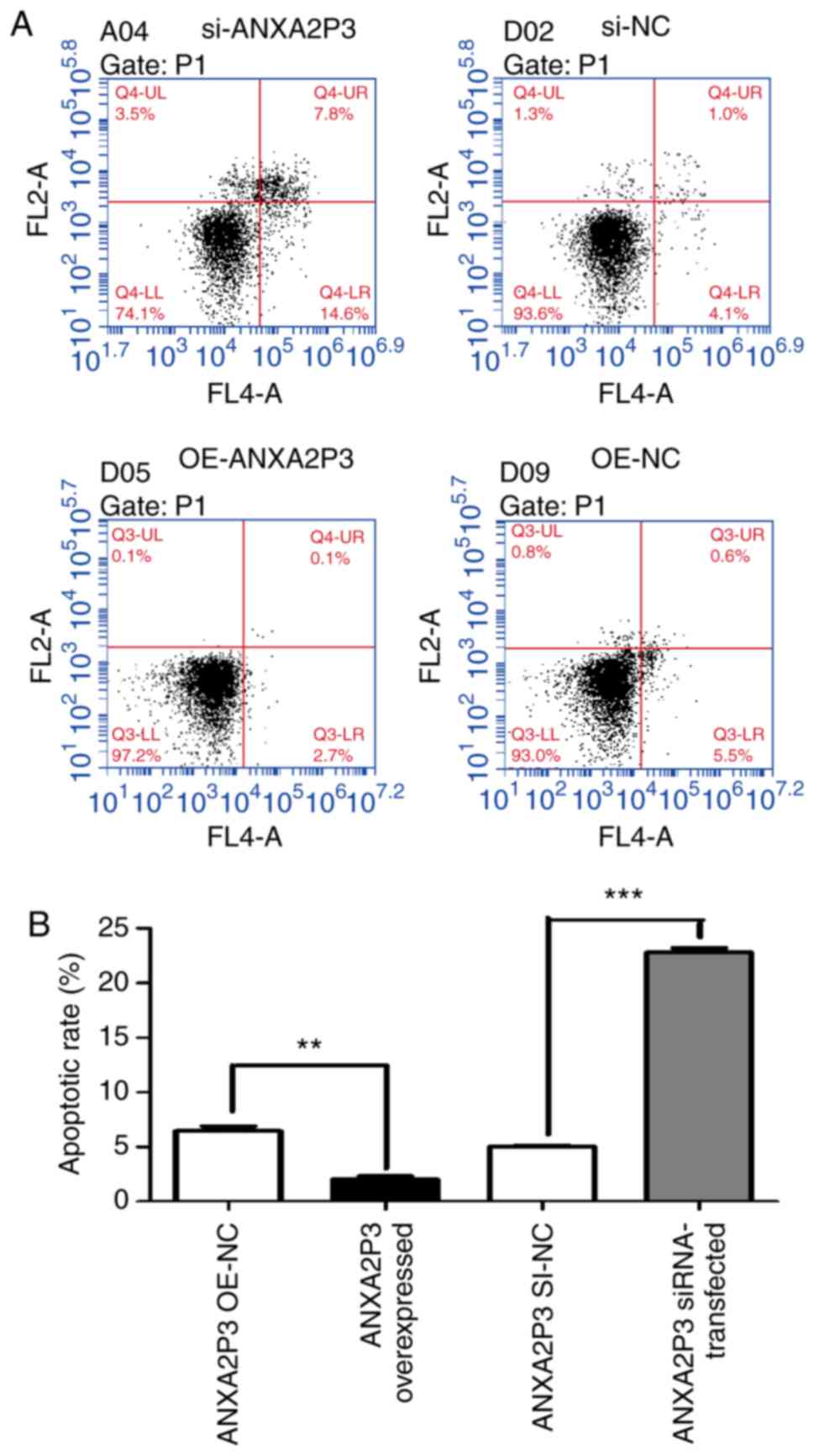 | Figure 7Results of flow cytometric analysis
of apoptosis. (A) Apoptotic rate of si-ANXA2P3-transfected liver
cells was increased compared with si-NC-transfected liver cells. In
the si-ANXA2P3 group, the values were as follows: Normal cells,
74.1%; early apoptotic cells, 14.6%; late apoptotic cells, 7.8%;
and necrotic cells, 3.5%. Conversely, in the si-NC group, the
values were as follows: Normal cells, 93.6%; early apoptotic cells,
4.1%; late apoptotic cells, 1.0%; and necrotic cells, 1.3%. In the
OE-ANXA2P3 group, the values were as follows: Normal cells, 97.2%;
early apoptotic cells, 2.7%; late apoptotic cells, 0.1%; and
necrotic cells, 0.1%. Conversely, in the OE-NC group, the values
were as follows: Normal cells, 93.0%; early apoptotic cells, 5.5%;
late apoptotic cells, 0.6%; and necrotic cells and 0.8%. (B)
Summary of cell apoptotic rates. Cells in the upper right quadrant
are late apoptotic cells and cells in the lower right quadrant are
early apoptotic cells. The total apoptotic rate of cells is the sum
of the apoptotic rates of the upper right and lower right
quadrants. Data are presented as the means ± standard deviation.
P-values were obtained by Student’s t-test. For all experiments,
n=3. **P<0.01, ***P<0.001. ANXA2P3,
Annexin A2 pseudogene 3; NC, negative control; OE, overexpression;
si/siRNA, small interfering RNA. |
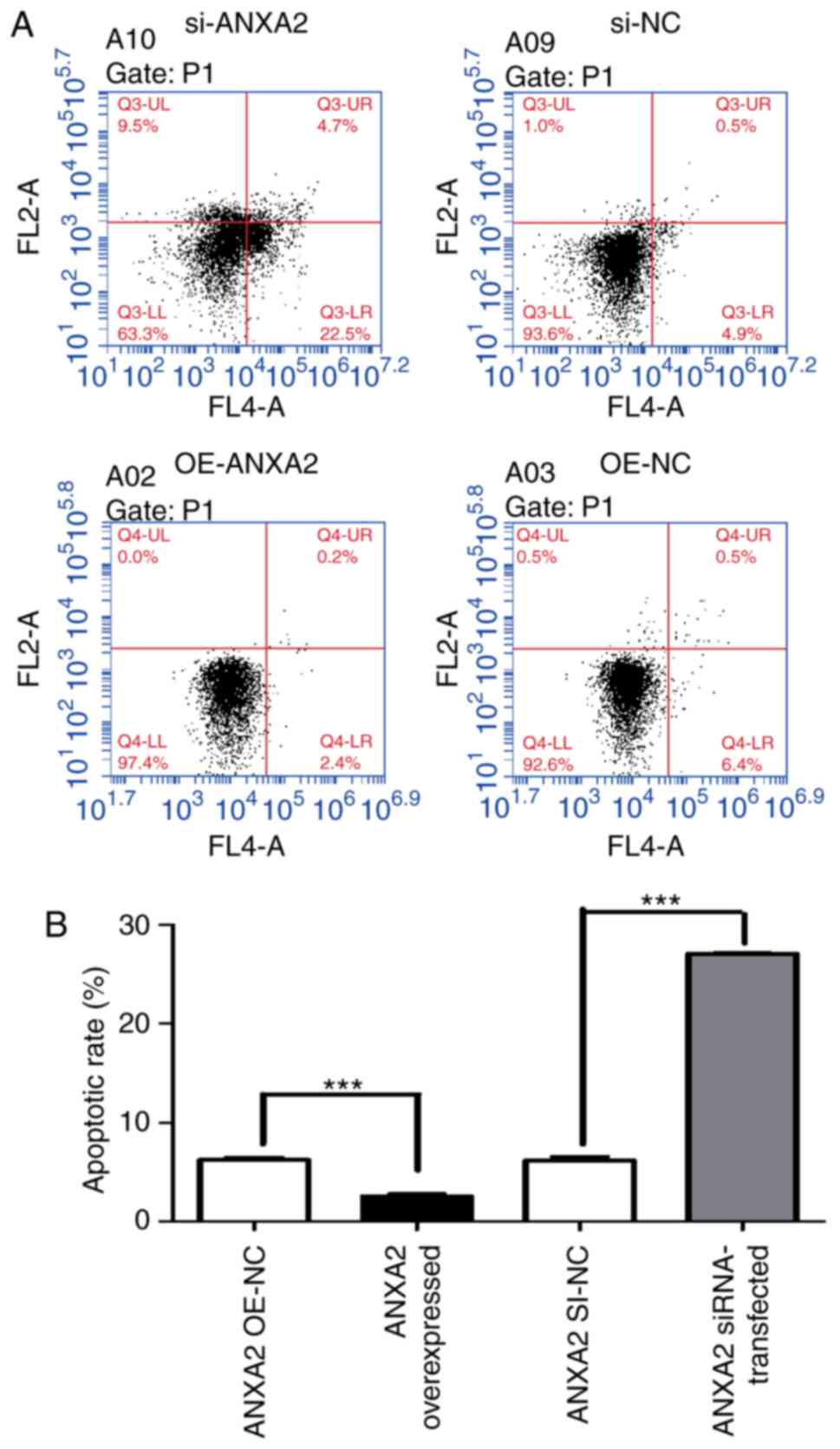 | Figure 8Results of flow cytometric analysis
of apoptosis. (A) si-ANXA2- transfected liver cells exhibited a
higher apoptotic rate compared with si-NC-transfected liver cells.
The values for the si-ANXA2 group were as follows: Normal cells,
63.3%; early apoptotic cells, 22.5%; late apoptotic cells, 4.7%;
and necrotic cells 9.5%. In the si-NC group, the values were as
follows: Normal cells, 93.6%; early apoptotic cells, 4.9%; late
apoptotic cells, 0.5%; and necrotic cells, 1.0%. In the OE-ANXA2
group, the values were as follows: Normal cells, 97.4%; early
apoptotic cells, 2.4%; late apoptotic cells, 0.2%; and necrotic
cells, 0.0%. Conversely, in the OE-NC group, the values were as
follows: Normal cells, 92.6%; early apoptotic cells, 6.4%; late
apoptotic cells, 0.5%; and necrotic cells, 0.5%. (B) Summary of
cell apoptotic rates. Cells in the upper right quadrant are late
apoptotic cells and cells in the lower right quadrant are early
apoptotic cells. The total apoptotic rate of cells is the sum of
the apoptotic rates of the upper right and lower right quadrants
Data are presented as the means ± standard deviation. P-values were
obtained by Student’s t-test. For all experiments, n=3.
***P<0.001. ANXA2, Annexin A2; NC, negative control;
OE, overexpression; si/siRNA, small interfering RNA. |
These in vitro findings suggested that
overexpression of ANXA2 and ANXA2P3 may induce a more active liver
cell phenotype. Conversely, inhibition of ANXA2 and ANXA2P3 may
result in more negative consequences towards normal liver
cells.
ANXA2P3 may activate ANXA2/ANXA2P3
signaling in liver cells
Western blot analysis revealed that knockdown of
ANXA2P3 expression using si-ANXA2P3-2 and si-ANXA2P3-3 inhibited
the protein expression levels of ANXA2 in vitro. Conversely,
si-ANXA2P3-1 increased ANXA2 expression, which may be due to its
reduced ANXA2P3 knockdown efficiency. Overexpression of ANXA2P3
markedly increased ANXA2 expression in vitro (Fig. 9). Taken together, these findings
indicated that ANXA2P3 may affect the activity of the ANXA2/ANXA2P3
pathway in human liver cells in vitro.
Discussion
LncRNAs are mRNA-like transcripts >200
nucleotides in length that lack protein-coding functions (32). In recent decades, overwhelming
evidence has indicated that lncRNAs are implicated in a wide range
of biological functions, including cell proliferation, apoptosis
and metastasis (33,34). The association between lncRNA
dysregulation and the development of fibrosis is considered a major
focus of hepatology studies. The present study aimed to detect
ANXA2 and ANXA2P3 expression in clinical samples and to investigate
their effects on liver cells in vitro.
Aberrant activation of the canonical ANXA2P3/ANXA2
signaling pathway is often observed during the initiation and
progression of liver fibrosis. In previous liver fibrosis studies,
the expression of ANXA2 was revealed to be positively correlated
with ANXA2P3 (26,27). Therefore, it was hypothesized that
an ANXA2P3/ANXA2 signaling pathway exists, which may serve an
important role in the process of BA-induced liver injury, which is
characterized by liver fibrosis. According to a previous study
regarding the functions of pseudogenes (35), it was suggested that abnormal
expression of ANXA2P3 may influence the ANXA2P3/ANXA2 signaling
pathway. In addition, the present study revealed that
downregulation of ANXA2P3 in liver cells, using si-ANXA2P3-2 and
si-ANXA2P3-3, resulted in suppression of the ANXA2P3/ANXA2
signaling pathway. Since there is a close association between these
genes, functional analyses of both ANXA2P3 and ANXA2 were
conducted.
The present study identified the role of the ANXA2
and ANXA2P3 in BA-induced liver injury, which is characterized by
liver fibrosis. The results revealed that the expression levels of
ANXA2 and ANXA2P3 were significantly elevated in tissues derived
from patients with BA when compared with in paracarcinoma liver
tissues from patients with hepatoblastoma. These findings indicated
that upregulation of ANXA2P3 and ANXA2 may be positively associated
with the characteristics of liver injury. Since aberrant cell
proliferation and dysregulated cell cycle progression are two main
features of fibrosis-associated liver injury, further in
vitro mechanistic experiments were conducted. Previous studies
reported that ANXA2 is closely associated with cell proliferation
and cell cycle progression, although the cells used in these
studies differ (23,24,36). In the present in vitro
mechanistic studies, it was revealed that knockdown of ANXA2 and
ANXA2P3 reduced cell proliferation and promoted cell apoptosis.
Furthermore, overexpression of ANXA2 and ANXA2P3 accelerated cell
cycle progression and slightly inhibited cell apoptosis. Therefore,
ANXA2 and ANXA2P3 expression may have promising effects on liver
cell cycle progression and cell proliferation. To the best of our
knowledge, the present study is the first to report the biological
function of ANXA2 and ANXA2P3 in liver cells, which contributes
toward improving the understanding of the mechanisms underlying
liver injury progression and development. The present study
indicated that, according to flow cytometry and cell cycle
progression analysis, overexpression of ANXA2 and ANXA2P3 reduced
cell apoptosis rates and induced cell cycle arrest in G2
phase; therefore, ANXA2 and ANXA2P3 may serve a protective role in
the process of liver injury. In addition, the expression levels of
ANXA2 and ANXA2P3 were significantly increased in patients with BA;
all of these patients suffered from liver injury caused by liver
fibrosis, as demonstrated by Masson staining. Therefore, it may be
hypothesized that these genes are upregulated in order to exert
protective effects and to hinder the process of liver injury, thus
reversing the negative consequences of injury. However, the
specific details and underlying mechanism of action require further
elucidation.
Although the results of this study are promising,
there are two potential limitations. Firstly, the clinical study
involved retrospective validation, and the cohort of patients was
with BA relatively small. Secondly, although the possible
association between ANXA2P3 and ANXA2P3/ANXA2 signaling was
revealed in liver cell lines, the underlying mechanisms by which
ANXA2P3 exerts protective effects against liver injury remains to
be elucidated.
In conclusion, to the best of our knowledge, the
present study is the first to reveal that the expression levels of
ANXA2P3 and ANXA2 are increased in the liver tissue of patients
with BA, and their association with liver injury. ANXA2P3
expression may influence the biological behavior of liver cells
through activation of ANXA2. In addition, the expression of both
genes had a positive effect on cell proliferation and inhibited
cell apoptosis. These findings suggested that ANXA2P3 and ANXA2 may
be considered novel molecular targets for the prognosis and
treatment of liver injury. However, a further investigation with a
larger sample size is required to support these results.
Funding
The present study received financial support from
the Shanghai Key Disciplines (grant no. 2017ZZ02022), the National
Natural Science Foundation of China (grant nos. 81770519 and
81771633) and the Shanghai Natural Science Foundation (grant no.
17ZR1403000).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors’ contributions
YN carried out the experiments and wrote the
manuscript, with support from ZS and SZ. RD contributed to sample
preparation, performed the calculations and designed the figures.
ZS and SZ helped supervise the project and conceived the original
idea. All authors discussed the results and contributed to the
final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethical Review
Board of Fudan University Children’s Hospital, and written informed
consent was obtained from the parents of all participants
enrolled.
Patient consent for publication
Written informed consent for publication of the data
was obtained from the participant and the patient’s family,
according to federal and institutional guidelines.
Competing interests
The authors declare that they have no competing
interests.
Acknowledgments
Not applicable.
References
|
1
|
Asai A, Miethke A and Bezerra JA:
Pathogenesis of biliary atresia: Defining biology to understand
clinical phenotypes. Nat Rev Gastroenterol Hepatol. 12:342–352.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dehghani SM, Efazati N, Shahramian I,
Haghighat M and Imanieh MH: Evaluation of cholestasis in Iranian
infants less than three months of age. Gastroenterol Hepatol Bed
Bench. 8:42–48. 2015.PubMed/NCBI
|
|
3
|
Hoerning A, Raub S, Dechêne A, Brosch MN,
Kathemann S, Hoyer PF and Gerner P: Diversity of disorders causing
neonatal cholestasis-the experience of a tertiary pediatric center
in Germany. Front Pediatr. 2:652014. View Article : Google Scholar
|
|
4
|
Lishuang M, Zhen C, Guoliang Q, Zhen Z,
Chen W, Long L and Shuli L: Laparoscopic portoenterostomy versus
open portoenterostomy for the treatment of biliary atresia: A
systematic review and meta-analysis of comparative studies. Pediatr
Surg Int. 31:261–269. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Venter JC, Adams MD, Myers EW, Li PW,
Mural RJ, Sutton GG, Smith HO, Yandell M, Evans CA, Holt RA, et al:
The sequence of the human genome. Science. 291:1304–1351. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yang Y, Wen L and Zhu H: Unveiling the
hidden function of long non-coding RNA by identifying its major
partner-protein. Cell Biosci. 5:592015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wilczynska A and Bushell M: The complexity
of miRNA-mediated repression. Cell Death Differ. 22:22–33. 2015.
View Article : Google Scholar
|
|
8
|
Fang XY, Pan HF, Leng RX and Ye DQ: Long
noncoding RNAs: Novel insights into gastric cancer. Cancer Lett.
356:357–366. 2015. View Article : Google Scholar
|
|
9
|
Chen Z, Luo Y, Yang W, Ding L, Wang J, Tu
J, Geng B, Cui Q and Yang J: Comparison analysis of dysregulated
LncRNA profile in mouse plasma and liver after hepatic
ischemia/reperfusion injury. PLoS One. 10:e01334622015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
He Y, Wu YT, Huang C, Meng XM, Ma TT, Wu
BM, Xu FY, Zhang L, Lv XW and Li J: Inhibitory effects of long
noncoding RNA MEG3 on hepatic stellate cells activation and liver
fibro-genesis. Biochim Biophys Acta. 1842:2204–2215. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Qiao J, Yao H, Xia Y, Chu P, Li M, Wu Y,
Li W, Ding L, Qi K, Li D, et al: Long non-coding RNAs expression
profiles in hepatocytes of mice after hematopoietic stem cell
transplantation. IUBMB Life. 68:232–241. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Su S, Liu J, He K, Zhang M, Feng C, Peng
F, Li B and Xia X: Overexpression of the long noncoding RNA TUG1
protects against cold-induced injury of mouse livers by inhibiting
apoptosis and inflammation. FEBS J. 283:1261–1274. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liu H, Song G, Zhou L, Hu X, Liu M, Nie J,
Lu S, Wu X, Cao Y, Tao L, et al: Compared analysis of LncRNA
expression profiling in pdk1 gene knockout mice at two time points.
Cell Physiol Biochem. 32:1497–1508. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xu D, Yang F, Yuan JH, Zhang L, Bi HS,
Zhou CC, Liu F, Wang F and Sun SH: Long noncoding RNAs associated
with liver regeneration 1 accelerates hepatocyte proliferation
during liver regeneration by activating Wnt/beta-catenin signaling.
Hepatology. 58:739–751. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Groen JN, Capraro D and Morris KV: The
emerging role of pseudogene expressed non-coding RNAs in cellular
functions. Int J Biochem Cell Biol. 54:350–355. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Piehler AP, Hellum M, Wenzel JJ, Kaminski
E, Haug KB, Kierulf P and Kaminski WE: The human ABC transporter
pseudogene family: Evidence for transcription and gene-pseudogene
interference. BMC Genomics. 9:1652008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lin H, Shabbir A, Molnar M and Lee T: Stem
cell regulatory function mediated by expression of a novel mouse
Oct4 pseudogene. Biochem Biophys Res Commun. 355:111–116. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Karreth FA, Reschke M, Ruocco A, Ng C,
Chapuy B, Léopold V, Sjoberg M, Keane TM, Verma A, Ala U, et al:
The BRAF pseudogene functions as a competitive endogenous RNA and
induces lymphoma in vivo. Cell. 161:319–332. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li S, Zou H, Shao YY, Mei Y, Cheng Y, Hu
DL, Tan ZR and Zhou HH: Pseudogenes of annexin A2, novel prognosis
biomarkers for diffuse gliomas. Oncotarget. 8:106962–106975.
2017.
|
|
20
|
Pan BL, Tong ZW, Wu L, Pan L, Li JE, Huang
YG, Li SD, Du SX and Li XD: Effects of MicroRNA-206 on osteosarcoma
cell proliferation, apoptosis, migration and invasion by targeting
ANXA2 through the AKT signaling pathway. Cell Physiol Biochem.
45:1410–1422. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pérez-Sánchez G, Jiménez A,
Quezada-Ramírez MA, Estudillo E, Ayala-Sarmiento AE,
Mendoza-Hernández G, Hernández-Soto J, Hernández-Hernández FC,
Cázares-Raga FE and Segovia J: Annexin A1, Annexin A2, and Dyrk 1B
are upregulated during GAS1-induced cell cycle arrest. J Cell
Physiol. 233:4166–4182. 2018. View Article : Google Scholar
|
|
22
|
Chen J, Cui Z, Yang S, Wu C, Li W, Bao G,
Xu G, Sun Y, Wang L and Zhang J: The upregulation of annexin A2
after spinal cord injury in rats may have implication for astrocyte
proliferation. Neuropeptides. 61:67–76. 2017. View Article : Google Scholar
|
|
23
|
Stewart AG, Xia YC, Harris T, Royce S,
Hamilton JA and Schuliga M: Plasminogen-stimulated airway smooth
muscle cell proliferation is mediated by urokinase and annexin A2,
involving plasmin-activated cell signalling. Br J Pharmacol.
170:1421–1435. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dong Z, Yao M, Zhang H, Wang L, Huang H,
Yan M, Wu W and Yao D: Inhibition of Annexin A2 gene transcription
is a promising molecular target for hepatoma cell proliferation and
metastasis. Oncol Lett. 7:28–34. 2014. View Article : Google Scholar
|
|
25
|
Jiang SL, Pan DY, Gu C, Qin HF and Zhao
SH: Annexin A2 silencing enhances apoptosis of human umbilical vein
endothelial cells in vitro. Asian Pac J Trop Med. 8:952–957. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kolgelier S, Demir NA, Inkaya AC, Sumer S,
Ozcimen S, Demir LS, Pehlivan FS, Arslan M and Arpaci A: Serum
levels of Annexin A2 as a candidate biomarker for hepatic fibrosis
in patients with chronic hepatitis B. Hepat Mon. 15:e306552015.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang L, Peng X, Zhang Z, Feng Y, Jia X,
Shi Y, Yang H, Zhang Z, Zhang X, Liu L, et al: Subcellular proteome
analysis unraveled annexin A2 related to immune liver fibrosis. J
Cell Biochem. 110:219–228. 2010.PubMed/NCBI
|
|
28
|
Yang M, Wang C, Li S, Xv X, She S, Ran X,
Li S, Hu H, Hu P, Zhang D, et al: Annexin A2 promotes liver
fibrosis by mediating von Willebrand factor secretion. Dig Liver
Dis. 49:780–788. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dadhania VP, Muskhelishvili L, Latendresse
JR and Mehendale HM: Hepatic overexpression of Annexin A1 and A2 in
thioacetamide-primed mice protects them against
acetaminophen-induced liver failure and death. Int J Toxicol.
35:654–665. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
31
|
Weerasooriya VS, White FV and Shepherd RW:
Hepatic fibrosis and survival in biliary atresia. J Pediatr.
144:123–125. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Blythe AJ, Fox AH and Bond CS: The ins and
outs of lncRNA structure: How, why and what comes next. Biochim
Biophys Acta. 1859:46–58. 2016. View Article : Google Scholar
|
|
33
|
Liz J and Esteller M: lncRNAs and
microRNAs with a role in cancer development. Biochim Biophys Acta.
1859:169–176. 2016. View Article : Google Scholar
|
|
34
|
Zhang H, Chen Z, Wang X, Huang Z, He Z and
Chen Y: Long non-coding RNA: A new player in cancer. J Hematol
Oncol. 6:372013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Pink RC and Carter DR: Pseudogenes as
regulators of biological function. Essays Biochem. 54:103–112.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhou X, Deng S, Liu H, Liu Y, Yang Z, Xing
T, Jing B and Zhang X: Knockdown of ubiquitin protein ligase E3A
affects proliferation and invasion, and induces apoptosis of breast
cancer cells through regulation of annexin A2. Mol Med Rep.
12:1107–1113. 2015. View Article : Google Scholar : PubMed/NCBI
|