Introduction
Psoriasis is a chronic autoimmune inflammatory
disease with epidermal hyperkeratosis and parakeratosis, and its
prevalence rate ranges between 0.09 and 5.1% globally, with the
highest prevalence rate of 5.1% reported in the USA in 2017
(1). The clinical epidemiological
characteristics of psoriasis may vary in different regions and
populations. The prevalence of psoriasis in China was revealed to
be 0.123%, and had grown to 0.47% according to a community-based
survey conducted in six cities from six provinces in 2010 (2). The pathogenesis of psoriasis is
complex, and there are multiple risk factors including smoking,
excessive alcohol intake, hypertension, hyperlipidemia, obesity and
insulin resistance, which are in turn associated with
cardiovascular disease (3). The
majority of inflammatory cytokines, including tumor necrosis factor
(TNF)-α and interferon-γ (IFN-γ), in psoriasis lesions and immune
cells, including T helper cell type 1 (Th1) and Th17 in
circulation, are increased in patients with psoriasis (4). A previous study demonstrated that
psoriasis is associated with numerous types of comorbidities
including metabolic syndrome (MS), diabetes, depression and cancer
(5), thereby suggesting that
psoriasis is an inflammatory and metabolic disease.
The sirtuin (SIRT) family, consisting of seven
members (SIRT1-7), are a conserved superfamily of nicotinamide
adenine dinucleotide+-dependent deacetylases that are
involved in the regulation of energy metabolism, aging, cell
apoptosis, gene transcription, tumor development, autoimmune
inflammation and epigenetics (6).
SIRTs serve notable functions in metabolic and inflammatory
processes. Associations between pathogenetic pathways and the
localizations of SIRT have been reported. The proteins of SIRT1,
SIRT6 and SIRT7 are localized in the nucleus, those of SIRT3, SIRT4
and SIRT5 in the mitochondria, and those of SIRT2 in the cytoplasm
and/or nucleus (7). SIRT1 is able
to regulate inflammation-associated signaling pathways, and inhibit
mitochondrial reactive oxygen species (ROS), oxidative stress,
mitochondrial DNA mutations and mitochondrial damage to in turn
inhibit pancreatic β-islet cell injury, and subsequently inhibit
the occurrence of diabetes mellitus, obesity, insulin resistance
and fatty liver disease (8-10).
SIRT1, SIRT2 and SIRT6 affect metabolism and longevity by
regulating the nuclear factor-κB (NF-κB) signaling pathways and
fatty acid β-oxidation (11,12). SIRT3 is able to inhibit
proliferation capacity, promote fatty acid β-oxidation and activate
the key enzymes of the electron transport chain and the urea cycle
(13). SIRT4 and SIRT5 are able
to activate the pyruvate dehydrogenase complex (PDH), succinate
dehydrogenase and the glutamate dehydrogenase complex (GDH) to
regulate metabolism (14). SIRT7
serves a function in regulating the release of inflammatory
cytokines, avoiding DNA damage repair, adapting to environmental
challenges and cell survival (15).
Altogether, these studies imply that SIRTs may link
metabolism and inflammatory signaling. Furthermore, there have been
a number of previous studies (16,17) that have investigated the
association between SIRT1, SIRT6 and psoriasis, but to the best of
our knowledge the present study is the first to investigate the
altered expression of SIRT genes in psoriasis.
Materials and methods
Cell cultures
HaCaT, the human keratinocyte cell line, purchased
from Jiangsu KeyGEN BioTECH Corp., Ltd. (Jiangsu, China), which was
grown in the Central Laboratory of Shanghai Sixth People's Hospital
Affiliated to Shanghai Jiaotong University (Shanghai, China), and
cultured in Dulbecco's modified Eagle's medium (HyClone; GE
Healthcare Life Sciences, Logan, UT, USA) supplemented with 10%
heat inactivated fetal bovine serum (Gibco; Thermo Fisher
Scientific, Inc., Waltham, MA, USA). All cells were maintained in a
humidified incubator at 37°C with 5% CO2.
TNF-α-stimulated HaCaT cell model
A number of previous studies had exposed HaCaT cells
to 20 ng/ml TNF-α for 24 h and reported that TNF-α serves a notable
function in the pathogenesis of psoriasis (18,19). In the present study, a TNF-α (cat.
no. H8916; Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany)-stimulated HaCaT cell model was used to simulate the
environment of keratinocytes in psoriasis. Then, cell viability was
assessed using a Cell Counting Kit-8 assay (Beyotime Institute of
Biotechnology, Haimen, China) according to the manufacturer's
protocol. HaCaT cells were seeded into 96-well plates
(4x103 cells per well) and treated with TNF-α (20 ng/ml)
in culture medium without serum for 0, 4, 8, 12, 24 and 36 h at
37°C. Absorbance was assessed at 450 nm with a microplate reader
(Omega Bio-Tek, Inc., Norcross, GA, USA). Cells were divided into
the following three groups: Treatment, control and blank groups.
The control group contained no TNF-α, and the blank group contained
no TNF-α and HaCaT cells. Other experimental conditions were the
same as the treatment group. The most suitable induction time point
was determined to be the time point that induced evident changes in
cell morphology and relatively greater cell proliferation compared
with the control group. The mean optical density (OD) of three
wells in each group were used to calculate the percentage of cell
proliferation as follows: Cell proliferation (%) =
[(ODtreatment −
ODblank)/(ODcontrol − ODblank)]
×100.
Immunofluorescence (IF) examinations
IF staining was performed to assess the expression
levels and patterns of the SIRT family of proteins in cells. First,
HaCaT cells (2×104 cells/well) were inoculated into
24-well culture plates in which sterile coverslips were placed in
advance, until the cells were close to forming a monolayer. The
coverslips were then removed, and cells were washed twice with PBS.
Following 24 h, cells were treated with 4% paraformaldehyde for 15
min at room temperature and 0.1% Triton X-100 for 25 min at room
temperature. The cells were subsequently blocked with 5% bull serum
albumin (BSA; Bovogen Biologicals Pty., Ltd., Melbourne, VIC,
Australia) for 1 h at room temperature. Cultured HaCaT cells were
incubated with the following specific antibodies overnight at 4°C:
SIRT1 (1:50; cat. no. 13161-1-AP; ProteinTech Group, Inc., Chicago,
IL, USA), SIRT2 (1:100; cat. no. PB0174; Wuhan Boster Biological
Technology, Ltd., Wuhan, China), SIRT3 (1:100; cat. no. A01061-1;
Wuhan Boster Biological Technology, Ltd.), SIRT4 (1:100; cat. no.
ab10140; Abcam, Cambridge, MA, USA), SIRT5 (1:100; cat. no.
15122-1-AP; ProteinTech Group, Inc.), SIRT6 (1:100; cat. no.
PB0375; Wuhan Boster Biological Technology, Ltd.) and SIRT7 (1:100
cat. no. PB0376; Wuhan Boster Biological Technology, Ltd.). On the
following day, cells were incubated for 1 h at 37°C with secondary
antibodies: Donkey anti-rabbit immunoglobulin G (IgG; Alexa Fluor
488; 1:500; cat. no. ab150073; Abcam) was used to label SIRT1,
SIRT2, SIRT3, SIRT5, SIRT6 and SIRT7, and fluorescein
isothiocyanate (FITC)-conjugated donkey anti-goat IgG heavy and
light chain (H+L; 1:50; cat. no. GB22404; Wuhan Servicebio
Technology Co., Ltd., Wuhan, China) was used to label SIRT4.
Stained cells were counterstained with DAPI for ~10 min at room
temperature and visualized using an inverted fluorescence
microscope (Olympus Corporation, Tokyo, Japan; magnification,
×400).
Animal model
All animal experiments were performed in accordance
with the National Institutes of Health Guidelines on Laboratory
Research (20) and ethically
approved by the Animal Welfare Committees of Shanghai Sixth
People's Hospital (Shanghai, China). The Animal Experiment
Registration number was no. DWLL2017-0312. All eight mice were
obtained from the Animal Experiment Center at Shanghai Sixth
People's Hospital and bred in specific pathogen-free colony. All
mice were housed at 40% humidity at 25°C, with a 16 h light/8 h
dark cycle. All mice had free access to sterile water and sterile
food. Imiquimod (IMQ)-induced skin inflammation in mice resembles
psoriasis phenotypically and is a well-established technique
(20,21). BALB/c female mice (age 6-8 weeks,
weight 19±4 g) were used for the present study. Mice of the same
sex were selected to avoid self-reproduction subsequent to group
establishment and to provide a stable external environment.
Experimental mice received a daily topical dose of 62.5 mg of 5%
IMQ cream (cat. no. H20030128; Sichuan Med-Shine Pharmaceutical
Co., Ltd., Sichuan, China) on a 2×2 cm shaved area on their back
for 7 consecutive days. Control mice were treated similarly with
normal saline as a control treatment. To score the severity of
inflammation on the skin of mouse backs, an objective scoring
system was developed based on the clinical psoriasis area and
severity index (PASI) (20),
consisting of measures of skin erythema, thickness and scales. Each
parameter was scored from 0 to 4, where scores 0, 1, 2, 3 and 4
referred to no clinical signs, slight clinical signs, moderate
clinical signs, marked clinical signs and very marked clinical
signs, respectively. The cumulative score denotes the severity of
inflammation. At the end of the experiment on day 7, all mice were
sacrificed by cervical dislocation and skin samples were collected
within 2 h for additional experiments.
Clinical samples
The present study was performed once the patients'
written informed consent was obtained by the Department of
Dermatology, Shanghai Sixth People's Hospital, and was ethically
approved by the Ethics Committee of Shanghai Sixth People's
Hospital (approval no. 2018-029). Based on age and sex, a total of
22 clinical psoriasis and 22 normal specimens were divided into two
groups. In addition, the condition of each patient with psoriasis
was evaluated using the PASI. The inclusion criteria for the
psoriasis group were as follows: i) No restrictions on sex and age;
ii) psoriasis vulgaris: Scales on the basis of the erythema of the
whole body-wax dripping phenomenon, translucent film following
scaling-film phenomenon, and puncture hemorrhage following scraping
the film, Auspitz phenomenon; iii) pathological diagnosis:
Hyperkeratosis, including hyperkeratosis of keratin epithelial
tissues, the epidermis extended to the dermis, lymphocytes
infiltrated the dermis; and iv) no treatment for recurrence or the
initial symptoms. The exclusion criteria for the psoriasis group
were as follows: i) Pregnancy and lactation; ii) PASI<10; and
iii) patients who have been treated previously. The inclusion
criteria for the normal group were as follows: i) Matched with the
psoriasis group according to sex, age and surgical site; ii) no
skin disease or family history; and iii) PASI=0. The exclusion
criteria for the normal group were as follows: i) Pregnancy and
lactation; and ii) PASI≠0. Clinical tissues that had been diagnosed
with psoriasis vulgaris (PASI >10) or normal tissues were
collected using sterile enzyme-free tubes. The samples were quickly
stored in liquid nitrogen to freeze for subsequent use.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR) analyses
Total RNA of the cells and tissues was extracted
using an RNAiso Plus kit (Takara Bio, Inc., Otsu, Japan), and cDNA
was synthesized using a PrimeScript™ RT Reagent kit (cat. no.
RR037A; Takara Biotechnology Co., Ltd., Dalian, China). The RT
temperature protocol was as follows: Reaction at 37°C for 5 min and
RT inactivation at 85°C for 5 sec. RT-qPCR reactions (20 µl)
contained 2 µl cDNA, 10 µl SYBR-Green
(SYBR® Premix Ex TaqTli RNaseH Plus; cat. no. RR420A;
Takara Biotechnology Co., Ltd.) and the appropriate primers. All
the kits were used according to the manufacturer's protocol.
Product accumulation was monitored using SYBR-Green fluorescence
with an ABI Prism 7500 Sequence Detection System. The PCR cycling
parameters were set as follows: 95°C for 30 sec followed by 40
cycles of PCR reactions at 95°C for 5 sec and 60°C for 1 min. The
standard curves of different SIRT family primers indicated the
relative expression levels. The primers for GAPDH and β-actin were
used as internal controls for normalization. Finally, the data were
analysed using GraphPad Prism 5 (GraphPad Software, Inc., La Jolla,
CA, USA). Primers were synthesized by Sangon Biotech Co., Ltd.
(Shanghai, China). The primers for human and cellular RT-qPCR are
presented in Table I, and the
primers for mouse RT-qPCR are presented in Table II. The ratio of fold changes in
SIRT mRNA expression was calculated by normalizing the Cq values of
the target gene (SIRT family) to those of the housekeeping genes
(GAPDH and β-actin) and then using the 2−ΔΔCq method
(22) to compare the test groups
and calibrator groups. The formulas used were as follows: ΔCq
(test)=Cq (target, test)-Cq (reference, test); ΔCq (calibrator)=Cq
(target, calibrator)-Cq (reference, calibrator); and ΔΔCq=Δ Cq
(test)-Δ Cq (calibrator). The calculation for the expression level
rate was 2−ΔΔCq=the ratio of the expression.
2−ΔΔCq of the control groups were classified as '1', and
the treatment groups were compared.
 | Table IPrimers used for human reverse
transcription-quantitative polymerase chain reaction in the present
study. |
Table I
Primers used for human reverse
transcription-quantitative polymerase chain reaction in the present
study.
| Primer | Direction | Sequence, 5′ to
3′ | Tm, °C | Length, bp |
|---|
| SIRT1 | F |
ACGCTGGAACAGGTTGCGGG | 65.9 | 20 |
| R |
AGCGGTTCATCAGCTGGGCAC | 65.2 | 21 |
| SIRT2 | F |
TCACACTGCGTCAGCGCCAG | 65.6 | 20 |
| R |
GGGCTGCACCTGCAAGGAGG | 68.9 | 20 |
| SIRT3 | F |
AAGTGTTGTTGGAAGTGGAG | 49.9 | 20 |
| R |
TGTGAAAGAAGAATGGGAGT | 50.4 | 20 |
| SIRT4 | F |
AGACTCCTTGTGATGACTGG | 55.5 | 20 |
| R |
AGTACAGCTTTCCGAGTTTC | 52.1 | 20 |
| SIRT5 | F |
AGCTATATTGTGGCCTGAAG | 53.2 | 20 |
| R |
CACTTTCTGCACTAACACCA | 55.3 | 20 |
| SIRT6 | F |
AGTTCGACACCACCTTTGAG | 56.4 | 20 |
| R |
CGTACTGCGTCTTACACTTG | 53.8 | 20 |
| SIRT7 | F |
CGTCCGGAACGCCAAATAC | 59.3 | 19 |
| R |
GACGCTGCCGTGCTGATT | 61.1 | 18 |
| GAPDH | F |
CGGAGTCAACGGATTTGGTCGTATTGG | 65.8 | 27 |
| R |
GCTCCTGGAAGATGGTGATGGGATTTCC | 66.9 | 28 |
 | Table IIPrimers used for mouse reverse
transcription-quantitative polymerase chain reaction in the present
study. |
Table II
Primers used for mouse reverse
transcription-quantitative polymerase chain reaction in the present
study.
| Primer | Direction | Sequence, 5′ to
3′ | Tm, °C | Length, bp |
|---|
| SIRT1 | F |
AGTTCCAGCCGTCTCTGTGT | 58.8 | 20 |
| R |
GATCCTTTGGATTCCTGCAA | 52.4 | 20 |
| SIRT2 | F |
TAGACACGCTGGAACGAGTG | 57.2 | 20 |
| R |
TCTCTTTCATCCAGCCCATC | 54.3 | 20 |
| SIRT3 | F |
CAGCTACATGCACGGTCTGT | 57.9 | 20 |
| R |
ACACAATGTCGGGTTTCACA | 54.4 | 20 |
| SIRT4 | F |
CATCCAGCACATTGATTTCG | 51.7 | 20 |
| R |
CCAGTCTCTCCCAGTTGCTC | 58.1 | 20 |
| SIRT5 | F |
CCATCACCCAGAACATTGACG | 53.7 | 20 |
| R |
ACAGTGCCACACGAGGTACA | 59.0 | 20 |
| SIRT6 | F |
GTGGATGAGGTGATGTGCAG | 56.2 | 20 |
| R |
TCAGCCTTGAGTGCTACTGG | 57.1 | 20 |
| SIRT7 | F |
GACTGAGCGTACTGCCCTTC | 58.5 | 20 |
| R |
TTCAGAGGCTGCCCTAATGT | 56.1 | 20 |
| β-actin | F |
GGCTGTATTCCCCTCCATCG | 60.0 | 20 |
| R |
CCAGTTGGTAACAATGCCATGT | 59.4 | 22 |
Western blotting
Frozen clinical tissue and mouse skin tissue
specimens were prepared for protein extraction in advance using a
mortar, and then tissue proteins and cellular proteins were
extracted on ice using radioimmunoprecipitation assay lysis buffer
(cat. no. P0013B; Beyotime Institute of Biotechnology). The amount
of protein in the extracts was determined using an Enhanced
Bicinchoninic Acid Protein Assay kit (cat. no. P0010; Beyotime
Institute of Biotechnology). Following quantitative analysis, equal
amounts of protein (50 µg) were resolved in 12, 10 and 6%
SDS-PAGE gels and electrotransferred to polyvinylidene difluoride
membranes (EMD Millipore, Billerica, MA, USA). Membranes were
subsequently blocked with 5% non-fat milk for 1 h at room
temperature and probed with specific antibodies overnight at 4°C
against SIRT1 (1:600; cat. no. 13161-1-AP; ProteinTech Group,
Inc.), SIRT2 (1:600; cat. no. PB0174; Wuhan Boster Biological
Technology, Ltd.), SIRT3 (1:600; cat. no. A01061-1; Wuhan Boster
Biological Technology, Ltd.), SIRT4 (1:200, cat. no. ab10140;
Abcam), SIRT5 (1:600; cat. no. 15122-1-AP; ProteinTech Group,
Inc.), SIRT6 (1:600; cat. no. PB0375; Wuhan Boster Biological
Technology, Ltd.), SIRT7 (1:600; cat. no. PB0376; Wuhan Boster
Biological Technology, Ltd.), GAPDH (1:2,000; cat. no. GB11002;
Wuhan Servicebio Technology Co., Ltd.) and β-actin (1:1,000; cat.
no. ab8226; Abcam). Following three washes with PBS with Tween-20,
membranes were incubated with the following secondary antibodies
for about 1.5 h at room temperature: Horseradish peroxidase
(HRP)-labeled goat anti-rabbit IgG (H+L; 1:800; cat. no. A0208;
Beyotime Institute of Biotechnology) was used to detect SIRT1,
SIRT2, SIRT3, SIRT5, SIRT6, SIRT7 and GAPDH, HRP-labeled Donkey
Anti-Goat IgG (H+L; 1:15,00; cat. no. A0181; Beyotime Institute of
Biotechnology) was used to detect SIRT4, and HRP-labeled Goat
Anti-Mouse IgG (H+L; 1:1,000; cat. no. A0216; Beyotime Institute of
Biotechnology) was used to detect β-actin. Immunoreactive signals
were detected using enhanced chemiluminescence reagents (EMD
Millipore). Protein expression levels were compared with the
control group. Finally, the protein strips were analysed using
ImageJ (1.46r/Java 1.6.0_20(32-bit); National Institutes of Health,
Bethesda, MD, USA) and GraphPad Prism 5 (GraphPad Software, Inc.,
La Jolla, CA, USA).
Histopathological and IF
examinations
Tissues obtained from patients with diagnosed
psoriasis (n=22; PASI >10) and the control patients (n=22) and
the skin samples from the back lesions of mice (n=8) were fixed at
room temperature in 10% formalin and embedded in paraffin. For
histopathological examinations, 4-µm sections were stained
with hemotoxylin and eosin (H&E) and observed under an XDS-1B
light microscope (Olympus Corporation; magnification, ×100). For
H&E staining, sections were dewaxed and dehydrated by washing
three times in xylene for 10 min each time, and washing in a
descending alcohol gradient of 100, 95, 85 and 75% ethanol for 10
min each time. The sections were subsequently stained for 10 min in
H solution and 3 min in E solution at room temperature. The
sections were dehydrated in 85, 95 and 100% ethanol for 2 min each
time, and sealed slides with neutral balsam. For IF staining,
4-µm sections were dewaxed three times (10 min each time)
with xylene and rehydrated four times (3 min each time) with
alcohol (in a descending concentration gradient; 100, 95, 90 and
70%), quenched with endogenous peroxidase, and subsequently treated
for antigen retrieval (saline sodium citrate; pH=6.0; water bath
heating; 100°C; 20 min). The sections were then rinsed three times
(5 min each time) with PBS following each step. The sections were
subsequently blocked with 5% BSA for 1 h at room temperature. The
antibodies against SIRT1 (1:100; cat. no. 13161-1-AP; ProteinTech
Group, Inc.), SIRT2 (1:100; cat. no. PB0174; Wuhan Boster
Biological Technology, Ltd.), SIRT3 (1:100; cat. no. A01061-1;
Wuhan Boster Biological Technology, Ltd.), SIRT4 (1:100; cat. no.
ab10140; Abcam), SIRT5 (1:100; cat. no. 15122-1-AP; ProteinTech
Group, Inc.), SIRT6 (1:100; cat. no. PB0375; Wuhan Boster
Biological Technology, Ltd.) and SIRT7 (1:100; cat. no. PB0376;
Wuhan Boster Biological Technology, Ltd.) were incubated with the
sections overnight at 4°C. On the subsequent day, donkey
anti-rabbit IgG (Alexa Fluor 488; 1:500; cat. no. ab150073; Abcam)
was used to label SIRT1, SIRT2, SIRT3, SIRT5, SIRT6 and SIRT7, and
FITC-conjugated donkey anti-goat IgG (H+L; 1:50; cat. no. GB22404;
Wuhan Servicebio Technology Co., Ltd.) was used to label SIRT4 for
1 h at room temperature. DAPI was used for 10 min at room
temperature to stain nuclei and the cells were observed using a
fluorescent microscope (Olympus Corporation; magnification,
×400).
Statistical analysis
As the data were normally distributed, a Student's
t-test was used to compare the expression levels of the 7 SIRTs
between the experiment and control groups. All data are presented
as the mean ± standard deviation and were analysed by Student's
t-test using GraphPad Prism 5 (GraphPad Software, Inc.). All
statistical tests were two-sided. P<0.05 was considered to
indicate a statistically significant difference.
Results
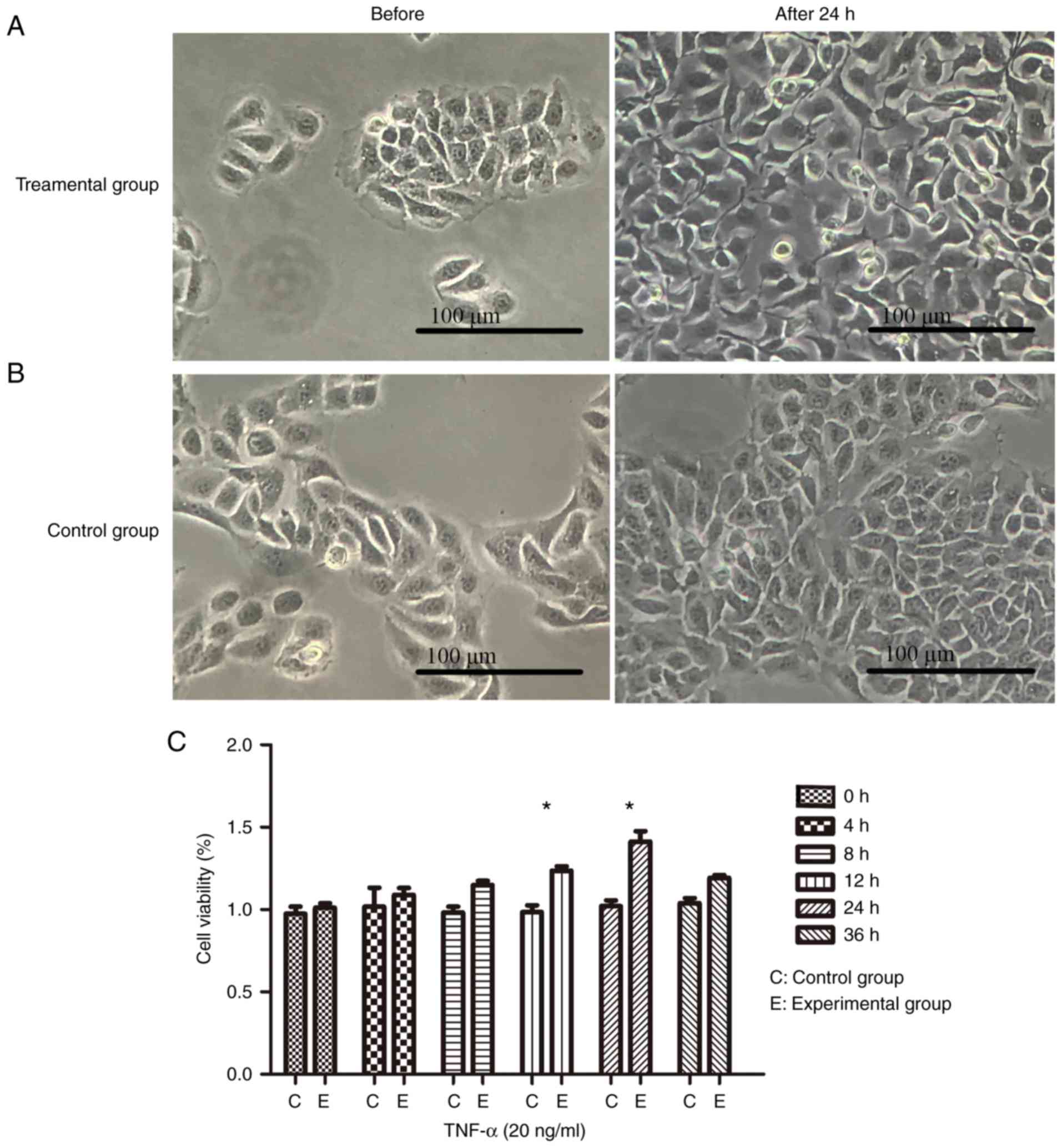
TNF-α-stimulated HaCaT cells
The most noticeable observed changes were in the
morphology, the intercellular space and the quantity of cells
(Fig. 1A and B). Under culture
conditions with TNF-α (20 ng/ml), cell viability assays revealed
that the maximum number of cells was at the 24 h mark, with a
higher number of cells in the experiment group compared with the
control group observed at all time points (Fig. 1C).
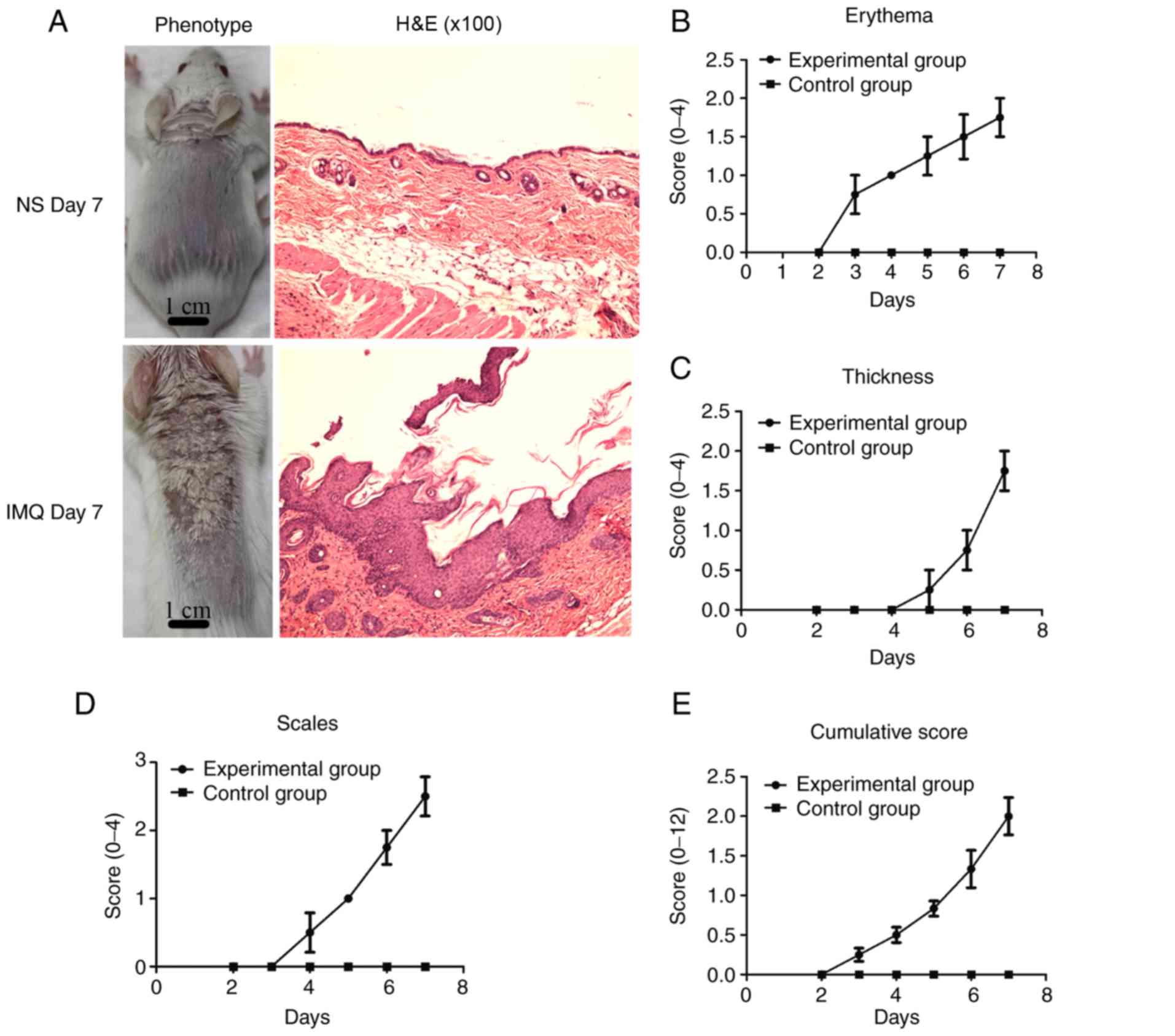
Animal model
In the present study, compared with the control
group, psoriasis-like lesions, including erythema, thickening and
scales (Fig. 2A), were gradually
observed on the back skin of the mice over the 7 days of IMQ
treatment. The skin lesions in the mice were confirmed by
corresponding histological analyses (H&E staining; Fig. 2A). To record the skin changes in
the mice, an objective scoring system was developed based on PASI,
which consists of measurements of skin erythema, thickness and
scales. The clinical scores included erythema (Fig. 2B), skin thickness (Fig. 2C), scaling (Fig. 2D), and cumulative scores (Fig. 2E). Compared with the control
group, the skin lesions in the experimental group were red and
edematous, with more scales and a thickened epidermis. The
cumulative score denotes the severity of inflammation.
Clinical data
A total of 44 samples were collected in the present
study, including 22 from patients diagnosed with psoriasis vulgaris
(PASI>10) and 22 from normal control subjects. All clinical
information is presented in Table
III. The mean ages were 43±15 and 42±15 years in the psoriasis
and control groups, respectively. The mean PASI score in the
psoriasis group was 14.1±3.1.
 | Table IIIPatient clinical information. |
Table III
Patient clinical information.
| No. | Age, years
| Sex | Site | PASI
|
|---|
| Psoriasis | Control | Psoriasis | Control |
|---|
| 1 | 45 | 41 | F | Leg | 10.2 | 0 |
| 2 | 35 | 30 | F | Back | 14.8 | 0 |
| 3 | 57 | 53 | F | Chest | 15 | 0 |
| 4 | 17 | 14 | F | Back | 16 | 0 |
| 5 | 23 | 24 | F | Chest | 13.6 | 0 |
| 6 | 56 | 61 | F | Arm | 22.8 | 0 |
| 7 | 47 | 59 | F | Back | 13 | 0 |
| 8 | 37 | 41 | F | Leg | 19.8 | 0 |
| 9 | 55 | 52 | F | Leg | 11.4 | 0 |
| 10 | 38 | 35 | M | Arm | 11.2 | 0 |
| 11 | 31 | 30 | M | Back | 14.4 | 0 |
| 12 | 30 | 30 | M | Arm | 10.8 | 0 |
| 13 | 23 | 29 | M | Chest | 14.6 | 0 |
| 14 | 29 | 29 | M | Back | 15 | 0 |
| 15 | 54 | 41 | M | Arm | 15.8 | 0 |
| 16 | 60 | 62 | M | Leg | 10.6 | 0 |
| 17 | 67 | 62 | M | Leg | 10.2 | 0 |
| 18 | 62 | 62 | M | Leg | 16 | 0 |
| 19 | 29 | 26 | M | Back | 16.2 | 0 |
| 20 | 44 | 42 | M | Leg | 13 | 0 |
| 21 | 38 | 36 | M | Back | 15.4 | 0 |
| 22 | 64 | 63 | M | Arm | 10.6 | 0 |
| Mean ± SD | 43±15 | 42±15 | NA | NA | 14.1±3.1 | 0 |
Altered expression of SIRTs in
TNF-α-stimulated HaCaT cells, IMQ-induced psoriasis-like skin
lesions in mice, and clinical psoriasis skin lesions
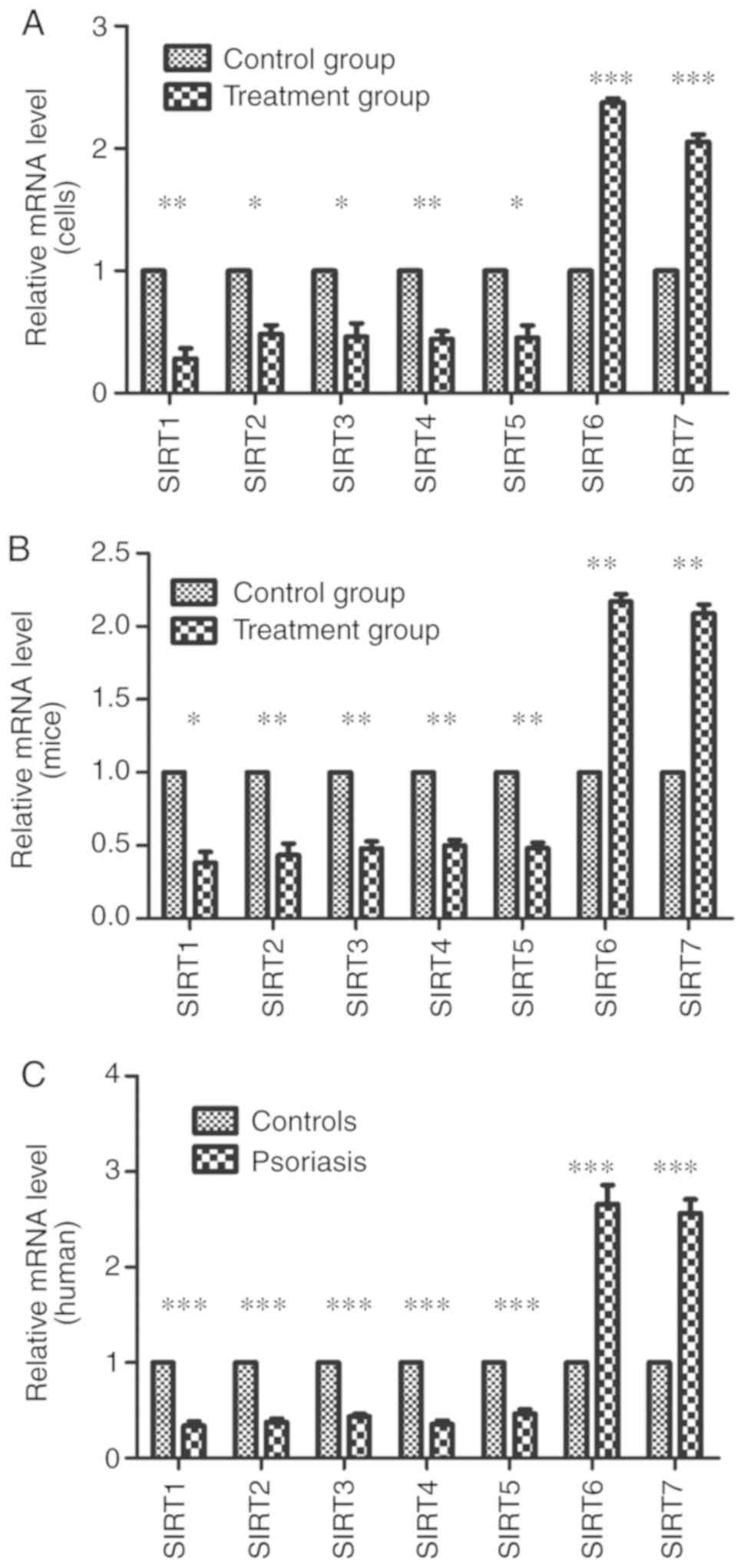
RT-qPCR was used to evaluate the mRNA expression
levels of SIRTs in skin lesions and TNF-α-stimulated HaCaT cells
compared with the control groups. The results demonstrated that the
mRNA expression levels of SIRT1, SIRT2, SIRT3, SIRT4 and SIRT5
significantly decreased; however, the mRNA expression levels of
SIRT6 and SIRT7 significantly increased compared with the control
groups (P<0.05; Fig. 3). To
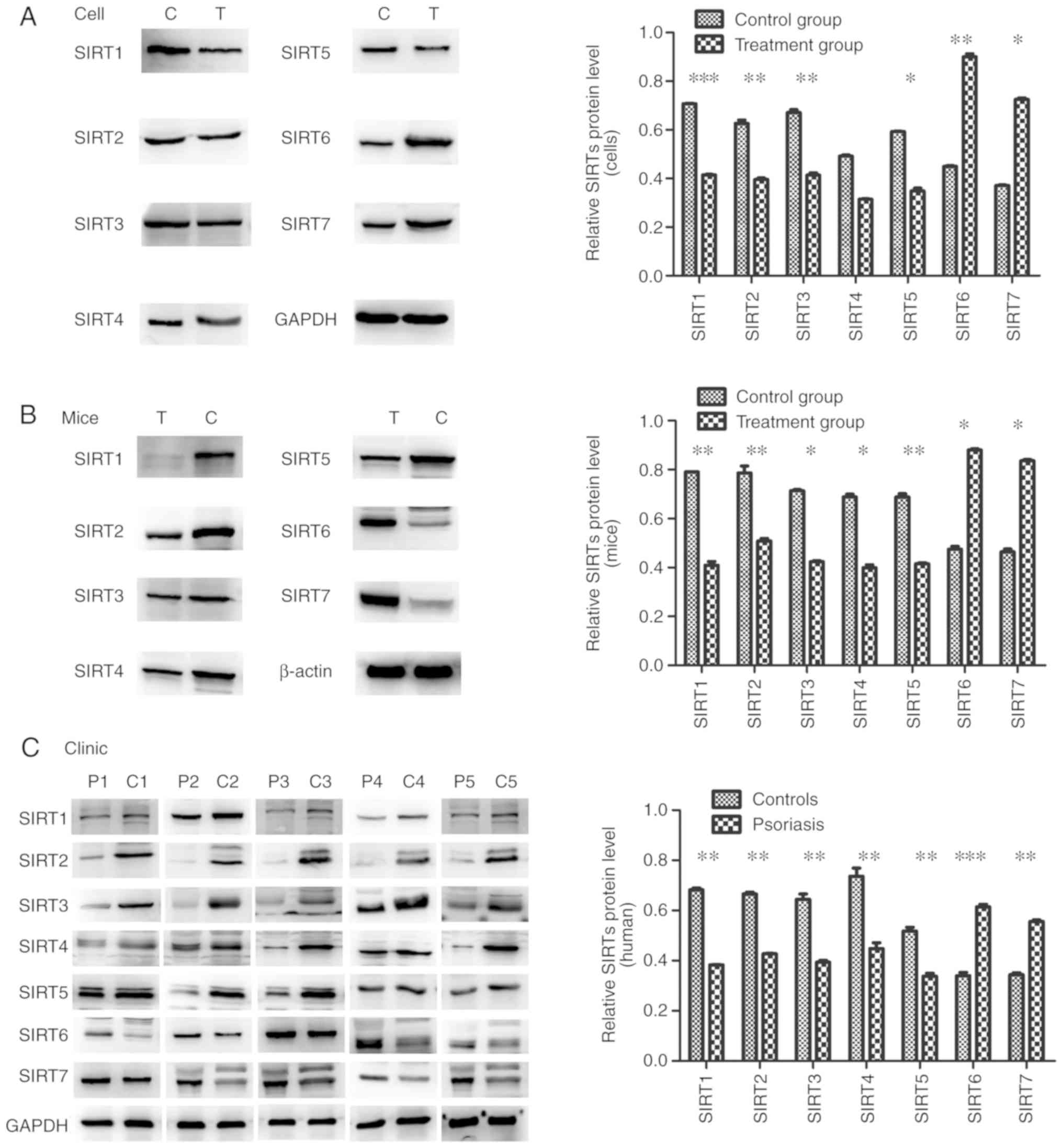
confirm this observation, the present study performed western
blotting with skin tissues and cells to investigate the protein
expression levels. The significantly lower protein expression
levels of SIRT1, SIRT2, SIRT3, SIRT4 and SIRT5 and the
significantly higher expression levels of SIRT6 and SIRT7 were
observed in skin lesions and TNF-α-stimulated HaCaT cells when
compared with the control groups (P<0.05; except for SIRT4), and
were indicative of their potential function in regulating psoriasis
dermatitis and psoriasis-like inflammation (Fig. 4).
IF assays
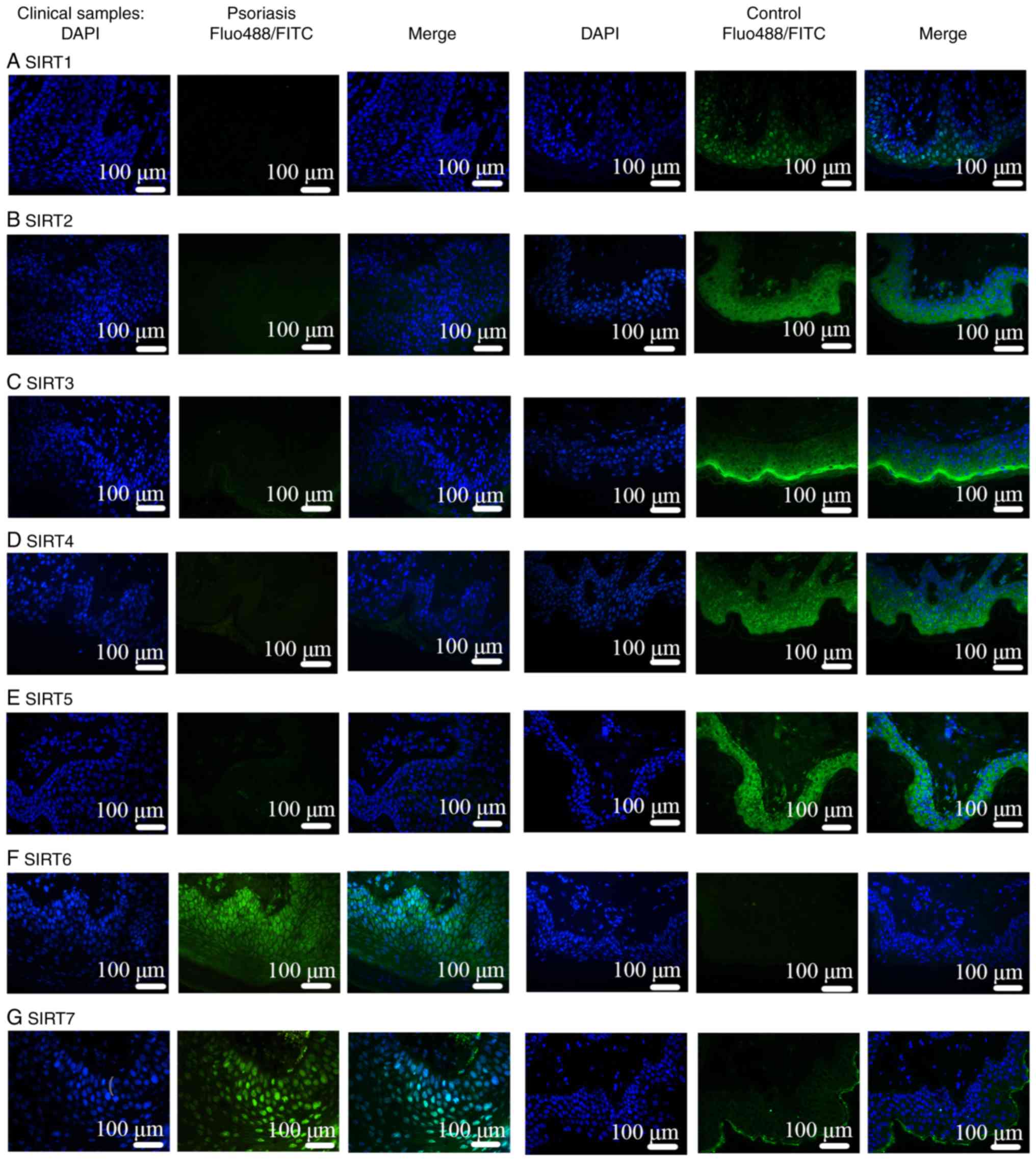
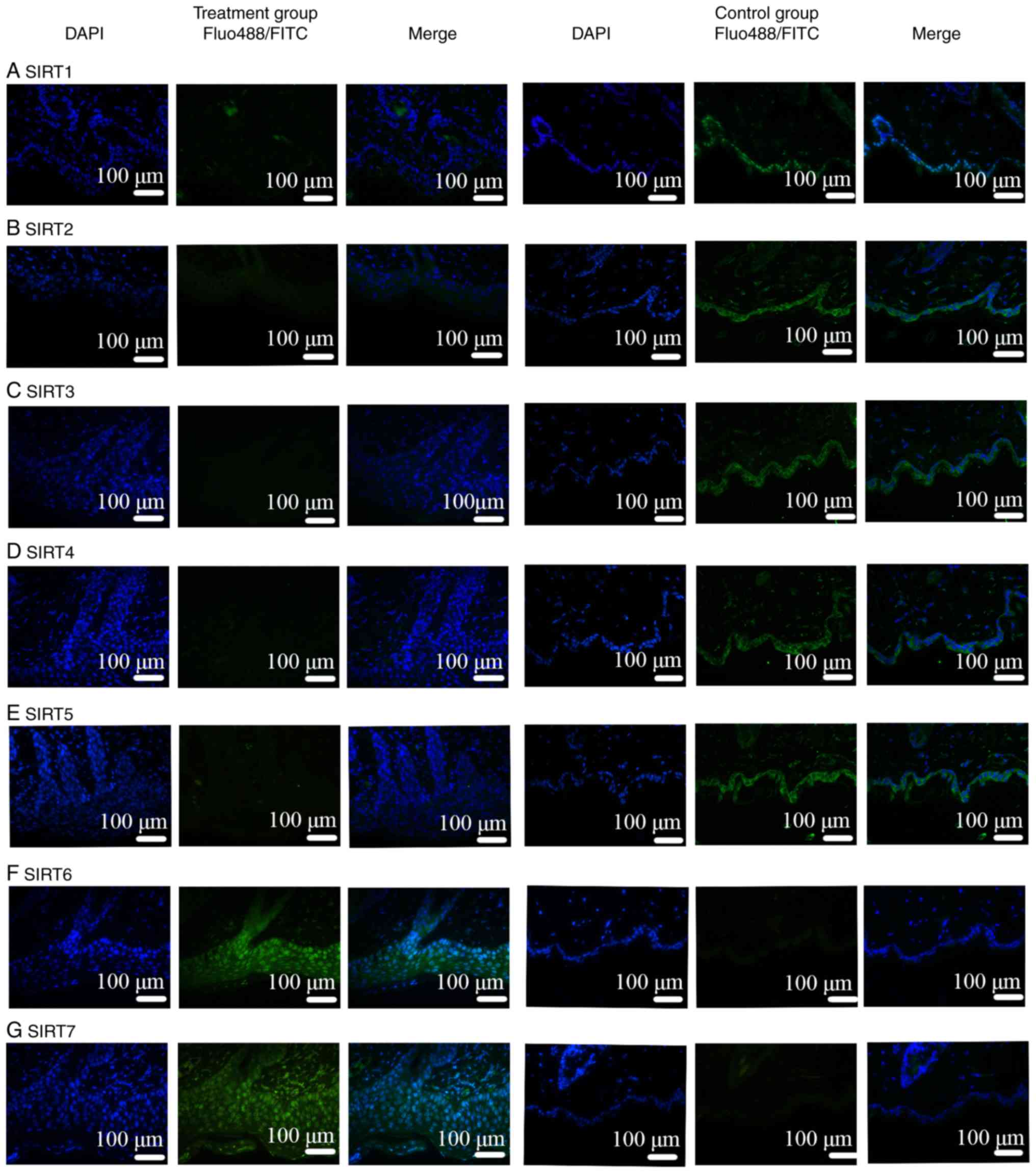
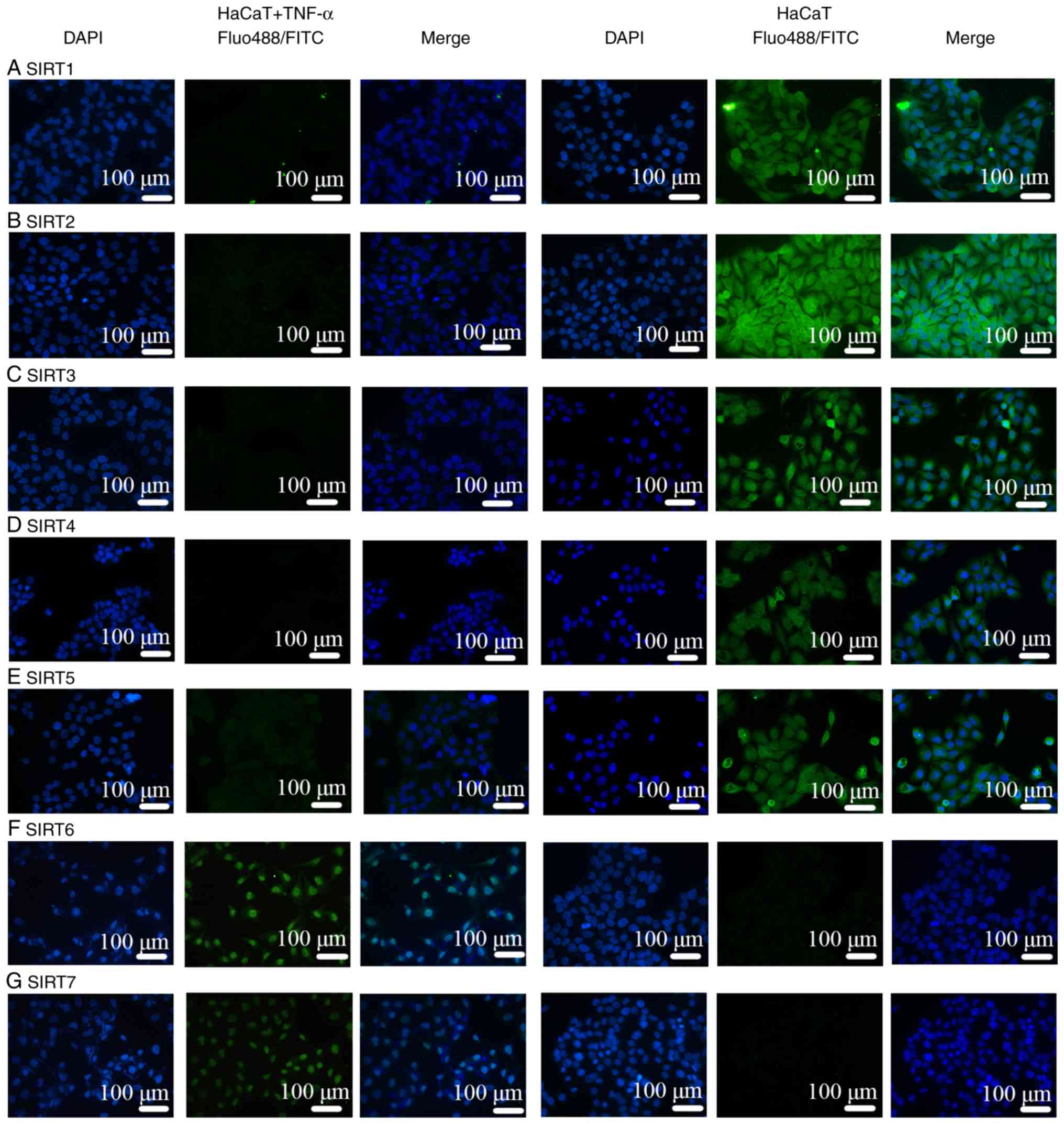
Comparisons of IMQ-induced psoriasis-like skin
lesions in mice and clinical psoriasis skin lesions in the control
groups based on DAPI staining revealed that the number of epidermal
and subcutaneous cells was increased under pathological conditions.
In addition, based on the results of FITC and Alexa Fluor-488
staining, the binding sites of the SIRT antibodies were mainly
located in the epidermis. Therefore, the expression of SIRT
proteins was revealed to be mainly in the epidermis instead of in
the subcutaneous tissue, as presented in Figs. 5 and 6. Notably, IF was negative for SIRT1,
SIRT2, SIRT3, SIRT4 and SIRT5 antibodies (Figs. 5A-E, 6A-E and 7A-E), and positive for SIRT6 (Figs. 5F, 6F and 7F) and SIRT7 (Figs. 5G, 6G and 7G) antibodies. Additionally, another
function of IF was to identify the localization of SIRTs. SIRT1 and
SIRT2 were localized in the nucleus and also the cytoplasm
(Fig. 7A and B). SIRT3, SIRT4,
and SIRT5 were primarily mitochondrial proteins (Fig. 7C-E). However, SIRT6 and SIRT7 were
nuclear SIRTs (Fig. 7F and G).
These results are consistent with previous literature (7).
Discussion
Psoriasis is a chronic autoimmune inflammatory
disease associated with multiple epithelial metabolism disorders
regulated by the interactions between keratinocytes, dendritic
cells and T lymphocytes (23).
The skin, as the first line of defense of the body, participates in
innate immune responses by activating surface receptors including
Toll-like receptors (TLRs) and Nod-like receptors (24). IMQ, a TLR activator, induces
cytokine (TNF-α and IFN-α/β) release (20). Keratinocytes, as nonprofessional
antigen-presenting cells, may cause skin immune responses through
TLRs and major histocompatibility complex (MHC) class II molecules
in inflammatory conditions, resulting in the release of
inflammatory molecules and cell adhesion molecules by various
signaling pathways (25,26). This process may be regulated by
SIRTs. In turn, these inflammatory molecules and cell adhesion
molecules exert their function on keratinocytes to regulate the
growth and differentiation of keratinocytes. This process is also
regulated by SIRTs (27). TNF-α
is a core cytokine in the development of psoriasis as it cannot
react only with keratinocytes or HaCaT cells to induce immune
responses, but also promote the expression of inhibitor of
apoptosis protein (IAP), intracellular adhesion molecule (ICAM-1),
epidermal growth factor receptors (EGFRs) and keratin 17 (K17)
(19,20). TNF-α-treated keratinocytes
increase the production of EGFR ligands through the classical
mitogen activated protein kinase (MAPK) and NF-κB signaling
pathways; thus, EFGR activation may promote epidermal proliferation
and inflammatory factor release (18,19,28). Therefore, TNF-α-induced MAPK/NF-κB
activation may result in cell proliferation and inflammatory
responses in HaCaT cells similar to psoriasis-induced inflammation
in vivo. Keratinocytes activate innate immune responses that
promote the expression of effective pro-inflammatory factors
(including TNF-α), which may react with keratinocytes to promote
the expression of other factors including MHC-II, K17 and IAPs
(29). IAP, K17 and ICAM-1,
produced via the regulation of TNF-α, may cause the epithelial
layer to thicken and become difficult to shed, while SIRTs modulate
inflammatory factor generation (16,30). These processes may be regulated by
SIRTs. IF in the present study revealed that SIRTs were mainly
localized in the epithelial layer as opposed to in the subcutaneous
tissue, which may mean that keratinocytes, as antigen-presenting
cells, may primarily cause the immune response rather than
subcutaneous lymphocytes.
SIRTs serve important functions in the mechanisms
underlying psoriasis. Numerous studies have reported associations
between SIRTs and longevity, insulin resistance and oxidative
stress, indicating that SIRTs have a close association with MS
(3,26,31). The inflammatory factor production
and immune cell differentiation processes are regulated by SIRTs
via deacetylation. In addition, accumulating evidence has suggested
that the sequential course of inflammation is associated with
metabolism via SIRTs (26,32).
Therefore, SIRTs may have a close association with psoriasis,
causing inflammatory lesions through multiple different
pathways.
SIRT1 serves a notable function in survival,
differentiation, metabolism and chromatin remodeling. SIRT1
controls immune responses by causing P65, P53, transcription factor
activator protein 1, c-Jun, Forkhead box O (FOXO), protein kinase B
and eukaryotic translation initiation factor 2A on Lys-141 (K141)
and Lys-143 (K143) to deacetylate, which in turn regulates
inflammatory factors including nitric oxide, TNF-α, interleukin
(IL)-12, arginase, TNF-β and IL-10; these serve key functions in
the pathogenesis of psoriasis and regulate insulin sensitivity
(3,8). SIRT1 attenuates inflammation and
oxidative stress via the inhibition of mitochondrial ROS production
and the reduction of hydrogen peroxide levels at the cardiovascular
level (33). The production of
ROS may cause mitochondrial DNA mutations, insulin resistance and
mitochondrial damage, which ultimately induce diabetes, obesity and
fatty liver disease (9). In
addition, obesity-induced insulin resistance and type 2 diabetes
mellitus, potentially stimulated by chronic inflammation to
influence insulin secretion in pancreatic β cells, are associated
with SIRT1 (10). Notably, SIRT1
positively binds with FOXO3a and nuclear respiratory factor 1 in
the promoter region of SIRT6 to form a complex that is associated
with longevity and metabolism (11). Furthermore, SIRT1 and SIRT6 alter
glycolysis to fatty acid β-oxidation for the rapid production of a
high energy supply and a timely inflammatory response to promote
mitochondrial biogenesis and recover homeostasis (33). SIRT6, which predominately mediates
metabolism, aging, cancer, DNA repair and genomic stability,
affects TNF-α production via the deacetylation of H3K9-Ac in the
promoter region of NF-κB target genes (33). The NF-κB protein complex, a key
regulator of the immune response, and TNF-α, a common inflammatory
pathway cyto-kine, are involved in a number of inflammatory skin
diseases including psoriasis (34). However, whether SIRT6 suppresses
the expression of pro-inflammatory cytokines and transcriptional
activity depends on the cell type and the transcriptional pathway
(11). Therefore, chronic
inflammation is stimulated by the activation of c-Jun-dependent
transcription and the enhanced expression of pro-inflammatory genes
in the livers of Sirt6-null (Sirt6-/-) mice, and SIRT6 is elevated
in psoriasis and arthritis; however, the mechanisms for this action
remain unknown (35,36). SIRT1 downregulation occurs in
mature psoriasis as the balance of SIRT1 and pro-inflammatory
cytokines is lost in immunologically mature psoriatic lesions and
cuticle epithelial metabolism disorders due to the bridging effect
of SIRT1 between metabolic changes and immune signals (16).
There is a hypothesis that SIRT2 combines with SIRT1
and SIRT6 via NF-κB p65 deacetylation and the modulation of FOXO3a
during oxidative stress, which appears to be a cooperative form of
SIRT function in the inflammation process (12).
Mitochondrial SIRTs (SIRT3, SIRT4 and SIRT5)
regulate energy metabolism and various homeostatic processes by
mediating the post-translational modifications of mitochondrial
proteins, including a diverse set of enzymes (7). Among the mitochondrial SIRTs, SIRT3
has a greater number of mitochondrial targets to suppress
proliferation capacity, increase fatty acid β-oxidation, and
deacetylate and activate the key enzymes in the electron transport
chain and urea cycle, thereby avoiding the emergence of a diverse
set of pathologies (13). The
downregulation of SIRT3 is associated with poor prognoses. However,
SIRT5 is a more selective deacetylase, modulating, for example, PDH
and succinate dehydrogenase, whereas SIRT4 modulates the activity
of PDH and GDH only via adenosine diphosphate-ribosyltransferase
activity (14). Mitochondrial
SIRTs serve a notable function in the regulation of insulin
sensitivity through all of the aforementioned pathways. Insulin
serves an important function in regulating the body's metabolism of
sugar, fats and proteins. When insulin resistance occurs in the
body, the physiological effects of insulin on the target tissue are
decreased, which may result in pathophysiological alterations in
the organism and cause the occurrence of various metabolic diseases
(37). Accumulating evidence
supports a positive association between psoriasis and insulin
resistance (38,39). Furthermore, a number of reports
have proposed that hyperglycemia and impaired insulin signaling
pathways may be involved in the occurrence of chronic diabetic
complications, the glucose utilization of skin keratinocytes, and
abnormal skin proliferation and differentiation (3,40).
SIRT7 is a critical regulator of multiple cellular
biological processes including transcription, chromatin structure,
genomic stability, tumorigenesis, energy homeostasis and cell
proliferation. As a pro-survival adaptor molecule, SIRT7 serves a
function in regulating specific transcription factors including
Myc, hypoxia-inducible factor (HIF)-1α and HIF2α via deacetylation
(15). The high expression of
SIRT7 results in cell proliferation, particularly in metabolically
active cells including keratinocytes, and represses the expression
of ribosomal proteins to alleviate stress, which allows cells to
adapt to environmental challenges and promotes survival. DNA damage
repair mediated by SIRT7 may maintain genomic integrity (41).
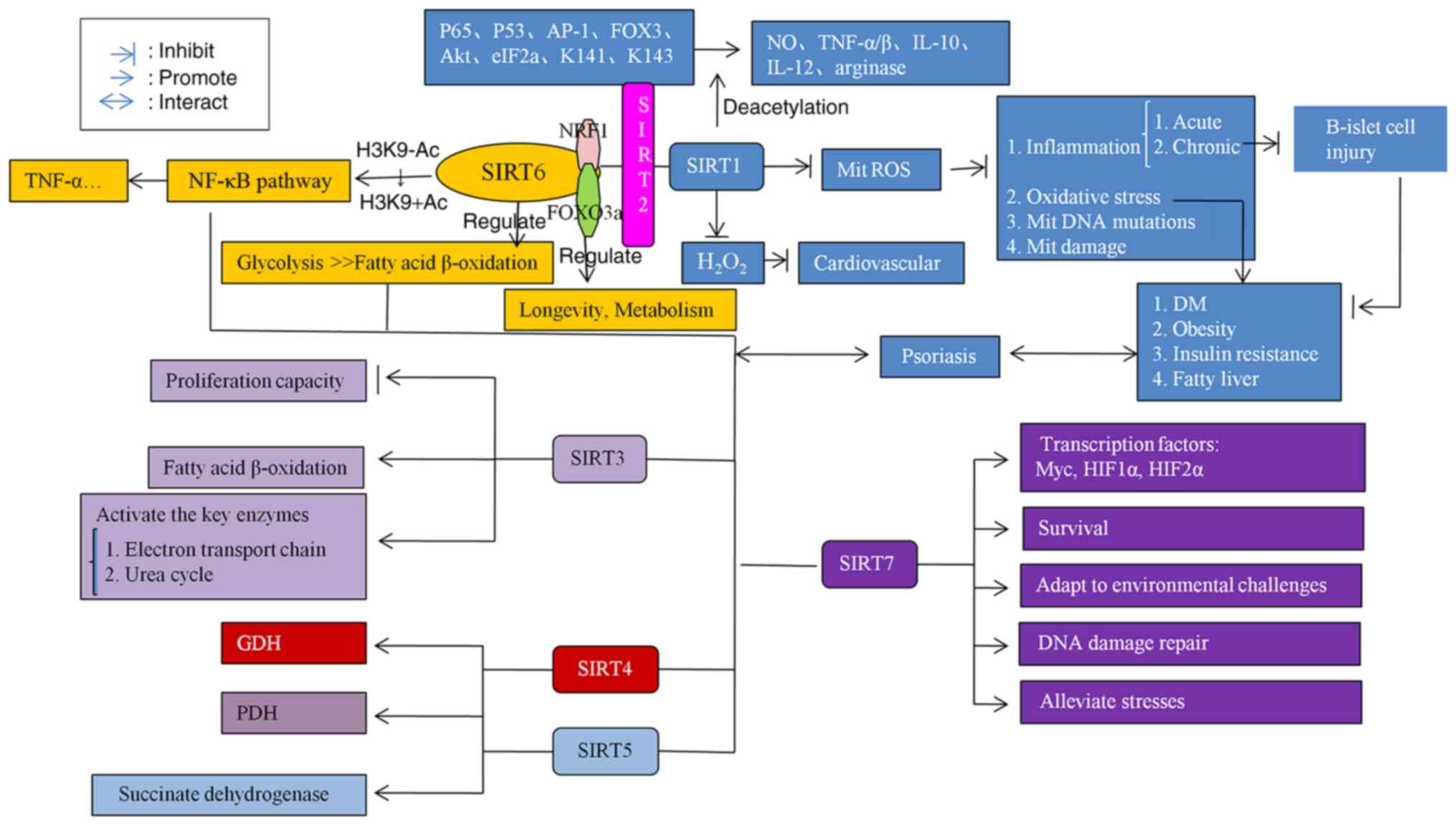
A summary of the SIRTs mechanism in inflammation and
metabolism is presented in Fig.
8.
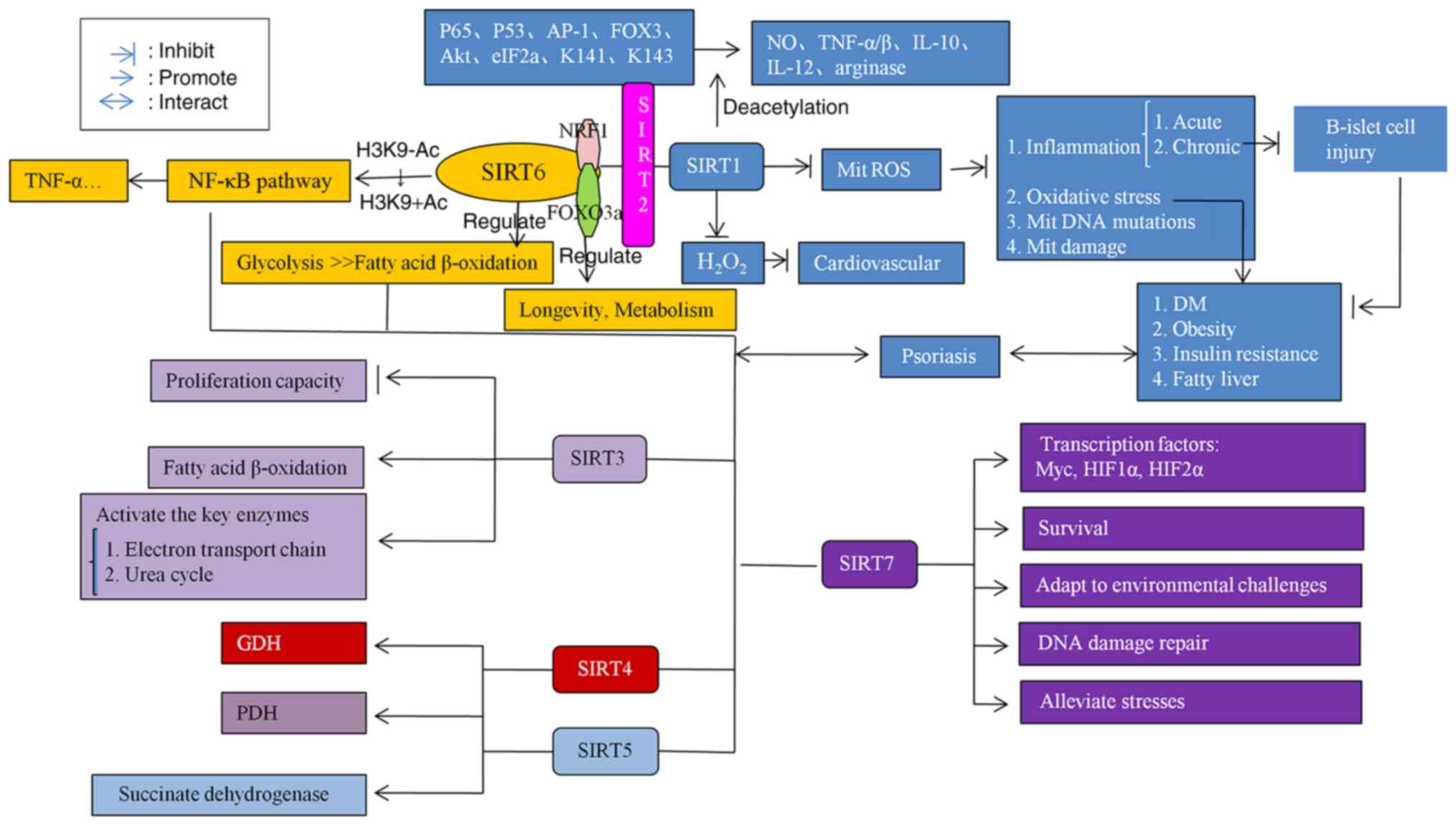 | Figure 8Mechanism of SIRTs in inflammation
and metabolism. SIRTs coordinate with each other and serve
functions in regulating inflammation and metabolism. When the SIRT
level is abnormal, inflammation and metabolic disorders may be
caused via a variety of pathways, and then the production of
psoriasis may be induced. SIRT, Sirtuin; NF-κB, nuclear factor-κB;
TNF-α/β, tumor necrosis factor α/β; FOX3, fork head transcription
factor 3; Akt, protein kinase B; eIF2a, Eukaryotic translation
initiation factor 2A; NO, nitric oxide; IL, interleukin; ROS,
reactive oxygen species; Mit, mitochondrial; HIF-1α
hypoxia-inducible factor 1α; HIF2α, hypoxia-inducible factor 2α;
K141, Lys-141; K143, Lys-143. |
The results of the present study provide a
hypothesis regarding the pathogenesis of psoriasis in a chronic
inflammation model. The dynamic equilibrium state of SIRTs under
physiological conditions was lost due to a variety of reasons. On
one hand, the expression levels of associated nuclear transcription
factors were altered, affecting the release of pro-inflammatory
factors including TNF-α and metabolic factors including ROS, which
function against specific targets that result in inflammatory
immune responses and metabolic disorders. On the other hand,
multiple cellular biological processes that are mediated by SIRTs,
including genome stability, energy homeostasis, cell proliferation,
post-translational modifications and insulin resistance, are
disrupted, ultimately leading to metabolic diseases and
inflammatory diseases. However, further mechanisms require
investigation, which will be attempted in the future.
In conclusion, psoriasis is an inflammatory,
metabolism-associated disease mediated by the SIRT family. The
present study revealed that overexpression of SIRT6 and SIRT7 force
the body to adapt to changes in the external environment through
various molecular biological mechanisms. However, the
downregulation of SIRT1, SIRT2, SIRT3, SIRT4 and SIRT5 is an effect
observed at the molecular level of severe psoriasis dermatitis due
to an imbalance in the physical state. Thus, SIRT1-SIRT5 agonists
and SIRT6 and SIRT7 inhibitors may be novel therapeutic options for
psoriasis.
Funding
The present study was supported by the National
Nature Science Foundation of China (grant nos. 81673054 and
81773322) and the Pudong New Area Committee on Health and Family
Planning (grant no. PWZxq2017-16).
Availability of data and materials
All date used and/or analysed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XF and HD contributed to the conception and design
of the study. XF, KY, XY, QM, RS and DY performed the experiments.
XF, KY and HD analysed the data. XF, KY, HD and FL interpreted the
results of the experiments. XF, KY and HD prepared the figures. XF,
KY, QM and HD drafted the manuscript. XF, QM and HD edited and
revised the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Patients' written informed consent was obtained and
was approved by the Ethics Committee of Shanghai Sixth People's
Hospital (registration no. 2018-029). The animal care and
experimental procedures were ethically approved by the Animal
Welfare Committees of Shanghai Sixth People's Hospital (Shanghai,
China; Animal Experiment registration no. DWLL2017-0312).
Patient consent for publication
Written informed consent was obtained from patients
who participated in this study.
Competing interests
The authors declare that they have no competing
interests.
Abbreviations:
|
SIRTs
|
sirtuins
|
|
IMQ
|
imiquimod
|
|
EGFR
|
epidermal growth factor receptor
|
|
MAPK
|
mitogen activated protein kinase
|
|
NF-κB
|
nuclear factor-κB
|
Acknowledgments
The authors would like to thank Mr. Meiliang Guo
(Central Laboratory of Shanghai Sixth People's Hospital Affiliated
to Shanghai Jiaotong University, Shanghai, China) for his network
support help.
References
|
1
|
Michalek IM, Loring B and John SM: A
systematic review of worldwide epidemiology of psoriasis. J Eur
Acad Dermatol Venereol. 31:205–212. 2017. View Article : Google Scholar
|
|
2
|
Zhao Na: Epidemiologycal analysis on
psoriasis vulgaris in a hospital for skin diseases (unpublished PhD
thesis). Shandong University; 2011
|
|
3
|
Napolitano M, Megna M and Monfrecola G:
Insulin resistance and skin diseases. ScientificWorldJournal.
2015:4793542015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gu Y and Nordstrom BL: The risk of
malignancy among biologic-naive pediatric psoriasis patients: A
retrospective cohort study in a US claims database. J Am Acad
Dermatol. 77:293–301.e1. 2017. View Article : Google Scholar
|
|
5
|
Di Meglio P, Villanova F and Nestle FO:
Psoriasis. Cold Spring Harb Perspect Med. 4:a0153542014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
McCormick R, McDonagh B and
Goljanek-Whysall K: microRNA-SIRT-1 interactions: Key regulators of
adult skeletal muscle homeostasis? J Physiol. 595:3253–3254. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
George J and Ahmad N: Mitochondrial
sirtuins in cancer: Emerging roles and therapeutic potential.
Cancer Res. 76:2500–2506. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Busch F, Mobasheri A, Shayan P, Stahlmann
R and Shakibaei M: Sirt-1 is required for the inhibition of
apoptosis and inflammatory responses in human tenocytes. J Biol
Chem. 287:25770–25781. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ding RB, Bao J and Deng CX: Emerging roles
of SIRT1 in fatty liver diseases. Int J Biol Sci. 13:852–867. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Moynihan KA, Grimm AA, Plueger MM,
Bernal-Mizrachi E, Ford E, Cras-Méneur C, Permutt MA and Imai S:
Increased dosage of mammalian Sir2 in pancreatic beta cells
enhances glucose-stimulated insulin secretion in mice. Cell Metab.
2:105–117. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gertler AA and Cohen HY: SIRT6, a protein
with many faces. Biogerontology. 14:629–639. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Buechler N, Wang X, Yoza BK, McCall CE and
Vachharajani V: Sirtuin 2 regulates microvascular inflammation
during sepsis. J Immunol Res. 2017:26489462017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sack MN and Finkel T: Mitochondrial
metabolism, sirtuins, and aging. Cold Spring Harb Perspect Biol.
4:a0131022012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mathias RA, Greco TM and Cristea IM:
Identification of Sirtuin4 (SIRT4) protein interactions: Uncovering
candidate acyl- modified mitochondrial substrates and enzymatic
regulators. Methods Mol Biol. 1436:213–239. 2016. View Article : Google Scholar
|
|
15
|
Kiran S, Anwar T, Kiran M and Ramakrishna
G: Sirtuin 7 in cell proliferation, stress and disease: Rise of the
seventh sirtuin! Cell Signal. 27:673–682. 2015. View Article : Google Scholar
|
|
16
|
Rasheed H, El-Komy M, Hegazy RA, Gawdat
HI, AlOrbani AM and Shaker OG: Expression of sirtuins 1, 6, tumor
necrosis factor, and interferon-gamma in psoriatic patients. Int J
Immunopathol Pharmacol. 29:764–768. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Xie S, Su Z, Zhang B, Ge J, Song S, Sun G,
Sun X, Yi L, Wang Y, Sun W, et al: SIRT1 activation ameliorates
aldara-induced psoriasiform phenotype and histology in mice. J
Invest Dermatol. 135:1915–1918. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sun J, Han J, Zhu Q, Li Z and Hu J:
Camptothecin fails to induce apoptosis in tumor necrosis
factor-alpha-treated HaCaT cells. Pharmacology. 89:58–63. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cho JW, Lee KS and Kim CW: Curcumin
attenuates the expression of IL-1beta, IL-6, and TNF-alpha as well
as cyclin E in TNF-alpha-treated HaCaT cells; NF-kappaB and MAPKs
as potential upstream targets. Int J Mol Med. 19:469–474.
2007.PubMed/NCBI
|
|
20
|
Xiong H, Xu Y, Tan G, Han Y, Tang Z, Xu W,
Zeng F and Guo Q: Glycyrrhizin ameliorates imiquimod-induced
psoriasis-like skin lesions in BALB/c mice and inhibits
TNF-α-induced ICAM-1 expression via NF-κB/MAPK in HaCaT cells. Cell
Physiol Biochem. 35:1335–1346. 2015. View Article : Google Scholar
|
|
21
|
Li R, Wang J, Wang X, Zhou J, Wang M, Ma H
and Xiao S: Increased βTrCP are associated with imiquimod-induced
psoriasis- like skin inflammation in mice via NF-κB signaling
pathway. Gene. 592:164–171. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
23
|
Cai Y, Fleming C and Yan J: New insights
of T cells in the pathogenesis of psoriasis. Cell Mol Immunol.
9:302–309. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jeon YJ, Sah SK, Yang HS, Lee JH, Shin J
and Kim TY: Rhododendrin inhibits toll-like receptor-7-mediated
psoriasis- like skin inflammation in mice. Exp Mol Med.
49:e3492017. View Article : Google Scholar
|
|
25
|
Schwarz G, Boehncke WH, Braun M, Schröter
CJ, Burster T, Flad T, Dressel D, Weber E, Schmid H and Kalbacher
H: Cathepsin S activity is detectable in human keratinocytes and is
selectively upregulated upon stimulation with interferon-gamma. J
Invest Dermatol. 119:44–49. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Vachharajani VT, Liu T, Wang X, Hoth JJ,
Yoza BK and McCall CE: Sirtuins link inflammation and metabolism. J
Immunol Res. 2016:81672732016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sestito R, Madonna S, Scarponi C,
Cianfarani F, Failla CM, Cavani A, Girolomoni G and Albanesi C:
STAT3-dependent effects of IL-22 in human keratinocytes are
counterregulated by sirtuin 1 through a direct inhibition of STAT3
acetylation. FASEB J. 25:916–927. 2011. View Article : Google Scholar
|
|
28
|
Torii S, Yamamoto T, Tsuchiya Y and
Nishida E: ERK MAP kinase in G cell cycle progression and cancer.
Cancer Sci. 97:697–702. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kwon TR, Oh CT, Choi EJ, Kim SR, Jang YJ,
Ko EJ, Suh D, Yoo KH and Kim BJ: Ultraviolet light-emitting-diode
irradiation inhibits TNF-α and IFN-gamma-induced expression of
ICAM-1 and STAT1 phosphorylation in human keratinocytes. Lasers
Surg Med. 47:824–832. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ma S, Rao L, Freedberg IM and Blumenberg
M: Transcriptional control of K5, K6, K14, and K17 keratin genes by
AP-1 and NF-kappaB family members. Gene Expr. 6:361–370.
1997.PubMed/NCBI
|
|
31
|
Harijith A, Ebenezer DL and Natarajan V:
Reactive oxygen species at the crossroads of inflammasome and
inflammation. Front Physiol. 5:3522014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liu TF, Vachharajani VT, Yoza BK and
McCall CE: NAD+-dependent sirtuin 1 and 6 proteins
coordinate a switch from glucose to fatty acid oxidation during the
acute inflammatory response. J Biol Chem. 287:25758–25769. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
D'Onofrio N, Servillo L and Balestrieri
ML: SIRT1 and SIRT6 signaling pathways in cardiovascular disease
protection. Antioxid Redox Signal. 28:711–732. 2018. View Article : Google Scholar :
|
|
34
|
Serravallo M, Jagdeo J, Glick SA, Siegel
DM and Brody NI: Sirtuins in dermatology: Applications for future
research and therapeutics. Arch Dermatol Res. 305:269–282. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Xiao C, Wang RH, Lahusen TJ, Park O,
Bertola A, Maruyama T, Reynolds D, Chen Q, Xu X, Young HA, et al:
Progression of chronic liver inflammation and fibrosis driven by
activation of c-JUN signaling in Sirt6 mutant mice. J Biol Chem.
287:41903–41913. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Hirschey MD, Shimazu T, Jing E, Grueter
CA, Collins AM, Aouizerat B, Stančáková A, Goetzman E, Lam MM,
Schwer B, et al: SIRT3 deficiency and mitochondrial protein
hyperacety-lation accelerate the development of the metabolic
syndrome. Mol Cell. 44:177–190. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kiran Z, Zuberi BF, Anis D, Qadeer R,
Hassan K and Afsar S: Insulin resistance in non-diabetic patients
of chronic Hepatitis C. Pak J Med Sci. 29:201–204. 2013.PubMed/NCBI
|
|
38
|
Milčić D, Janković S, Vesić S, Milinković
M, Marinković J, Ćirković A and Janković J: Prevalence of metabolic
syndrome in patients with psoriasis: A hospital-based
cross-sectional study. An Bras Dermatol. 92:46–51. 2017. View Article : Google Scholar
|
|
39
|
Liakou AI and Zouboulis CC: Links and
risks associated with psoriasis and metabolic syndrome. Psoriasis
(Auckl). 5:125–128. 2015.
|
|
40
|
Owczarczyk-Saczonek AB and Nowicki RJ:
Prevalence of cardiovascular disease risk factors, and metabolic
syndrome and its components in patients with psoriasis aged 30 to
49 years. Postepy Dermatol Alergol. 32:290–295. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Blank MF and Grummt I: The seven faces of
SIRT7. Transcription. 8:67–74. 2017. View Article : Google Scholar : PubMed/NCBI
|