Introduction
Male erectile dysfunction (ED) poses a serious
threat to the quality of life, particularly in older men, causing
extreme morbidity among elderly and diabetic patients. ED caused by
diabetes is a refractory symptom. The incidence of diabetes
mellitus-induced ED (DMED) is 19.0-86.3%, which is three times the
rate of ED in non-diabetic patients (1,2).
The mechanism of DMED is not entirely clear, but it is associated
with problems in blood vessels, nerves, neurotransmitters, and the
endocrine system, among others (3-5).
Vascular lesions caused by diabetes may induce atheromatous plaque
formation in the cavernous arteries of the penis, resulting in
reduced blood flow and structural or functional destruction of
arterioles and sinusoidal endothelial cells in the cavernous body,
further affecting erectile function. Phosphodiesterase 5
inhibitors, which are often used to treat ED in the general
population, have almost no therapeutic effect on DMED (6). There is thus a clear need for a new
approach to DMED treatment.
Adipose-derived mesenchymal stem cells (ADSCs) are
multipotent adult stem cells derived from adipose tissue (7). They have the advantages of easy
extraction, simple culture and rapid proliferation, and they have
become an important type of seed cell for use in regenerative
medicine (8). Some scientists
have used ADSCs to treat diabetic varicose veins by reprogramming
them into endothelial cells that promote capillary formation. In
addition, ADSCs have anti-inflammatory properties and can repair
nerve damage (9,10). ADSC transplantation therapy is
widely used to treat diseases such as myocardial ischemia. Studies
have shown that ADSCs can reduce myocardial infarction area,
promote angiogenesis and reverse ischemic injury disruption of
cardiac remodeling (11,12). ADSCs have also been used to treat
a variety of animal models of erectile dysfunction, including DMED
models, penile cavernous nerve injury models, penile induration
models, and penile cavernous radiation injury models (13-16).
Bone marrow mesenchymal stem cells (BMSCs) are a
type of pluripotent stem cells originating from the mesoderm. They
are able to differentiate into bone, cartilage and fat (17). Autologous bone marrow
transplantation can avoid the complications caused by transplant
rejection, but research on and application of this technique are
costly (18). Bivalacqua et
al (19) cultured BMSCs in
vitro, transfected them with angiogenic endothelial nitric
oxide synthase (eNOS), and injected these BMSCs into the corpora
cavernosa of aged male rats. Histological analysis revealed that
BMSCs survived at least 21 days in the corporal tissue and did not
cause an obvious inflammatory response. Studies have demonstrated
that BMSCs can improve erectile function in older rats (20,21). However, BMSCs are difficult to
obtain, and the limited number of available BMSCs cannot meet the
clinical demand.
Selecting the optimal type of stem cells to treat
DMED is crucial. To date, there is little research comparing the
therapeutic effects of ADSCs and BMSCs on diabetic erectile
dysfunction. In the present study, a rat model of diabetes was
established, the rats were treated with ADSCs and BMSCs, and the
therapeutic effects of both types of stem cells in the treatment of
DMED were evaluated.
Materials and methods
Reagents
CD34, CD45, CD73, CD90 and CD105 antibodies were
purchased from BD Biosciences. Streptozotocin, apomorphine (APO)
and vitamin C were purchased from Sigma-Aldrich; Merck KGaA.
Anti-eNOS and β-actin antibodies were purchased from Cell Signaling
Technology, Inc. Modified Lillie-Mayer hematoxylin staining
solution, ethanol eosin staining solution and Sirius Red staining
solution were purchased from Reagan.
Male Sprague-Dawley (SD) rats were provided by
Guangdong Pharmaceutical University. All animal experiments were
approved by the Animal Ethics Committee of Guangdong Pharmaceutical
University.
Isolation and culture of rat ADSCs and
BMSCs
Male 6-week-old SD rats were anesthetized,
sacrificed by cervical dislocation and soaked in iodophor for 2
min, followed by 75% alcohol for 5 min. Following removal of the
epididymal fat, type 1 collagenase was used to digest and separate
ADSCs.
To isolate BMSCs, the femur, tibia, and fibula were
separated, and the medullary cavity was rinsed with 0.9% saline
solution until the rinsing liquid was clear and the bones were
whitish. The rinsing liquid was centrifuged, the supernatant was
discarded, and the serum-containing medium was added to resuspend
cells.
Identification of ADSCs and BMSCs by flow
cytometry
ADSCs and BMSCs were washed once with 0.01 mol/l
phosphate-buffered saline (PBS) and mixed with CD34, CD45, CD73,
CD90 and CD105 monoclonal antibodies at a working concentration of
1:100. The resultant solutions were incubated at 4°C for 30 min and
washed twice with 0.01 mol/l PBS, after which time ADSCs and BMSCs
were detected by flow cytometry.
Establishment and stem cell treatments of
diabetic rat models
After 1 week of adaptive feeding, 40 male SD rats
were randomly divided into two groups (control group, n=10; and
diabetes group, n=30). The rats in the control group (Ctrl) were
provided with a normal diet, while the diabetic rats were fed a
high-fat, high-sugar diet. One month later, the diabetic rats were
intraperitoneally injected with streptozotocin (40 mg/kg) (22). Blood glucose was monitored
starting 3 days after streptozotocin injection. The animals were
considered as diabetic when the glucose levels were >16.7 mM for
3 consecutive days (reference range, 5-8 mM).
The 30 diabetic rats were randomly divided into
three groups (n=10 per group): One group was treated with ADSCs (AD
group), one with BMSCs (BM group), and one with PBS alone (PBS
group).
Injection sera were created by resuspending ADSCs
and BMSCs (1x107 cells) in 1 ml of PBS. Rats were
anesthetized with pentobarbital (50 mg/kg, i.p.), and injected with
the cell suspensions at the mid-penile corpus cavernosum (23). The AD group rats were injected
with 100 µl of ADSC suspension (1x106 cells), the
BM group rats were injected with 100 µl of BMSC suspension,
and animals in the PBS group were injected with 100 µl of
PBS. The control group did not receive any treatment.
APO-induced erection
APO was used to induce penile erections in rats
before and at 4 weeks after stem cell transplantation. The rats
were placed in a dark room under observation, kept calm, and
allowed to adapt to the environment for 10 min. They were then
subcutaneously injected with APO (100 µg/kg) in the back of
the neck, and the number of erections in 30 min was recorded, as
measured by intracavernous pressure (ICP) and mean arterial
pressure (MAP). Healthy 14-week-old rats were used as controls.
Measurement of ICP and MAP
ICP and MAP were measured as previously described
(24). The stimulus parameters
were 20 Hz, a pulse width of 0.2 m sec, 1.5 mA, and a duration of
50 sec. The ratio of maximum ICP (mmHg) to MAP (mmHg) was
calculated to normalize variations in systemic blood pressure.
Immunofluorescence analysis
After the completion of the APO experiment, five
animals from each group were randomly selected, anesthetized and
sacrificed by cervical dislocation. Half of the penile tissue from
each subject (10 µm) was dehydrated in 30% sucrose and then
frozen. After the sections were completely dried,
immunofluorescence staining for eNOS was performed, using the
penile tissue of normal rats as a control. At least five random
fields per section were examined, and the semi-quantitative
evaluations were analyzed with Image-Pro Plus software, version 6.0
(Media Cybernetics, Inc.).
Western blot analysis
The remaining half of the penile tissue from each
subject was combined with an appropriate amount of pre-cooled RIPA
lysis buffer (Fude) and homogenized at 4°C to extract proteins from
the tissue. The extracted proteins were denatured and used to
detect the expression of eNOS by western blotting. The protein
expression levels of β-actin served as the housekeeping control.
Images were captured with Tanon-5200 and quantified using Gel-pro
6.0 software.
Hematoxylin and eosin (H&E) staining
and Sirius Red staining
The remaining 5 animals in each group were
sacrificed by cervical dislocation, and the middle section of
penile tissue was removed. Half of this tissue from each subject
was fixed and dehydrated. Paraffin-embedded sections were stained
with H&E or Sirius Red. The numbers of blood vessels and the
levels of fibrosis in each group were compared. Images were
captured using an Olympus microscope (Olympus Corporation). At
least five random fields per section were examined, and
semi-quantitative evaluations were performed with Image-Pro Plus
software, version 6.0.
Transmission electron microscopy
The remaining half of the penile tissue from each
subject was fixed in 2% glutaraldehyde. The tissue was washed with
PBS, followed by 1% citric acid for 2 h at room temperature. The
tissue was then dehydrated, embedded in paraffin, and cut into
ultrathin sections. After double staining tissue samples with
uranyl acetate and lead citrate, the morphology of endothelial
cells and smooth muscle cells in the cavernous tissue was observed
under a transmission electron microscope.
Statistical analysis
All analyses were performed with the GraphPad Prism
4.0 software (GraphPad Software, Inc.). Data are expressed as the
mean ± standard deviation and then analyzed using one-way ANOVA
followed by Tukey's multiple comparisons test. P-values <0.05
were considered to indicate statistically significant
differences.
Results
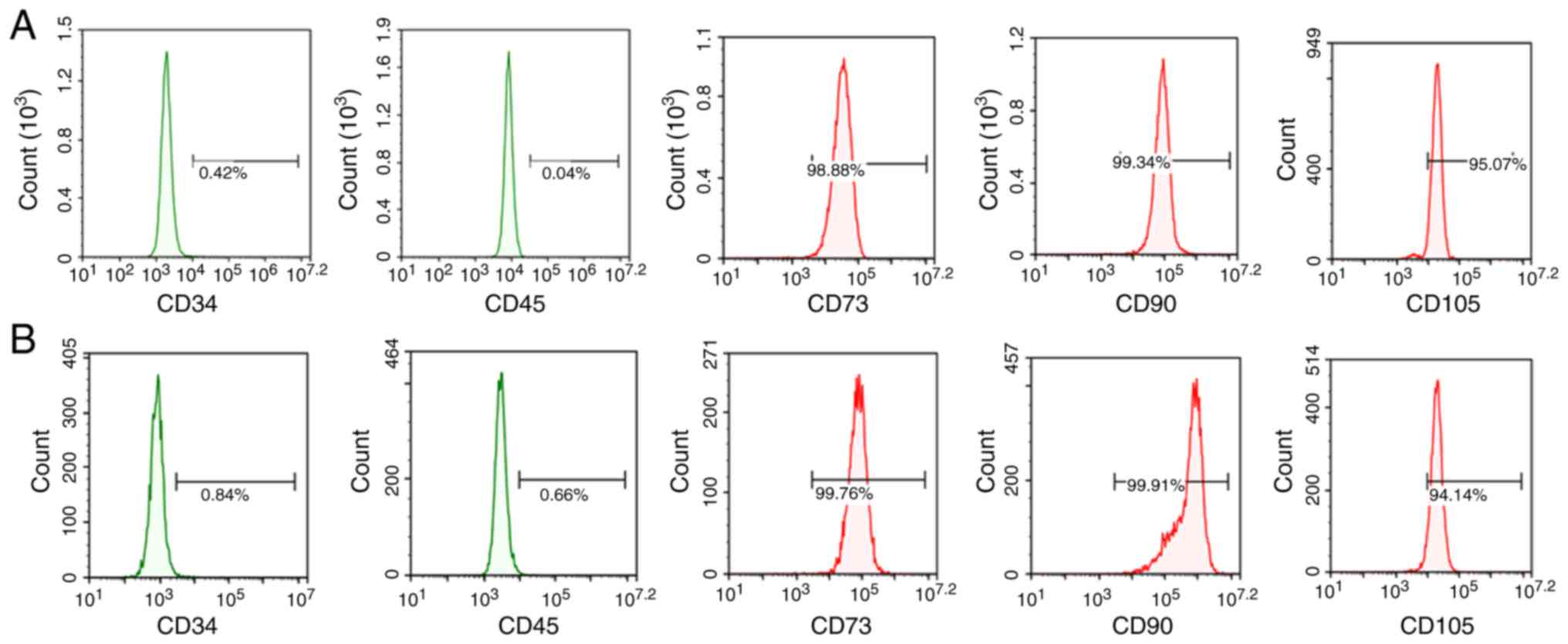
Identification of ADSCs and BMSCs by flow
cytometry
To determine whether the isolated cells were MSCs,
cell surface marker expression was examined. The isolated cells
expressed the known MSC markers CD73, CD90 and CD105, but not the
hematopoietic and endothelial markers CD34 and CD45 (Fig. 1). Flow cytometry results revealed
that the positive rates of CD73, CD90 and CD105 expression in ADSCs
were 98.88, 99.34 and 95.07%, respectively, while the positive
rates of CD34 and CD45 were 0.42 and 0.04%, respectively. The
positive rates of CD73, CD90, and CD105 in BMSCs were 99.76, 99.91
and 94.14%, respectively, and the positive rates of CD34 and CD45
were 0.84 and 0.66%, respectively.
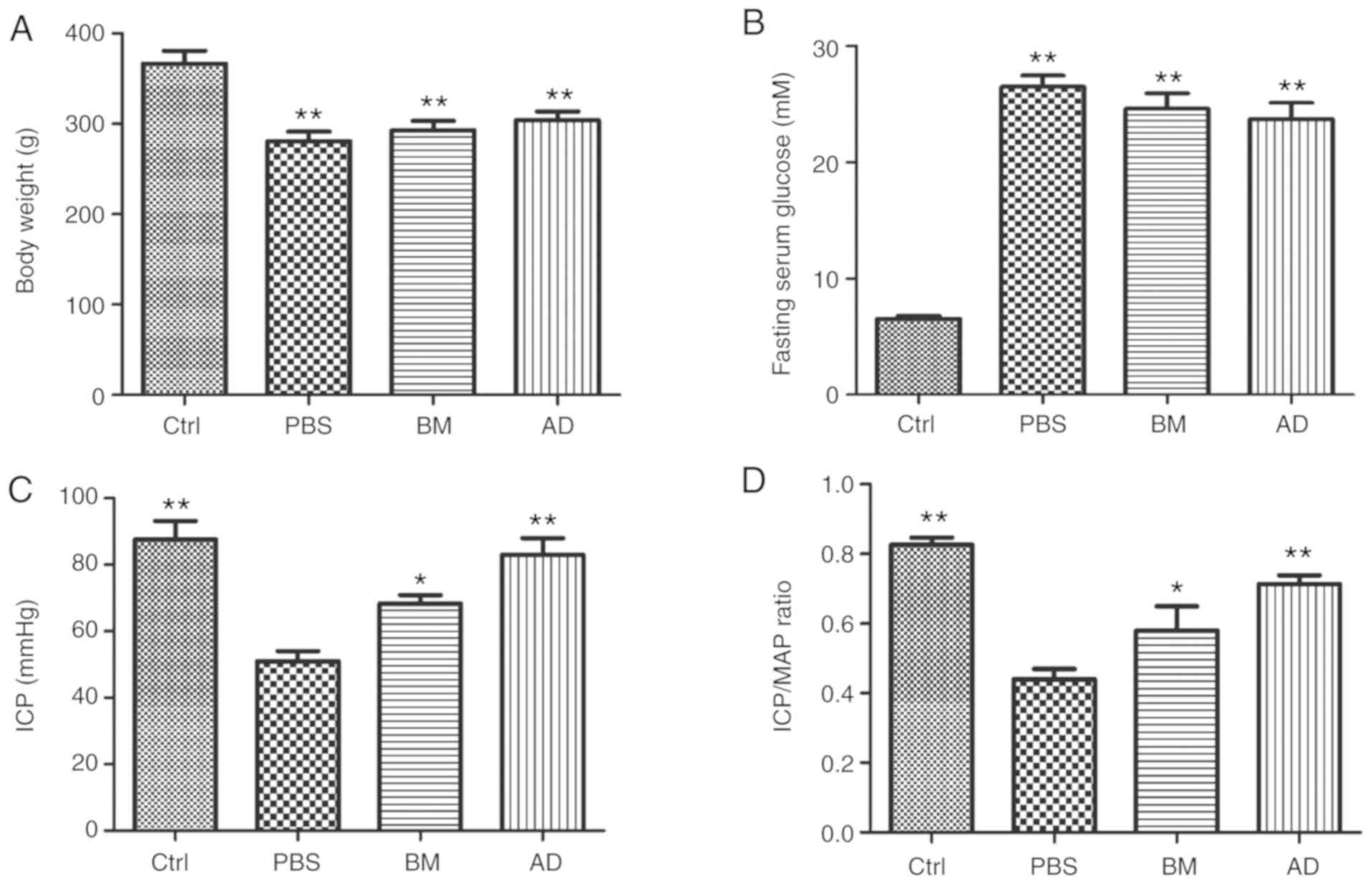
Characteristics of the animals
The mean body weight of the diabetic rats was
significantly lower (P<0.01) compared with that of the normal
and ADSC-treated diabetic rats (Table
I and Fig. 2A). No
significant differences in body weight were observed between the
diabetic and the AD or BM groups. The fasting blood glucose levels
were significantly higher (P<0.01) in diabetic rats compared
with controls (Table I and
Fig. 2B). No significant
differences in blood glucose levels were observed between the
diabetic group and the AD or BM groups.
 | Table ICharacteristic parameters and
functional responses in different treatment groups. |
Table I
Characteristic parameters and
functional responses in different treatment groups.
| Parameters | Groups
|
|---|
| Ctrl | PBS | BM | AD |
|---|
| Body weight
(g) | 366±13 | 280±10a | 292±11 | 304±9 |
| Glucose (mM) | 6.5±0.3 | 26.4±0.9a | 24.6±1.3 | 23.7±1.4 |
| ICP (mm Hg; 7.5
V) | 87±5 | 51±3a | 68±2 | 83±5 |
| ICP/MAP (7.5
V) | 0.82±0.02 | 0.44±0.03a | 0.62±0.01 | 0.71±0.02 |
Effect of ADSCs and BMSCs on erectile
function
The ICP/MAP ratios and total ICP values for all
groups are presented in Fig. 2C
and Table I. The ICP/MAP ratios
of diabetic rats were lower compared with those of normal rats
(P<0.01), a phenomenon that was reversed through treatment with
ADSCs (P<0.01) or BMSCs (P<0.05). The ICP/MAP ratios of
ADSC-treated diabetic rats were higher compared with those of
BMSC-treated diabetic rats. The total ICP values produced by
stimulation of the cavernous nerve were lower in diabetic rats
compared with normal rats (P<0.01), but returned to normal
levels following treatment with ADSCs (P<0.01) or BMSCs
(P<0.05). The total ICP values of ADSC-treated diabetic rats
were higher compared with those of BMSC-treated diabetic rats.
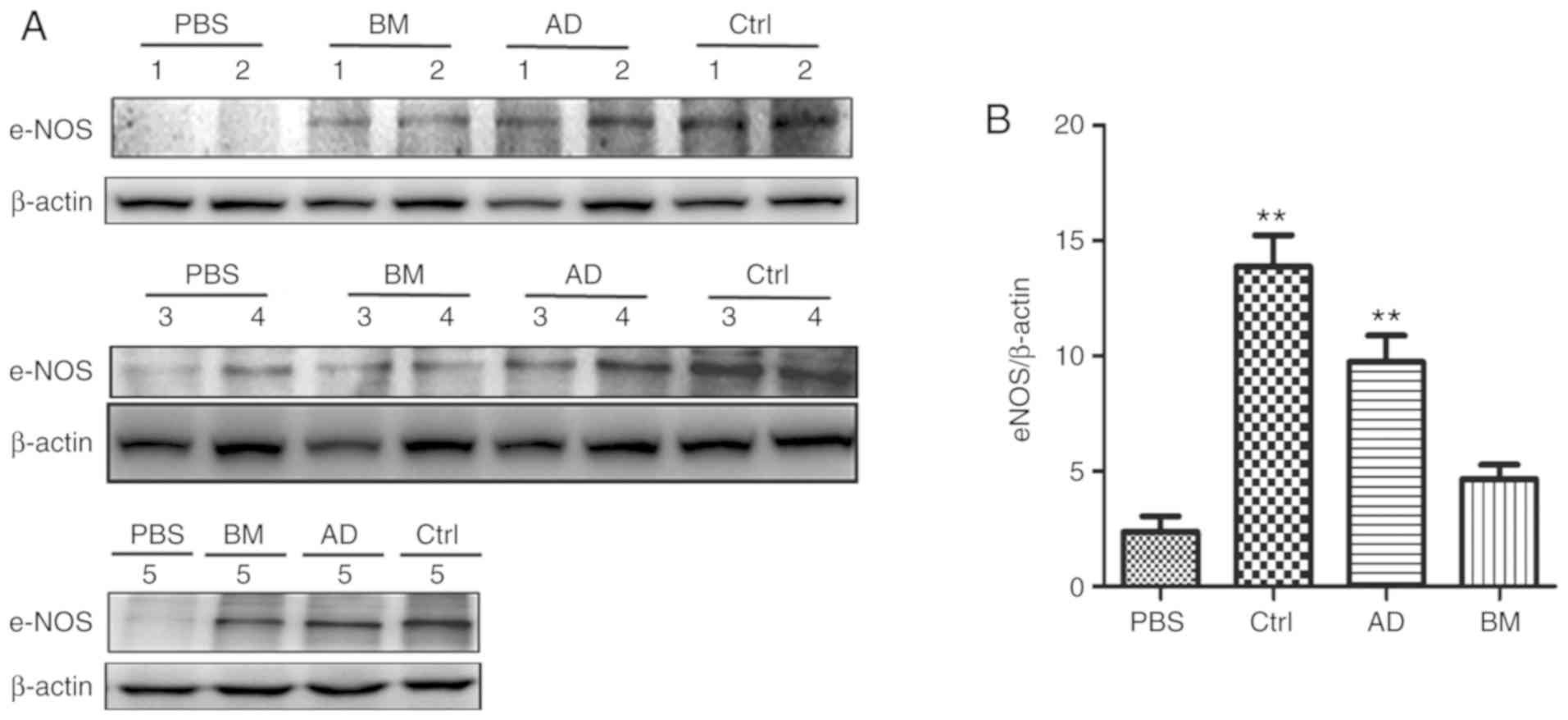
ADSCs improve the expression of eNOS in
the penile tissue of diabetic rats
The expression of eNOS in the penile tissues of the
four groups was determined by western blot analysis. As shown in
Fig. 3, the expression of eNOS
was significantly lower in the diabetic group compared with that in
the control group (P<0.05). The expression of eNOS was higher in
the AD and BM groups compared with that in the diabetic group
(P<0.05), and slightly higher in the AD group compared with that
in the BM group.
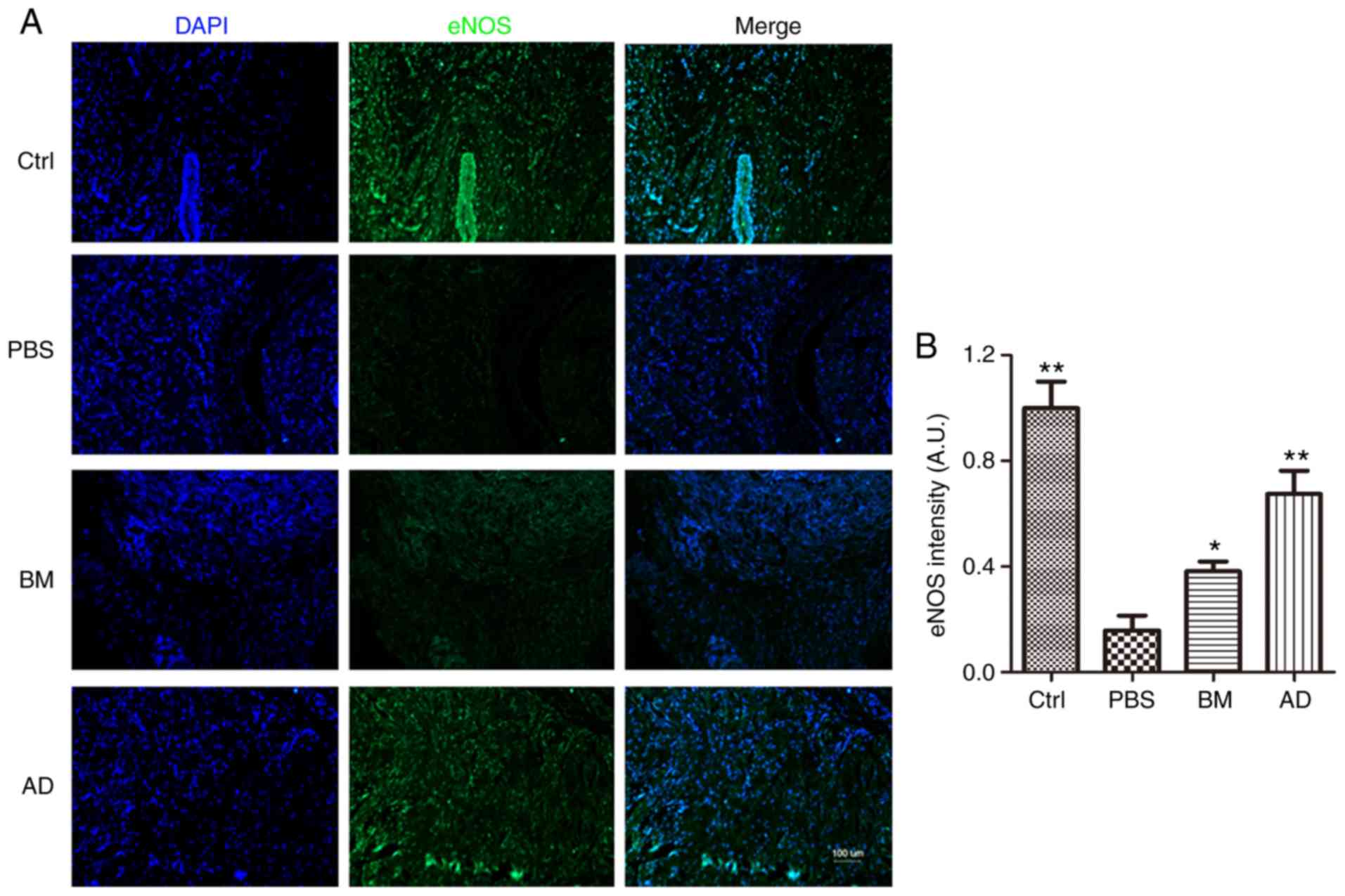
eNOS expression in the penile tissue was also
compared across groups by immunofluorescence analysis, which
yielded results similar to those of western blotting: The
expression of eNOS was significantly lower in the diabetic group
compared with that in the control group (P<0.05), higher in the
AD and BM groups compared with that in diabetic rats (P<0.05),
and slightly higher in ADSC-treated rats compared with BMSC-treated
rats (Fig. 4).
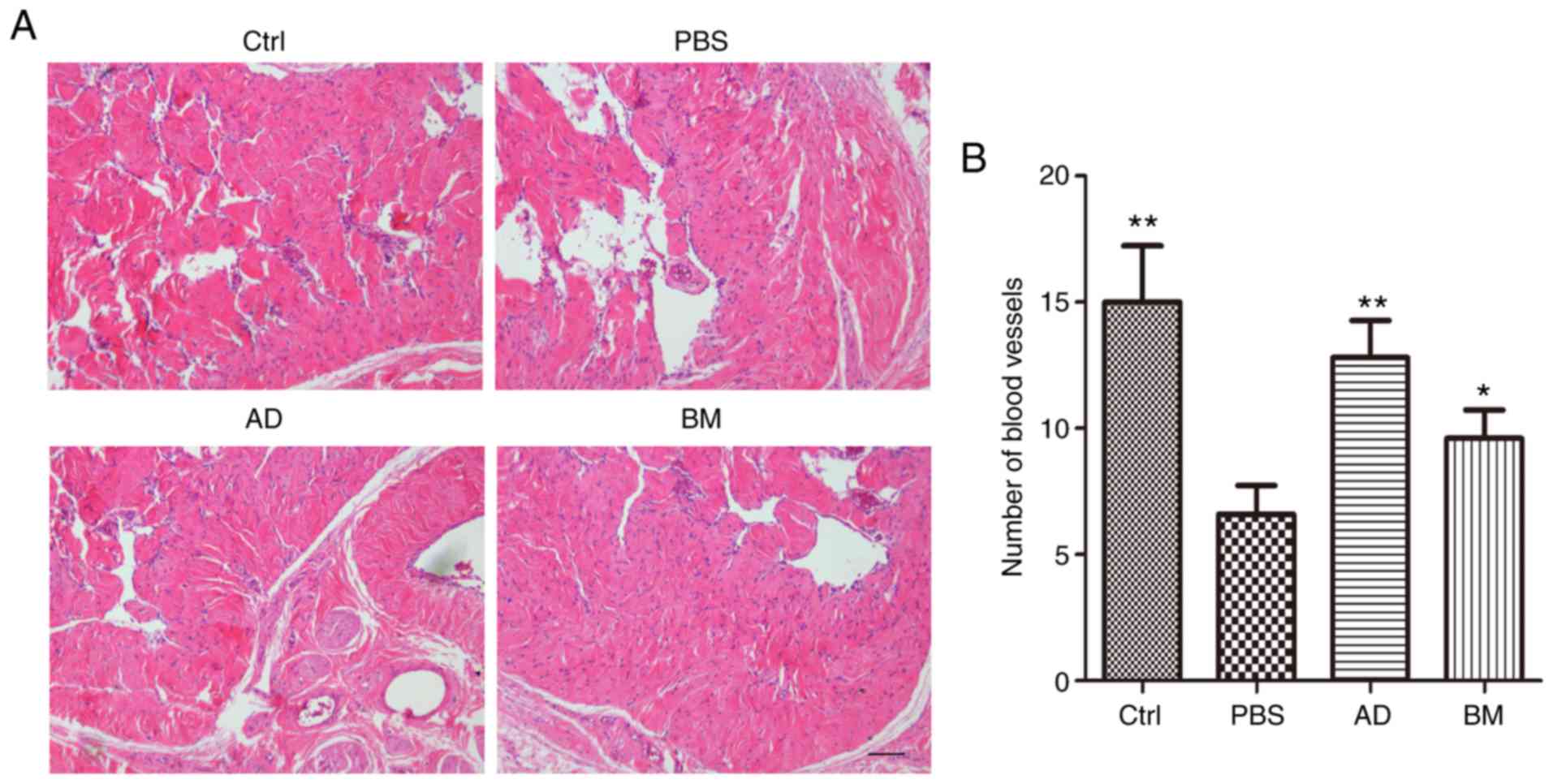
ADSC treatment promotes revascularization
in the corpus cavernosum of diabetic rats
H&E staining was used to observe the number of
blood vessels in the corpus cavernosum. As shown in Fig. 5, diabetic rats had significantly
fewer blood vessels compared with healthy controls (P<0.01).
This effect was reversed by treatment with ADSCs (P<0.01) or
BMSCs (P<0.05). The number of blood vessels in ADSC-treated
diabetic rats was higher compared with that in BMSC-treated
diabetic rats.
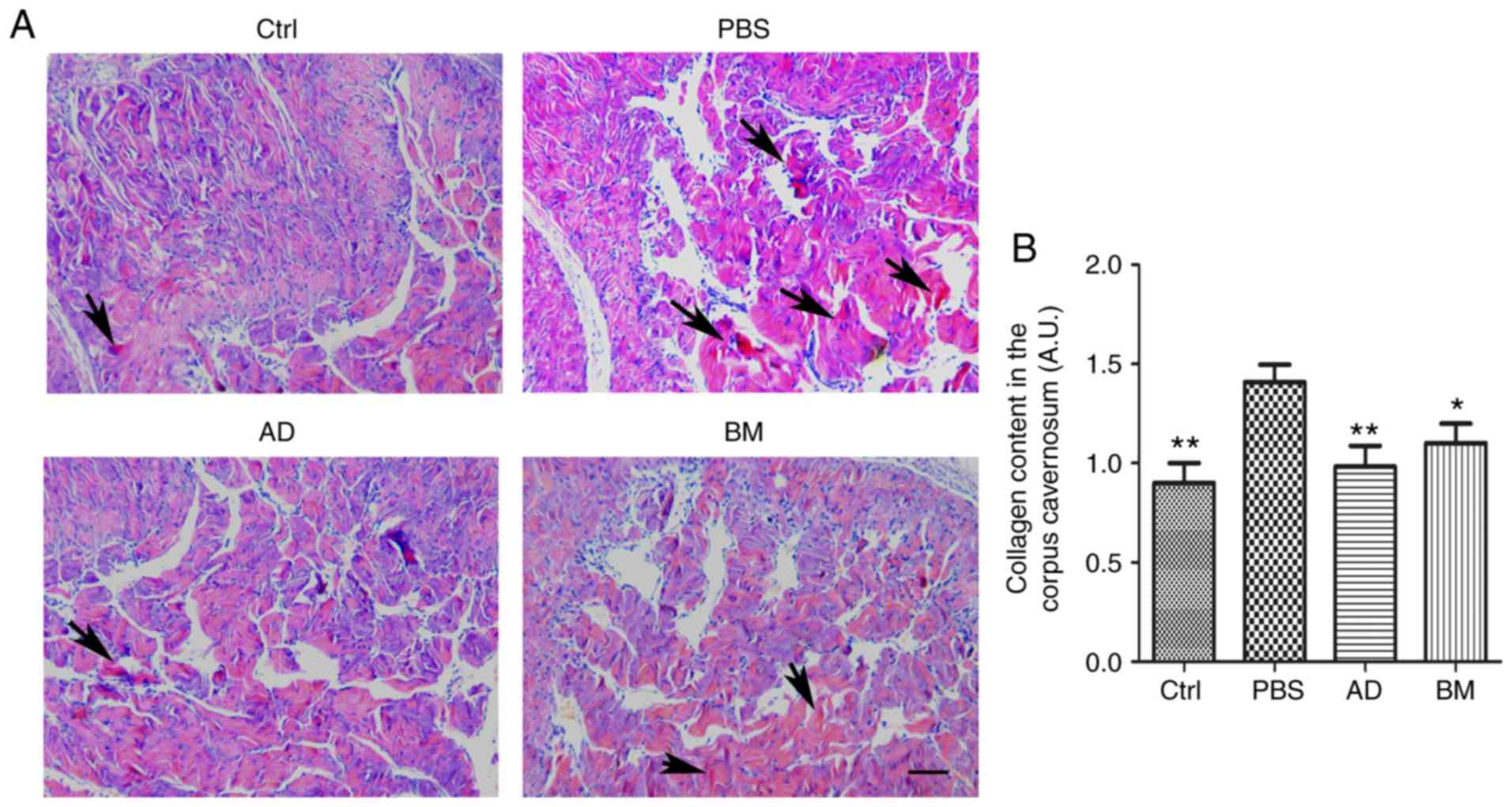
ADSC treatment reduces collagen content
in the corpus cavernosum of diabetic rats
Collagen fiber content in the penile tissue of
diabetic rats was investigated using Sirius Red staining. As shown
in Fig. 6, the penile tissue of
diabetic rats exhibited a significantly increased collagen content,
which was reversed by treatment with ADSCs (P<0.01) or BMSCs
(P<0.05). The collagen fiber content in ADSC-treated diabetic
rats was lower compared with that in BMSC-treated diabetic
rats.
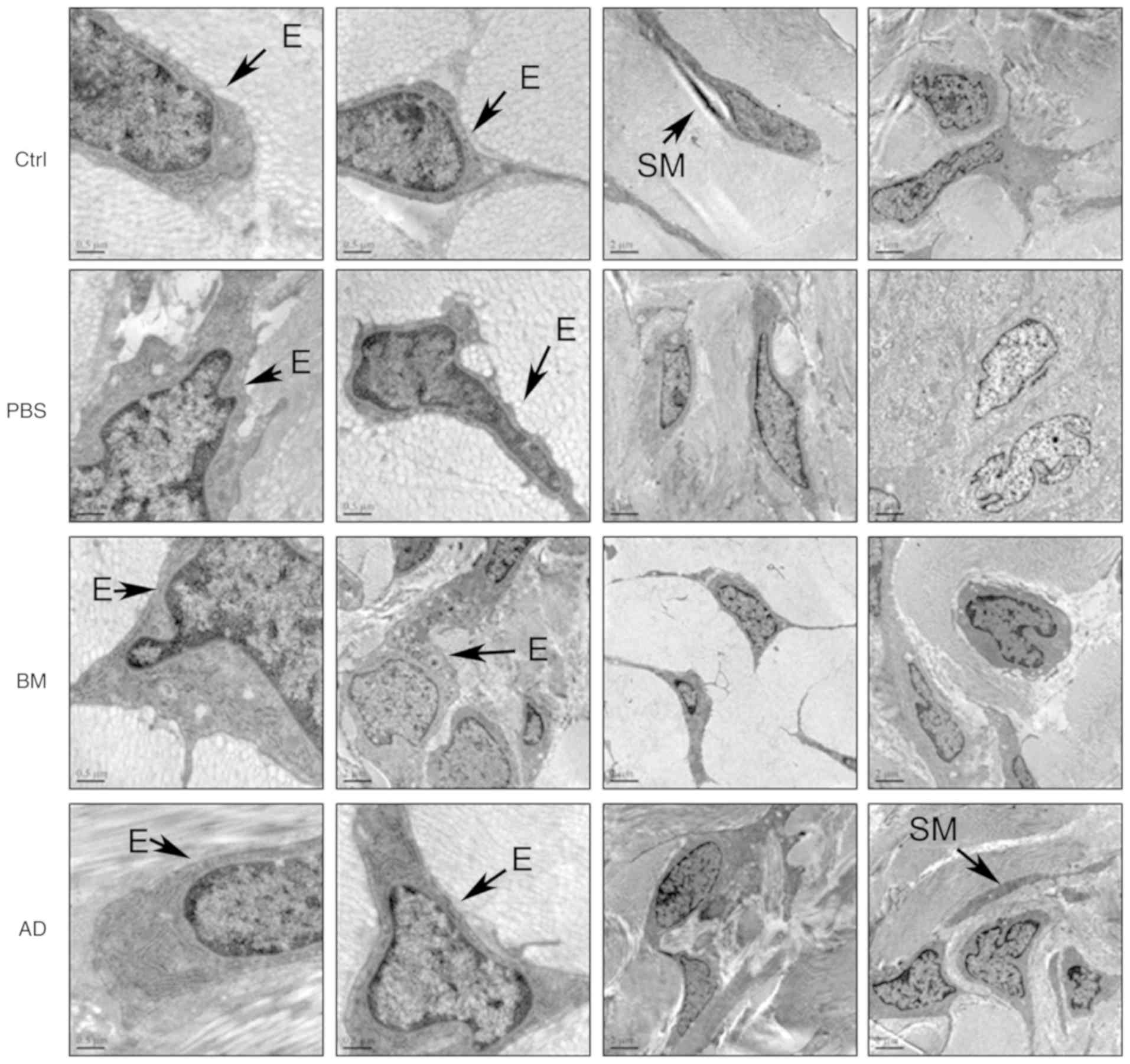
ADSC treatment ameliorates cell
impairment in penile tissue, as observed on transmission electron
microscopy
The ultrastructural characteristics of penile tissue
cells were observed by transmission electron microscopy. In the
corpora cavernosa of diabetic rats, endothelial cells and smooth
muscle cells were damaged (Fig.
7), with injuries to the plasma membrane, concentrated
cytoplasm and condensed nuclei. Stem cell treatment ameliorated
cellular impairments induced by diabetes; this effect was more
obvious in the ADSC-treated group compared with that in the
BMSC-treated group.
Discussion
There have been major advances in ED research over
the past decade (25), but DMED
remains difficult to treat. Stem cell therapy has been proposed as
a viable treatment strategy, and some clinical and preclinical
trials have been conducted in a few related areas (26,27). A small number of studies have
examined the use of ADSCs and BMSCs in the treatment of DMED
(28-30) but, to the best of our knowledge,
there is currently no report comparing the effects of ADSCs and
BMSCs on DMED. Therefore, in the present study, a diabetic rat
model was established by streptozocin induction, and ADSCs and
BMSCs were transplanted into the penile tissue. The effects of ADSC
and BMSC treatment were then compared, and the mechanism of action
of each type of stem cell was investigated.
ADSCs and BMSCs were successfully isolated, cultured
in vitro, and their identity was confirmed by flow
cytometry. Diabetic rats were treated with ADSCs and BMSCs, and
their erectile function following treatment was determined by their
ICP/MAP ratio. The results demonstrated that ADSC treatment
restored the erectile function of diabetic rats.
Several studies have reported that ED is induced by
inadequate relaxation of the corpus cavernosum with defects in NO
production (31). NO is formed
from the conversion of L-arginine by NOS, which exists in three
isoforms: Endothelial (eNOS), neuronal (nNOS), and inducible
(iNOS). eNOS expression has been identified both in the cavernosal
endothelium and in smooth muscle cells (32). Endothelium-generated NO appears to
be crucial for maintaining an erection (33). Therefore, in the present study,
the expression of eNOS in the penile tissues was examined.
According to both western blot and immunofluorescence analyses,
ADSC treatment increased the expression of eNOS in diabetic rats,
and eNOS expression was slightly higher in the ADSC-treated group
compared with that in the BMSC group. Accordingly, H&E staining
revealed that ADSC treatment increased the number of blood vessels
in the penile tissue of diabetic rats. These findings suggest that
ADSC treatment was more effective compared with BMSC treatment in
promoting revascularization of the corpus cavernosum in diabetic
rats.
In addition, the ultrastructural characteristics of
endothelial and smooth muscle cells in each group were observed
under a transmission electron microscope. Cellular morphological
characteristics suggested that ADSCs were more effective compared
with BMSCs in ameliorating diabetes-induced impairment of
endothelial and smooth muscle cells in penile tissue.
A mounting number of studies have demonstrated that
ADSC treatment can promote revascularization, which suggests that
ADSCs are a promising approach to the treatment of diseases such as
critical limb ischemia (11),
ischemic cardiomyopathy (34) and
myocardial infarction (35).
ADSCs are adult stem cells isolated from adipose tissue that are
capable of self-renewal and multi-directional differentiation
(36). They have low
immunogenicity and can be easily collected with minimal risk. In
the field of regenerative medicine, ADSCs are widely used in tissue
repair and regeneration. All these characteristics make ADSCs the
most suitable type of stem cell for use in the treatment of ED
(37). ADSC transplantation has
achieved encouraging results in multiple ED models, including DMED
(38,39). There is increasing evidence that
the therapeutic effects of ADSCs on ED may be mediated through
paracrine indirect effects of growth factors or cytokines, rather
than by direct differentiation into specific cell types (40), a subject which requires further
study.
Several studies have indicated that BMSC treatment
may also promote revascularization (41,42). However, in the present study,
ADSCs promoted angiogenesis more effectively compared with BMSCs,
which is consistent with the earlier findings of Wu et al
(43). To the best of our
knowledge, this is the first study to directly compare the
therapeutic effects of ADSCs and BMSCs on ED in diabetic rats.
However, this was a preliminary study that mainly
focuses on comparing the therapeutic effects of ADSCs and BMSCs on
DMED. On this basis, more in-depth mechanism research is still
needed, and experiments for protein or non-coding RNA are required
as the next step.
In conclusion, treatment with ADSCs significantly
restored erectile function in diabetic rats by improving eNOS
expression, promoting revascularization, and reversing cellular
functional impairment. ADSC treatment was found to be more
effective compared with BMSC treatment in restoring erectile
function in diabetic rats. These findings may provide a new
approach to the treatment of DMED.
Funding
The authors would like to thank the Guangdong
Province Science and Technology Fund (grant. no. 2017ZC0208) for
their financial support.
Availability of materials and data
All the datasets generated and analyzed in the
present study are available from the corresponding author on
reasonable request.
Authors' contributions
XC, YW and XY conceived and designed the study. SC,
JZ and MW conducted the experiments. YH, ZQ, HC, MX, XC, JJL and MS
participated in the completion of the experiments. JL and HL
analyzed the data. SC wrote the manuscript. XC, YW and XY revised
the manuscript. All the authors have read and approved the final
version of this manuscript for publication.
Ethics approval and consent to
participate
All animal experiments were approved by the Animal
Ethics Committee of Guangdong Pharmaceutical University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Acknowledgments
Not applicable.
References
|
1
|
Jangir RN and Jain GC: Diabetes mellitus
induced impairment of male reproductive functions: A review. Curr
Diabetes Rev. 10:147–157. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tamás V and Kempler P: Sexual dysfunction
in diabetes. Handb Clin Neurol. 126:223–232. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sun X, Luo LH, Feng L and Li DS:
Down-regulation of lncRNA MEG-3 promotes endothelial
differentiation of bone marrow derived mesenchymal stem cells in
repairing erectile dysfunction. Life Sci. 208:246–252. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hu LL, Zhang KQ, Tian T, Zhang H and Fu Q:
Probucol improves erectile function via Activation of Nrf2 and
coordinates the HO-1 / DDAH / PPAR-γ/ eNOS pathways in
streptozotocin-induced diabetic rats. Biochem Biophys Res Commun.
507:9–14. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wu Y, Yang C, Meng F, Que F, Xiao W, Rao
H, Wan Y, Taylor HS and Lu L: Nerve growth factor improves the
outcome of type 2 diabetes-induced hypotestosteronemia and erectile
dysfunction. Reprod Sci. 26:386–393. 2019. View Article : Google Scholar
|
|
6
|
Shamloul R and Ghanem H: Erectile
dysfunction. Lancet. 381:153–65. 2013. View Article : Google Scholar
|
|
7
|
Xu X, Li L, Wang C, Liu Y, Chen C, Yan J,
Ding H and Tang SY: The expansion of autologous adipose-derived
stem cells in vitro for the functional reconstruction of nasal
mucosal tissue. Cell Biosci. 5:542015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen S, Wang M, Chen X, Chen S, Liu L, Zhu
J, Wang J, Yang X and Cai X: In vitro expression of Cytokeratin 19
in adipose-derived stem cells is induced by epidermal growth
factor. Med Sci Monit. 24:4254–4261. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu YP, Li SZ, Yuan F, Xia J, Yu X, Liu X
and Yu GR: Infrapatellar fat pad may be with tendon repairing
ability and closely related with the developing process of patella
Baja. Med Hypotheses. 77:620–623. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gadelkarim M, Abushouk AI, Ghanem E,
Hamaad AM, Saad AM and Abdel-Daim MM: Adipose-derived stem cells:
Effectiveness and advances in delivery in diabetic wound healing.
Biomed Pharmacother. 107:625–633. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu J, Zhu P, Song P, Xiong W, Chen H,
Peng W, Wang S, Li S, Fu Z, Wang Y and Wang H: Pretreatment of
adipose derived stem cells with curcumin facilitates myocardial
recovery via antiapoptosis and angiogenesis. Stem Cells Int.
2015:6381532015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Burchfield JS, Paul AL, Lanka V, Tan W,
Kong Y, McCallister C, Rothermel BA, Schneider JW, Gillette TG and
Hill JA: Pharmacological priming of adipose-derived stem cells
promotes myocardial repair. J Investig Med. 64:50–62. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fandel TM, Albersen M, Lin G, Qiu X, Ning
H, Banie L, Lue TF and Lin CS: Recruitment of intracavernously
injected adipose-derived stem cells to the major pelvic ganglion
improves erectile function in a rat model of cavernous nerve
injury. Eur Urol. 61:201–210. 2012. View Article : Google Scholar
|
|
14
|
Qiu X, Villalta J, Ferretti L, Fandel TM,
Albersen M, Lin G, Dai Y, Lue TF and Lin CS: Effects of intravenous
injection of adipose-derived stem cells in a rat model of radiation
therapy-induced erectile dysfunction. J Sex Med. 9:1834–1841. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Garcia MM, Fandel TM, Lin G, Shindel AW,
Banie L, Lin CS and Lue TF: Treatment of erectile dysfunction in
the obese type 2 diabetic ZDF rat with adipose tissue-derived stem
cells. J Sex Med. 7:89–98. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gokce A, Abd Elmageed ZY, Lasker GF,
Bouljihad M, Kim H, Trost LW, Kadowitz PJ, Abdel-Mageed AB, Sikka
SC and Hellstrom WJ: Adipose tissue-derived stem cell therapy for
prevention and treatment of erectile dysfunction in a rat model of
Peyronie's disease. Andrology. 2:244–251. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Singh A, Lee D, Sopko N, Matsui H,
Sabnekar P, Liu X, Elisseeff J, Schoenberg MP, Pienta K and
Bivalacqua TJ: Biomanufacturing seamless tubular and hollow
collagen scaffolds with unique design features and biomechanical
properties. Adv Healthc Mater. 6:2017. View Article : Google Scholar
|
|
18
|
Abdel-Latif A, Bolli R, Tleyjeh IM,
Montori VM, Perin EC, Hornung CA, Zuba-Surma EK, Al-Mallah M and
Dawn B: Adult bone marrow-derived cells for cardiac repair: A
systematic review and meta-analysis. Arch Intern Med. 167:989–997.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bivalacqua TJ, Deng W, Kendirci M, Usta
MF, Robinson C, Taylor BK, Murthy SN, Champion HC, Hellstrom WJ and
Kadowitz PJ: Mesenchymal stem cells alone or ex vivo gene modified
with endothelial nitric oxide synthase reverse age-associated
erectile dysfunction. Am J Physiol Heart Circ Physiol.
292:H1278–H1290. 2007. View Article : Google Scholar
|
|
20
|
Ryu JK, Kim DH, Song KM, Yi T, Suh JK and
Song SU: Intracavernous delivery of clonal mesenchymal stem cells
restores erectile function in a mouse model of cavernous nerve
injury. J Sex Med. 11:411–423. 2014. View Article : Google Scholar
|
|
21
|
Ryu JK, Kim DH, Song KM, Ryu DS, Kim SN,
Shin DH, Yi T, Suh JK and Song SU: Intracavernous delivery of
clonal mesenchymal stem cells rescues erectile function in the
streptozotocin-induced diabetic mouse. Andrology. 4:172–184. 2016.
View Article : Google Scholar
|
|
22
|
Cai X, Li J, Wang M, She M, Tang Y, Li J,
Li H and Hui H: GLP-1 treatment improves diabetic retinopathy by
alleviating autophagy through GLP- 1R ERK1/2 HDAC6 signaling
pathway. Int J Med Sci. 14:1203–1212. 2017. View Article : Google Scholar :
|
|
23
|
Liu G, Sun X, Bian J, Wu R, Guan X, Ouyang
B, Huang Y, Xiao H, Luo D, Atala A, et al: Correction of diabetic
erectile dysfunction with adipose derived stem cells modified with
the vascular endothelial growth factor gene in a rodent diabetic
model. PLoS One. 8:pp. e727902013, View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xu Y, Guan R, Lei H, Li H, Wang L, Gao Z,
Song W and Xin Z: Therapeutic potential of adipose-derived stem
cells-based micro-tissues in a rat model of postprostatectomy
erectile dysfunction. J Sex Med. 11:2439–2448. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Decaluwé K, Pauwels B, Boydens C and Van
de Voorde J: Treatment of erectile dysfunction: New targets and
strategies from recent research. Pharmacol Biochem Behav.
121:146–157. 2014. View Article : Google Scholar
|
|
26
|
Zhou F, Hui Y, Xin H, Xu YD, Lei HE, Yang
BC, Guan RL, Li M, Hou JQ and Xin ZC: Therapeutic effects of
adipose-derived stem cells-based microtissues on erectile
dysfunction in streptozotocin-induced diabetic rats. Asian J
Androl. 19:91–97. 2017.
|
|
27
|
Hou QL, Ge MY, Zhang CD, Tian DD, Wang LK,
Tian HZ, Wang WH and Zhang WD: Adipose tissue-derived stem cell
therapy for erectile dysfunction in rats: A systematic review and
meta-analysis. Int Urol Nephrol. 49:1127–1137. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen F, Zhang H, Wang Z, Ding W, Zeng Q,
Liu W, Huang C, He S and Wei A: Adipose-derived stem cell-derived
exosomes ameliorate erectile dysfunction in a rat model of type 2
Diabetes. J Sex Med. 14:1084–1094. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mangır N and Türkeri L: Stem cell
therapies in post-prostatectomy erectile dysfunction: A critical
review. Can J Urol. 24:8609–8619. 2017.
|
|
30
|
Shan HT, Zhang HB, Chen WT, Chen FZ, Wang
T, Luo JT, Yue M, Lin JH and Wei AY: Combination of low-energy
shock-wave therapy and bone marrow mesenchymal stem cell
transplantation to improve the erectile function of diabetic rats.
Asian J Androl. 19:26–33. 2017.
|
|
31
|
Azadzoi KM, Goldstein I, Siroky MB, Traish
AM, Krane RJ and Saenz de Tejada I: Mechanisms of ischemia-induced
cavernosal smooth muscle relaxation impairment in a rabbit model of
vasculogenic erectile dysfunction. J Urol. 160:2216–2222. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Burnett AL, Lowenstein CJ, Bredt DS, Chang
TS and Snyder SH: Nitric oxide: A physiologic mediator of penile
erection. Science. 257:401–403. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Andersson KE: Erectile physiological and
pathophysiological pathways involved in erectile dysfunction. J
Urol. 170:S6–S13. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Procházka V, Jurčíková J, Laššák O,
Vítková K, Pavliska L, Porubová L, Buszman PP, Krauze A, Fernandez
C, Jalůvka F, et al: Therapeutic potential of adipose-derived
therapeutic factor concentrate for treating critical limb ischemia.
Cell Transplant. 25:1623–1633. 2016. View Article : Google Scholar
|
|
35
|
Mazo M, Hernández S, Gavira JJ, Abizanda
G, Araña M, López-Martínez T, Moreno C, Merino J, Martino-Rodríguez
A, Uixeira A, et al: Treatment of reperfused ischemia with
adipose-derived stem cells in a preclinical Swine model of
myocardial infarction. Cell Transplant. 21:2723–2733. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Salibian AA, Widgerow AD, Abrouk M and
Evans GR: Stem cells in plastic surgery: A review of current
clinical and translational applications. Arch Plast Surg.
40:666–675. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li M, Li H, Ruan Y, Wang T and Liu J: Stem
cell therapy for diabetic erectile dysfunction in rats: A
meta-analysis. PLoS One. 11:pp. e01543412016, View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wang X, Liu C, Li S, Xu Y, Chen P, Liu Y,
Ding Q, Wahafu W, Hong B and Yang M: Hypoxia precondition promotes
adipose-derived mesenchymal stem cells based repair of diabetic
erectile dysfunction via augmenting angiogenesis and
neuroprotection. PLoS One. 10:pp. e01189512015, View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Liu T, Peng Y, Jia C, Fang X, Li J and
Zhong W: Hepatocyte growth factor-modified adipose tissue-derived
stem cells improve erectile function in streptozotocin-induced
diabetic rats. Growth Factors. 33:282–289. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Albersen M, Weyne E and Bivalacqua TJ:
Stem cell therapy for erectile dysfunction: Progress and future
directions. Sex Med Rev. 1:50–64. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Liu Y, Yang X, Maureira P, Falanga A,
Marie V, Gauchotte G, Poussier S, Groubatch F, Marie PY and Tran N:
Permanently hypoxic cell culture yields rat bone marrow mesenchymal
cells with higher therapeutic potential in the treatment of chronic
myocardial infarction. Cell Physiol Biochem. 44:1064–1077. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ju X, Xue D, Wang T, Ge B, Zhang Y and Li
Z: Catalpol promotes the survival and VEGF secretion of bone
marrow-derived stem cells and their role in myocardial repair after
myocardial infarction in rats. Cardiovasc Toxicol. 18:471–481.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wu H, Li JZ, Xie BD, Tian H, Fang SH,
Jiang SL and Kang K: Lower senescence of adipose-derived stem cells
than donor-matched bone marrow stem cells for surgical ventricular
restoration. Stem Cells Dev. 27:612–623. 2018. View Article : Google Scholar : PubMed/NCBI
|