Introduction
Cardiovascular diseases (CVDs) represent the major
causes of mortality worldwide ranging to 17.3 million of deaths per
year, although in more progressed countries a consistent and
progressive decline is witnessed (1). However, both coronary artery disease
and cerebrovascular disease remain the two main causes of death
with 1.8 and 1.0 million per year respectively (2). Atherosclerotic clinical symptoms are
preceded by the so-called subclinical atherosclerosis, an early
stage without clinical evidence. It is crucial to evaluate the
subclinical condition to achieve a better clinical outcome of
patients. Inflammation plays a pivotal role for starting and
progressing of atherosclerosis disease. High sensitive C-reactive
protein (hsCRP) stimulates and increases phagocytosis and
chemotaxis. Elevated levels of hsCRP represent a risk marker for
potential atherosclerotic plaque instability in patients with
coronary artery disease (3,4).
It is known that fibrinogen (F) is associated with incremental risk
of coronary artery disease. Subjects with high plasma level of F
have a 3-fold increase of global cardiovascular disease (5). Furthermore, homocysteine, leptin,
adiponectin, tumor necrosis factor alfa (TNF-α), interleukin-1
(IL-1) and interleukin-6 (IL-6) act in determining both higher
prevalence and severity of CVDs (6,7).
Platelet-to-lymphocyte ratio (PLR), neutrophil-to-lymphocyte ratio
(NLR) and monocyt-to-HDL cholesterol ratio (MHR) have been widely
studied as markers of inflammation, and they may be considered as
simply and helpful biomarkers available with routinely blood tests
(8-10). PLR is the ratio between absolute
count of platelets (tiny blood cells related to thrombotic events)
and lymphocytes (a decrease in lymphocyte count is associated to
generalized stress). NLR is calculated by dividing the number of
neutrophils (notoriously increased in inflammatory events) by
number of lymphocytes and is used as a marker of subclinical
inflammation. The utility of MHR is related to an evaluation of
inflammatory state (monocytes absolute count) and to
HDL-cholesterol, a well-known cardiovascular protecting factor.
Both NLR and PLR were considered to be linked to the severity and
progression of peripheral arterial disease (PAD) in general
population (11,12). There are limited data examining
the role of these two markers in elderly patients and also the
predictive value of MHR in PAD. In the present study we determined
the association between PLR, NLR, MHR with PAD. PAD was diagnosed
by measuring the ankle brachial index (ABI).
Materials and methods
Study population
We consecutively screened 300 subjects aged over 70
years, without manifest concomitant atherosclerotic disease,
hospitalized from July 1, 2015 to December 31, 2018, in the
geriatric Department, ARNAS garibaldi, Catania. Patients were
informed on research, they were asked to give their verbal informed
consent. Verbal informed consent was obtained from all patients.
The study was conducted acording to the ethical guidelines of the
1975 Declaration of Helsinki. To avoid confounding data, we
excluded patients with malignancies, inflammatory disease,
autoimmune disease, hematologic disease, hepatic insufficiency,
chronic kidney disease, acute coronary syndrome, severe
consequences of type 2 diabetes, and patients who had received
immunosuppressive drugs or corticosteroids in the previous three
months. Gender, age, weight, body mass index (BMI), and
cardiovascular risk factors (diabetes, arterial hypertension,
smoke, dyslipidaemia) were recorded. The diagnosis of diabetes was
made according to the criteria of American Diabetes Association
(13). Hypertension and
dyslipidaemia were diagnosed according to the seventh report of the
Joint National Committee on prevention, detection, evaluation, and
treatment of high blood pressure (JNC 7) and guideline of the
National Cholesterol Education Program (ATP III), respectively
(14,15). BMI was calculated using the
formula of weight/height2 (kg/m2). Blood
pressure was measured manually on the non-dominant arm in a seated
position after a 10-min rest.
Clinical and biochemical assessments
Blood samples were collected when patients were
admitted to the hospital division. Complete blood count, serum
glucose, blood urea nitrogen, creatinine, total cholesterol,
low-density lipoprotein-cholesterol (LDL-C), high-density
lipoprotein cholesterol (HDL-C), triglycerides, high sensitive
hsCRP, erythrocytes sedimentation rate (ESR), and F were assessed.
Cell count was performed by flow cytometry; in particular PLR was
calculated by platelets counts (×103/l)/total lymphocyte
counts (×103/l). NLR was calculated by neutrophil counts
(×103/l)/total lymphocyte count (×103/l). MHR
was calculated by monocyte counts (×103/l)/HDL-C
(mg/dl).
ABI measurement
ABI measurements were performed using a B-mode
tomographic ultrasound system (Esaote Mylab 5) with a linear 7-12
MHz transducer and measuring systolic blood pressure in
non-dominant arm brachial, posterior and anterior tibial arteries.
The ABI was calculated as the ratio of the ankle (lower value
between posterior and anterior tibial artery) and brachial
(brachial artery) systolic blood pressure. ABI is considered as
normal in a range between 1 and 1.4. The ABI value ≤0.9 is used to
diagnose the low-extremity artery disease (LEAD), as a marker of
lower extremity artery stenosis (>50% stenosis). ABI values
ranging from 0.90 to 0.99 are considered 'borderline', while values
higher than 1.4 indicate non-compressible arteries (16). Patients were divided into four
groups, according to the ABI values: ≤0.9 (g1); 0.9-0.99 (g2);
1-1.4 (g3) and >1.4 (g4).
Statistical analysis
Continuous variables were presented as mean ±
standard deviation (SD) and categorical data were summarized as
frequencies (percentage). For more than two level variables,
analysis by ANOVA test, followed by post hoc (Tukey) were
performed. Differences among groups were analysed by non-parametric
Wilcoxon test.
For continuous variables, correlation was evaluated
with simply linear univariate, Pearson's correlation method (ρ) and
multivariate regression (included age, history of hypertension,
smoking, diabetes mellitus, dyslipidaemia, high sensitive hsCRP,
ESR, and F. P-value <0.05 was considered statistically
significant. Statistical analysis was performed by using 'R'
software.
Results
A total of 300 patients, 132 men (44%) and 168 women
(56%) were analysed in the study. Mean age was 81.2 (±6.9) years.
Among these subjects, 167 (56%) were affected by arterial
hypertension, 92 (31%) by type 2 diabetes, 141 (47%) by
dyslipidaemia and 85 (28.3%) were smokers. The mean and SD of PLR,
NLR and MHR were, respectively, 184.92 (±70.84), 3.91 (±2.15) and
26.39 (±19.38). The demographic, clinical and laboratory
characteristics and PLR, NLR, MHR means with SD of four groups
(g1-g4) are summarized in Table
I.
 | Table IBaseline clinical and laboratory
findings reported as mean and standard deviation (SD). |
Table I
Baseline clinical and laboratory
findings reported as mean and standard deviation (SD).
| Baseline
characteristics | Mean ± SD |
|---|
| Age (years) | 81.2±6.9 |
| Sex | F 168 (56%); |
| M 132 (44%) |
| Weight (MHz) | 71.9±12.2 |
| Height (cm) | 161.2±8.1 |
| Body mass index - BMI
(kg/m2) | 28±5 |
| Abdominal
circumference (cm) | 97±13 |
| Cardiovascular (CV)
risk factors | |
| Arterial
hypertension | 167 (56%) |
| Diabetes
mellitus | 92 (31%) |
| Smoking | 85 (28.3%) |
| Dyslipidaemia | 141 (47%) |
| Laboratory
findings | |
| Platelets |
227±93.066×103/ml |
| Lymphocytes |
1.625±0.698×103/ml |
| Neutrophil |
6.012±1.851×103/ml |
| Monocytes |
0.8±0.3×103/ml |
| HDL-cholesterol | 26.5±11.2 mg/dl |
| Creatinine | 1.3±0.9 mg/dl |
| Erythrocyte
sedimentation rate (ESR) | 32±19 mm/h |
| C-reactive protein
(CRP) | 2.72±3.42 mg/dl |
| Fibrinogen (F) | 449.5±108.5
mg/dl |
|
Platelet-to-lymphocyte ratio (PLR) | 184.92±70.84 |
|
Neutrophil-to-lymphocyte ratio (NLR) | 3.91±2.15 |
| Monocytes-to-HDL-C
ratio (MHR) | 26.39±19.38 |
| PLR | |
| G1 | 225.61±157.71 |
| G2 | 151.04±85.08 |
| G3 | 160.53±127.21 |
| G4 | 206.54±141.77 |
| NLR | |
| G1 | 4.58±3.55 |
| G2 | 3.44±2.70 |
| G3 | 3.17±1.98 |
| G4 | 6.96±9.21 |
| MHR | |
| G1 | 31.58±15.61 |
| G2 | 24.01±9.89 |
| G3 | 22.77±12.46 |
| G4 | 27.92±14.21 |
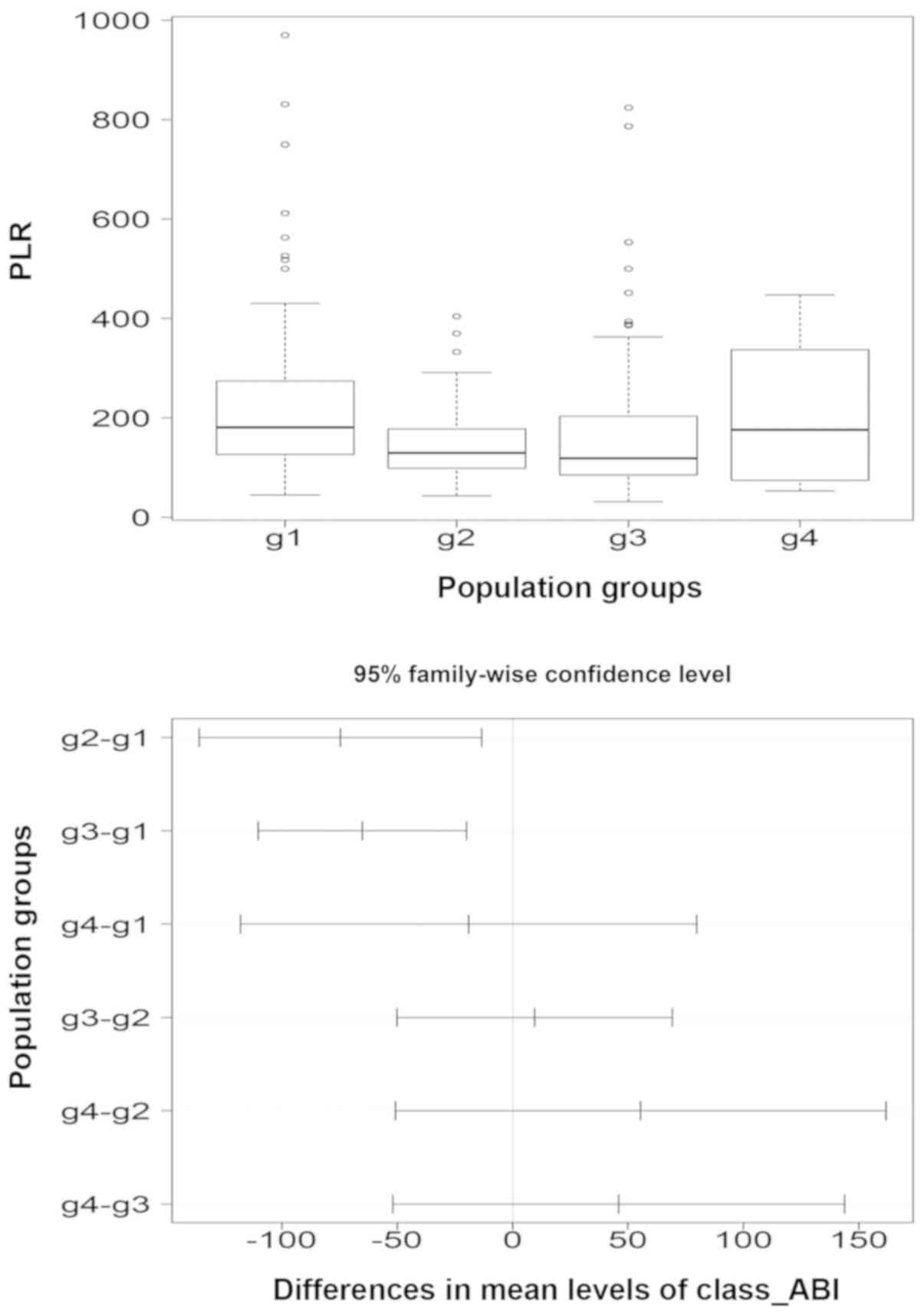
Comparison between groups shows higher PLR in
patients with ABI ≤0.9 (g1) than in patients with a >0.9 ABI
(P=0007). Tukey's post hoc analysis revealed a statistically
significant difference between g1 and g2 (P=0.0098), g1 and g3
(P=0.0013), but a non-significant difference between g1 and g4
(P=0.8594). PLR values in g4 patients were higher than in subjects
of g2 (P=0.5323) and g3 (P=0.6183) with non-statistically relevant
differences (Fig. 1).
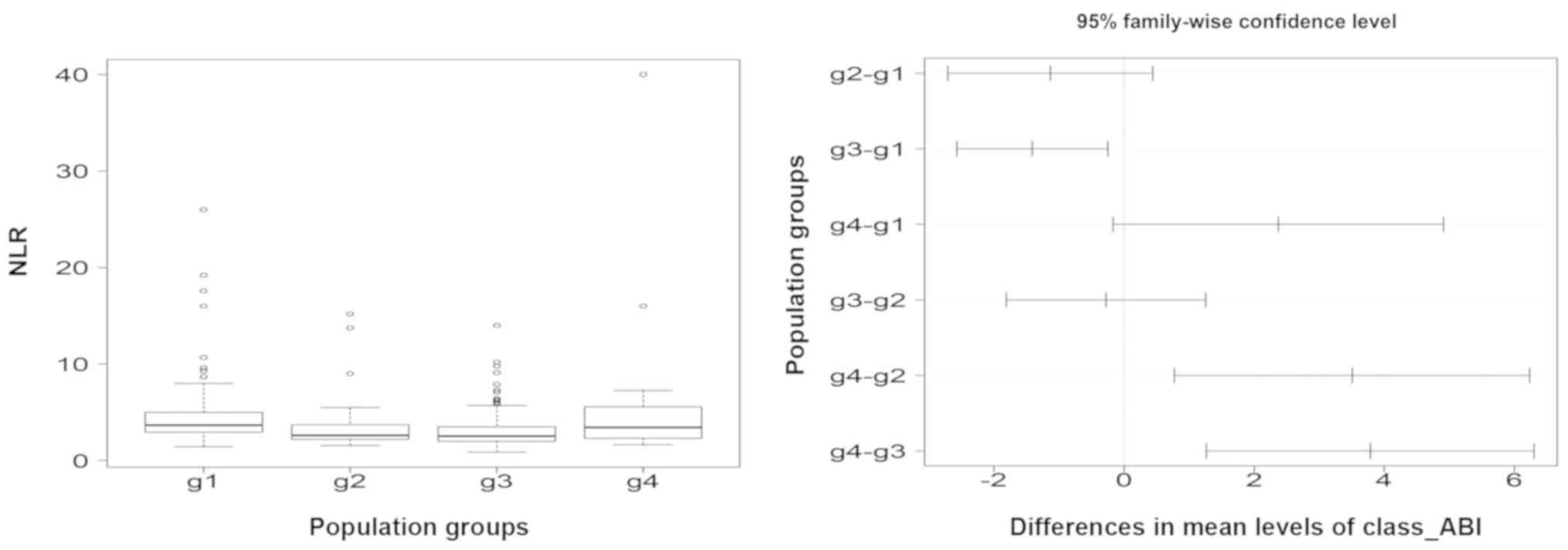
A greater NLR was found in patients with ABI ≤0.9
(g1) than in patients with a 0.9-1.4 ABI (P=0.0001). Tukey's post
hoc analysis showed a statistically significant difference between
g1 and g3 (P=0.0099) and a non-statistically difference between g1
and g2 (P=0.2460).
Subjects of g4 presented NLR values higher than
other groups. Statistically significant differences were shown
between g4 and g2 (P=0.0056), g4 and g3 (P=0.0007); statistically
non-significant variations were found between g4 and g1 (Fig. 2).
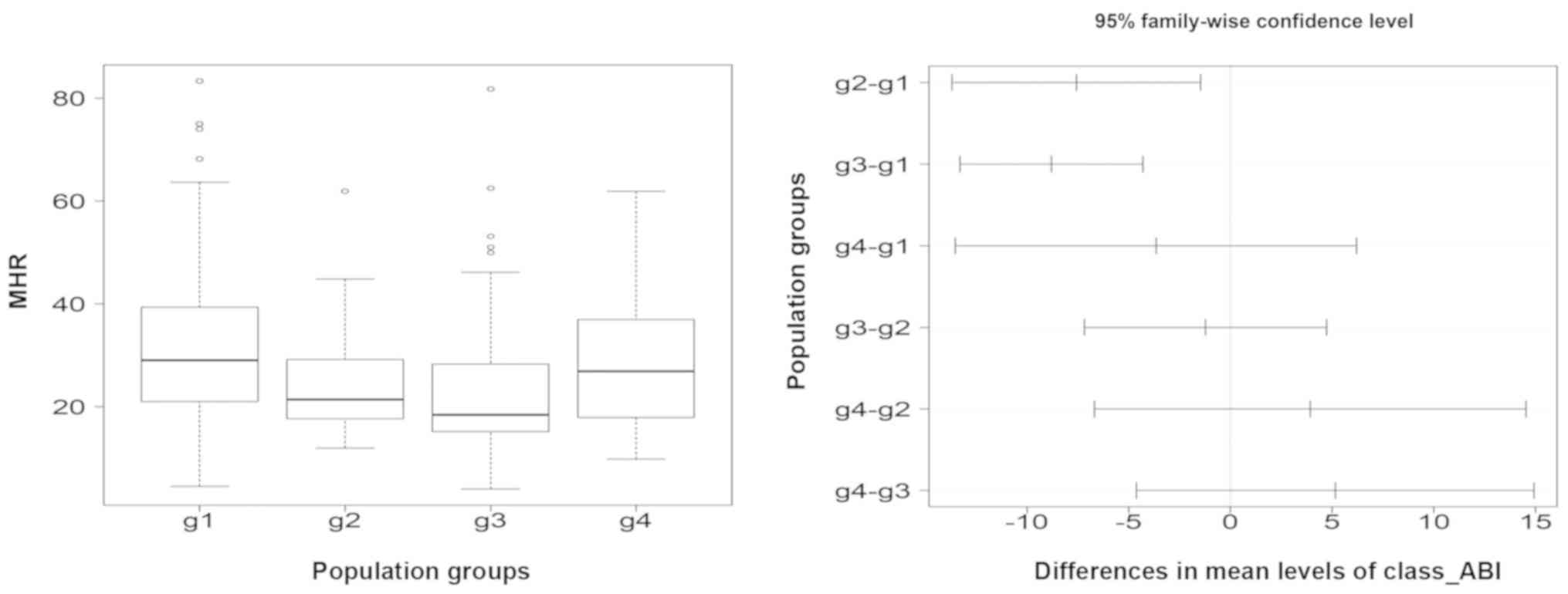
Comparison between groups highlights higher MHR
values in patients with ABI ≤0.9 (g1) than in patients with a
>0.9 ABI (P<0.0001). Tukey's post hoc analysis revealed a
statistically significant difference between g1 and g2
(P<0.0001), between g1 and g3 (P<0.0001) and a
non-statistically difference between g1 and g4. Subjects of g4
presented higher MHR than individuals of g2 and g3, but with no
relevant statistical differences (Fig
3).
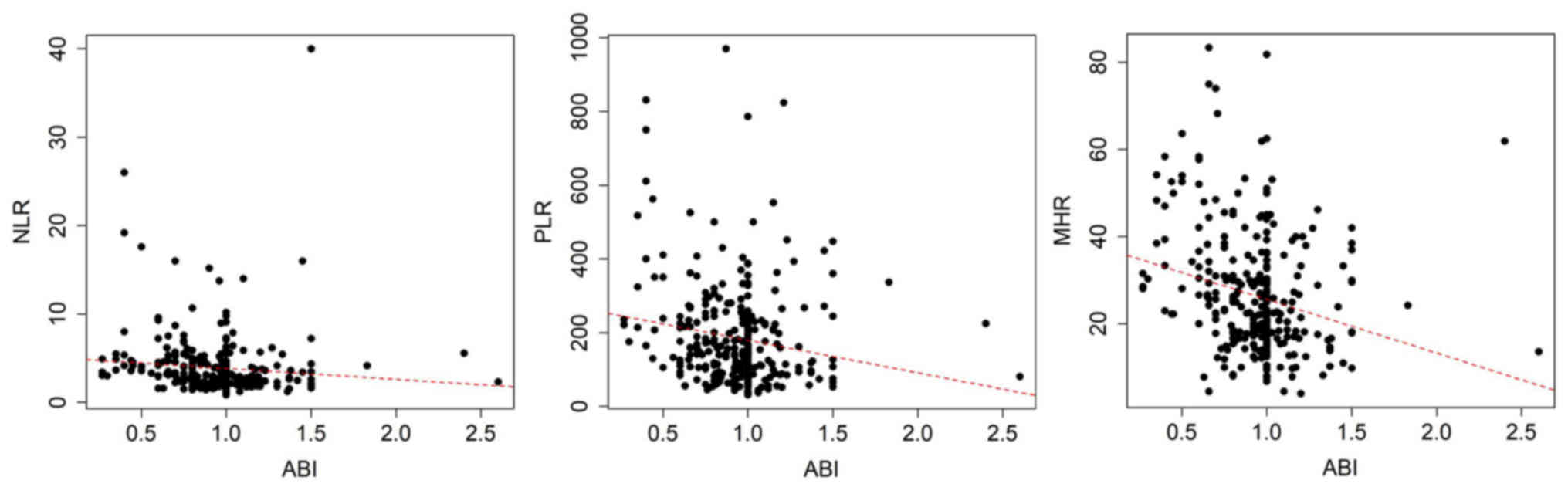
A negative correlation was found between PLR, NLR,
MHR and ABI. The strongest correlation was found between the MHR
and ABI (ρ=−0.24) and PLR and ABI (ρ=−0.18); the analysis
demonstrated a weaker correlation between NLR and ABI (ρ=−0.09).
Univariate linear regression analysis demonstrated a strong
correlation between an increase in PLR and a decrease in ABI
(r=0.0276; F-statistic = 9.496; P=0.0023). Similar relationship was
found for MHR (r=0.0551; F-statistic = 18.44; P<0.0001). For NLR
a non-significant correlation was found (r=0.0055; F-statistic =
2.65; P=0.1046) (Fig. 4).
Non parametric analysis (Wilcoxon test) demonstrated
a strong relation between pathological ABI with the increasing of
PLR (P=2.2×10−16), NLR (P=4.2×10−13) and MHR
(P=1.2×10−15 (Table
IIA).
 | Table IIResults of the statistical
analysis. |
Table II
Results of the statistical
analysis.
A, Non parametric
analysis (Wilcoxon test) to evaluate correlation between
pathological ABI and an increasing of PLR (P=2.2×10−16),
NLR (P=4.2×10−13) and MHR (P=1.2×10−15)
values.
|
|---|
| Markers | ≤0.9 ABI
|
|---|
| Wilcoxon | P-value |
|---|
| PLR | 89.877 |
2.2×10−16 |
| NLR | 84.547 |
4.2×10−13 |
| MHR | 77.877 |
1.2×10−15 |
|
| B, Multivariate
linear regression analysis for predicting a decreased ABI (adjusted
R-squared = 0.06603, F-statistic = 2.922, P=0.0011). |
|
| Parameters | r | P−value |
|
| MHR | −2.993 | 0.00300 |
| NLR | 0.587 | 0.04557 |
| PLR | −1.107 | 0.02691 |
| Hypertension | −0.781 | 0.03560 |
| Diabetes
mellitus | −2.625 | 0.00912 |
| Dyslipidemia | 0.365 | 0.71551 |
| Smoking | 2.085 | 0.03793 |
| ESR | −0.501 | 0.61691 |
| CRP | 0.265 | 0.79131 |
| F | 1.090 | 0.27650 |
| Age | 0.288 | 0.77344 |
In multivariate linear regression analysis, it was
found that hypertension, diabetes mellitus, smoke, PLR, NLR and MHR
were independent factors for predicting a decreased ABI. The model
shows an independent association with pathological values in ABI
measurements (adjusted R-squared = 0.06603, F-statistic = 2.922,
P=0.0011). These data are shown in Table IIB.
Discussion
The present study evaluated the three blood tests
derived indexes (PLR, NLR and MHR) to predict the PAD diagnosed by
using the ABI.
Platelets are able to release inflammatory mediators
leading to adhesion and transmigration of monocytes and interact
with endothelial barrier of the arterial wall promoting
atherosclerotic lesions. Low lymphocyte count indicates generalized
stress or various underlying illnesses. PLR, the ratio between
platelet and lymphocyte absolute counts, is raised in non-dipper
hypertensive patients, in patients with venous thromboembolism, in
patients with chronic PAD or critical limb ischemia (CLI) and in
patients suffering from chronic kidney disease (17,18). The >144 PLR ratio was found to
be associated with raised mortality in patients treated with
percutaneous coronary angioplasty after NSTEMI or STEMI myocardial
infarction (19).
Neutrophils increase in acute inflammation, and NLR
represents a helpful prognostic marker in patients with acute
coronary syndrome (ACS). NLR >5.9 correlates with raised 90-day
mortality in patients with ischemic stroke (20). Subjects suffering from increased
PAD value of the NLR was found to be associated with a greater
prevalence of CLI (21).
Circulating monocytes as a source of various cytokines and
molecules interact primarily with platelets and endothelial cells
leading to aggravation of inflammatory, pro-thrombotic pathways.
MHR is an index related to inflammatory processes, especially those
linked to atherosclerotic lesions. The activation of Pattern
Recognition Receptor (PRR) in the vascular wall is a pivotal event
in atherogenesis. Activation of inflammation has been shown to
induce production of monocyte chemoattractant protein 1 (MCP1),
recruiting monocytes in vascular lumen (22). A significant amount of surface
lymphocyte antigen 6 complex (Ly6Chi monocytes) is expressed on
CD14+CD16− monocytes, a subtype having
pro-inflammatory activity, it was found elevated in patients with
dyslipidaemia (23). MHR has been
reported as a helpful marker to identify subjects with high risk
for the major cardiovascular events (MACE) (24). Our results demonstrate a similar
prevalence of principal CV risk factors (arterial hypertension,
diabetes mellitus, dyslipidaemia, and smoking) compared to general
population. Prevalence of PAD (ABI <0.90) was up to 34%,
slightly higher compared to epidemiological data in non-geriatric
patients. Prevalence of the PAD ranged between 20 and 28% (25). Recent studies showed a positive
association between NLR and PLR with the severity of lower
extremity PAD, poor prognosis, particularly with risk of one-year
readmission. NLR also correlates with one-year mortality (26). According to ABI value, we obtained
4 subgroups (g1, g2, g3 and g4). Our results demonstrated that
patients with ABI <0.9, a well-recognized PAD diagnostic index,
showed higher PLR and MHR values. Increased NLR values were found
to be associated to >1.4 ABI (lower limb arterial
incompressibility). A statistically significant correlation was
found between lower ABI values with the increase of PLR and MHR
values; correlation was found as non-significant for NLR. In a
model including well-known cardiovascular risk factors such as
arterial hypertension, diabetes mellitus, dyslipidaemia, smoking,
age and bio-humoral tests (ESR, CRP and F), we found that PLR, NLR
and MHR represent independent variables for predicting PAD. This
work highlighted that PLR and MHR represent two reliable markers of
PAD. In particular, their increase is associated with decreased of
the ABI values. NLR presented a weaker relationship with decreasing
ABI (statistically non-significant), but an elevated value is
strongly related to a condition of arterial incompressibility,
likely due to medial calcification in subjects with long-lasting
atherosclerotic disease.
Limitations and strength
It is noteworthy that the present study was planned
as an observational study, so it may be considered a limitation.
However, the study focused on value of interesting blood cell
parameters in patients affected by one of the atherosclerotic
diseases. Additionally, the study shows the relationship between
some of the above referred blood cell parameters with the ABI value
as validated diagnostic tool for PAD. Limitation of this study
could be related to the typology of research. Study enrolled 300
patients admitted to geriatric internal medicine unit, so we
believe that the population was homogeneous and numerous. The
present study was not planed as longitudinal study, it did not
allow us to discuss the capability of the markers to predict both
outcome and prognosis of PAD patients. Further evaluations will be
targeted to achieving data concerning the bloodstream cells
pathways related to the clinical outcome or prognosis in elderly
patients.
In conclusion, the present study confirms that
ultrasound plays a pivotal role in diagnosis and follow-up of PAD.
The importance of inflammation is largely accepted as a key player
leading to promotion and acceleration of atherosclerosis and
consequences such as PAD. Our group has contributed to this concern
showing increased plasma level of inflammatory, endothelial and
metalloproteinase markers in PAD (27-29). The present study suggests that
elevated PLR, NLR and MHR are related to PAD diagnosed by the ABI
measurement. PLR and MHR were shown to be more reliable markers
than NLR in PAD. NLR seems to be more related to the
incompressibility condition of lower limb arteries. Based on our
findings we can hypothesize that these complete blood counts may be
considered, as favourable, simple, potential and repeatable markers
for PAD.
Acknowledgments
Not applicable.
Funding
No funding was received.
Availability of data and materials
The data used and/or analysed in this study are
available from the corresponding author with reasonable
request.
Authors' contributions
All authors (SS, AA, GB, CM, MDG, CGD, ESDV, MR, SL
and SSS) made substantial contributions to the study design, data
acquisition and interpretation of the data. Each author
participated sufficiently in the work to take public responsibility
for appropriate portions of the content and agree all aspects of
the work in ensuring that questions related to the accuracy or
integrity of any part of the work are appropriately investigated
and resolved.
Ethics approval and consent to
participate
Verbal informed consent was obtained from each
patient and the study protocol conforms to the ethical guidelines
of the 1975 Declaration of Helsinki as reflected in a priori
approval by the institution's human research committee.
Patient consent for publication
Identifying information, including names, initials,
date of birth or hospital numbers, images or statements are not
included in the manuscript.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Writing group Members; Mozaffarian D,
Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de
Ferranti S, Després JP, Fullerton HJ, et al American Heart
Association Statistics Committee; Stroke Statistics Subcommittee:
Heart disease and stroke statistics-2016 update: A report from the
American Heart Association. Circulation. 133:e38–360. 2016.
|
|
2
|
Townsend N, Wilson L, Bhatnagar P,
Wickramasinghe K, Rayner M and Nichols M: Cardiovascular disease in
Europe: Epidemiological update 2016. Eur Heart J. 37:3232–3245.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Corrado E, Rizzo M, Muratori I, Coppola G
and Novo S: Older age and markers of inflammation are strong
predictors of clinical events in women with asymptomatic carotid
lesions. Menopause. 15:240–247. 2008. View Article : Google Scholar
|
|
4
|
Corrado E and Novo S: High sensitivity of
C-reactive protein in primary prevention. G Ital Cardiol (Rome).
8:327–334. 2007.In Italian.
|
|
5
|
Maresca G, Di Blasio A, Marchioli R and Di
Minno G: Measuring plasma fibrinogen to predict stroke and
myocardial infarction: An update. Arterioscler Thromb Vasc Biol.
19:1368–1377. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wierzbicki AS: Homocysteine and
cardiovascular disease: A review of the evidence. Diab Vasc Dis
Res. 4:143–150. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Michaud M, Balardy L, Moulis G, Gaudin C,
Peyrot C, Vellas B, Cesari M and Nourhashemi F: Proinflammatory
cytokines, aging, and age-related diseases. J Am Med Dir Assoc.
14:877–882. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim NY, Chun DH, Kim SY, Kim NK, Baik SH,
Hong JH, Kim KS and Shin CS: Prognostic value of systemic
inflammatory indices, NLR, PLR, and MPV, for predicting 1-year
survival of patients undergoing cytoreductive surgery with HIPEC. J
Clin Med. 8:5892019. View Article : Google Scholar :
|
|
9
|
Kurtul A and Ornek E: Platelet to
lymphocyte ratio in cardiovascular diseases: A systematic review.
Angiology. 70:802–818. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ganjali S, Gotto AM Jr, Ruscica M, Atkin
SL, Butler AE, Banach M and Sahebkar A: Monocyte-to-HDL-cholesterol
ratio as a prognostic marker in cardiovascular diseases. J Cell
Physiol. 233:9237–9246. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Toor IS, Jaumdally RJ, Moss MS and Babu
SB: Preprocedural neutrophil count predicts outcome in patients
with advanced peripheral vascular disease undergoing percutaneous
trans-luminal angioplasty. J Vasc Surg. 48:1504–1508. 2008.
View Article : Google Scholar
|
|
12
|
Liang RF, Li M, Li JH, Zuo MR, Yang Y and
Liu YH: The significance of preoperative haematological
inflammatory markers in patients with meningiomas. Clin Neurol
Neurosurg. 182:1–4. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
American Diabetes Association: Standards
of medical care in diabetes - 2012. Diabetes Care. 35(Suppl 1):
S11–S63. 2012. View Article : Google Scholar
|
|
14
|
Chobanian AV, Bakris GL, Black HR, Cushman
WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright
JT Jr, et al National High Blood Pressure Education Program
Coordinating Committee: The seventh report of the Joint Ntional
Committee on prevention, detection, evaluation, and treatment of
high blood pressure: The JNC 7 report. JAMA. 289:2560–2572. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Grundy SM, Cleeman JI, Merz CN, Brewer HB
Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC Jr and Stone
NJ; National Heart, Lung, and Blood Institute; American College of
Cardiology Foundation; American Heart Association: Implications of
recent clinical trials for the national cholesterol education
program adult treatment panel III guidelines. Circulation.
110:227–239. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Khan TH, Farooqui FA and Niazi K: Critical
review of the ankle brachial index. Curr Cardiol Rev. 4:101–106.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Balta S and Ozturk C: The
platelet-lymphocyte ratio: A simple, inexpensive and rapid
prognostic marker for cardiovascular events. Platelets. 26:680–681.
2015. View Article : Google Scholar
|
|
18
|
Gary T, Pichler M, Belaj K, Hafner F,
Gerger A, Froehlich H, Eller P, Rief P, Hackl G, Pilger E, et al:
Platelet-to-lymphocyte ratio: A novel marker for critical limb
ischemia in peripheral arterial occlusive disease patients. PLoS
One. 8:e676882013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Çiçek G, Açıkgoz SK, Bozbay M, Altay S,
Uğur M, Uluganyan M and Uyarel H: Neutrophil-lymphocyte ratio and
platelet-lymphocyte ratio combination can predict prognosis in
patients with ST-segment elevation myocardial infarction undergoing
primary percutaneous coronary intervention. Angiology. 66:441–447.
2015. View Article : Google Scholar
|
|
20
|
Paquissi FC: The role of inflammation in
cardiovascular diseases: The predictive value of
neutrophil-lymphocyte ratio as a marker in peripheral arterial
disease. Ther Clin Risk Manag. 12:851–860. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Belaj K, Pichler M, Hackl G, Rief P, Eller
P, Hafner F, Brodmann M and Gary T: Association of the derived
neutrophil-lymphocyte ratio with critical limb ischemia. Angiology.
67:350–354. 2016. View Article : Google Scholar
|
|
22
|
Tacke F, Alvarez D, Kaplan TJ, Jakubzick
C, Spanbroek R, Llodra J, Garin A, Liu J, Mack M, van Rooijen N, et
al: Monocyte subsets differentially employ CCR2, CCR5, and CX3CR1
to accumulate within atherosclerotic plaques. J Clin Invest.
117:185–194. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sala F, Cutuli L, Grigore L, Pirillo A,
Chiesa G, Catapano AL and Norata GD: Prevalence of classical
CD14++/CD16− but not of intermediate
CD14++/CD16+ monocytes in
hypoalphalipoproteinemia. Int J Cardiol. 168:2886–2889. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cetin MS, Ozcan Cetin EH, Kalender E,
Aydin S, Topaloglu S, Kisacik HL and Temizhan A: Monocyte to HDL
cholesterol ratio predicts coronary artery disease severity and
future major cardiovascular adverse events in acute coronary
syndrome. Heart Lung Circ. 25:1077–1086. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Criqui MH and Aboyans V: Epidemiology of
peripheral artery disease. Circ Res. 116:1509–1526. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xue G, Deng H and Zhang L:
Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio predict
severity and prognosis of lower limb arteriosclerosis obliterans.
Ann Vasc Surg. 64:221–227. 2020. View Article : Google Scholar
|
|
27
|
Signorelli SS, Malaponte G, Libra M, Di
Pino L, Celotta G, Bevelacqua V, Petrina M, Nicotra GS, Indelicato
M, Navolanic PM, et al: Plasma levels and zymographic activities of
matrix metal-loproteinases 2 and 9 in type II diabetics with
peripheral arterial disease. Vasc Med. 10:1–6. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Signorelli SS, Anzaldi M, Libra M,
Navolanic PM, Malaponte G, Mangano K, Quattrocchi C, Di Marco R,
Fiore V and Neri S: Plasma levels of Inflammatory Biomarkers in
Peripheral Arterial Disease: Results of a cohort study. Angiology.
67:870–874. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Signorelli SS, Mazzarino MC, Spandidos DA
and Malaponte G: Proinflammatory circulating molecules in
peripheral arterial disease. Int J Mol Med. 20:279–286.
2007.PubMed/NCBI
|