|
1
|
World Health Organization (WHO):
Coronavirus disease 2019 (COVID-19): situation report, 139. WHO;
Geneva: 2020, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
Accessed June 8, 2020.
|
|
2
|
Pellegrino R, Cooper KW, Di Pizio A,
Joseph PV, Bhutani S and Parma V: Corona Viruses and the Chemical
Senses: Past, Present, and Future. Chem Senses.
bjaa0312020.PubMed/NCBI
|
|
3
|
Mainland JD, Keller A, Li YR, Zhou T,
Trimmer C, Snyder LL, Moberly AH, Adipietro KA, Liu WL, Zhuang H,
et al: The missense of smell: Functional variability in the human
odorant receptor repertoire. Nat Neurosci. 17:114–120. 2014.
View Article : Google Scholar :
|
|
4
|
Maßberg D and Hatt H: Human olfactory
receptors: Novel cellular functions outside of the nose. Physiol
Rev. 98:1739–1763. 2018. View Article : Google Scholar
|
|
5
|
An SS and Liggett SB: Taste and smell
GPCRs in the lung: Evidence for a previously unrecognized
widespread chemo-sensory system. Cell Signal. 41:82–88. 2018.
View Article : Google Scholar
|
|
6
|
Neuhaus EM, Zhang W, Gelis L, Deng Y,
Noldus J and Hatt H: Activation of an olfactory receptor inhibits
proliferation of prostate cancer cells. J Biol Chem.
284:16218–16225. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gosain R, Abdou Y, Singh A, Rana N,
Puzanov I and Ernstoff MS: COVID-19 and cancer: a comprehensive
review. Curr Oncol Rep. 22:532020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hoffmann M, Kleine-Weber H, Schroeder S,
Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH,
Nitsche A, et al: SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2
and is blocked by a clinically proven protease inhibitor. Cell.
181:271–280.e8. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Walls AC, Park YJ, Tortorici MA, Wall A,
McGuire AT and Veesler D: Structure, function, and antigenicity of
the SARS-CoV-2 spike glycoprotein. Cell. 181:281–292.e6. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yuki K, Fujiogi M and Koutsogiannaki S:
COVID-19 pathophysiology: A review. Clin Immunol. 215:1084272020.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Butowt R and Bilinska K: SARS-CoV-2:
olfaction, brain infection, and the urgent need for clinical
samples allowing earlier virus detection. ACS Chem Neurosci.
11:1200–1203. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brann DH, Tsukahara T, Weinreb C, Lipovsek
M, Van den Berge K, Gong B, Chance R, Macaulay IC, Chou H, Fletcher
R, et al: Non-neuronal expression of SARS-CoV-2 entry genes in the
olfactory system suggests mechanisms underlying COVID-19-associated
anosmia. bioRxiv. View Article : Google Scholar
|
|
13
|
Chai P, Yu J, Ge S, Jia R and Fan X:
Genetic alteration, RNA expression, and DNA methylation profiling
of coronavirus disease 2019 (COVID-19) receptor ACE2 in
malignancies: A pan-cancer analysis. J Hematol Oncol. 13:432020.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Katopodis P, Anikin V, Randeva HS,
Spandidos DA, Chatha K, Kyrou I and Karteris E: Pan-cancer analysis
of transmembrane protease serine 2 and cathepsin L that mediate
cellular SARS-CoV-2 infection leading to COVID-19. Int J Oncol.
57:533–539. 2020.PubMed/NCBI
|
|
15
|
Eliezer M, Hautefort C, Hamel AL,
Verillaud B, Herman P, Houdart E and Eloit C: Sudden and complete
olfactory loss function as a possible symptom of COVID-19. JAMA
Otolaryngol Head Neck Surg. April 8–2020.Epub ahead of print.
|
|
16
|
Bilinska K, Jakubowska P, Von Bartheld CS
and Butowt R: Von Bartheld CS and Butowt R: Expression of the
SARS-CoV-2 entry proteins, ACE2 and TMPRSS2, in cells of the
olfactory epithelium: identification of cell types and trends with
age. ACS Chem Neurosci. 11:1555–1562. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang S, Zhou X, Zhang T and Wang Z: The
need for urogenital tract monitoring in COVID-19. Nat Rev Urol.
17:314–315. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Reghunathan R, Jayapal M, Hsu LY, Chng HH,
Tai D, Leung BP and Melendez AJ: Expression profile of immune
response genes in patients with Severe Acute Respiratory Syndrome.
BMC Immunol. 6:22005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hu W, Yen YT, Singh S, Kao CL and Ba WH:
SARS-CoV regulates immune function-related gene expression in human
monocytic cells. Viral Immunol. 25:277–288. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
VanLeuven JT, Ridenhour BJ, Gonzalez AJ,
Miller CR and Miura TA: Lung epithelial cells have virus-specific
and shared gene expression responses to infection by diverse
respiratory viruses. PLoS One. 12:e01784082017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wajed SA, Laird PW and DeMeester TR: DNA
methylation: An alternative pathway to cancer. Ann Surg. 234:10–20.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xia C, Ma W, Wang F, Hua SB and Liu M:
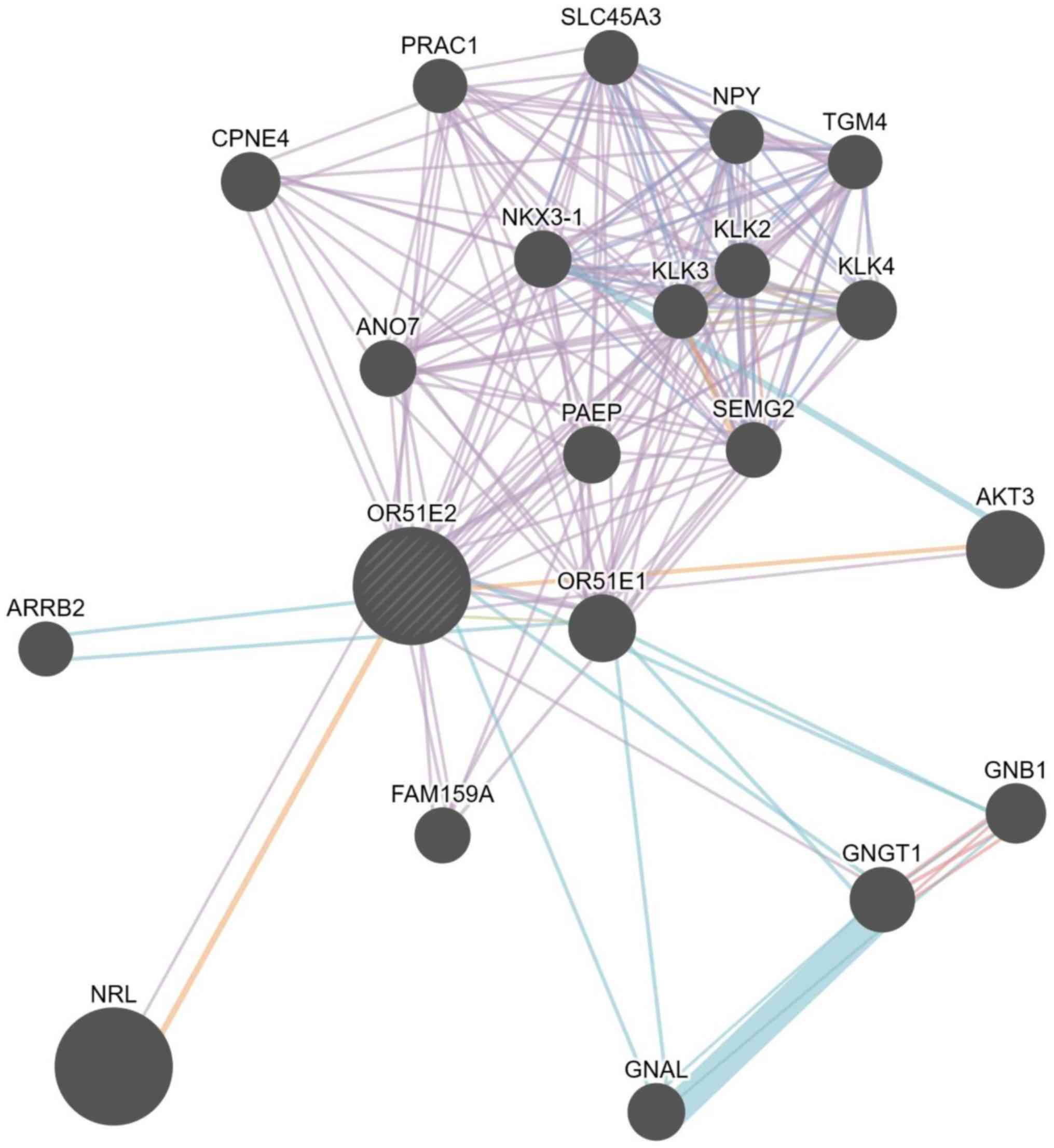
Identification of a prostate-specific G-protein coupled receptor in
prostate cancer. Oncogene. 20:5903–5907. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Abaffy T, Bain JR, Muehlbauer MJ,
Spasojevic I, Lodha S, Bruguera E, O'Neal SK, Kim SY and Matsunami
H: A testosterone metabolite 19-hydroxyandrostenedione induces
neuroendocrine trans-differentiation of prostate cancer cells via
an ectopic olfactory receptor. Front Oncol. 8:1622018. View Article : Google Scholar :
|
|
24
|
Wambier CG, Goren A, Vaño-Galván S, Ramos
PM, Ossimetha A, Nau G, Herrera S and McCoy J: Androgen sensitivity
gateway to COVID-19 disease severity. Drug Dev Res. May
15–2020.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Stopsack KH, Mucci LA, Antonarakis ES,
Nelson PS and Kantoff PW: TMPRSS2 and COVID-19: Serendipity or
opportunity for intervention? Cancer Discov. 10:779–782. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hong SK: Kallikreins as biomarkers for
prostate cancer. BioMed Res Int. 2014:5263412014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kaikkonen E, Rantapero T, Zhang Q, Taimen
P, Laitinen V, Kallajoki M, Jambulingam D, Ettala O, Knaapila J,
Boström PJ, et al PRACTICAL Consortium: ANO7 is associated with
aggressive prostate cancer. Int J Cancer. 143:2479–2487. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gurel B, Ali TZ, Montgomery EA, Begum S,
Hicks J, Goggins M, Eberhart CG, Clark DP, Bieberich CJ, Epstein
JI, et al: NKX3.1 as a marker of prostatic origin in metastatic
tumors. Am J Surg Pathol. 34:1097–1105. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hu WY, Hu DP, Xie L, Li Y, Majumdar S,
Nonn L, Hu H, Shioda T and Prins GS: Isolation and functional
interrogation of adult human prostate epithelial stem cells at
single cell resolution. Stem Cell Res (Amst). 23:1–12. 2017.
View Article : Google Scholar
|
|
30
|
Zhang P, He X, Tan J, Zhou X and Zou L:
β-arrestin2 mediates β-2 adrenergic receptor signaling inducing
prostate cancer cell progression. Oncol Rep. 26:1471–1477.
2011.PubMed/NCBI
|
|
31
|
Lin HP, Lin CY, Huo C, Jan YJ, Tseng JC,
Jiang SS, Kuo YY, Chen SC, Wang CT, Chan TM, et al: AKT3 promotes
prostate cancer proliferation cells through regulation of Akt,
B-Raf, and TSC1/TSC2. Oncotarget. 6:27097–27112. 2015. View Article : Google Scholar : PubMed/NCBI
|