|
1
|
Dam H: The antihaemorrhagic vitamin of the
chick. Biochem J. 29:1273–1285. 1935. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Palmer CR, Blekkenhorst LC, Lewis JR, Ward
NC, Schultz CJ, Hodgson JM, Croft KD and Sim M: Quantifying dietary
vitamin K and its link to cardiovascular health: A narrative
review. Food Funct. 11:2826–2837. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hirota Y, Tsugawa N, Nakagawa K, Suhara Y,
Tanaka K, Uchino Y, Takeuchi A, Sawada N, Kamao M, Wada A, et al:
Menadione (vitamin K3) is a catabolic product of oral phylloquinone
(vitamin K1) in the intestine and a circulating precursor of tissue
menaquinone-4 (vitamin K2) in rats. J Biol Chem. 288:33071–33080.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Simes DC, Viegas CSB, Araújo N and
Marreiros C: Vitamin K as a diet supplement with impact in human
health: Current evidence in age-related diseases. Nutrients.
12:1382020. View Article : Google Scholar :
|
|
5
|
Mirza F and Canalis E: Management of
endocrine disease: Secondary osteoporosis: Pathophysiology and
management. Eur J Endocrinol. 173:R131–R151. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cheung CL, Ang SB, Chadha M, Chow ES,
Chung YS, Hew FL, Jaisamrarn U, Ng H, Takeuchi Y, Wu CH, et al: An
updated hip fracture projection in Asia: The Asian federation of
osteoporosis societies study. Osteoporos Sarcopenia. 4:16–21. 2018.
View Article : Google Scholar
|
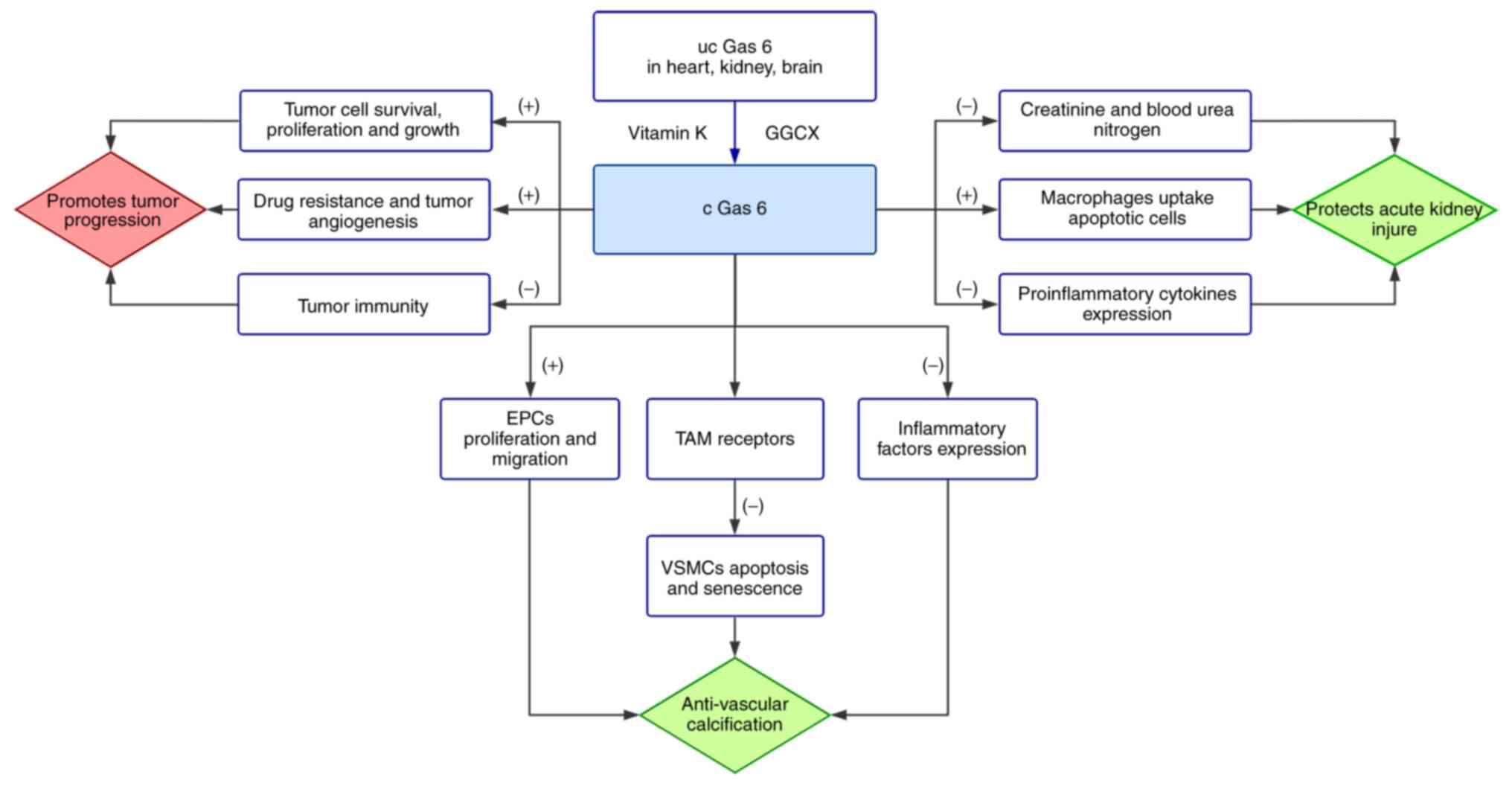
|
7
|
Wasilewski GB, Vervloet MG and Schurgers
LJ: The bone-vasculature axis: Calcium supplementation and the role
of vitamin K. Front Cardiovasc Med. 6:62019. View Article : Google Scholar : PubMed/NCBI
|
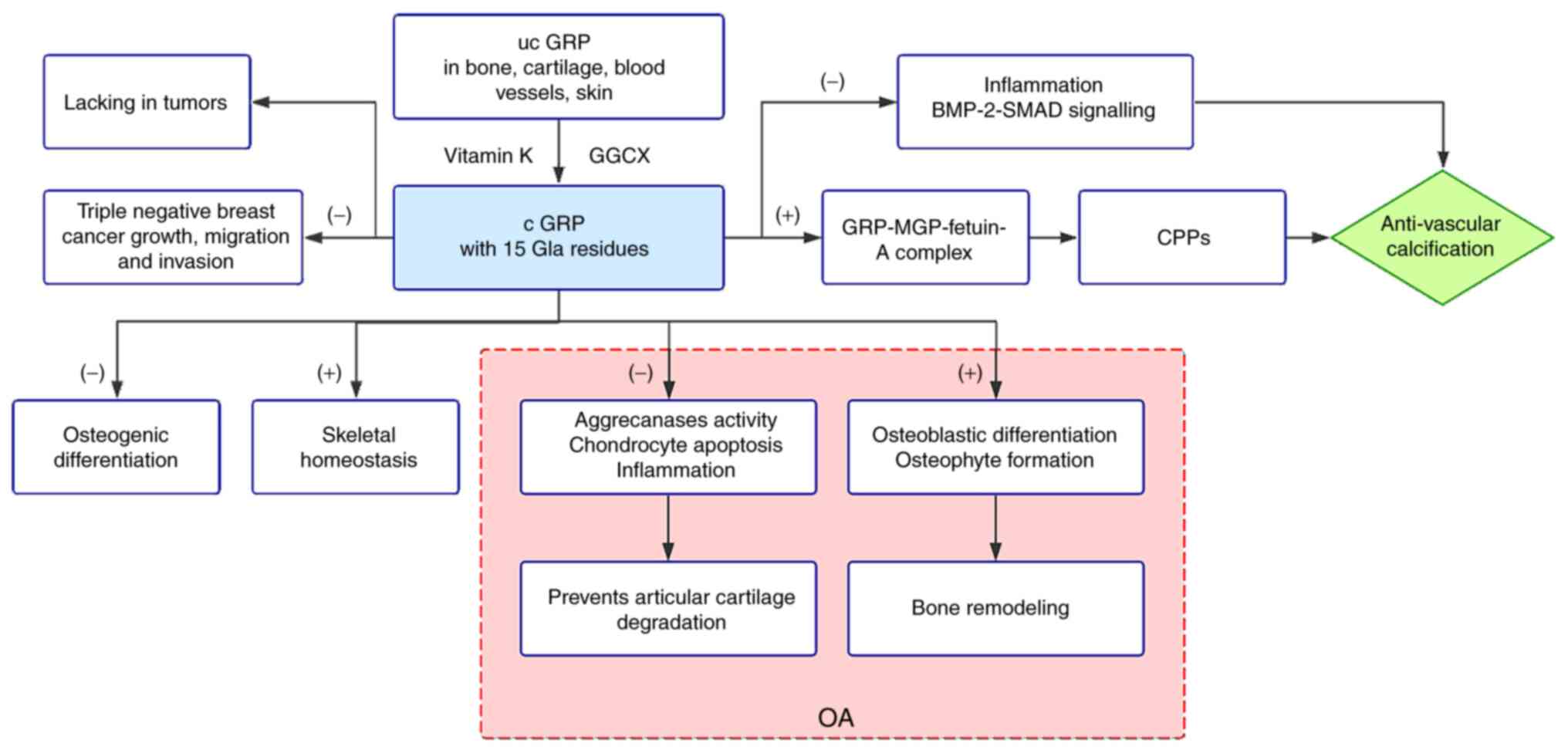
|
8
|
Danziger J, Young RL, Shea MK, Tracy RP,
Ix JH, Jenny NS and Mukamal KJ: Vitamin K-dependent protein
activity and incident ischemic cardiovascular disease: The
multi-ethnic study of atherosclerosis. Arterioscler Thromb Vasc
Biol. 36:1037–1042. 2016. View Article : Google Scholar : PubMed/NCBI
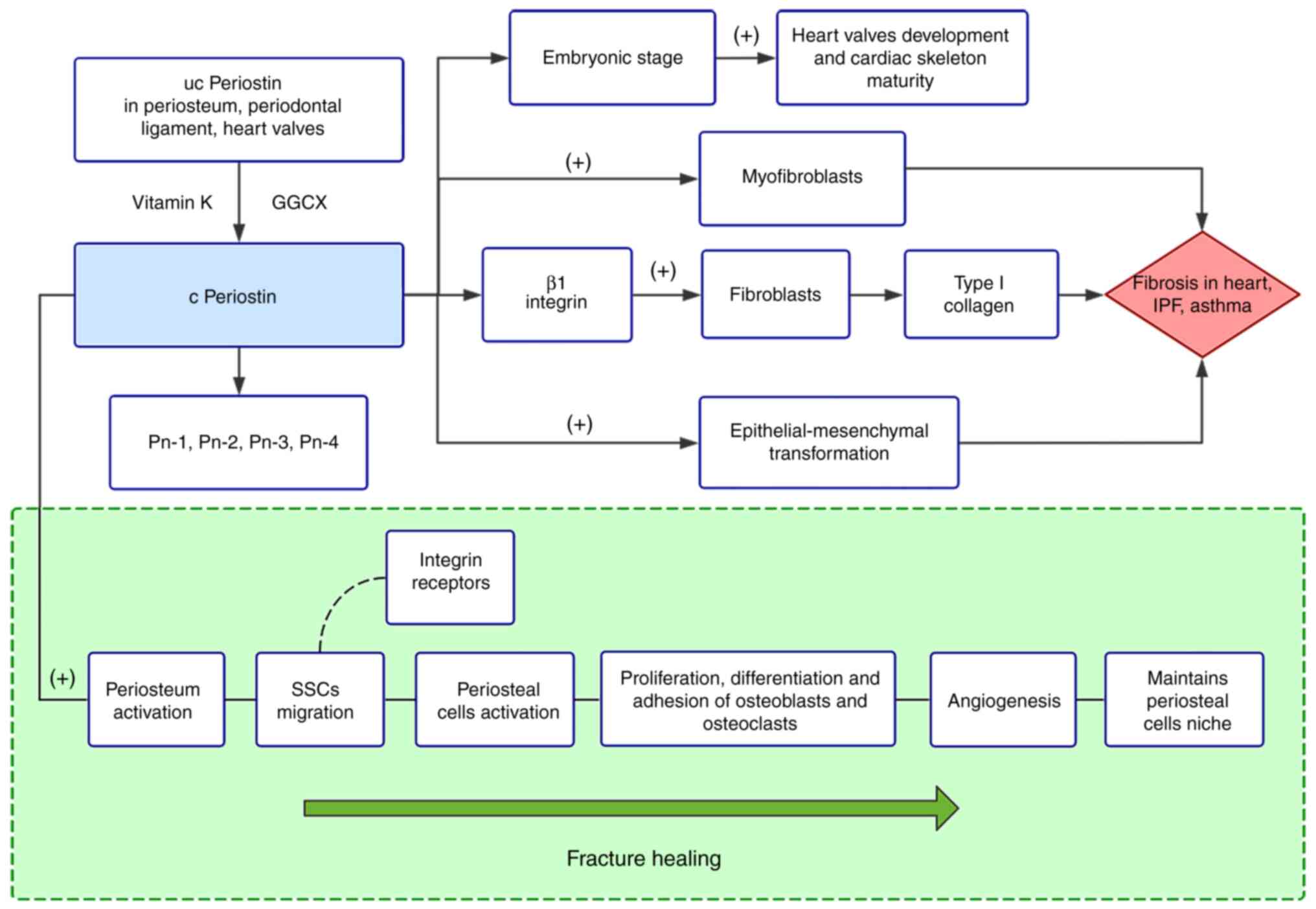
|
|
9
|
Iribarren C, Sidney S, Sternfeld B and
Browner WS: Calcification of the aortic arch: Risk factors and
association with coronary heart disease, stroke, and peripheral
vascular disease. JAMA. 283:2810–2815. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kondos GT, Hoff JA, Sevrukov A, Daviglus
ML, Garside DB, Devries SS, Chomka EV and Liu K: Electron-beam
tomography coronary artery calcium and cardiac events: A 37-month
follow-up of 5635 initially asymptomatic low- to intermediate-risk
adults. Circulation. 107:2571–2576. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ferland G: The discovery of vitamin K and
its clinical applications. Ann Nutr Metab. 61:213–218. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cheung CL, Sahni S, Cheung BM, Sing CW and
Wong IC: Vitamin K intake and mortality in people with chronic
kidney disease from NHANES III. Clin Nutr. 34:235–240. 2015.
View Article : Google Scholar
|
|
13
|
Fusaro M, Plebani M, Iervasi G and
Gallieni M: Vitamin K deficiency in chronic kidney disease:
Evidence is building up. Am J Nephrol. 45:1–3. 2017. View Article : Google Scholar
|
|
14
|
Turner ME, Adams MA and Holden RM: The
vitamin K metabolome in chronic kidney disease. Nutrients.
10:10762018. View Article : Google Scholar :
|
|
15
|
Kaesler N, Magdeleyns E, Herfs M,
Schettgen T, Brandenburg V, Fliser D, Vermeer C, Floege J,
Schlieper G and Krüger T: Impaired vitamin K recycling in uremia is
rescued by vitamin K supplementation. Kidney Int. 86:286–293. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Di Lullo L, House A, Gorini A, Santoboni
A, Russo D and Ronco C: Chronic kidney disease and cardiovascular
complications. Heart Fail Rev. 20:259–272. 2015. View Article : Google Scholar
|
|
17
|
Shearer MJ, Mallinson CN, Webster GR and
Barkhan P: Clearance from plasma and excretion in urine, faeces and
bile of an intravenous dose of tritiated vitamin K 1 in man. Br J
Haematol. 22:579–588. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schurgers LJ, Teunissen KJF, Hamulyák K,
Knapen MH, Vik H and Vermeer C: Vitamin K-containing dietary
supplements: Comparison of synthetic vitamin K1 and natto-derived
menaquinone-7. Blood. 109:3279–3283. 2007. View Article : Google Scholar
|
|
19
|
Halder M, Petsophonsakul P, Akbulut AC,
Pavlic A, Bohan F, Anderson E, Maresz K, Kramann R and Schurgers L:
Vitamin K: Double bonds beyond coagulation insights into
differences between vitamin K1 and K2 in health and disease. Int J
Mol Sci. 20:8962019. View Article : Google Scholar :
|
|
20
|
Willems BAG, Vermeer C, Reutelingsperger
CP and Schurgers LJ: The realm of vitamin K dependent proteins:
Shifting from coagulation toward calcification. Mol Nutr Food Res.
58:1620–1635. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kearon C, Akl EA, Comerota AJ, Prandoni P,
Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali
F, et al: Antithrombotic therapy for VTE disease: Antithrombotic
therapy and prevention of thrombosis, 9th ed: American college of
chest physicians evidence-based clinical practice guidelines.
Chest. 141(2 Suppl): e419S–e496S. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tie JK and Stafford DW: Structural and
functional insights into enzymes of the vitamin K cycle. J Thromb
Haemost. 14:236–247. 2016. View Article : Google Scholar :
|
|
23
|
Huang M, Rigby AC, Morelli X, Grant MA,
Huang G, Furie B, Seaton B and Furie BC: Structural basis of
membrane binding by Gla domains of vitamin K-dependent proteins.
Nat Struct Biol. 10:751–756. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Girolami A, Ferrari S, Cosi E, Santarossa
C and Randi ML: Vitamin K-dependent coagulation factors that may be
responsible for both bleeding and thrombosis (FII, FVII, and FIX).
Clin Appl Thromb Hemost. 24(9 Suppl): 42S–47S. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mahdi AJ, Obaji SG and Collins PW: Role of
enhanced half-life factor VIII and IX in the treatment of
haemophilia. Br J Haematol. 169:768–776. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Muller MP, Wang Y, Morrissey JH and
Tajkhorshid E: Lipid specificity of the membrane binding domain of
coagulation factor X. J Thromb Haemost. 15:2005–2016. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rezaie AR: Regulation of the protein C
anticoagulant and antiinflammatory pathways. Curr Med Chem.
17:2059–2069. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mosnier LO, Zlokovic BV and Griffin JH:
The cytoprotective protein C pathway. Blood. 109:3161–3172. 2007.
View Article : Google Scholar
|
|
29
|
Mosnier LO and Griffin JH: Protein C
anticoagulant activity in relation to anti-inflammatory and
anti-apoptotic activities. Front Biosci. 11:2381–2399. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Majid Z, Tahir F, Ahmed J, Bin Arif T and
Haq A: Protein C deficiency as a risk factor for stroke in young
adults: A review. Cureus. 12:e74722020.PubMed/NCBI
|
|
31
|
Bernard GR, Vincent JL, Laterre PF, LaRosa
SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE,
Helterbrand JD, Ely EW, et al: Efficacy and safety of recombinant
human activated protein C for severe sepsis. N Engl J Med.
344:699–709. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Dahlbäck B: Vitamin K-dependent protein S:
Beyond the protein C pathway. Semin Thromb Hemost. 44:176–184.
2018. View Article : Google Scholar
|
|
33
|
Suleiman L, Négrier C and Boukerche H:
Protein S: A multi-functional anticoagulant vitamin K-dependent
protein at the crossroads of coagulation, inflammation,
angiogenesis, and cancer. Crit Rev Oncol Hematol. 88:637–654. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Fricke DR, Chatterjee S and Majumder R:
Protein S in preventing thrombosis. Aging (Albany NY). 11:847–848.
2019. View Article : Google Scholar
|
|
35
|
Yasuma T, Yano Y, D'Alessandro-Gabazza CN,
Toda M, Gil-Bernabe P, Kobayashi T, Nishihama K, Hinneh JA,
Mifuji-Moroka R, Roeen Z, et al: Amelioration of diabetes by
protein S. Diabetes. 65:1940–1951. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Topalidou M, Effraimidou S, Farmakiotis D,
Papadakis E, Papaioannou G, Korantzis I and Garipidou V: Low
protein Z levels, but not the intron F G79A polymorphism, are
associated with unexplained pregnancy loss. Thromb Res. 124:24–27.
2009. View Article : Google Scholar
|
|
37
|
Ghozlan MF, Mohamed AAE, Eissa DS and
Eldawy HS: Low protein Z level: A thrombophilic risk biomarker for
acute coronary syndrome. Indian J Hematol Blood Transfus.
35:339–346. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kulman JD, Harris JE, Haldeman BA and
Davie EW: Primary structure and tissue distribution of two novel
proline-rich gamma-carboxyglutamic acid proteins. Proc Natl Acad
Sci USA. 94:9058–9062. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kulman JD, Harris JE, Xie L and Davie EW:
Proline-rich Gla protein 2 is a cell-surface vitamin K-dependent
protein that binds to the transcriptional coactivator
Yes-associated protein. Proc Natl Acad Sci USA. 104:8767–8772.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kulman JD, Harris JE, Xie L and Davie EW:
Identification of two novel transmembrane gamma-carboxyglutamic
acid proteins expressed broadly in fetal and adult tissues. Proc
Natl Acad Sci USA. 98:1370–1375. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Iwamoto J: Vitamin K2 therapy
for postmenopausal osteoporosis. Nutrients. 6:1971–1980. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Mizokami A, Kawakubo-Yasukochi T and
Hirata M: Osteocalcin and its endocrine functions. Biochem
Pharmacol. 132:1–8. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wen L, Chen J, Duan L and Li S: Vitamin
K-dependent proteins involved in bone and cardiovascular health
(Review). Mol Med Rep. 18:3–15. 2018.PubMed/NCBI
|
|
44
|
Naito K, Watari T, Obayashi O, Katsube S,
Nagaoka I and Kaneko K: Relationship between serum
undercarboxylated osteocalcin and hyaluronan levels in patients
with bilateral knee osteoarthritis. Int J Mol Med. 29:756–760.
2012.PubMed/NCBI
|
|
45
|
Sweatt A, Sane DC, Hutson SM and Wallin R:
Matrix Gla protein (MGP) and bone morphogenetic protein-2 in aortic
calcified lesions of aging rats. J Thromb Haemost. 1:178–185. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yao Y, Zebboudj AF, Shao E, Perez M and
Boström K: Regulation of bone morphogenetic protein-4 by matrix GLA
protein in vascular endothelial cells involves activin-like kinase
receptor 1. J Biol Chem. 281:33921–33930. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Roy ME and Nishimoto SK: Matrix Gla
protein binding to hydroxyapatite is dependent on the ionic
environment: Calcium enhances binding affinity but phosphate and
magnesium decrease affinity. Bone. 31:296–302. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zuo PY, Chen XL, Lei YH, Liu CY and Liu
YW: Growth arrest-specific gene 6 protein promotes the
proliferation and migration of endothelial progenitor cells through
the PI3K/AKT signaling pathway. Int J Mol Med. 34:299–306. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Qiu C, Zheng H, Tao H, Yu W, Jiang X, Li
A, Jin H, Lv A and Li H: Vitamin K2 inhibits rat vascular smooth
muscle cell calcification by restoring the Gas6/Axl/Akt
anti-apoptotic pathway. Mol Cell Biochem. 433:149–159. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Jiang X, Tao H, Qiu C, Ma X, Li S, Guo X,
Lv A and Li H: Vitamin K2 regression aortic calcification induced
by warfarin via Gas6/Axl survival pathway in rats. Eur J Pharmacol.
786:10–18. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kawamoto A, Tkebuchava T, Yamaguchi J,
Nishimura H, Yoon YS, Milliken C, Uchida S, Masuo O, Iwaguro H, Ma
H, et al: Intramyocardial transplantation of autologous endothelial
progenitor cells for therapeutic neovascularization of myocardial
ischemia. Circulation. 107:461–468. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Jiang L, Liu CY, Yang QF, Wang P and Zhang
W: Plasma level of growth arrest-specific 6 (GAS6) protein and
genetic variations in the GAS6 gene in patients with acute coronary
syndrome. Am J Clin Pathol. 131:738–743. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Chen LW, Chen W, Hu ZQ, Bian JL, Ying L,
Hong GL, Qiu QM, Zhao GJ and Lu ZQ: Protective effects of growth
arrest-specific protein 6 (Gas6) on sepsis-induced acute kidney
injury. Inflammation. 39:575–582. 2016. View Article : Google Scholar
|
|
54
|
Novitskiy SV, Zaynagetdinov R, Vasiukov G,
Gutor S, Han W, Serezani A, Matafonov A, Gleaves LA, Sherrill TP,
Polosukhin VV and Blackwell TS: Gas6/MerTK signaling is negatively
regulated by NF-κB and supports lung carcinogenesis. Oncotarget.
10:7031–7042. 2019. View Article : Google Scholar
|
|
55
|
Eitzinger N, Surmann-Schmitt C, Bösl M,
Schett G, Engelke K, Hess A, von der Mark K and Stock M: Ucma is
not necessary for normal development of the mouse skeleton. Bone.
50:670–680. 2012. View Article : Google Scholar
|
|
56
|
Stock M, Menges S, Eitzinger N, Geßlein M,
Botschner R, Wormser L, Distler A, Schlötzer-Schrehardt U, Dietel
K, Distler J, et al: A dual role of upper zone of growth plate and
cartilage matrix-associated protein in human and mouse
osteoarthritic cartilage: Inhibition of aggrecanases and promotion
of bone turnover. Arthritis Rheumatol. 69:1233–1245. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Seuffert F, Weidner D, Baum W, Schett G
and Stock M: Upper zone of growth plate and cartilage matrix
associated protein protects cartilage during inflammatory
arthritis. Arthritis Res Ther. 20:882018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Cavaco S, Viegas CS, Rafael MS, Ramos A,
Magalhães J, Blanco FJ, Vermeer C and Simes DC: Gla-rich protein is
involved in the cross-talk between calcification and inflammation
in osteoarthritis. Cell Mol Life Sci. 73:1051–1065. 2016.
View Article : Google Scholar
|
|
59
|
Viegas CS, Cavaco S, Neves PL, Ferreira A,
João A, Williamson MK, Price PA, Cancela ML and Simes DC: Gla-rich
protein is a novel vitamin K-dependent protein present in serum
that accumulates at sites of pathological calcifications. Am J
Pathol. 175:2288–2298. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Lee YJ, Park SY, Lee SJ, Boo YC, Choi JY
and Kim JE: Ucma, a direct transcriptional target of Runx2 and
Osterix, promotes osteoblast differentiation and nodule formation.
Osteoarthritis Cartilage. 23:1421–1431. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
O'Grady S and Morgan MP:
Microcalcifications in breast cancer: From pathophysiology to
diagnosis and prognosis. Biochim Biophys Acta Rev Cancer.
1869:310–320. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Lee SH, Lee YJ, Park SI and Kim JE: Unique
cartilage matrix-associated protein inhibits the migratory and
invasive potential of triple-negative breast cancer. Biochem
Biophys Res Commun. 530:680–685. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Duchamp de Lageneste O, Julien A,
Abou-Khalil R, Frangi G, Carvalho C, Cagnard N, Cordier C, Conway
SJ and Colnot C: Periosteum contains skeletal stem cells with high
bone regenerative potential controlled by Periostin. Nat Commun.
9:7732018. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Zhu S, Barbe MF, Liu C, Hadjiargyrou M,
Popoff SN, Rani S, Safadi FF and Litvin J: Periostin-like-factor in
osteogenesis. J Cell Physiol. 218:584–592. 2009. View Article : Google Scholar
|
|
65
|
Cobo T, Viloria CG, Solares L, Fontanil T,
González-Chamorro E, De Carlos F, Cobo J, Cal S and Obaya AJ: Role
of periostin in adhesion and migration of bone remodeling cells.
PLoS One. 11:e01478372016. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Heo SC, Shin WC, Lee MJ, Kim BR, Jang IH,
Choi EJ, Lee JS and Kim JH: Periostin accelerates bone healing
mediated by human mesenchymal stem cell-embedded
hydroxyapatite/tricalcium phosphate scaffold. PLoS One.
10:e01166982015. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Kanisicak O, Khalil H, Ivey MJ, Karch J,
Maliken BD, Correll RN, Brody MJ, J Lin SC, Aronow BJ and Tallquist
MD: Genetic lineage tracing defines myofibroblast origin and
function in the injured heart. Nat Commun. 7:122602016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kaur H, Takefuji M, Ngai CY, Carvalho J,
Bayer J, Wietelmann A, Poetsch A, Hoelper S, Conway SJ, Möllmann H,
et al: Targeted ablation of periostin-expressing activated
fibroblasts prevents adverse cardiac remodeling in mice. Circ Res.
118:1906–1917. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Taniyama Y, Katsuragi N, Sanada F, Azuma
J, Iekushi K, Koibuchi N, Okayama K, Ikeda-Iwabu Y, Muratsu J, Otsu
R, et al: Selective blockade of periostin exon 17 preserves cardiac
performance in acute myocardial infarction. Hypertension.
67:356–361. 2016. View Article : Google Scholar
|
|
70
|
Izuhara K, Conway SJ, Moore BB, Matsumoto
H, Holweg CT, Matthews JG and Arron JR: Roles of periostin in
respiratory disorders. Am J Respir Crit Care Med. 193:949–956.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
James A, Janson C, Malinovschi A, Holweg
C, Alving K, Ono J, Ohta S, Ek A, Middelveld R, Dahlén B, et al:
Serum periostin relates to type-2 inflammation and lung function in
asthma: Data from the large population-based cohort Swedish
GA(2)LEN. Allergy. 72:1753–1760. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Litvin J, Blagg A, Mu A, Matiwala S,
Montgomery M, Berretta R, Houser S and Margulies K: Periostin and
periostin-like factor in the human heart: Possible therapeutic
targets. Cardiovasc Pathol. 15:24–32. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Zoch ML, Clemens TL and Riddle RC: New
insights into the biology of osteocalcin. Bone. 82:42–49. 2016.
View Article : Google Scholar
|
|
74
|
Cagman Z, Bingol Ozakpinar O, Cirakli Z,
Gedikbasi A, Ay P, Colantonio D, Uras AR, Adeli K and Uras F:
Reference intervals for growth arrest-specific 6 protein in adults.
Scand J Clin Lab Invest. 77:109–114. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Varnum BC, Young C, Elliott G, Garcia A,
Bartley TD, Fridell YW, Hunt RW, Trail G, Clogston C, Toso RJ, et
al: Axl receptor tyrosine kinase stimulated by the vitamin
K-dependent protein encoded by growth-arrest-specific gene 6.
Nature. 373:623–626. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Li M, Ye J, Zhao G, Hong G, Hu X, Cao K,
Wu Y and Lu Z: Gas6 attenuates lipopolysaccharide-induced TNF-α
expression and apoptosis in H9C2 cells through NF-κB and MAPK
inhibition via the Axl/PI3K/Akt pathway. Int J Mol Med. 44:982–994.
2019.PubMed/NCBI
|
|
77
|
Tanabe K, Nagata K, Ohashi K, Nakano T,
Arita H and Mizuno K: Roles of gamma-carboxylation and a sex
hormone-binding globulin-like domain in receptor-binding and in
biological activities of Gas6. FEBS Lett. 408:306–310. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Bellido-Martín L and de Frutos PG: Vitamin
K-dependent actions of Gas6. Vitam Horm. 78:185–209. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Wu G, Ma Z, Cheng Y, Hu W, Deng C, Jiang
S, Li T, Chen F and Yang Y: Targeting Gas6/TAM in cancer cells and
tumor microenvironment. Mol Cancer. 17:202018. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Melaragno MG, Cavet ME, Yan C, Tai LK, Jin
ZG, Haendeler J and Berk BC: Gas6 inhibits apoptosis in vascular
smooth muscle: Role of Axl kinase and Akt. J Mol Cell Cardiol.
37:881–887. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
McCloskey P, Fridell YW, Attar E, Villa J,
Jin Y, Varnum B and Liu ET: GAS6 mediates adhesion of cells
expressing the receptor tyrosine kinase Axl. J Biol Chem.
272:23285–23291. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Stenhoff J, Dahlbäck B and Hafizi S:
Vitamin K-dependent Gas6 activates ERK kinase and stimulates growth
of cardiac fibroblasts. Biochem Biophys Res Commun. 319:871–878.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Rizzoni D, Rizzoni M, Nardin M, Chiarini
G, Agabiti-Rosei C, Aggiusti C, Paini A, Salvetti M and Muiesan ML:
Vascular aging and disease of the small vessels. High Blood Press
Cardiovasc Prev. 26:183–189. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Jin CW, Wang H, Chen YQ, Tang MX, Fan GQ,
Wang ZH, Li L, Zhang Y, Zhang W and Zhong M: Gas6 delays senescence
in vascular smooth muscle cells through the PI3K/Akt/FoxO signaling
pathway. Cell Physiol Biochem. 35:1151–1166. 2015. View Article : Google Scholar
|
|
85
|
Clauser S, Meilhac O, Bièche I, Raynal P,
Bruneval P, Michel JB and Borgel D: Increased secretion of Gas6 by
smooth muscle cells in human atherosclerotic carotid plaques.
Thromb Haemost. 107:140–149. 2012. View Article : Google Scholar
|
|
86
|
Holden RM, Hétu MF, Li TY, Ward EC,
Couture LE, Herr JE, Christilaw E, Adams MA and Johri AM:
Circulating Gas6 is associated with reduced human carotid
atherosclerotic plaque burden in high risk cardiac patients. Clin
Biochem. 64:6–11. 2019. View Article : Google Scholar
|
|
87
|
Tjwa M, Moons L and Lutgens E: Pleiotropic
role of growth arrest-specific gene 6 in atherosclerosis. Curr Opin
Lipidol. 20:386–392. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Meir KS and Leitersdorf E: Atherosclerosis
in the apolipoprotein-E-deficient mouse: A decade of progress.
Arterioscler Thromb Vasc Biol. 24:1006–1014. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Park JK, Theuer S, Kirsch T, Lindschau C,
Klinge U, Heuser A, Plehm R, Todiras M, Carmeliet P, Haller H, et
al: Growth arrest specific protein 6 participates in DOCA-induced
target-organ damage. Hypertension. 54:359–364. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Zhao YF, Xu DC, Zhu GF, Zhu M, Tang K, Li
WM and Xu YW: Growth arrest-specific 6 exacerbates pressure
overload-induced cardiac hypertrophy. Hypertension. 67:118–129.
2016. View Article : Google Scholar
|
|
91
|
van der Meer JH, van der Poll T and van 't
Veer C: TAM receptors, Gas6, and protein S: Roles in inflammation
and hemostasis. Blood. 123:2460–2469. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Zhao GJ, Zheng JY, Bian JL, Chen LW, Dong
N, Yu Y, Hong GL, Chandoo A, Yao YM and Lu ZQ: Growth
arrest-specific 6 enhances the suppressive function of
CD4+CD25+ regulatory T cells mainly through
axl receptor. Mediators Inflamm. 2017:68484302017.
|
|
93
|
Haase VH: Mechanisms of hypoxia responses
in renal tissue. J Am Soc Nephrol. 24:537–541. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Giangola MD, Yang WL, Rajayer SR,
Kuncewitch M, Molmenti E, Nicastro J, Coppa GF and Wang P: Growth
arrest-specific protein 6 protects against renal
ischemia-reperfusion injury. J Surg Res. 199:572–579. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Ishimoto Y, Ohashi K, Mizuno K and Nakano
T: Promotion of the uptake of PS liposomes and apoptotic cells by a
product of growth arrest-specific gene, gas6. J Biochem.
127:411–417. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Lee IJ, Hilliard B, Swami A, Madara JC,
Rao S, Patel T, Gaughan JP, Lee J, Gadegbeku CA, Choi ET and Cohen
PL: Growth arrest-specific gene 6 (Gas6) levels are elevated in
patients with chronic renal failure. Nephrol Dial Transplant.
27:4166–4172. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Hallajzadeh J, Ghorbanihaghjo A, Argani H,
Dastmalchi S and Rashtchizadeh N: Growth arrest-specific 6 protein
and matrix Gla protein in hemodialysis patients. Iran J Kidney Dis.
9:249–255. 2015.PubMed/NCBI
|
|
98
|
Panichi V, Migliori M, De Pietro S,
Taccola D, Bianchi AM, Giovannini L, Norpoth M, Metelli MR,
Cristofani R, Bertelli AAE, et al: C-reactive protein and
interleukin-6 levels are related to renal function in predialytic
chronic renal failure. Nephron. 91:594–600. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Weiner DE, Tabatabai S, Tighiouart H,
Elsayed E, Bansal N, Griffith J, Salem DN, Levey AS and Sarnak MJ:
Cardiovascular outcomes and all-cause mortality: Exploring the
interaction between CKD and cardiovascular disease. Am J Kidney
Dis. 48:392–401. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Silaghi CN, Ilyés T, Filip VP, Farca M,
van Ballegooijen AJ and Crăciun AM: Vitamin K dependent proteins in
kidney disease. Int J Mol Sci. 20:15712019. View Article : Google Scholar :
|
|
101
|
Wu CS, Hu CY, Tsai HF, Chyuan IT, Chan CJ,
Chang SK and Hsu PN: Elevated serum level of growth arrest-specific
protein 6 (Gas6) in systemic lupus erythematosus patients is
associated with nephritis and cutaneous vasculitis. Rheumatol Int.
34:625–629. 2014. View Article : Google Scholar
|
|
102
|
Nagai K, Miyoshi M, Kake T, Fukushima N,
Matsuura M, Shibata E, Yamada S, Yoshikawa K, Kanayama HO, Fukawa
T, et al: Dual involvement of growth arrest-specific gene 6 in the
early phase of human IgA nephropathy. PLoS One. 8:e667592013.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Nagai K, Arai H, Yanagita M, Matsubara T,
Kanamori H, Nakano T, Iehara N, Fukatsu A, Kita T and Doi T: Growth
arrest-specific gene 6 is involved in glomerular hypertrophy in the
early stage of diabetic nephropathy. J Biol Chem. 278:18229–18234.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Nagai K, Matsubara T, Mima A, Sumi E,
Kanamori H, Iehara N, Fukatsu A, Yanagita M, Nakano T, Ishimoto Y,
et al: Gas6 induces Akt/mTOR-mediated mesangial hypertrophy in
diabetic nephropathy. Kidney Int. 68:552–561. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Hung YJ, Lee CH, Chu NF and Shieh YS:
Plasma protein growth arrest-specific 6 levels are associated with
altered glucose tolerance, inflammation, and endothelial
dysfunction. Diabetes Care. 33:1840–1844. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Li W, Wang J, Ge L, Shan J, Zhang C and
Liu J: Growth arrest-specific protein 6 (Gas6) as a noninvasive
biomarker for early detection of diabetic nephropathy. Clin Exp
Hypertens. 39:382–387. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Tian W, Wang L, Yuan L, Duan W, Zhao W,
Wang S and Zhang Q: A prognostic risk model for patients with
triple negative breast cancer based on stromal natural killer
cells, tumor-associated macrophages and growth-arrest specific
protein 6. Cancer Sci. 107:882–889. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Ammoun S, Provenzano L, Zhou L, Barczyk M,
Evans K, Hilton DA, Hafizi S and Hanemann CO: Axl/Gas6/NFκB
signalling in schwannoma pathological proliferation, adhesion and
survival. Oncogene. 33:336–346. 2014. View Article : Google Scholar
|
|
109
|
Buehler M, Tse B, Leboucq A, Jacob F,
Caduff R, Fink D, Goldstein DR and Heinzelmann-Schwarz V:
Meta-analysis of microarray data identifies GAS6 expression as an
independent predictor of poor survival in ovarian cancer. Biomed
Res Int. 2013:2382842013. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Loges S, Schmidt T, Tjwa M, van Geyte K,
Lievens D, Lutgens E, Vanhoutte D, Borgel D, Plaisance S, Hoylaerts
M, et al: Malignant cells fuel tumor growth by educating
infiltrating leukocytes to produce the mitogen Gas6. Blood.
115:2264–2273. 2010. View Article : Google Scholar
|
|
111
|
Waizenegger JS, Ben-Batalla I, Weinhold N,
Meissner T, Wroblewski M, Janning M, Riecken K, Binder M,
Atanackovic D, Taipaleenmaeki H, et al: Role of growth
arrest-specific gene 6-Mer axis in multiple myeloma. Leukemia.
29:696–704. 2015. View Article : Google Scholar
|
|
112
|
Husain H, Scur M, Murtuza A, Bui N,
Woodward B and Kurzrock R: Strategies to overcome bypass mechanisms
mediating clinical resistance to EGFR tyrosine kinase inhibition in
lung cancer. Mol Cancer Ther. 16:265–272. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Paolino M, Choidas A, Wallner S, Pranjic
B, Uribesalgo I, Loeser S, Jamieson AM, Langdon WY, Ikeda F, Fededa
JP, et al: The E3 ligase Cbl-b and TAM receptors regulate cancer
metastasis via natural killer cells. Nature. 507:508–512. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Viegas CS, Simes DC, Laizé V, Williamson
MK, Price PA and Cancela ML: Gla-rich protein (GRP), a new vitamin
K-dependent protein identified from sturgeon cartilage and highly
conserved in vertebrates. J Biol Chem. 283:36655–36664. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Viegas CS, Rafael MS, Enriquez JL,
Teixeira A, Vitorino R, Luís IM, Costa RM, Santos S, Cavaco S,
Neves J, et al: Gla-rich protein acts as a calcification inhibitor
in the human cardiovascular system. Arterioscler Thromb Vasc Biol.
35:399–408. 2015. View Article : Google Scholar
|
|
116
|
Surmann-Schmitt C, Dietz U, Kireva T, Adam
N, Park J, Tagariello A, Onnerfjord P, Heinegård D,
Schlötzer-Schrehardt U, Deutzmann R, et al: Ucma, a novel secreted
cartilage-specific protein with implications in osteogenesis. J
Biol Chem. 283:7082–7093. 2008. View Article : Google Scholar
|
|
117
|
Neacsu CD, Grosch M, Tejada M, Winterpacht
A, Paulsson M, Wagener R and Tagariello A: Ucmaa (Grp-2) is
required for zebrafish skeletal development. Evidence for a
functional role of its glutamate γ-carboxylation. Matrix Biol.
30:369–378. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Cancela ML, Conceição N and Laizé V:
Gla-rich protein, a new player in tissue calcification? Adv Nutr.
3:174–181. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Mackie EJ, Tatarczuch L and Mirams M: The
skeleton: A multi-functional complex organ: The growth plate
chondrocyte and endochondral ossification. J Endocrinol.
211:109–121. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Granadeiro L, Dirks RP, Ortiz-Delgado JB,
Gavaia PJ, Sarasquete C, Laizé V, Cancela ML and Fernández I:
Warfarin-exposed zebrafish embryos resembles human warfarin
embryopathy in a dose and developmental-time dependent manner-from
molecular mechanisms to environmental concerns. Ecotoxicol Environ
Saf. 181:559–571. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
R Sousa A, Barreira R and Santos E:
Low-dose warfarin maternal anticoagulation and fetal warfarin
syndrome. BMJ Case Rep. 2018:bcr20172231592018. View Article : Google Scholar
|
|
122
|
Maruotti N, Corrado A and Cantatore FP:
Osteoblast role in osteoarthritis pathogenesis. J Cell Physiol.
232:2957–2963. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Sanchez C, Deberg MA, Piccardi N, Msika P,
Reginster JYL and Henrotin YE: Subchondral bone osteoblasts induce
phenotypic changes in human osteoarthritic chondrocytes.
Osteoarthritis Cartilage. 13:988–997. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Sokolove J and Lepus CM: Role of
inflammation in the pathogenesis of osteoarthritis: Latest findings
and interpretations. Ther Adv Musculoskelet Dis. 5:77–94. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Okuyan HM, Terzi MY, Ozcan O and Kalaci A:
Association of UCMA levels in serum and synovial fluid with
severity of knee osteoarthritis. Int J Rheum Dis. 22:1884–1890.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Misra D, Booth SL, Tolstykh I, Felson DT,
Nevitt MC, Lewis CE, Torner J and Neogi T: Vitamin K deficiency is
associated with incident knee osteoarthritis. Am J Med.
126:243–248. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Hunt JL, Fairman R, Mitchell ME, Carpenter
JP, Golden M, Khalapyan T, Wolfe M, Neschis D, Milner R, Scoll B,
et al: Bone formation in carotid plaques: A clinicopathological
study. Stroke. 33:1214–1219. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Cozzolino M, Fusaro M, Ciceri P, Gasperoni
L and Cianciolo G: The role of vitamin K in vascular calcification.
Adv Chronic Kidney Dis. 26:437–444. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Hruska KA: Vascular smooth muscle cells in
the pathogenesis of vascular calcification. Circ Res. 104:710–711.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Dhore CR, Cleutjens JP, Lutgens E,
Cleutjens KB, Geusens PP, Kitslaar PJ, Tordoir JH, Spronk HM,
Vermeer C and Daemen MJ: Differential expression of bone matrix
regulatory proteins in human atherosclerotic plaques. Arterioscler
Thromb Vasc Biol. 21:1998–2003. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Kapustin AN and Shanahan CM: Calcium
regulation of vascular smooth muscle cell-derived matrix vesicles.
Trends Cardiovasc Med. 22:133–137. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Kapustin AN, Davies JD, Reynolds JL,
McNair R, Jones GT, Sidibe A, Schurgers LJ, Skepper JN, Proudfoot
D, Mayr M and Shanahan CM: Calcium regulates key components of
vascular smooth muscle cell-derived matrix vesicles to enhance
mineralization. Circ Res. 109:e1–e12. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Toroian D, Lim JE and Price PA: The size
exclusion characteristics of type I collagen: Implications for the
role of noncollagenous bone constituents in mineralization. J Biol
Chem. 282:22437–22447. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Price PA, Toroian D and Lim JE:
Mineralization by inhibitor exclusion: The calcification of
collagen with fetuin. J Biol Chem. 284:17092–17101. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
135
|
New SEP and Aikawa E: Molecular imaging
insights into early inflammatory stages of arterial and aortic
valve calcification. Circ Res. 108:1381–1391. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Ikeda K, Souma Y, Akakabe Y, Kitamura Y,
Matsuo K, Shimoda Y, Ueyama T, Matoba S, Yamada H, Okigaki M and
Matsubara H: Macrophages play a unique role in the plaque
calcification by enhancing the osteogenic signals exerted by
vascular smooth muscle cells. Biochem Biophys Res Commun.
425:39–44. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
New SEP, Goettsch C, Aikawa M, Marchini
JF, Shibasaki M, Yabusaki K, Libby P, Shanahan CM, Croce K and
Aikawa E: Macrophage-derived matrix vesicles: An alternative novel
mechanism for microcalcification in atherosclerotic plaques. Circ
Res. 113:72–77. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Evrard S, Delanaye P, Kamel S, Cristol JP
and Cavalier E: SFBC/SN joined working group on vascular
calcifications: Vascular calcification: From pathophysiology to
biomarkers. Clin Chim Acta. 438:401–414. 2015. View Article : Google Scholar
|
|
139
|
Tesfamariam B: Involvement of vitamin
K-dependent proteins in vascular calcification. J Cardiovasc
Pharmacol Ther. 24:323–333. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Viegas CSB, Santos L, Macedo AL, Matos AA,
Silva AP, Neves PL, Staes A, Gevaert K, Morais R, Vermeer C, et al:
Chronic kidney disease circulating calciprotein particles and
extracellular vesicles promote vascular calcification: A role for
GRP (Gla-Rich Protein). Arterioscler Thromb Vasc Biol. 38:575–587.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Pasch A, Farese S, Gräber S, Wald J,
Richtering W, Floege J and Jahnen-Dechent W: Nanoparticle-based
test measures overall propensity for calcification in serum. J Am
Soc Nephrol. 23:1744–1752. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Viegas CSB, Costa RM, Santos L, Videira
PA, Silva Z, Araújo N, Macedo AL, Matos AP, Vermeer C and Simes DC:
Gla-rich protein function as an anti-inflammatory agent in
monocytes/macrophages: Implications for calcification-related
chronic inflammatory diseases. PLoS One. 12:e01778292017.
View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Willems BA, Furmanik M, Caron MMJ, Chatrou
MLL, Kusters DHM, Welting TJM, Stock M, Rafael MS, Viegas CSB,
Simes DC, et al: Ucma/GRP inhibits phosphate-induced vascular
smooth muscle cell calcification via SMAD-dependent BMP signalling.
Sci Rep. 8:49612018. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Karamouzis MV, Likaki-Karatza E, Ravazoula
P, Badra FA, Koukouras D, Tzorakoleftherakis E, Papavassiliou AG
and Kalofonos HP: Non-palpable breast carcinomas: Correlation of
mammographically detected malignant-appearing microcalcifications
and molecular prognostic factors. Int J Cancer. 102:86–90. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Kim JH, Ko ES, Kim DY, Han H, Sohn JH and
Choe DH: Noncalcified ductal carcinoma in situ: Imaging and
histologic findings in 36 tumors. J Ultrasound Med. 28:903–910.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Avdan Aslan A, Gültekin S, Esendağli
Yilmaz G and Kurukahvecioğlu O: Is there any association between
mammographic features of microcalcifications and breast cancer
subtypes in ductal carcinoma in situ? Acad Radiol. Jun
30–2020.Online ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Viegas CS, Herfs M, Rafael MS, Enriquez
JL, Teixeira A, Luís IM, van 't Hoofd CM, João A, Maria VL, Cavaco
S, et al: Gla-rich protein is a potential new vitamin K target in
cancer: Evidences for a direct GRP-mineral interaction. Biomed Res
Int. 2014:3402162014. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Huisse MG, Leclercq M, Belghiti J, Flejou
JF, Suttie JW, Bezeaud A, Stafford DW and Guillin MC: Mechanism of
the abnormal vitamin K-dependent gamma-carboxylation process in
human hepatocellular carcinomas. Cancer. 74:1533–1541. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Pasierski T: Vitamin K antagonists in
anticoagulant therapy of patients with cancer. Pol Arch Med Wewn.
122:60–64. 2012.PubMed/NCBI
|
|
150
|
Vermeer C: Vitamin K: The effect on health
beyond coagulation-an overview. Food Nutr Res. 56:2012. View Article : Google Scholar
|
|
151
|
Cox RF, Hernandez-Santana A, Ramdass S,
McMahon G, Harmey JH and Morgan MP: Microcalcifications in breast
cancer: Novel insights into the molecular mechanism and functional
consequence of mammary mineralisation. Br J Cancer. 106:525–537.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Takeshita S, Kikuno R, Tezuka K and Amann
E: Osteoblast-specific factor 2: Cloning of a putative bone
adhesion protein with homology with the insect protein fasciclin I.
Biochem J. 294:271–278. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Coutu DL, Wu JH, Monette A, Rivard GE,
Blostein MD and Galipeau J: Periostin, a member of a novel family
of vitamin K-dependent proteins, is expressed by mesenchymal
stromal cells. J Biol Chem. 283:17991–8001. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Zhong H, Li X, Zhang J and Wu X:
Overexpression of periostin is positively associated with gastric
cancer metastasis through promoting tumor metastasis and invasion.
J Cell Biochem. 120:9927–9935. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Nakazawa T, Nakajima A, Seki N, Okawa A,
Kato M, Moriya H, Amizuka N, Einhorn TA and Yamazaki M: Gene
expression of periostin in the early stage of fracture healing
detected by cDNA microarray analysis. J Orthop Res. 22:520–525.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Li W, Gao P, Zhi Y, Xu W, Wu Y, Yin J and
Zhang J: Periostin: Its role in asthma and its potential as a
diagnostic or therapeutic target. Respir Res. 16:572015. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Duchamp de Lageneste O and Colnot C:
Periostin in bone regeneration. Adv Exp Med Biol. 1132:49–61. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Ai-Aql ZS, Alagl AS, Graves DT,
Gerstenfeld LC and Einhorn TA: Molecular mechanisms controlling
bone formation during fracture healing and distraction
osteogenesis. J Dent Res. 87:107–118. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Einhorn TA and Gerstenfeld LC: Fracture
healing: Mechanisms and interventions. Nat Rev Rheumatol. 11:45–54.
2015. View Article : Google Scholar :
|
|
160
|
Zhang X, Xie C, Lin AS, Ito H, Awad H,
Lieberman JR, Rubery PT, Schwarz EM, O'Keefe RJ and Guldberg RE:
Periosteal progenitor cell fate in segmental cortical bone graft
transplantations: Implications for functional tissue engineering. J
Bone Miner Res. 20:2124–2137. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Neagu TP, Ţigliş M, Cocoloş I and Jecan
CR: The relationship between periosteum and fracture healing. Rom J
Morphol Embryol. 57:1215–1220. 2016.
|
|
162
|
Kudo A: Periostin in bone biology. Adv Exp
Med Biol. 1132:43–47. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Allen MR, Hock JM and Burr DB: Periosteum:
Biology, regulation, and response to osteoporosis therapies. Bone.
35:1003–1012. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Kashima TG, Nishiyama T, Shimazu K,
Shimazaki M, Kii I, Grigoriadis AE, Fukayama M and Kudo A:
Periostin, a novel marker of intramembranous ossification, is
expressed in fibrous dysplasia and in c-Fos-overexpressing bone
lesions. Hum Pathol. 40:226–237. 2009. View Article : Google Scholar
|
|
165
|
Varughese R, Semprini R, Munro C,
Fingleton J, Holweg C, Weatherall M, Beasley R and Braithwaite I:
Serum periostin levels following small bone fractures, long bone
fractures and joint replacements: An observational study. Allergy
Asthma Clin Immunol. 14:302018. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Roberts SJ, van Gastel N, Carmeliet G,
Carmeliet G and Luyten FP: Uncovering the periosteum for skeletal
regeneration: The stem cell that lies beneath. Bone. 70:10–18.
2015. View Article : Google Scholar
|
|
167
|
Matsuzawa M, Arai C, Nomura Y, Murata T,
Yamakoshi Y, Oida S, Hanada N and Nakamura Y: Periostin of human
periodontal ligament fibroblasts promotes migration of human
mesenchymal stem cell through the αvβ3 integrin/FAK/PI3K/Akt
pathway. J Periodont Res. 50:855–863. 2015. View Article : Google Scholar
|
|
168
|
Hwang EY, Jeong MS, Park EK, Kim JH and
Jang SB: Structural characterization and interaction of periostin
and bone morphogenetic protein for regulation of collagen
cross-linking. Biochem Biophys Res Commun. 449:425–431. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Rezaieyazdi Z, Falsoleiman H, Khajehdaluee
M, Saghafi M and Mokhtari-Amirmajdi E: Reduced bone density in
patients on long-term warfarin. Int J Rheum Dis. 12:130–135. 2009.
View Article : Google Scholar
|
|
170
|
Tufano A, Coppola A, Contaldi P, Franchini
M and Minno GD: Oral anticoagulant drugs and the risk of
osteoporosis: New anticoagulants better than old? Semin Thromb
Hemost. 41:382–388. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Jeong HM, Cho DH, Jin YH, Chung JO, Chung
MY, Chung DJ and Lee KY: Inhibition of osteoblastic differentiation
by warfarin and 18-α-glycyrrhetinic acid. Arch Pharm Res.
34:1381–1387. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Verma D, Kumar R, Pereira RS, Karantanou
C, Zanetti C, Minciacchi VR, Fulzele K, Kunz K, Hoelper S,
Zia-Chahabi S, et al: Vitamin K antagonism impairs the bone marrow
microenvironment and hematopoiesis. Blood. 134:227–238. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Sugimoto I, Hirakawa K, Ishino T, Takeno S
and Yajin K: Vitamin D3, vitamin K2, and warfarin regulate bone
metabolism in human paranasal sinus bones. Rhinology. 45:208–213.
2007.PubMed/NCBI
|
|
174
|
Rousseau JC, Sornay-Rendu E, Bertholon C,
Chapurlat R and Garnero P: Serum periostin is associated with
fracture risk in postmenopausal women: A 7-year prospective
analysis of the OFELY study. J Clin Endocrinol Metab. 99:2533–2539.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Kim BJ, Rhee Y, Kim CH, Baek KH, Min YK,
Kim DY, Ahn SH, Kim H, Lee SH, Lee SY, et al: Plasma periostin
associates significantly with non-vertebral but not vertebral
fractures in post-menopausal women: Clinical evidence for the
different effects of periostin depending on the skeletal site.
Bone. 81:435–441. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Rousseau JC, Sornay-Rendu E, Bertholon C,
Garnero P and Chapurlat R: Serum periostin is associated with
prevalent knee osteoarthritis and disease incidence/progression in
women: The OFELY study. Osteoarthr Cartil. 23:1736–1742. 2015.
View Article : Google Scholar
|
|
177
|
Snider P, Hinton RB, Moreno-Rodriguez RA,
Wang J, Rogers R, Lindsley A, Li F, Ingram DA, Menick D, Field L,
et al: Periostin is required for maturation and extracellular
matrix stabilization of noncardiomyocyte lineages of the heart.
Circ Res. 102:752–760. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Nagaraju CK, Robinson EL, Abdesselem M,
Trenson S, Dries E, Gilbert G, Janssens S, Van Cleemput J, Rega F,
Meyns B, et al: Myofibroblast phenotype and reversibility of
fibrosis in patients with end-stage heart failure. J Am Coll
Cardiol. 73:2267–2282. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Zheng X, Wang S, Zou X, Jing Y, Yang R, Li
S and Wang F: Ginsenoside Rb1 improves cardiac function and
remodeling in heart failure. Exp Anim. 66:217–228. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Chen Z, Xie J, Hao H, Lin H, Wang L, Zhang
Y, Chen L, Cao S, Huang X, Liao W, et al: Ablation of periostin
inhibits post-infarction myocardial regeneration in neonatal mice
mediated by the phosphatidylinositol 3 kinase/glycogen synthase
kinase 3β/cyclin D1 signalling pathway. Cardiovasc Res.
113:620–632. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Hixson JE, Shimmin LC, Montasser ME, Kim
DK, Zhong Y, Ibarguen H, Follis J, Malcom G, Strong J, Howard T, et
al: Common variants in the periostin gene influence development of
atherosclerosis in young persons. Arterioscler Thromb Vasc Biol.
31:1661–1667. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Hakuno D, Kimura N, Yoshioka M, Mukai M,
Kimura T, Okada Y, Yozu R, Shukunami C, Hiraki Y, Kudo A, et al:
Periostin advances atherosclerotic and rheumatic cardiac valve
degeneration by inducing angiogenesis and MMP production in humans
and rodents. J Clin Invest. 120:2292–2306. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Lindner V, Wang Q, Conley BA, Friesel RE
and Vary CP: Vascular injury induces expression of periostin:
Implications for vascular cell differentiation and migration.
Arterioscler Thromb Vasc Biol. 25:77–83. 2005. View Article : Google Scholar
|
|
184
|
Schwanekamp JA, Lorts A, Vagnozzi RJ,
Vanhoutte D and Molkentin JD: Deletion of periostin protects
against atherosclerosis in mice by altering inflammation and
extracellular matrix remodeling. Arterioscler Thromb Vasc Biol.
36:60–68. 2016. View Article : Google Scholar
|
|
185
|
Ahlfeld SK, Gao Y, Wang J, Horgusluoglu E,
Bolanis E, Clapp DW and Conway SJ: Periostin downregulation is an
early marker of inhibited neonatal murine lung alveolar septation.
Birth Defects Res A Clin Mol Teratol. 97:373–385. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Bozyk PD, Bentley JK, Popova AP, Anyanwu
AC, Linn MD, Goldsmith AM, Pryhuber GS, Moore BB and Hershenson MB:
Neonatal periostin knockout mice are protected from
hyperoxia-induced alveolar simplication. PLoS One. 7:e313362012.
View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Naik PK, Bozyk PD, Bentley JK, Popova AP,
Birch CM, Wilke CA, Fry CD, White ES, Sisson TH, Tayob N, et al:
Periostin promotes fibrosis and predicts progression in patients
with idiopathic pulmonary fibrosis. Am J Physiol Lung Cell Mol
Physiol. 303:L1046–L1056. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Kanemitsu Y, Suzuki M, Fukumitsu K, Asano
T, Takeda N, Nakamura Y, Ozawa Y, Masaki A, Ono J, Kurokawa R, et
al: A novel pathophysiologic link between upper and lower airways
in patients with chronic rhinosinusitis: Association of sputum
periostin levels with upper airway inflammation and olfactory
function. World Allergy Organ J. 13:1000942020. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Katoh S, Matsumoto N, Tanaka H, Yasokawa
N, Kittaka M, Kurose K, Abe M, Yoshioka D, Shirai R, Nakazato M and
Kobashi Y: Elevated levels of periostin and TGF-β1 in the
bronchoalveolar lavage fluid of patients with idiopathic
eosinophilic pneumonia. Asian Pac J Allergy Immunol. 38:208–213.
2020.
|
|
190
|
Tanaka J, Hebisawa A, Oguma T, Tomomatsu
K, Suzuki J, Shimizu H, Kawabata Y, Ishiguro T, Takayanagi N, Ueda
S, et al: Evaluating serum periostin levels in allergic
bronchopulmonary aspergillosis. Allergy. 75:974–977. 2020.
View Article : Google Scholar
|
|
191
|
Wilson MS and Wynn TA: Pulmonary fibrosis:
Pathogenesis, etiology and regulation. Mucosal Immunol. 2:103–121.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Behr J, Kreuter M, Hoeper MM, Wirtz H,
Klotsche J, Koschel D, Andreas S, Claussen M, Grohé C, Wilkens H,
et al: Management of patients with idiopathic pulmonary fibrosis in
clinical practice: The INSIGHTS-IPF registry. Eur Respir J.
46:186–196. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Okamoto M, Hoshino T, Kitasato Y, Sakazaki
Y, Kawayama T, Fujimoto K, Ohshima K, Shiraishi H, Uchida M, Ono J,
et al: Periostin, a matrix protein, is a novel biomarker for
idiopathic interstitial pneumonias. Eur Respir J. 37:1119–1127.
2011. View Article : Google Scholar
|
|
194
|
Nance T, Smith KS, Anaya V, Richardson R,
Ho L, Pala M, Mostafavi S, Battle A, Feghali-Bostwick C, Rosen G
and Montgomery SB: Transcriptome analysis reveals differential
splicing events in IPF lung tissue. PLoS One. 9:e975502014.
View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Ashley SL, Wilke CA, Kim KK and Moore BB:
Periostin regulates fibrocyte function to promote myofibroblast
differentiation and lung fibrosis. Mucosal Immunol. 10:341–351.
2017. View Article : Google Scholar :
|
|
196
|
Yoshihara T, Nanri Y, Nunomura S,
Yamaguchi Y, Feghali-Bostwick C, Ajito K, Murakami S, Mawatari M
and Izuhara K: Periostin plays a critical role in the cell cycle in
lung fibroblasts. Respir Res. 21:382020. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Nanri Y, Nunomura S, Terasaki Y, Yoshihara
T, Hirano Y, Yokosaki Y, Yamaguchi Y, Feghali-Bostwick C, Ajito K,
Murakami S, et al: Cross-talk between transforming growth
factor-beta and periostin can be targeted for pulmonary fibrosis.
Am J Respir Cell Mol Biol. 62:204–216. 2020. View Article : Google Scholar
|
|
198
|
De Brouwer B, Piscaer I, Von Der Thusen
JH, Grutters JC, Schutgens RE, Wouters EF and Janssen R: Should
vitamin K be supplemented instead of antagonised in patients with
idiopathic pulmonary fibrosis? Expert Rev Respir Med. 12:169–175.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Woodruff PG, Boushey HA, Dolganov GM,
Barker CS, Yang YH, Donnelly S, Ellwanger A, Sidhu SS, Dao-Pick TP,
Pantoja C, et al: Genome-wide profiling identifies epithelial cell
genes associated with asthma and with treatment response to
corticosteroids. Proc Natl Acad Sci USA. 104:15858–15863. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Izuhara K, Nunomura S, Nanri Y, Ogawa M,
Ono J, Mitamura Y and Yoshihara T: Periostin in inflammation and
allergy. Cell Mol Life Sci. 74:4293–4303. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Tartibi HM and Bahna SL: Clinical and
biological markers of asthma control. Expert Rev Clin Immunol.
10:1453–1461. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Johansson MW, Annis DS and Mosher DF:
α(M)β(2) integrin-mediated adhesion and motility of IL-5-stimulated
eosinophils on periostin. Am J Respir Cell Mol Biol. 48:503–510.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Sidhu SS, Yuan S, Innes AL, Kerr S,
Woodruff PG, Hou L, Muller SJ and Fahy JV: Roles of epithelial
cell-derived periostin in TGF-beta activation, collagen production,
and collagen gel elasticity in asthma. Proc Natl Acad Sci USA.
107:14170–14175. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Kimur I, Tanizaki Y, Sato S, Saito K and
Takahashi K: Menaquinone (vitamin K2) therapy for bronchial asthma.
II. Clinical effect of menaquinone on bronchial asthma. Acta medica
Okayama. 29:127–135. 1975.PubMed/NCBI
|
|
205
|
Litonjua AA: Fat-soluble vitamins and
atopic disease: What is the evidence? Proc Nutr Soc. 71:67–74.
2012. View Article : Google Scholar :
|
|
206
|
El Basha NR, Osman HM, Abdelaal AA, Saed
SM and Shaaban HH: Increased expression of serum periostin and
YKL40 in children with severe asthma and asthma exacerbation. J
Investig Med. 66:1102–1108. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Matsusaka M, Kabata H, Fukunaga K, Suzuki
Y, Masaki K, Mochimaru T, Sakamaki F, Oyamada Y, Inoue T, Oguma T,
et al: Phenotype of asthma related with high serum periostin
levels. Allergol Int. 64:175–180. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Kim MA, Izuhara K, Ohta S, Ono J, Yoon MK,
Ban GY, Yoo HS, Shin YS, Ye YM, Nahm DH and Park HS: Association of
serum periostin with aspirin-exacerbated respiratory disease. Ann
Allergy Asthma Immunol. 113:314–320. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
209
|
Asano T, Kanemitsu Y, Takemura M, Yokota
M, Fukumitsu K, Takeda N, Ichikawa H, Uemura T, Takakuwa O, Ohkubo
H, et al: Serum periostin as a biomarker for comorbid chronic
rhinosinusitis in patients with asthma. Ann Am Thorac Soc.
14:667–675. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Cianchetti S, Cardini C, Puxeddu I,
Latorre M, Bartoli ML, Bradicich M, Dente F, Bacci E, Celi A and
Paggiaro P: Distinct profile of inflammatory and remodelling
biomarkers in sputum of severe asthmatic patients with or without
persistent airway obstruction. World Allergy Organ J.
12:1000782019. View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Li Y, Chen JP, Duan L and Li S: Effect of
vitamin K2 on type 2 diabetes mellitus: A review. Diabetes Res Clin
Pract. 136:39–51. 2018. View Article : Google Scholar
|
|
212
|
Mukai K, Morimoto H, Kikuchi S and Nagaoka
S: Kinetic study of free-radical-scavenging action of biological
hydroquinones (reduced forms of ubiquinone, vitamin K and
tocopherol quinone) in solution. Biochim Biophys Acta.
1157:313–317. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
213
|
Westhofen P, Watzka M, Marinova M, Hass M,
Kirfel G, Müller J, Bevans CG, Müller CR and Oldenburg J: Human
vitamin K 2,3-epoxide reductase complex subunit 1-like 1 (VKORC1L1)
mediates vitamin K-dependent intracellular anti-oxidant function. J
Biol Chem. 286:15085–15094. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
214
|
Vos M, Esposito G, Edirisinghe JN, Vilain
S, Haddad DM, Slabbaert JR, Van Meensel S, Schaap O, De Strooper B,
Meganathan R, et al: Vitamin K2 is a mitochondrial electron carrier
that rescues pink1 deficiency. Science. 336:1306–1310. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Fujii S, Shimizu A, Takeda N, Oguchi K,
Katsurai T, Shirakawa H, Komai M and Kagechika H: Systematic
synthesis and anti-inflammatory activity of ω-carboxylated
menaquinone derivatives-investigations on identified and putative
vitamin K2 metabolites. Bioorg Med Chem. 23:2344–2352. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
216
|
Myneni VD and Mezey E: Immunomodulatory
effect of vitamin K2: Implications for bone health. Oral Dis.
24:67–71. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
217
|
Ishizuka M, Kubota K, Shimoda M, Kita J,
Kato M, Park KH and Shiraki T: Effect of menatetrenone, a vitamin
k2 analog, on recurrence of hepatocellular carcinoma after surgical
resection: A prospective randomized controlled trial. Anticancer
Res. 32:5415–5420. 2012.PubMed/NCBI
|
|
218
|
Zhong JH, Mo XS, Xiang BD, Yuan WP, Jiang
JF, Xie GS and Li LQ: Postoperative use of the chemopreventive
vitamin K2 analog in patients with hepatocellular carcinoma. PLoS
One. 8:e580822013. View Article : Google Scholar : PubMed/NCBI
|
|
219
|
Enomoto M, Tsuchida A, Miyazawa K,
Yokoyama T, Kawakita H, Tokita H, Naito M, Itoh M, Ohyashiki K and
Aoki T: Vitamin K2-induced cell growth inhibition via autophagy
formation in cholangiocellular carcinoma cell lines. Int J Mol Med.
20:801–808. 2007.PubMed/NCBI
|
|
220
|
Sibayama-Imazu T, Fujisawa Y, Masuda Y,
Aiuchi T, Nakajo S, Itabe H and Nakaya K: Induction of apoptosis in
PA-1 ovarian cancer cells by vitamin K2 is associated with an
increase in the level of TR3/Nur77 and its accumulation in
mitochondria and nuclei. J Cancer Res Clin Oncol. 134:803–812.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
221
|
Showalter SL, Wang Z, Costantino CL,
Witkiewicz AK, Yeo CJ, Brody JR and Carr BI: Naturally occurring K
vitamins inhibit pancreatic cancer cell survival through a
caspase-dependent pathway. J Gastroenterol Hepatol. 25:738–744.
2010. View Article : Google Scholar
|
|
222
|
Xv F, Chen J, Duan L and Li S: Research
progress on the anticancer effects of vitamin K2. Oncol Lett.
15:8926–8934. 2018.PubMed/NCBI
|