|
1
|
International Diabetes Federation (IDF):
IDF Diabetes Atlas. 8th Edition. IDF; 2017, https://www.diabetesatlas.org/upload/resources/previous/files/8/IDF_DA_8e-EN-final.pdf.
|
|
2
|
Logue J, Walker JJ, Colhoun HM, Leese GP,
Lindsay RS, McKnight JA, Morris AD, Pearson DW, Petrie JR, Philip
S, et al: Do men develop type 2 diabetes at lower body mass indices
than women? Diabetologia. 54:3003–3006. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hartwig S, Greiser KH, Medenwald D, Tiller
D, Herzog B, Schipf S, Ittermann T, Völzke H, Müller G, Haerting J
and Kluttig A: Association of change of anthropometric measurements
with incident type 2 diabetes mellitus: A pooled analysis of the
prospective population-based CARLA and SHIP cohort studies.
Medicine(Baltimore). 94:e13942015.
|
|
4
|
Wannamethee SG, Papacosta O, Lawlor DA,
Whincup PH, Lowe GD, Ebrahim S and Sattar N: Do women exhibit
greater differences in established and novel risk factors between
diabetes and non-diabetes than men? the British regional heart
study and British women's heart health study. Diabetologia.
55:80–87. 2012. View Article : Google Scholar
|
|
5
|
Shigiyama F, Kumashiro N, Tsuneoka Y,
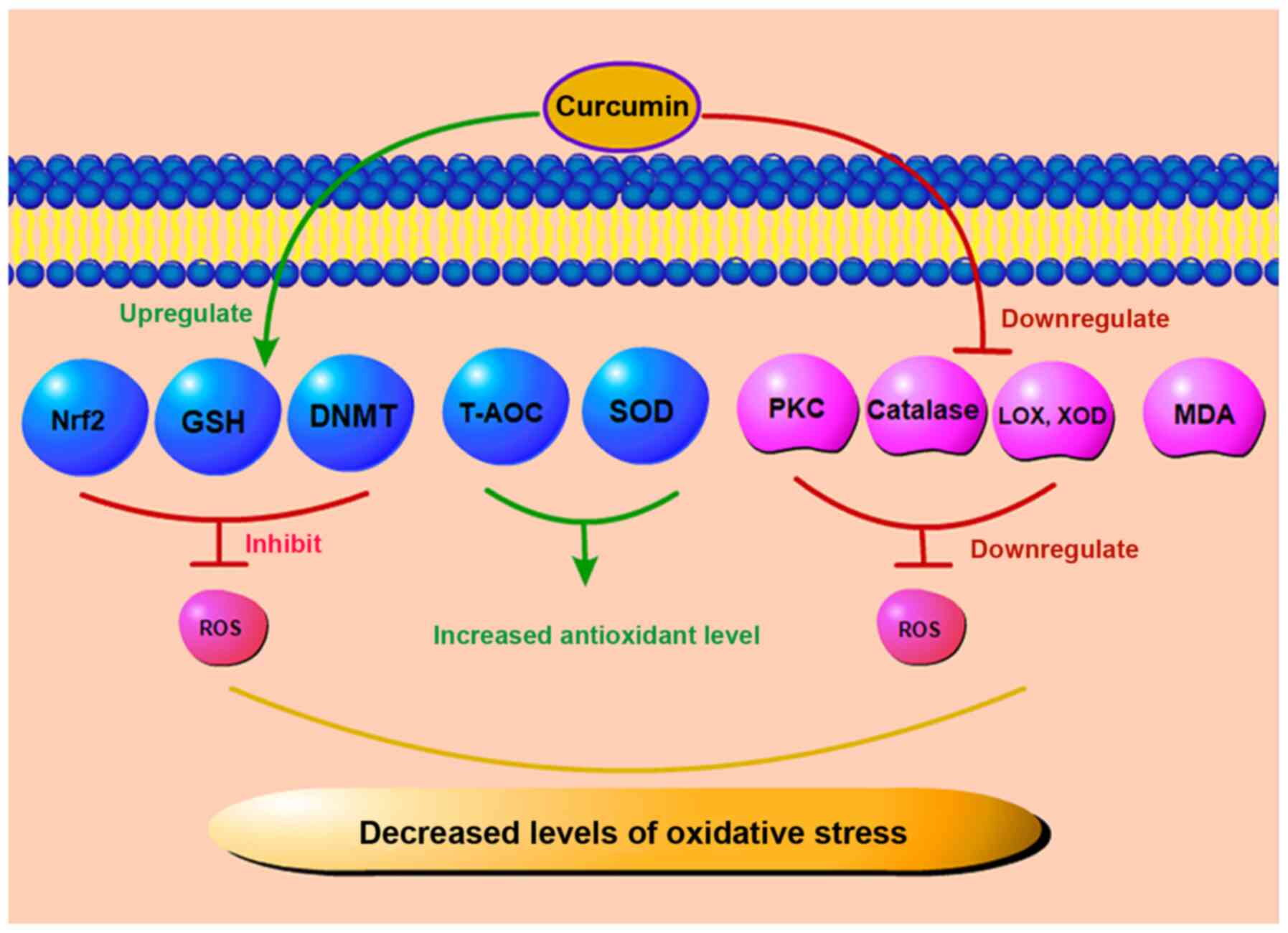
Igarashi H, Yoshikawa F, Kakehi S, Funato H and Hirose T:
Mechanisms of sleep deprivation-induced hepatic steatosis and
insulin resistance in mice. Am J Physiol Endocrinol Metab.
315:E848–E858. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
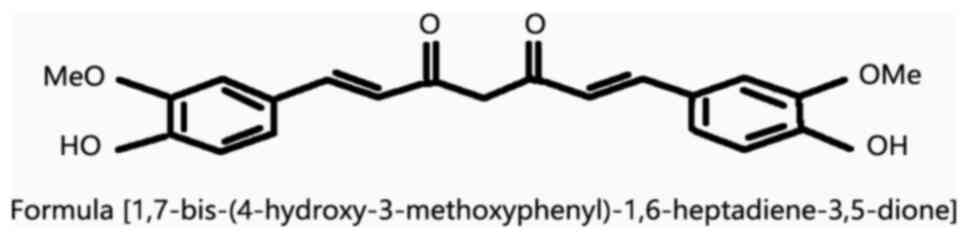
|
Pan KY, Xu W, Mangialasche F, Fratiglioni
L and Wang HX: Work-related psychosocial stress and the risk of
type 2 diabetes in later life. J Intern Med. 281:601–610. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sohn EH, van Dijk HW, Jiao C, Kok PHB,
Jeong W, Demirkaya N, Garmager A, Wit F, Kucukevcilioglu M, van
Velthoven ME, et al: Retinal neurodegeneration may precede
microvascular changes characteristic of diabetic retinopathy in
diabetes mellitus. Proc Natl Acad Sci USA. 113:E2655–E2664. 2016.
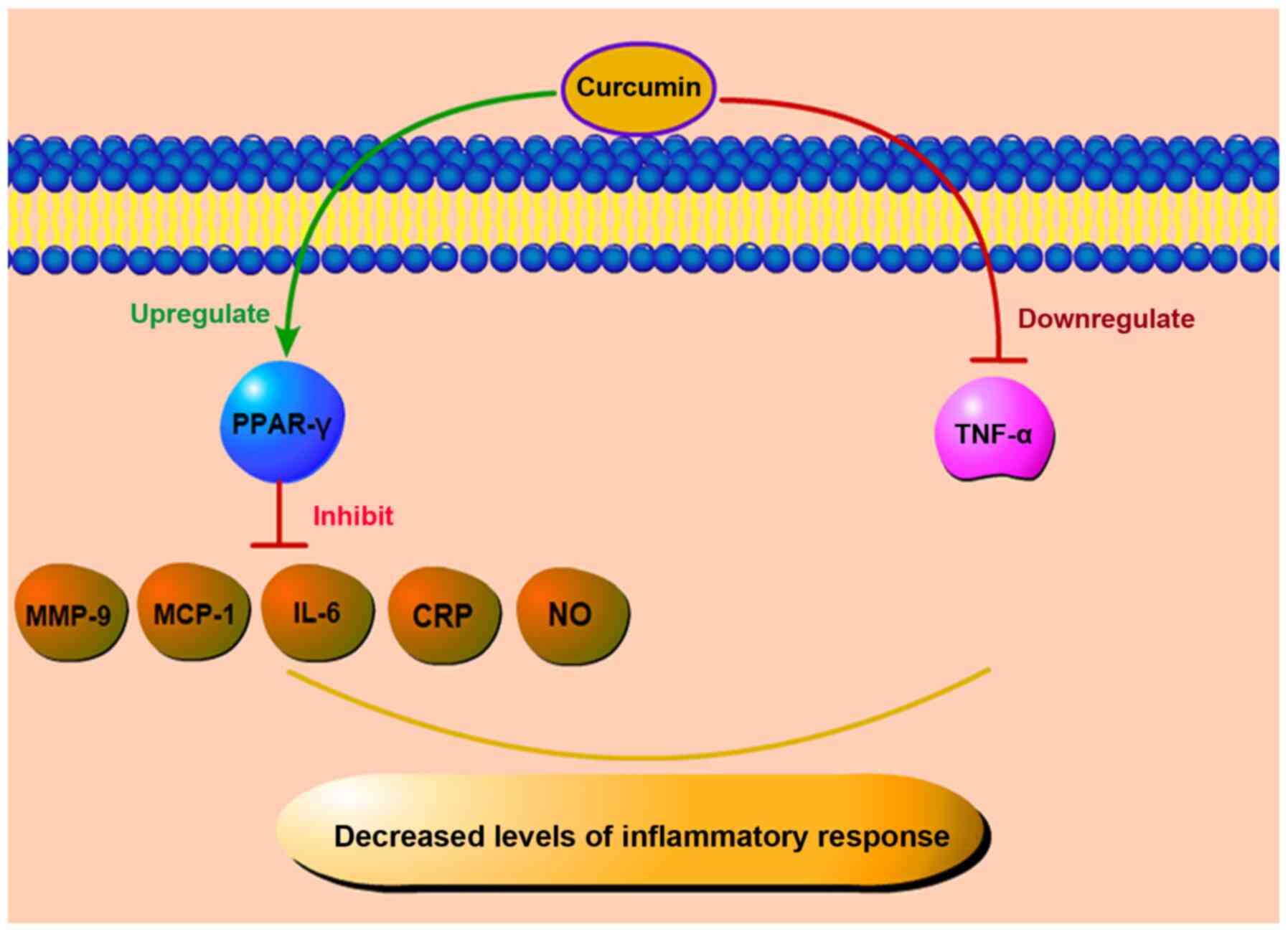
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sahin K, Orhan C, Tuzcu M, Sahin N, Tastan
H, Özercan IH, Güler O, Kahraman N, Kucuk O and Ozpolat B:
Chemopreventive and antitumor efficacy of curcumin in a
spontaneously developing hen ovarian cancer model. Cancer Prev Res
(Phila). 11:59–67. 2018. View Article : Google Scholar
|
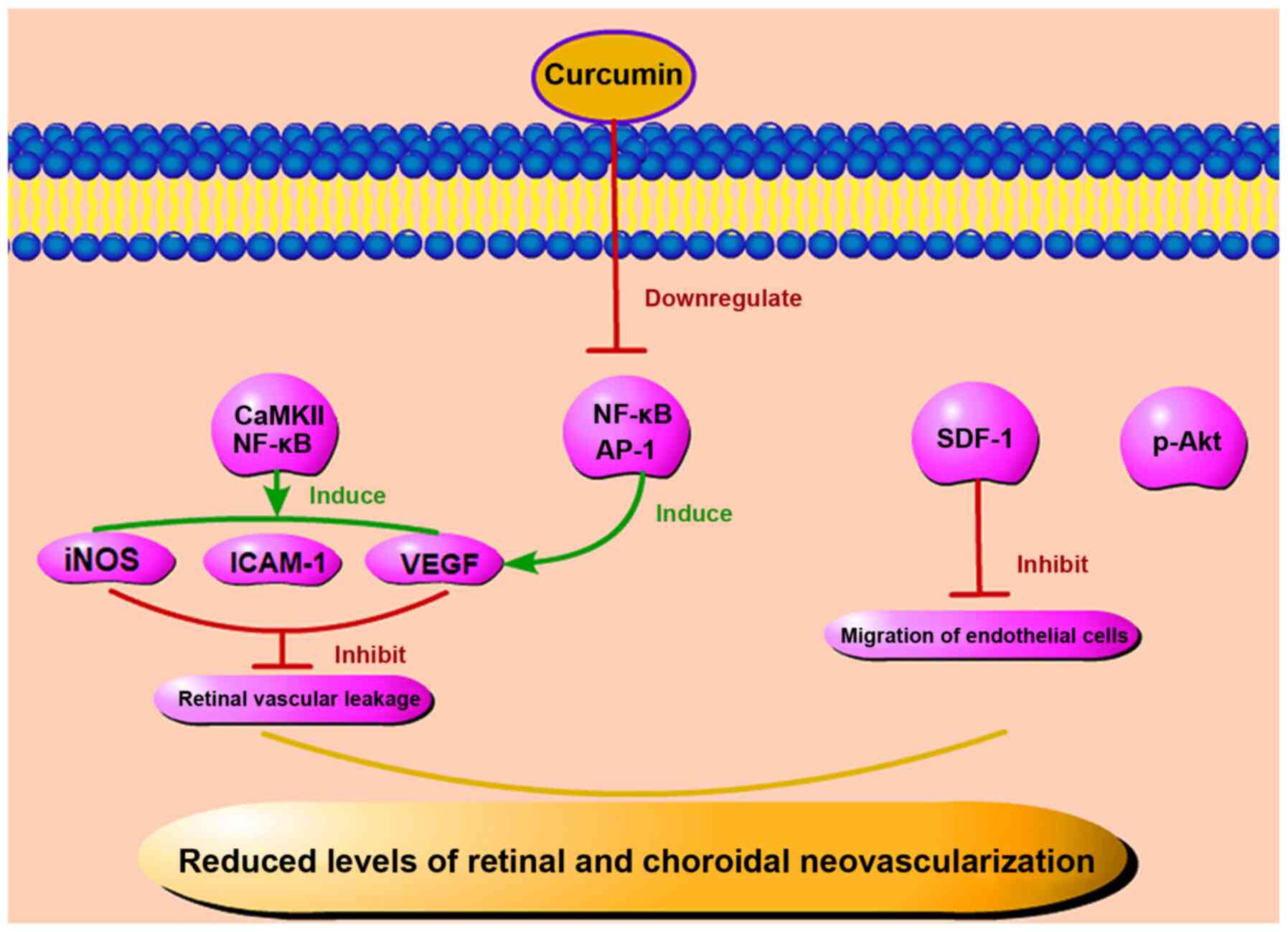
|
9
|
Fu H, Wang C, Yang D, Wei Z, Xu J, Hu Z,
Zhang Y, Wang W, Yan R and Cai Q: Curcumin regulates proliferation,
autophagy, and apoptosis in gastric cancer cells by affecting PI3K
and P53 signaling. J Cell Physiol. 233:4634–4642. 2018. View Article : Google Scholar
|
|
10
|
Kronski E, Fiori ME, Barbieri O, Astigiano
S, Mirisola V, Killian PH, Bruno A, Pagani A, Rovera F, Pfeffer U,
et al: miR181b is induced by the chemopreventive polyphenol
curcumin and inhibits breast cancer metastasis via down-regulation
of the inflammatory cytokines CXCL1 and -2. Mol Oncol. 8:581–595.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ide H, Lu Y, Noguchi T, Muto S, Okada H,
Kawato S and Horie S: Modulation of AKR1C2 by curcumin decreases
testosterone production in prostate cancer. Cancer Sci.
109:1230–1238. 2018. View Article : Google Scholar : PubMed/NCBI
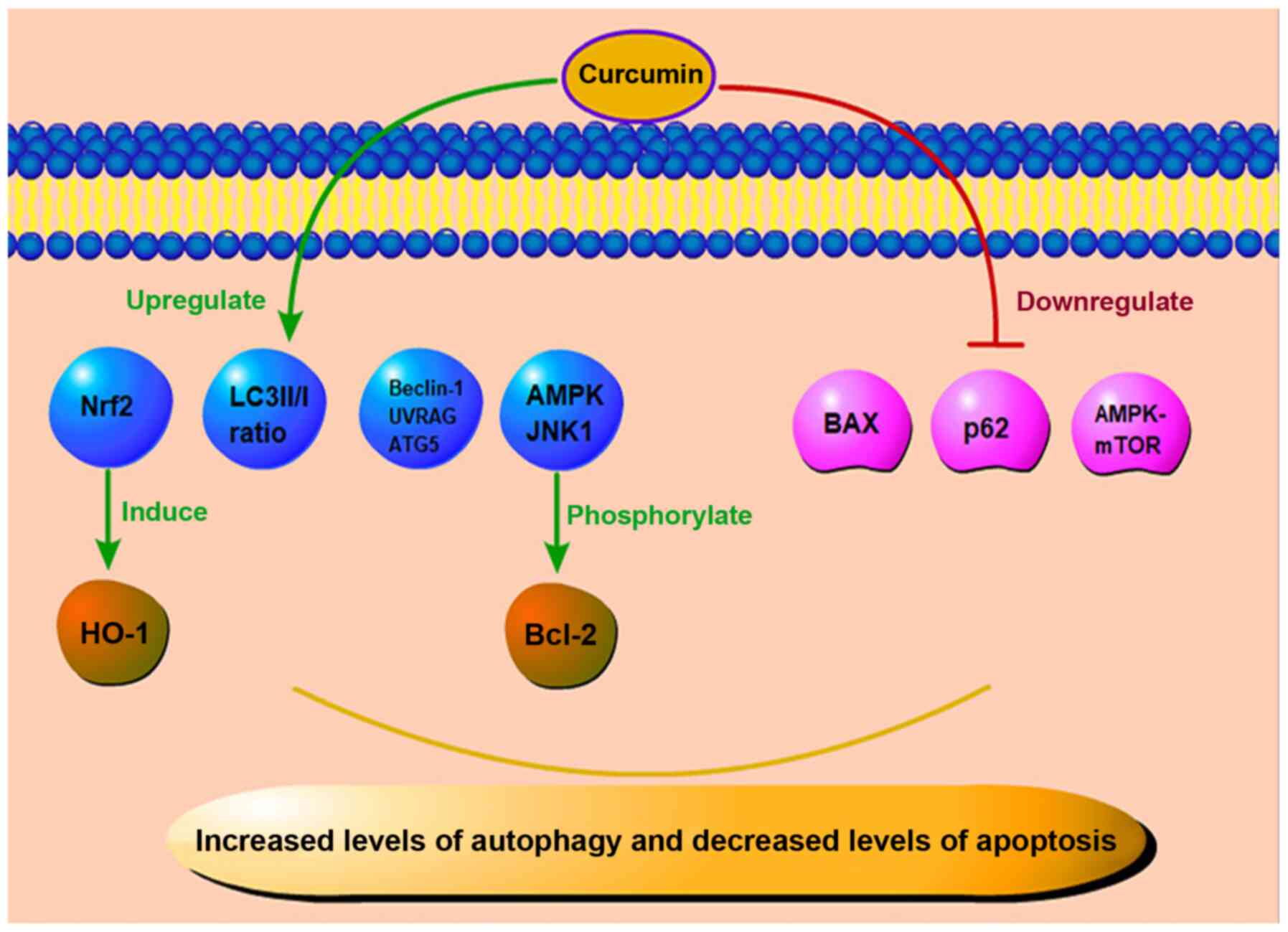
|
|
12
|
Yuan J, Liu R, Ma Y, Zhang Z and Xie Z:
Curcumin attenuates airway inflammation and airway remolding by
inhibiting NF-κB signaling and COX-2 in cigarette smoke-induced
COPD mice. Inflammation. 41:1804–1814. 2018. View Article : Google Scholar : PubMed/NCBI
|
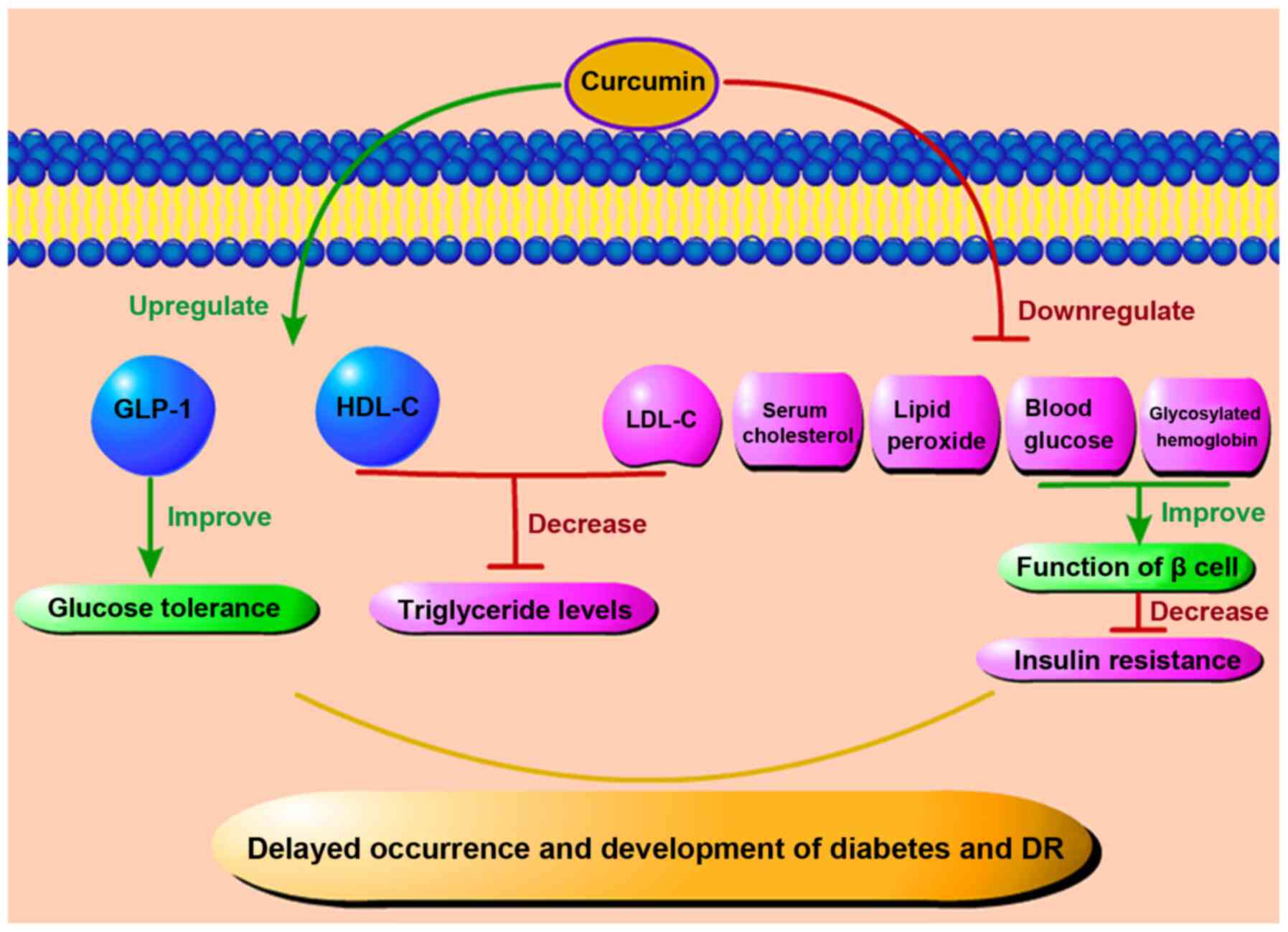
|
13
|
Ding XQ, Wu WY, Jiao RQ, Gu TT, Xu Q, Pan
Y and Kong LD: Curcumin and allopurinol ameliorate fructose-induced
hepatic inflammation in rats via miR-200a-mediated TXNIP/NLRP3
inflammasome inhibition. Pharmacol Res. 137:64–75. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xiao Y, Xia J, Wu S, Lv Z, Huang S, Huang
H, Su X, Cheng J and Ke Y: Curcumin inhibits acute vascular
inflammation through the activation of heme oxygenase-1. Oxid Med
Cell Longev. 2018:32958072018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sharma S, Kulkarni SK and Chopra K:
Curcumin, the active principle of turmeric (Curcuma longa),
ameliorates diabetic nephropathy in rats. Clin Exp Pharmacol
Physiol. 33:940–945. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kadiyala CSR, Zheng L, Du Y, Yohannes E,
Kao HY, Miyagi M and Kern TS: Acetylation of retinal histones in
diabetes increases inflammatory proteins: Effects of minocycline
and manipulation of histone acetyltransferase (HAT) and histone
deacetylase (HDAC). J Biol Chem. 287:25869–25880. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang LL, Chen H, Huang K and Zheng L:
Elevated histone acetylations in Müller cells contribute to
inflammation: A novel inhibitory effect of minocycline. Glia.
60:1896–1905. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yun JM, Jialal I and Devaraj S: Epigenetic
regulation of high glucose-induced proinflammatory cytokine
production in monocytes by curcumin. J Nutr Biochem. 22:450–458.
2011. View Article : Google Scholar
|
|
19
|
Gui L, Jiang S, Xie D, Yu L, Huang Y,
Zhang Z and Liu Y: Analysis of complete chloroplast genomes of
Curcuma and the contribution to phylogeny and adaptive evolution.
Gene. 732:1443552020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nishino H, Tokuda H, Satomi Y, Masuda M,
Osaka Y, Yogosawa S, Wada S, Mou XY, Takayasu J, Murakoshi M, et
al: Cancer prevention by antioxidants. Biofactors. 22:57–61. 2004.
View Article : Google Scholar
|
|
21
|
Boyanapalli SSS, Huang Y, Su Z, Cheng D,
Zhang C, Guo Y, Rao R, Androulakis IP and Kong AN: Pharmacokinetics
and pharmacodynamics of curcumin in regulating anti-inflammatory
and epigenetic gene expression. Biopharm Drug Dispos. 39:289–297.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lao CD, Ruffin MT, Normolle D, Heath DD,
Murray SI, Bailey JM, Boggs ME, Crowell J, Rock CL and Brenner DE:
Dose escalation of a curcuminoid formulation. BMC Complement Altern
Med. 6:102006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Falconieri MC, Adamo M, Monasterolo C,
Bergonzi MC, Coronnello M and Bilia AR: New dendrimer-based
nanoparticles enhance curcumin solubility. Planta Med. 83:420–425.
2017.
|
|
24
|
Tiyaboonchai W, Tungpradit W and
Plianbangchang P: Formulation and characterization of curcuminoids
loaded solid lipid nanoparticles. Int J Pharm. 337:299–306. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wang W, Zhu R, Xie Q, Li A, Xiao Y, Li K,
Liu H, Cui D, Chen Y and Wang S: Enhanced bioavailability and
efficiency of curcumin for the treatment of asthma by its
formulation in solid lipid nanoparticles. Int J Nanomedicine.
7:3667–3677. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Shoba G, Joy D, Joseph T, Majeed M,
Rajendran R and Srinivas PS: Influence of piperine on the
pharmacokinetics of curcumin in animals and human volunteers.
Planta Med. 64:353–356. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Skoupa N, Dolezel P, Ruzickova E and
Mlejnek P: Apoptosis induced by the curcumin analogue EF-24 is
neither mediated by oxidative stress-related mechanisms nor
affected by expression of main drug transporters ABCB1 and ABCG2 in
human leukemia cells. Int J Mol Sci. 18:22892017. View Article : Google Scholar :
|
|
28
|
Ingelfinger JR and Jarcho JA: Increase in
the incidence of diabetes and its implications. N Engl J Med.
376:1473–1474. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Javidi MA, Kaeidi A, Mortazavi Farsani SS,
Babashah S and Sadeghizadeh M: Investigating curcumin potential for
diabetes cell therapy, in vitro and in vivo study. Life Sci.
239:1169082019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chuengsamarn S, Rattanamongkolgul S,
Luechapudiporn R, Phisalaphong C and Jirawatnotai S: Curcumin
extract for prevention of type 2 diabetes. Diabetes Care.
35:2121–2127. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Al-Saud NBS: Impact of curcumin treatment
on diabetic albino rats. Saudi J Biol Sci. 27:689–694. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Qihui L, Shuntian D, Xin Z, Xiaoxia Y and
Zhongpei C: Protection of curcumin against streptozocin-induced
pancreatic cell destruction in T2D rats. Planta Med. 86:113–120.
2020. View Article : Google Scholar
|
|
33
|
Bulboacă AE, Boarescu PM, Bolboacă SD,
Blidaru M, Feștilă D, Dogaru G and Nicula CA: Comparative effect of
curcumin versus liposomal curcumin on systemic pro-inflammatory
cytokines profile, MCP-1 and RANTES in experimental diabetes
mellitus. Int J Nanomedicine. 14:8961–8972. 2019. View Article : Google Scholar
|
|
34
|
Li J, Wu N, Chen X, Chen H, Yang X and Liu
C: Curcumin protects islet cells from glucolipotoxicity by
inhibiting oxidative stress and NADPH oxidase activity both in
vitro and in vivo. Islets. 11:152–164. 2019. View Article : Google Scholar
|
|
35
|
Xia ZH, Jiang X, Li K, Li LX, Chen WB,
Wang YX and Liu YQ: Curcumin inhibits alloxan-induced pancreatic
islet cell damage via antioxidation and antiapoptosis. J Biochem
Mol Toxicol. 34:e224992020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Gupta A, Tripathi AK, Tripathi RL, Madhu
SV and Banerjee BD: Advanced glycosylated end products-mediated
activation of polymorphonuclear neutrophils in diabetes mellitus
and associated oxidative stress. Indian J Biochem Biophys.
44:373–378. 2007.
|
|
37
|
Aplin AC, Gelati M, Fogel E, Carnevale E
and Nicosia RF: Angiopoietin-1 and vascular endothelial growth
factor induce expression of inflammatory cytokines before
angiogenesis. Physiol Genomics. 27:20–28. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kowluru RA and Kanwar M: Effects of
curcumin on retinal oxidative stress and inflammation in diabetes.
Nutr Metab (Lond). 4:82007. View Article : Google Scholar
|
|
39
|
Assis RP, Arcaro CA, Gutierres VO,
Oliveira JO, Costa PI, Baviera AM and Brunetti IL: Combined effects
of curcumin and lycopene or bixin in yoghurt on inhibition of LDL
oxidation and increases in HDL and paraoxonase levels in
streptozotocin-diabetic rats. Int J Mol Sci. 18:3322017. View Article : Google Scholar :
|
|
40
|
Gutierres VO, Pinheiro CM, Assis RP,
Vendramini RC, Pepato MT and Brunetti IL: Curcumin-supplemented
yoghurt improves physiological and biochemical markers of
experimental diabetes. Br J Nutr. 108:440–448. 2012. View Article : Google Scholar
|
|
41
|
Jiménez-Osorio AS, González-Reyes S and
Pedraza-Chaverri J: Natural Nrf2 activators in diabetes. Clin Chim
Acta. 448:182–192. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zuo ZF, Zhang Q and Liu XZ: Protective
effects of curcumin on retinal Müller cell in early diabetic rats.
Int J Ophthalmol. 6:422–424. 2013.
|
|
43
|
Liu Z, Lin H, Ye S, Liu QY, Meng Z, Zhang
CM, Xia Y, Margoliash E, Rao Z and Liu XJ: Remarkably high
activities of testicular cytochrome c in destroying reactive oxygen
species and in triggering apoptosis. Proc Natl Acad Sci USA.
103:8965–8970. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Maugeri A, Mazzone MG, Giuliano F,
Vinciguerra M, Basile G, Barchitta M and Agodi A: Curcumin
modulates DNA methyltransferase functions in a cellular model of
diabetic retinopathy. Oxid Med Cell Longev. 2018:54074822018.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Shishodia S, Sethi G and Aggarwal BB:
Curcumin: Getting back to the roots. Ann N Y Acad Sci.
1056:206–217. 2005. View Article : Google Scholar
|
|
46
|
Chen Y, Li C, Duan S, Yuan X, Liang J and
Hou S: Curcumin attenuates potassium oxonate-induced hyperuricemia
and kidney inflammation in mice. Biomed Pharmacother.
118:1091952019. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Balasubramanyam M, Koteswari AA, Kumar RS,
Monickaraj SF, Maheswari JU and Mohan V: Curcumin-induced
inhibition of cellular reactive oxygen species generation: Novel
therapeutic implications. J Biosci. 28:715–721. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Yang F, Yu J, Ke F, Lan M and Li D, Tan K,
Ling J, Wang Y, Wu K and Li D: Curcumin alleviates diabetic
retinopathy in experimental diabetic rats. Ophthalmic Res.
60:43–54. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Bulboacă AE, Porfire AS, Tefas LR,
Boarescu PM, Bolboacă SD, Stănescu IC, Bulboacă AC and Dogaru G:
Liposomal curcumin is better than curcumin to alleviate
complications in experimental diabetic mellitus. Molecules.
24:8462019. View Article : Google Scholar
|
|
50
|
Zhou P, Xie W, Meng X, Zhai Y, Dong X,
Zhang X, Sun G and Sun X: Notoginsenoside R1 ameliorates diabetic
retinopathy through PINK1-dependent activation of mitophagy. Cells.
8:2132019. View Article : Google Scholar :
|
|
51
|
Brucklacher RM, Patel KM, VanGuilder HD,
Bixler GV, Barber AJ, Antonetti DA, Lin CM, LaNoue KF, Gardner TW,
Bronson SK and Freeman WM: Whole genome assessment of the retinal
response to diabetes reveals a progressive neurovascular
inflammatory response. BMC Med Genomics. 1:262008. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yuuki T, Kanda T, Kimura Y, Kotajima N,
Tamura J, Kobayashi I and Kishi S: Inflammatory cytokines in
vitreous fluid and serum of patients with diabetic
vitreoretinopathy. J Diabetes Complications. 15:257–259. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Joussen AM, Murata T, Tsujikawa A,
Kirchhof B, Bursell SE and Adamis AP: Leukocyte-mediated
endothelial cell injury and death in the diabetic retina. Am J
Pathol. 158:147–152. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Khalfaoui T, Lizard G and Ouertani-Meddeb
A: Adhesion molecules (ICAM-1 and VCAM-1) and diabetic retinopathy
in type 2 diabetes. J Mol Histol. 39:243–249. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Boss JD, Singh PK, Pandya HK, Tosi J, Kim
C, Tewari A, Juzych MS, Abrams GW and Kumar A: Assessment of
neurotrophins and inflammatory mediators in vitreous of patients
with diabetic retinopathy. Invest Ophthalmol Vis Sci. 58:5594–5603.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Luo DW, Zheng Z, Wang H, Fan Y, Chen F,
Sun Y, Wang WJ, Sun T and Xu X: UPP mediated diabetic retinopathy
via ROS/PARP and NF-κB inflammatory factor pathways. Curr Mol Med.
15:790–799. 2015. View Article : Google Scholar
|
|
57
|
Hollanders K, Van Hove I, Sergeys J, Van
Bergen T, Lefevere E, Kindt N, Castermans K, Vandewalle E, van Pelt
J, Moons L and Stalmans I: AMA0428, a potent rock inhibitor,
attenuates early and late experimental diabetic retinopathy. Curr
Eye Res. 42:260–272. 2017. View Article : Google Scholar
|
|
58
|
Ran Z, Zhang Y, Wen X and Ma J: Curcumin
inhibits high glucose induced inflammatory injury in human retinal
pigment epithelial cells through the ROS PI3K/AKT/mTOR signaling
pathway. Mol Med Rep. 19:1024–1031. 2019.
|
|
59
|
Costagliola C, Romano V, De Tollis M,
Aceto F, dell'Omo R, Romano MR, Pedicino C and Semeraro F:
TNF-alpha levels in tears: A novel biomarker to assess the degree
of diabetic retinopathy. Mediators Inflamm. 2013:6295292013.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Gupta SK, Kumar B, Nag TC, Agrawal SS,
Agrawal R, Agrawal P, Saxena R and Srivastava S: Curcumin prevents
experimental diabetic retinopathy in rats through its hypoglycemic,
anti-oxidant, and anti-inflammatory mechanisms. J Ocul Pharmacol
Ther. 27:123–130. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Jiang C, Ting AT and Seed B: PPAR-gamma
agonists inhibit production of monocyte inflammatory cytokines.
Nature. 391:82–86. 1998. View
Article : Google Scholar : PubMed/NCBI
|
|
62
|
Charrier A, Wang L, Stephenson EJ, Ghanta
SV, Ko CW, Croniger CM, Bridges D and Buchner DA: Zinc finger
protein 407 overexpression upregulates PPAR target gene expression
and improves glucose homeostasis in mice. Am J Physiol Endocrinol
Metab. 311:E869–E880. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Aljada A, Garg R, Ghanim H, Mohanty P,
Hamouda W, Assian E and Dandona P: Nuclear factor-kappaB
suppressive and inhibitor-kappaB stimulatory effects of
troglitazone in obese patients with type 2 diabetes: Evidence of an
antiinflammatory action? J Clin Endocrinol Metab. 86:3250–3256.
2001.PubMed/NCBI
|
|
64
|
Haffner SM, Greenberg AS, Weston WM, Chen
H, Williams K and Freed MI: Effect of rosiglitazone treatment on
nontraditional markers of cardiovascular disease in patients with
type 2 diabetes mellitus. Circulation. 106:679–684. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Shafabakhsh R, Mobini M, Raygan F,
Aghadavod E, Ostadmohammadi V, Amirani E, Mansournia MA and Asemi
Z: Curcumin administration and the effects on psychological status
and markers of inflammation and oxidative damage in patients with
type 2 diabetes and coronary heart disease. Clin Nutr ESPEN.
40:77–82. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Li HY, Yang M, Li Z and Meng Z: Curcumin
inhibits angiotensin II-induced inflammation and proliferation of
rat vascular smooth muscle cells by elevating PPAR-γ activity and
reducing oxidative stress. Int J Mol Med. 39:1307–1316. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Yun JH, Park SW, Kim KJ, Bae JS, Lee EH,
Paek SH, Kim SU, Ye S, Kim JH and Cho CH: Endothelial STAT3
activation increases vascular leakage through downregulating tight
junction proteins: Implications for diabetic retinopathy. J Cell
Physiol. 232:1123–1134. 2017. View Article : Google Scholar
|
|
68
|
Shibuya M: Vascular endothelial growth
factor and its receptor system: Physiological functions in
angiogenesis and pathological roles in various diseases. J Biochem.
153:13–19. 2013. View Article : Google Scholar
|
|
69
|
Miyamoto K, Khosrof S, Bursell SE, Rohan
R, Murata T, Clermont AC, Aiello LP, Ogura Y and Adamis AP:
Prevention of leukostasis and vascular leakage in
streptozotocin-induced diabetic retinopathy via intercellular
adhesion molecule-1 inhibition. Proc Natl Acad Sci USA.
96:10836–10841. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Mrudula T, Suryanarayana P, Srinivas PNBS
and Reddy GB: Effect of curcumin on hyperglycemia-induced vascular
endothelial growth factor expression in streptozotocin-induced
diabetic rat retina. Biochem Biophys Res Commun. 361:528–532. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Li J, Wang P, Ying J, Chen Z and Yu S:
Curcumin attenuates retinal vascular leakage by inhibiting
calcium/calmodulin-dependent protein kinase II activity in
streptozotocin-induced diabetes. Cell Physiol Biochem.
39:1196–1208. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Pradhan D, Dasmohapatra T and Tripathy G:
Pharmacognostic evaluation of curcumin on diabetic retinopathy in
alloxan-induced diabetes through NF-KB and Brn3a related mechanism.
Pharmacogn J. 10:324–332. 2018. View Article : Google Scholar
|
|
73
|
Khimmaktong W, Petpiboolthai H, Sriya P
and Anupunpisit V: Effects of curcumin on restoration and
improvement of microvasculature characteristic in diabetic rat's
choroid of eye. J Med Assoc Thai. 97(Suppl 2): S39–S46.
2014.PubMed/NCBI
|
|
74
|
Lee TK, Park JY, Yu JS, Jang TS, Oh ST,
Pang C, Ko YJ, Kang KS and Kim KH: 7α,15-Dihydroxydehydroabietic
acid from Pinus koraiensis inhibits the promotion of angiogenesis
through down-regulation of VEGF, p-Akt and p-ERK in HUVECs. Bioorg
Med Chem Lett. 28:1084–1089. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Farajipour H, Rahimian S and Taghizadeh M:
Curcumin: A new candidate for retinal disease therapy? J Cell
Biochem. 2018.Epub ahead of print. PubMed/NCBI
|
|
76
|
Ran Z, Zhang Y, Wen X and Ma J: Curcumin
inhibits high glucose induced inflammatory injury in human retinal
pigment epithelial cells through the ROS PI3K/AKT/mTOR signaling
pathway. Mol Med Rep. 19:1024–1031. 2019.
|
|
77
|
Okamoto T, Yamagishi SI, Inagaki Y, Amano
S, Koga K, Abe R, Takeuchi M, Ohno S, Yoshimura A and Makita Z:
Angiogenesis induced by advanced glycation end products and its
prevention by cerivastatin. FASEB J. 16:1928–1930. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Salvucci O, Basik M, Yao L, Bianchi R and
Tosato G: Evidence for the involvement of SDF-1 and CXCR4 in the
disruption of endothelial cell-branching morphogenesis and
angiogenesis by TNF-alpha and IFN-gamma. J Leukoc Biol. 76:217–226.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Butler JM, Guthrie SM, Koc M, Afzal A,
Caballero S, Brooks HL, Mames RN, Segal MS, Grant MB and Scott EW:
SDF-1 is both necessary and sufficient to promote proliferative
retinopathy. J Clin Invest. 115:86–93. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Arbiser JL, Klauber N, Rohan R, van
Leeuwen R, Huang MT, Fisher C, Flynn E and Byers HR: Curcumin is an
in vivo inhibitor of angiogenesis. Mol Med. 4:376–383. 1998.
View Article : Google Scholar
|
|
81
|
Sameermahmood Z, Balasubramanyam M,
Saravanan T and Rema M: Curcumin modulates SDF-1alpha/CXCR4-induced
migration of human retinal endothelial cells (HRECs). Invest
Ophthalmol Vis Sci. 49:3305–3311. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Salven P, Hattori K, Heissig B and Rafii
S: Interleukin-1alpha promotes angiogenesis in vivo via VEGFR-2
pathway by inducing inflammatory cell VEGF synthesis and secretion.
FASEB J. 16:1471–1473. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Mohammad G and Kowluru RA: Novel role of
mitochondrial matrix metalloproteinase-2 in the development of
diabetic retinopathy. Invest Ophthalmol Vis Sci. 52:3832–3841.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Mohammad G and Kowluru RA: Matrix
metalloproteinase-2 in the development of diabetic retinopathy and
mitochondrial dysfunction. Lab Invest. 90:1365–1372. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Fu Y, Wang Y, Gao X, Li H and Yuan Y:
Dynamic expression of HDAC3 in db/db mouse RGCs and its
relationship with apoptosis and autophagy. J Diabetes Res.
2020:60867802020. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Zhang X, He N, Xing Y and Lu Y: Knockdown
of GCN2 inhibits high glucose-induced oxidative stress and
apoptosis in retinal pigment epithelial cells. Clin Exp Pharmacol
Physiol. 47:591–598. 2020. View Article : Google Scholar
|
|
87
|
Mathew R and White E: Why sick cells
produce tumors: The protective role of autophagy. Autophagy.
3:502–505. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Hara T, Nakamura K, Matsui M, Yamamoto A,
Nakahara Y, Suzuki-Migishima R, Yokoyama M, Mishima K, Saito I,
Okano H and Mizushima N: Suppression of basal autophagy in neural
cells causes neurodegenerative disease in mice. Nature.
441:885–889. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Pahari S, Negi S, Aqdas M, Arnett E,
Schlesinger LS and Agrewala JN: Induction of autophagy through
CLEC4E in combination with TLR4: An innovative strategy to restrict
the survival of mycobacterium tuberculosis. Autophagy.
16:1021–1043. 2020. View Article : Google Scholar :
|
|
90
|
Fernández ÁF, Sebti S, Wei Y, Zou Z, Shi
M, McMillan KL, He C, Ting T, Liu Y, Chiang WC, et al: Disruption
of the beclin 1-BCL2 autophagy regulatory complex promotes
longevity in mice. Nature. 558:136–140. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Luo Y, Dong X, Lu S, Gao Y, Sun G and Sun
X: Gypenoside XVII alleviates early diabetic retinopathy by
regulating Müller cell apoptosis and autophagy in db/db mice. Eur J
Pharmacol. 895:1738932021. View Article : Google Scholar
|
|
92
|
de Faria JML, Duarte DA, Montemurro C,
Papadimitriou A, Consonni SR and de Faria JBL: Defective autophagy
in diabetic retinopathy. Invest Ophthalmol Vis Sci. 57:4356–4366.
2016. View Article : Google Scholar
|
|
93
|
Pereira C: Crosstalk between endoplasmic
reticulum stress and protein misfolding in neurodegenerative
diseases. ISRN Cell Biol. 2013:2013. View Article : Google Scholar
|
|
94
|
Pittalà V, Fidilio A, Lazzara F, Platania
CBM, Salerno L, Foresti R, Drago F and Bucolo C: Effects of novel
nitric oxide-releasing molecules against oxidative stress on
retinal pigmented epithelial cells. Oxid Med Cell Longev.
2017:14208922017. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Bucolo C, Drago F, Maisto R, Romano GL,
D'Agata V, Maugeri G and Giunta S: Curcumin prevents high glucose
damage in retinal pigment epithelial cells through ERK1/2-mediated
activation of the Nrf2/HO-1 pathway. J Cell Physiol.
234:17295–17304. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Chen W, Zou P, Zhao Z, Weng Q, Chen X,
Ying S, Ye Q, Wang Z, Ji J and Liang G: Selective killing of
gastric cancer cells by a small molecule via targeting TrxR1 and
ROS-mediated ER stress activation. Oncotarget. 7:16593–16609. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Ye M, Qiu H, Cao Y, Zhang M, Mi Y, Yu J
and Wang C: Curcumin improves palmitate-induced insulin resistance
in human umbilical vein endothelial cells by maintaining
proteostasis in endoplasmic reticulum. Front Pharmacol. 8:1482017.
View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Zhang P, Fang J, Zhang J, Ding S and Gan
D: Curcumin inhibited podocyte cell apoptosis and accelerated cell
autophagy in diabetic nephropathy via regulating
beclin1/UVRAG/Bcl2. Diabetes Metab Syndr Obes. 13:641–652. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Yao Q, Ke ZQ, Guo S, Yang XS, Zhang FX,
Liu XF, Chen X, Chen HG, Ke HY and Liu C: Curcumin protects against
diabetic cardiomyopathy by promoting autophagy and alleviating
apoptosis. J Mol Cell Cardiol. 124:26–34. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Gürler B, Vural H, Yilmaz N, Oguz H,
Satici A and Aksoy N: The role of oxidative stress in diabetic
retinopathy. Eye (Lond). 5:730–735. 2000. View Article : Google Scholar
|
|
101
|
Chew EY, Klein ML, Ferris FL III, Remaley
NA, Murphy RP, Chantry K, Hoogwerf BJ and Miller D: Association of
elevated serum lipid levels with retinal hard exudate in diabetic
retinopathy. Early treatment diabetic retinopathy study (ETDRS)
report 22. Arch Ophthalmol. 114:1079–1084. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Kumar B, Kowluru A and Kowluru RA:
Lipotoxicity augments glucotoxicity-induced mitochondrial damage in
the development of diabetic retinopathy. Invest Ophthalmol Vis Sci.
56:2985–2995. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Kowluru RA, Mishra M, Kowluru A and Kumar
B: Hyperlipidemia and the development of diabetic retinopathy:
Comparison between type 1 and type 2 animal models. Metabolism.
65:1570–1581. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
de Melo ISV, Dos Santos AF and Bueno NB:
Curcumin or combined curcuminoids are effective in lowering the
fasting blood glucose concentrations of individuals with
dysglycemia: Systematic review and meta-analysis of randomized
controlled trials. Pharmacol Res. 128:137–144. 2018. View Article : Google Scholar
|
|
105
|
Seo KI, Choi MS, Jung UJ, Kim HJ, Yeo J,
Jeon SM and Lee MK: Effect of curcumin supplementation on blood
glucose, plasma insulin, and glucose homeostasis related enzyme
activities in diabetic db/db mice. Mol Nutr Food Res. 52:995–1004.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Das KK, Razzaghi-Asl N, Tikare SN, Di
Santo R, Costi R, Messore A, Pescatori L, Crucitti GC, Jargar JG,
Dhundasi SA and Saso L: Hypoglycemic activity of curcumin synthetic
analogues in alloxan-induced diabetic rats. J Enzyme Inhib Med
Chem. 31:99–105. 2016. View Article : Google Scholar
|
|
107
|
Kaur G, Invally M and Chintamaneni M:
Influence of piperine and quercetin on antidiabetic potential of
curcumin. J Complement Integr Med. 13:247–255. 2016.PubMed/NCBI
|
|
108
|
Song Z, Wang H, Zhu L, Han M, Gao Y, Du Y
and Wen Y: Curcumin improves high glucose-induced INS-1 cell
insulin resistance via activation of insulin signaling. Food Funct.
6:461–469. 2015. View Article : Google Scholar
|
|
109
|
Pivari F, Mingione A, Brasacchio C and
Soldati L: Curcumin and type 2 diabetes mellitus: Prevention and
treatment. Nutrients. 11:18372019. View Article : Google Scholar :
|
|
110
|
Kato M, Nishikawa S, Ikehata A, Dochi K,
Tani T, Takahashi T, Imaizumi A and Tsuda T: Curcumin improves
glucose tolerance via stimulation of glucagon-like peptide-1
secretion. Mol Nutr Food Res. 61:2017. View Article : Google Scholar
|
|
111
|
Yang YS, Su YF, Yang HW, Lee YH, Chou JI
and Ueng KC: Lipid-lowering effects of curcumin in patients with
metabolic syndrome: A randomized, double-blind, placebo-controlled
trial. Phytother Res. 28:1770–1777. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Peschel D, Koerting R and Nass N: Curcumin
induces changes in expression of genes involved in cholesterol
homeostasis. J Nutr Biochem. 18:113–119. 2007. View Article : Google Scholar
|
|
113
|
Dou X, Fan C, Wo L, Yan J, Qian Y and Wo
X: Curcumin up-regulates LDL receptor expression via the sterol
regulatory element pathway in HepG2 cells. Planta Med.
74:1374–1379. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Fan C, Qian Y, Wo X, Yan J and Gao L:
Effect of curcumin on the gene expression of low density
lipoprotein receptors. Chin J Integr Med. 11:201–204. 2005.In
Chinese. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Soni KB and Kuttan R: Effect of oral
curcumin administration on serum peroxides and cholesterol levels
in human volunteers. Indian J Physiol Pharmacol. 36:273–275.
1992.PubMed/NCBI
|
|
116
|
Um MY, Hwang KH, Choi WH, Ahn J, Jung CH
and Ha TY: Curcumin attenuates adhesion molecules and matrix
metalloproteinase expression in hypercholesterolemic rabbits. Nutr
Res. 34:886–893. 2014. View Article : Google Scholar : PubMed/NCBI
|