Stroke was the leading cause of disabilities and
cognitive deficits, and the fifth leading cause of mortality in the
USA in 2017 (1). Moreover,
ischemic stroke accounted for 5.2% of all deaths worldwide in 2015
(2). The basic pathological
cause of ischemic stroke is intravascular thrombosis, which can
result in cerebral tissue necrosis and focal neuronal deficits.
There are three known leading causes of ischemic strokes: 50% are
caused by arteriosclerotic plaques of the cerebral vessels and the
rupture of the arteriosclerotic plaque, 20% are caused by
cardiogenic cerebral infarction, and 25% are caused by Lacunar
infarcts from small vessel lesions (3). Furthermore, the remaining 5% are
due to other exceptional cause such as vasculitis and extracranial
arterial dissection (4).
Acute ischemic stroke (AIS) is a type of ischemic
stroke that can cause severe brain and neuronal damage in a very
short time after the ischemic episode (5). Various degrees and types of brain
damage are caused by ischemic stroke and cerebral infarcts,
including cerebral tissue lesions and structural damage, and
neuronal death and deficits, amongst others. Clinical symptoms of
these types of damage can be observed in patients with conditions
such as Alzheimer's disease (6-11), motor functional deficits
(12), impaired intelligence
quotient score (13) and
multiple cognitive functional deficits (selective attention,
working memory, information processing, abstract reasoning and
verbal comprehension), amongst others (14-19). According to the findings of
numerous studies examining the mechanisms and clinical management
of ischemic stroke and cerebral infarction, there are three major
mechanisms underlying the neuronal injuries caused by ischemic
stroke and cerebral infarcts. Firstly, the loss of neurons induced
by ischemia and infarcts is one of the most direct cause of
neuronal injuries (20). With
regards to this mechanism, researchers have been focusing on the
processes of neuroprotection and regeneration, as well as related
biomarkers and molecular pathways (20). Secondly, vascular obstruction
caused by ischemia excessively produces reactive oxygen species
(ROS), and it has been shown that oxidative stress exacerbates
neuronal damage and leads to severe functional deficits (21). Pathways reacting to and relieving
oxidative stress are widely investigated to help decrease neuronal
injuries. Inflammation induced by ischemia is an additional factor
that leads to further neuronal damage after strokes (22). Therefore, effectively
manipulating the immune responses may help to reduce neuronal
injuries.
The ultimate therapeutic goal for ischemic stroke
and brain infarcts is to reduce neuronal injuries by relieving
arterial occlusion (recanalization) and recovering cerebral blood
flow (reperfusion) (28). The
basic hypothesis of the pathophysiological response during AIS
treatment is that once the cerebral artery has been occluded,
hypo-perfused brain tissues are at risk of permanent infarction,
but such tissues can be effectively rescued via the rapid recovery
of the blood flow (29). These
tissues are known as ischemic penumbras, and preventing the
conversion of ischemic penumbra to inversible infarction is the aim
of AIS treatment (28). Primary
stroke treatment challenges are partly a result of distinguishing
the penumbra from the core zone and the penumbra from benign
hypoperfusion tissues, which have poor perfusion but without the
risk of infarction (30).
Investigations into ischemic stroke and neuronal
injuries have indicated that neuronal damage is caused by neuron
loss, oxidative stress and immune responses (31-33). Various biomarkers and molecular
pathways are involved in rescuing neuronal damage caused by
ischemic stroke and cerebral infarction.
The survival of neurons influences the stability and
completeness of brain functions, and neuron loss directly results
in cerebral functional deficits (34). Hence, neuronal protection and
regeneration has been the major focus for effectively rescuing
cerebral functional deficits. There are various methods to achieve
this goal, which include enhancing neuron protection, promoting
neuron repair and neuron regeneration, and direct mediation of
neuronal survival or death, amongst others. For instance,
astrocytes contribute to angiogenesis, neurogenesis, synaptogenesis
and axonal remodeling (35).
Thus, promoting neurological recovery during the late recovery
phase after stroke could provide benefits for neuroprotection.
Astrocytes limit lesion extension by exerting anti-excitotoxicity
effects and releasing neurotrophins (36). Therefore, the pivotal involvement
of astrocyte responses to an ischemic lesion designates them as
excellent therapeutic targets to improve the functional outcome
following stroke. In addition, the blockade of the GSK-3β-induced
degradation of β-catenin, which in turn promotes neuronal survival,
represents a key step in the ability of Wnt1 to safeguard midbrain
dopaminergic neurons (37).
Within the central nervous system, Wnt signaling cascades
orchestrate all aspects of neuronal functions, including
differentiation, neuron death or survival, axonal extension,
synapse formation and plasticity, neurotrophin transcription,
neurogenesis and regeneration (38-41).
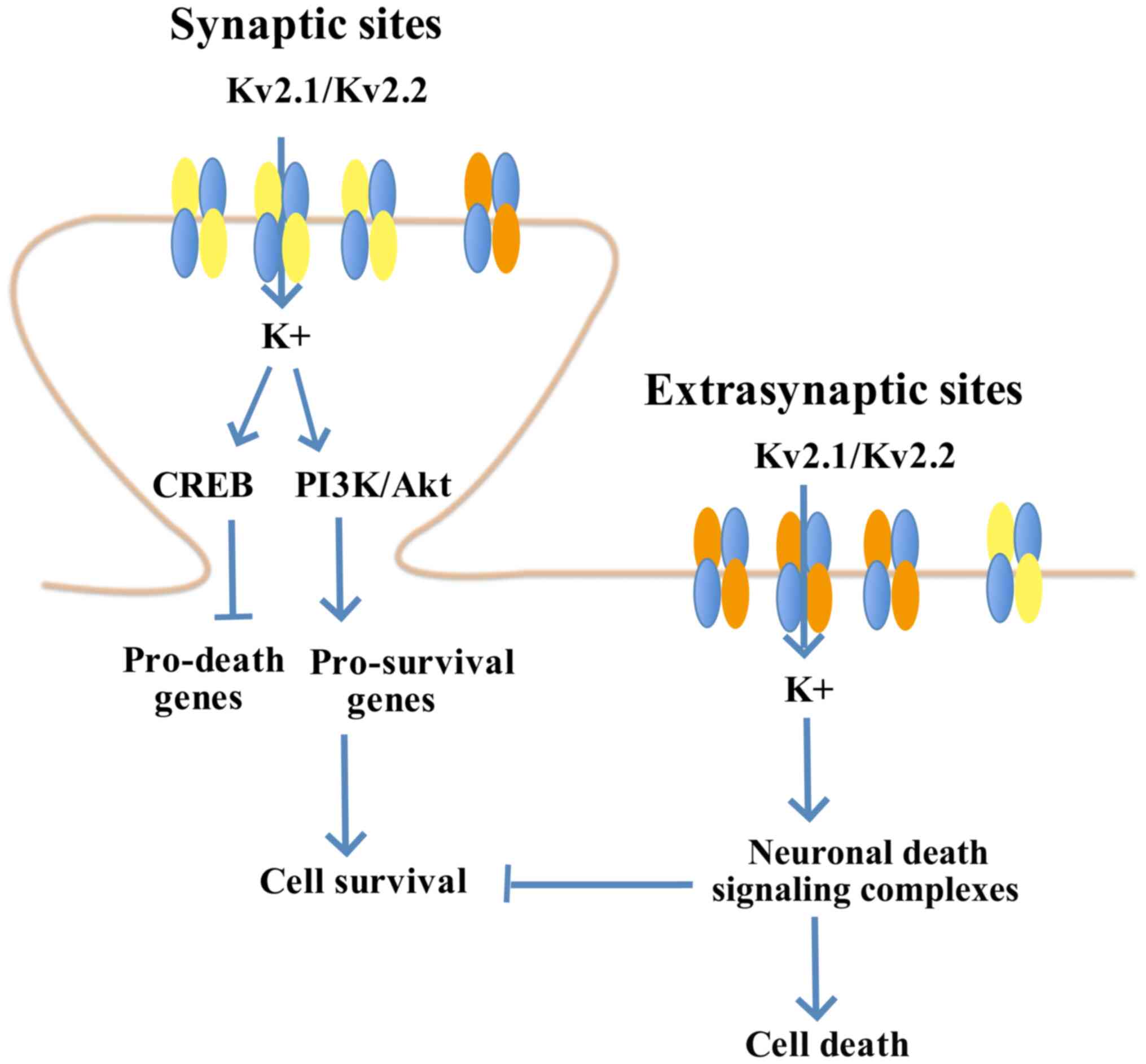
Kv2.1 is involved in the neuron apoptosis pathway.
Neurons characterized with low functional expression of Kv2.1 are
observed to have high resistance against apoptotic stimuli
(42). However, overexpression
of the C terminal in its homologous Kv2.2 pathway interferes with
the Kv2.1 cluster, without affecting other active channels. Such
interference leads to neuron protection by blocking the increased
current intensity of the K+ pathway (43,44). In a previous study, it was
identified that a seven-amino acid declustering domain, SIDSFTS,
induces the dispersion of the Kv2.1 cluster to protect neurons in a
murine ischemia-reperfusion model (45). Furthermore, the
membrane-permeable derivative, TAT-DP-2, induces Kv2.1 surface
cluster dispersal, prevents post-injurious pro-apoptotic potassium
current intensity enhancement, reduces infarct size and improves
long-term neurological function following stroke (45). The therapeutic peptide derived
from TAT-DP-2 is permeable to the blood brain barrier (BBB),
providing effective neuron protection in murine models after
ischemic stroke in vivo (45). Thus, destruction of the Kv2.1
cluster provides neuronal protection (Fig. 1) (45).
It has been shown that WRAP53 expression induces DNA
double strand repair in neurons to promote functional recovery
after ischemic stroke (46).
Moreover, oxygen/glucose deprivation induces excessive production
of ROS in murine stroke models, and ROS break DNA double strands in
neurons (47). Furthermore,
WRAP53 activation promotes DNA repair after its translocation into
the nucleus. Knockdown of WRAP53 exacerbates DNA double strand
damage, which results in lower resistance to apoptotic stimuli in
neurons. By contrast, overexpression of WRAP53 activates DNA double
strand repair, and consequently promotes neuron protection and
survival (46). Clinical trials
have demonstrated that high WRAP53, a telomere-related gene, may be
beneficial for healthspan in humans, reversing certain deleterious
metabolic consequences of prediabetes (48).
NPCs facilitate the survival, proliferation and
regeneration of neurons in stroke areas and infarct zones in animal
models (9-11). Some clinical trials have reported
positive results for the use of NPCs in patients (49). Moreover, transplantation of
external NPCs is another potential clinical treatment for strokes
(6-8). Neurotrophic factors are used to
amplify neuron regeneration in adult mammalian brains via embedded
neurogenesis, but this only contributes to <1% of the neuron
loss caused by ischemic strokes (50-54).
Having been transplanted into damaged cortical
zones, neural stem cells (NSCs) from the cerebral pituitary chamber
are responsible for producing astrocytes rather than neurons
(55,56). Furthermore, transplanted external
NSCs are associated with various challenges, such as immunological
rejection, tumor progression and poor long-term survival (12,49,57-59). In addition, astrocytes can be
converted to neurons after ischemic stroke in vitro and
in vivo (13-17,19,60-62). For instance, Chen et al
(20) reported a 74.3%
astrocyte-neuron conversion rate in murine models after stroke.
However, the clinical effects of this conversion in patients has
not been investigated.
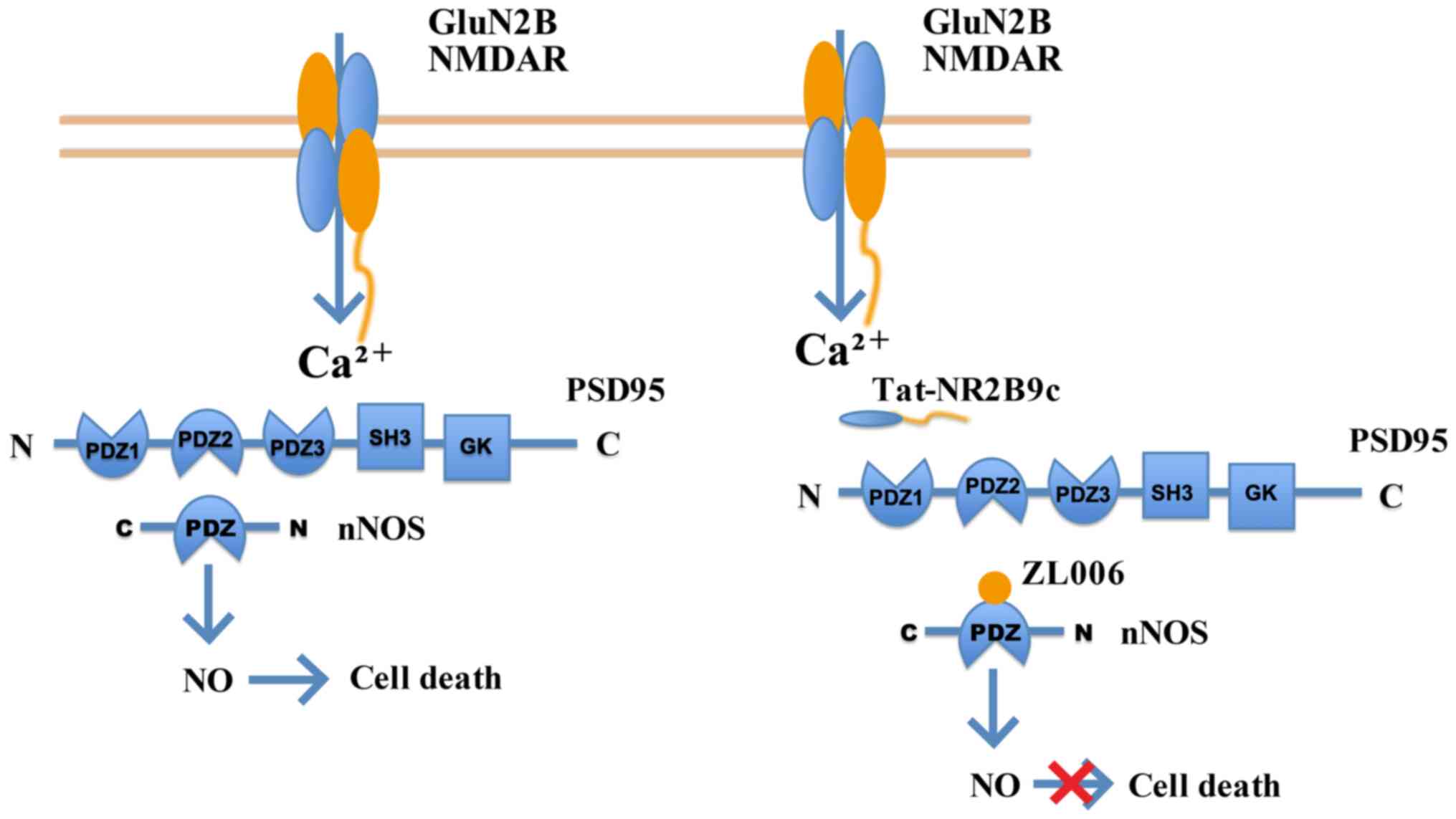
NMDARs are a crucial regulatory factor of neuron
injuries and ischemic stroke. NMDARs serve a double-edged role in
the regulation of neuronal survival or death (63-65). Firstly, different subtypes of
NMDARs regulate neuronal survival and death (66-68). It has shown that NMDAR
antagonists, containing NMDA receptor 2B (GluN2B), relieve the
toxicity caused by NMDA in temporary MCAO (tMCAO) models in
vitro and in vivo. However, NMDAR antagonists containing
GluN2A aggravate neuronal death rather than relieving its effects
(66,68-74). Secondly, the functions of NMDARs
vary with their locations. Indeed, NMDARs inside and outside the
synapse exert opposite functions (63,75,76). NMDAR downstream mechanisms and
pathways are complex (77-81). NMDARs inside and outside of
synapses evoke ERK1/2 kinases, but only the NMDARs inside the
synapse increase the level of ERK phosphorylation to provide
protection for neurons under toxic conditions (80,82). Notably, stimulation of the NMDAR
outside the synapse inactivates ERK1/2 (82). Thirdly, NMDARs serve various
roles in signaling pathways that modulate neuronal survival and
death (64,65). A low concentration of NMDA
activates NSCs to exert a neuroprotective response. Furthermore,
the PI3K/Akt kinase and MAPK pathways are downstream of NMDARs
involved in neuron survival (Fig.
2) (63,83). MAPK signaling pathway members,
including p44/42 MAPK (ERK1/2), JNK and p38 MAPK, regulate cell
proliferation and differentiation, and the responses to cytokines
and stress during protein kinase cascades. However, NMDARs induce
neural toxicity by activating NSCs, in the form of the
GluN2B-postsynaptic density protein 95-neuronal nitric oxides
synthase complex (84,85), GluN2B-death associated protein
kinase 1-p53 complex (86,87) or GluN1-PTEN complex (88) (Fig. 3).
Heme oxygenase 1 (HO-1) is highly expressed in brain
tissues after cerebral injuries, including stroke and infarction,
and a high expression level of HO-1 symbolizes the activation of
the protective mechanism against oxidative stress (89). Brain injuries are associated with
oxidative stress. It has been revealed that Persian blue (PB)
nanoparticles effectively eliminate excessive ROS produced by
ischemic stroke and cerebral infarcts. PB exerts a similar function
to catalase, superoxide dismutase and peroxidase (90,91). Moreover, hollow Prussian blue
nanozymes (HPBZs) react and neutralize inflammation caused by
immune responses, as well as suppressing neuron apoptosis in
vitro and in vivo. Thus, HPBZs increase the tolerance to
strokes and minimize neural injuries (92).
Stroke interrupts the blood flow into the brain. The
pathophysiology of stroke involves a progressive systematic
response after brain damage (93). Animal stroke models (94) and clinical patients (95) show dynamic BBB rupture. The BBB
fracture induced by stroke initiates a series of pathological
responses. The hyperinflammatory responses caused by strokes
include increased levels of inflammatory cells, cytokines and
chemokines in the circulating blood (96). Recently, it has been shown that
infarct sizes are effectively decreased and that a promising
recovery of neural injuries occurs at 6.5-7 h after the stroke in
an animal model of tMCAO (22).
The intervention used in this model was blood substitution therapy
to replace the blood of mice suffering from strokes with the whole
blood from healthy infant mice (22). The possible underlying mechanisms
in this therapy may be as follows: Firstly, the brain antigens
released after the rupture of the BBB may activate the immune
system after stroke. Therefore, replacing the blood in mice with
strokes may reduce the amount of brain antigens in the circulating
blood to alleviate the immune responses after stroke. Secondly,
replacing the blood in mice with strokes effectively reduces the
number of activated leukocytes. Thus, large amounts of harmful
signals in circulating blood after stroke, including cytokines,
chemokines and proteases, are decreased. Finally, new replacement
blood may provide oxygen and various other neuroprotective
factors.
The molecular mechanism of neuronal damage caused by
ischemic stroke and cerebral infarction is complex. In addition to
the molecular processes previously mentioned, multiple other
factors also provide new insights into the treatment of stroke.
Recently, PMVs have been found to significantly improve the
recovery of neurological function in mice with cerebral infarction
and promote angiogenesis at the infarction edge (97). The procoagulant and
proinflammatory phenotype of circulating PMVs may contribute to
acetylsalicylic acid treatment failure in patients with
convalescent stroke (98).
Accumulating evidence has shown that exosomal miRNAs
are one of the most important factors involved in the pathogenesis
of stroke. Exosomal miRNAs are used as non-invasive biomarkers in
stroke diagnosis and for monitoring the response during therapy
(99). Antagomirs (anti-miRNAs)
are an effective treatment method to enhance neuronal survival in
various animal models, for example, administration of an antisense
oligonucleotide inhibitor of miR-129-5p to an amyotrophic lateral
sclerosis animal model, SOD1 (G93A) mice, resulted in a significant
increase in survival and improved the neuromuscular phenotype in
treated mice (100); and some
miRNAs show therapeutic effects in stroke (101). These miRNAs affect the pathways
induced by stroke, including leukocyte extravasation signaling,
NF-κB signaling, Toll-like receptor signaling and the prothrombin
activation pathway (102). For
instance, miR-122, miR-9, miR-298 and miR-155-5p participate in
brain injury after stroke by targeting different genes involved in
the NF-κB signaling pathway (103-106). Thus, miRNAs are crucial in
stroke progression, diagnosis, therapy and prognosis.
At present, thrombolytic therapy is the most widely
applied treatment for ischemic stroke and brain infarction
(107). The basic principle of
thrombolysis is to recanalize and reperfuse cerebral arteries using
thrombolytic drugs and mechanical thrombectomy devices, eventually
leading to the partial recovery of brain tissues and neural
functions (108). The clinical
effectiveness of intravenous thrombolytic therapy has been
established for patients within 4.5 h of stroke onset. However,
numerous patients experience complicated situations, such as
proximal artery occlusion, >4.5 h of stroke onset and
contraindication of systemic thrombolysis due to recent major
surgeries or active hemorrhage. Such patients are not suitable for
intravenous thrombolysis therapy (109). Therefore, a recent review
indicated that several studies and clinical trials have focused on
catheter or artery-based treatments that directly remove occlusions
in blood vessels and recover the blood flow (28).
Clinical trials funded by the United States Natural
Institute of Neurological Diseases and Stroke and the European
Acute Stroke Study have shown that intra-venous thrombolysis has
strong effects in patients with mild symptoms or no disability, and
that intravenous thrombolysis has more benefits than limitations in
patients with a full range of disabilities (110,111). For instance, treatment with
tissue plasminogen activator in the 3- to 4.5-h window confers
benefit on approximately half as many patients as treatment for
<3 h, with no increase in the conferral of harm; ~1 in 6
patients has a better outcome and 1 in 35 has a worse outcome as a
result of therapy. Previous studies (112-114) have established intravenous
thrombolysis as the standard therapy for patients with AIS within 3
h of stroke onset. Intravenous thrombolysis is beneficial for all
levels and subtypes of strokes (115), and 35-40% of patients displayed
a good therapeutic outcome. However, only 10-15% of internal
carotid artery occlusions and 25-50% of proximal MCAO were
alleviated by intravenous thrombolysis therapy alone. These data
indicated that the proximal artery occlusion (internal carotid
artery and MCAO) may be resistant to intravenous thrombolysis
therapy alone (116,117). Proximal artery occlusion leads
to one-third of AIS cases with severe stroke symptoms and has the
negative outcome of ineffective reperfusion (118). Thus, several large-scale
clinical trials have been focusing on identifying other
substitutional or adjunctive therapies based on intravenous
thrombolysis to improve recanalization and the reperfusion
rate.
Arterial thrombolysis consists of chemical
thrombolysis and mechanical thrombectomy, and the use of
intravenous therapy prior to mechanical thrombectomy has been
recently questioned (118). The
clinical efficacy and safety of arterial thrombolysis with the
selective thrombolytic recombinant-pro-urokinse (r-proUK) has been
investigated in two randomized acute stroke treatment trials,
namely PROACT I and PROACT II (119). It has been shown that patients
treated with such therapy experience the risk of cerebral
hemorrhage. Moreover, the outcome of combining arterial
thrombolysis with other agents as therapy remains unclear.
Therefore, the Food and Drug Administration (FDA) did not grant the
clinical application of arterial r-proUK. Nevertheless, a recent
study reported that r-proUK promoted thrombolysis and
recanalization, with a decreased risk of cerebral hemorrhage, and
thus, this treatment exerted protective effects on cerebral
ischemia in rabbits (120).
Different from recently developed chemical
thrombolysis, mechanical thrombectomy has been widely applied in
the clinic (121). The FDA
granted permission of several mechanical thrombectomy devices based
on positive results yielded by numerous large-scale clinical trials
(122). These devices can
effectively recanalize proximal artery occlusion with an acceptable
rate of complications (123,124). Indeed, any type of
intracerebral hemorrhage was observed less frequently in the
mechanical thrombectomy alone group compared with that in the group
using the combination of intravenous thrombolysis with mechanical
thrombectomy (125). However,
the mechanical thrombectomy alone group failed to show a favorable
functional outcome among patients with acute large vessel occlusion
stroke compared with the combined group. Furthermore, a recent
finding supported the hypothesis that intravenous therapy before
mechanical thrombectomy does not influence the prognosis of
patients with stroke (126).
Trials of novel recanalization methods based on MRI
tool selection of patients are ongoing. Unless a specific lesion
site is taken into account, functional deficits due to medium-sized
infarcts are difficult to predict (127). Accurate information regarding
the location of the lesion and the progression of the disease is
crucial for clinic therapy. Therefore, promising neuroprotective
compounds in the pre-clinical phase can be subsequently dismissed
for ineffectiveness in large-scale clinical trials due to
inaccurate information. Infarction of the internal capsule (IC) may
be associated with motor impairment and poor prognosis in patients
with stroke (128).
Pre-clinical MRI information regarding volume size and the precise
location of the lesion into the IC is required for subsequent
therapy. Moreover, the state of neurological damage according to
MRI, as well as the destruction of axonal structures and
pathological changes according to immunostaining, provide
information for the precise injection site of neuroprotective drugs
(129). Thus, combined MRI and
histological methods provide a powerful method of assessing
neuronal damage during cerebral ischemia therapy (129).
Ischemic stroke leads to severe outcomes, including
cerebral infarcts, permanent brain damage and neural functional
deficits. Therefore, decreasing and preventing neural injuries
caused by stroke and infarctions has been the focus of mechanistic
and therapeutic studies. The current review summarized the
pathophysiology, molecular mechanisms, animal models, and clinical
management and therapies in ischemic strokes. The related molecular
mechanisms in clinical trials should be further investigated. The
American Heart Association has suggested that arterial thrombolysis
is an acceptable alternative therapy for strokes. Multiple stroke
centers provide arterial thrombolysis for patients experiencing a
major acute stroke attack within 6 h. However, the molecular
mechanism underlying arterial thrombolysis remains to be fully
investigated.
Not applicable.
YZ and XZ wrote the manuscript. YZ, XZ, YW and XC
searched the relevant literature. XC and YW critically reviewed the
manuscript. All authors have read and approved the final version of
the manuscript. Data authentication is not applicable.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
Not applicable.
No funding was received.
|
1
|
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman
M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C,
et al: Heart disease and stroke statistics-2017 update: A report
from the American Heart Association. Circulation. 135:e146–e603.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
GBD 2015 Mortality and Causes of Death
Collaborators: Global, regional, and national life expectancy,
all-cause mortality, and cause-specific mortality for 249 causes of
death, 1980-2015: A systematic analysis for the Global Burden of
Disease Study 2015. Lancet. 388:1459–1544. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bailey EL, Smith C, Sudlow CL and Wardlaw
JM: Pathology of lacunar ischemic stroke in humans-a systematic
review. Brain Pathol. 22:583–591. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Warlow C, Sudlow C, Dennis M, Wardlaw J
and Sandercock P: Stroke. Lancet. 362:1211–1224. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Balch MHH, Nimjee SM, Rink C and Hannawi
Y: Beyond the brain: The systemic pathophysiological response to
acute ischemic stroke. J Stroke. 22:159–172. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Boyle PA, Yang J, Yu L, Leurgans SE,
Capuano AW, Schneider JA, Wilson RS and Bennett DA: Varied effects
of age-related neuropathologies on the trajectory of late life
cognitive decline. Brain. 140:804–812. 2017.PubMed/NCBI
|
|
7
|
Boyle PA, Yu L, Wilson RS, Schneider JA
and Bennett DA: Relation of neuropathology with cognitive decline
among older persons without dementia. Front Aging Neurosci.
5:502013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Corrada MM, Sonnen JA, Kim RC and Kawas
CH: Microinfarcts are common and strongly related to dementia in
the oldest-old: The 90+ study. Alzheimers Dement. 12:900–908. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ince PG, Minett T, Forster G, Brayne C and
Wharton SB: Medical Research Council Cognitive Function and Ageing
Neuropathology Study: Microinfarcts in an older
population-representative brain donor cohort (MRC CFAS):
Prevalence, relation to dementia and mobility, and implications for
the evaluation of cerebral Small Vessel Disease. Neuropathol Appl
Neurobiol. 43:409–418. 2017. View Article : Google Scholar
|
|
10
|
Kawas CH, Kim RC, Sonnen JA, Bullain SS,
Trieu T and Corrada MM: Multiple pathologies are common and related
to dementia in the oldest-old: The 90+ study. Neurology.
85:535–542. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
White LR, Edland SD, Hemmy LS, Montine KS,
Zarow C, Sonnen JA, Uyehara-Lock JH, Gelber RP, Ross GW, Petrovitch
H, et al: Neuropathologic comorbidity and cognitive impairment in
the Nun and Honolulu-Asia aging studies. Neurology. 86:1000–1008.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Buchman AS, Yu L, Boyle PA, Levine SR, Nag
S, Schneider JA and Bennett DA: Microvascular brain pathology and
late-life motor impairment. Neurology. 80:712–718. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hogan AM, Kirkham FJ, Prengler M, Telfer
P, Lane R, Vargha-Khadem F and Haan M: An exploratory study of
physiological correlates of neurodevelopmental delay in infants
with sickle cell anaemia. Br J Haematol. 132:99–107. 2006.
View Article : Google Scholar
|
|
14
|
Bernaudin F, Verlhac S, Freard F,
Roudot-Thoraval F, Benkerrou M, Thuret I, Mardini R, Vannier JP,
Ploix E, Romero M, et al: Multicenter prospective study of children
with sickle cell disease: Radiographic and psychometric
correlation. J Child Neurol. 15:333–343. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Brown RT, Davis PC, Lambert R, Hsu L,
Hopkins K and Eckman J: Neurocognitive functioning and magnetic
resonance imaging in children with sickle cell disease. J Pediatr
Psychol. 25:503–513. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
DeBaun MR, Schatz J, Siegel MJ, Koby M,
Craft S, Resar L, Chu JY, Launius G, Dadash-Zadeh M, Lee RB and
Noetzel M: Cognitive screening examinations for silent cerebral
infarcts in sickle cell disease. Neurology. 50:1678–1682. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hogan AM, Pit-ten Cate IM, Vargha-Khadem
F, Prengler M and Kirkham FJ: Physiological correlates of
intellectual function in children with sickle cell disease:
Hypoxaemia, hyperaemia and brain infarction. Dev Sci. 9:379–387.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Steen RG, Miles MA, Helton KJ, Strawn S,
Wang W, Xiong X and Mulhern RK: Cognitive impairment in children
with hemoglobin SS sickle cell disease: Relationship to MR imaging
findings and hematocrit. AJNR Am J Neuroradiol. 24:382–389.
2003.PubMed/NCBI
|
|
19
|
Watkins KE, Hewes DK, Connelly A, Kendall
BE, Kingsley DP, Evans JE, Gadian DG, Vargha-Khadem F and Kirkham
FJ: Cognitive deficits associated with frontal-lobe infarction in
children with sickle cell disease. Dev Med Child Neurol.
40:536–543. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen YC, Ma NX, Pei ZF, Wu Z, Do-Monte FH,
Keefe S, Yellin E, Chen MS, Yin JC, Lee G, et al: A neuroD1
AAV-based gene therapy for functional brain repair after ischemic
injury through in vivo astrocyte-to-neuron conversion. Mol Ther.
28:217–234. 2020. View Article : Google Scholar
|
|
21
|
Hu X, Wu D, He X, Zhao H, He Z, Lin J,
Wang K, Wang W, Pan Z, Lin H and Wang M: circGSK3β promotes
metastasis in esophageal squamous cell carcinoma by augmenting
β-catenin signaling. Mol Cancer. 18:1602019. View Article : Google Scholar
|
|
22
|
Ren X, Hu H, Farooqi I and Simpkins JW:
Blood substitution therapy rescues the brain of mice from ischemic
damage. Nat Commun. 11:40782020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sommer CJ: Ischemic stroke: Experimental
models and reality. Acta Neuropathol. 133:245–261. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang L, Zhang RL, Jiang Q, Ding G, Chopp
M and Zhang ZG: Focal embolic cerebral ischemia in the rat. Nat
Protoc. 10:539–547. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
McBride DW and Zhang JH: Precision stroke
animal models: The permanent MCAO model should be the primary
model, not transient MCAO. Transl Stroke Res. Jul 17–2017.Epub
ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lunardi Baccetto S and Lehmann C:
Microcirculatory changes in experimental models of stroke and
CNS-injury induced immunodepression. Int J Mol Sci. 20:51842019.
View Article : Google Scholar :
|
|
27
|
Fujie W, Kirino T, Tomukai N, Iwasawa T
and Tamura A: Progressive shrinkage of the thalamus following
middle cerebral artery occlusion in rats. Stroke. 21:1485–1488.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Prabhakaran S, Ruff I and Bernstein RA:
Acute stroke intervention: A systematic review. JAMA.
313:1451–1462. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhao Y, Yuan B, Chen J, Feng D, Zhao B,
Qin C and Chen YF: Endothelial progenitor cells: Therapeutic
perspective for ischemic stroke. CNS Neurosci Ther. 19:67–75. 2013.
View Article : Google Scholar
|
|
30
|
Kidwell CS, Alger JR and Saver JL: Beyond
mismatch: Evolving paradigms in imaging the ischemic penumbra with
multimodal magnetic resonance imaging. Stroke. 34:2729–2735. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Khoshnam SE, Winlow W, Farzaneh M, Farbood
Y and Moghaddam HF: Pathogenic mechanisms following ischemic
stroke. Neurol Sci. 38:1167–1186. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Guo JD, Zhao X, Li Y, Li GR and Liu XL:
Damage to dopaminergic neurons by oxidative stress in Parkinson's
disease (Review). Int J Mol Med. 41:1817–1825. 2018.PubMed/NCBI
|
|
33
|
Kierdorf K, Wang Y and Neumann H:
Immune-mediated CNS damage. Results Probl Cell Differ. 51:173–196.
2010. View Article : Google Scholar
|
|
34
|
Lazarov O and Hollands C: Hippocampal
neurogenesis: Learning to remember. Prog Neurobiol. 138-140:1–18.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sun L, Zhang Y, Liu E, Ma Q, Anatol M, Han
H and Yan J: The roles of astrocyte in the brain pathologies
following ischemic stroke. Brain Inj. 33:712–716. 2019. View Article : Google Scholar
|
|
36
|
Liu Z and Chopp M: Astrocytes, therapeutic
targets for neuroprotection and neurorestoration in ischemic
stroke. Prog Neurobiol. 144:103–120. 2016. View Article : Google Scholar :
|
|
37
|
L'Episcopo F, Serapide MF, Tirolo C, Testa
N, Caniglia S, Morale MC, Pluchino S and Marchetti B: A Wnt1
regulated Frizzled-1/β-Catenin signaling pathway as a candidate
regulatory circuit controlling mesencephalic dopaminergic
neuron-astrocyte crosstalk: Therapeutical relevance for neuron
survival and neuroprotection. Mol Neurodegener. 6:492011.
View Article : Google Scholar
|
|
38
|
Salinas PC: Wnt signaling in the
vertebrate central nervous system: From axon guidance to synaptic
function. Cold Spring Harb Perspect Biol. 4:a0080032012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Grainger S and Willert K: Mechanisms of
Wnt signaling and control. Wiley Interdiscip Rev Syst Biol Med. Mar
30–2018, Epub ahead of print. View Article : Google Scholar
|
|
40
|
Kalani MY, Cheshier SH, Cord BJ, Bababeygy
SR, Vogel H, Weissman IL, Palmer TD and Nusse R: Wnt-mediated
self-renewal of neural stem/progenitor cells. Proc Natl Acad Sci
USA. 105:16970–16975. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Clevers H, Loh KM and Nusse R: Stem cell
signaling. An integral program for tissue renewal and regeneration:
Wnt signaling and stem cell control. Science. 346:12480122014.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Pal S, Hartnett KA, Nerbonne JM, Levitan
ES and Aizenman E: Mediation of neuronal apoptosis by Kv2.1-encoded
potassium channels. J Neurosci. 23:4798–4802. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Baver SB and O'Connell KM: The C-terminus
of neuronal Kv2.1 channels is required for channel localization and
targeting but not for NMDA-receptor-mediated regulation of channel
function. Neuroscience. 217:56–66. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Justice JA, Schulien AJ, He K, Hartnett
KA, Aizenman E and Shah NH: Disruption of KV2.1 somato-dendritic
clusters prevents the apoptogenic increase of potassium currents.
Neuroscience. 354:158–167. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Schulien AJ, Yeh CY, Orange BN, Pav OJ,
Hopkins MP, Moutal A, Khanna R, Sun D, Justice JA and Aizenman E:
Targeted disruption of Kv2.1-VAPA association provides
neuroprotection against ischemic stroke in mice by declustering
Kv2.1 channels. Sci Adv. 6:eaaz81102020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Sánchez-Morán I, Rodríguez C, Lapresa R,
Agulla J, Sobrino T, Castillo J, Bolaños JP and Almeida A: Nuclear
WRAP53 promotes neuronal survival and functional recovery after
stroke. Sci Adv. 6:eabc57022020. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Ji HJ, Wang DM, Hu JF, Sun MN, Li G, Li
ZP, Wu DH, Liu G and Chen NH: IMM-H004, a novel courmarin
derivative, protects against oxygen-and
glucose-deprivation/restoration-induced apoptosis in PC12 cells.
Eur J Pharmacol. 723:259–266. 2014. View Article : Google Scholar
|
|
48
|
Canudas S, Hernández-Alonso P, Galié S,
Muralidharan J, Morell-Azanza L, Zalba G, García-Gavilán J, Martí
A, Salas-Salvadó J and Bulló M: Pistachio consumption modulates DNA
oxidation and genes related to telomere maintenance: A crossover
randomized clinical trial. Am J Clin Nutr. 109:1738–1745. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
van Rooden S, Goos JD, van Opstal AM,
Versluis MJ, Webb AG, Blauw GJ, van der Flier WM, Scheltens P,
Barkhof F, van Buchem MA and van der Grond J: Increased number of
microinfarcts in Alzheimer disease at 7-T MR imaging. Radiology.
270:205–211. 2014. View Article : Google Scholar
|
|
50
|
Bernaudin F, Verlhac S, Arnaud C, Kamdem
A, Chevret S, Hau I, Coïc L, Leveillé E, Lemarchand E, Lesprit E,
et al: Impact of early transcranial Doppler screening and intensive
therapy on cerebral vasculopathy outcome in a newborn sickle cell
anemia cohort. Blood. 117:1130–1140. 2011. View Article : Google Scholar
|
|
51
|
Hindmarsh PC, Brozovic M, Brook CG and
Davies SC: Incidence of overt and covert neurological damage in
children with sickle cell disease. Postgrad Med J. 63:751–753.
1987. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kwiatkowski JL, Zimmerman RA, Pollock AN,
Seto W, Smith-Whitley K, Shults J, Blackwood-Chirchir A and
Ohene-Frempong K: Silent infarcts in young children with sickle
cell disease. Br J Haematol. 146:300–305. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Moser FG, Miller ST, Bello JA, Pegelow CH,
Zimmerman RA, Wang WC, Ohene-Frempong K, Schwartz A, Vichinsky EP,
Gallagher D and Kinney TR: The spectrum of brain MR abnormalities
in sickle-cell disease: A report from the cooperative study of
sickle cell disease. AJNR Am J Neuroradiol. 17:965–972.
1996.PubMed/NCBI
|
|
54
|
Westover MB, Bianchi MT, Yang C, Schneider
JA and Greenberg SM: Estimating cerebral microinfarct burden from
autopsy samples. Neurology. 80:1365–1369. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hilal S, Sikking E, Shaik MA, Chan QL, van
Veluw SJ, Vrooman H, Cheng CY, Sabanayagam C, Cheung CY, Wong TY,
et al: Cortical cerebral microinfarcts on 3T MRI: A novel marker of
cerebrovascular disease. Neurology. 87:1583–1590. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
van Veluw SJ, Hilal S, Kuijf HJ, Ikram MK,
Xin X, Yeow TB, Venketasubramanian N, Biessels GJ and Chen C:
Cortical microinfarcts on 3T MRI: Clinical correlates in
memory-clinic patients. Alzheimers Dement. 11:1500–1509. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Anenberg E, Arstikaitis P, Niitsu Y,
Harrison TC, Boyd JD, Hilton BJ, Tetzlaff W and Murphy TH:
Ministrokes in channel-rhodopsin-2 transgenic mice reveal
widespread deficits in motor output despite maintenance of cortical
neuronal excitability. J Neurosci. 34:1094–1104. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Summers PM, Hartmann DA, Hui ES, Nie X,
Deardorff RL, McKinnon ET, Helpern JA, Jensen JH and Shih AY:
Functional deficits induced by cortical microinfarcts. J Cereb
Blood Flow Metab. 37:3599–3614. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Wang M, Iliff JJ, Liao Y, Chen MJ,
Shinseki MS, Venkataraman A, Cheung J, Wang W and Nedergaard M:
Cognitive deficits and delayed neuronal loss in a mouse model of
multiple microinfarcts. J Neurosci. 32:17948–17960. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Armstrong FD, Thompson RJ Jr, Wang W,
Zimmerman R, Pegelow CH, Miller S, Moser F, Bello J, Hurtig A and
Vass K: Cognitive functioning and brain magnetic resonance imaging
in children with sickle cell disease. Neuropsychology committee of
the cooperative study of sickle cell disease. Pediatrics.
97:864–870. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Steen RG, Reddick WE, Mulhern RK, Langston
JW, Ogg RJ, Bieberich AA, Kingsley PB and Wang WC: Quantitative MRI
of the brain in children with sickle cell disease reveals
abnormalities unseen by conventional MRI. J Magn Reson Imaging.
8:535–543. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Wang W, Enos L, Gallagher D, Thompson R,
Guarini L, Vichinsky E, Wright E, Zimmerman R and Armstrong FD:
Cooperative Study of Sickle Cell Disease: Neuropsychologic
performance in school-aged children with sickle cell disease: A
report from the cooperative study of sickle cell disease. J
Pediatr. 139:391–397. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Hardingham GE and Bading H: Synaptic
versus extrasynaptic NMDA receptor signalling: Implications for
neurodegenerative disorders. Nat Rev Neurosci. 11:682–696. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Lai TW, Shyu WC and Wang YT: Stroke
intervention pathways: NMDA receptors and beyond. Trends Mol Med.
17:266–275. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Wu QJ and Tymianski M: Targeting NMDA
receptors in stroke: New hope in neuroprotection. Mol Brain.
11:152018. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Chen M, Lu TJ, Chen XJ, Zhou Y, Chen Q,
Feng XY, Xu L, Duan WH and Xiong ZQ: Differential roles of NMDA
receptor subtypes in ischemic neuronal cell death and ischemic
tolerance. Stroke. 39:3042–3048. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Choo AM, Geddes-Klein DM, Hockenberry A,
Scarsella D, Mesfin MN, Singh P, Patel TP and Meaney DF: NR2A and
NR2B subunits differentially mediate MAP kinase signaling and
mitochondrial morphology following excitotoxic insult. Neurochem
Int. 60:506–516. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Liu Y, Wong TP, Aarts M, Rooyakkers A, Liu
L, Lai TW, Wu DC, Lu J, Tymianski M, Craig AM and Wang YT: NMDA
receptor subunits have differential roles in mediating excitotoxic
neuronal death both in vitro and in vivo. J Neurosci. 27:2846–2857.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
DeRidder MN, Simon MJ, Siman R, Auberson
YP, Raghupathi R and Meaney DF: Traumatic mechanical injury to the
hippocampus in vitro causes regional caspase-3 and calpain
activation that is influenced by NMDA receptor subunit composition.
Neurobiol Dis. 22:165–176. 2006. View Article : Google Scholar
|
|
70
|
Eyo UB, Bispo A, Liu J, Sabu S, Wu R,
DiBona VL, Zheng J, Murugan M, Zhang H, Tang Y and Wu LJ: The
GluN2A subunit regulates neuronal NMDA receptor-induced
microglia-neuron physical interactions. Sci Rep. 8:8282018.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Manzerra P, Behrens MM, Canzoniero LM,
Wang XQ, Heidinger V, Ichinose T, Yu SP and Choi DW: Zinc induces a
Src family kinase-mediated up-regulation of NMDA receptor activity
and excitotoxicity. Proc Natl Acad Sci USA. 98:11055–11061. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Terasaki Y, Sasaki T, Yagita Y, Okazaki S,
Sugiyama Y, Oyama N, Omura-Matsuoka E, Sakoda S and Kitagawa K:
Activation of NR2A receptors induces ischemic tolerance through
CREB signaling. J Cereb Blood Flow Metab. 30:1441–1449. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Zhang X, Zhang Q, Tu J, Zhu Y, Yang F, Liu
B, Brann D and Wang R: Prosurvival NMDA 2A receptor signaling
mediates postconditioning neuroprotection in the hippocampus.
Hippocampus. 25:286–296. 2015. View Article : Google Scholar
|
|
74
|
Zhou M and Baudry M: Developmental changes
in NMDA neurotoxicity reflect developmental changes in subunit
composition of NMDA receptors. J Neurosci. 26:2956–2963. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Hardingham GE, Fukunaga Y and Bading H:
Extrasynaptic NMDARs oppose synaptic NMDARs by triggering CREB
shut-off and cell death pathways. Nat Neurosci. 5:405–414. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Lu W, Man H, Ju W, Trimble WS, MacDonald
JF and Wang YT: Activation of synaptic NMDA receptors induces
membrane insertion of new AMPA receptors and LTP in cultured
hippocampal neurons. Neuron. 29:243–254. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Karpova A, Mikhaylova M, Bera S, Bar J,
Reddy PP, Behnisch T, Rankovic V, Spilker C, Bethge P, Sahin J, et
al: Encoding and transducing the synaptic or extrasynaptic origin
of NMDA receptor signals to the nucleus. Cell. 152:1119–1133. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Kaufman AM, Milnerwood AJ, Sepers MD,
Coquinco A, She K, Wang L, Lee H, Craig AM, Cynader M and Raymond
LA: Opposing roles of synaptic and extrasynaptic NMDA receptor
signaling in cocultured striatal and cortical neurons. J Neurosci.
32:3992–4003. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Lau D, Bengtson CP, Buchthal B and Bading
H: BDNF reduces toxic extrasynaptic NMDA receptor signaling via
synaptic NMDA receptors and nuclear-calcium-induced transcription
of inhba/activin A. Cell Rep. 12:1353–1366. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Wang WY, Jia LJ, Luo Y, Zhang HH, Cai F,
Mao H, Xu WC, Fang JB, Peng ZY, Ma ZW, et al: Location- and
subunit-specific NMDA receptors determine the developmental
sevoflurane neurotoxicity through ERK1/2 signaling. Mol Neurobiol.
53:216–230. 2016. View Article : Google Scholar
|
|
81
|
Wang Y, Briz V, Chishti A, Bi X and Baudry
M: Distinct roles for µ-calpain and m-calpain in synaptic
NMDAR-mediated neuroprotection and extrasynaptic NMDAR-mediated
neurodegeneration. J Neurosci. 33:18880–18892. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Ivanov A, Pellegrino C, Rama S, Dumalska
I, Salyha Y, Ben-Ari Y and Medina I: Opposing role of synaptic and
extra-synaptic NMDA receptors in regulation of the extracellular
signal-regulated kinases (ERK) activity in cultured rat hippocampal
neurons. J Physiol. 572:789–798. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Wu GY, Deisseroth K and Tsien RW:
Activity-dependent CREB phosphorylation: Convergence of a fast,
sensitive calmodulin kinase pathway and a slow, less sensitive
mitogen-activated protein kinase pathway. Proc Natl Acad Sci USA.
98:2808–2813. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Aarts M, Liu Y, Liu L, Besshoh S, Arundine
M, Gurd JW, Wang YT, Salter MW and Tymianski M: Treatment of
ischemic brain damage by perturbing NMDA receptor-PSD-95 protein
interactions. Science. 298:846–850. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Sattler R, Xiong Z, Lu WY, Hafner M,
MacDonald JF and Tymianski M: Specific coupling of NMDA receptor
activation to nitric oxide neurotoxicity by PSD-95 protein.
Science. 284:1845–1848. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Pei L, Shang Y, Jin H, Wang S, Wei N, Yan
H, Wu Y, Yao C, Wang X, Zhu LQ and Lu Y: DAPK1-p53 interaction
converges necrotic and apoptotic pathways of ischemic neuronal
death. J Neurosci. 34:6546–6556. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Tu W, Xu X, Peng L, Zhong X, Zhang W,
Soundarapandian MM, Balel C, Wang M, Jia N, Zhang W, et al: DAPK1
interaction with NMDA receptor NR2B subunits mediates brain damage
in stroke. Cell. 140:222–234. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Ning K, Pei L, Liao M, Liu B, Zhang Y,
Jiang W, Mielke JG, Li L, Chen Y, El-Hayek YH, et al: Dual
neuroprotective signaling mediated by downregulating two distinct
phosphatase activities of PTEN. J Neurosci. 24:4052–4060. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Beschorner R, Adjodah D, Schwab JM,
Mittelbronn M, Pedal I, Mattern R, Schluesener HJ and Meyermann R:
Long-term expression of heme oxygenase-1 (HO-1, HSP-32) following
focal cerebral infarctions and traumatic brain injury in humans.
Acta Neuropathol. 100:377–384. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Komkova MA, Karyakina EE and Karyakin AA:
Catalytically synthesized prussian blue nanoparticles defeating
natural enzyme peroxidase. J Am Chem Soc. 140:11302–11307. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Zhang W, Hu S, Yin JJ, He W, Lu W, Ma M,
Gu N and Zhang Y: Prussian blue nanoparticles as multienzyme
mimetics and reactive oxygen species scavengers. J Am Chem Soc.
138:5860–5865. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Zhang K, Tu M, Gao W, Cai X, Song F, Chen
Z, Zhang Q, Wang J, Jin C, Shi J, et al: Hollow prussian blue
nanozymes drive neuroprotection against ischemic stroke via
attenuating oxidative stress, counteracting inflammation, and
suppressing cell apoptosis. Nano Lett. 19:2812–2823. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Dirnagl U, Klehmet J, Braun JS, Harms H,
Meisel C, Ziemssen T, Prass K and Meisel A: Stroke-induced
immunodepression: Experimental evidence and clinical relevance.
Stroke. 38(Suppl 2): S770–S773. 2007. View Article : Google Scholar
|
|
94
|
Sarvari S, Moakedi F, Hone E, Simpkins JW
and Ren X: Mechanisms in blood-brain barrier opening and
metabolism-challenged cerebrovascular ischemia with emphasis on
ischemic stroke. Metab Brain Dis. 35:851–868. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Simpkins AN, Dias C and Leigh R: National
Institutes of Health Natural History of Stroke Investigators:
Identification of reversible disruption of the human blood-brain
barrier following acute ischemia. Stroke. 47:2405–2408. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Lakhan SE, Kirchgessner A and Hofer M:
Inflammatory mechanisms in ischemic stroke: Therapeutic approaches.
J Transl Med. 7:972009. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Wang Q, Wei J and Shi Y: Platelet
microvesicles promote the recovery of neurological function in
mouse model of cerebral infarction by inducing angiogenesis.
Biochem Biophys Res Commun. 513:997–1004. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Rosińska J, Maciejewska J, Narożny R,
Kozubski W and Łukasik M: Association of platelet-derived
microvesicles with high on-treatment platelet reactivity in
convalescent ischemic stroke patients treated with acetylsalicylic
acid. Wiad Lek. 72:1426–1436. 2019. View Article : Google Scholar
|
|
99
|
Ghoreishy A, Khosravi A and Ghaemmaghami
A: Exosomal microRNA and stroke: A review. J Cell Biochem.
120:16352–16361. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Loffreda A, Nizzardo M, Arosio A, Ruepp
MD, Calogero RA, Volinia S, Galasso M, Bendotti C, Ferrarese C,
Lunetta C, et al: miR-129-5p: A key factor and therapeutic target
in amyotrophic lateral sclerosis. Prog Neurobiol. 190:1018032020.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Krützfeldt J, Kuwajima S, Braich R, Rajeev
KG, Pena J, Tuschl T, Manoharan M and Stoffel M: Specificity,
duplex degradation and subcellular localization of antagomirs.
Nucleic Acids Res. 35:2885–2892. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Jickling GC, Ander BP, Zhan X, Noblett D,
Stamova B and Liu D: microRNA expression in peripheral blood cells
following acute ischemic stroke and their predicted gene targets.
PLoS One. 9:e992832014. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Shi Y, Li K, Xu K and Liu QH: MiR-155-5p
accelerates cerebral ischemia-reperfusion injury via targeting
DUSP14 by regulating NF-κB and MAPKs signaling pathways. Eur Rev
Med Pharmacol Sci. 24:1408–1419. 2020.PubMed/NCBI
|
|
104
|
Sun H, Zhong D, Wang C, Sun Y, Zhao J and
Li G: MiR-298 exacerbates ischemia/reperfusion injury following
ischemic stroke by targeting act1. Cell Physiol Biochem.
48:528–539. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Liu W, Wang X, Zheng Y, Shang G, Huang J,
Tao J and Chen L: Electroacupuncture inhibits inflammatory injury
by targeting the miR-9-mediated NF-κB signaling pathway following
ischemic stroke. Mol Med Rep. 13:1618–1626. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Guo D, Ma J, Li T and Yan L: Up-regulation
of miR-122 protects against neuronal cell death in ischemic stroke
through the heat shock protein 70-dependent NF-κB pathway by
targeting FOXO3. Exp Cell Res. 369:34–42. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Block HS and Biller J: Commonly asked
questions: Thrombolytic therapy in the management of acute stroke.
Expert Rev Neurother. 13:157–165. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Murray V, Norrving B, Sandercock PA,
Terént A, Wardlaw JM and Wester P: The molecular basis of
thrombolysis and its clinical application in stroke. J Intern Med.
267:191–208. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Röther J, Ford GA and Thijs VN:
Thrombolytics in acute ischaemic stroke: Historical perspective and
future opportunities. Cerebrovasc Dis. 35:313–319. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Saver JL: Number needed to treat estimates
incorporating effects over the entire range of clinical outcomes:
Novel derivation method and application to thrombolytic therapy for
acute stroke. Arch Neurol. 61:1066–1070. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Saver JL, Gornbein J, Grotta J, Liebeskind
D, Lutsep H, Schwamm L, Scott P and Starkman S: Number needed to
treat to benefit and to harm for intravenous tissue plasminogen
activator therapy in the 3- to 4.5-h window: Joint outcome table
analysis of the ECASS 3 trial. Stroke. 40:2433–2437. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Ahmed N, Wahlgren N, Grond M, Hennerici M,
Lees KR, Mikulik R, Parsons M, Roine RO and Toni D: Implementation
and outcome of thrombolysis with alteplase 3-4.5 h after an acute
stroke: An updated analysis from SITS-ISTR. Lancet Neurol.
9:866–874. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Schwamm LH, Ali SF, Reeves MJ, Smith EE,
Saver JL, Messe S, Bhatt DL, Grau-Sepulveda MV, Peterson ED and
Fonarow GC: Temporal trends in patient characteristics and
treatment with intravenous thrombolysis among acute ischemic stroke
patients at Get With The Guidelines-Stroke hospitals. Circ
Cardiovasc Qual Outcomes. 6:543–549. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Wahlgren N, Ahmed N, Davalos A, Ford GA,
Grond M, Hacke W, Hennerici MG, Kaste M, Kuelkens S, Larrue V, et
al: Thrombolysis with alteplase for acute ischaemic stroke in the
safe implementation of thrombolysis in stroke-monitoring study
(SITS-MOST): An observational study. Lancet. 369:275–282. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Ingall TJ, O'Fallon WM, Asplund K,
Goldfrank LR, Hertzberg VS, Louis TA and Christianson TJH: Findings
from the reanalysis of the NINDS tissue plasminogen activator for
acute ischemic stroke treatment trial. Stroke. 35:2418–2424. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Jansen O, von Kummer R, Forsting M, Hacke
W and Sartor K: Thrombolytic therapy in acute occlusion of the
intracranial internal carotid artery bifurcation. AJNR Am J
Neuroradiol. 16:1977–1986. 1995.PubMed/NCBI
|
|
117
|
Wolpert SM, Bruckmann H, Greenlee R,
Wechsler L, Pessin MS and del Zoppo GJ: Neuroradiologic evaluation
of patients with acute stroke treated with recombinant tissue
plasminogen activator. The rt-PA acute stroke study group. AJNR Am
J Neuroradiol. 14:3–13. 1993.PubMed/NCBI
|
|
118
|
Mandavia R, Qureshi MI, Dharmarajah B,
Head K and Davies AH: Safety of carotid intervention following
thrombolysis in acute ischaemic stroke. Eur J Vasc Endovasc Surg.
48:505–512. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Furlan AJ and Abou-Chebl A: The role of
recombinant pro-urokinase (r-pro-UK) and intra-arterial
thrombolysis in acute ischaemic stroke: The PROACT trials. Prolyse
in acute cerebral thromboembolism. Curr Med Res Opin. 18(Suppl 2):
S44–S47. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Hao C, Ding W, Xu X, Sun Q, Li X, Wang W,
Zhao Z and Tang L: Effect of recombinant human prourokinase on
thrombolysis in a rabbit model of thromboembolic stroke. Biomed
Rep. 8:77–84. 2018.PubMed/NCBI
|
|
121
|
Agrawal A, Golovoy D, Nimjee S, Ferrell A,
Smith T and Britz G: Mechanical thrombectomy devices for
endovascular management of acute ischemic stroke: Duke stroke
center experience. Asian J Neurosurg. 7:166–170. 2012. View Article : Google Scholar
|
|
122
|
Deng L, Qiu S, Wang L, Li Y, Wang D and
Liu M: Comparison of four food and drug administration-approved
mechanical thrombectomy devices for acute ischemic stroke: A
network meta-analysis. World Neurosurg. 127:e49–e57. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Nogueira RG, Lutsep HL, Gupta R, Jovin TG,
Albers GW, Walker GA, Liebeskind DS and Smith WS: TREVO 2
Trialists: Trevo versus Merci retrievers for thrombectomy
revascularisation of large vessel occlusions in acute ischaemic
stroke (TREVO 2): A randomised trial. Lancet. 380:1231–1240. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Saver JL, Jahan R, Levy EI, Jovin TG,
Baxter B, Nogueira RG, Clark W, Budzik R and Zaidat OO: SWIFT
Trialists: Solitaire flow restoration device versus the merci
retriever in patients with acute ischaemic stroke (SWIFT): A
randomised, parallel-group, non-inferiority trial. Lancet.
380:1241–1249. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Suzuki K, Matsumaru Y, Takeuchi M,
Morimoto M, Kanazawa R, Takayama Y, Kamiya Y, Shigeta K, Okubo S,
Hayakawa M, et al: Effect of mechanical thrombectomy without vs
with intravenous thrombolysis on functional outcome among patients
with acute ischemic stroke: The SKIP randomized clinical trial.
JAMA. 325:244–253. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Machado M, Alves M, Fior A, Fragata I,
Papoila AL, Reis J and Nunes AP: Functional outcome after
mechanical thrombectomy with or without previous thrombolysis. J
Stroke Cerebrovasc Dis. 30:1054952021. View Article : Google Scholar
|
|
127
|
Cirillo C, Le Friec A, Frisach I, Darmana
R, Robert L, Desmoulin F and Loubinoux I: Focal malonate injection
into the internal capsule of rats as a model of lacunar stroke.
Front Neurol. 9:10722018. View Article : Google Scholar
|
|
128
|
Fries W, Danek A, Scheidtmann K and
Hamburger C: Motor recovery following capsular stroke. Role of
descending pathways from multiple motor areas. Brain. 116:369–382.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Haga KK, Gregory LJ, Hicks CA, Ward MA,
Beech JS, Bath PW, Williams SC and O'Neill MJ: The neuronal nitric
oxide synthase inhibitor, TRIM, as a neuroprotective agent: Effects
in models of cerebral ischaemia using histological and magnetic
resonance imaging techniques. Brain Res. 993:42–53. 2003.
View Article : Google Scholar : PubMed/NCBI
|