|
1
|
Knap D, Honkowicz M, Kirmes T, Koroński M,
Bukański M, Kysiak M, Kadłubicki B, Dymon I, Sieroń D and Baron J:
Endovascular treatment of acute ischemic stroke-own experience.
Neurol Neurochir Pol. 49:81–89. 2015.
|
|
2
|
Wang HE, Kabeto MM, Gray M, Wadley VG,
Muntner P, Judd SE, Safford MM, Kempker J and Levine DA: Trajectory
of cognitive decline after sepsis. Crit Care Med. 49:1083–1094.
2021.
|
|
3
|
Feigin VL, Roth GA, Naghavi M, Parmar P,
Krishnamurthi R, Chugh S, Mensah GA, Norrving B, Shiue I, Ng M, et
al: Global burden of stroke and risk factors in 188 countries,
during 1990-2013: A systematic analysis for the global burden of
disease study 2013. Lancet Neurol. 15:913–924. 2016.
|
|
4
|
Sun Y, Yang X, Xu L, Jia M, Zhang L, Li P
and Yang P: The role of Nrf2 in relieving cerebral
ischemia-reperfusion injury. Curr Neuropharmacol. 21:1405–1420.
2023.
|
|
5
|
Jayaraj RL, Azimullah S, Beiram R, Jalal
FY and Rosenberg GA: Neuroinflammation: Friend and foe for ischemic
stroke. J Neuroinflammation. 16:1422019.
|
|
6
|
Boullerne AI and Feinstein DL: History of
neuroscience I. Pío del Río-Hortega (1882-1945): The discoverer of
microglia and oligodendroglia. ASN Neuro.
12:17590914209532592020.
|
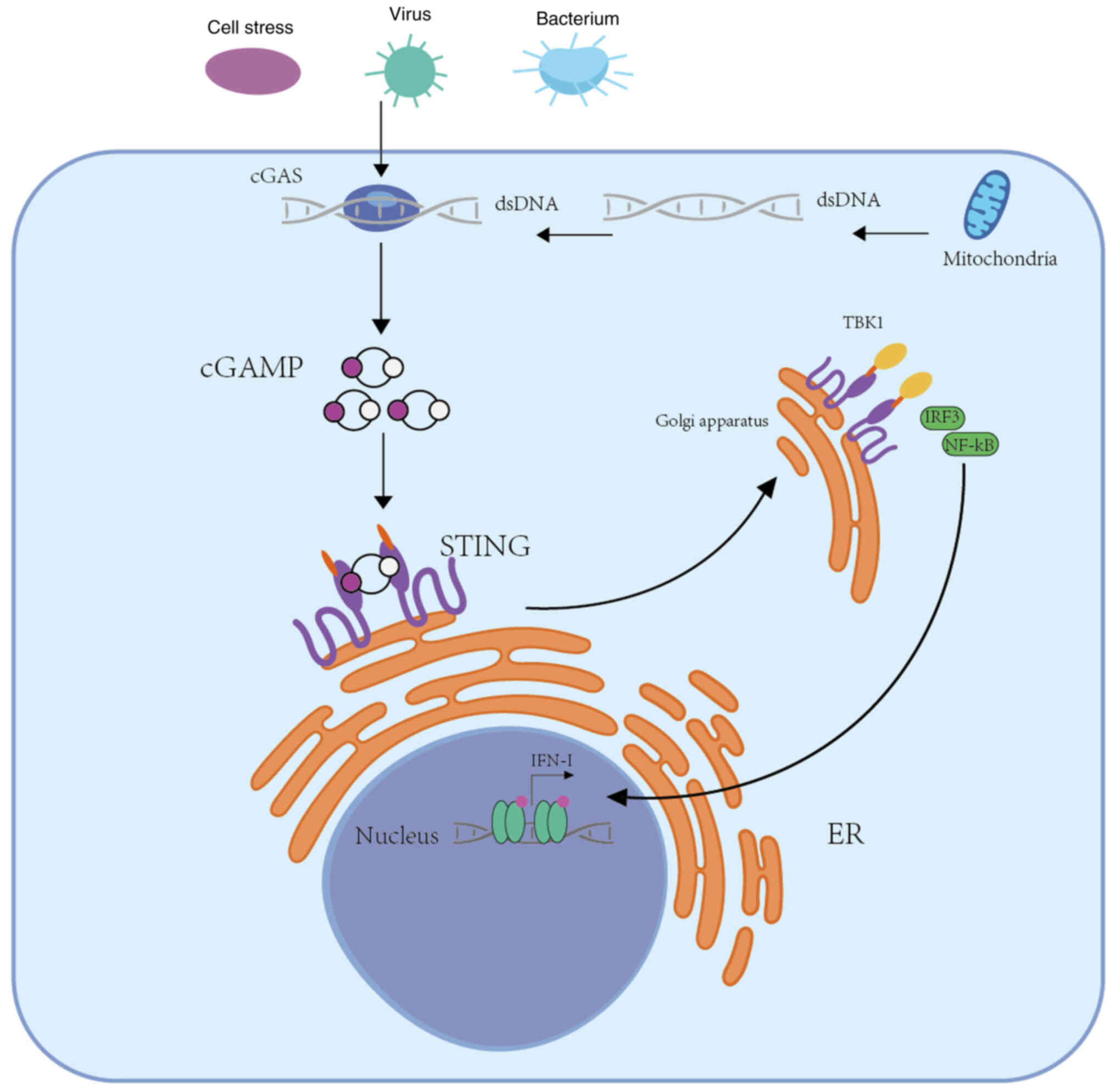
|
7
|
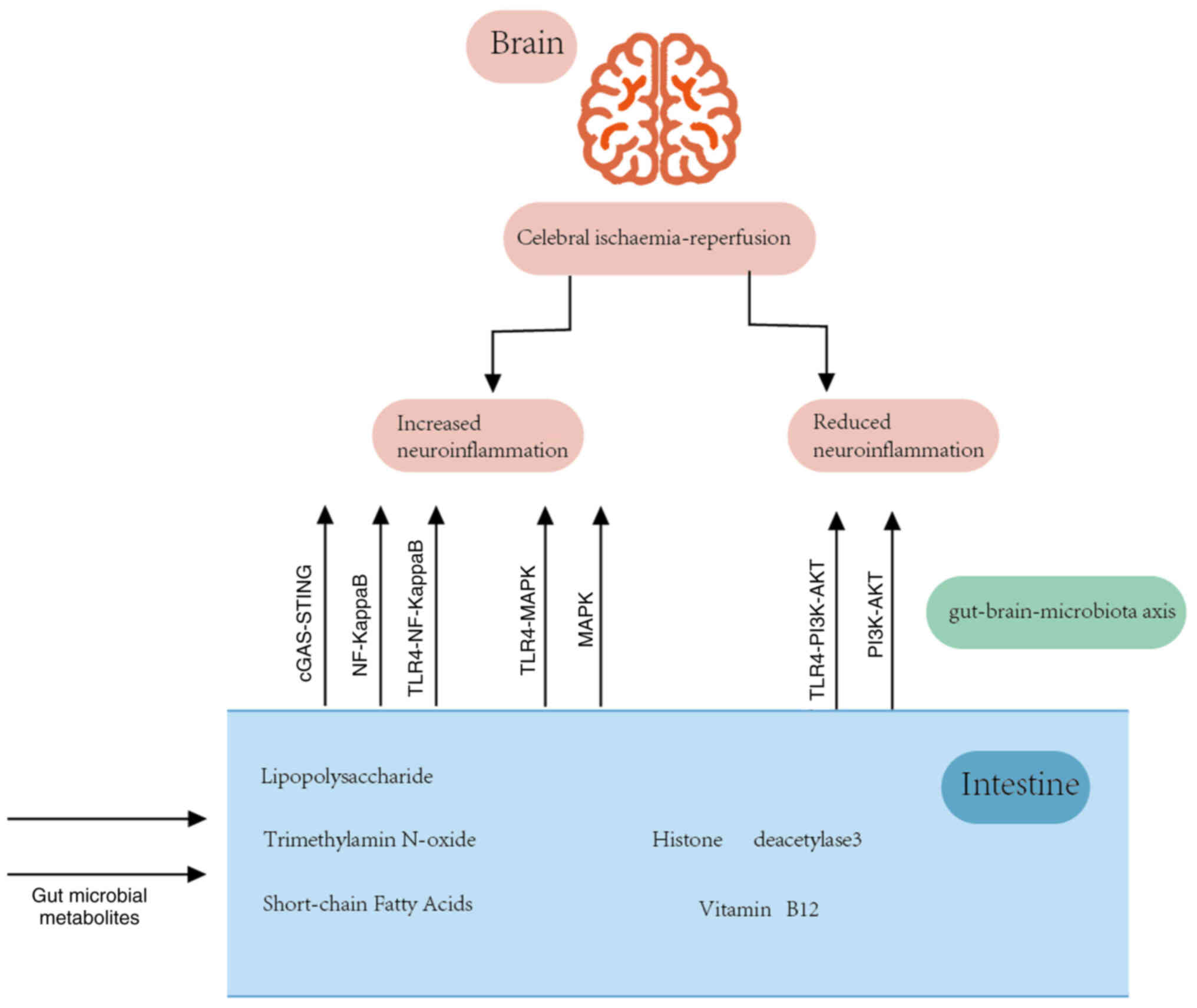
Del Río-Hortega Bereciartu J: Pío del
Río-Hortega: The revolution of glia. Anat Rec (Hoboken).
303:1232–1241. 2020.
|
|
8
|
Kanazawa M, Ninomiya I, Hatakeyama M,
Takahashi T and Shimohata T: Microglia and monocytes/macrophages
polarization reveal novel therapeutic mechanism against stroke. Int
J Mol Sci. 18:21352017.
|
|
9
|
Ito D, Tanaka K, Suzuki S, Dembo T and
Fukuuchi Y: Enhanced expression of Iba1, ionized calcium-binding
adapter molecule 1, after transient focal cerebral ischemia in rat
brain. Stroke. 32:1208–1215. 2001.
|
|
10
|
Wu P, Zeng F, Li YX, Yu BL, Qiu LH, Qin W,
Li J, Zhou YM and Liang FR: Changes of resting cerebral activities
in subacute ischemic stroke patients. Neural Regen Res. 10:760–765.
2015.
|
|
11
|
Guruswamy R and ElAli A: Complex roles of
microglial cells in ischemic stroke pathobiology: New insights and
future directions. Int J Mol Sci. 18:4962017.
|
|
12
|
Perego C, Fumagalli S and De Simoni MG:
Temporal pattern of expression and colocalization of
microglia/macrophage phenotype markers following brain ischemic
injury in mice. J Neuroinflammation. 8:1742011.
|
|
13
|
West AP, Brodsky IE, Rahner C, Woo DK,
Erdjument-Bromage H, Tempst P, Walsh MC, Choi Y, Shadel GS and
Ghosh S: TLR signalling augments macrophage bactericidal activity
through mitochondrial ROS. Nature. 472:476–480. 2011.
|
|
14
|
Chen AQ, Fang Z, Chen XL, Yang S, Zhou YF,
Mao L, Xia YP, Jin HJ, Li YN, You MF, et al: Microglia-derived
TNF-α mediates endothelial necroptosis aggravating blood
brain-barrier disruption after ischemic stroke. Cell Death Dis.
10:4872019.
|
|
15
|
Perez-de-Puig I, Miró-Mur F, Ferrer-Ferrer
M, Gelpi E, Pedragosa J, Justicia C, Urra X, Chamorro A and Planas
AM: Neutrophil recruitment to the brain in mouse and human ischemic
stroke. Acta Neuropathol. 129:239–257. 2015.
|
|
16
|
Roca H, Varsos ZS, Sud S, Craig MJ, Ying C
and Pienta KJ: CCL2 and interleukin-6 promote survival of human
CD11b+ peripheral blood mononuclear cells and induce M2-type
macrophage polarization. J Biol Chem. 284:34342–34354. 2009.
|
|
17
|
Gleissner CA, Shaked I, Little KM and Ley
K: CXC chemokine ligand 4 induces a unique transcriptome in
monocyte-derived macrophages. J Immunol. 184:4810–4818. 2010.
|
|
18
|
Ortega-Gómez A, Perretti M and Soehnlein
O: Resolution of inflammation: An integrated view. EMBO Mol Med.
5:661–674. 2013.
|
|
19
|
Li C, Wu Z, Zhou L, Shao J, Hu X, Xu W,
Ren Y, Zhu X, Ge W, Zhang K, et al: Temporal and spatial cellular
and molecular pathological alterations with single-cell resolution
in the adult spinal cord after injury. Signal Transduct Target
Ther. 7:652022.
|
|
20
|
Ma Y, Wang J, Wang Y and Yang GY: The
biphasic function of microglia in ischemic stroke. Prog Neurobiol.
157:247–272. 2017.
|
|
21
|
Orihuela R, McPherson CA and Harry GJ:
Microglial M1/M2 polarization and metabolic states. Br J Pharmacol.
173:649–665. 2016.
|
|
22
|
Bell-Temin H, Culver-Cochran AE, Chaput D,
Carlson CM, Kuehl M, Burkhardt BR, Bickford PC, Liu B and Stevens
SM Jr: Novel molecular insights into classical and alternative
activation states of microglia as revealed by stable isotope
labeling by amino acids in cell culture (SILAC)-based proteomics.
Mol Cell Proteomics. 14:3173–3184. 2015.
|
|
23
|
Jiang CT, Wu WF, Deng YH and Ge JW:
Modulators of microglia activation and polarization in ischemic
stroke (review). Mol Med Rep. 21:2006–2018. 2020.
|
|
24
|
Suenaga J, Hu X, Pu H, Shi Y, Hassan SH,
Xu M, Leak RK, Stetler RA, Gao Y and Chen J: White matter injury
and microglia/macrophage polarization are strongly linked with
age-related long-term deficits in neurological function after
stroke. Exp Neurol. 272:109–119. 2015.
|
|
25
|
Ritzel RM, Lai YJ, Crapser JD, Patel AR,
Schrecengost A, Grenier JM, Mancini NS, Patrizz A, Jellison ER,
Morales-Scheihing D, et al: Aging alters the immunological response
to ischemic stroke. Acta Neuropathol. 136:89–110. 2018.
|
|
26
|
Badan I, Buchhold B, Hamm A, Gratz M,
Walker LC, Platt D, Kessler Ch and Popa-Wagner A: Accelerated glial
reactivity to stroke in aged rats correlates with reduced
functional recovery. J Cereb Blood Flow Metab. 23:845–854.
2003.
|
|
27
|
Yenari MA: Microglia, the brain's double
agent. J Cereb Blood Flow Metab. 40(1 Suppl): S3–S5. 2020.
|
|
28
|
Kim JW, Park MS, Kim JT, Kang HJ, Bae KY,
Kim SW, Shin MG, Cho KH and Kim JM: The impact of tumor necrosis
factor-α and interleukin-1β levels and polymorphisms on long-term
stroke outcomes. Eur Neurol. 79:38–44. 2018.
|
|
29
|
Pascotini ET, Flores AE, Kegler A, Gabbi
P, Bochi GV, Algarve TD, Prado AL, Duarte MM, da Cruz IB, Moresco
RN, et al: Apoptotic markers and DNA damage are related to late
phase of stroke: Involvement of dyslipidemia and inflammation.
Physiol Behav. 151:369–378. 2015.
|
|
30
|
Wu L, Xiong X, Wu X, Ye Y, Jian Z, Zhi Z
and Gu L: Targeting oxidative stress and inflammation to prevent
ischemia-reperfusion injury. Front Mol Neurosci. 13:282020.
|
|
31
|
Ooboshi H, Ibayashi S, Shichita T, Kumai
Y, Takada J, Ago T, Arakawa S, Sugimori H, Kamouchi M, Kitazono T
and Iida M: Postischemic gene transfer of interleukin-10 protects
against both focal and global brain ischemia. Circulation.
111:913–919. 2005.
|
|
32
|
Yu C, Zhu C, Zhang Y, Chen H, Qin W, Wang
M and Li K: A longitudinal diffusion tensor imaging study on
Wallerian degeneration of corticospinal tract after motor pathway
stroke. Neuroimage. 47:451–458. 2009.
|
|
33
|
Thiel A, Radlinska BA, Paquette C, Sidel
M, Soucy JP, Schirrmacher R and Minuk J: The temporal dynamics of
poststroke neuroinflammation: A longitudinal diffusion tensor
imaging-guided PET study with 11C-PK11195 in acute subcortical
stroke. J Nucl Med. 51:1404–1412. 2010.
|
|
34
|
Price CJ, Wang D, Menon DK, Guadagno JV,
Cleij M, Fryer T, Aigbirhio F, Baron JC and Warburton EA: Intrinsic
activated microglia map to the peri-infarct zone in the subacute
phase of ischemic stroke. Stroke. 37:1749–1753. 2006.
|
|
35
|
Huang T, Yin J, Ren S and Zhang X:
Protective effects of KLF4 on blood-brain barrier and oxidative
stress after cerebral ischemia-reperfusion in rats through the
Nrf2/Trx1 pathway. Cytokine. 169:1562882023.
|
|
36
|
Liddelow SA and Barres BA: Reactive
astrocytes: Production, function, and therapeutic potential.
Immunity. 46:957–967. 2017.
|
|
37
|
Liddelow SA, Guttenplan KA, Clarke LE,
Bennett FC, Bohlen CJ, Schirmer L, Bennett ML, Münch AE, Chung WS,
Peterson TC, et al: Neurotoxic reactive astrocytes are induced by
activated microglia. Nature. 541:481–487. 2017.
|
|
38
|
John GR, Lee SC and Brosnan CF: Cytokines:
powerful regulators of glial cell activation. Neuroscientist.
9:10–22. 2003.
|
|
39
|
Li X, Yin X, Pang J, Chen Z and Wen J:
Hydrogen sulfide inhibits lipopolysaccharide-based
neuroinflammation-induced astrocyte polarization after cerebral
ischemia/reperfusion injury. Eur J Pharmacol. 949:1757432023.
|
|
40
|
Li J, Xu P, Hong Y, Xie Y, Peng M, Sun R,
Guo H, Zhang X, Zhu W, Wang J and Liu X: Lipocalin-2-mediated
astrocyte pyroptosis promotes neuroinflammatory injury via NLRP3
inflammasome activation in cerebral ischemia/reperfusion injury. J
Neuroinflammation. 20:1482023.
|
|
41
|
Okada S, Hara M, Kobayakawa K, Matsumoto Y
and Nakashima Y: Astrocyte reactivity and astrogliosis after spinal
cord injury. Neurosci Res. 126:39–43. 2018.
|
|
42
|
Yuan Y, Liu L, Du Y, Fan R, Zhang R and
Zhou N: p-hydroxy benzaldehyde revitalizes the microenvironment of
peri-infarct cortex in rats after cerebral ischemia-reperfusion.
Phytomedicine. 105:1543792022.
|
|
43
|
Li Z, Song Y, He T, Wen R, Li Y, Chen T,
Huang S, Wang Y, Tang Y, Shen F, et al: M2 microglial small
extracellular vesicles reduce glial scar formation via the
miR-124/STAT3 pathway after ischemic stroke in mice. Theranostics.
11:1232–1248. 2021.
|
|
44
|
Patel JP and Frey BN: Disruption in the
blood-brain barrier: The missing link between brain and body
inflammation in bipolar disorder? Neural Plast.
2015:7083062015.
|
|
45
|
Zhang S, An Q, Wang T, Gao S and Zhou G:
Corrigendum to 'Autophagy- and MMP-2/9-mediated reduction and
redistribution of ZO-1 contribute to hyperglycemia-increased
blood-brain barrier permeability during early reperfusion in
stroke' [Neuroscience 377 (2018) 126-137]. Neuroscience.
386:3512018.
|
|
46
|
Yang Y, Estrada EY, Thompson JF, Liu W and
Rosenberg GA: Matrix metalloproteinase-mediated disruption of tight
junction proteins in cerebral vessels is reversed by synthetic
matrix metalloproteinase inhibitor in focal ischemia in rat. J
Cereb Blood Flow Metab. 27:697–709. 2007.
|
|
47
|
Clemente JC, Ursell LK, Parfrey LW and
Knight R: The impact of the gut microbiota on human health: An
integrative view. Cell. 148:1258–1270. 2012.
|
|
48
|
Erttmann SF, Swacha P, Aung KM, Brindefalk
B, Jiang H, Härtlova A, Uhlin BE, Wai SN and Gekara NO: The gut
microbiota prime systemic antiviral immunity via the
cGAS-STING-IFN-I axis. Immunity. 55:847–861.e10. 2022.
|
|
49
|
Yu H, Liao K, Hu Y, Lv D, Luo M, Liu Q,
Huang L and Luo S: Role of the cGAS-STING pathway in aging-related
endothelial dysfunction. Aging Dis. 13:1901–1918. 2022.
|
|
50
|
Yu CH, Davidson S, Harapas CR, Hilton JB,
Mlodzianoski MJ, Laohamonthonkul P, Louis C, Low RRJ, Moecking J,
De Nardo D, et al: TDP-43 triggers mitochondrial DNA release via
mPTP to activate cGAS/STING in ALS. Cell. 183:636–649.e18.
2020.
|
|
51
|
Kong L, Li W, Chang E, Wang W, Shen N, Xu
X, Wang X, Zhang Y, Sun W, Hu W, et al: mtDNA-STING axis mediates
microglial polarization via IRF3/NF-κB signaling after ischemic
stroke. Front Immunol. 13:8609772022.
|
|
52
|
Ding R, Li H, Liu Y, Ou W, Zhang X, Chai
H, Huang X, Yang W and Wang Q: Activating cGAS-STING axis
contributes to neuroinflammation in CVST mouse model and induces
inflammasome activation and microglia pyroptosis. J
Neuroinflammation. 19:1372022.
|
|
53
|
Gao D, Hao JP, Li BY, Zheng CC, Miao BB
and Zhang L, Li YL, Li L, Li XJ and Zhang L: Tetrahydroxy stilbene
glycoside ameliorates neuroinflammation for Alzheimer's disease via
cGAS-STING. Eur J Pharmacol. 953:1758092023.
|
|
54
|
Wu W, Zhang X, Wang S, Li T, Hao Q, Li S,
Yao W and Sun R: Pharmacological inhibition of the cGAS-STING
signaling pathway suppresses microglial M1-polarization in the
spinal cord and attenuates neuropathic pain. Neuropharmacology.
217:1092062022.
|
|
55
|
Chen Y, Hu Y, He X, Zang H, Sun R, Zhu C
and Yao W: Activation of mitochondrial DNA-mediated cGAS-STING
pathway contributes to chronic postsurgical pain by inducing type I
interferons and A1 reactive astrocytes in the spinal cord. Int
Immunopharmacol. 127:1113482024.
|
|
56
|
Han C, Qian X, Ren X, Zhang S, Hu L, Li J,
Huang Y, Huang R, Ooi K, Lin H and Xia C: Inhibition of cGAS in
paraventricular nucleus attenuates hypertensive heart injury via
regulating microglial autophagy. Mol Neurobiol. 59:7006–7024.
2022.
|
|
57
|
Paludan SR, Reinert LS and Hornung V:
DNA-stimulated cell death: Implications for host defence,
inflammatory diseases and cancer. Nat Rev Immunol. 19:141–153.
2019.
|
|
58
|
Kim HY, Kim TJ, Kang L, Kim YJ, Kang MK,
Kim J, Ryu JH, Hyeon T, Yoon BW, Ko SB and Kim BS: Mesenchymal stem
cell-derived magnetic extracellular nanovesicles for targeting and
treatment of ischemic stroke. Biomaterials. 243:1199422020.
|
|
59
|
Liao Y, Cheng J, Kong X, Li S, Li X, Zhang
M, Zhang H, Yang T, Dong Y, Li J, et al: HDAC3 inhibition
ameliorates ischemia/reperfusion-induced brain injury by regulating
the microglial cGAS-STING pathway. Theranostics. 10:9644–9662.
2020.
|
|
60
|
Nieto-Estevez V, Changarathil G, Adeyeye
AO, Coppin MO, Kassim RS, Zhu J and Hsieh J: HDAC1 regulates
neuronal differentiation. Front Mol Neurosci. 14:8158082021.
|
|
61
|
Wang M, Zhou C, Yu L, Kong D, Ma W, Lv B,
Wang Y, Wu W, Zhou M and Cui G: Upregulation of MDH1 acetylation by
HDAC6 inhibition protects against oxidative stress-derived neuronal
apoptosis following intracerebral hemorrhage. Cell Mol Life Sci.
79:3562022.
|
|
62
|
Gao Y, Liu Y, Zheng D, Ho C, Wen D, Sun J,
Huang L, Liu Y, Li Q and Zhang Y: HDAC5-mediated Smad7 silencing
through MEF2A is critical for fibroblast activation and
hypertrophic scar formation. Int J Biol Sci. 18:5724–5739.
2022.
|
|
63
|
Kang L, Yu H, Yang X, Zhu Y, Bai X, Wang
R, Cao Y, Xu H, Luo H, Lu L, et al: Neutrophil extracellular traps
released by neutrophils impair revascularization and vascular
remodeling after stroke. Nat Commun. 11:24882020.
|
|
64
|
Rosell A, Ortega-Aznar A, Alvarez-Sabín J,
Fernández-Cadenas I, Ribó M, Molina CA, Lo EH and Montaner J:
Increased brain expression of matrix metalloproteinase-9 after
ischemic and hemorrhagic human stroke. Stroke. 37:1399–1406.
2006.
|
|
65
|
Allen ER, Whitefoot-Keliin KM, Palmatier
EM, Mahon AR and Greenlee-Wacker MC: Extracellular vesicles from
A23187-treated neutrophils cause cGAS-STING-dependent IL-6
production by macrophages. Front Immunol. 13:9494512022.
|
|
66
|
Powers WJ, Rabinstein AA, Ackerson T,
Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk
BM, Hoh B, et al: Guidelines for the early management of patients
with acute ischemic stroke: 2019 Update to the 2018 guidelines for
the early management of acute ischemic stroke: A guideline for
healthcare professionals from the american heart
association/American stroke association. Stroke. 50:e344–e418.
2019.
|
|
67
|
Whiteley WN, Slot KB, Fernandes P,
Sandercock P and Wardlaw J: Risk factors for intracranial
hemorrhage in acute ischemic stroke patients treated with
recombinant tissue plasminogen activator: A systematic review and
meta-analysis of 55 studies. Stroke. 43:2904–2909. 2012.
|
|
68
|
Wang R, Zhu Y, Liu Z, Chang L, Bai X, Kang
L, Cao Y, Yang X, Yu H, Shi MJ, et al: Neutrophil extracellular
traps promote tPA-induced brain hemorrhage via cGAS in mice with
stroke. Blood. 138:91–103. 2021.
|
|
69
|
Yang LY, Luo Q, Lu L, Zhu WW, Sun HT, Wei
R, Lin ZF, Wang XY, Wang CQ, Lu M, et al: Increased neutrophil
extracellular traps promote metastasis potential of hepatocellular
carcinoma via provoking tumorous inflammatory response. J Hematol
Oncol. 13:32020.
|
|
70
|
Liu M, Xu Z, Wang L, Zhang L, Liu Y, Cao
J, Fu Q, Liu Y, Li H, Lou J, et al: Cottonseed oil alleviates
ischemic stroke injury by inhibiting the inflammatory activation of
microglia and astrocyte. J Neuroinflammation. 17:2702020.
|
|
71
|
Luo L, Liu M, Fan Y, Zhang J, Liu L, Li Y,
Zhang Q, Xie H, Jiang C, Wu J, et al: Intermittent theta-burst
stimulation improves motor function by inhibiting neuronal
pyroptosis and regulating microglial polarization via
TLR4/NFκB/NLRP3 signaling pathway in cerebral ischemic mice. J
Neuroinflammation. 19:1412022.
|
|
72
|
Zhu H, Jian Z, Zhong Y, Ye Y, Zhang Y, Hu
X, Pu B, Gu L and Xiong X: Janus kinase inhibition ameliorates
ischemic stroke injury and neuroinflammation through reducing NLRP3
inflammasome activation via JAK2/STAT3 pathway inhibition. Front
Immunol. 12:7149432021.
|
|
73
|
Ning L, Wei W, Wenyang J, Rui X and Qing
G: Cytosolic DNA-STING-NLRP3 axis is involved in murine acute lung
injury induced by lipopolysaccharide. Clin Transl Med.
10:e2282020.
|
|
74
|
Liu X, Lv X, Liu Z, Zhang M and Leng Y:
MircoRNA-29a in astrocyte-derived extracellular vesicles suppresses
brain ischemia reperfusion injury via TP53INP1 and the NF-κB/NLRP3
axis. Cell Mol Neurobiol. 42:1487–1500. 2022.
|
|
75
|
He M, Fan J, Zhou R, Gao G, Li R, Zuo Y,
Li B, Li Y and Sun T: NLRP3/Caspase-1-mediated pyroptosis of
astrocytes induced by antipsychotics is inhibited by a histamine H1
receptor-selective agonist. Front Aging Neurosci.
14:8475612022.
|
|
76
|
Grenham S, Clarke G, Cryan JF and Dinan
TG: Brain-gutmicrobe communication in health and disease. Front
Physiol. 2:942011.
|
|
77
|
Vogt NM, Kerby RL, Dill-McFarland KA,
Harding SJ, Merluzzi AP, Johnson SC, Carlsson CM, Asthana S,
Zetterberg H, Blennow K, et al: Gut microbiome alterations in
Alzheimer's disease. Sci Rep. 7:135372017.
|
|
78
|
Qin J, Li R, Raes J, Arumugam M, Burgdorf
KS, Manichanh C, Nielsen T, Pons N, Levenez F, Yamada T, et al: A
human gut microbial gene catalogue established by metagenomic
sequencing. Nature. 464:59–65. 2010.
|
|
79
|
Ling Y, Gong T, Zhang J, Gu Q, Gao X, Weng
X, Liu J and Sun J: Gut microbiome signatures are biomarkers for
cognitive impairment in patients with ischemic stroke. Front Aging
Neurosci. 12:5115622020.
|
|
80
|
Huang QX, Liang JL, Yang CH, Li K, Niu MT,
Fan JX and Zhang XZ: Stimulation-responsive mucoadhesive probiotics
for inflammatory bowel disease treatment by scavenging reactive
oxygen species and regulating gut microbiota. Biomaterials.
301:1222742023.
|
|
81
|
Zhou Y, Xie L, Schröder J, Schuster IS,
Nakai M, Sun G, Sun YBY, Mariño E, Degli-Esposti MA, Marques FZ, et
al: Dietary fiber and microbiota metabolite receptors enhance
cognition and alleviate disease in the 5xFAD mouse model of
Alzheimer's disease. J Neurosci. 43:6460–6475. 2023.
|
|
82
|
Qiao CM, Zhou Y, Quan W, Ma XY, Zhao LP,
Shi Y, Hong H, Wu J, Niu GY, Chen YN, et al: Fecal microbiota
transplantation from aged mice render recipient mice resistant to
MPTP-induced nigrostriatal degeneration via a
neurogenesis-dependent but inflammation-independent manner.
Neurotherapeutics. 20:1405–1426. 2023.
|
|
83
|
Liu C, Cheng X, Zhong S, Liu Z, Liu F, Lin
X, Zhao Y, Guan M, Xiao T, Jolkkonen J, et al: Long-term
modification of gut microbiota by broad-spectrum antibiotics
improves stroke outcome in rats. Stroke Vasc Neurol. 7:381–389.
2022.
|
|
84
|
Peter I, Dubinsky M, Bressman S, Park A,
Lu C, Chen N and Wang A: Anti-tumor necrosis factor therapy and
incidence of parkinson disease among patients with inflammatory
bowel disease. JAMA Neurol. 75:939–946. 2018.
|
|
85
|
Huang PY, Liu HM, Ko YR, Chang ZY and Lee
TY: Electroacupuncture relieves portal hypertension by improving
vascular angiogenesis and linking gut microbiota in bile duct
ligation rats. Front Microbiol. 14:12071372023.
|
|
86
|
Martin-Gallausiaux C, Marinelli L,
Blottière HM, Larraufie P and Lapaque N: SCFA: Mechanisms and
functional importance in the gut. Proc Nutr Soc. 80:37–49.
2021.
|
|
87
|
Louis P, Hold GL and Flint HJ: The gut
microbiota, bacterial metabolites and colorectal cancer. Nat Rev
Microbiol. 12:661–672. 2014.
|
|
88
|
Awoniyi M, Wang J, Ngo B, Meadows V, Tam
J, Viswanathan A, Lai Y, Montgomery S, Farmer M, Kummen M, et al:
Protective and aggressive bacterial subsets and metabolites modify
hepatobiliary inflammation and fibrosis in a murine model of PSC.
Gut. 72:671–685. 2023.
|
|
89
|
Chen R, Xu Y, Wu P, Zhou H, Lasanajak Y,
Fang Y, Tang L, Ye L, Li X, Cai Z and Zhao J: Transplantation of
fecal microbiota rich in short chain fatty acids and butyric acid
treat cerebral ischemic stroke by regulating gut microbiota.
Pharmacol Res. 148:1044032019.
|
|
90
|
Lee J, d'Aigle J, Atadja L, Quaicoe V,
Honarpisheh P, Ganesh BP, Hassan A, Graf J, Petrosino J, Putluri N,
et al: Gut microbiota-derived short-chain fatty acids promote
poststroke recovery in aged mice. Circ Res. 127:453–465. 2020.
|
|
91
|
Erny D, Hrabě de Angelis AL, Jaitin D,
Wieghofer P, Staszewski O, David E, Keren-Shaul H, Mahlakoiv T,
Jakobshagen K, Buch T, et al: Host microbiota constantly control
maturation and function of microglia in the CNS. Nat Neurosci.
18:965–977. 2015.
|
|
92
|
Jaworska J, Zalewska T, Sypecka J and
Ziemka-Nalecz M: Effect of the HDAC inhibitor, sodium butyrate, on
neurogenesis in a rat model of neonatal hypoxia-ischemia: Potential
mechanism of action. Mol Neurobiol. 56:6341–6370. 2019.
|
|
93
|
Sadler R, Cramer JV, Heindl S, Kostidis S,
Betz D, Zuurbier KR, Northoff BH, Heijink M, Goldberg MP, Plautz
EJ, et al: Short-chain fatty acids improve poststroke recovery via
immunological mechanisms. J Neurosci. 40:1162–1173. 2020.
|
|
94
|
Fryc J and Naumnik B: Thrombolome and its
emerging role in chronic kidney diseases. Toxins (Basel).
13:2232021.
|
|
95
|
Wu C, Li C, Zhao W, Xie N, Yan F, Lian Y,
Zhou L, Xu X, Liang Y, Wang L, et al: Elevated trimethylamine
N-oxide related to ischemic brain lesions after carotid artery
stenting. Neurology. 90:e1283–e1290. 2018.
|
|
96
|
Cho CE, Taesuwan S, Malysheva OV, Bender
E, Tulchinsky NF, Yan J, Sutter JL and Caudill MA:
Trimethylamine-N-oxide (TMAO) response to animal source foods
varies among healthy young men and is influenced by their gut
microbiota composition: A randomized controlled trial. Mol Nutr
Food Res. 61:16003242017.
|
|
97
|
Garcia-Perez I, Posma JM, Gibson R,
Chambers ES, Hansen TH, Vestergaard H, Hansen T, Beckmann M,
Pedersen O, Elliott P, et al: Objective assessment of dietary
patterns by use of metabolic phenotyping: A randomised, controlled,
crossover trial. Lancet Diabetes Endocrinol. 5:184–195. 2017.
|
|
98
|
Wang Z, Klipfell E, Bennett BJ, Koeth R,
Levison BS, Dugar B, Feldstein AE, Britt EB, Fu X, Chung YM, et al:
Gut flora metabolism of phosphatidylcholine promotes cardiovascular
disease. Nature. 472:57–63. 2011.
|
|
99
|
Wang Z, Hazen J, Jia X, Org E, Zhao Y,
Osborn LJ, Nimer N, Buffa J, Culley MK, Krajcik D, et al: The
nutritional supplement l-alpha glycerylphosphorylcholine promotes
atherosclerosis. Int J Mol Sci. 22:134772021.
|
|
100
|
Rexidamu M, Li H, Jin H and Huang J: Serum
levels of trimethylamine-N-oxide in patients with ischemic stroke.
Biosci Rep. 39:BSR201905152019.
|
|
101
|
Zheng L, Zheng J, Xie Y, Li Z, Guo X, Sun
G, Sun Z, Xing F and Sun Y: Serum gut microbe-dependent
trimethylamine N-oxide improves the prediction of future
cardiovascular disease in a community-based general population.
Atherosclerosis. 280:126–131. 2019.
|
|
102
|
Zhu W, Gregory JC, Org E, Buffa JA, Gupta
N, Wang Z, Li L, Fu X, Wu Y, Mehrabian M, et al: Gut microbial
metabolite TMAO enhances platelet hyperreactivity and thrombosis
risk. Cell. 165:111–124. 2016.
|
|
103
|
Svingen GFT, Zuo H, Ueland PM, Seifert R,
Løland KH, Pedersen ER, Schuster PM, Karlsson T, Tell GS,
Schartum-Hansen H, et al: Increased plasma trimethylamine-N-oxide
is associated with incident atrial fibrillation. Int J Cardiol.
267:100–106. 2018.
|
|
104
|
Qi J, You T, Li J, Pan T, Xiang L, Han Y
and Zhu L: Circulating trimethylamine N-oxide and the risk of
cardiovascular diseases: A systematic review and meta-analysis of
11 prospective cohort studies. J Cell Mol Med. 22:185–194.
2018.
|
|
105
|
Dávalos A and Secades J: Citicoline
preclinical and clinical update 2009-2010. Stroke. 42(1 Suppl):
S36–S39. 2011.
|
|
106
|
Agarwal A, Vishnu VY, Sharma J, Bhatia R,
Garg A, Dwivedi S, Upadhyay A, Goyal V, Singh MB, Gupta A, et al:
Citicoline in acute ischemic stroke: A randomized controlled trial.
PLoS One. 17:e02692242022.
|
|
107
|
Martí-Carvajal AJ, Valli C, Martí-Amarista
CE, Solà I, Martí-Fàbregas J and Bonfill Cosp X: Citicoline for
treating people with acute ischemic stroke. Cochrane Database Syst
Rev. 8:CD0130662020.
|
|
108
|
Synoradzki K and Grieb P: Citicoline: A
superior form of choline? Nutrients. 11:15692019.
|
|
109
|
Lurz E, Horne RG, Määttänen P, Wu RY,
Botts SR, Li B, Rossi L, Johnson-Henry KC, Pierro A, Surette MG and
Sherman PM: Vitamin B12 deficiency alters the gut microbiota in a
murine model of colitis. Front Nutr. 7:832020.
|
|
110
|
Thakkar K and Billa G: Treatment of
vitamin B12 deficiency-methylcobalamine? Cyancobalamine?
Hydroxocobalamin?-clearing the confusion. Eur J Clin Nutr. 69:1–2.
2015.
|
|
111
|
Van Guelpen B, Hultdin J, Johansson I,
Stegmayr B, Hallmans G, Nilsson TK, Weinehall L, Witthöft C,
Palmqvist R and Winkvist A: Folate, vitamin B12, and risk of
ischemic and hemorrhagic stroke: A prospective, nested
case-referent study of plasma concentrations and dietary intake.
Stroke. 36:1426–1431. 2005.
|
|
112
|
Arora K, Sequeira JM, Alarcon JM, Wasek B,
Arning E, Bottiglieri T and Quadros EV: Neuropathology of vitamin
B12 deficiency in the Cd320−/− mouse. FASEB
J. 33:2563–2573. 2019.
|
|
113
|
Wang M, Liang X, Cheng M, Yang L, Liu H,
Wang X, Sai N and Zhang X: Homocysteine enhances neural stem cell
autophagy in in vivo and in vitro model of ischemic stroke. Cell
Death Dis. 10:5612019.
|
|
114
|
Gurwara S, Ajami NJ, Jang A, Hessel FC,
Chen L, Plew S, Wang Z, Graham DY, Hair C, White DL, et al: Dietary
nutrients involved in one-carbon metabolism and colonic
mucosa-associated gut microbiome in individuals with an
endoscopically normal colon. Nutrients. 11:6132019.
|
|
115
|
Zhang Q, Wei J, Liu Z, Huang X, Sun M, Lai
W, Chen Z, Wu J, Chen Y, Guo X and Huang Q: STING signaling sensing
of DRP1-dependent mtDNA release in kupffer cells contributes to
lipopolysaccharide-induced liver injury in mice. Redox Biol.
54:1023672022.
|
|
116
|
Zhao Z, Ning J, Bao XQ, Shang M, Ma J, Li
G and Zhang D: Fecal microbiota transplantation protects
rotenone-induced Parkinson's disease mice via suppressing
inflammation mediated by the lipopolysaccharide-TLR4 signaling
pathway through the microbiota-gut-brain axis. Microbiome.
9:2262021.
|
|
117
|
Ryu KY, Lee HJ, Woo H, Kang RJ, Han KM,
Park H, Lee SM, Lee JY, Jeong YJ, Nam HW, et al: Dasatinib
regulates LPS-induced microglial and astrocytic neuroinflammatory
responses by inhibiting AKT/STAT3 signaling. J Neuroinflammation.
16:1902019.
|
|
118
|
Wang P, Zhang X, Zheng X, Gao J, Shang M,
Xu J and Liang H: Folic acid protects against hyperuricemia in
C57BL/6J mice via ameliorating gut-kidney axis dysfunction. J Agric
Food Chem. 70:15787–15803. 2022.
|
|
119
|
Darbandi ZK, Amirahmadi S, Goudarzi I,
Hosseini M and Rajabian A: Folic acid improved memory and learning
function in a rat model of neuroinflammation induced by
lipopolysaccharide. Inflammopharmacology. Aug 23–2023.Epub ahead of
print.
|
|
120
|
Yi J, Lu J, Yang A and Marsh EB:
In-hospital predictors of post-stroke depression for targeted
initiation of selective serotonin reuptake inhibitors (SSRIs). BMC
Psychiatry. 22:7222022.
|
|
121
|
Liu F, Song M, Huang X, Yi H, Chen H and
Tian F: Symptomatic plaque enhancement is associated with
early-onset post-stroke depression. J Affect Disord. 306:281–287.
2022.
|
|
122
|
Chen Z, Luo J, Li J, Kim G, Stewart A,
Urban JF Jr, Huang Y, Chen S, Wu LG, Chesler A, et al:
Interleukin-33 promotes serotonin release from enterochromaffin
cells for intestinal homeostasis. Immunity. 54:151–163.e6.
2021.
|
|
123
|
Li T, Fu B, Zhang X, Zhou Y, Yang M, Cao
M, Chen Y, Tan Y and Hu R: Overproduction of gastrointestinal 5-HT
promotes colitis-associated colorectal cancer progression via
enhancing NLRP3 inflammasome activation. Cancer Immunol Res.
9:1008–1023. 2021.
|
|
124
|
Franke M, Bieber M, Kraft P, Weber ANR,
Stoll G and Schuhmann MK: The NLRP3 inflammasome drives
inflammation in ischemia/reperfusion injury after transient middle
cerebral artery occlusion in mice. Brain Behav Immun. 92:223–233.
2021.
|
|
125
|
Zhang S, Wei D, Lv S, Wang L, An H, Shao
W, Wang Y, Huang Y, Peng D and Zhang Z: Scutellarin modulates the
microbiota-gut-brain axis and improves cognitive impairment in
APP/PS1 mice. J Alzheimers Dis. 89:955–975. 2022.
|
|
126
|
Wang X, Wang Z, Cao J, Dong Y and Chen Y:
Gut microbiota-derived metabolites mediate the neuroprotective
effect of melatonin in cognitive impairment induced by sleep
deprivation. Microbiome. 11:172023.
|
|
127
|
Zhao C, Bao L, Zhao Y, Wu K, Qiu M, Feng
L, Zhang N, Hu X and Fu Y: A fiber-enriched diet alleviates
Staphylococcus aureus-induced mastitis by activating the
HDAC3-mediated antimicrobial program in macrophages via butyrate
production in mice. PLoS Pathog. 19:e10111082023.
|
|
128
|
Round JL and Mazmanian SK: The gut
microbiota shapes intestinal immune responses during health and
disease. Nat Rev Immunol. 9:313–323. 2009.
|
|
129
|
Gelderblom M, Weymar A, Bernreuther C,
Velden J, Arunachalam P, Steinbach K, Orthey E, Arumugam TV,
Leypoldt F, Simova O, et al: Neutralization of the IL-17 axis
diminishes neutrophil invasion and protects from ischemic stroke.
Blood. 120:3793–3802. 2012.
|
|
130
|
Lim K, Hyun YM, Lambert-Emo K, Capece T,
Bae S, Miller R, Topham DJ and Kim M: Neutrophil trails guide
influenza-specific CD8+ T cells in the airways. Science.
349:aaa43522015.
|
|
131
|
Huppert J, Closhen D, Croxford A, White R,
Kulig P, Pietrowski E, Bechmann I, Becher B, Luhmann HJ, Waisman A
and Kuhlmann CR: Cellular mechanisms of IL-17-induced blood-brain
barrier disruption. FASEB J. 24:1023–1034. 2010.
|
|
132
|
Ni P, Dong H, Wang Y, Zhou Q, Xu M, Qian Y
and Sun J: IL-17A contributes to perioperative neurocognitive
disorders through blood-brain barrier disruption in aged mice. J
Neuroinflammation. 15:3322018.
|
|
133
|
Li T, Zhang YM, Han D, Hua R, Guo BN, Hu
SQ, Yan XL and Xu T: Involvement of IL-17 in secondary brain injury
after a traumatic brain injury in rats. Neuromolecular Med.
19:541–554. 2017.
|
|
134
|
Liu T, Han S, Dai Q, Zheng J, Liu C, Li S
and Li J: IL-17A-mediated excessive autophagy aggravated neuronal
ischemic injuries via Src-PP2B-mTOR pathway. Front Immunol.
10:29522019.
|
|
135
|
Benakis C, Brea D, Caballero S, Faraco G,
Moore J, Murphy M, Sita G, Racchumi G, Ling L, Pamer EG, et al:
Commensal microbiota affects ischemic stroke outcome by regulating
intestinal γδ T cells. Nat Med. 22:516–523. 2016.
|
|
136
|
Park KP, Rosell A, Foerch C, Xing C, Kim
WJ, Lee S, Opdenakker G, Furie KL and Lo EH: Plasma and brain
matrix metalloproteinase-9 after acute focal cerebral ischemia in
rats. Stroke. 40:2836–2842. 2009.
|
|
137
|
Li TT, Zhao DM, Wei YT, Li JB, Li XF, Wan
Q, Zhang X, Liu XN, Yang WC and Li WZ: Effect and mechanism of
sodium butyrate on neuronal recovery and prognosis in diabetic
stroke. J Neuroimmune Pharmacol. 18:366–382. 2023.
|
|
138
|
Yuan C, Shi L, Sun Z, Xu F, Wang C, Shan
J, Hitchens TK, Foley LM, Ye Q, Chen J, et al: Regulatory T cell
expansion promotes white matter repair after stroke. Neurobiol Dis.
179:1060632023.
|
|
139
|
Kim HJ, Wei Y, Wojtkiewicz GR, Lee JY,
Moskowitz MA and Chen JW: Reducing myeloperoxidase activity
decreases inflammation and increases cellular protection in
ischemic stroke. J Cereb Blood Flow Metab. 39:1864–1877. 2019.
|
|
140
|
Rosell A, Cuadrado E, Ortega-Aznar A,
Hernández-Guillamon M, Lo EH and Montaner J: MMP-9-positive
neutrophil infiltration is associated to blood-brain barrier
breakdown and basal lamina type IV collagen degradation during
hemorrhagic transformation after human ischemic stroke. Stroke.
39:1121–1126. 2008.
|
|
141
|
Si W, Liang H, Bugno J, Xu Q, Ding X, Yang
K, Fu Y, Weichselbaum RR, Zhao X and Wang L: Lactobacillus
rhamnosus GG induces cGAS/STING-dependent type I interferon and
improves response to immune checkpoint blockade. Gut. 71:521–533.
2022.
|
|
142
|
Dooyema SDR, Noto JM, Wroblewski LE,
Piazuelo MB, Krishna U, Suarez G, Romero-Gallo J, Delgado AG and
Peek RM: Helicobacter pylori actively suppresses innate
immune nucleic acid receptors. Gut Microbes. 14:21051022022.
|
|
143
|
Hu Q, Ren H, Li G, Wang D, Zhou Q, Wu J,
Zheng J, Huang J, Slade DA, Wu X and Ren J: STING-mediated
intestinal barrier dysfunction contributes to lethal sepsis.
EBioMedicine. 41:497–508. 2019.
|
|
144
|
Canesso MCC, Lemos L, Neves TC, Marim FM,
Castro TBR, Veloso ÉS, Queiroz CP, Ahn J, Santiago HC, Martins FS,
et al: The cytosolic sensor STING is required for intestinal
homeostasis and control of inflammation. Mucosal Immunol.
11:820–834. 2018.
|
|
145
|
Yang K, Hou Y, Zhang Y, Liang H, Sharma A,
Zheng W, Wang L, Torres R, Tatebe K, Chmura SJ, et al: Suppression
of local type I interferon by gut microbiota-derived butyrate
impairs antitumor effects of ionizing radiation. J Exp Med.
218:e202019152021.
|
|
146
|
Wang H, Chen S, Zhang Y, Xu H and Sun H:
Electroacupuncture ameliorates neuronal injury by
Pink1/Parkin-mediated mitophagy clearance in cerebral
ischemia-reperfusion. Nitric Oxide. 91:23–34. 2019.
|
|
147
|
Liu Z, Wang M, Wang X, Bu Q, Wang Q, Su W,
Li L, Zhou H and Lu L: XBP1 deficiency promotes hepatocyte
pyroptosis by impairing mitophagy to activate mtDNA-cGAS-STING
signaling in macrophages during acute liver injury. Redox Biol.
52:1023052022.
|
|
148
|
Sliter DA, Martinez J, Hao L, Chen X, Sun
N, Fischer TD, Burman JL, Li Y, Zhang Z, Narendra DP, et al: Parkin
and PINK1 mitigate STING-induced inflammation. Nature. 561:258–262.
2018.
|
|
149
|
Gao X, Yin Y, Liu S, Dong K, Wang J and
Guo C: Fucoidan-proanthocyanidins nanoparticles protect against
cisplatin-induced acute kidney injury by activating mitophagy and
inhibiting mtDNA-cGAS/STING signaling pathway. Int J Biol Macromol.
245:1255412023.
|
|
150
|
Tian T, Cao L, He C, Ye Q, Liang R, You W,
Zhang H, Wu J, Ye J, Tannous BA and Gao J: Targeted delivery of
neural progenitor cell-derived extracellular vesicles for
anti-inflammation after cerebral ischemia. Theranostics.
11:6507–6521. 2021.
|
|
151
|
Dong X, Wang L, Song G, Cai X, Wang W,
Chen J and Wang G: Physcion protects rats against cerebral
ischemia-reperfusion injury via inhibition of TLR4/NF-kB signaling
pathway. Drug Des Devel Ther. 15:277–287. 2021.
|
|
152
|
Hou Y, Wang K, Wan W, Cheng Y, Pu X and Ye
X: Resveratrol provides neuroprotection by regulating the
JAK2/STAT3/PI3K/AKT/mTOR pathway after stroke in rats. Genes Dis.
5:245–255. 2018.
|
|
153
|
Fu C, Wu Y, Liu S, Luo C, Lu Y, Liu M,
Wang L, Zhang Y and Liu X: Rehmannioside A improves cognitive
impairment and alleviates ferroptosis via activating PI3K/AKT/Nrf2
and SLC7A11/GPX4 signaling pathway after ischemia. J
Ethnopharmacol. 289:1150212022.
|
|
154
|
Li N, Zhou H, Wu H, Wu Q, Duan M, Deng W
and Tang Q: STING-IRF3 contributes to lipopolysaccharide-induced
cardiac dysfunction, inflammation, apoptosis and pyroptosis by
activating NLRP3. Redox Biol. 24:1012152019.
|
|
155
|
Xie X, Wu X, Zhao D, Liu Y, Du Q, Li Y, Xu
Y, Li Y, Qiu Y and Yang Y: Fluvoxamine alleviates bleomycin-induced
lung fibrosis via regulating the cGAS-STING pathway. Pharmacol Res.
187:1065772023.
|
|
156
|
Sun J, Zhou YQ, Xu BY, Li JY, Zhang LQ, Li
DY, Zhang S, Wu JY, Gao SJ, Ye DW and Mei W:
STING/NF-κB/IL-6-mediated inflammation in microglia contributes to
spared nerve injury (SNI)-induced pain initiation. J Neuroimmune
Pharmacol. 17:453–469. 2022.
|
|
157
|
Zhou Q, Zhang Y, Lu L, Zhang H, Zhao C, Pu
Y and Yin L: Copper induces microglia-mediated neuroinflammation
through ROS/NF-κB pathway and mitophagy disorder. Food Chem
Toxicol. 168:1133692022.
|
|
158
|
Osanai T, Fujiwara N, Sasaki S, Metoki N,
Saitoh G, Tomita H, Nishimura T, Shibutani S, Yokoyama H, Konta Y,
et al: Novel pro-atherogenic molecule coupling factor 6 is elevated
in patients with stroke: A possible linkage to homocysteine. Ann
Med. 42:79–86. 2010.
|
|
159
|
Somensi N, Rabelo TK, Guimarães AG,
Quintans-Junior LJ, de Souza Araújo AA, Moreira JCF and Gelain DP:
Carvacrol suppresses LPS-induced pro-inflammatory activation in RAW
264.7 macrophages through ERK1/2 and NF-kB pathway. Int
Immunopharmacol. 75:1057432019.
|
|
160
|
Tian M, Yang M, Li Z, Wang Y, Chen W, Yang
L, Li Y and Yuan H: Fluoxetine suppresses inflammatory reaction in
microglia under OGD/R challenge via modulation of NF-κB signaling.
Biosci Rep. 39:BSR201815842019.
|
|
161
|
Rahimian R, Fakhfouri G, Ejtemaei Mehr S,
Ghia JE, Genazzani AA, Payandemehr B, Dehpour AR, Mousavizadeh K
and Lim D: Tropisetron attenuates amyloid-beta-induced inflammatory
and apoptotic responses in rats. Eur J Clin Invest. 43:1039–1051.
2013.
|
|
162
|
Feng C, Wan H, Zhang Y, Yu L, Shao C, He
Y, Wan H and Jin W: Neuroprotective effect of danhong injection on
cerebral ischemia-reperfusion injury in rats by activation of the
PI3K-Akt pathway. Front Pharmacol. 11:2982020.
|
|
163
|
Li Y, Xiang L, Wang C, Song Y, Miao J and
Miao M: Protection against acute cerebral ischemia/reperfusion
injury by Leonuri Herba Total Alkali via modulation of
BDNF-TrKB-PI3K/Akt signaling pathway in rats. Biomed Pharmacother.
133:1110212021.
|
|
164
|
Pan B, Sun J, Liu Z, Wang L, Huo H, Zhao
Y, Tu P, Xiao W, Zheng J and Li J: Longxuetongluo Capsule protects
against cerebral ischemia/reperfusion injury through endoplasmic
reticulum stress and MAPK-mediated mechanisms. J Adv Res.
33:215–225. 2021.
|
|
165
|
Tsai YT, Huang HC, Kao ST, Chang TT and
Cheng CY: Neuroprotective effects of alpinia oxyphylla Miq against
mitochondria-related apoptosis by the interactions between
upregulated p38 MAPK signaling and downregulated JNK signaling in
the subacute phase of cerebral ischemia-reperfusion in rats. Am J
Chin Med. 50:2057–2083. 2022.
|
|
166
|
Xu D, Kong T, Shao Z, Liu M, Zhang R,
Zhang S, Kong Q, Chen J, Cheng B and Wang C: Orexin-A alleviates
astrocytic apoptosis and inflammation via inhibiting OX1R-mediated
NF-κB and MAPK signaling pathways in cerebral ischemia/reperfusion
injury. Biochim Biophys Acta Mol Basis Dis. 1867:1662302021.
|
|
167
|
Chen B, Cao P, Guo X, Yin M, Li X, Jiang
L, Shao J, Chen X, Jiang C, Tao L, et al: Maraviroc, an inhibitor
of chemokine receptor type 5, alleviates neuroinflammatory response
after cerebral Ischemia/reperfusion injury via regulating
MAPK/NF-κB signaling. Int Immunopharmacol. 108:1087552022.
|
|
168
|
Xian M, Cai J, Zheng K, Liu Q, Liu Y, Lin
H, Liang S and Wang S: Aloe-emodin prevents nerve injury and
neuroinflammation caused by ischemic stroke via the PI3K/AKT/mTOR
and NF-κB pathway. Food Funct. 12:8056–8067. 2021.
|
|
169
|
Kikuchi DS, Campos ACP, Qu H, Forrester
SJ, Pagano RL, Lassègue B, Sadikot RT, Griendling KK and Hernandes
MS: Poldip2 mediates blood-brain barrier disruption in a model of
sepsis-associated encephalopathy. J Neuroinflammation.
16:2412019.
|
|
170
|
Alhadidi Q and Shah ZA: Cofilin mediates
LPS-induced microglial cell activation and associated neurotoxicity
through activation of NF-κB and JAK-STAT pathway. Mol Neurobiol.
55:1676–1691. 2018.
|
|
171
|
Cui Y, Wu J, Jung SC, Kim GO, Kyeong Ko R,
Lee HJ, Yoo ES, Kang HK, Suk K and Eun SY: Neuroprotective effect
of methyl lucidone against microglia-mediated neurotoxicity. Eur J
Pharmacol. 690:4–12. 2012.
|
|
172
|
Li M, Wang S, Zhang C, Chi C, Liu R, Wang
T and Fu F: Escin alleviates stress-induced intestinal dysfunction
to protect brain injury by regulating the gut-brain axis in
ischemic stroke rats. Int Immunopharmacol. 115:1096592023.
|
|
173
|
Yang H, Chen Y, Yu L and Xu Y:
Esculentoside A exerts anti-inflammatory activity in microglial
cells. Int Immunopharmacol. 51:148–157. 2017.
|
|
174
|
Ge JW, Deng SJ, Xue ZW, Liu PY, Yu LJ, Li
JN, Xia SN, Gu Y, Bao XY, Lan Z, et al: Imperatorin inhibits
mitogen-activated protein kinase and nuclear factor kappa-B
signaling pathways and alleviates neuroinflammation in ischemic
stroke. CNS Neurosci Ther. 28:116–125. 2022.
|
|
175
|
Lei B, Mace B, Dawson HN, Warner DS,
Laskowitz DT and James ML: Anti-inflammatory effects of
progesterone in lipopolysaccharide-stimulated BV-2 microglia. PLoS
One. 9:e1039692014.
|
|
176
|
Jung YS, Park JH, Kim H, Kim SY, Hwang JY,
Hong KW, Bae SS, Choi BT, Lee SW and Shin HK: Probucol inhibits
LPS-induced microglia activation and ameliorates brain ischemic
injury in normal and hyperlipidemic mice. Acta Pharmacol Sin.
37:1031–1044. 2016.
|
|
177
|
Lv Y, Qian Y, Ou-Yang A and Fu L:
Hydroxysafflor yellow A attenuates neuron damage by suppressing the
lipopolysaccharide-Induced TLR4 pathway in activated microglial
cells. Cell Mol Neurobiol. 36:1241–1256. 2016.
|
|
178
|
Kim DC, Quang TH, Oh H and Kim YC:
Steppogenin isolated from cudrania tricuspidata shows
antineuroinflammatory effects via NF-κB and MAPK pathways in
LPS-stimulated BV2 and primary rat microglial cells. Molecules.
22:21302017.
|
|
179
|
Zou CG, Zhao YS, Gao SY, Li SD, Cao XZ,
Zhang M and Zhang KQ: Homocysteine promotes proliferation and
activation of microglia. Neurobiol Aging. 31:2069–2079. 2010.
|
|
180
|
Jindal A, Rajagopal S, Winter L, Miller
JW, Jacobsen DW, Brigman J, Allan AM, Paul S and Poddar R:
Hyperhomocysteinemia leads to exacerbation of ischemic brain
damage: Role of GluN2A NMDA receptors. Neurobiol Dis. 127:287–302.
2019.
|
|
181
|
Guo HH, Shen HR, Tang MZ, Sheng N, Ding X,
Lin Y, Zhang JL, Jiang JD, Gao TL, Wang LL and Han YX:
Microbiota-derived short-chain fatty acids mediate the effects of
dengzhan shengmai in ameliorating cerebral ischemia via the
gut-brain axis. J Ethnopharmacol. 306:1161582023.
|
|
182
|
Zhou Z, Xu N, Matei N, McBride DW, Ding Y,
Liang H, Tang J and Zhang JH: Sodium butyrate attenuated neuronal
apoptosis via GPR41/Gβγ/PI3K/Akt pathway after MCAO in rats. J
Cereb Blood Flow Metab. 41:267–281. 2021.
|
|
183
|
Xu S, Wang J, Jiang J, Song J, Zhu W,
Zhang F, Shao M, Xu H, Ma X and Lyu F: TLR4 promotes microglial
pyroptosis via lncRNA-F630028O10Rik by activating PI3K/AKT pathway
after spinal cord injury. Cell Death Dis. 11:6932020.
|