|
1
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Park EH, Jung KW, Park NJ, Kang MJ, Yun
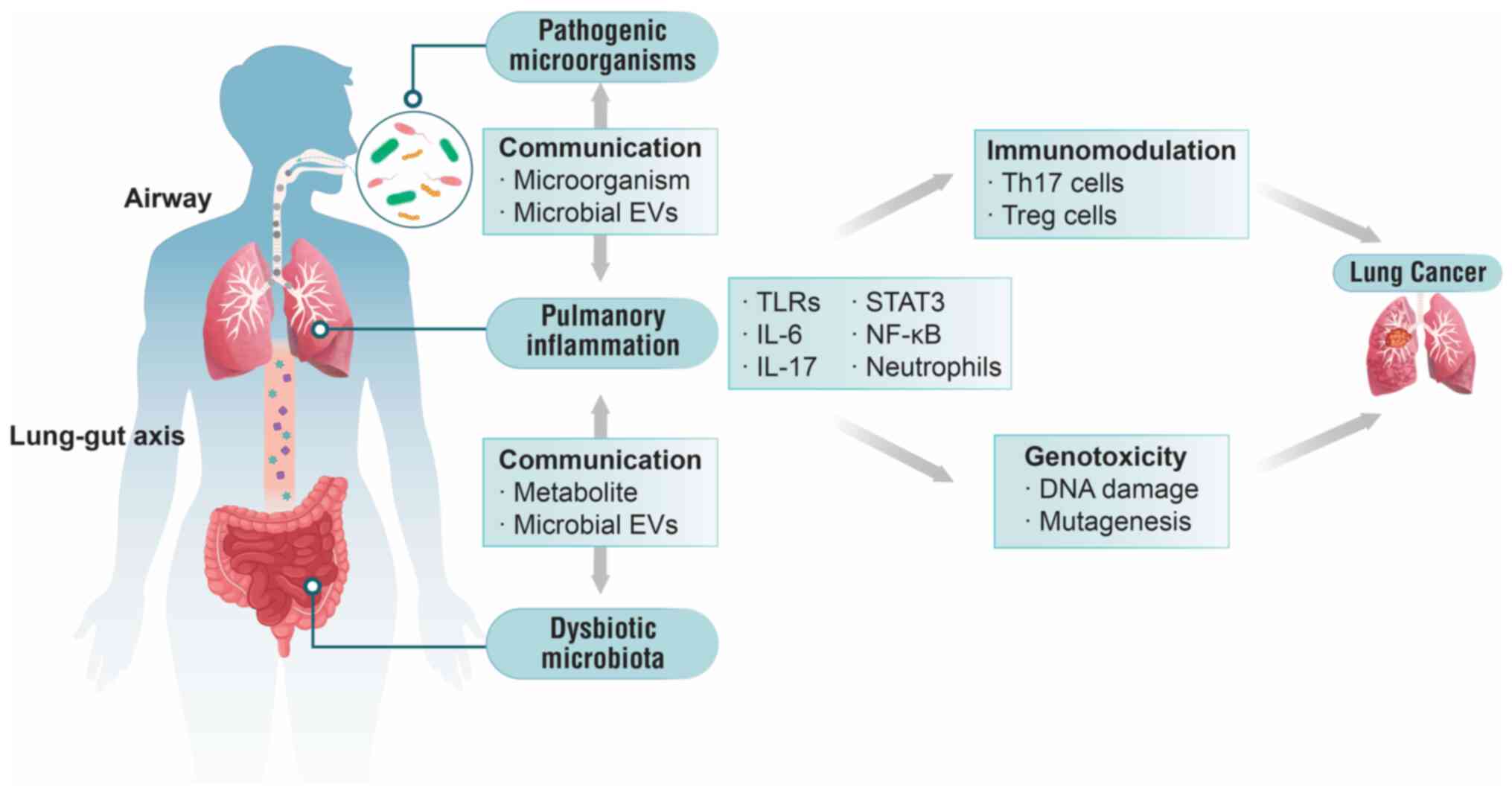
EH, Kim HJ, Kim JE, Kong HJ, Im JS and Seo HG; Community of
Population-Based Regional Cancer Registries: Cancer statistics in
Korea: Incidence, Mortality, survival, and prevalence in 2021.
Cancer Res Treat. 56:357–371. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zito Marino F, Bianco R, Accardo M, Ronchi
A, Cozzolino I, Morgillo F, Rossi G and Franco R: Molecular
heterogeneity in lung cancer: from mechanisms of origin to clinical
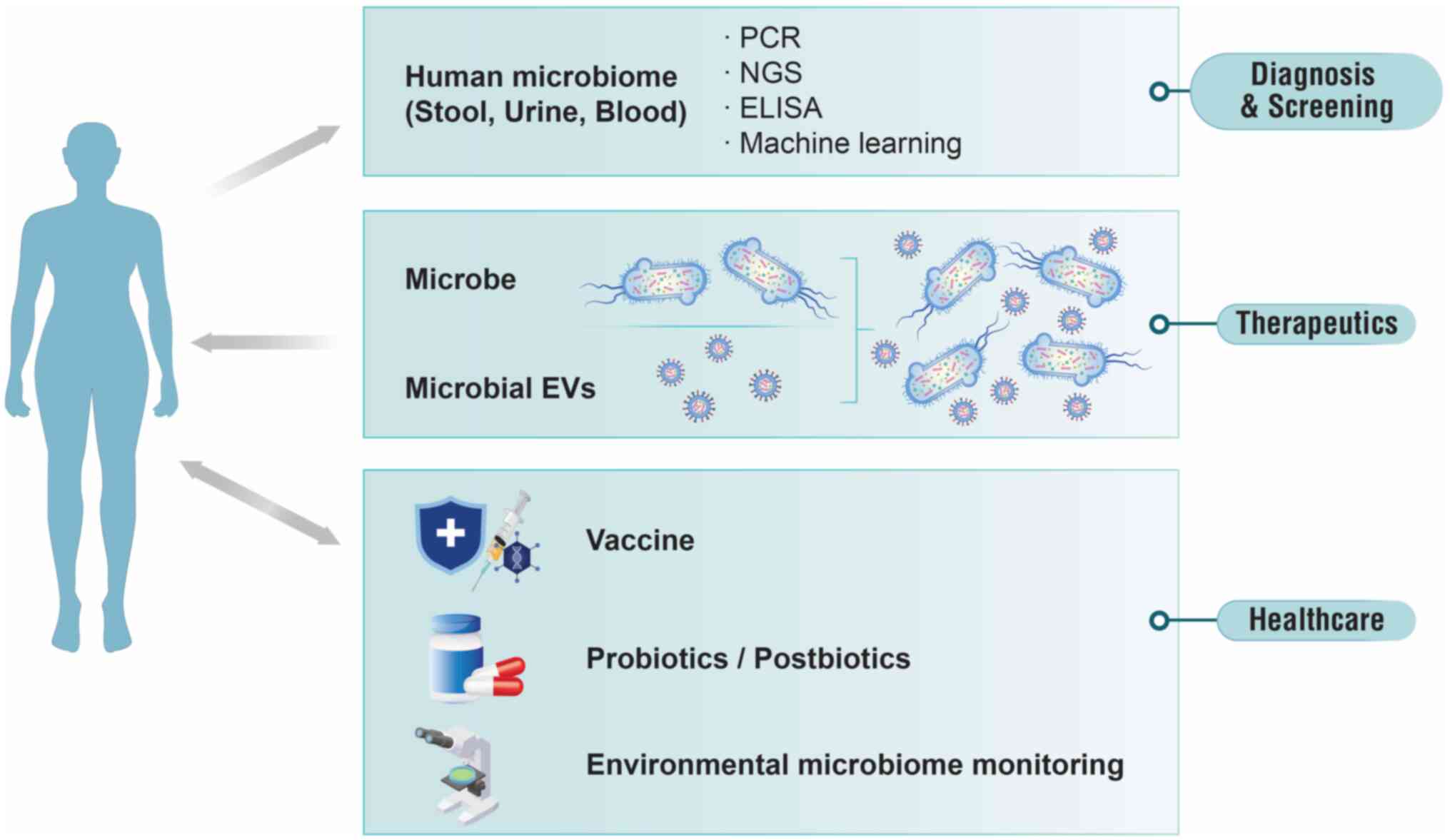
implications. Int J Med Sci. 16:981–989. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
de Sousa VML and Carvalho L: Heterogeneity
in lung cancer. Pathobiology. 85:96–107. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
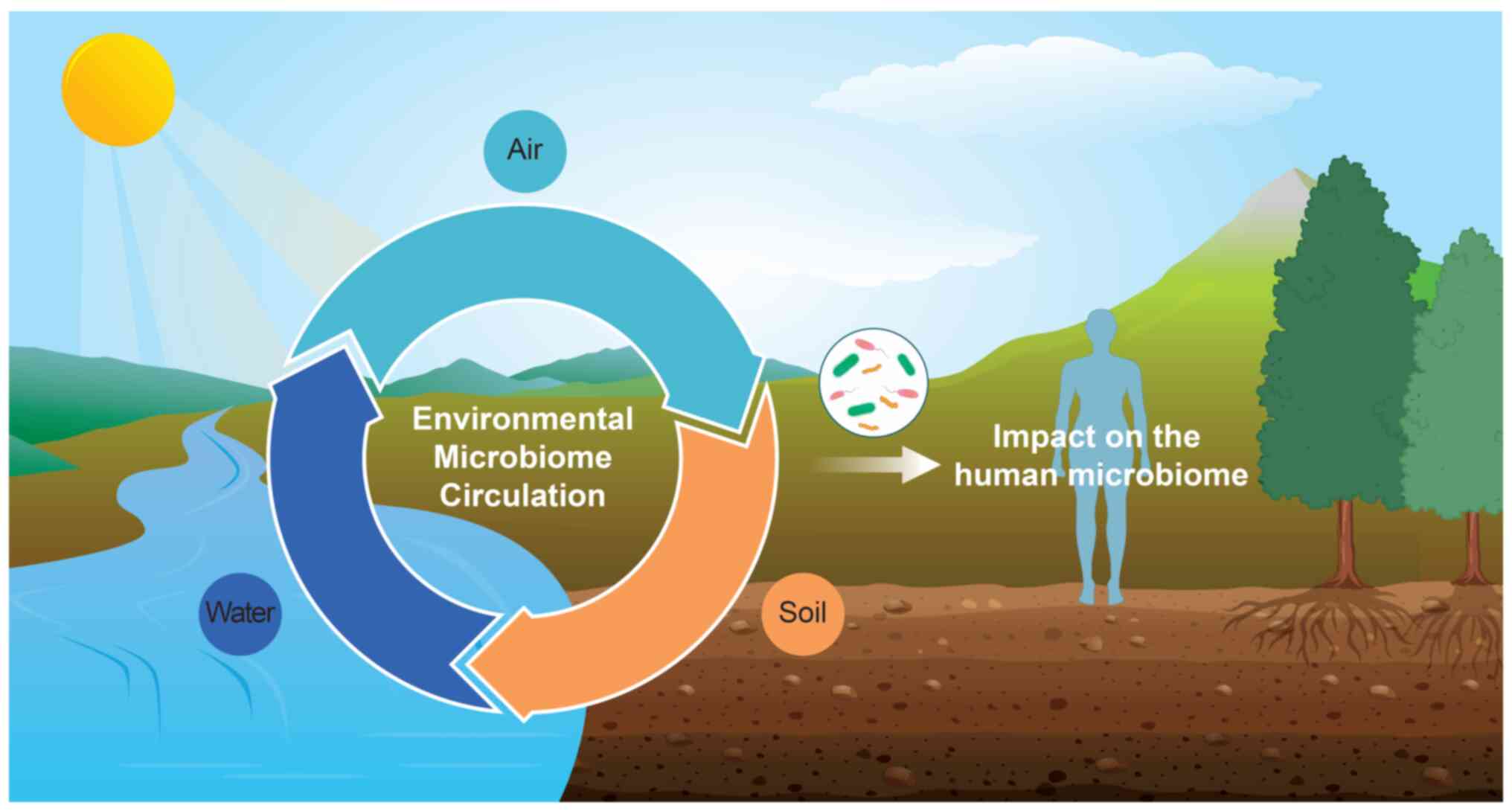
5
|
Lim ZF and Ma PC: Emerging insights of
tumor heterogeneity and drug resistance mechanisms in lung cancer
targeted therapy. J Hematol Oncol. 12:1342019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Malhotra J, Malvezzi M, Negri E, La
Vecchia C and Boffetta P: Risk factors for lung cancer worldwide.
Eur Respir J. 48:889–902. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rahman MM, Islam MR, Shohag S, Ahasan MT,
Sarkar N, Khan H, Hasan AM, Cavalu S and Rauf A: Microbiome in
cancer: Role in carcinogenesis and impact in therapeutic
strategies. Biomed Pharmacother. 149:1128982022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dickson RP, Erb-Downward JR, Freeman CM,
McCloskey L, Beck JM, Huffnagle GB and Curtis JL: Spatial variation
in the healthy human lung microbiome and the adapted Island model
of lung biogeography. Ann Am Thorac Soc. 12:821–830. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yu G, Gail MH, Consonni D, Carugno M,
Humphrys M, Pesatori AC, Caporaso NE, Goedert JJ, Ravel J and Landi
MT: Characterizing human lung tissue microbiota and its
relationship to epidemiological and clinical features. Genome Biol.
17:1632016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yagi K, Huffnagle GB, Lukacs NW and Asai
N: The lung microbiome during health and disease. Int J Mol Sci.
22:108722021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ruan R, Deng X, Dong X, Wang Q, Lv X and
Si C: Microbiota emergencies in the diagnosis of lung diseases: A
meta-analysis. Front Cell Infect Microbiol. 11:7096342021.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jang HJ, Choi JY, Kim K, Yong SH, Kim YW,
Kim SY, Kim EY, Jung JY, Kang YA, Park MS, et al: Relationship of
the lung microbiome with PD-L1 expression and immunotherapy
response in lung cancer. Respir Res. 22:3222021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yang D, Xing Y, Song X and Qian Y: The
impact of lung microbiota dysbiosis on inflammation. Immunology.
159:156–166. 2020. View Article : Google Scholar :
|
|
14
|
Xu N, Wang L, Li C, Ding C, Li C, Fan W,
Cheng C and Gu B: Microbiota dysbiosis in lung cancer: Evidence of
association and potential mechanisms. Transl Lung Cancer Res.
9:1554–1568. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hosgood HD III, Sapkota AR, Rothman N,
Rohan T, Hu W, Xu J, Vermeulen R, He X, White JR, Wu G, et al: The
potential role of lung microbiota in lung cancer attributed to
household coal burning exposures. Environ Mol Mutagen. 55:643–651.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Liu HX, Tao LL, Zhang J, Zhu YG, Zheng Y,
Liu D, Zhou M, Ke H, Shi MM and Qu JM: Difference of lower airway
microbiome in bilateral protected specimen brush between lung
cancer patients with unilateral lobar masses and control subjects.
Int J Cancer. 142:769–778. 2018. View Article : Google Scholar
|
|
17
|
Zhang W, Luo J, Dong X, Zhao S, Hao Y,
Peng C, Shi H, Zhou Y, Shan L, Sun Q, et al: Salivary microbial
dysbiosis is associated with systemic inflammatory markers and
predicted oral metabolites in non-small cell lung cancer patients.
J Cancer. 10:1651–1662. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang M, Zhou H, Xu S, Liu D, Cheng Y, Gao
B, Li X and Chen J: The gut microbiome can be used to predict the
gastrointestinal response and efficacy of lung cancer patients
undergoing chemotherapy. Ann Palliat Med. 9:4211–4227. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lu H, Gao NL, Tong F, Wang J, Li H, Zhang
R, Ma H, Yang N, Zhang Y, Wang Y, et al: Alterations of the human
lung and gut microbiomes in non-small cell lung carcinomas and
distant metastasis. Microbiol Spectr. 9:e00802212021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shen W, Tang D, Deng Y, Li H, Wang T, Wan
P and Liu R: Association of gut microbiomes with lung and
esophageal cancer: A pilot study. World J Microbiol Biotechnol.
37:1282021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhuang H, Cheng L, Wang Y, Zhang YK, Zhao
MF, Liang GD, Zhang MC, Li YG, Zhao JB, Gao YN, et al: Dysbiosis of
the gut microbiome in lung cancer. Front Cell Infect Microbiol.
9:1122019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zheng Y, Fang Z, Xue Y, Zhang J, Zhu J,
Gao R, Yao S, Ye Y, Wang S, Lin C, et al: Specific gut microbiome
signature predicts the early-stage lung cancer. Gut Microbes.
11:1030–1042. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee SH, Sung JY, Yong D, Chun J, Kim SY,
Song JH, Chung KS, Kim EY, Jung JY, Kang YA, et al:
Characterization of microbiome in bronchoalveolar lavage fluid of
patients with lung cancer comparing with benign mass like lesions.
Lung Cancer. 102:89–95. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yang J, Shin TS, Kim JS, Jee YK and Kim
YK: A new horizon of precision medicine: Combination of the
microbiome and extracellular vesicles. Exp Mol Med. 54:466–482.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Castelino M, Eyre S, Moat J, Fox G, Martin
P, Ho P, Upton M and Barton A: Optimisation of methods for
bacterial skin microbiome investigation: Primer selection and
comparison of the 454 versus MiSeq platform. BMC Microbiol.
17:232017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Balvočiūtė M and Huson DH: SILVA, RDP,
Greengenes, NCBI and OTT-how do these taxonomies compare? BMC
Genomics. 18(Suppl 2): S1142017. View Article : Google Scholar
|
|
27
|
Rajagopala SV, Vashee S, Oldfield LM,
Suzuki Y, Venter JC, Telenti A and Nelson KE: The human microbiome
and cancer. Cancer Prev Res (Phila). 10:226–234. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Russo E, Taddei A, Ringressi MN, Ricci F
and Amedei A: The interplay between the microbiome and the adaptive
immune response in cancer development. Therap Adv Gastroenterol.
9:594–605. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Choi Y, Park H, Park HS and Kim YK:
Extracellular vesicles, a key mediator to link environmental
microbiota to airway immunity. Allergy Asthma Immunol Res.
9:101–106. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Karimi K, Inman MD, Bienenstock J and
Forsythe P: Lactobacillus reuteri-induced regulatory T cells
protect against an allergic airway response in mice. Am J Respir
Crit Care Med. 179:186–193. 2009. View Article : Google Scholar
|
|
31
|
Atarashi K, Tanoue T, Shima T, Imaoka A,
Kuwahara T, Momose Y, Cheng G, Yamasaki S, Saito T, Ohba Y, et al:
Induction of colonic regulatory T cells by indigenous Clostridium
species. Science. 331:337–341. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yang J, Seo JH, Jee YK, Kim YK and Sohn
JR: Composition analysis of airborne microbiota in outdoor and
indoor based on dust separated by micro-sized and nano-sized.
Aerosol Air Qual Res. 23:2102312023. View Article : Google Scholar
|
|
33
|
Panthee B, Gyawali S, Panthee P and
Techato K: Environmental and human microbiome for health. Life
(Basel). 12:4562022.PubMed/NCBI
|
|
34
|
Mbareche H, Morawska L and Duchaine C: On
the interpretation of bioaerosol exposure measurements and impacts
on health. J Air Waste Manag Assoc. 69:789–804. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Shin SK, Kim J, Ha SM, Oh HS, Chun J, Sohn
J and Yi H: Metagenomic insights into the bioaerosols in the indoor
and outdoor environments of childcare facilities. PLoS One.
10:e01269602015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wolf M and Lai PS: Indoor microbial
exposures and chronic lung disease: From microbial toxins to the
microbiome. Clin Chest Med. 41:777–796. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Park KS, Lee J, Jang SC, Kim SR, Jang MH,
Lötvall J, Kim YK and Gho YS: Pulmonary inflammation induced by
bacteria-free outer membrane vesicles from Pseudomonas aeruginosa.
Am J Respir Cell Mol Biol. 49:637–645. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kim KH, Kabir E and Jahan SA: Airborne
bioaerosols and their impact on human health. J Environ Sci
(China). 67:23–35. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Baldacci S, Maio S, Cerrai S, Sarno G,
Baïz N, Simoni M, Annesi-Maesano I and Viegi G; HEALS Study:
Allergy and asthma: Effects of the exposure to particulate matter
and biological allergens. Respir Med. 109:1089–1104. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hayleeyesus SF, Ejeso A and Derseh FA:
Quantitative assessment of bio-aerosols contamination in indoor air
of University dormitory rooms. Int J Health Sci (Qassim).
9:249–256. 2015.PubMed/NCBI
|
|
41
|
Lee EY, Bang JY, Park GW, Choi DS, Kang
JS, Kim HJ, Park KS, Lee JO, Kim YK, Kwon KH, et al: Global
proteomic profiling of native outer membrane vesicles derived from
Escherichia coli. Proteomics. 7:3143–3153. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Lee EY, Choi DY, Kim DK, Kim JW, Park JO,
Kim S, Kim SH, Desiderio DM, Kim YK, Kim KP and Gho YS:
Gram-positive bacteria produce membrane vesicles: Proteomics-based
characterization of Staphylococcus aureus-derived membrane
vesicles. Proteomics. 9:5425–5436. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Choi Y, Kwon Y, Kim DK, Jeon J, Jang SC,
Wang T, Ban M, Kim MH, Jeon SG, Kim MS, et al: Gut microbe-derived
extracellular vesicles induce insulin resistance, thereby impairing
glucose metabolism in skeletal muscle. Sci Rep. 5:158782015.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Conlon MA and Bird AR: The impact of diet
and lifestyle on gut microbiota and human health. Nutrients.
7:17–44. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Yang J, Moon HE, Park HW, McDowell A, Shin
TS, Jee YK, Kym S, Paek SH and Kim YK: Brain tumor diagnostic model
and dietary effect based on extracellular vesicle microbiome data
in serum. Exp Mol Med. 52:1602–1613. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yang J, McDowell A, Kim EK, Seo H, Yum K,
Lee WH, Jee YK and Kim YK: Consumption of a Leuconostoc
holzapfelii-enriched synbiotic beverage alters the composition of
the microbiota and microbial extracellular vesicles. Exp Mol Med.
51:1–11. 2019.
|
|
47
|
Son T, Cho YJ, Lee H, Cho MY, Goh B, Kim
HM, Hoa PTN, Cho SH, Park YJ, Park HS and Hong KS: Monitoring in
vivo behavior of size-dependent fluorescent particles as a model
fine dust. J Nanobiotechnology. 20:2272022. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kim YS, Choi EJ, Lee WH, Choi SJ, Roh TY,
Park J, Jee YK, Zhu Z, Koh YY, Gho YS and Kim YK: Extracellular
vesicles, especially derived from Gram-negative bacteria, in indoor
dust induce neutrophilic pulmonary inflammation associated with
both Th1 and Th17 cell responses. Clin Exp Allergy. 43:443–454.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Kim YS, Choi JP, Kim MH, Park HK, Yang S,
Kim YS, Kim TB, Cho YS, Oh YM, Jee YK, et al: IgG sensitization to
extracellular vesicles in indoor dust is closely associated with
the prevalence of non-eosinophilic asthma, COPD, and lung cancer.
Allergy Asthma Immunol Res. 8:198–205. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Yang J, Hong G, Kim YS, Seo H, Kim S,
McDowell A, Lee WH, Kim YS, Oh YM, Cho YS, et al: Lung disease
diagnostic model through IgG sensitization to microbial
extracellular vesicles. Allergy Asthma Immunol Res. 12:669–683.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Raposo G and Stoorvogel W: Extracellular
vesicles: Exosomes, microvesicles, and friends. J Cell Biol.
200:373–383. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Colombo M, Raposo G and Théry C:
Biogenesis, secretion, and intercellular interactions of exosomes
and other extracellular vesicles. Ann Rev Cell Dev Biol.
30:255–289. 2014. View Article : Google Scholar
|
|
53
|
Mishra S, Tejesvi MV, Hekkala J, Turunen
J, Kandikanti N, Kaisanlahti A, Suokas M, Leppä S, Vihinen P,
Kuitunen H, et al: Gut microbiome-derived bacterial extracellular
vesicles in patients with solid tumours. J Adv Res. 68:375–386.
2025. View Article : Google Scholar :
|
|
54
|
Yang J, Kim EK, Park HJ, McDowell A and
Kim YK: The impact of bacteria-derived ultrafine dust particles on
pulmonary diseases. Exp Mol Med. 52:338–347. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kim YS, Lee WH, Choi EJ, Choi JP, Heo YJ,
Gho YS, Jee YK, Oh YM and Kim YK: Extracellular vesicles derived
from gram-negative bacteria, such as Escherichia coli, induce
emphysema mainly via IL-17A-mediated neutrophilic inflammation. J
Immunol. 194:3361–3368. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Park KS, Choi KH, Kim YS, Hong BS, Kim OY,
Kim JH, Yoon CM, Koh GY, Kim YK and Gho YS: Outer membrane vesicles
derived from Escherichia coli induce systemic inflammatory response
syndrome. PLoS One. 5:e113342010. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Lundin JI and Checkoway H: Endotoxin and
cancer. Environ Health Perspect. 117:1344–1350. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Kim MR, Hong SW, Choi EB, Lee WH, Kim YS,
Jeon SG, Jang MH, Gho YS and Kim YK: Staphylococcus aureus-derived
extracellular vesicles induce neutrophilic pulmonary inflammation
via both Th1 and Th17 cell responses. Allergy. 67:1271–1281. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Jun SH, Lee JH, Kim BR, Kim SI, Park TI,
Lee JC and Lee YC: Acinetobacter baumannii outer membrane vesicles
elicit a potent innate immune response via membrane proteins. PLoS
One. 8:e717512013. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Jafari B, Khavari Nejad RA, Vaziri F and
Siadat SD: Evaluation of the effects of extracellular vesicles
derived from Faecalibacterium prausnitzii on lung cancer cell line.
Biologia. 74:889–898. 2019. View Article : Google Scholar
|
|
61
|
Yang J: Insight into the potential of
algorithms using AI technology as in vitro diagnostics utilizing
microbial extracellular vesicles. Mol Cell Probes. 78:1019922024.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Yang J, Kim EK, McDowell A and Kim YK:
Microbe-derived extracellular vesicles as a smart drug delivery
system. Transl Clin Pharmacol. 26:103–110. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Whitaker K: Earlier diagnosis: The
importance of cancer symptoms. Lancet Oncol. 21:6–8. 2020.
View Article : Google Scholar
|
|
64
|
Seo JH, Lee JW and Cho D: The market trend
analysis and prospects of cancer molecular diagnostics kits.
Biomater Res. 22:22018. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Yang J, McDowell A, Kim EK, Seo H, Lee WH,
Moon CM, Kym SM, Lee DH, Park YS, Jee YK and Kim YK: Development of
a colorectal cancer diagnostic model and dietary risk assessment
through gut microbiome analysis. Exp Mol Med. 51:1–15. 2019.
|
|
66
|
Yang J, Li D, Yang Z, Dai W, Feng X, Liu
Y, Jiang Y, Li P, Li Y, Tang B, et al: Establishing high-accuracy
biomarkers for colorectal cancer by comparing fecal microbiomes in
patients with healthy families. Gut Microbes. 11:918–929. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Kim G, Park C, Yoon YK, Park D, Lee JE,
Lee D, Sun P, Park S, Yun C, Kang DH and Chung C: Prediction of
lung cancer using novel biomarkers based on microbiome profiling of
bronchoalveolar lavage fluid. Sci Rep. 14:16912024. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
McDowell A, Kang J, Yang J, Jung J, Oh YM,
Kym SM, Shin TS, Kim TB, Jee YK and Kim YK: Machine-learning
algorithms for asthma, COPD, and lung cancer risk assessment using
circulating microbial extracellular vesicle data and their
application to assess dietary effects. Exp Mol Med. 54:1586–1595.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Kim DJ, Yang J, Seo H, Lee WH, Ho Lee D,
Kym S, Park YS, Kim JG, Jang IJ, Kim YK and Cho JY: Colorectal
cancer diagnostic model utilizing metagenomic and metabolomic data
of stool microbial extracellular vesicles. Sci Rep. 10:28602020.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Cho EJ, Leem S, Kim SA, Yang J, Lee YB,
Kim SS, Cheong JY, Cho SW, Kim JW, Kim SM, et al: Circulating
microbiota-based metagenomic signature for detection of
hepatocellular carcinoma. Sci Rep. 9:75362019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Park JY, Kang CS, Seo HC, Shin JC, Kym SM,
Park YS, Shin TS, Kim JG and Kim YK: Bacteria-derived extracellular
vesicles in urine as a novel biomarker for gastric cancer:
Integration of liquid biopsy and metagenome analysis. Cancers
(Basel). 13:46872021. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Kim JR, Han K, Han Y, Kang N, Shin TS,
Park HJ, Kim H, Kwon W, Lee S, Kim YK, et al: Microbiome markers of
pancreatic cancer based on bacteria-derived extracellular vesicles
acquired from blood samples: A retrospective propensity score
matching analysis. Biology (Basel). 10:2192021. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Kim SI, Kang N, Leem S, Yang J, Jo H, Lee
M, Kim HS, Dhanasekaran DN, Kim YK, Park T and Song YS: Metagenomic
analysis of serum microbe-derived extracellular vesicles and
diagnostic models to differentiate ovarian cancer and benign
ovarian tumor. Cancers (Basel). 12:13092020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Ağagündüz D, Gençer Bingöl F, Çelik E,
Cemali Ö, Özenir Ç, Özoğul F and Capasso R: Recent developments in
the probiotics as live biotherapeutic products (LBPs) as modulators
of gut brain axis related neurological conditions. J Transl Med.
20:4602022. View Article : Google Scholar :
|
|
75
|
Cordaillat-Simmons M, Rouanet A and Pot B:
Live biotherapeutic products: The importance of a defined
regulatory framework. Exp Mol Med. 52:1397–1406. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Lee NK, Han KJ, Son SH, Eom SJ, Lee SK and
Paik HD: Multifunctional effect of probiotic Lactococcus lactis
KC24 isolated from kimchi. LWT Food Sci Technol. 64:1036–1041.
2015. View Article : Google Scholar
|
|
77
|
Han KJ, Lee NK, Park H and Paik HD:
Anticancer and anti-inflammatory activity of probiotic Lactococcus
lactis NK34. J Microbiol Biotechnol. 25:1697–1701. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Peymaeei F, Sadeghi F, Safari E, Khorrami
S, Falahati M, Roudbar Mohammadi S and Roudbary M: Candida albicans
beta-glucan induce anti-cancer activity of mesenchymal stem cells
against lung cancer cell line: An in-vitro experimental study.
Asian Pac J Cancer Prev. 21:837–843. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Albeituni SH, Ding C, Liu M, Hu X, Luo F,
Kloecker G, Bousamra M II, Zhang HG and Yan J: Yeast-derived
particulate β-glucan treatment subverts the suppression of
myeloid-derived suppressor cells (MDSC) by inducing
polymorphonuclear MDSC apoptosis and monocytic MDSC differentiation
to APC in cancer. J Immunol. 196:2167–2180. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Kim K, Kwon O, Ryu TY, Jung CR, Kim J, Min
JK, Kim DS, Son MY and Cho HS: Propionate of a microbiota
metabolite induces cell apoptosis and cell cycle arrest in lung
cancer. Mol Med Rep. 20:1569–1574. 2019.PubMed/NCBI
|
|
81
|
Kotzampassi K, Stavrou G, Damoraki G,
Georgitsi M, Basdanis G, Tsaousi G and Giamarellos-Bourboulis EJ: A
four-probiotics regimen reduces postoperative complications after
colorectal surgery: A randomized, double-blind, placebo-controlled
study. World J Surg. 39:2776–2783. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Wada M, Nagata S, Saito M, Shimizu T,
Yamashiro Y, Matsuki T, Asahara T and Nomoto K: Effects of the
enteral administration of Bifidobacterium breve on patients
undergoing chemotherapy for pediatric malignancies. Support Care
Cancer. 18:751–759. 2010. View Article : Google Scholar
|
|
83
|
Gui QF, Lu HF, Zhang CX, Xu ZR and Yang
YH: Well-balanced commensal microbiota contributes to anti-cancer
response in a lung cancer mouse model. Genet Mol Res. 14:5642–5651.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Zhou X, Xie F, Wang L, Zhang L, Zhang S,
Fang M and Zhou F: The function and clinical application of
extracellular vesicles in innate immune regulation. Cell Mol
Immunol. 17:323–334. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Choi JH, Moon CM, Shin TS, Kim EK,
McDowell A, Jo MK, Joo YH, Kim SE, Jung HK, Shim KN, et al:
Lactobacillus paracasei-derived extracellular vesicles attenuate
the intestinal inflammatory response by augmenting the endoplasmic
reticulum stress pathway. Exp Mol Med. 52:423–437. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Lee DH, Park HK, Lee HR, Sohn H, Sim S,
Park HJ, Shin YS, Kim YK, Choi Y and Park HS: Immunoregulatory
effects of Lactococcus lactis-derived extracellular vesicles in
allergic asthma. Clin Transl Allergy. 12:e121382022. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Sim S, Lee DH, Kim KS, Park HJ, Kim YK,
Choi Y and Park HS: Micrococcus luteus-derived extracellular
vesicles attenuate neutrophilic asthma by regulating miRNAs in
airway epithelial cells. Exp Mol Med. 55:196–204. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Kim MH, Choi SJ, Choi HI, Choi JP, Park
HK, Kim EK, Kim MJ, Moon BS, Min TK, Rho M, et al: Lactobacillus
plantarum-derived extracellular vesicles protect atopic dermatitis
induced by Staphylococcus aureus-derived extracellular vesicles.
Allergy Asthma Immunol Res. 10:516–532. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Kim JH, Jeun EJ, Hong CP, Kim SH, Jang MS,
Lee EJ, Moon SJ, Yun CH, Im SH, Jeong SG, et al: Extracellular
vesicle-derived protein from Bifidobacterium longum alleviates food
allergy through mast cell suppression. J Allergy Clin Immunol.
137:507–516.e8. 2016. View Article : Google Scholar
|
|
90
|
Chen J, Zhang H, Wang S, Du Y, Wei B, Wu Q
and Wang H: Inhibitors of bacterial extracellular vesicles. Front
Microbiol. 13:8350582022. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Guo H, Zhao L, Zhu J, Chen P, Wang H,
Jiang M, Liu X, Sun H, Zhao W, Zheng Z, et al: Microbes in lung
cancer initiation, treatment, and outcome: Boon or bane? Semin
Cancer Biol. 86:1190–1206. 2022. View Article : Google Scholar
|
|
92
|
Kim SI, Ha JY, Choi SY, Hong SH and Lee
HJ: Use of bacterial extracellular vesicles for gene delivery to
host cells. Biomolecules. 12:11712022. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Liu H, Zhang Q, Wang S, Weng W, Jing Y and
Su J: Bacterial extracellular vesicles as bioactive nanocarriers
for drug delivery: Advances and perspectives. Bioact Mater.
14:169–181. 2021.
|
|
94
|
Lee EY, Choi DS, Kim KP and Gho YS:
Proteomics in gram-negative bacterial outer membrane vesicles. Mass
Spectrom Rev. 27:535–555. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Papahadjopoulos D, Poste G, Schaeffer BE
and Vail WJ: Membrane fusion and molecular segregation in
phospholipid vesicles. Biochim Biophys Acta. 352:10–28. 1974.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Papahadjopoulos D, Mayhew E, Poste G,
Smith S and Vail WJ: Incorporation of lipid vesicles by mammalian
cells provides a potential method for modifying cell behaviour.
Nature. 252:163–166. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Poste G and Papahadjopoulos D: Lipid
vesicles as carriers for introducing materials into cultured cells:
Influence of vesicle lipid composition on mechanism(s) of vesicle
incorporation into cells. Proc Natl Acad Sci USA. 73:1603–1607.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Casal JI, Rueda P and Hurtado A:
Parvovirus-like particles as vaccine vectors. Methods. 19:174–186.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Parmar MM, Edwards K and Madden TD:
Incorporation of bacterial membrane proteins into liposomes:
Factors influencing protein reconstitution. Biochim Biophys Acta.
1421:77–90. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Kim SH, Kim KS, Lee SR, Kim E, Kim MS, Lee
EY, Gho YS, Kim JW, Bishop RE and Chang KT: Structural
modifications of outer membrane vesicles to refine them as vaccine
delivery vehicles. Biochim Biophys Acta. 1788:2150–2159. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Goldin BR and Gorbach SL: Effect of
Lactobacillus acidophilus dietary supplements on
1,2-dimethylhydrazine dihydrochloride-induced intestinal cancer in
rats. J Natl Cancer Inst. 64:263–265. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Ghoneum M and Gimzewski J: Apoptotic
effect of a novel kefir product, PFT, on multidrug-resistant
myeloid leukemia cells via a hole-piercing mechanism. Int J Oncol.
44:830–837. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Thirabunyanon M and Hongwittayakorn P:
Potential probiotic lactic acid bacteria of human origin induce
antiproliferation of colon cancer cells via synergic actions in
adhesion to cancer cells and short-chain fatty acid bioproduction.
Appl Biochem Biotechnol. 169:511–525. 2013. View Article : Google Scholar
|
|
104
|
Orlando A, Refolo MG, Messa C, Amati L,
Lavermicocca P, Guerra V and Russo F: Antiproliferative and
proapoptotic effects of viable or heat-killed Lactobacillus
paracasei IMPC2.1 and Lactobacillus rhamnosus GG in HGC-27 gastric
and DLD-1 colon cell lines. Nutr Cancer. 64:1103–1111. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Baldwin C, Millette M, Oth D, Ruiz MT,
Luquet FM and Lacroix M: Probiotic Lactobacillus acidophilus and L.
casei mix sensitize colorectal tumoral cells to
5-fluorouracil-induced apoptosis. Nutr Cancer. 62:371–378. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Kim Y, Lee D, Kim D, Cho J, Yang J, Chung
M, Kim K and Ha N: Inhibition of proliferation in colon cancer cell
lines and harmful enzyme activity of colon bacteria by
Bifidobacterium adolescentis SPM0212. Arch Pharm Res. 31:468–473.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Park E, Jeon GI, Park JS and Paik HD: A
probiotic strain of Bacillus polyfermenticus reduces DMH induced
precancerous lesions in F344 male rat. Biol Pharm Bull. 30:569–574.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Ma EL, Choi YJ, Choi J, Pothoulakis C,
Rhee SH and Im E: The anticancer effect of probiotic Bacillus
polyfermenticus on human colon cancer cells is mediated through
ErbB2 and ErbB3 inhibition. Int J Cancer. 127:780–790. 2010.
View Article : Google Scholar
|
|
109
|
Gamallat Y, Meyiah A, Kuugbee ED, Hago AM,
Chiwala G, Awadasseid A, Bamba D, Zhang X, Shang X, Luo F and Xin
Y: Lactobacillus rhamnosus induced epithelial cell apoptosis,
ameliorates inflammation and prevents colon cancer development in
an animal model. Biomed Pharmacother. 83:536–541. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Hu J, Wang C, Ye L, Yang W, Huang H, Meng
F, Shi S and Ding Z: Anti-tumour immune effect of oral
administration of Lactobacillus plantarum to CT26 tumour-bearing
mice. J Biosci. 40:269–279. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Walia S, Kamal R, Dhawan DK and Kanwar SS:
Chemoprevention by probiotics during 1,2-dimethylhydrazine-induced
colon carcinogenesis in rats. Dig Dis Sci. 63:900–909. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Jacouton E, Torres Maravilla E, Boucard
AS, Pouderous N, Pessoa Vilela AP, Naas I, Chain F, Azevedo V,
Langella P and Bermúdez-Humarán LG: Anti-tumoral effects of
recombinant Lactococcus lactis strain secreting IL-17A cytokine.
Front Microbiol. 9:33552019. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Aguilar-Toalá JE, Garcia-Varela R, Garcia
HS, Mata-Haro V, González-Córdova AF, Vallejo-Cordoba B and
Hernández-Mendoza A: Postbiotics: An evolving term within the
functional foods field. Trends Food Sci Technol. 75:105–114. 2018.
View Article : Google Scholar
|
|
114
|
Fafián-Labora JA and O'Loghlen A:
Classical and nonclassical intercellular communication in
senescence and ageing. Trends Cell Biol. 30:628–639. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Liu Y, Defourny KAY, Smid EJ and Abee T:
Gram-positive bacterial extracellular vesicles and their impact on
health and disease. Front Microbiol. 9:15022018. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Kang CS, Ban M, Choi EJ, Moon HG, Jeon JS,
Kim DK, Park SK, Jeon SG, Roh TY, Myung SJ, et al: Extracellular
vesicles derived from gut microbiota, especially Akkermansia
muciniphila, protect the progression of dextran sulfate
sodium-induced colitis. PLoS One. 8:e765202013. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Kim YJ, Lee BG, Shim JE, Lee H, Park JH
and Yeo MK: Airborne bacteria in institutional and commercial
buildings in Korea: Characterization with 16S rRNA gene sequencing
and association with environmental conditions. Aerosol Sci Technol.
58:1281–1292. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Fahlgren C, Hagström Å, Nilsson D and
Zweifel UL: Annual variations in the diversity, viability, and
origin of airborne bacteria. Appl Environ Microbiol. 76:3015–3025.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Cho YS, Kim HR, Ko HS, Jeong SB, Chan Kim
B and Jung JH: Continuous surveillance of bioaerosols on-site using
an automated bioaerosol-monitoring system. ACS Sens. 5:395–403.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Gerdes L, Iwobi A, Busch U and Pecoraro S:
Optimization of digital droplet polymerase chain reaction for
quantification of genetically modified organisms. Biomol Detect
Quantif. 7:9–20. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Biron VL, Kostiuk M, Isaac A, Puttagunta
L, O'Connell DA, Harris J, Côté DW and Seikaly H: Detection of
human papillomavirus type 16 in oropharyngeal squamous cell
carcinoma using droplet digital polymerase chain reaction. Cancer.
122:1544–1551. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Brambati C, Galbiati S, Xue E, Toffalori
C, Crucitti L, Greco R, Sala E, Crippa A, Chiesa L, Soriani N, et
al: Droplet digital polymerase chain reaction for DNMT3A and IDH1/2
mutations to improve early detection of acute myeloid leukemia
relapse after allogeneic hematopoietic stem cell transplantation.
Haematologica. 101:e157–e161. 2016. View Article : Google Scholar :
|
|
123
|
Patterson B, Morrow C, Singh V, Moosa A,
Gqada M, Woodward J, Mizrahi V, Bryden W, Call C, Patel S, et al:
Detection of Mycobacterium tuberculosis bacilli in bio-aerosols
from untreated TB patients. Gates Open Res. 1:112018. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Lu X, Xiong L, Zheng X, Yu Q, Xiao Y and
Xie Y: Structure of gut microbiota and characteristics of fecal
metabolites in patients with lung cancer. Front Cell Infect
Microbiol. 13:11703262023. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Najafi S, Abedini F, Azimzadeh Jamalkandi
S, Shariati P, Ahmadi A and Gholami Fesharaki M: The composition of
lung microbiome in lung cancer: A systematic review and
meta-analysis. BMC Microbiol. 21:3152021. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Greathouse KL, White JR, Vargas AJ,
Bliskovsky VV, Beck JA, von Muhlinen N, Polley EC, Bowman ED, Khan
MA, Robles AI, et al: Interaction between the microbiome and TP53
in human lung cancer. Genome Biol. 19:1232018. View Article : Google Scholar : PubMed/NCBI
|