|
1
|
Singer M, Deutschman CS, Seymour CW,
Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche
JD, Coopersmith CM, et al: The third international consensus
definitions for sepsis and septic shock (Sepsis-3). JAMA.
315:801–810. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rudd KE, Johnson SC, Agesa KM, Shackelford
KA, Tsoi D, Kievlan DR, Colombara DV, Ikuta KS, Kissoon N, Finfer
S, et al: Global, regional, and national sepsis incidence and
mortality, 1990-2017: Analysis for the Global Burden of Disease
Study. Lancet. 395:200–211. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fleischmann C, Scherag A, Adhikari NK,
Hartog CS, Tsaganos T, Schlattmann P, Angus DC and Reinhart K;
International Forum of Acute Care Trialists: Assessment of global
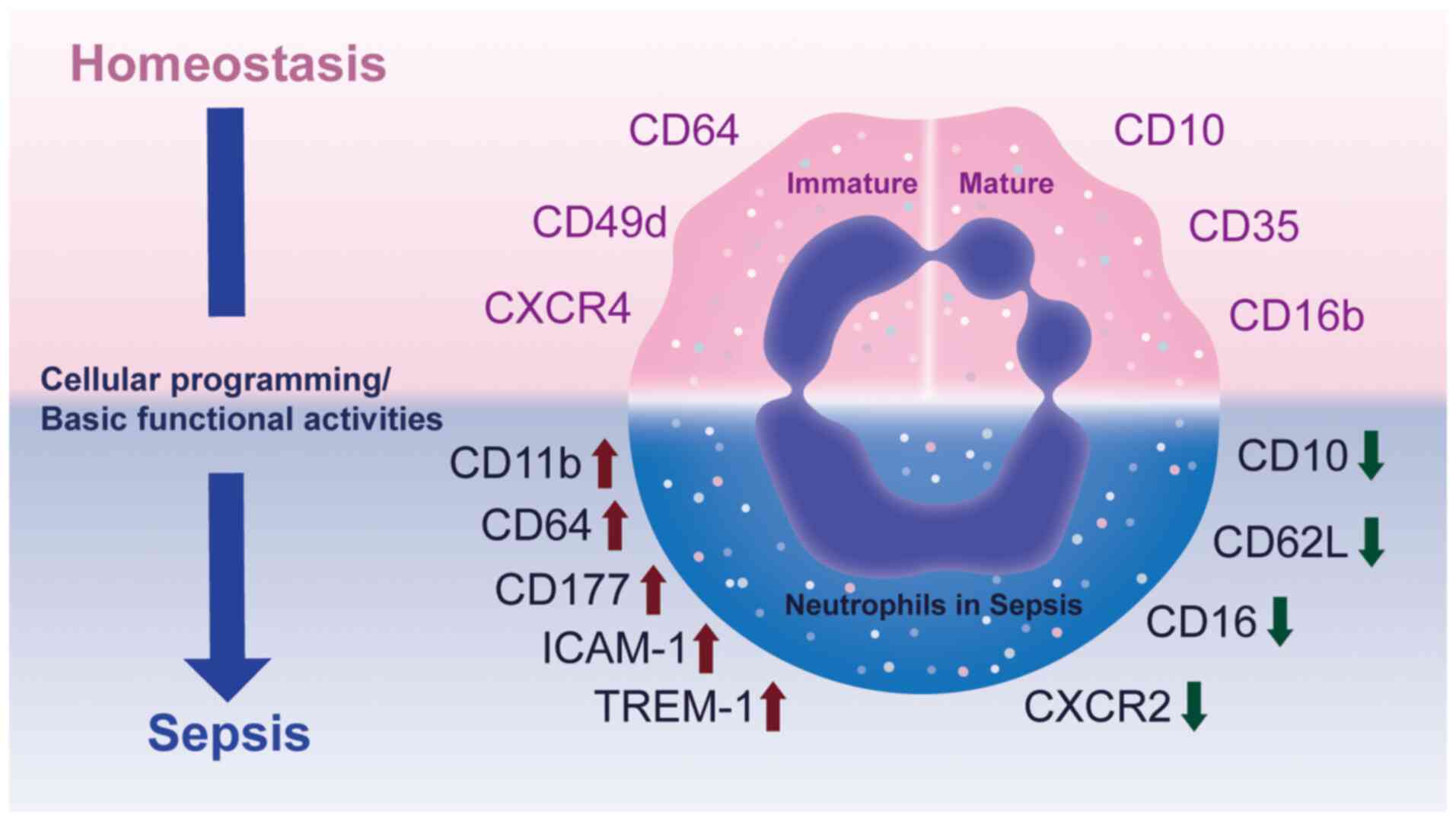
incidence and mortality of hospital-treated sepsis. Current
estimates and limitations. Am J Respir Crit Care Med. 193:259–272.
2016. View Article : Google Scholar
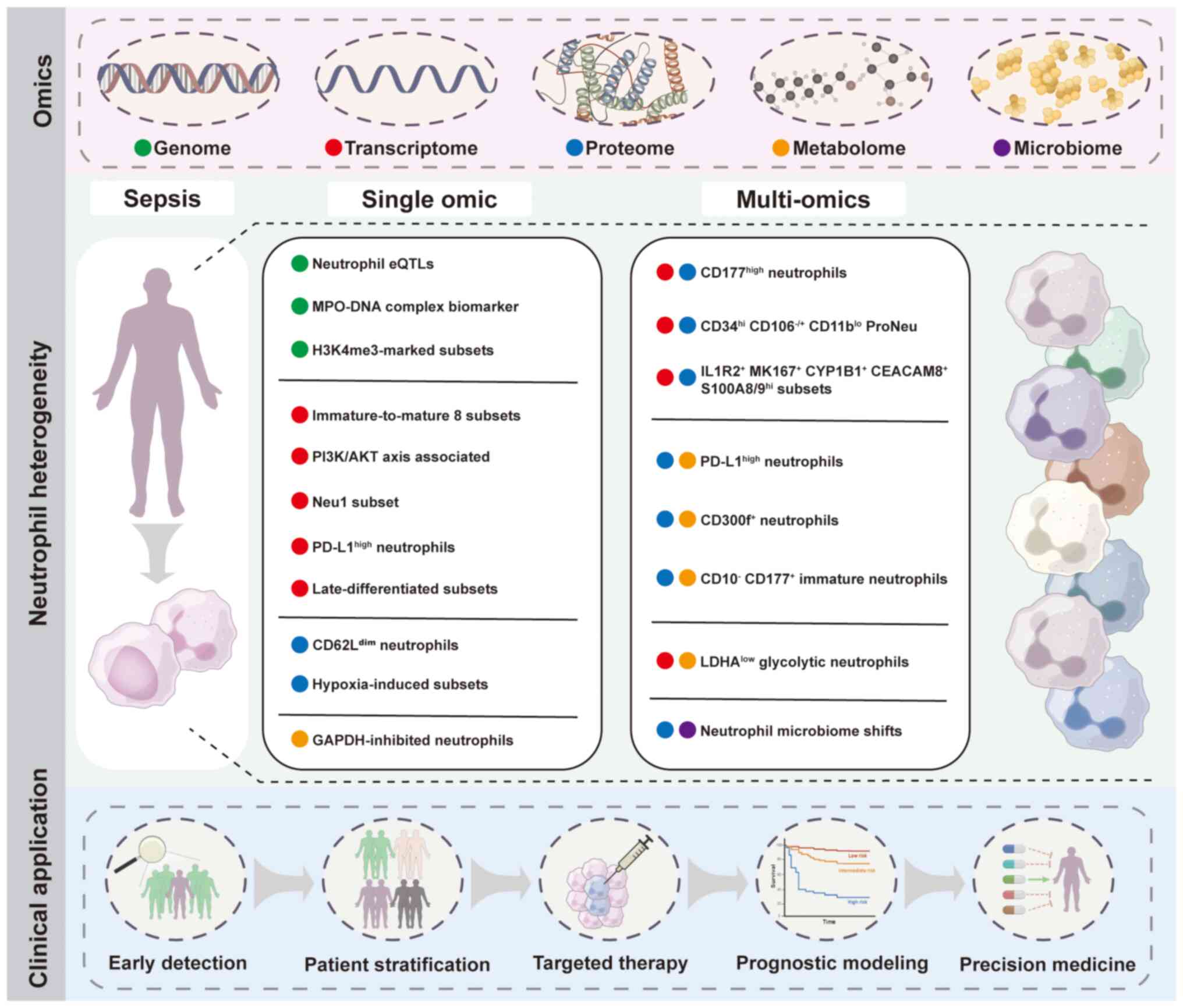
|
|
4
|
Prescott HC and Angus DC: Enhancing
recovery from sepsis: A review. JAMA. 319:62–75. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Prescott HC, Langa KM and Iwashyna TJ:
Readmission diagnoses after hospitalization for severe sepsis and
other acute medical conditions. JAMA. 313:1055–1057. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shankar-Hari M, Saha R, Wilson J, Prescott
HC, Harrison D, Rowan K, Rubenfeld GD and Adhikari NKJ: Rate and
risk factors for rehospitalisation in sepsis survivors: Systematic
review and meta-analysis. Intensive Care Med. 46:619–636. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
van der Poll T, van de Veerdonk FL,
Scicluna BP and Netea MG: The immunopathology of sepsis and
potential therapeutic targets. Nat Rev Immunol. 17:407–420. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen S, Zhang C, Luo J, Lin Z, Chang T,
Dong L, Chen D and Tang ZH: Macrophage activation syndrome in
Sepsis: from pathogenesis to clinical management. Inflamm Res.
73:2179–2197. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chang TD, Chen D, Luo JL, Wang YM, Zhang
C, Chen SY, Lin ZQ, Zhang PD, Tang TX, Li H, et al: The different
paradigms of NK cell death in patients with severe trauma. Cell
Death Dis. 15:6062024. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen S, Zhang C, Chen D, Dong L, Chang T
and Tang ZH: Advances in attractive therapeutic approach for
macrophage activation syndrome in COVID-19. Front Immunol.
14:12002892023. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen D, Zhang C, Luo J, Deng H, Yang J,
Chen S, Zhang P, Dong L, Chang T and Tang ZH: Activated autophagy
of innate immune cells during the early stages of major trauma.
Front Immunol. 13:10903582023. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang J, Chang T, Tang L, Deng H, Chen D,
Luo J, Wu H, Tang T, Zhang C, Li Z, et al: Increased expression of
Tim-3 is associated with depletion of NKT Cells In SARS-CoV-2
infection. Front Immunol. 13:7966822022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fine N, Tasevski N, McCulloch CA,
Tenenbaum HC and Glogauer M: The Neutrophil: Constant defender and
first responder. Front Immunol. 11:5710852020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kangelaris KN, Clemens R, Fang X, Jauregui
A, Liu T, Vessel K, Deiss T, Sinha P, Leligdowicz A, Liu KD, et al:
A neutrophil subset defined by intracellular olfactomedin 4 is
associated with mortality in sepsis. Am J Physiol Lung Cell Mol
Physiol. 320:L892–L902. 2021. View Article : Google Scholar :
|
|
15
|
Shen XF, Cao K, Jiang JP, Guan WX and Du
JF: Neutrophil dysregulation during sepsis: an overview and update.
J Cell Mol Med. 21:1687–1697. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Silvestre-Roig C, Hidalgo A and Soehnlein
O: Neutrophil heterogeneity: Implications for homeostasis and
pathogenesis. Blood. 127:2173–2181. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Naranbhai V, Fairfax BP, Makino S, Humburg
P, Wong D, Ng E, Hill AV and Knight JC: Genomic modulators of gene
expression in human neutrophils. Nat Commun. 6:75452015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Coit P, Yalavarthi S, Ognenovski M, Zhao
W, Hasni S, Wren JD, Kaplan MJ and Sawalha AH: Epigenome profiling
reveals significant DNA demethylation of interferon signature genes
in lupus neutrophils. J Autoimmun. 58:59–66. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pillay J, den Braber I, Vrisekoop N, Kwast
LM, de Boer RJ, Borghans JA, Tesselaar K and Koenderman L: In vivo
labeling with 2H2O reveals a human neutrophil lifespan of 5.4 days.
Blood. 116:625–627. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ericson JA, Duffau P, Yasuda K,
Ortiz-Lopez A, Rothamel K, Rifkin IR and Monach PA; ImmGen
Consortium: Gene expression during the generation and activation of
mouse neutrophils: Implication of novel functional and regulatory
pathways. PLoS One. 9:e1085532014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ng LG, Ostuni R and Hidalgo A:
Heterogeneity of neutrophils. Nat Rev Immunol. 19:255–265. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Grecian R, Whyte MKB and Walmsley SR: The
role of neutrophils in cancer. Br Med Bull. 128:5–14. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Day RB and Link DC: Regulation of
neutrophil trafficking from the bone marrow. Cell Mol Life Sci.
69:1415–1423. 2012. View Article : Google Scholar
|
|
24
|
Elghetany MT: Surface antigen changes
during normal neutrophilic development: A critical review. Blood
Cells Mol Dis. 28:260–274. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Seree-Aphinan C, Vichitkunakorn P,
Navakanitworakul R and Khwannimit B: Distinguishing sepsis from
infection by neutrophil dysfunction: A promising role of CXCR2
surface level. Front Immunol. 11:6086962020. View Article : Google Scholar
|
|
26
|
Silvestre-Roig C, Fridlender ZG, Glogauer
M and Scapini P: Neutrophil diversity in health and disease. Trends
Immunol. 40:565–583. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang X, Fan D, Yang Y, Gimple RC and Zhou
S: Integrative multi-omics approaches to explore immune cell
functions: Challenges and opportunities. iScience. 26:1063592023.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Xie X, Shi Q, Wu P, Zhang X, Kambara H, Su
J, Yu H, Park SY, Guo R, Ren Q, et al: Single-cell transcriptome
profiling reveals neutrophil heterogeneity in homeostasis and
infection. Nat Immunol. 21:1119–1133. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Shaath H, Vishnubalaji R, Elkord E and
Alajez NM: Single-cell transcriptome analysis highlights a role for
neutrophils and inflammatory macrophages in the pathogenesis of
severe COVID-19. Cells. 9:23742020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Deerhake ME, Reyes EY, Xu-Vanpala S and
Shinohara ML: Single-Cell transcriptional heterogeneity of
neutrophils during acute pulmonary cryptococcus neoformans
infection. Front Immunol. 12:6705742021. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Civelek M and Lusis AJ: Systems genetics
approaches to understand complex traits. Nat Rev Genet. 15:34–48.
2014. View Article : Google Scholar :
|
|
32
|
Johnson Chavarria EC: A primer of human
genetics. Yale J Biol Med. 89:6032016.
|
|
33
|
van der Poll T, Shankar-Hari M and
Wiersinga WJ: The immunology of sepsis. Immunity. 54:2450–2464.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Borregaard N: Neutrophils, from marrow to
microbes. Immunity. 33:657–670. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Stadtmann A and Zarbock A: CXCR2: From
bench to bedside. Front Immunol. 3:2632012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Phillipson M and Kubes P: The neutrophil
in vascular inflammation. Nat Med. 17:1381–1390. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chishti AD, Shenton BK, Kirby JA and
Baudouin SV: Neutrophil chemotaxis and receptor expression in
clinical septic shock. Intensive Care Med. 30:605–611. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Rios-Santos F, Alves-Filho JC, Souto FO,
Spiller F, Freitas A, Lotufo CM, Soares MB, Dos Santos RR, Teixeira
MM and Cunha FQ: Down-regulation of CXCR2 on neutrophils in severe
sepsis is mediated by inducible nitric oxide synthase-derived
nitric oxide. Am J Respir Crit Care Med. 175:490–497. 2007.
View Article : Google Scholar
|
|
39
|
Demaret J, Venet F, Friggeri A, Cazalis
MA, Plassais J, Jallades L, Malcus C, Poitevin-Later F, Textoris J,
Lepape A and Monneret G: Marked alterations of neutrophil functions
during sepsis-induced immunosuppression. J Leukoc Biol.
98:1081–1090. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Pillay J, Kamp VM, van Hoffen E, Visser T,
Tak T, Lammers JW, Ulfman LH, Leenen LP, Pickkers P and Koenderman
L: A subset of neutrophils in human systemic inflammation inhibits
T cell responses through Mac-1. J Clin Invest. 122:327–336. 2012.
View Article : Google Scholar :
|
|
41
|
Geng S, Matsushima H, Okamoto T, Yao Y, Lu
R, Page K, Blumenthal RM, Ward NL, Miyazaki T and Takashima A:
Emergence, origin, and function of neutrophil-dendritic cell
hybrids in experimentally induced inflammatory lesions in mice.
Blood. 121:1690–1700. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ode Y, Aziz M and Wang P: CIRP increases
ICAM-1(+) phenotype of neutrophils exhibiting elevated iNOS and
NETs in sepsis. J Leukoc Biol. 103:693–707. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hoffmann JJ: Neutrophil CD64: A diagnostic
marker for infection and sepsis. Clin Chem Lab Med. 47:903–916.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Hoffmann JJ: Neutrophil CD64 as a sepsis
biomarker. Biochem Med (Zagreb). 21:282–290. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Cid J, Aguinaco R, Sánchez R, García-Pardo
G and Llorente A: Neutrophil CD64 expression as marker of bacterial
infection: A systematic review and meta-analysis. J Infect.
60:313–319. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Li S, Huang X, Chen Z, Zhong H, Peng Q,
Deng Y, Qin X and Zhao J: Neutrophil CD64 expression as a biomarker
in the early diagnosis of bacterial infection: A meta-analysis. Int
J Infect Dis. 17:e12–e23. 2013. View Article : Google Scholar
|
|
47
|
Bouchon A, Facchetti F, Weigand MA and
Colonna M: TREM-1 amplifies inflammation and is a crucial mediator
of septic shock. Nature. 410:1103–1107. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Demaret J, Venet F, Plassais J, Cazalis
MA, Vallin H, Friggeri A, Lepape A, Rimmelé T, Textoris J and
Monneret G: Identification of CD177 as the most dysregulated
parameter in a microarray study of purified neutrophils from septic
shock patients. Immunol Lett. 178:122–130. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Amulic B, Cazalet C, Hayes GL, Metzler KD
and Zychlinsky A: Neutrophil function: From mechanisms to disease.
Annu Rev Immunol. 30:459–489. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Boeltz S, Amini P, Anders HJ, Andrade F,
Bilyy R, Chatfield S, Cichon I, Clancy DM, Desai J, Dumych T, et
al: To NET or not to NET: Current opinions and state of the science
regarding the formation of neutrophil extracellular traps. Cell
Death Differ. 26:395–408. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Patel JM, Sapey E, Parekh D, Scott A,
Dosanjh D, Gao F and Thickett DR: Sepsis Induces a Dysregulated
Neutrophil Phenotype That Is Associated with Increased Mortality.
Mediators Inflamm. 2018:40653622018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Martins PS, Kallas EG, Neto MC, Dalboni
MA, Blecher S and Salomão R: Upregulation of reactive oxygen
species generation and phagocytosis, and increased apoptosis in
human neutrophils during severe sepsis and septic shock. Shock.
20:208–212. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Alves-Filho JC, Spiller F and Cunha FQ:
Neutrophil paralysis in sepsis. Shock. 34(Suppl 1): S15–S21. 2010.
View Article : Google Scholar
|
|
54
|
Reddy RC and Standiford TJ: Effects of
sepsis on neutrophil chemotaxis. Curr Opin Hematol. 17:18–24. 2010.
View Article : Google Scholar
|
|
55
|
Tavares-Murta BM, Zaparoli M, Ferreira RB,
Silva-Vergara ML, Oliveira CH, Murta EF, Ferreira SH and Cunha FQ:
Failure of neutrophil chemotactic function in septic patients. Crit
Care Med. 30:1056–1061. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Brown KA, Brain SD, Pearson JD, Edgeworth
JD, Lewis SM and Treacher DF: Neutrophils in development of
multiple organ failure in sepsis. Lancet. 368:157–169. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Arraes SM, Freitas MS, da Silva SV, de
Paula Neto HA, Alves-Filho JC, Auxiliadora Martins M, Basile-Filho
A, Tavares-Murta BM, Barja-Fidalgo C and Cunha FQ: Impaired
neutrophil chemotaxis in sepsis associates with GRK expression and
inhibition of actin assembly and tyrosine phosphorylation. Blood.
108:2906–2913. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Martins PS, Brunialti MK, Martos LS,
Machado FR, Assunçao MS, Blecher S and Salomao R: Expression of
cell surface receptors and oxidative metabolism modulation in the
clinical continuum of sepsis. Crit Care. 12:R252008. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Kalyan S and Kabelitz D: When neutrophils
meet T cells: Beginnings of a tumultuous relationship with
underappreciated potential. Eur J Immunol. 44:627–633. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Kovach MA and Standiford TJ: The function
of neutrophils in sepsis. Curr Opin Infect Dis. 25:321–327. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Chen D, Tang TX, Deng H, Yang XP and Tang
ZH: Interleukin-7 biology and its effects on immune cells: Mediator
of generation, differentiation, survival, and homeostasis. Front
Immunol. 12:7473242021. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Bone RC, Grodzin CJ and Balk RA: Sepsis: A
new hypothesis for pathogenesis of the disease process. Chest.
112:235–243. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Alves-Filho JC, de Freitas A, Spiller F,
Souto FO and Cunha FQ: The role of neutrophils in severe sepsis.
Shock. 30(Suppl 1): S3–S9. 2008. View Article : Google Scholar
|
|
64
|
Drifte G, Dunn-Siegrist I, Tissières P and
Pugin J: Innate immune functions of immature neutrophils in
patients with sepsis and severe systemic inflammatory response
syndrome. Crit Care Med. 41:820–832. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Taneja R, Sharma AP, Hallett MB, Findlay
GP and Morris MR: Immature circulating neutrophils in sepsis have
impaired phagocytosis and calcium signaling. Shock. 30:618–622.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Uhl B, Vadlau Y, Zuchtriegel G, Nekolla K,
Sharaf K, Gaertner F, Massberg S, Krombach F and Reichel CA: Aged
neutrophils contribute to the first line of defense in the acute
inflammatory response. Blood. 128:2327–2337. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Yang P, Li Y, Xie Y and Liu Y: Different
faces for different places: Heterogeneity of neutrophil phenotype
and function. J Immunol Res. 2019:80162542019. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
van Dijk EL, Jaszczyszyn Y, Naquin D and
Thermes C: The third revolution in sequencing technology. Trends
Genet. 34:666–681. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Warr A, Robert C, Hume D, Archibald A,
Deeb N and Watson M: Exome sequencing: Current and future
perspectives. G3 (Bethesda). 5:1543–1550. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Goldman AD and Landweber LF: What is a
genome? PLoS Genet. 12:e10061812016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Wang KC and Chang HY: Epigenomics:
Technologies and applications. Circ Res. 122:1191–1199. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Wang Z, Gerstein M and Snyder M: RNA-Seq:
A revolutionary tool for transcriptomics. Nat Rev Genet. 10:57–63.
2009. View Article : Google Scholar
|
|
73
|
Timp W and Timp G: Beyond mass
spectrometry, the next step in proteomics. Sci Adv. 6:eaax89782020.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Fu Q, Vegesna M, Sundararaman N, Damoc E,
Arrey TN, Pashkova A, Mengesha E, Debbas P, Joung S, Li D, et al: A
proteomics pipeline for generating clinical grade biomarker
candidates from data-independent acquisition mass spectrometry
(DIA-MS) discovery. Angew Chem Int Ed Engl. 63:e2024094462024.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Moco S, Vervoort J, Moco S, Bino RJ, De
Vos RC and Bino R: Metabolomics technologies and metabolite
identification. TrAC Trends in Analytical Chemistry.
2007.26:855–866. 2007. View Article : Google Scholar
|
|
76
|
Bedair M and Sumner LW: Current and
emerging mass-spectrometry technologies for metabolomics. TrAC
Trends in Analytical Chemistry. 27:238–250. 2008. View Article : Google Scholar
|
|
77
|
Andiappan AK, Melchiotti R, Poh TY, Nah M,
Puan KJ, Vigano E, Haase D, Yusof N, San Luis B, Lum J, et al:
Genome-wide analysis of the genetic regulation of gene expression
in human neutrophils. Nat Commun. 6:79712015. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Wang J, Zhang Y, Cheng L, Geng Y, Lu J and
Zhou J: Neutrophil extracellular trap increase the risk of sepsis:
A two-sample, one-way Mendelian randomization study. Zhonghua Wei
Zhong Bing Ji Jiu Yi Xue. 35:1045–1052. 2023.In Chinese. PubMed/NCBI
|
|
79
|
Zhang H, Wang Y, Qu M, Li W, Wu D, Cata JP
and Miao C: Neutrophil, neutrophil extracellular traps and
endothelial cell dysfunction in sepsis. Clin Transl Med.
13:e11702023. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Piatek P, Namiecinska M, Lewkowicz N,
Kulińska-Michalska M, Jabłonowski Z, Matysiak M, Dulska J,
Michlewska S, Wieczorek M and Lewkowicz P: Changes WIthin
H3K4me3-marked histone reveal molecular background of neutrophil
functional plasticity. Front Immunol. 13:9063112022. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Liu Z, Chen Y, Pan T, Liu J, Tian R, Sun
S, Qu H and Chen E: Comprehensive analysis of common different gene
expression signatures in the neutrophils of sepsis. Biomed Res Int.
2021:66554252021. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Xu P, Tao Z and Zhang C: Integrated
multi-omics and artificial intelligence to explore new neutrophils
clusters and potential biomarkers in sepsis with experimental
validation. Front Immunol. 15:13778172024. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Hong Y, Chen L, Sun J, Xing L, Yang Y, Jin
X, Cai H, Dong L, Zhou L and Zhang Z: Single-cell transcriptome
profiling reveals heterogeneous neutrophils with prognostic values
in sepsis. iScience. 25:1053012022. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Goswami DG, Garcia LF, Dodoo C, Dwivedi
AK, Zhou Y, Pappas D and Walker WE: Evaluating the Timeliness and
Specificity of CD69, CD64, and CD25 as Biomarkers of Sepsis in
Mice. Shock. 55:507–518. 2021. View Article : Google Scholar
|
|
85
|
Zhou Y, Zhang Y, Johnson A, Venable A,
Griswold J and Pappas D: Combined CD25, CD64, and CD69 biomarker
panel for flow cytometry diagnosis of sepsis. Talanta. 191:216–221.
2019. View Article : Google Scholar
|
|
86
|
Meghraoui-Kheddar A, Chousterman BG,
Guillou N, Barone SM, Granjeaud S, Vallet H, Corneau A, Guessous K,
de Roquetaillade C, Boissonnas A, et al: Two new neutrophil subsets
define a discriminating sepsis signature. Am J Respir Crit Care
Med. 205:46–59. 2022. View Article : Google Scholar
|
|
87
|
Wang P, Wang J, Li YH, Wang L, Shang HC
and Wang JX: Phenotypical changes of hematopoietic stem and
progenitor cells in sepsis patients: Correlation with immune
status? Front Pharmacol. 11:6402032020. View Article : Google Scholar
|
|
88
|
Qi X, Yu Y, Sun R, Huang J, Liu L, Yang Y,
Rui T and Sun B: Identification and characterization of neutrophil
heterogeneity in sepsis. Crit Care. 25:502021. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Tak T, Wijten P, Heeres M, Pickkers P,
Scholten A, Heck AJR, Vrisekoop N, Leenen LP, Borghans JAM,
Tesselaar K and Koenderman L: Human CD62L(dim) neutrophils
identified as a separate subset by proteome profiling and in vivo
pulse-chase labeling. Blood. 129:3476–3485. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Mallat J, Rahman N, Hamed F, Hernandez G
and Fischer MO: Pathophysiology, mechanisms, and managements of
tissue hypoxia. Anaesth Crit Care Pain Med.
41:1010872022.PubMed/NCBI
|
|
91
|
Watts ER, Howden AJ, Morrison T, Sadiku P,
Hukelmann J, von Kriegsheim A, Ghesquiere B, Murphy F, Mirchandani
AS, Humphries DC, et al: Hypoxia drives murine neutrophil protein
scavenging to maintain central carbon metabolism. J Clin Invest.
131:e1340732021. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Sun L, Yang X, Yuan Z and Wang H:
Metabolic reprogramming in immune response and tissue inflammation.
Arterioscler Thromb Vasc Biol. 40:1990–2001. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Kumar S and Dikshit M: Metabolic insight
of neutrophils in health and disease. Front Immunol. 10:20992019.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Li Y, Hook JS, Ding Q, Xiao X, Chung SS,
Mettlen M, Xu L, Moreland JG and Agathocleous M: Neutrophil
metabolomics in severe COVID-19 reveal GAPDH as a suppressor of
neutrophil extracellular trap formation. Nat Commun. 14:26102023.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Khoyratty TE, Ai Z, Ballesteros I, Eames
HL, Mathie S, Martín-Salamanca S, Wang L, Hemmings A, Willemsen N,
von Werz V, et al: Distinct transcription factor networks control
neutrophil-driven inflammation. Nat Immunol. 22:1093–1106. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Grieshaber-Bouyer R, Radtke FA, Cunin P,
Stifano G, Levescot A, Vijaykumar B, Nelson-Maney N, Blaustein RB,
Monach PA and Nigrovic PA; ImmGen Consortium: The neutrotime
transcriptional signature defines a single continuum of neutrophils
across biological compartments. Nat Commun. 12:28562021. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Tsukahara Y, Lian Z, Zhang X, Whitney C,
Kluger Y, Tuck D, Yamaga S, Nakayama Y, Weissman SM and Newburger
PE: Gene expression in human neutrophils during activation and
priming by bacterial lipopolysaccharide. J Cell Biochem.
89:848–861. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Kaiser R, Gold C, Joppich M, Loew Q,
Akhalkatsi A, Mueller TT, Offensperger F, Droste Zu, Senden A, Popp
O, di Fina L, et al: Peripheral priming induces plastic
transcriptomic and proteomic responses in circulating neutrophils
required for pathogen containment. Sci Adv. 10:eadl17102024.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Grieshaber-Bouyer R and Nigrovic PA:
Neutrophil heterogeneity as therapeutic opportunity in
immune-mediated disease. Front Immunol. 10:3462019. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Eulenberg-Gustavus C, Bähring S, Maass PG,
Luft FC and Kettritz R: Gene silencing and a novel monoallelic
expression pattern in distinct CD177 neutrophil subsets. J Exp Med.
214:2089–2101. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Wu Z, Liang R, Ohnesorg T, Cho V, Lam W,
Abhayaratna WP, Gatenby PA, Perera C, Zhang Y, Whittle B, et al:
Heterogeneity of human neutrophil CD177 expression results from
CD177P1 pseudogene conversion. PLoS Genet. 12:e10060672016.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Kwok I, Becht E, Xia Y, Ng M, The YC, Tan
L, Evrard M, Li JLY, Tran HTN, Tan Y, et al: Combinatorial
single-cell analyses of granulocyte-monocyte progenitor
heterogeneity reveals an early uni-potent neutrophil progenitor.
Immunity. 53:303–318.e5. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Kwok AJ, Allcock A, Ferreira RC,
Cano-Gamez E, Smee M, Burnham KL, Zurke YX; Emergency Medicine
Research Oxford (EMROx); McKechnie S, Mentzer AJ, et al:
Neutrophils and emergency granulopoiesis drive immune suppression
and an extreme response endotype during sepsis. Nat Immunol.
24:767–779. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Borregaard N and Herlin T: Energy
metabolism of human neutrophils during phagocytosis. J Clin Invest.
70:550–557. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Bao Y, Ledderose C, Graf AF, Brix B,
Birsak T, Lee A, Zhang J and Junger WG: mTOR and differential
activation of mitochondria orchestrate neutrophil chemotaxis. J
Cell Biol. 210:1153–1164. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Rodríguez-Espinosa O, Rojas-Espinosa O,
Moreno-Altamirano MM, López-Villegas EO and Sánchez-García FJ:
Metabolic requirements for neutrophil extracellular traps
formation. Immunology. 145:213–224. 2015. View Article : Google Scholar :
|
|
107
|
Pan T, Sun S, Chen Y, Tian R, Chen E, Tan
R, Wang X, Liu Z, Liu J and Qu H: Immune effects of
PI3K/Akt/HIF-1α-regulated glycolysis in polymorphonuclear
neutrophils during sepsis. Crit Care. 26:292022. View Article : Google Scholar
|
|
108
|
Ratter JM, Rooijackers HMM, Hooiveld GJ,
Hijmans AGM, de Galan BE, Tack CJ and Stienstra R: In vitro and in
vivo effects of lactate on metabolism and cytokine production of
human primary PBMCs and monocytes. Front Immunol. 9:25642018.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Dietl K, Renner K, Dettmer K, Timischl B,
Eberhart K, Dorn C, Hellerbrand C, Kastenberger M, Kunz-Schughart
LA, Oefner PJ, et al: Lactic acid and acidification inhibit TNF
secretion and glycolysis of human monocytes. J Immunol.
184:1200–1209. 2010. View Article : Google Scholar
|
|
110
|
Nolt B, Tu F, Wang X, Ha T, Winter R,
Williams DL and Li C: Lactate and immunosuppression in sepsis.
Shock. 49:120–125. 2018. View Article : Google Scholar :
|
|
111
|
Colegio OR, Chu NQ, Szabo AL, Chu T,
Rhebergen AM, Jairam V, Cyrus N, Brokowski CE, Eisenbarth SC,
Phillips GM, et al: Functional polarization of tumour-associated
macrophages by tumour-derived lactic acid. Nature. 513:559–563.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Parthasarathy U, Kuang Y, Thakur G, Hogan
JD, Wyche TP, Norton JE Jr, Killough JR, Sana TR, Beakes C, Shyong
B, et al: Distinct subsets of neutrophils crosstalk with cytokines
and metabolites in patients with sepsis. iScience. 26:1059482023.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Marini O, Costa S, Bevilacqua D, Calzetti
F, Tamassia N, Spina C, De Sabata D, Tinazzi E, Lunardi C, Scupoli
MT, et al: Mature CD10(+) and immature CD10(-) neutrophils present
in G-CSF-treated donors display opposite effects on T cells. Blood.
129:1343–1356. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Wang JF, Li JB, Zhao YJ, Yi WJ, Bian JJ,
Wan XJ, Zhu KM and Deng XM: Up-regulation of programmed cell death
1 ligand 1 on neutrophils may be involved in sepsis-induced
immunosuppression: An animal study and a prospective case-control
study. Anesthesiology. 122:852–863. 2015. View Article : Google Scholar
|
|
115
|
Zhang Y, Zhou Y, Lou J, Li J, Bo L, Zhu K,
Wan X, Deng X and Cai Z: PD-L1 blockade improves survival in
experimental sepsis by inhibiting lymphocyte apoptosis and
reversing monocyte dysfunction. Crit Care. 14:R2202010. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Brahmamdam P, Inoue S, Unsinger J, Chang
KC, McDunn JE and Hotchkiss RS: Delayed administration of anti-PD-1
antibody reverses immune dysfunction and improves survival during
sepsis. J Leukoc Biol. 88:233–240. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Izawa K, Maehara A, Isobe M, Yasuda Y,
Urai M, Hoshino Y, Ueno K, Matsukawa T, Takahashi M, Kaitani A, et
al: Disrupting ceramide-CD300f interaction prevents septic
peritonitis by stimulating neutrophil recruitment. Sci Rep.
7:42982017. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Hu N, Mora-Jensen H, Theilgaard-Mönch K,
Doornbosvan der Meer B, Huitema MG, Stegeman CA, Heeringa P,
Kallenberg CG and Westra J: Differential expression of
granulopoiesis related genes in neutrophil subsets distinguished by
membrane expression of CD177. PLoS One. 9:e996712014. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Davis RE, Sharma S, Conceição J, Carneiro
P, Novais F, Scott P, Sundar S, Bacellar O, Carvalho EM and Wilson
ME: Phenotypic and functional characteristics of HLA-DR(+)
neutrophils in Brazilians with cutaneous leishmaniasis. J Leukoc
Biol. 101:739–749. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Chakravarti A, Rusu D, Flamand N, Borgeat
P and Poubelle PE: Reprogramming of a subpopulation of human blood
neutrophils by prolonged exposure to cytokines. Lab Invest.
89:1084–1099. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Vincent JL and Beumier M: Diagnostic and
prognostic markers in sepsis. Expert Rev Anti Infect Ther.
11:265–275. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Parlato M and Cavaillon JM: Host response
biomarkers in the diagnosis of sepsis: A general overview. Methods
Mol Biol. 1237:149–211. 2015. View Article : Google Scholar
|
|
123
|
Daigo K and Hamakubo T: Host-protective
effect of circulating pentraxin 3 (PTX3) and complex formation with
neutrophil extracellular traps. Front Immunol. 3:3782012.
View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Jaillon S, Peri G, Delneste Y, Frémaux I,
Doni A, Moalli F, Garlanda C, Romani L, Gascan H, Bellocchio S, et
al: The humoral pattern recognition receptor PTX3 is stored in
neutrophil granules and localizes in extracellular traps. J Exp
Med. 204:793–804. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Caironi P, Masson S, Mauri T, Bottazzi B,
Leone R, Magnoli M, Barlera S, Mamprin F, Fedele A, Mantovani A, et
al: Pentraxin 3 in patients with severe sepsis or shock: The ALBIOS
trial. Eur J Clin Invest. 47:73–83. 2017. View Article : Google Scholar
|
|
126
|
Lee YT, Gong M, Chau A, Wong WT, Bazoukis
G, Wong SH, Lampropoulos K, Xia Y, Li G, Wong MCS, et al:
Pentraxin-3 as a marker of sepsis severity and predictor of
mortality outcomes: A systematic review and meta-analysis. J
Infect. 76:1–10. 2018. View Article : Google Scholar
|
|
127
|
Wang C, Li Q, Tang C, Zhao X, He Q, Tang X
and Ren J: Characterization of the blood and neutrophil-specific
microbiomes and exploration of potential bacterial biomarkers for
sepsis in surgical patients. Immun Inflamm Dis. 9:1343–1357. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Kalkoff M, Cursons RT, Sleigh JW and
Jacobson GM: The use of real time rtPCR to quantify inflammatory
mediator expression in leukocytes from patients with severe sepsis.
Anaesth Intensive Care. 32:746–755. 2004. View Article : Google Scholar
|
|
129
|
Lu RJ, Taylor S, Contrepois K, Kim M,
Bravo JI, Ellenberger M, Sampathkumar NK and Benayoun BA:
Multi-omic profiling of primary mouse neutrophils predicts a
pattern of sex-and age-related functional regulation. Nat Aging.
1:715–733. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Bongers SH, Chen N, van Grinsven E, van
Staveren S, Hassani M, Spijkerman R, Hesselink L, Lo Tam Loi AT,
van Aalst C, Leijte GP, et al: Kinetics of neutrophil subsets in
acute, subacute, and chronic inflammation. Front Immunol.
12:6740792021. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Kingren MS, Starr ME and Saito H:
Divergent sepsis pathophysiology in older adults. Antioxid Redox
Signal. 35:1358–1375. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Arcaroli J, Fessler MB and Abraham E:
Genetic polymorphisms and sepsis. Shock. 24:300–312. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Shurtz-Swirski R, Sela S, Herskovits AT,
Shasha SM, Shapiro G, Nasser L and Kristal B: Involvement of
peripheral polymorphonuclear leukocytes in oxidative stress and
inflammation in type 2 diabetic patients. Diabetes Care.
24:104–110. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
van der Poll T and Opal SM: Host-pathogen
interactions in sepsis. Lancet Infect Dis. 8:32–43. 2008.
View Article : Google Scholar
|
|
135
|
Ma Y, Zhao Y and Zhang X: Factors
affecting neutrophil functions during sepsis: Human microbiome and
epigenetics. J Leukoc Biol. 116:672–688. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Shukla P, Rao GM, Pandey G, Sharma S,
Mittapelly N, Shegokar R and Mishra PR: Therapeutic interventions
in sepsis: Current and anticipated pharmacological agents. Br J
Pharmacol. 171:5011–5031. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Sun R, Huang J, Yang Y, Liu L, Shao Y, Li
L and Sun B: Dysfunction of low-density neutrophils in peripheral
circulation in patients with sepsis. Sci Rep. 12:6852022.
View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Dagur PK and McCoy JP Jr: Collection,
storage, and preparation of human blood cells. Curr Protoc Cytom.
73:5.1.–5.1.16. 2015.
|
|
139
|
Hardisty GR, Llanwarne F, Minns D, Gillan
JL, Davidson DJ, Gwyer Findlay E and Gray RD: High purity isolation
of low density neutrophils casts doubt on their exceptionality in
health and disease. Front Immunol. 12:6259222021. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Yennemadi AS, Keane J and Leisching G: The
isolation and characterization of low-and normal-density
neutrophils from whole blood. J Vis Exp. 7(216)2025.
|
|
141
|
Thomas HB, Moots RJ, Edwards SW and Wright
HL: Whose gene is it anyway? The effect of preparation purity on
neutrophil transcriptome studies. PLoS One. 10:e01389822015.
View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Bersanelli M, Mosca E, Remondini D,
Giampieri E, Sala C, Castellani G and Milanesi L: Methods for the
integration of multi-omics data: mathematical aspects. BMC
Bioinformatics. 17(Suppl 2): S152016. View Article : Google Scholar
|
|
143
|
Picard M, Scott-Boyer MP, Bodein A, Périn
O and Droit A: Integration strategies of multi-omics data for
machine learning analysis. Comput Struct Biotechnol J.
19:3735–3746. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Flores JE, Claborne DM, Weller ZD,
Webb-Robertson BM, Waters KM and Bramer LM: Missing data in
multi-omics integration: Recent advances through artificial
intelligence. Front Artif Intell. 6:10983082023. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Hoogendijk AJ, Pourfarzad F, Aarts CEM,
Tool ATJ, Hiemstra IH, Grassi L, Frontini M, Meijer AB, van den
Biggelaar M and Kuijpers TW: Dynamic transcriptome-proteome
correlation networks reveal human myeloid differentiation and
neutrophil-specific programming. Cell Rep. 29:2505–2519.e4. 2019.
View Article : Google Scholar : PubMed/NCBI
|