|
1
|
Li H, Xiao Z, Quarles LD and Li W:
Osteoporosis: Mechanism, molecular target and current status on
drug development. Curr Med Chem. 28:1489–1507. 2021. View Article : Google Scholar
|
|
2
|
Zhang X, Wang Z, Zhang D, Ye D, Zhou Y,
Qin J and Zhang Y: The prevalence and treatment rate trends of
osteoporosis in postmenopausal women. PLoS One. 18:e02902892023.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang L, Yu W, Yin X, Cui L, Tang S, Jiang
N, Cui L, Zhao N, Lin Q, Chen L, et al: Prevalence of osteoporosis
and fracture in China: The China osteoporosis prevalence study.
JAMA Netw Open. 4:e21211062021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Center JR, Nguyen TV, Schneider D,
Sambrook PN and Eisman JA: Mortality after all major types of
osteoporotic fracture in men and women: An observational study.
Lancet. 353:878–882. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Harada S and Rodan GA: Control of
osteoblast function and regulation of bone mass. Nature.
423:349–355. 2003. View Article : Google Scholar : PubMed/NCBI
|
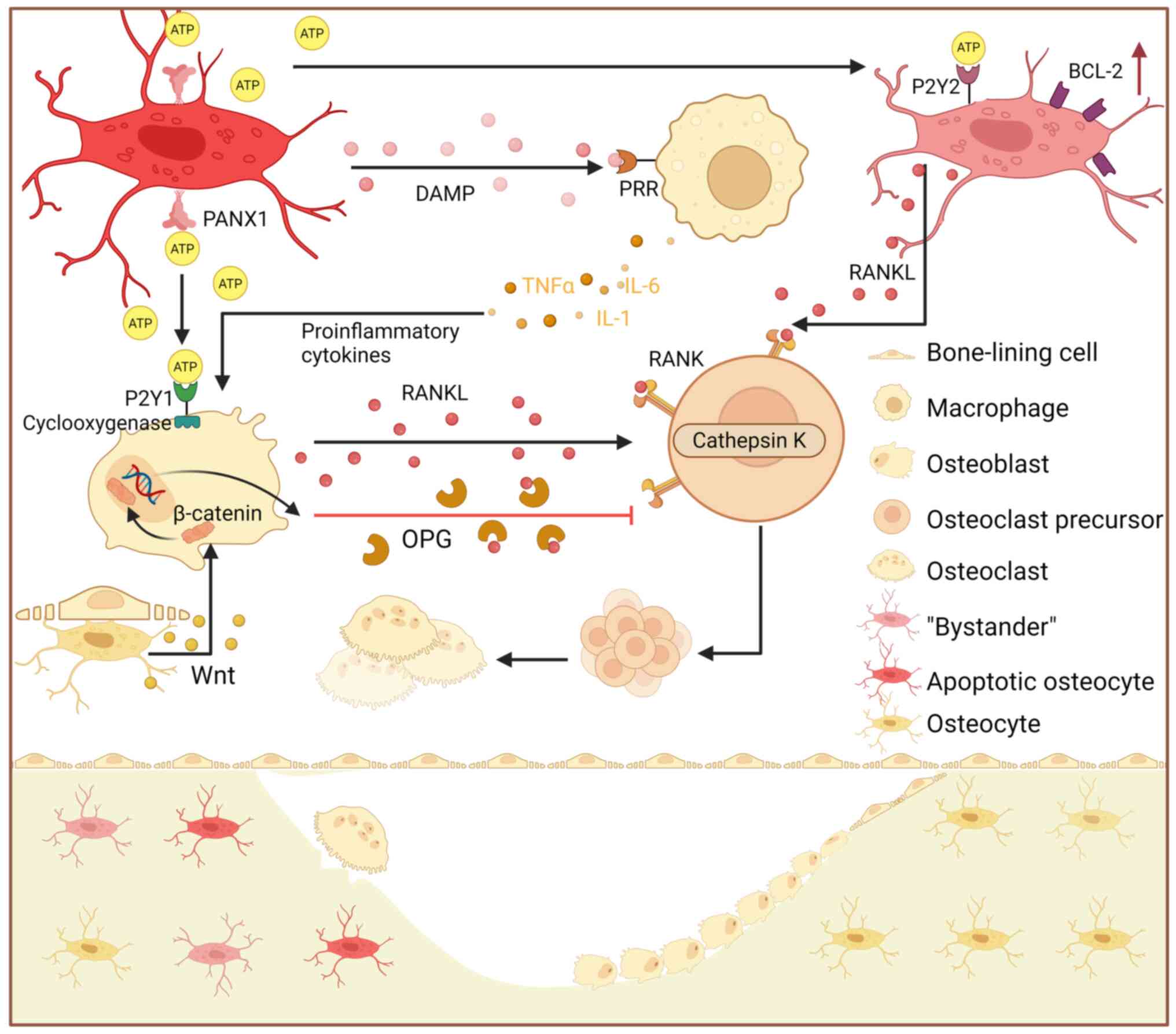
|
6
|
Raisz LG: Pathogenesis of osteoporosis:
Concepts, conflicts, and prospects. J Clin Invest. 115:3318–3325.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gao M, Gao W, Papadimitriou JM, Zhang C,
Gao J and Zheng M: Exosomes-the enigmatic regulators of bone
homeostasis. Bone Res. 6:362018. View Article : Google Scholar : PubMed/NCBI
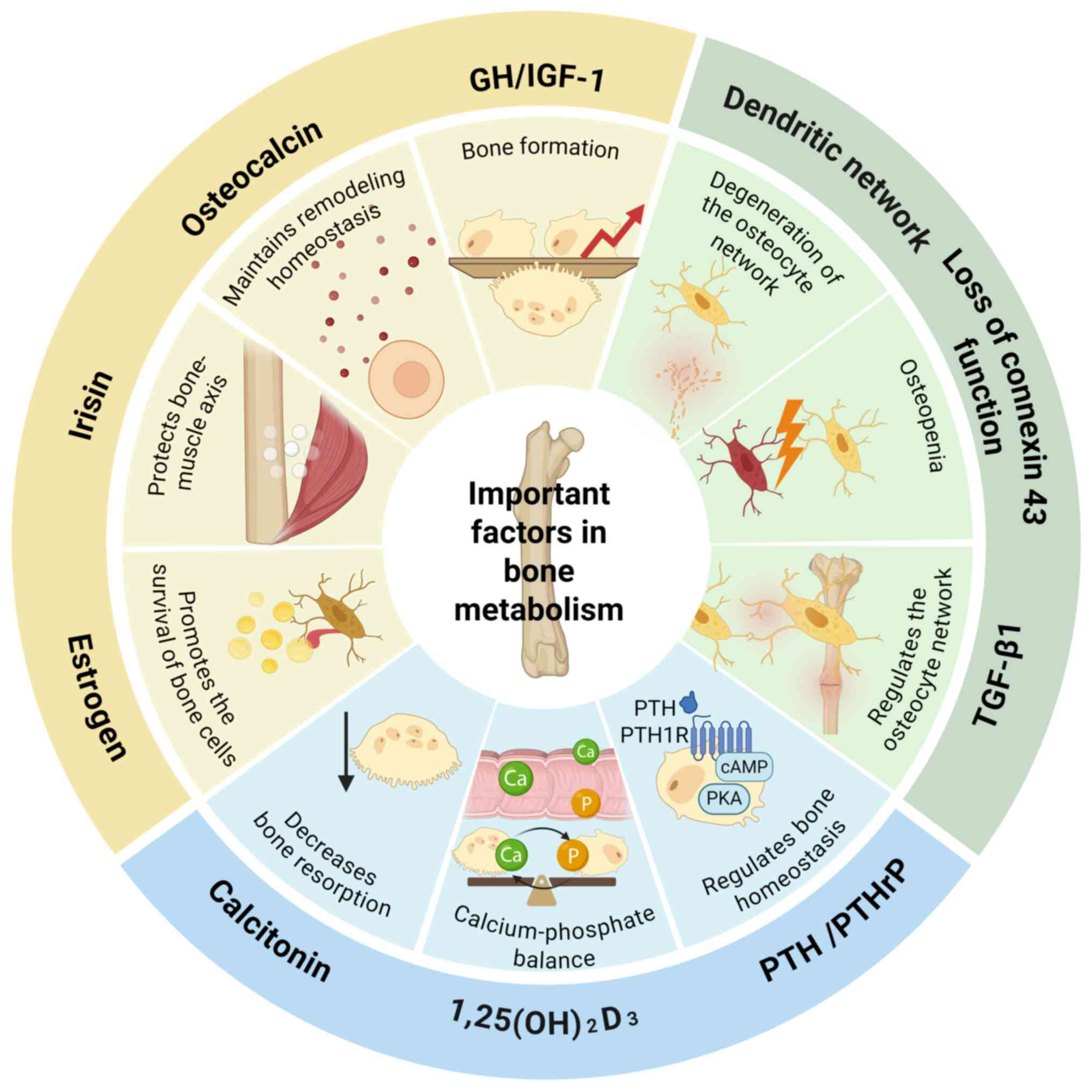
|
|
8
|
Zhang Y, Li Q, Peng X, Ji P, Zhang Y, Jin
J, Yuan Z, Jiang J, Tian G, Cai M, et al: Targeting
chaperone-mediated autophagy to regulate osteoclast activity as a
therapeutic strategy for osteoporosis. Mater Today Bio.
35:1023112025. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Harper AE, Miller RH and Block KP:
Branched-chain amino acid metabolism. Annu Rev Nutr. 4:409–454.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mansoori S, Ho MY, Ng KK and Cheng KK:
Branched-chain amino acid metabolism: Pathophysiological mechanism
and therapeutic intervention in metabolic diseases. Obes Rev.
26:e138562025. View Article : Google Scholar
|
|
11
|
Trautman ME, Richardson NE and Lamming DW:
Protein restriction and branched-chain amino acid restriction
promote geroprotective shifts in metabolism. Aging Cell.
21:e136262022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Go M, Shin E, Jang SY, Nam M, Hwang GS and
Lee SY: BCAT1 promotes osteoclast maturation by regulating
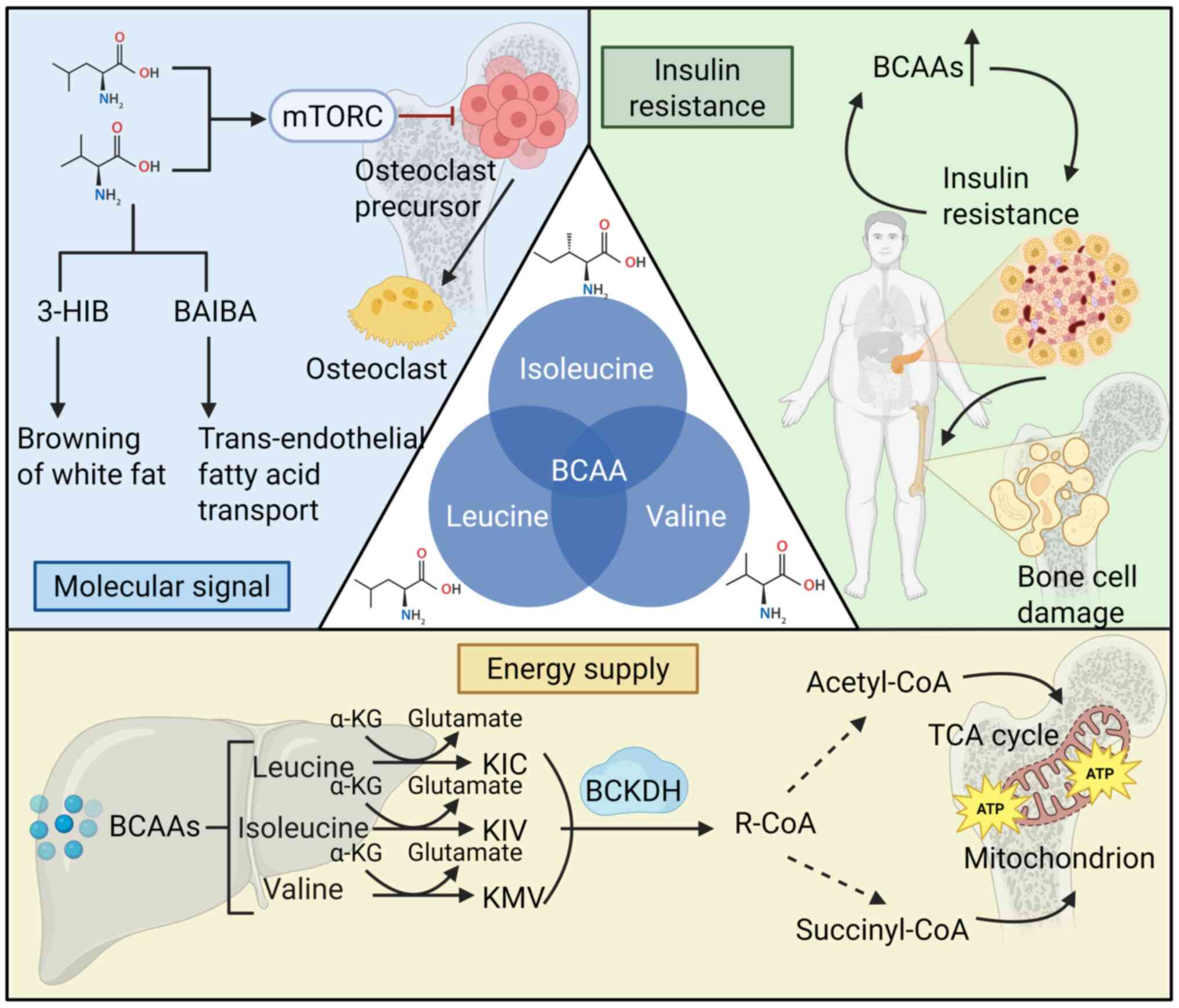
branched-chain amino acid metabolism. Exp Mol Med. 54:825–833.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Weiner S and Traub W: Bone structure: From
angstroms to microns. FASEB J. 6:879–885. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hua R, Han Y, Ni Q, Fajardo RJ, Iozzo RV,
Ahmed R, Nyman JS, Wang X and Jiang JX: Pivotal roles of biglycan
and decorin in regulating bone mass, water retention, and bone
toughness. Bone Res. 13:22025. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Calvi LM, Adams GB, Weibrecht KW, Weber
JM, Olson DP, Knight MC, Martin RP, Schipani E, Divieti P,
Bringhurst FR, et al: Osteoblastic cells regulate the
haematopoietic stem cell niche. Nature. 425:841–846. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang J, Niu C, Ye L, Huang H, He X, Tong
WG, Ross J, Haug J, Johnson T, Feng JQ, et al: Identification of
the haematopoietic stem cell niche and control of the niche size.
Nature. 425:836–841. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Taichman RS and Emerson SG: Human
osteoblasts support hematopoiesis through the production of
granulocyte colony-stimulating factor. J Exp Med. 179:1677–1682.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bolamperti S, Villa I and Rubinacci A:
Bone remodeling: an operational process ensuring survival and bone
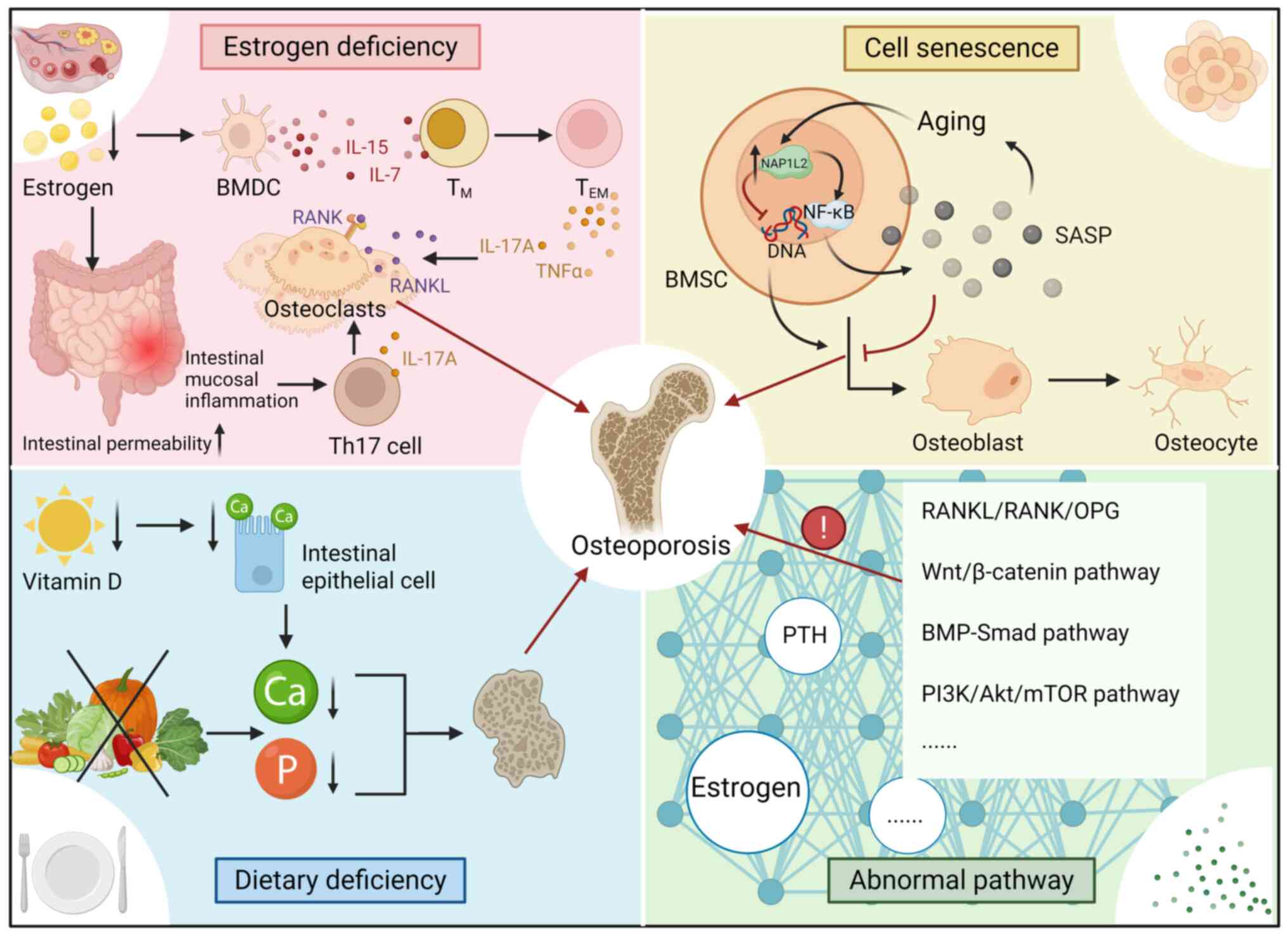
mechanical competence. Bone Res. 10:482022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hattner R, Epker BN and Frost HM:
Suggested sequential mode of control of changes in cell behaviour
in adult bone remodelling. Nature. 206:489–490. 1965. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Barak MM: Bone modeling or bone
remodeling: That is the question. Am J Phys Anthropol. 172:153–155.
2020. View Article : Google Scholar
|
|
21
|
Yan C, Zhang P, Qin Q, Jiang K, Luo Y,
Xiang C, He J, Chen L, Jiang D, Cui W and Li Y: 3D-printed bone
regeneration scaffolds modulate bone metabolic homeostasis through
vascularization for osteoporotic bone defects. Biomaterials.
311:1226992024. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Udagawa N, Takahashi N, Akatsu T, Tanaka
H, Sasaki T, Nishihara T, Koga T, Martin TJ and Suda T: Origin of
osteoclasts: mature monocytes and macrophages are capable of
differentiating into osteoclasts under a suitable microenvironment
prepared by bone marrow-derived stromal cells. Proc Natl Acad Sci
USA. 87:7260–7264. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Boyle WJ, Simonet WS and Lacey DL:
Osteoclast differentiation and activation. Nature. 423:337–342.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Teitelbaum SL: Bone resorption by
osteoclasts. Science. 289:1504–1508. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nakahama KI, Hidaka S, Goto K, Tada M, Doi
T, Nakamura H, Akiyama M and Shinohara M: Visualization and
quantification of RANK-RANKL binding for application to disease
investigations and drug discovery. Bone. 195:1174732025. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Holliday LS, Patel SS and Rody WJ Jr:
RANKL and RANK in extracellular vesicles: Surprising new players in
bone remodeling. Extracell Vesicles Circ Nucl Acids. 2:18–28.
2021.PubMed/NCBI
|
|
27
|
Soriano P, Montgomery C, Geske R and
Bradley A: Targeted disruption of the c-src proto-oncogene leads to
osteopetrosis in mice. Cell. 64:693–702. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Boyce BF, Yoneda T, Lowe C, Soriano P and
Mundy GR: Requirement of pp60c-src expression for osteoclasts to
form ruffled borders and resorb bone in mice. J Clin Invest.
90:1622–1627. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gelb BD, Shi GP, Chapman HA and Desnick
RJ: Pycnodysostosis, a lysosomal disease caused by cathepsin K
deficiency. Science. 273:1236–1238. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Saftig P, Hunziker E, Everts V, Jones S,
Boyde A, Wehmeyer O, Suter A and von Figura K: Functions of
cathepsin K in bone resorption. Lessons from cathepsin K deficient
mice. Adv Exp Med Biol. 477:293–303. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Mizoguchi T and Ono N: The diverse origin
of bone-forming osteoblasts. J Bone Miner Res. 36:1432–1447. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tang Y, Wu X, Lei W, Pang L, Wan C, Shi Z,
Zhao L, Nagy TR, Peng X, Hu J, et al: TGF-beta1-induced migration
of bone mesenchymal stem cells couples bone resorption with
formation. Nat Med. 15:757–765. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bodine PV and Komm BS: Wnt signaling and
osteoblastogenesis. Rev Endocr Metab Disord. 7:33–39. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Eriksen EF: Cellular mechanisms of bone
remodeling. Rev Endocr Metab Disord. 11:219–227. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hong AR, Kim K, Lee JY, Yang JY, Kim JH,
Shin CS and Kim SW: Transformation of mature osteoblasts into bone
lining cells and RNA sequencing-based transcriptome profiling of
mouse bone during mechanical unloading. Endocrinol Metab (Seoul).
35:456–469. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang JS and Wein MN: Pathways controlling
formation and maintenance of the osteocyte dendrite network. Curr
Osteoporos Rep. 20:493–504. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Komori T: Cell death in chondrocytes,
osteoblasts, and osteocytes. Int J Mol Sci. 17:20452016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Takeuchi O and Akira S: Pattern
recognition receptors and inflammation. Cell. 140:805–820. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Messmer D, Yang H, Telusma G, Knoll F, Li
J, Messmer B, Tracey KJ and Chiorazzi N: High mobility group box
protein 1: An endogenous signal for dendritic cell maturation and
Th1 polarization. J Immunol. 173:307–313. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Giannoni P, Marini C, Cutrona G, Matis S,
Capra MC, Puglisi F, Luzzi P, Pigozzi S, Gaggero G, Neri A, et al:
Chronic lymphocytic leukemia cells impair osteoblastogenesis and
promote osteoclastogenesis: Role of TNFα, IL-6 and IL-11 cytokines.
Haematologica. 106:2598–2612. 2021. View Article : Google Scholar
|
|
41
|
Kringelbach TM, Aslan D, Novak I, Schwarz
P and Jørgensen NR: UTP-induced ATP release is a fine-tuned
signalling pathway in osteocytes. Purinergic Signal. 10:337–347.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Verborgt O, Gibson GJ and Schaffler MB:
Loss of osteocyte integrity in association with microdamage and
bone remodeling after fatigue in vivo. J Bone Miner Res. 15:60–67.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Cheung WY, Fritton JC, Morgan SA,
Seref-Ferlengez Z, Basta-Pljakic J, Thi MM, Suadicani SO, Spray DC,
Majeska RJ and Schaffler MB: Pannexin-1 and P2X7-receptor are
required for apoptotic osteocytes in fatigued bone to trigger RANKL
production in neighboring bystander osteocytes. J Bone Miner Res.
31:890–899. 2016. View Article : Google Scholar
|
|
44
|
Luckprom P, Wongkhantee S, Yongchaitrakul
T and Pavasant P: Adenosine triphosphate stimulates RANKL
expression through P2Y1 receptor-cyclo-oxygenase-dependent pathway
in human periodontal ligament cells. J Periodontal Res. 45:404–411.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Buckley KA, Hipskind RA, Gartland A,
Bowler WB and Gallagher JA: Adenosine triphosphate stimulates human
osteoclast activity via upregulation of osteoblast-expressed
receptor activator of nuclear factor-kappa B ligand. Bone.
31:582–590. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Gallagher JA: ATP P2 receptors and
regulation of bone effector cells. J Musculoskelet Neuronal
Interact. 4:125–127. 2004.PubMed/NCBI
|
|
47
|
Cusato K, Bosco A, Rozental R, Guimarães
CA, Reese BE, Linden R and Spray DC: Gap junctions mediate
bystander cell death in developing retina. J Neurosci.
23:6413–6422. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Cawley KM, Bustamante-Gomez NC, Guha AG,
MacLeod RS, Xiong J, Gubrij I, Liu Y, Mulkey R, Palmieri M,
Thostenson JD, et al: Local production of osteoprotegerin by
osteoblasts suppresses bone resorption. Cell Rep. 32:1080522020.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Kennedy OD, Laudier DM, Majeska RJ, Sun HB
and Schaffler MB: Osteocyte apoptosis is required for production of
osteoclastogenic signals following bone fatigue in vivo. Bone.
64:132–137. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Verborgt O, Tatton NA, Majeska RJ and
Schaffler MB: Spatial distribution of Bax and Bcl-2 in osteocytes
after bone fatigue: complementary roles in bone remodeling
regulation? J Bone Miner Res. 17:907–914. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lieben L, Carmeliet G and Masuyama R:
Calcemic actions of vitamin D: Effects on the intestine, kidney and
bone. Best Pract Res Clin Endocrinol Metab. 25:561–572. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zarei A, Morovat A, Javaid K and Brown CP:
Vitamin D receptor expression in human bone tissue and
dose-dependent activation in resorbing osteoclasts. Bone Res.
4:160302016. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Lips P and van Schoor NM: The effect of
vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol
Metab. 25:585–591. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Bikle DD: Vitamin D and bone. Curr
Osteoporos Rep. 10:151–159. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Arnaud CD Jr, Tenenhouse AM and Rasmussen
H: Parathyroid hormone. Annu Rev Physiol. 29:349–372. 1967.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Martin TJ, Sims NA and Seeman E:
Physiological and pharmacological roles of PTH and PTHrP in bone
using their shared receptor, PTH1R. Endocr Rev. 42:383–406. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Quarles LD: Skeletal secretion of FGF-23
regulates phosphate and vitamin D metabolism. Nat Rev Endocrinol.
8:276–286. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Jüppner H: Phosphate and FGF-23. Kidney
Int. 79121:S24–S27. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Naot D, Musson DS and Cornish J: The
activity of peptides of the calcitonin family in bone. Physiol Rev.
99:781–805. 2019. View Article : Google Scholar
|
|
60
|
Xu J, Wang J, Chen X, Li Y, Mi J and Qin
L: The effects of calcitonin gene-related peptide on bone
homeostasis and regeneration. Curr Osteoporos Rep. 18:621–632.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Lecanda F, Warlow PM, Sheikh S, Furlan F,
Steinberg TH and Civitelli R: Connexin43 deficiency causes delayed
ossification, craniofacial abnormalities, and osteoblast
dysfunction. J Cell Biol. 151:931–944. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Chung DJ, Castro CH, Watkins M, Stains JP,
Chung MY, Szejnfeld VL, Willecke K, Theis M and Civitelli R: Low
peak bone mass and attenuated anabolic response to parathyroid
hormone in mice with an osteoblast-specific deletion of connexin43.
J Cell Sci. 119(Pt 20): 4187–4198. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Zhang Y, Paul EM, Sathyendra V, Davison A,
Sharkey N, Bronson S, Srinivasan S, Gross TS and Donahue HJ:
Enhanced osteoclastic resorption and responsiveness to mechanical
load in gap junction deficient bone. PLoS One. 6:e235162011.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Tiede-Lewis LM, Xie Y, Hulbert MA, Campos
R, Dallas MR, Dusevich V, Bonewald LF and Dallas SL: Degeneration
of the osteocyte network in the C57BL/6 mouse model of aging. Aging
(Albany NY). 9:2190–2208. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Dole NS, Mazur CM, Acevedo C, Lopez JP,
Monteiro DA, Fowler TW, Gludovatz B, Walsh F, Regan JN, Messina S,
et al: Osteocyte-Intrinsic TGF-β signaling regulates bone quality
through perilacunar/canalicular remodeling. Cell Rep. 21:2585–2596.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Kreis NN, Friemel A, Ritter A, Hentrich
AE, Siebelitz E, Louwen F and Yuan J: In-depth analysis of
obesity-associated changes in adipose tissue-derived mesenchymal
stromal/stem cells and primary cilia function. Commun Biol.
8:14622025. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Olney RC: Regulation of bone mass by
growth hormone. Med Pediatr Oncol. 41:228–234. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Iglesias L, Yeh JK, Castro-Magana M and
Aloia JF: Effects of growth hormone on bone modeling and remodeling
in hypophysectomized young female rats: A bone histomorphometric
study. J Bone Miner Metab. 29:159–167. 2011. View Article : Google Scholar
|
|
69
|
Hayashi M, Nakashima T, Yoshimura N,
Okamoto K, Tanaka S and Takayanagi H: Autoregulation of osteocyte
Sema3A orchestrates estrogen action and counteracts bone aging.
Cell Metab. 29:627–637.e5. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Sharma D, Larriera AI, Palacio-Mancheno
PE, Gatti V, Fritton JC, Bromage TG, Cardoso L, Doty SB and Fritton
SP: The effects of estrogen deficiency on cortical bone
microporosity and mineralization. Bone. 110:1–10. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Jackson E, Lara-Castillo N, Akhter MP,
Dallas M, Scott JM, Ganesh T and Johnson ML: Osteocyte
Wnt/β-catenin pathway activation upon mechanical loading is altered
in ovariectomized mice. Bone Rep. 15:1011292021. View Article : Google Scholar
|
|
72
|
Ma L, Hua R, Tian Y, Cheng H, Fajardo RJ,
Pearson JJ, Guda T, Shropshire DB, Gu S and Jiang JX: Connexin 43
hemichannels protect bone loss during estrogen deficiency. Bone
Res. 7:112019. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
He Z, Li H, Han X, Zhou F, Du J, Yang Y,
Xu Q, Zhang S, Zhang S, Zhao N, et al: Irisin inhibits osteocyte
apoptosis by activating the Erk signaling pathway in vitro and
attenuates ALCT-induced osteoarthritis in mice. Bone.
141:1155732020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Al-Suhaimi EA and Al-Jafary MA: Endocrine
roles of vitamin K-dependent-osteocalcin in the relation between
bone metabolism and metabolic disorders. Rev Endocr Metab Disord.
21:117–125. 2020. View Article : Google Scholar
|
|
75
|
Yang D, Gong G, Song J, Chen J, Wang S, Li
J and Wang G: Ferroptosis-mediated osteoclast-osteoblast crosstalk:
Signaling pathways governing bone remodeling in osteoporosis. J
Orthop Surg Res. 20:8882025. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Baek KH, Chung YS, Koh JM, Kim IJ, Kim KM,
Min YK, Park KD, Dinavahi R, Maddox J, Yang W, et al: Romosozumab
in postmenopausal Korean women with osteoporosis: A Randomized,
double-blind, placebo-controlled efficacy and safety study.
Endocrinol Metab (Seoul). 36:60–69. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Kasiske BL, Kumar R, Kimmel PL, Pesavento
TE, Kalil RS, Kraus ES, Rabb H, Posselt AM, Anderson-Haag TL,
Steffes MW, et al: Abnormalities in biomarkers of mineral and bone
metabolism in kidney donors. Kidney Int. 90:861–868. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Schwetz V, Pieber T and Obermayer-Pietsch
B: The endocrine role of the skeleton: Background and clinical
evidence. Eur J Endocrinol. 166:959–967. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Kärkkäinen M, Tuppurainen M, Salovaara K,
Sandini L, Rikkonen T, Sirola J, Honkanen R, Jurvelin J, Alhava E
and Kröger H: Effect of calcium and vitamin D supplementation on
bone mineral density in women aged 65-71 years: A 3-year randomized
population-based trial (OSTPRE-FPS). Osteoporos Int. 21:2047–2055.
2010. View Article : Google Scholar
|
|
80
|
Remer T, Krupp D and Shi L: Dietary
protein's and dietary acid load's influence on bone health. Crit
Rev Food Sci Nutr. 54:1140–1150. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Langeveld M and Hollak CEM: Bone health in
patients with inborn errors of metabolism. Rev Endocr Metab Disord.
19:81–92. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Yang K, Li J and Tao L: Purine metabolism
in the development of osteoporosis. Biomed Pharmacother.
155:1137842022. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Iantomasi T, Romagnoli C, Palmini G,
Donati S, Falsetti I, Miglietta F, Aurilia C, Marini F, Giusti F
and Brandi ML: Oxidative stress and inflammation in osteoporosis:
Molecular mechanisms involved and the relationship with microRNAs.
Int J Mol Sci. 24:37722023. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Johnson JT, Hussain MA, Cherian KE, Kapoor
N and Paul TV: Chronic alcohol consumption and its impact on bone
and metabolic health - A narrative review. Indian J Endocrinol
Metab. 26:206–212. 2022.PubMed/NCBI
|
|
85
|
Ehnert S, Aspera-Werz RH, Ihle C, Trost M,
Zirn B, Flesch I, Schröter S, Relja B and Nussler AK: Smoking
dependent alterations in bone formation and inflammation represent
major risk factors for complications following total joint
arthroplasty. J Clin Med. 8:4062019. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Huang YS, Gao JW, Ao RF, Liu XY, Wu DZ,
Huang JL, Tu C, Zhuang JS, Zhu SY and Zhong ZM: Accumulation of
advanced oxidation protein products aggravates bone-fat imbalance
during skeletal aging. J Orthop Translat. 51:24–36. 2025.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Schröder K: NADPH oxidases in bone
homeostasis and osteoporosis. Free Radic Biol Med. 132:67–72. 2019.
View Article : Google Scholar
|
|
88
|
Jiang N, Liu J, Guan C, Ma C, An J and
Tang X: Thioredoxin-interacting protein: A new therapeutic target
in bone metabolism disorders? Front Immunol. 13:9551282022.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Le Couteur DG, Solon-Biet SM, Cogger VC,
Ribeiro R, de Cabo R, Raubenheimer D, Cooney GJ and Simpson SJ:
Branched chain amino acids, aging and age-related health. Ageing
Res Rev. 64:1011982020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Brosnan JT and Brosnan ME: Branched-chain
amino acids: Enzyme and substrate regulation. J Nutr. 136(1 Suppl):
207S–211S. 2006. View Article : Google Scholar
|
|
91
|
Han JM, Jeong SJ, Park MC, Kim G, Kwon NH,
Kim HK, Ha SH, Ryu SH and Kim S: Leucyl-tRNA synthetase is an
intracellular leucine sensor for the mTORC1-signaling pathway.
Cell. 149:410–424. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Zhang S, Zeng X, Ren M, Mao X and Qiao S:
Novel metabolic and physiological functions of branched chain amino
acids: A review. J Anim Sci Biotechnol. 8:102017. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Neinast MD, Jang C, Hui S, Murashige DS,
Chu Q, Morscher RJ, Li X, Zhan L, White E, Anthony TG, et al:
Quantitative analysis of the whole-body metabolic fate of
branched-chain amino acids. Cell Metab. 29:417–429.e4. 2019.
View Article : Google Scholar
|
|
94
|
Wang W, Liu Z, Liu L, Han T, Yang X and
Sun C: Genetic predisposition to impaired metabolism of the
branched chain amino acids, dietary intakes, and risk of type 2
diabetes. Genes Nutr. 16:202021. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Bonvini A, Coqueiro AY, Tirapegui J,
Calder PC and Rogero MM: Immunomodulatory role of branched-chain
amino acids. Nutr Rev. 76:840–856. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Deng AF, Wang FX, Wang SC, Zhang YZ, Bai L
and Su JC: Bone-organ axes: Bidirectional crosstalk. Mil Med Res.
11:372024.PubMed/NCBI
|
|
97
|
Hasegawa T, Kikuta J, Sudo T, Matsuura Y,
Matsui T, Simmons S, Ebina K, Hirao M, Okuzaki D, Yoshida Y, et al:
Identification of a novel arthritis-associated osteoclast precursor
macrophage regulated by FoxM1. Nat Immunol. 20:1631–1643. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Anthony JC, Yoshizawa F, Anthony TG, Vary
TC, Jefferson LS and Kimball SR: Leucine stimulates translation
initiation in skeletal muscle of postabsorptive rats via a
rapamycin-sensitive pathway. J Nutr. 130:2413–2419. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Yang M, Zhang X, Ding Y, Yang L, Ren W,
Gao Y, Yao K, Zhou Y and Shao W: The effect of valine on the
synthesis of α-Casein in MAC-T cells and the expression and
phosphorylation of genes related to the mTOR signaling pathway. Int
J Mol Sci. 26:31792025. View Article : Google Scholar
|
|
100
|
Glantschnig H, Fisher JE, Wesolowski G,
Rodan GA and Reszka AA: M-CSF, TNFalpha and RANK ligand promote
osteoclast survival by signaling through mTOR/S6 kinase. Cell Death
Differ. 10:1165–1177. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Kneissel M, Luong-Nguyen NH, Baptist M,
Cortesi R, Zumstein-Mecker S, Kossida S, O'Reilly T, Lane H and
Susa M: Everolimus suppresses cancellous bone loss, bone
resorption, and cathepsin K expression by osteoclasts. Bone.
35:1144–1156. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Ory B, Moriceau G, Redini F and Heymann D:
mTOR inhibitors (rapamycin and its derivatives) and nitrogen
containing bisphosphonates: Bi-functional compounds for the
treatment of bone tumours. Curr Med Chem. 14:1381–1387. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Benslimane-Ahmim Z, Heymann D, Dizier B,
Lokajczyk A, Brion R, Laurendeau I, Bièche I, Smadja DM,
Galy-Fauroux I, Colliec-Jouault S, et al: Osteoprotegerin, a new
actor in vasculogenesis, stimulates endothelial colony-forming
cells properties. J Thromb Haemost. 9:834–843. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Gnant M, Baselga J, Rugo HS, Noguchi S,
Burris HA, Piccart M, Hortobagyi GN, Eakle J, Mukai H, Iwata H, et
al: Effect of everolimus on bone marker levels and progressive
disease in bone in BOLERO-2. J Natl Cancer Inst. 105:654–663. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Roberts LD, Boström P, O'Sullivan JF,
Schinzel RT, Lewis GD, Dejam A, Lee YK, Palma MJ, Calhoun S,
Georgiadi A, et al: β-Aminoisobutyric acid induces browning of
white fat and hepatic β-oxidation and is inversely correlated with
cardiometabolic risk factors. Cell Metab. 19:96–108. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Jang C, Oh SF, Wada S, Rowe GC, Liu L,
Chan MC, Rhee J, Hoshino A, Kim B, Ibrahim A, et al: A
branched-chain amino acid metabolite drives vascular fatty acid
transport and causes insulin resistance. Nat Med. 22:421–426. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Batch BC, Shah SH, Newgard CB, Turer CB,
Haynes C, Bain JR, Muehlbauer M, Patel MJ, Stevens RD, Appel LJ, et
al: Branched chain amino acids are novel biomarkers for
discrimination of metabolic wellness. Metabolism. 62:961–969. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Connelly MA, Wolak-Dinsmore J and Dullaart
RPF: Branched chain amino acids are associated with insulin
resistance independent of leptin and adiponectin in subjects with
varying degrees of glucose tolerance. Metab Syndr Relat Disord.
15:183–186. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Lotta LA, Scott RA, Sharp SJ, Burgess S,
Luan J, Tillin T, Schmidt AF, Imamura F, Stewart ID, Perry JR, et
al: Genetic predisposition to an impaired metabolism of the
branched-chain amino acids and risk of type 2 diabetes: A mendelian
randomisation analysis. PLoS Med. 13:e10021792016. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Felig P, Marliss E and Cahill GF Jr:
Plasma amino acid levels and insulin secretion in obesity. N Engl J
Med. 281:811–816. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Newgard CB, An J, Bain JR, Muehlbauer MJ,
Stevens RD, Lien LF, Haqq AM, Shah SH, Arlotto M, Slentz CA, et al:
A branched-chain amino acid-related metabolic signature that
differentiates obese and lean humans and contributes to insulin
resistance. Cell Metab. 9:311–326. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Wang Q, Holmes MV, Davey Smith G and
Ala-Korpela M: Genetic support for a causal role of insulin
resistance on circulating branched-chain amino acids and
inflammation. Diabetes Care. 40:1779–1786. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Mahendran Y, Jonsson A, Have CT, Allin KH,
Witte DR, Jørgensen ME, Grarup N, Pedersen O, Kilpeläinen TO and
Hansen T: Genetic evidence of a causal effect of insulin resistance
on branched-chain amino acid levels. Diabetologia. 60:873–878.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Lynch CJ and Adams SH: Branched-chain
amino acids in metabolic signalling and insulin resistance. Nat Rev
Endocrinol. 10:723–736. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Liang Z, Su Z, Yang H, Zheng J, Wu X,
Huang M, Duan L, Chen S, Wei B, Fan X and Lin S: Branched-chain
amino acids in bone health: From molecular mechanisms to
therapeutic potential. Biomed Pharmacother. 192:1186452025.
View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Zhao H, Zhang F, Sun D, Wang X, Zhang X,
Zhang J, Yan F, Huang C, Xie H, Lin C, et al: Branched-Chain amino
acids exacerbate obesity-related hepatic glucose and lipid
metabolic disorders via attenuating Akt2 signaling. Diabetes.
69:1164–1177. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Pereira M, Ko JH, Logan J, Protheroe H,
Kim KB, Tan ALM, Croucher PI, Park KS, Rotival M, Petretto E, et
al: A trans-eQTL network regulates osteoclast multinucleation and
bone mass. Elife. 9:e555492020. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Kim JH and Kim N: Regulation of NFATc1 in
osteoclast differentiation. J Bone Metab. 21:233–241. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Yagi M, Miyamoto T, Sawatani Y, Iwamoto K,
Hosogane N, Fujita N, Morita K, Ninomiya K, Suzuki T, Miyamoto K,
et al: DC-STAMP is essential for cell-cell fusion in osteoclasts
and foreign body giant cells. J Exp Med. 2005. 202:345–351. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Ishii M, Iwai K, Koike M, Ohshima S,
Kudo-Tanaka E, Ishii T, Mima T, Katada Y, Miyatake K, Uchiyama Y
and Saeki Y: RANKL-induced expression of tetraspanin CD9 in lipid
raft membrane microdomain is essential for cell fusion during
osteoclastogenesis. J Bone Miner Res. 21:965–976. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Singha UK, Jiang Y, Yu S, Luo M, Lu Y,
Zhang J and Xiao G: Rapamycin inhibits osteoblast proliferation and
differentiation in MC3T3-E1 cells and primary mouse bone marrow
stromal cells. J Cell Biochem. 103:434–446. 2008. View Article : Google Scholar
|
|
122
|
Han HS, Ahn E, Park ES, Huh T, Choi S,
Kwon Y, Choi BH, Lee J, Choi YH, Jeong YL, et al: Impaired BCAA
catabolism in adipose tissues promotes age-associated metabolic
derangement. Nat Aging. 3:982–1000. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Chen A, Jin J, Cheng S, Liu Z, Yang C,
Chen Q, Liang W, Li K, Kang D, Ouyang Z, et al: mTORC1 induces
plasma membrane depolarization and promotes preosteoblast
senescence by regulating the sodium channel Scn1a. Bone Res.
10:252022. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Gayatri MB, Gajula NN, Chava S and Reddy
ABM: High glutamine suppresses osteogenesis through mTORC1-mediated
inhibition of the mTORC2/AKT-473/RUNX2 axis. Cell Death Discov.
8:2772022. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Arany Z and Neinast M: Branched chain
amino acids in metabolic disease. Curr Diab Rep. 18:762018.
View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Yoon MS: The emerging role of
branched-chain amino acids in insulin resistance and metabolism.
Nutrients. 8:4052016. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Zhou M, Shao J, Wu CY, Shu L, Dong W, Liu
Y, Chen M, Wynn RM, Wang J, Wang J, et al: Targeting BCAA
Catabolism to Treat Obesity-Associated Insulin Resistance.
Diabetes. 68:1730–1746. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Zhou C, Zhang J, Liu Q, Guo Y, Li M, Tao
J, Peng S, Li R, Deng X, Zhang G and Liu H: Role of amino acid
metabolism in osteoporosis: Effects on the bone microenvironment
and treatment strategies (Review). Mol Med Rep. 32:2122025.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Lerin C, Goldfine AB, Boes T, Liu M, Kasif
S, Dreyfuss JM, De Sousa-Coelho AL, Daher G, Manoli I, Sysol JR, et
al: Defects in muscle branched-chain amino acid oxidation
contribute to impaired lipid metabolism. Mol Metab. 5:926–936.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
White PJ, Lapworth AL, An J, Wang L,
McGarrah RW, Stevens RD, Ilkayeva O, George T, Muehlbauer MJ, Bain
JR, et al: Branched-chain amino acid restriction in Zucker-fatty
rats improves muscle insulin sensitivity by enhancing efficiency of
fatty acid oxidation and acyl-glycine export. Mol Metab. 5:538–551.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Jian H, Xu Q, Wang X, Liu Y, Miao S, Li Y,
Mou T, Dong X and Zou X: Amino acid and fatty acid metabolism
disorders trigger oxidative stress and inflammatory response in
excessive dietary valine-induced NAFLD of laying hens. Front Nutr.
9:8497672022. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Ye Z, Wang S, Zhang C and Zhao Y:
Coordinated modulation of energy metabolism and inflammation by
branched-chain amino acids and fatty acids. Front Endocrinol
(Lausanne). 11:6172020. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Surugihalli C, Muralidaran V, Ryan CE,
Patel K, Zhao D and Sunny NE: Branched-chain amino acids alter
cellular redox to induce lipid oxidation and reduce de novo
lipogenesis in the liver. Am J Physiol Endocrinol Metab.
324:E299–E313. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Lin S, Miao Y, Zheng X, Dong Y, Yang Q,
Yang Q, Du S, Xu J, Zhou S and Yuan T: ANGPTL4 negatively regulates
the progression of osteosarcoma by remodeling branched-chain amino
acid metabolism. Cell Death Discov. 8:2252022. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Rachner TD, Khosla S and Hofbauer LC:
Osteoporosis: Now and the future. Lancet. 377:1276–1287. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Riggs BL, Wahner HW, Seeman E, Offord KP,
Dunn WL, Mazess RB, Johnson KA and Melton LJ III: Changes in bone
mineral density of the proximal femur and spine with aging.
Differences between the postmenopausal and senile osteoporosis
syndromes. J Clin Invest. 70:716–723. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Wang LT, Chen LR and Chen KH:
Hormone-related and drug-induced osteoporosis: A cellular and
molecular overview. Int J Mol Sci. 24:58142023. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Wu D, Cline-Smith A, Shashkova E, Perla A,
Katyal A and Aurora R: T-cell mediated inflammation in
postmenopausal osteoporosis. Front Immunol. 12:6875512021.
View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Bruyère O, Malaise O, Neuprez A, Collette
J and Reginster JY: Prevalence of vitamin D inadequacy in European
postmenopausal women. Curr Med Res Opin. 23:1939–1944. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Lee YH, Lim YW, Ling PS, Tan YY, Cheong M
and Lam KS: Inadequate dietary calcium intake in elderly patients
with hip fractures. Singapore Med J. 48:1117–1121. 2007.PubMed/NCBI
|
|
141
|
Nieves JW: Osteoporosis: The role of
micronutrients. Am J Clin Nutr. 81:1232S–1239S. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Hu M, Xing L, Zhang L, Liu F, Wang S, Xie
Y, Wang J, Jiang H, Guo J, Li X, et al: NAP1L2 drives mesenchymal
stem cell senescence and suppresses osteogenic differentiation.
Aging Cell. 21:e135512022. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Xue Y, Hu S, Chen C, He J, Sun J, Jin Y,
Zhang Y, Zhu G, Shi Q and Rui Y: Myokine Irisin promotes
osteogenesis by activating BMP/SMAD signaling via αV integrin and
regulates bone mass in mice. Int J Biol Sci. 18:572–584. 2022.
View Article : Google Scholar :
|
|
144
|
Mi B, Yan C, Xue H, Chen L, Panayi AC, Hu
L, Hu Y, Cao F, Sun Y, Zhou W, et al: Inhibition of circulating
miR-194-5p reverses osteoporosis through Wnt5a/β-catenin-dependent
induction of osteogenic differentiation. Mol Ther Nucleic Acids.
21:814–823. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Futai M, Sun-Wada GH, Wada Y, Matsumoto N
and Nakanishi-Matsui M: Vacuolar-type ATPase: A proton pump to
lysosomal trafficking. Proc Jpn Acad Ser B Phys Biol Sci.
95:261–277. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Shen S, Si M, Zeng C, Liu EK, Chen Y,
Vacher J, Zhao H, Mohan S and Xing W: Leucine repeat rich kinase 1
controls osteoclast activity by managing lysosomal trafficking and
secretion. Biology (Basel). 12:5112023.PubMed/NCBI
|
|
147
|
Li MCM, Chow SKH, Wong RMY, Qin L and
Cheung WH: The role of osteocytes-specific molecular mechanism in
regulation of mechanotransduction - A systematic review. J Orthop
Translat. 29:1–9. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Vasiliadis ES, Evangelopoulos DS, Kaspiris
A, Benetos IS, Vlachos C and Pneumaticos SG: The role of sclerostin
in bone diseases. J Clin Med. 11:8062022. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Mann G, Mora S, Madu G and Adegoke OAJ:
Branched-chain amino acids: Catabolism in skeletal muscle and
implications for muscle and whole-body metabolism. Front Physiol.
12:7028262021. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Hatazawa Y, Tadaishi M, Nagaike Y, Morita
A, Ogawa Y, Ezaki O, Takai-Igarashi T, Kitaura Y, Shimomura Y,
Kamei Y and Miura S: PGC-1α-mediated branched-chain amino acid
metabolism in the skeletal muscle. PLoS One. 9:e910062014.
View Article : Google Scholar
|
|
151
|
Lv Z, Shi W and Zhang Q: Role of essential
amino acids in age-induced bone loss. Int J Mol Sci. 23:112812022.
View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Takegahara N, Kim H and Choi Y: Unraveling
the intricacies of osteoclast differentiation and maturation:
Insight into novel therapeutic strategies for bone-destructive
diseases. Exp Mol Med. 56:264–272. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Liang Y, Cardoso FF, Parys C, Cardoso FC
and Loor JJ: Branched-Chain amino acid supplementation alters the
abundance of mechanistic target of rapamycin and insulin signaling
proteins in subcutaneous adipose explants from lactating holstein
cows. Animals (Basel). 11:27142021. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Kim JM, Yang YS, Hong J, Chaugule S, Chun
H, van der Meulen MCH, Xu R, Greenblatt MB and Shim JH: Biphasic
regulation of osteoblast development via the ERK MAPK-mTOR pathway.
Elife. 11:e780692022. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Carbone L, Bůžková P, Fink HA, Robbins JA,
Barzilay JI, Elam RE, Isales C, Connelly MA and Mukamal KJ: Plasma
levels of branched chain amino acids, incident hip fractures, and
bone mineral density of the hip and spine. J Clin Endocrinol Metab.
108:e1358–e1364. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Urano T, Kuroda T, Uenishi K and Shiraki
M: Serum branched-chain amino acid levels are associated with
fracture risk in Japanese women. Geriatr Gerontol Int. 24:603–608.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Plotkin DL, Delcastillo K, Van Every DW,
Tipton KD, Aragon AA and Schoenfeld BJ: Isolated leucine and
branched-chain amino acid supplementation for enhancing muscular
strength and hypertrophy: A narrative review. Int J Sport Nutr
Exerc Metab. 31:292–301. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Cereda E, Pisati R, Rondanelli M and
Caccialanza R: Whey protein, leucine- and vitamin-D-enriched oral
nutritional supplementation for the treatment of sarcopenia.
Nutrients. 14:15242022. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Ely IA, Phillips BE, Smith K, Wilkinson
DJ, Piasecki M, Breen L, Larsen MS and Atherton PJ: A focus on
leucine in the nutritional regulation of human skeletal muscle
metabolism in ageing, exercise and unloading states. Clin Nutr.
42:1849–1865. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Kitajima Y, Takahashi H, Akiyama T,
Murayama K, Iwane S, Kuwashiro T, Tanaka K, Kawazoe S, Ono N,
Eguchi T, et al: Supplementation with branched-chain amino acids
ameliorates hypoalbuminemia, prevents sarcopenia, and reduces fat
accumulation in the skeletal muscles of patients with liver
cirrhosis. J Gastroenterol. 53:427–437. 2018. View Article : Google Scholar
|
|
161
|
Wang S, Guo W and Dong R: Unraveling the
transcriptomic effects of leucine supplementation on muscle growth
and performance in basketball athletes. PLoS One. 20:e03166032025.
View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Dong Y, Yuan H, Ma G and Cao H:
Bone-muscle crosstalk under physiological and pathological
conditions. Cell Mol Life Sci. 81:3102024. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Watanabe-Takano H, Ochi H, Chiba A, Matsuo
A, Kanai Y, Fukuhara S, Ito N, Sako K, Miyazaki T, Tainaka K, et
al: Mechanical load regulates bone growth via periosteal osteocrin.
Cell Rep. 36:1093802021. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Klein-Nulend J, van Oers RF, Bakker AD and
Bacabac RG: Nitric oxide signaling in mechanical adaptation of
bone. Osteoporos Int. 25:1427–1437. 2014.
|
|
165
|
Holmes D: Bone: Irisin boosts bone mass.
Nat Rev Endocrinol. 11:6892015.
|
|
166
|
Sheng R, Cao M, Song M, Wang M, Zhang Y,
Shi L, Xie T, Li Y, Wang J and Rui Y: Muscle-bone crosstalk via
endocrine signals and potential targets for osteosarcopenia-related
fracture. J Orthop Translat. 43:36–46. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Zhang L, Guo Q, Duan Y, Wang W, Yang Y and
Yin Y, Gong S, Han M, Li F and Yin Y: Potential nutritional
healthy-aging strategy: Enhanced protein metabolism by balancing
branched-chain amino acids in a finishing pig model. Food Funct.
13:6217–6232. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Ikeda T, Matsunaga Y, Kanbara M, Kamono A,
Masuda T, Watanabe M, Nakanishi R and Jinno T: Effect of exercise
therapy combined with branched-chain amino acid supplementation on
muscle strength in elderly women after total hip arthroplasty: A
randomized controlled trial. Asia Pac J Clin Nutr. 28:720–726.
2019.PubMed/NCBI
|
|
169
|
Huynh H and Wan Y: mTORC1 impedes
osteoclast differentiation via calcineurin and NFATc1. Commun Biol.
1:292018. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Ozaki K, Yamada T, Horie T, Ishizaki A,
Hiraiwa M, Iezaki T, Park G, Fukasawa K, Kamada H, Tokumura K, et
al: The L-type amino acid transporter LAT1 inhibits
osteoclastogenesis and maintains bone homeostasis through the
mTORC1 pathway. Sci Signal. 12:eaaw39212019. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Rivera CN, Watne RM, Wommack AJ and
Vaughan RA: The effect of insulin resistance on extracellular BCAA
accumulation and SLC25A44 expression in a myotube model of skeletal
muscle insulin resistance. Amino Acids. 55:1701–1705. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
172
|
da Silva FMO, Pimenta AM, Juvanhol LL,
Hermsdorff HHM and Bressan J: Obesity incidence according to
branched-chain amino acid intake and plant-based diet index among
Brazilian adults: A six-year follow-up of the CUME study.
Nutrients. 17:2272025. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Holeček M: The role of skeletal muscle in
the pathogenesis of altered concentrations of branched-chain amino
acids (valine, leucine, and isoleucine) in liver cirrhosis,
diabetes, and other diseases. Physiol Res. 70:293–305. 2021.
View Article : Google Scholar
|
|
174
|
You Y, Leng S, Shi J, Yang H, Chang M, Ma
Q, Zhang D, Sun H, Wang L, Gao Z, et al: Integration of
bone-targeted delivery and crosstalk modulation of liver-bone axis
for improved osteoporosis therapy. ACS Nano. 19:23955–23968. 2025.
View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Zuo X, Zhao R, Wu M, Wang Y, Wang S, Tang
K, Wang Y, Chen J, Yan X, Cao Y and Li T: Multi-omic profiling of
sarcopenia identifies disrupted branched-chain amino acid
catabolism as a causal mechanism and therapeutic target. Nat Aging.
5:419–436. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Tilg H and Moschen AR: Adipocytokines:
Mediators linking adipose tissue, inflammation and immunity. Nat
Rev Immunol. 6:772–783. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Olson OC, Quail DF and Joyce JA: Obesity
and the tumor microenvironment. Science. 358:1130–1131. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Jarvis SE, Nguyen M and Malik VS:
Association between adherence to plant-based dietary patterns and
obesity risk: A systematic review of prospective cohort studies.
Appl Physiol Nutr Metab. 47:1115–1133. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Singh L, Tyagi S, Myers D and Duque G:
Good, bad, or ugly: The biological roles of bone marrow fat. Curr
Osteoporos Rep. 16:130–137. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Bo T and Fujii J: Primary roles of
branched chain amino acids (BCAAs) and their metabolism in
physiology and metabolic disorders. Molecules. 30:562024.
View Article : Google Scholar
|
|
181
|
Habibi M, Shili CN, Sutton J, Goodarzi P
and Pezeshki A: Dietary branched-chain amino acids modulate the
dynamics of calcium absorption and reabsorption in
protein-restricted pigs. J Anim Sci Biotechnol. 13:152022.
View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Salem A, Ben Maaoui K, Jahrami H,
AlMarzooqi MA, Boukhris O, Messai B, Clark CCT, Glenn JM, Ghazzaoui
HA, Bragazzi NL, et al: Attenuating muscle damage biomarkers and
muscle soreness after an exercise-induced muscle damage with
branched-chain amino acid (BCAA) supplementation: A systematic
review and meta-analysis with meta-regression. Sports Med Open.
10:422024. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Choi BH, Hyun S and Koo SH: The role of
BCAA metabolism in metabolic health and disease. Exp Mol Med.
56:1552–1559. 2024. View Article : Google Scholar : PubMed/NCBI
|