|
1
|
Rogers MP and Kuo PC: Pain as the fifth
vital sign. J Am Coll Surg. 231:601–602. 2020. View Article : Google Scholar
|
|
2
|
Carroll CP and Brandow AM: Chronic pain:
Prevalence and management. Hematol Oncol Clin North Am.
36:1151–1165. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ushida T: Chronic pain:
Definition/conception/classification of pain. Brain Nerve.
75:201–205. 2023.In Japanese. PubMed/NCBI
|
|
4
|
Raja SN, Carr DB, Cohen M, Finnerup NB,
Flor H, Gibson S, Keefe FJ, Mogil JS, Ringkamp M, Sluka KA, et al:
The revised international association for the study of pain
definition of pain: Concepts, challenges, and compromises. Pain.
161:1976–1982. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Peters ML: Emotional and cognitive
influences on pain experience. Mod Trends Pharmacopsychiatry.
30:138–152. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cohen SP, Vase L and Hooten WM: Chronic
pain: An update on burden, best practices, and new advances.
Lancet. 397:2082–2097. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Patel EA and Perloff MD: Radicular pain
syndromes: Cervical, lumbar, and spinal stenosis. Semin Neurol.
38:634–639. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ashburn MA and Fine PG: Persistent pain
following trauma. Mil Med. 154:86–89. 2020. View Article : Google Scholar
|
|
9
|
Roicke H, Köhler W, Baum P and Krasselt M:
Non-inflammatory muscle pain. Dtsch Med Wochenschr. 145:887–894.
2020.In German. PubMed/NCBI
|
|
10
|
Ford AC, Vanner S, Kashyap PC and Nasser
Y: Chronic visceral pain: new peripheral mechanistic insights and
resulting treatments. Gastroenterology. 166:976–994. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Finnerup NB, Kuner R and Jensen TS:
Neuropathic pain: From mechanisms to treatment. Physiol Rev.
101:259–301. 2021. View Article : Google Scholar
|
|
12
|
Erpelding N and Borsook D: Capturing brain
metrics of neuropathic pain using nuclear magnetic resonance. Pain
Manag. 3:395–409. 2013. View Article : Google Scholar
|
|
13
|
Scheuren PS, Rosner J, Curt A and Hubli M:
Pain-autonomic interaction: A surrogate marker of central
sensitization. Eur J Pain. 24:2015–2026. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hawker GA, Mian S, Kendzerska T and French
M: Measures of adult pain: Visual analog scale for pain (VAS pain),
numeric rating scale for pain (NRS pain), McGill pain questionnaire
(MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain
grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS),
and measure of intermittent and constant osteoarthritis pain
(ICOAP). Arthritis Care Res (Hoboken). 63(Suppl 11): S240–S252.
2011. View Article : Google Scholar
|
|
15
|
Weigl M, Letzel J and Angst F: Prognostic
factors for the improvement of pain and disability following
multidisciplinary rehabilitation in patients with chronic neck
pain. BMC Musculoskelet Disord. 22:3302021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rutter-Locher Z, Kirkham BW, Bannister K,
Bennett DL, Buckley CD, Taams LS and Denk F: An interdisciplinary
perspective on peripheral drivers of pain in rheumatoid arthritis.
Nat Rev Rheumatol. 20:671–682. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Todd A, McNamara CL, Balaj M, Huijts T,
Akhter N, Thomson K, Kasim A, Eikemo TA and Bambra C: The European
epidemic: Pain prevalence and socioeconomic inequalities in pain
across 19 European countries. Eur J Pain. 23:1425–1436. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ito A and Yoshimura M: Mechanisms of the
analgesic effect of calcitonin on chronic pain by alteration of
receptor or channel expression. Mol Pain. 13:17448069177203162017.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bannister K, Sachau J, Baron R and
Dickenson AH: Neuropathic pain: Mechanism-based therapeutics. Annu
Rev Pharmacol Toxicol. 60:257–274. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang R, Han L, Gao Q, Chen D, Wang Y,
Zhang X, Yu X, Zhang Y, Li Z and Bai C: Progress on active
analgesic components and mechanisms of commonly used traditional
Chinese medicines: A comprehensive review. J Pharm Pharm Sci.
21:437–480. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Boscan P, Monnet E, Mama K, Twedt DC,
Congdon J, Eickhoff JC and Steffey EP: A dog model to study ovary,
ovarian ligament and visceral pain. Vet Anaesth Analg. 38:260–266.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
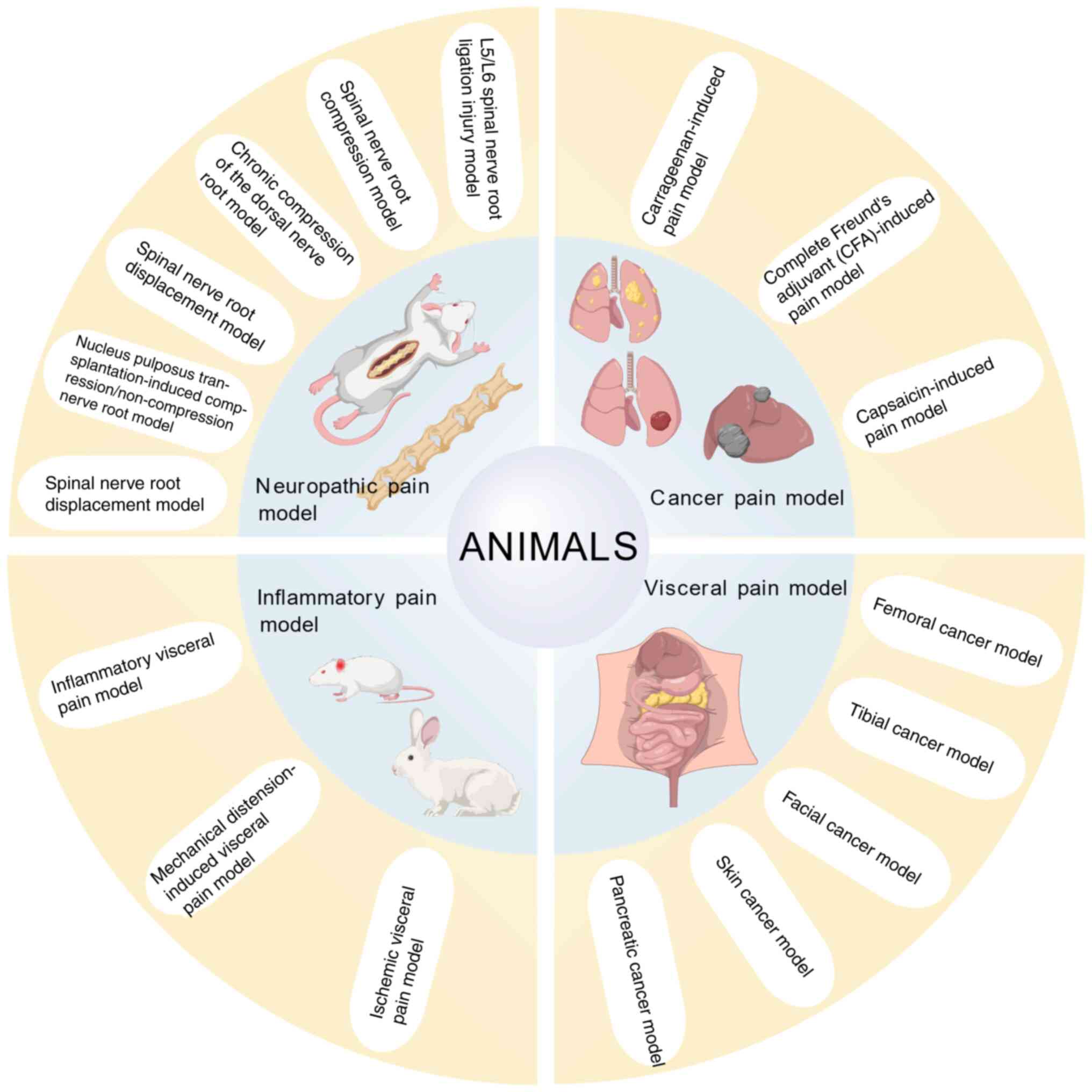
Mogil JS: Animal models of pain: Progress
and challenges. Nat Rev Neurosci. 10:283–294. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Milinkeviciute G, Gentile C and Neely GG:
Drosophila as a tool for studying the conserved genetics of pain.
Clin Genet. 82:359–366. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bao WD, Volgin AD, Alpyshov ET, Friend AJ,
Strekalova TV, de Abreu MS, Collins C, Amstislavskaya TG, Demin KA
and Kalueff AV: Opioid neurobiology, neurogenetics and
neuropharmacology in zebrafish. Neuroscience. 404:218–232. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chaplan SR, Bach FW, Pogrel JW, Chung JM
and Yaksh TL: Quantitative assessment of tactile allodynia in the
rat paw. J Neurosci Methods. 53:55–63. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hargreaves K, Dubner R, Brown F, Flores C
and Joris J: A new and sensitive method for measuring thermal
nociception in cutaneous hyperalgesia. Pain. 32:77–88. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gunn A, Bobeck EN, Weber C and Morgan MM:
The influence of non-nociceptive factors on hot-plate latency in
rats. J Pain. 12:222–227. 2011. View Article : Google Scholar
|
|
28
|
Wang JS, Chen B, Li MY, Zhao X and Guo Y:
Animal models and analgesia mechanism analysis commonly used of
acupuncture analgesia. Liaoning J Tradit Chin Med. 44:435–438.
2017.In Chinese.
|
|
29
|
Ho Kim S and Mo Chung J: An experimental
model for peripheral neuropathy produced by segmental spinal nerve
ligation in the rat. Pain. 50:355–363. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang JS and Li BF: Choice and
establishment of mirror-image pain model of selective spinal nerve
ligation in rats. Med Innov China. 11:30–32. 2014.In Chinese.
|
|
31
|
Chung JM, Kim HK and Chung KS: Segmental
spinal nerve ligation model of neuropathic pain. Methods Mol Med.
99:35–45. 2004.PubMed/NCBI
|
|
32
|
Huang YG, Zhang Q, Wu H and Zhang CQ: A
comparison of surgical invasions for spinal nerve ligation with or
without paraspinal muscle removal in a rat neuropathic pain model.
Biomed Res Int. 2016:67412952016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wang YJ, Wan C, Shen PZ, Wang HB, Shi YY
and Shi Q: A model study of experimental lumbar nerve root
compression. Chin J Tradit Med Traumatol Orthop. 7:9–12. 1999.In
Chinese.
|
|
34
|
Xue F, Wei Y, Chen Y, Wang Y and Gao L: A
rat model for chronic spinal nerve root compression. Eur Spine J.
23:435–446. 2014. View Article : Google Scholar :
|
|
35
|
Zhang Y, Zhao D, Li X, Gao B, Sun C, Zhou
S, Ma Y, Chen X and Xu D: The Wnt/β-Catenin pathway regulated
cytokines for pathological neuropathic pain in chronic compression
of dorsal root ganglion model. Neural Plast. 2021:66801922021.
View Article : Google Scholar
|
|
36
|
Lin ZG, Jiang SC, Cheng YB, Song PF and
Fang M: Experimental study of Tuina on DRG neurons P2X3 receptor of
lumbar disc herniation rats. Chin Arch Tradit Chin Med.
35:2475–2479. 2017.In Chinese.
|
|
37
|
Finskas O, Blixt A, Fujioka Y and Olmarker
K: New, clinically more relevant model for nerve root injury in the
rat. Spine (Phila Pa 1976). 38:1744–1748. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lai A, Moon A, Purmessur D, Skovrlj B,
Laudier DM, Winkelstein BA, Cho SK, Hecht AC and Iatridis JC:
Annular puncture with tumor necrosis factor-alpha injection
enhances painful behavior with disc degeneration in vivo. Spine J.
16:420–431. 2016. View Article : Google Scholar :
|
|
39
|
Shamji MF, Allen KD, So S, Jing L, Adams
SB Jr, Schuh R, Huebner J, Kraus VB, Friedman AH, Setton LA and
Richardson WJ: Gait abnormalities and inflammatory cytokines in an
autologous nucleus pulposus model of radiculopathy. Spine (Phila Pa
1976). 34:648–654. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kim SJ, Park SM, Cho YW, Jung YJ, Lee DG,
Jang SH, Park HW, Hwang SJ and Ahn SH: Changes in expression of
mRNA for interleukin-8 and effects of interleukin-8 receptor
inhibitor in the spinal dorsal horn in a rat model of lumbar disc
herniation. Spine (Phila Pa 1976). 36:2139–2146. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhang JJ, Song W, Luo WY, Wei M, Sun LB,
Zou XN and Liao WM: Autologous nucleus pulposus transplantation to
lumbar 5 dorsal root ganglion after epineurium dissection in rats:
A modified model of non-compressive lumbar herniation. Chin Med J
(Engl). 124:2009–2014. 2011.PubMed/NCBI
|
|
42
|
Cho HK, Ahn SH, Kim SY, Choi MJ, Hwang SJ
and Cho YW: Changes in the expressions of Iba1 and calcitonin
gene-related peptide in adjacent lumbar spinal segments after
lumbar disc herniation in a rat model. J Korean Med Sci.
30:1902–1910. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Zhao CP, Zhu ML, Wang TT, Liu XL and Liu
CL: A chemical radiculitis model in the rat: Establishment and
evaluation. Chin J Tissue Eng Res. 23:1030–1034. 2019.In
Chinese.
|
|
44
|
Zhang JJ, Wei M, Lai YR, Sun LB and Liao
WM: Non-compressive effect on ultra-structural changes in the
dorsal root ganglion following autograft of nucleus pulposus in
rats. Chin J Nerv Ment Dis. 35:280–284. 2009.In Chinese.
|
|
45
|
Bennett GJ and Xie YK: A peripheral
mononeuropathy in rat that produces disorders of pain sensation
like those seen in man. Pain. 33:87–107. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Zhang G, Liu N, Zhu C, Ma L, Yang J, Du J,
Zhang W, Sun T, Niu J and Yu J: Antinociceptive effect of
isoorientin against neuropathic pain induced by the chronic
constriction injury of the sciatic nerve in mice. Int
Immunopharmacol. 75:1057532019. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Zhu CY, Xu QH, Mao ZY and Lin N:
Application of three artemisinin derivatives in neuropathic pain:
Evaluating co-curation of nociceptive and emotional syndromes in
spinal cord ligation mice. Zhongguo Zhong Yao Za Zhi. 43:3058–3063.
2018.In Chinese. PubMed/NCBI
|
|
48
|
Meng K and Wang Y: Effect of BMP7 on
neuropathic pain in rats with spinal cord injury. Chin J Pain Med.
26:174–179. 2020.In Chinese.
|
|
49
|
Shih HC, Kuan YH and Shyu BC: Targeting
brain-derived neurotrophic factor in the medial thalamus for the
treatment of central poststroke pain in a rodent model. Pain.
158:1302–1313. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Lu HF, Xu CY, Zhang L, Gan L, Chen C, Yan
MY, Guo XN, Fang Q, Xu GY, Zhang YB, et al: A new central
post-stroke pain rat model: Autologous blood injected thalamic
hemorrhage involved increased expression of P2X4 receptor. Neurosci
Lett. 687:124–130. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Li Y, Jiao H, Ren W and Ren F: TRESK
alleviates trigeminal neuralgia induced by infraorbital nerve
chronic constriction injury in rats. Mol Pain.
15:17448069198825112019. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Cao Y, Wang H, Chiang CY, Dostrovsky JO
and Sessle BJ: Pregabalin suppresses nociceptive behavior and
central sensitization in a rat trigeminal neuropathic pain model. J
Pain. 14:193–204. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Bennett MI, Kaasa S, Barke A, Korwisi B,
Rief W and Treede RD: IASP Taskforce for the Classification of
Chronic Pain: The IASP classification of chronic pain for ICD-11:
Chronic cancer-related pain. Pain. 160:38–44. 2019. View Article : Google Scholar
|
|
54
|
Luger NM, Mach DB, Sevcik MA and Mantyh
PW: Bone cancer pain: From model to mechanism to therapy. J Pain
Symptom Manage. 29(5 Suppl): S32–4S6. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Currie GL, Delaney A, Bennett MI,
Dickenson AH, Egan KJ, Vesterinen HM, Sena ES, Macleod MR, Colvin
LA and Fallon MT: Animal models of bone cancer pain: systematic
review and meta-analyses. Pain. 54:917–926. 2013. View Article : Google Scholar
|
|
56
|
He XX: Study on the mechanism of
autophagy-NLRP3 inflammasome pathway in the relief of bone cancer
pain by electroacupuncture. China Three Gorges University; 2023, In
Chinese.
|
|
57
|
Fan SD: Role of NRG1/ErbB2 signal pathway
in electroacupunture treating cancer pain. Shanghai Univ Tradit
Chin Med; 2020, In Chinese.
|
|
58
|
Kopruszinski CM, Dos Reis RC, Gambeta E,
Acco A, Rae GA, King T and Chichorro JG: Blockade of endothelin
receptors reduces tumor-induced ongoing pain and evoked
hypersensitivity in a rat model of facial carcinoma induced pain.
Eur J Pharmacol. 818:132–140. 2018. View Article : Google Scholar
|
|
59
|
Kopruszinski CM, Dos Reis RC, Rae GA and
Chichorro JG: Blockade of peripheral endothelin receptors abolishes
heat hyperalgesia and spontaneous nociceptive behavior in a rat
model of facial cancer. Arch Oral Biol. 97:231–237. 2019.
View Article : Google Scholar
|
|
60
|
Gambeta E, Kopruszinski CM, Reis RC,
Zanoveli JM and Chichorro JG: Evaluation of heat hyperalgesia and
anxiety like-behaviors in a rat model of orofacial cancer. Neurosci
Lett. 619:100–105. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Gambeta E, Kopruszinski CM, Reis RC,
Zanoveli JM and Chichorro JG: Facial pain and anxiety-like behavior
are reduced by pregabalin in a model of facial carcinoma in rats.
Neuropharmacology. 125:263–271. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Guo TT, Wumaier TA, Hu JJ and Yang LL:
Analysis of the prognosis of cutaneous melanoma and its influencing
factors. Oncol Prog. 22:141–145. 2024.In Chinese.
|
|
63
|
Olbrich K, Costard L, Moser CV, Syhr KM,
King-Himmelreich TS, Wolters MC, Schmidtko A, Geisslinger G and
Niederberger E: Cleavage of SNAP-25 ameliorates cancer pain in a
mouse model of melanoma. Eur J Pain. 21:101–111. 2017. View Article : Google Scholar
|
|
64
|
Wang H, Shao DH and Ma P: Analgesic effect
of gastrodin on metastasizing in cancer-induced pain mouse model. J
Jiangsu Univ (Med Ed). 25:195–198. 2015.In Chinese.
|
|
65
|
Xie R and Wang H: Effect of intrathecal
amiloride on the ASIC-3 expression and pain behavior in mice skin
cancer pain. Chin Clin Oncol. 22:588–591. 2017.In Chinese.
|
|
66
|
Tabata M, Murata E, Ueda K, Kato-Kogoe N,
Kuroda Y and Hirose M: Effects of TrkA inhibitory peptide on
cancer-induced pain in a mouse melanoma model. J Anesth.
26:545–551. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Yan ZL, Xu XF, Xin JQ and Zhang H:
Comparison and selection of animal models of pancreatic cancer. J
Clin Hepatol. 38:2908–2912. 2022.In Chinese.
|
|
68
|
Mallya K, Gautam SK, Aithal A, Batra SK
and Jain M: Modeling pancreatic cancer in mice for experimental
therapeutics. Biochim Biophys Acta Rev Cancer. 1876:1885542021.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Xu D and Yang F: Current state and future
perspectives of biological models in pancreatic cancer. Lab Anim
Sci. 40:76–82. 2023.In Chinese.
|
|
70
|
Hu RP, Shang LF, Wang HJ, Che HX, Wang ML,
Yang H, Jin YY, Zhang FF and Zhang JL: Mechanism of effect of
rosiglitazone on pancreatic cancer in diabetic mice based on impact
of PPARγ on glucose transport and metabolism. Chin Pharmacol Bull.
40:1325–1334. 2024.In Chinese.
|
|
71
|
Xu Y, Huang X, Tang Z, Li R and Qin W:
Establishment and in vivo imaging observation of a nude mouse model
of type 2 diabetes mellitus and pancreatic cancer. J Clin Hepatol.
40:1231–1239. 2024.In Chinese.
|
|
72
|
Schwei MJ, Honore P, Rogers SD,
Salak-Johnson JL, Finke MP, Ramnaraine ML, Clohisy DR and Mantyh
PW: Neurochemical and cellular reorganization of the spinal cord in
a murine model of bone cancer pain. J Neurosci. 19:10886–10897.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Wang W, Jiang Q, Wu J, Tang W and Xu M:
Upregulation of bone morphogenetic protein 2 (Bmp2) in dorsal root
ganglion in a rat model of bone cancer pain. Mol Pain.
15:17448069188242502019. View Article : Google Scholar :
|
|
74
|
Huang HQ, Liu YP, Wu X and He XM:
Establishment of a rat model of skin cancer pain. J Zhengzhou Univ
(Med Sci). 54:236–240. 2019.In Chinese.
|
|
75
|
Wang L, Xu H, Ge Y, Zhu H, Yu D, Yu W and
Lu Z: Establishment of a murine pancreatic cancer pain model and
microarray analysis of pain associated genes in the spinal cord
dorsal horn. Mol Med Rep. 16:4429–4436. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Grundy L, Erickson A and Brierley SM:
Visceral pain. Annu Rev Physiol. 81:261–284. 2019. View Article : Google Scholar
|
|
77
|
Ayoub R, Jarrar Q, Ali D, Moshawih S,
Jarrar Y, Hakim M and Zakaria Z: Synthesis of mefenamic acid with
pronounced anti-nociceptive effects and a proposed activity on
GABA, opioid and glutamate receptors. Eur J Pharm Sci.
163:1058652021. View Article : Google Scholar
|
|
78
|
Vasincu IM, Apotrosoaei M, Constantin S,
Butnaru M, Vereștiuc L, Lupușoru CE, Buron F, Routier S, Lupașcu D,
Taușer RG and Profire L: New ibuprofen derivatives with
thiazolidine-4-one scaffold with improved pharmaco-toxicological
profile. BMC Pharmacol Toxicol. 22:102021. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Liu X, Zhang Q, Han M and Du J:
Intrapericardial capsaicin and bradykinin induce different
cardiac-somatic and cardiovascular reflexes in rats. Auton
Neurosci. 198:28–32. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
McDermott DA, Meller ST, Gebhart GF and
Gutterman DD: Use of an indwelling catheter for examining
cardiovascular responses to pericardial administration of
bradykinin in rat. Cardiovasc Res. 30:39–46. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Cen Y, Liu C, Li X, Yan Z, Kuang M, Su Y,
Pan X, Qin R, Liu X, Zheng J and Zhou H: Artesunate ameliorates
severe acute pancreatitis (SAP) in rats by inhibiting expression of
pro-inflammatory cytokines and Toll-like receptor 4. Int
Immunopharmacol. 38:252–260. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Yang JJ, Zhang D and Chen JY: Advances in
animal models of acute pancreatitis. Med J Chin PLA. 44:984–990.
2019.In Chinese.
|
|
83
|
Wang YT and Lv GW: A model of formalin
induced acute visceral inflammatory pain. Chin J Appl Physiol.
15:372–376. 1999.In Chinese.
|
|
84
|
Ness TJ and Gebhart GF: Characterization
of neuronal responses to noxious visceral and somatic stimuli in
the medial lumbosacral spinal cord of the rat. J Neurophysiol.
57:1867–1892. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Wirtz S, Popp V, Kindermann M, Gerlach K,
Weigmann B, Fichtner-Feigl S and Neurath MF: Chemically induced
mouse models of acute and chronic intestinal inflammation. Nat
Protoc. 12:1295–1309. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Lu Y, Lin H, Zhang J, Wei J, Sun J and Han
L: Sijunzi Decoction attenuates 2, 4, 6-trinitrobenzene sulfonic
acid (TNBS)-induced colitis in rats and ameliorates TNBS-induced
claudin-2 damage via NF-κB pathway in Caco2 cells. BMC Complement
Altern Med. 17:352017. View Article : Google Scholar
|
|
87
|
Mazor Y, Engelmayer N, Nashashibi H,
Rottenfußer L, Lev S and Binshtok AM: Attenuation of
colitis-induced visceral hypersensitivity and pain by selective
silencing of TRPV1-expressing fibers in rat colon. Inflamm Bowel
Dis. 30:1843–1851. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Weng RX, Chen W, Tang JN, Sun Q, Li M, Xu
X, Zhang PA, Zhang Y, Hu CY and Xu GY: Targeting spinal TRAF6
expression attenuates chronic visceral pain in adult rats with
neonatal colonic inflammation. Mol Pain. 16:17448069209180592020.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Ryu CM, Yu HY, Lee HY, Shin JH, Lee S, Ju
H, Paulson B, Lee S, Kim S, Lim J, et al: Longitudinal intravital
imaging of transplanted mesenchymal stem cells elucidates their
functional integration and therapeutic potency in an animal model
of interstitial cystitis/bladder pain syndrome. Theranostics.
8:5610–5624. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
El-Hamamsy D: Bladder wall injection of
mesenchymal stem cells ameliorates bladder inflammation,
overactivity and nociception in a chemically induced interstitial
cystitis-like rat model. Int Urogynecol J. 30:845–846. 2019.
View Article : Google Scholar
|
|
91
|
Song PH, Chun SY, Chung JW, Kim YY, Lee
HJ, Lee JN, Ha YS, Yoo ES, Kwon TG, Kim J, et al: Comparison of 5
different rat models to establish a standard animal model for
research into interstitial cystitis. Int Neurourol J. 21:163–170.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Sakurai J, Obata K, Ozaki N, Tokunaga A,
Kobayashi K, Yamanaka H, Dai Y, Kondo T, Miyoshi K, Sugiura Y, et
al: Activation of extracellular signal-regulated protein kinase in
sensory neurons after noxious gastric distention and its
involvement in acute visceral pain in rats. Gastroenterology.
134:1094–1103. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Julia V, Mezzasalma T and Buéno L:
Influence of bradykinin in gastrointestinal disorders and visceral
pain induced by acute or chronic inflammation in rats. Dig Dis Sci.
40:1913–1921. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
İlkaya F, Bilge SS, Bozkurt A, Baş DB,
Erdal A, Çiftçioğlu E and Kesim Y: The antinociceptive effect of
intravenous imipramine in colorectal distension-induced visceral
pain in rats: The role of serotonergic and noradrenergic receptors.
Pharmacol Biochem Behav. 122:1–6. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Al-Chaer ED, Kawasaki M and Pasricha PJ: A
new model of chronic visceral hypersensitivity in adult rats
induced by colon irritation during postnatal development.
Gastroenterology. 119:1276–1285. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
An ZY, Tian JF, Zhao X, Zhang MD, Zhang
LJ, Yang XY, Liu LB, Chen LY and Song XT: PET evaluation of
myocardial perfusion function after percutaneous coronary
intervention in patients with chronic total occlusion: A systematic
review and meta-analysis. Scand Cardiovasc J. 58:23021742024.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Wang WW, Lei J and You HJ: Research
progress of experimental animal models of visceral pain. Prog
Biochem Biophys. 49:858–866. 2022.In Chinese.
|
|
98
|
Hu S, Xiao Y, Zhu L, Li L, Hu CY, Jiang X
and Xu GY: Neonatal maternal deprivation sensitizes voltage-gated
sodium channel currents in colon-specific dorsal root ganglion
neurons in rats. Am J Physiol Gastrointest Liver Physiol.
304:G311–G321. 2013. View Article : Google Scholar
|
|
99
|
Barreau F, Ferrier L, Fioramonti J and
Bueno L: New insights in the etiology and pathophysiology of
irritable bowel syndrome: Contribution of neonatal stress models.
Pediatr Res. 62:240–245. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Bondar NP, Lepeshko AA and Reshetnikov VV:
Effects of early-life stress on social and anxiety-like behaviors
in adult mice: Sex-specific effects. Behav Neurol.
2018:15389312018. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Wang C, Sun DF, Sun LJ, Wang YL, Hu LH, Ye
WC, Fang ZJ and Deng Q: The intervention of shrimp head enzymatic
hydrolysate on capsaicin-induced systemic low-grade inflammation
and the structure and function of gut microbiota in mice. Chin J
Microecol. 33:1–9. 2021.In Chinese.
|
|
102
|
Yao JP, Zhao Y, Chen Y, Chen LP, Feng XM,
Li Y and Zhou SY: Effect of electroacupuncture on intestinal
epithelial mucosal barrier function in rats with
diarrhea-predominant irritable bowel syndrome. Zhen Ci Yan Jiu.
45:357–362. 2020.In Chinese. PubMed/NCBI
|
|
103
|
Felice VD, Gibney SM, Gosselin RD, Dinan
TG, O'Mahony SM and Cryan JF: Differential activation of the
prefrontal cortex and amygdala following psychological stress and
colorectal distension in the maternally separated rat.
Neuroscience. 267:252–262. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Wu J, Wang H, Wang JX, Luo YF, Yang Y and
Gong XX: Effects of Dajianzhong decoction on serum IL-6, TNF-α and
IRAK-4 mRNA expression in colon mucosa of chronic inflammatory
visceral pain model rats. J Tradit Chin Med. 59:1592–1596. 2018.In
Chinese.
|
|
105
|
Liu Q, Ko CY, Zheng C, Ye L, Liu B, Gao H,
Huang D and Chou D: Decreased glutamatergic synaptic strength in
the periaqueductal gray contributes to maintenance of visceral pain
in male rats with experimental pancreatitis. Neuroscience.
428:60–69. 2020. View Article : Google Scholar
|
|
106
|
Furuta A, Yamamoto T, Igarashi T, Suzuki
Y, Egawa S and Yoshimura N: Bladder wall injection of mesenchymal
stem cells ameliorates bladder inflammation, overactivity, and
nociception in a chemically induced interstitial cystitis-like rat
model. Int Urogynecol J. 29:1615–1622. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Deng W, Zou H, Qian L, de Souza SC, Chen Q
and Cao S: Stauntonia chinensis injection relieves neuropathic pain
by increasing the expression of PSD-95 and reducing the
proliferation of phagocytic microglia. Ibrain. 10:3–18. 2023.
View Article : Google Scholar
|
|
108
|
Kandhare AD, Raygude KS, Ghosh P, Ghule AE
and Bodhankar SL: Therapeutic role of curcumin in prevention of
biochemical and behavioral aberration induced by alcoholic
neuropathy in laboratory animals. Neurosci Lett. 511:18–22. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Liu YR, Lian KX and Gu XL: Research
progress in mouse models of inflammatory diseases. Chin J Comp Med.
32:120–126. 2022.In Chinese.
|
|
110
|
Ghosh S, Wise LE, Chen Y, Gujjar R,
Mahadevan A, Cravatt BF and Lichtman AH: The monoacylglycerol
lipase inhibitor JZL184 suppresses inflammatory pain in the mouse
carrageenan model. Life Sci. 92:498–505. 2013. View Article : Google Scholar :
|
|
111
|
Wang WJ, Lu J, Huang YR, Niu CS, Ma Q, Hao
HW, Li LM, Wang JR and Tu Y: Influences of electroacupuncture on
content of hypothalamus ENK and spinal OFQ in rats with chronic
inflammatory pain. J Beijing Univ Tradit Chin Med. 33:196–199.
2010.
|
|
112
|
Melo-Carrillo A and Lopez-Avila A: A
chronic animal model of migraine, induced by repeated meningeal
nociception, characterized by a behavioral and pharmacological
approach. Cephalalgia. 33:1096–1105. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Burgos-Vega CC, Quigley LD, Trevisan Dos
Santos G, Yan F, Asiedu M, Jacobs B, Motina M, Safdar N, Yousuf H,
Avona A, et al: Non-invasive dural stimulation in mice: A novel
preclinical model of migraine. Cephalalgia. 39:123–134. 2019.
View Article : Google Scholar :
|
|
114
|
Sufka KJ, Staszko SM, Johnson AP, Davis
ME, Davis RE and Smitherman TA: Clinically relevant behavioral
endpoints in a recurrent nitroglycerin migraine model in rats. J
Headache Pain. 17:402016. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Philpott HT and McDougall JJ: Combatting
joint pain and inflammation by dual inhibition of monoacylglycerol
lipase and cyclooxygenase-2 in a rat model of osteoarthritis.
Arthritis Res Ther. 22:92020. View Article : Google Scholar :
|
|
116
|
Shi X, Yu W, Wang T, Battulga O, Wang C,
Shu Q, Yang X, Liu C and Guo C: Electroacupuncture alleviates
cartilage degradation: Improvement in cartilage biomechanics via
pain relief and potentiation of muscle function in a rabbit model
of knee osteoarthritis. Biomed Pharmacother. 123:1097242020.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Katri A, Dąbrowska A, Löfvall H, Ding M,
Karsdal MA, Andreassen KV, Thudium CS and Henriksen K: Combining
naproxen and a dual amylin and calcitonin receptor agonist improves
pain and structural outcomes in the collagen-induced arthritis rat
model. Arthritis Res Ther. 21:682019. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
He JY, Qin SY, Zheng JQ, Luo S, Xiong ZY
and Yu QQ: Therapeutic effect of total triterpenoids of Chaenomeles
speciosa combined with indomethacin on rheumatoid arthritis induced
by Freund's complete adjuvant in rats. Pharmacol Clin Chin Mater
Med. 40:42–50. 2024.In Chinese.
|
|
119
|
Bai Q, Li HL, Yang JJ, Cheng WG, Lv CH,
Bai SS, Wang ZD, Jin FM and Wang HD: Effect of Yiqi Juanbi formula
on synovial inflammation and the TLR4/MAPKs/NF-κB signaling pathway
in collagen-induced arthritis rats. Chin Tradit Patent Med.
47:590–595. 2025.In Chinese.
|
|
120
|
Koo ST, Park YI, Lim KS, Chung K and Chung
JM: Acupuncture analgesia in a new rat model of ankle sprain pain.
Pain. 99:423–431. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Wu D, Nan LT, Li SS, Yao TY and Yu SQ:
AMPK-mediated analgesic mechanism in rats with carrageenan-induced
inflammatory pain. J Youjiang Med Univ Nationalities. 45:435–438.
2023.In Chinese.
|
|
122
|
Deuis JR, Dvorakova LS and Vetter I:
Methods used to evaluate pain behaviors in rodents. Front Mol
Neurosci. 10:2482017. View Article : Google Scholar
|
|
123
|
Mizoguchi H, Fukumoto K, Sakamoto G, Jin
S, Toyama A, Wang T, Suzumura A and Sato J: Maternal separation as
a risk factor for aggravation of neuropathic pain in later life in
mice. Behav Brain Res. 359:942–949. 2019. View Article : Google Scholar
|
|
124
|
Muralidharan A, Sotocinal SG, Austin JS
and Mogil JS: The influence of aging and duration of nerve injury
on the antiallodynic efficacy of analgesics in laboratory mice.
Pain Rep. 5:e8242020. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Schwartz ES and Gebhart GF: Visceral pain.
Curr Top Behav Neurosci. 20:171–197. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Peng H and Huang D: Advances in pain
assessment methods in rodent models. Chin J Pain Med. 20:505–508.
2014.In Chinese.
|
|
127
|
Su S, Shao J, Zhao Q, Ren X, Cai W, Li L,
Bai Q, Chen X, Xu B, Wang J, et al: MiR-30b attenuates neuropathic
pain by regulating voltage-gated sodium channel Nav1.3 in rats.
Front Mol Neurosci. 10:1262017. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Gomez K, Stratton HJ, Duran P, Loya S,
Tang C, Calderon-Rivera A, François-Moutal L, Khanna M, Madura CL,
Luo S, et al: Identification and targeting of a unique NaV1.7
domain driving chronic pain. Proc Natl Acad Sci USA.
120:e22178001202023. View Article : Google Scholar :
|
|
129
|
Shen T and Wang DM: Sodium channel NaV1. 7
and neuropathic pain. Chin J Biochem Mol Biol. 38:725–735. 2022.In
Chinese.
|
|
130
|
Zhou X, Ma T, Yang L, Peng S, Li L, Wang
Z, Xiao Z, Zhang Q, Wang L, Huang Y, et al: Spider venom-derived
peptide induces hyperalgesia in Nav1.7 knockout mice by activating
Nav1.9 channels. Nat Commun. 11:22932020. View Article : Google Scholar :
|
|
131
|
Strickland IT, Martindale JC, Woodhams PL,
Reeve AJ, Chessell IP and McQueen DS: Changes in the expression of
NaV1.7, NaV1.8 and NaV1.9 in a distinct population of dorsal root
ganglia innervating the rat knee joint in a model of chronic
inflammatory joint pain. Eur J Pain. 12:564–572. 2008. View Article : Google Scholar
|
|
132
|
Kingwell K: Nav1.7 withholds its pain
potential. Nat Rev Drug Discov. Apr 8–2019.Epub ahead of print.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Cardoso FC, Castro J, Grundy L, Schober G,
Garcia-Caraballo S, Zhao T, Herzig V, King GF, Brierley SM and
Lewis RJ: A spider-venom peptide with multitarget activity on
sodium and calcium channels alleviates chronic visceral pain in a
model of irritable bowel syndrome. Pain. 162:569–581. 2021.
View Article : Google Scholar
|
|
134
|
Wolkerstorfer A, Handler N and Buschmann
H: New approaches to treating pain. Bioorg Med Chem Lett.
26:1103–1119. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Wang HR, Hu SW, Zhang S, Song Y, Wang XY,
Wang L, Li YY, Yu YM, Liu H, Liu D, et al: KCNQ Channels in the
mesolimbic reward circuit regulate nociception in chronic pain in
mice. Neurosci Bull. 37:597–610. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Nestler EJ and Waxman SG: Resilience to
stress and resilience to pain: Lessons from molecular neurobiology
and genetics. Trends Mol Med. 26:924–935. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Han Y, Zhai XJ, Chen DD, Zhou Y, Zhou DY,
Zhang WX, Ji R, Li QZ, Gao YH, Cao JL and Zhang H: Recent advances
in the neurobiology of susceptibility and resilience to pain. Chin
J Pain Med. 28:571–581. 2022.In Chinese.
|
|
138
|
Li T, Wu K, Yue Z, Wang Y, Zhang F and
Shen H: Structural basis for the modulation of human KCNQ4 by
small-molecule drugs. Mol Cell. 81:25–37.e4. 2021. View Article : Google Scholar
|
|
139
|
Tsantoulas C and McMahon SB: Opening paths
to novel analgesics: The role of potassium channels in chronic
pain. Trends Neurosci. 37:146–158. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Alloui A, Zimmermann K, Mamet J, Duprat F,
Noel J, Chemin J, Guy N, Blondeau N, Voilley N, Rubat-Coudert C, et
al: TREK-1, a K+ channel involved in polymodal pain perception.
EMBO J. 25:2368–2376. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Zhou RP and Chen FH: Research progress on
role of acid-sensing ion channels in rheumatoid arthritis. Chin
Pharmacol Bull. 31:315–318. 2015.In Chinese.
|
|
142
|
Duan B, Wu LJ, Yu YQ, Ding Y, Jing L, Xu
L, Chen J and Xu TL: Upregulation of acid-sensing ion channel
ASIC1a in spinal dorsal horn neurons contributes to inflammatory
pain hypersensitivity. J Neurosci. 27:11139–11148. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Ma MJ: Study on the analgesic and
antipruritic mechanisms of saponins from Stauntonia chinensis and
its active components by modulating acid-sensing ion channels.
South-Central Univ Nationalities; 2021, In Chinese.
|
|
144
|
Xiong Z, Xie JX, Zhu KB, Zhang YT and Yang
R: Anti-nociceptive effects of paeoniflorin in formalin-induced
pain by regulating acid-sensing ion channels. Herald Med.
38:1403–1407. 2019.In Chinese.
|
|
145
|
Su SS, Liu J, Lin S and Wang DL: Research
progress on the application of ketamine combined with
dexmedetomidine. Med Innov China. 22:184–188. 2025.In Chinese.
|
|
146
|
Nirogi R, Goura V, Abraham R and Jayarajan
P: α4β2* neuronal nicotinic receptor ligands (agonist, partial
agonist and positive allosteric modulators) as therapeutic
prospects for pain. Eur J Pharmacol. 712:22–29. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Li L, Wu Y, Bai Z, Hu Y and Li W: Blockade
of NMDA receptors decreased spinal microglia activation in bee
venom induced acute inflammatory pain in rats. Neurol Res.
39:271–280. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Franceschini A and Adinolfi E: P2X
receptors: New players in cancer pain. World J Biol Chem.
5:4292014. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Souza Monteiro de Araujo D, Nassini R,
Geppetti P and De Logu F: TRPA1 as a therapeutic target for
nociceptive pain. Expert Opin Ther Targets. 24:997–1008. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Wei J, Su W, Zhao Y, Wei Z, Hua Y, Xue P,
Zhu X, Chen Y and Chen G: Maresin 1 promotes nerve regeneration and
alleviates neuropathic pain after nerve injury. J
Neuroinflammation. 19:322022. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Mahmoud O, Soares GB and Yosipovitch G:
Transient receptor potential channels and itch. Int J Mol Sci.
24:4202022. View Article : Google Scholar
|
|
152
|
Iftinca M, Defaye M and Altier C:
TRPV1-targeted drugs in development for human pain conditions.
Drugs. 81:7–27. 2021. View Article : Google Scholar
|
|
153
|
Zhang Y, Gao ZB, Xin XM and Zheng YM:
Research progress on the pharmacological activity of lappaconitine.
Chin Bull Life Sci. 33:1089–1095. 2021.In Chinese.
|
|
154
|
Cai S, Gomez K, Moutal A and Khanna R:
Targeting T-type/CaV3.2 channels for chronic pain. Transl Res.
234:20–30. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Yi SP, Chen ZM, Zhang JH and Zhang KJ:
Research progress of interactions among different opioid receptor
subtypes. Chin Pharmacol Bull. 28:1493–1496. 2012.In Chinese.
|
|
156
|
Stein C: Opioids, sensory systems and
chronic pain. Eur J Pharmacol. 716:179–187. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Wang D, Chen T, Zhou X, Couture R and Hong
Y: Activation of Mas oncogene-related gene (Mrg) C receptors
enhances morphine-induced analgesia through modulation of coupling
of μ-opioid receptor to Gi-protein in rat spinal dorsal horn.
Neuroscience. 253:455–464. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Montana MC and Gereau RW: Metabotropic
glutamate receptors as targets for analgesia: Antagonism,
activation, and allosteric modulation. Curr Pharm Biotechnol.
12:1681–1688. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Sawynok J: Adenosine receptor targets for
pain. Neuroscience. 338:1–18. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Chiou LC, Hu SS and Ho YC: Targeting the
cannabinoid system for pain relief? Acta Anaesthesiol Taiwan.
51:161–170. 2013. View Article : Google Scholar
|
|
161
|
Gong N, Fan H, Ma AN, Xiao Q and Wang YX:
Geniposide and its iridoid analogs exhibit antinociception by
acting at the spinal GLP-1 receptors. Neuropharmacology. 84:31–45.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Li JX, Zhang Y and Winter JC:
Morphine-induced antinociception in the rat: Supra-additive
interactions with-additive interactions with imidazoline
I2 receptor ligands. Eur J Pharmacol. 669:59–65. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Thorn DA, Siemian JN, Zhang Y and Li JX:
Anti-hyperalgesic effects of imidazoline I2 receptor ligands in a
rat model of inflammatory pain: Interactions with oxycodone.
Psychopharmacology (Berl). 232:3309–3318. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Falcicchia C, Tozzi F, Arancio O,
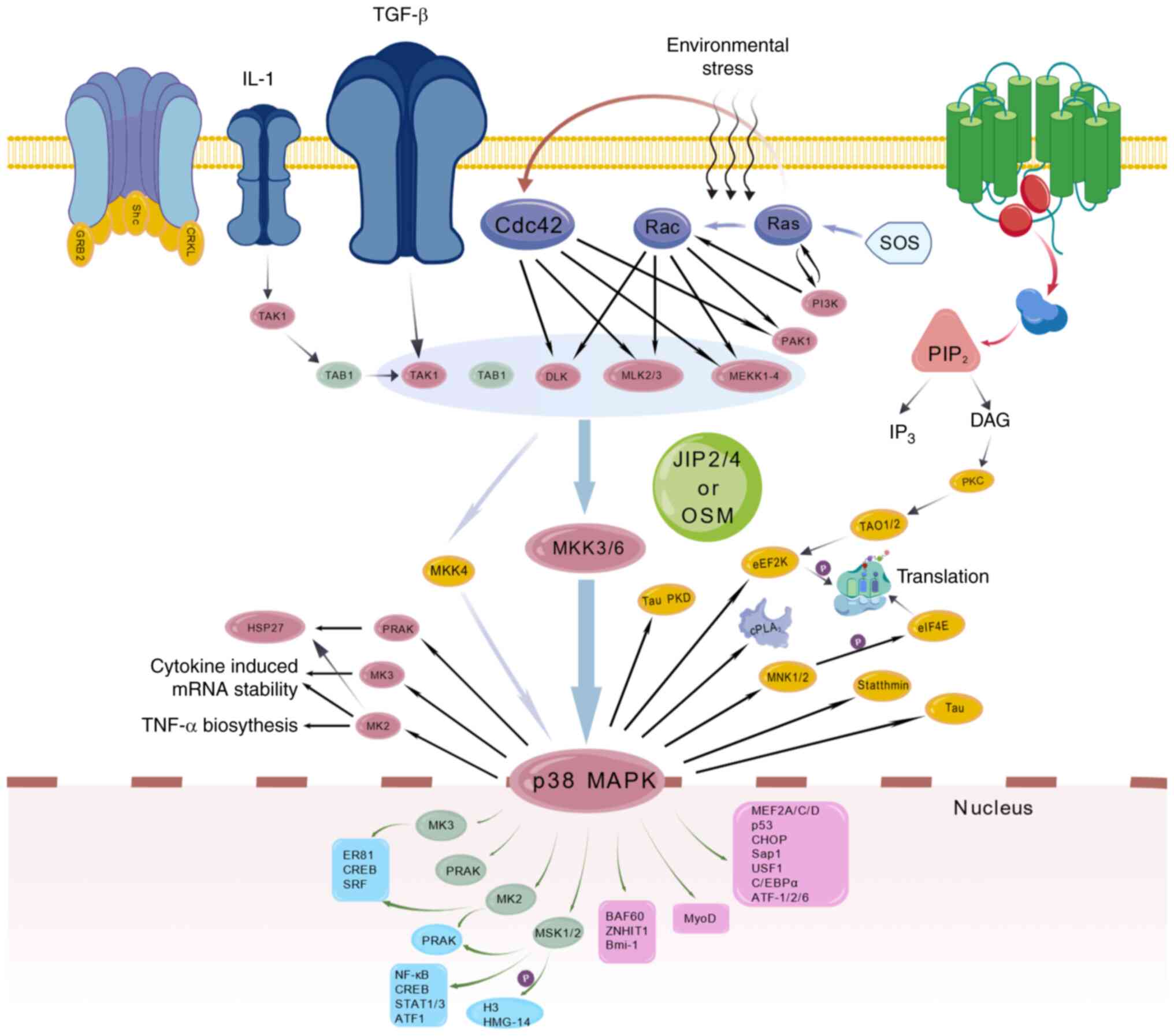
Watterson DM and Origlia N: Involvement of p38 MAPK in synaptic
function and dysfunction. Int J Mol Sci. 21:56242020. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Melamed Kadosh D, Beenstock J, Engelberg D
and Admon A: Differential modulation of the phosphoproteome by the
MAP kinases isoforms p38α and p38β. Int J Mol Sci. 24:124422023.
View Article : Google Scholar
|
|
166
|
Dong N, Li X, Xue C, Zhang L, Wang C, Xu X
and Shan A: Astragalus polysaccharides alleviates LPS-induced
inflammation via the NF-κB/MAPK signaling pathway. J Cell Physiol.
235:5525–5540. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Liu BP, Zhang YP, Yang ZY, Liu MJ, Zhang
C, Zhao YT and Cai S: ω-3 DPA protected neurons from
neuroinflammation by balancing microglia M1/M2 polarizations
through inhibiting NF-κB/MAPK p38 signaling and activating
neuron-BDNF-PI3K/AKT pathways. Mar Drugs. 19:5872021. View Article : Google Scholar
|
|
168
|
Li FS and Weng JK: Demystifying
traditional herbal medicine with modern approach. Nat Plants.
3:171092017. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Huang Y, Zhang D, Li ZY, Yang YT, Wu LJ,
Zhang J, Zhi FY, Li XY, Shi Z, Hong J and Ma XP: Moxibustion eases
chronic inflammatory visceral pain in rats via MAPK signaling
pathway in the spinal cord. J Pain Res. 12:2999–3012. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Jimi E, Huang F and Nakatomi C: NF-κB
signaling regulates physiological and pathological chondrogenesis.
Int J Mol Sci. 20:62752019. View Article : Google Scholar
|
|
171
|
Liang W, Zhang T, Zhang M, Gao J, Huang R,
Huang X, Chen J, Cheng L, Zhang L, Huang Z, et al: Daphnetin
ameliorates neuropathic pain via regulation of microglial responses
and glycerophospholipid metabolism in the spinal cord.
Pharmaceuticals (Basel). 17:7892024. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Lu ZH, Xiong XY, Lin GC, Meng JR and Mei
QB: Change of COX-1/2 expression in brain after spared nerve
injury-induced neuropathic pain and analgesic effects of COX
inhibitors with different selectivity. Chin J Neuroanat. 22:27–32.
2006.In Chinese.
|
|
173
|
Zhou XL, Wang Y, Zhang CJ, Yu LN, Cao JL
and Yan M: COX-2 is required for the modulation of spinal
nociceptive information related to ephrinB/EphB signalling. Eur J
Pain. 19:1277–1287. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Chandrasekharan NV, Dai H, Roos KL,
Evanson NK, Tomsik J, Elton TS and Simmons DL: COX-3, a
cyclooxygenase-1 variant inhibited by acetaminophen and other
analgesic/antipyretic drugs: Cloning, structure, and expression.
Proc Natl Acad Sci USA. 99:13926–13931. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Kuboyama K, Tsuda M, Tsutsui M, Toyohara
Y, Tozaki-Saitoh H, Shimokawa H, Yanagihara N and Inoue K: Reduced
spinal microglial activation and neuropathic pain after nerve
injury in mice lacking all three nitric oxide synthases. Mol Pain.
7:502011. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Wu Y, Yang Y, Wang L, Chen Y, Han X, Sun
L, Chen H and Chen Q: Effect of bifidobacterium on osteoclasts:
TNF-α/NF-κB inflammatory signal pathway-mediated mechanism. Front
Endocrinol (Lausanne). 14:11092962023. View Article : Google Scholar
|
|
177
|
Verma S, Dutta A, Dahiya A and Kalra N:
Quercetin-3-Rutinoside alleviates radiation-induced lung
inflammation and fibrosis via regulation of NF-κB/TGF-β1 signaling.
Phytomedicine. 99:1540042022. View Article : Google Scholar
|
|
178
|
Sun Y and Wang HX: Astragaloside IV
alleviates inflammatory response in pulmonary hypertension rats
through the NF-KB/NLRP3 signaling pathway. Chin Tradit Patent Med.
45:578–582. 2023.In Chinese.
|
|
179
|
Sun YL, Zhao JY, Qin YS and Ren GH:
Research progress on Traditional Chinese Medicine for migraine
treatment based on signaling pathways. J Pract Tradit Chin Intern
Med. 38:88–91. 2024.In Chinese.
|
|
180
|
Wang D, Chen B, Tang Y, Liu HQ, Li J and
Yang SL: Acupuncture and moxibustion regulation of NF - κB
signaling pathway in the treatment of rheumatoid arthritis. Chin J
Ethnomed Ethnopharm. 33:68–71. 2024.In Chinese.
|
|
181
|
Chen QZ, Huang YJ and Gu CM: Dezocine
alleviates remifentanil-induced hyperalgesia via targeting the
Toll-like receptor 4/nuclear factor kappa-B pathway. Hebei Med J.
46:181–185. 1912024.In Chinese.
|
|
182
|
Cao J, Liu H, An Q and Han F: Metformin
alleviates pathologic pain in mice with radiation dermatitis by
inhibiting p38MAPK/NF-κB signaling pathway. Nan Fang Yi Ke Da Xue
Xue Bao. 43:1815–1820. 2023.PubMed/NCBI
|
|
183
|
Benke D: GABA(B) receptors and pain. Curr
Top Behav Neurosci. 52:213–239. 2022. View Article : Google Scholar
|
|
184
|
Zeilhofer HU, Mohler H and Di Lio A:
GABAergic analgesia: New insights from mutant mice and
subtype-selective agonists. Trends Pharmacol Sci. 30:397–402. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Zhu Q, Sun Y, Zhu J, Fang T, Zhang W and
Li JX: Antinociceptive effects of sinomenine in a rat model of
neuropathic pain. Sci Rep. 4:72702014. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Bowery NG: GABAB receptor: A site of
therapeutic benefit. Curr Opin Pharmacol. 6:37–43. 2006. View Article : Google Scholar
|
|
187
|
Zeng XY, Zhang Q, Wang J, Yu J, Han SP and
Wang JY: Distinct role of tumor necrosis factor receptor subtypes 1
and 2 in the red nucleus in the development of neuropathic pain.
Neurosci Lett. 569:43–48. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Vogel C, Stallforth S and Sommer C:
Altered pain behavior and regeneration after nerve injury in TNF
receptor deficient mice. J Peripher Nerv Syst. 11:294–303. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Wang Y, Zhuang Y, DiBerto JF, Zhou XE,
Schmitz GP, Yuan Q, Jain MK, Liu W, Melcher K, Jiang Y, et al:
Structures of the entire human opioid receptor family. Cell.
186:413–427.e17. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Siuda ER, Carr R III, Rominger DH and
Violin JD: Biased mu-opioid receptor ligands: A promising new
generation of pain therapeutics. Curr Opin Pharmacol. 32:77–84.
2017. View Article : Google Scholar
|
|
191
|
Obeng S, Hiranita T, Leon F, McMahon LR
and McCurdy CR: Novel approaches, drug candidates, and targets in
pain drug discovery. J Med Chem. 64:6523–6548. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Abrimian A, Kraft T and Pan YX: Endogenous
opioid peptides and alternatively spliced mu opioid receptor seven
transmembrane carboxyl-terminal variants. Int J Mol Sci.
22:37792021. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Paul AK, Smith CM, Rahmatullah M,
Nissapatorn V, Wilairatana P, Spetea M, Gueven N and Dietis N:
Opioid analgesia and opioid-induced adverse effects: A review.
Pharmaceuticals (Basel). 14:10912021. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Baldo BA and Rose MA: Mechanisms of
opioid-induced respiratory depression. Arch Toxicol. 96:2247–2260.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Dang VC and Christie MJ: Mechanisms of
rapid opioid receptor desensitization, resensitization and
tolerance in brain neurons. Br J Pharmacol. 165:1704–1716. 2012.
View Article : Google Scholar :
|
|
196
|
Faouzi A, Varga BR and Majumdar S: Biased
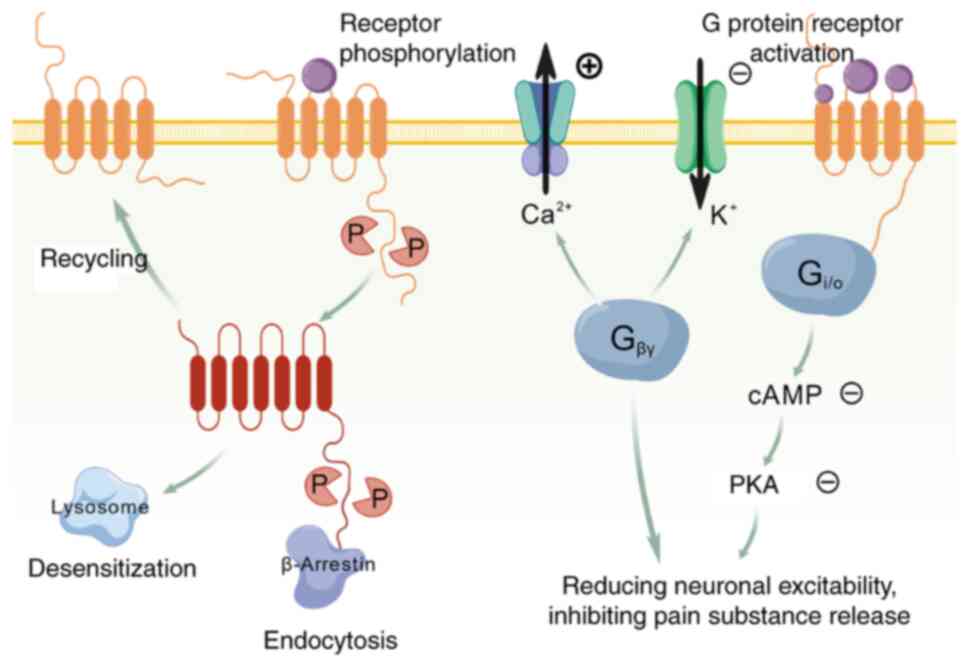
opioid ligands. Molecules. 25:42572022. View Article : Google Scholar
|
|
197
|
Bagley EE and Ingram SL: Endogenous opioid
peptides in the descending pain modulatory circuit.
Neuropharmacology. 173:1081312020. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Kliewer A, Gillis A, Hill R, Schmiedel F,
Bailey C, Kelly E, Henderson G, Christie MJ and Schulz S:
Morphine-induced respiratory depression is independent of
beta-arrestin2 signalling. Br J Pharmacol. 177:2923–2931. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Fujita W: The possible role of MOPr-DOPr
heteromers and its regulatory protein RTP4 at sensory neurons in
relation to pain perception. Front Cell Neurosci. 14:6093622020.
View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Schröder W, Lambert DG, Ko MC and Koch T:
Functional plasticity of the N/OFQ-NOP receptor system determines
analgesic properties of NOP receptor agonists. Br J Pharmacol.
171:3777–3800. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Williams JT, Ingram SL, Henderson G,
Chavkin C, Von Zastrow M, Schulz S, Koch T, Evans CJ and Christie
MJ: Regulation of μ-opioid receptors: desensitization,
phosphorylation, internalization, and tolerance. Pharmacol Rev.
65:223–254. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Violin JD, Crombie AL, Soergel DG and Lark
MW: Biased ligands at G-protein-coupled receptors: promise and
progress. Trends Pharmacol Sci. 35:308–316. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Soergel DG, Subach RA, Burnham N, Lark MW,
James IE, Sadler BM, Skobieranda F, Violin JD and Webster LR:
Biased agonism of the μ-opioid receptor by TRV130 increases
analgesia and reduces on-target adverse effects versus morphine: A
randomized, double-blind, placebo-controlled, crossover study in
healthy volunteers. Pain. 155:1829–1835. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Manglik A, Lin H, Aryal DK, McCorvy JD,
Dengler D, Corder G, Levit A, Kling RC, Bernat V, Hübner H, et al:
Structure-based discovery of opioid analgesics with reduced side
effects. Nature. 537:185–190. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
205
|
Botting R and Ayoub SS: COX-3 and the
mechanism of action of paracetamol/acetaminophen. Prostaglandins
Leukot Essent Fatty Acids. 72:85–87. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
206
|
Kautio AL, Haanpää M, Kautiainen H, Kalso
E and Saarto T: Burden of chemotherapy-induced neuropathy-a
cross-sectional study. Support Care Cancer. 19:1991–1996. 2011.
|
|
207
|
Van Poznak CH, Temin S, Yee GC, Janjan NA,
Barlow WE, Biermann JS, Bosserman LD, Geoghegan C, Hillner BE,
Theriault RL, et al: American society of clinical oncology
executive summary of the clinical practice guideline update on the
role of bone-modifying agents in metastatic breast cancer. J Clin
Oncol. 29:1221–1227. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Findlay DM and Haynes DR: Mechanisms of
bone loss in rheumatoid arthritis. Mod Rheumatol. 15:232–240. 2005.
View Article : Google Scholar
|
|
209
|
Jones DH, Nakashima T, Sanchez OH,
Kozieradzki I, Komarova SV, Sarosi I, Morony S, Rubin E, Sarao R,
Hojilla CV, et al: Regulation of cancer cell migration and bone
metastasis by RANKL. Nature. 440:692–696. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Lipton A, Fizazi K, Stopeck AT, Henry DH,
Brown JE, Yardley DR, Richardson GE, Siena S, Maroto P, Clemens M,
et al: Superiority of denosumab to zoledronic acid for prevention
of skeletal-related events: A combined analysis of 3 pivotal,
randomised, phase 3 trials. Eur J Cancer. 48:3082–3092. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Committee of Cancer Overall Evaluation,
China Anti-Cancer Association: Expert consensus on integrated
prevention and treatment of opioid-related adverse drug reactions
(2024 edition). Chin J Clin Oncol. 51:757–763. 2024.In Chinese.
|
|
212
|
Suh SY, Choi YS, Oh SC, Kim YS, Cho K, Bae
WK, Lee JH, Seo AR and Ahn HY: Caffeine as an adjuvant therapy to
opioids in cancer pain: A randomized, double-blind,
placebo-controlled trial. J Pain Symptom Manage. 46:474–482. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
213
|
Zhang JM and An J: Cytokines,
inflammation, and pain. Int Anesthesiol Clin. 45:27–37. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
214
|
Salerno A and Hermann R: Efficacy and
safety of steroid use for postoperative pain relief. Update and
review of the medical literature. J Bone Joint Surg Am.
88:1361–1372. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Ryan R, Booth S and Price S:
Corticosteroid-use in primary and secondary brain tumour patients:
A review. J Neurooncol. 106:449–459. 2012. View Article : Google Scholar
|
|
216
|
Paulsen Ø, Klepstad P, Rosland JH, Aass N,
Albert E, Fayers P and Kaasa S: Efficacy of methylprednisolone on
pain, fatigue, and appetite loss in patients with advanced cancer
using opioids: A randomized, placebo-controlled, double-blind
trial. J Clin Oncol. 32:3221–3228. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
217
|
Mihaljević S, Pavlović M, Reiner K and
Ćaćić M: Therapeutic mechanisms of ketamine. Psychiatr Danub.
32:325–333. 2020. View Article : Google Scholar
|
|
218
|
Chang M, Hu D, Chen FQ, Shi F, Yu Y, Wang
X, Fu SO and Xie P: Efficacy and immunomodulatory effects of
low-dose ketamine as an adjunct to morphine in patient-controlled
analgesia for advanced cancer pain. Chin J Pain Med. 21:152–155.
2015.In Chinese.
|
|
219
|
Morita K, Kitayama T, Morioka N and Dohi
T: Glycinergic mediation of tactile allodynia induced by
platelet-activating factor (PAF) through glutamate-NO-cyclic GMP
signalling in spinal cord in mice. Pain. 138:525–536. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
220
|
Hasegawa S, Kohro Y, Shiratori M, Ishii S,
Shimizu T, Tsuda M and Inoue K: Role of PAF receptor in
proinflammatory cytokine expression in the dorsal root ganglion and
tactile allodynia in a rodent model of neuropathic pain. PLoS One.
5:e104672010. View Article : Google Scholar : PubMed/NCBI
|
|
221
|
Morita K, Shiraishi S, Motoyama N,
Kitayama T, Kanematsu T, Uezono Y and Dohi T: Palliation of bone
cancer pain by antagonists of platelet-activating factor receptors.
PLoS One. 9:e917462014. View Article : Google Scholar : PubMed/NCBI
|
|
222
|
García de Paredes ML, Del Moral González
F, Martínez Del Prado P, Martí Ciriquián JL, Enrech Francés S, Cobo
Dols M, Esteban González E, Ortega Granados AL, Majem Tarruella M,
Cumplido Burón JD, et al: First evidence of oncologic neuropathic
pain prevalence after screening 8615 cancer patients. Results of
the On study. Ann Oncol. 22:924–930. 2011. View Article : Google Scholar
|
|
223
|
Fleming JA and O'Connor BD: Use of
lidocaine patches for neuropathic pain in a comprehensive cancer
centre. Pain Res Manag. 14:381–388. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
224
|
Portenoy RK, Ganae-Motan ED, Allende S,
Yanagihara R, Shaiova L, Weinstein S, McQuade R, Wright S and
Fallon MT: Nabiximols for opioid-treated cancer patients with
poorly-controlled chronic pain: A randomized, placebo-controlled,
graded-dose trial. J Pain. 13:438–449. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
225
|
Colloca L, Ludman T, Bouhassira D, Baron
R, Dickenson AH, Yarnitsky D, Freeman R, Truini A, Attal N,
Finnerup NB, et al: Neuropathic pain. Nat Rev Dis Primers.
3:170022017. View Article : Google Scholar : PubMed/NCBI
|
|
226
|
Ye H, Song GP, Wang SJ, Shen XG, Qin LY
and Long SL: Clinical efficacy of radiofrequency ablation in the
treatment of lumbar spine nerve posterior branch entrapment
syndrome. Guangdong Med J. 46:228–232. 2025.In Chinese.
|
|
227
|
Li JZ, Yan WP, Qiang TL, Liu JP, Li JK and
Mao JW: Advances in research on intravertebral basivertebral nerve
radiofrequency ablation for treatment of chronic low back pain due
to Modic changes. J Tradit Chin Orthop Traumatol. 36:55–58.
622024.In Chinese.
|
|
228
|
Han S, Xiao B, Hou SY and Sun JJ: Effect
of DSA-based radiofrequency ablation and TACE interventional
surgery on the short-term efficacy and complications of
hepatocellular carcinoma. Pract J Cancer. 40:147–150. 1552025.In
Chinese.
|
|
229
|
Abd-Elsayed A, Nguyen S and Fiala K:
Radiofrequency ablation for treating headache. Curr Pain Headache
Rep. 23:182019. View Article : Google Scholar : PubMed/NCBI
|
|
230
|
Horsch S and Claeys L: Epidural spinal
cord stimulation in the treatment of severe peripheral arterial
occlusive disease. Ann Vasc Surg. 8:468–474. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
231
|
Yin J, Sun SS, Cai M, Liu HJ and Jin Y:
Analgesic mechanism study of neuropathic pain relieved by early
spinal cord stimulation in rats with spinal cord injury. Chin J
Pain Med. 30:494–500. 2024.In Chinese.
|
|
232
|
Sivaramakrishnan A, Solomon JM and
Manikandan N: Comparison of transcutaneous electrical nerve
stimulation (TENS) and functional electrical stimulation (FES) for
spasticity in spinal cord injury - a pilot randomized cross-over
trial. J Spinal Cord Med. 41:397–406. 2018. View Article : Google Scholar :
|
|
233
|
Li T and Chen J: Spinal cord stimulation
for functional restoration in spinal cord injury: A narrative
review. Cureus. 17:e786102025.PubMed/NCBI
|
|
234
|
Zong YF, Dong TY and Bao M: Progress on
spinal cord stimulation in treatment of peripheral neuropathy. Chin
J Contemp Neurol Neurosurg. 25:72–77. 2025.In Chinese.
|
|
235
|
Qi DB and Zhao SB: Treatment of lumbar
disc herniation complicated with cauda equina symptoms by
percutaneous transforaminal endoscopic discectomy. J Clin Orthop.
28:34–37. 2025.In Chinese.
|
|
236
|
He Y, Li ZL, Jia T, Ren DW and Xi TP: The
effect of percutaneous transforaminal endoscopic discectomy in the
treatment of lumbar disc herniation. J Clin Orthop. 27:780–784.
2024.In Chinese.
|
|
237
|
Zhang B, Zhu HH, Dong H, Wang K, Xu LZ, Li
YW and Mei W: Clinical efficacy of percutaneous endoscopic
transforaminal technique for recurrent lumbar disc herniation. Chin
J Min Inv Surg. 23:813–817. 2023.In Chinese.
|
|
238
|
Ji T, Chen SL, Li N, Cao M and Cui W:
Effect of percutaneous transforaminal endoscopic discectomy on pain
and serum biomarkers (CPK/Myoglobin) in patients with lumbar disc
herniation: A mechanistic and clinical correlation study. J
Cervicodynia Lumbodynia. 44:827–830. 2023.In Chinese.
|
|
239
|
Miscov R, Gulisano HA and Bjarkam CR:
Treatment of patients with chronic malignant pain with intrathecal
morphine. Ugeskr Laeger. 186:082305412024.In Danish.
|
|
240
|
Rosen SM, Bromberg TA, Padda G, Barsa J,
Dunbar E, Dwarakanath G, Navalgund Y, Jaffe T, Yearwood TL, Creamer
M and Deer T: Intrathecal administration of Infumorph® vs
compounded morphine for treatment of intractable pain using the
Prometra® programmable pump. Pain Med. 14:865–873. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
241
|
Sun C, Wang YT, Dai YJ, Liu ZH, Yang J,
Cheng ZQ, Dong DS, Wang CF, Zhao GL, Lu GJ, et al: Programmable
pump for intrathecal morphine delivery to cisterna magna: clinical
implications in novel management of refractory pain above middle
thoracic vertebrae level utilizing a prospective trial protocol and
review. Anesth Pain Med. 11:e1158732021. View Article : Google Scholar : PubMed/NCBI
|
|
242
|
De Andrés J, Rubio-Haro R, De
Andres-Serrano C, Asensio-Samper JM and Fabregat-Cid G: Intrathecal
drug delivery. Methods Mol Biol. 2059:75–108. 2020. View Article : Google Scholar
|
|
243
|
The polyanalgesic consensus conference
(PACC): Recommendations on intrathecal drug infusion systems best
practices and guidelines. Neuromodulation. 20:405–406. 2017.
View Article : Google Scholar
|
|
244
|
Penn RD: Intrathecal medication delivery.
Neurosurg Clin N Am. 14:381–387. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
245
|
Zhang HF, Guo XQ and Wang QJ: Qianghuo
Shengshi decoction combined with radiofrequency ablation for
cervical radiculopathy with wind-cold obstruction syndrome: A
randomized controlled trial on pain relief and functional recovery.
TCM Res. 38:42–46. 2025.In Chinese.
|
|
246
|
Wang J and Wang YT: Efficacy of celecoxib
combined with radiofrequency ablation of posterior branch of
cervical spinal nerve in treatment for cervicogenic headache and
its effect on cervical hemodynamics, pain and sleep quality. China
Med Eng. 33:72–76. 2025.In Chinese.
|
|
247
|
Zhang SC: Clinical observation of
percutaneous radiofrequency ablation of hepatocellular carcinoma
combined with Traditional Chinese Medicine enema. Guide China Med.
23:154–156. 2025.In Chinese.
|
|
248
|
Zhou XQ, Jiang CY, Fang JL and Li G:
Effect of nerve block combined with spinal cord electrical
stimulation on sleep quality and pain degree of patients with
postherpetic neuralgia. J Clin Exp Med. 23:659–662. 2024.In
Chinese.
|
|
249
|
Han J: Effect of temporary spinal cord
stimulation combined with ozone injection on mechanical pain
thresholds and inflammatory factors in patients with neuropathic
pain. Pract Clin J Integr Tradit Chin West Med. 23:5–8. 2023.In
Chinese.
|
|
250
|
Wang Z, Jia BQ, Zhang XG, Li YZ, Wang SF
and Yao Y: The therapeutic effect of red light irradiation plus
oral TCM medicine and TESSYS on lumbar disc herniation. Clin J Chin
Med. 14:110–113. 2022.In Chinese.
|
|
251
|
Peng LP, Liu LH, Gu ZC, Jiang DF, Yin ZY
and Li ZY: Clinical efficacy of Qizhu Yin combined with
percutaneous transforaminal endoscopic discectomy in the treatment
of lumbar disc herniation. North Pharm. 19:90–92. 2022.In
Chinese.
|
|
252
|
Liu HP and Dong XH: Clinical effect of
percutaneous foraminoscopy combined with Tenghuang Jiangu Capsule
in the treatment of lumbar intervertebral disc herniation patients.
Lab Med Clin. 18:2981–2983. 2021.In Chinese.
|
|
253
|
Sun LH, Tang Q, Gu GL, Fan XS and Yuan M:
Therapeutic effect of intrathecal drug delivery system combined
with pain management on middle- and late-stage homebound severe
cancer pain patients. J Guizhou Med Univ. 49:1353–1359. 2024.In
Chinese.
|
|
254
|
Qiao YY, Liu B and Lu Y: Clinical efficacy
of conventional intravenous and intrathecal drug therapies in acute
neuromyelitis optica spectrum disorders. Chin Gen Pract.
23:1513–1516. 15222020.In Chinese.
|
|
255
|
Li JJ, Zhao Y, Gu CM and Liu J: Research
progress of intrathecal analgesia. China Contin Med Educ. 8:60–61.
2016.In Chinese.
|
|
256
|
Zhu L and Zhao XT: The effect of
percutaneous nerve electrical stimulation combined with isokinetic
centrifugal training on pain severity and muscle strength in
patients with knee osteoarthritis. Proceed Clin Med. 34:109–112.
2025.In Chinese.
|
|
257
|
Ren HX, Xin ZJ, Ji WS, Wang N and Meng XZ:
Clinical efficacy of transcutaneous auricular vagus nerve
stimulation in treatment of lumbar disc herniation. Med J Chin PAP.
35:740–744. 2024.In Chinese.
|
|
258
|
Gu YY, Xu FP, Li ZZ, Zhang GY and Gu CY:
Meta-analysis on transcutaneous electrical nerve stimulation (TENS)
for pain relief among women undergoing vaginal trial of labor. Chin
J Women Child Health. 15:63–72. 2024.In Chinese.
|
|
259
|
Feng YH, Feng YL and Zheng CS: Sanyinjiao
(SP6) moxibustion combined with transcutaneous electrical nerve
stimulation in the treatment of primary dysmenorrhea. Chin Med Mod
Distance Educ China. 22:124–126. 2024.In Chinese.
|
|
260
|
Nie XM, Jin F and Shi JL: Efficacy of
transcutaneous spinal cord stimulation in alleviating
pregnancy-related postpartum low back pain: A prospective clinical
study. Med Forum. 28(4-6): 212024.In Chinese.
|
|
261
|
Liu GH, Cai YJ, Wei MX, Guan LP, Zhao XJ
and Liu XM: Efficacy of self-developed Yanwu formula combined with
ultrasound-mediated drug delivery in treating chronic pelvic pain
with dampness-heat and blood stasis syndrome: a randomized
controlled trial. Chin J Clin Rational Drug Use. 16:95–97. 2023.In
Chinese.
|
|
262
|
Guan CY and Sun ZC: Clinical efficacy of
combined ultrasound and low-level laser therapy in the management
of chronic heel pain: A randomized controlled trial. Chin J
Convalescent Med. 18:6242009.In Chinese.
|
|
263
|
Luo FZ: Curative effect analysis of
ultrasound on non-specific low back pain. Smart Healthcare.
6:47–48. 2020.In Chinese.
|
|
264
|
Yang H, Cai JH, Zhou C, Zhang SJ, Xiao T,
Hu BC, Ai JF and Li Z: Effects of ultrasound combined with
transcutaneous electrical nerve stimulation on knee joint pain and
function in patients with knee osteoarthritis. Chin J Rehabil Med.
39:1174–1179. 2024.In Chinese.
|
|
265
|
Bi YL, Zhai HW, Zhang JL and Wang SY:
Observation on the efficacy of high-frequency repetitive
transcranial magnetic stimulation at different frequencies in
treating central post-stroke pain. Chin J Rehabil. 40:32–35.
2025.In Chinese.
|
|
266
|
Zhang YW, Wang H, Gao SN, Sun XX, Chen C,
Shen YY and Ding L: Efficacy of repetitive transcranial magnetic
stimulation in relieving pain and quality of life in patients with
acute central poststroke pain. Pract Geriatr. 38:1250–1254. 2024.In
Chinese.
|
|
267
|
Wang J, Song JY, Xu B, Lyu HZ, Zhao XB,
Gong HR and Li YX: Effects of repetitive transcranial magnetic
stimulation combined with exercise training on patients with
incomplete spinal cord injuries. J Trauma Surg. 26:936–940. 2024.In
Chinese.
|
|
268
|
Sun YJ, Zhang JF, Yan L, Fan SY, Qian YL,
Cong S, Wang Y and Yu T: Mechanism of transcranial magnetic
stimulation therapy for neuropathic pain. Rehabilitation Med.
34:625–632. 2024.In Chinese. View Article : Google Scholar
|
|
269
|
Xie Y, Pan J, Chen J, Zhang D and Jin S:
Acupuncture combined with repeated transcranial magnetic
stimulation for upper limb motor function after stroke: A
systematic review and meta-analysis. Neurorehabilitation.
53:423–438. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
270
|
Luo WW and Li TL: Observation of the
clinical efficacy of electro-acupuncture combined with infrared ray
in the treatment of chronic pelvic pain caused by pelvic
inflammatory diseases. Guiding J Tradit Chin Med Pharmacol.
29:110–113. 2023.In Chinese.
|
|
271
|
Gan PQ, Wang YY, Pan Q and Shi FF: Nursing
and effection of Piwei Peiyuansan combined with infrared lamp
irradiation in treating 35 patients with epigastric pain. Anhui
Med. 20:1412–1414. 2016.In Chinese.
|
|
272
|
Ou JW, Wang XP, Zhang XT and Sun XS:
Effect of Aitong Gao acupoint application combined with whole-body
infrared hyperthermia on cancer-related pain. Guangdong Med J.
38:1761–1763. 2017.In Chinese.
|
|
273
|
Liao TH, Hu LM, Yu ZS, Huang CJ, Liu JB
and Mo CM: Clinical efficacy of Xietong Gao external application
combined with infrared irradiation in alleviating hepatocellular
carcinoma-related pain: A case series of 40 patients. J Pract
Tradit Chin Med. 28:1048–1049. 2012.In Chinese.
|
|
274
|
Men JR, Gao SF, Yin JF, Lei YW and Hu YF:
Efficacy of external application of traditional Chinese medicine
combined with far infrared irradiation and dialectical dietary
intervention in patients with lumbar disc herniation. Hebei J TCM.
46:1863–1866. 2024.In Chinese.
|
|
275
|
Pang ZH, Qin TM and Ruan MJ: Clinical
efficacy of combined deep hyperthermia and Sihuang powder external
application in managing intermediate-advanced primary liver cancer
with cancer-related pain. Mod Med Health Res. 8:102–105. 2024.In
Chinese.
|
|
276
|
Chen XH and Yan Y: Clinical study on
transcutaneous auricular vagus nerve stimulation combined with
multimodal analgesia for rehabilitation after total knee
arthroplasty. Chin J Convalescent Med. 34:22–26. 2025.In
Chinese.
|
|
277
|
Mao M, Sun YH and Peng YG: Clinical
research of external application of 'Aitongxiao̓ combined with
thermal therapy in releasing moderate to severe pain due to cancer.
Shanghai J Tradit Chin Med. 48:44–47. 2014.In Chinese.
|
|
278
|
Yang J, Lo WAL, Zheng F, Cheng X, Yu Q and
Wang C: Evaluation of cognitive behavioral therapy on improving
pain, fear avoidance, and self-efficacy in patients with chronic
low back pain: A systematic review and meta-analysis. Pain Res
Manag. 2022:42761752022. View Article : Google Scholar : PubMed/NCBI
|
|
279
|
Darnall BD, Roy A, Chen AL, Ziadni MS,
Keane RT, You DS, Slater K, Poupore-King H, Mackey I, Kao MC, et
al: Comparison of a single-session pain management skills
intervention with a single-session health education intervention
and 8 sessions of cognitive behavioral therapy in adults with
chronic low back pain: A randomized clinical trial. JAMA Netw Open.
4:e21134012021. View Article : Google Scholar : PubMed/NCBI
|
|
280
|
Cherkin DC, Sherman KJ, Balderson BH, Cook
AJ, Anderson ML, Hawkes RJ, Hansen KE and Turner JA: Effect of
mindfulness-based stress reduction vs cognitive behavioral therapy
or usual care on back pain and functional limitations in adults
with chronic low back pain: A Randomized clinical trial. JAMA.
315:1240–1249. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
281
|
Hajihasani A, Rouhani M, Salavati M,
Hedayati R and Kahlaee AH: The influence of cognitive behavioral
therapy on pain, quality of life, and depression in patients
receiving physical therapy for chronic low back pain: A systematic
review. PM R. 11:167–176. 2019. View Article : Google Scholar
|
|
282
|
Mariano TY, Urman RD, Hutchison CA,
Jamison RN and Edwards RR: Cognitive behavioral therapy (CBT) for
subacute low back pain: A systematic review. Curr Pain Headache
Rep. 22:152018. View Article : Google Scholar : PubMed/NCBI
|
|
283
|
Hadley G and Novitch MB: CBT and CFT for
chronic pain. Curr Pain Headache Rep. 25:352021. View Article : Google Scholar : PubMed/NCBI
|
|
284
|
Torres CB, Barona EJG, Molina MG, Sánchez
MEG and Manso JMM: A systematic review of EEG neurofeedback in
fibromyalgia to treat psychological variables, chronic pain and
general health. Eur Arch Psychiatry Clin Neurosci. 274:981–999.
2024. View Article : Google Scholar :
|
|
285
|
Goldway N, Ablin J, Lubin O, Zamir Y,
Keynan JN, Or-Borichev A, Cavazza M, Charles F, Intrator N, Brill
S, et al: Volitional limbic neuromodulation exerts a beneficial
clinical effect on Fibromyalgia. NeuroImage. 186:758–770. 2019.
View Article : Google Scholar
|
|
286
|
Hassett AL, Radvanski DC, Vaschillo EG,
Vaschillo B, Sigal LH, Karavidas MK, Buyske S and Lehrer PM: A
pilot study of the efficacy of heart rate variability (HRV)
biofeedback in patients with fibromyalgia. Appl Psychophysiol
Biofeedback. 32:1–10. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
287
|
Burch JB, Ginsberg JP, McLain AC, Franco
R, Stokes S, Susko K, Hendry W, Crowley E, Christ A, Hanna J, et
al: Symptom management among cancer survivors: randomized pilot
intervention trial of heart rate variability biofeedback. Appl
Psychophysiol Biofeedback. 45:99–108. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
288
|
Stern MJ, Guiles RAF and Gevirtz R: HRV
biofeedback for pediatric irritable bowel syndrome and functional
abdominal pain: A clinical replication series. Appl Psychophysiol
Biofeedback. 39:287–291. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
289
|
Jensen MP, Gianas A, George HR, Sherlin
LH, Kraft GH and Ehde D: Use of neurofeedback to enhance response
to hypnotic analgesia in individuals with multiple sclerosis. Int J
Clin Exp Hypn. 64:1–23. 2016. View Article : Google Scholar
|
|
290
|
Zhao X: Clinical observation on
acupuncture combined with meridian-based tuina in treating elderly
patients with neck, shoulder, lower back, and leg pain. Inner
Mongolia J Tradit Chin Med. 43:134–135. 1682024.In Chinese.
|
|
291
|
Su L, Li X and Yu P: Effect of Yiqi Shujin
decoction combined with meridian massage on TCM symptoms and
functional recovery in patients with neck, shoulder, low back and
leg pain. J Med Inform. 37:130–134. 2024.In Chinese.
|
|
292
|
Gausel AM, Dalen I, Kjærmann I, Malmqvist
S, Andersen K, Larsen JP and Økland I: Adding chiropractic
treatment to individual rehabilitation for persistent pelvic girdle
pain 3 to 6 months after delivery: A pilot randomized trial. J
Manipulative Physiol Ther. 42:601–607. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
293
|
Duan JQ, Chen ZX, Hu P, Zhang XL, Zhang W
and Wang Y: Effect of chiropractic therapy for spinal epigastric
pain. Chin J Convalescent Med. 33:80–84. 2024.In Chinese.
|
|
294
|
Chen B, Dai GW, Tian XY, Chen ZR, Wang LK
and Yang XK: The clinical effect of chiropractic therapy in the
treatment of 30 cases of spinal calcaneodynia. Chin Community
Doctors. 30:96–97. 2014.In Chinese.
|
|
295
|
Wei YH, Xu M and Chen XF: Study for the
effect of Traditional Chinese medicine enema combined with fructus
Evodiae Rutecarpae on preemptive analgesia after pelvic operation.
J Nurses Train. 31:772–774. 2016.In Chinese.
|
|
296
|
Xiong ZL: Clinical observation on massage
combined with Shentong Zhuyu decoction in treating Qi Stagnation
and blood stasis lumbago. Chin Med Mod Distance Educ China.
18:82–84. 2024.In Chinese.
|
|
297
|
Song S, Liu Y, Zhang BX, Teng C and Zhao
SS: Clinical efficacy observation of low intensity pulse ultrasound
combined with quadriceps femoris muscle strength intensive training
in the treatment of patients with knee osteoarthritis. Prog Mod
Biomed. 20:2668–2671. 2020.In Chinese.
|
|
298
|
Chen C, Zhang JP, Peng J, Cao AH, Chen XM,
Zhang C and Shen L: Efficacy of low-intensity pulsed ultrasound
therapy on heart rate variability in elderly patients with coronary
heart disease. Chin J Med Front (Electron Version). 15:44–49.
2023.In Chinese.
|
|
299
|
Liu L, Wu JY, Zhang CL and Zhu BL:
Percutaneous transforaminal endoscopic discectomy for treatment of
lumbar disc herniation under epidural anesthesia. J Clin Orthop.
27:636–639. 2024.In Chinese.
|
|
300
|
Chen YD: Clinical research of acupuncture,
chiropractic therapy combined with amitriptyline in the treatment
of fibromyalgia syndrome. China Pract Med. 10:24–25. 2015.In
Chinese.
|
|
301
|
Russo AF and Hay DL: CGRP physiology,
pharmacology, and therapeutic targets: Migraine and beyond. Physiol
Rev. 103:1565–1644. 2023. View Article : Google Scholar :
|
|
302
|
Markham A: Erenumab: First global
approval. Drugs. 78:1157–1161. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
303
|
Zhou W, Ye C, Wang H, Mao Y, Zhang W, Liu
A, Yang CL, Li T, Hayashi L, Zhao W, et al: Sound induces analgesia
through corticothalamic circuits. Science. 377:198–204. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
304
|
Gu X, Zhang YZ, O'Malley JJ, De Preter CC,
Penzo M and Hoon MA: Neurons in the caudal ventrolateral medulla
mediate descending pain control. Nat Neurosci. 26:594–605. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
305
|
Grandi FC, Baskar R, Smeriglio P,
Murkherjee S, Indelli PF, Amanatullah DF, Goodman S, Chu C, Bendall
S and Bhutani N: Single-cell mass cytometry reveals cross-talk
between inflammation-dampening and inflammation-amplifying cells in
osteoarthritic cartilage. Sci Adv. 6:eaay53522020. View Article : Google Scholar : PubMed/NCBI
|
|
306
|
Li X, Lin S, Lin Y, Su Y, Wang C, Huang L,
Zhao J and Tian G: The analgesic mechanism of Xi Shao Formula
research on pain based on metabolomics. J Tradit Chin Med Sci.
10:448–460. 2023.
|
|
307
|
Schneeberger M, Brice NL, Pellegrino K,
Parolari L, Shaked JT, Page KJ, Marchildon F, Barrows DW, Carroll
TS, Topilko T, et al: Pharmacological targeting of glutamatergic
neurons within the brainstem for weight reduction. Nat Metab.
4:1495–1513. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
308
|
Woolf CJ: Capturing novel non-opioid pain
targets. Biol Psychiatry. 87:74–81. 2020. View Article : Google Scholar
|
|
309
|
Eisenstein M: Treading the tightrope of
opioid restrictions. Nature. 573:S13–S15. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
310
|
DeWeerdt S: Tracing the US opioid crisis
to its roots. Nature. 573:S10–S12. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
311
|
Stein C: Pain inhibition by opioids-new
concepts. Anaesthesist. 68:97–103. 2019.In German. View Article : Google Scholar : PubMed/NCBI
|
|
312
|
Stanley TH: The fentanyl story. J Pain.
15:1215–1226. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
313
|
Ni Y, Gao H, Ouyang W, Yang G, Cheng M and
Ding L: Pharmacokinetics, metabolite profiling, safety and
tolerability of YZJ-4729 tartrate, a novel G protein-biased
μ-opioid receptor agonist, in healthy Chinese subjects. Front
Pharmacol. 14:12953192024. View Article : Google Scholar
|
|
314
|
Hou Y, Zou G, Wang X, Guo H, Ma X, Cheng
X, Xie Z, Zuo X, Xia J, Mao H, et al: Coordinated activity of a
central pathway drives associative opioid analgesic tolerance. Sci
Adv. 9:eabo56272023. View Article : Google Scholar : PubMed/NCBI
|
|
315
|
Dart RC, Cicero TJ, Surratt HL, Rosenblum
A, Bartelson BB and Adams EH: Assessment of the abuse of tapentadol
immediate release: the first 24 months. J Opioid Manag. 8:395–402.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
316
|
Grosser T, Woolf CJ and FitzGerald GA:
Time for nonaddictive relief of pain. Science. 355:1026–1027. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
317
|
Zhang G, Cui M, Ji R, Zou S, Song L, Fan
B, Yang L, Wang D, Hu S, Zhang X, et al: Neural and molecular
investigation into the paraventricular thalamic-nucleus accumbens
circuit for pain sensation and non-opioid analgesia. Pharmacol Res.
191:1067762023. View Article : Google Scholar : PubMed/NCBI
|
|
318
|
Ai L, Han Y, Ji R, Zhou DY, Zhang WX, Xie
A, Zhai XJ, Cao JL and Zhang HX: Research progress in pain
treatment and analgesic targets. Chin J Pain Med. 29:484–494.
2023.In Chinese.
|
|
319
|
Neubert MJ, Kincaid W and Heinricher MM:
Nociceptive facilitating neurons in the rostral ventromedial
medulla. Pain. 110:158–165. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
320
|
Shi R, Chai Y, Feng H, Xie L, Zhang L,
Zhong T, Chen J, Yan P, Zhu B, Zhao J and Zhou C: Study of the mass
balance, biotransformation and safety of [14C] SHR8554, a novel
μ-opioid receptor injection, in healthy Chinese subjects. Front
Pharmacol. 14:12311022023. View Article : Google Scholar
|
|
321
|
Wang D, Pan X, Zhou Y, Wu Z, Ren K, Liu H,
Huang C, Yu Y, He T, Zhang X, et al: Lateral septum-lateral
hypothalamus circuit dysfunction in comorbid pain and anxiety. Mol
Psychiatry. 28:1090–1100. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
322
|
Ji YW, Shen ZL, Zhang X, Zhang K, Jia T,
Xu X, Geng H, Han Y, Yin C, Yang JJ, et al: Plasticity in ventral
pallidal cholinergic neuron-derived circuits contributes to
comorbid chronic pain-like and depression-like behaviour in male
mice. Nat Commun. 14:21822023. View Article : Google Scholar : PubMed/NCBI
|
|
323
|
Zhang Y, Feng J, Ou C, Zhou X and Liao Y:
AQP4 mitigates chronic neuropathic pain-induced cognitive
impairment in mice. Behav Brain Res. 440:1142822023. View Article : Google Scholar : PubMed/NCBI
|
|
324
|
Sun H, Li Z, Qiu Z, Shen Y, Guo Q, Hu SW,
Ding HL, An S and Cao JL: A common neuronal ensemble in nucleus
accumbens regulates pain-like behaviour and sleep. Nat Commun.
14:47002023. View Article : Google Scholar : PubMed/NCBI
|
|
325
|
Zhou W, Jin Y, Meng Q, Zhu X, Bai T, Tian
Y, Mao Y, Wang L, Xie W, Zhong H, et al: A neural circuit for
comorbid depressive symptoms in chronic pain. Nat Neurosci.
22:1649–1658. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
326
|
Zhang CK, Wang P, Ji YY, Zhao JS, Gu JX,
Yan XX, Fan HW, Zhang MM, Qiao Y, Liu XD, et al: Potentiation of
the lateral habenula-ventral tegmental area pathway underlines the
susceptibility to depression in mice with chronic pain. Sci China
Life Sci. 67:67–82. 2024. View Article : Google Scholar
|
|
327
|
Dong Y, Li Y, Xiang X, Xiao ZC, Hu J, Li
Y, Li H and Hu H: Stress relief as a natural resilience mechanism
against depression-like behaviors. Neuron. 111:3789–3801.e6. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
328
|
Dai W, Huang S, Luo Y, Cheng X, Xia P,
Yang M, Zhao P, Zhang Y, Lin WJ and Ye X: Sex-specific
transcriptomic signatures in brain regions critical for neuropathic
pain-induced depression. Front Mol Neurosci. 15:8869162022.
View Article : Google Scholar : PubMed/NCBI
|
|
329
|
Nguyen VT, Hill B, Sims N, Heck A, Negron
M, Lusk C and Galindo CL: Brain-derived neurotrophic factor rs6265
(Val66Met) single nucleotide polymorphism as a master modifier of
human pathophysiology. Neural Regen Res. 18:102–106. 2023.
View Article : Google Scholar
|
|
330
|
Wang CS, Kavalali ET and Monteggia LM:
BDNF signaling in context: From synaptic regulation to psychiatric
disorders. Cell. 185:62–76. 2022. View Article : Google Scholar :
|
|
331
|
Martínez T, Mariscal G, de la Rubia Ortí
JE and Barrios C: Efficacy and safety of pregabalin and gabapentin
in spinal stenosis: A systematic review and meta-analysis. Front
Pharmacol. 14:12494782023. View Article : Google Scholar : PubMed/NCBI
|
|
332
|
Pu ZH, Peng C, Xie XF, Luo M, Zhu H, Feng
R and Xiong L: Alkaloids from the rhizomes of Ligusticum striatum
exert anti-migraine effects through regulating 5-HT1B
receptor and c-Jun. J Ethnopharmacol. 237:39–46. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
333
|
Pang LN, Chen XM, Lan YY, Huang QL, Yu XM,
Qi L and Wang ZF: Research progress of acupuncture analgesia based
on autonomic nerve regulation pathway. Acupunct Herbal Med.
3:285–295. 2023. View Article : Google Scholar
|
|
334
|
Zhao ZQ: Neural mechanism underlying
acupuncture analgesia. Prog Neurobiol. 85:355–375. 2008. View Article : Google Scholar : PubMed/NCBI
|