|
1
|
Hung LY and Margolis KG: Autism spectrum
disorders and the gastrointestinal tract: Insights into mechanisms
and clinical relevance. Nat Rev Gastroenterol Hepatol. 21:142–163.
2024. View Article : Google Scholar
|
|
2
|
Kanner L: Autistic disturbances of
affective contact. Nerv Child. 2:217–250. 1943.
|
|
3
|
Association AP: Diagnostic and Statistical
Manual of Mental Disorders. 2022.
|
|
4
|
Shaw KA, Williams S, Patrick ME,
Valencia-Prado M, Durkin MS, Howerton EM, Ladd-Acosta CM, Pas ET,
Bakian AV, Bartholomew P, et al: Prevalence and early
identification of autism spectrum disorder among children aged 4
and 8 years-autism and developmental disabilities monitoring
network, 16 sites, United States, 2022. MMWR Surveill Summ.
74:1–22. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bai D, Yip BHK, Windham GC, Sourander A,
Francis R, Yoffe R, Glasson E, Mahjani B, Suominen A, Leonard H, et
al: Association of genetic and environmental factors with autism in
a 5-country cohort. JAMA Psychiatry. 76:1035–1043. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sanders SJ, He X, Willsey AJ,
Ercan-Sencicek AG, Samocha KE, Cicek AE, Murtha MT, Bal VH, Bishop
SL, Dong S, et al: Insights into autism spectrum disorder genomic
architecture and biology from 71 risk loci. Neuron. 87:1215–1233.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
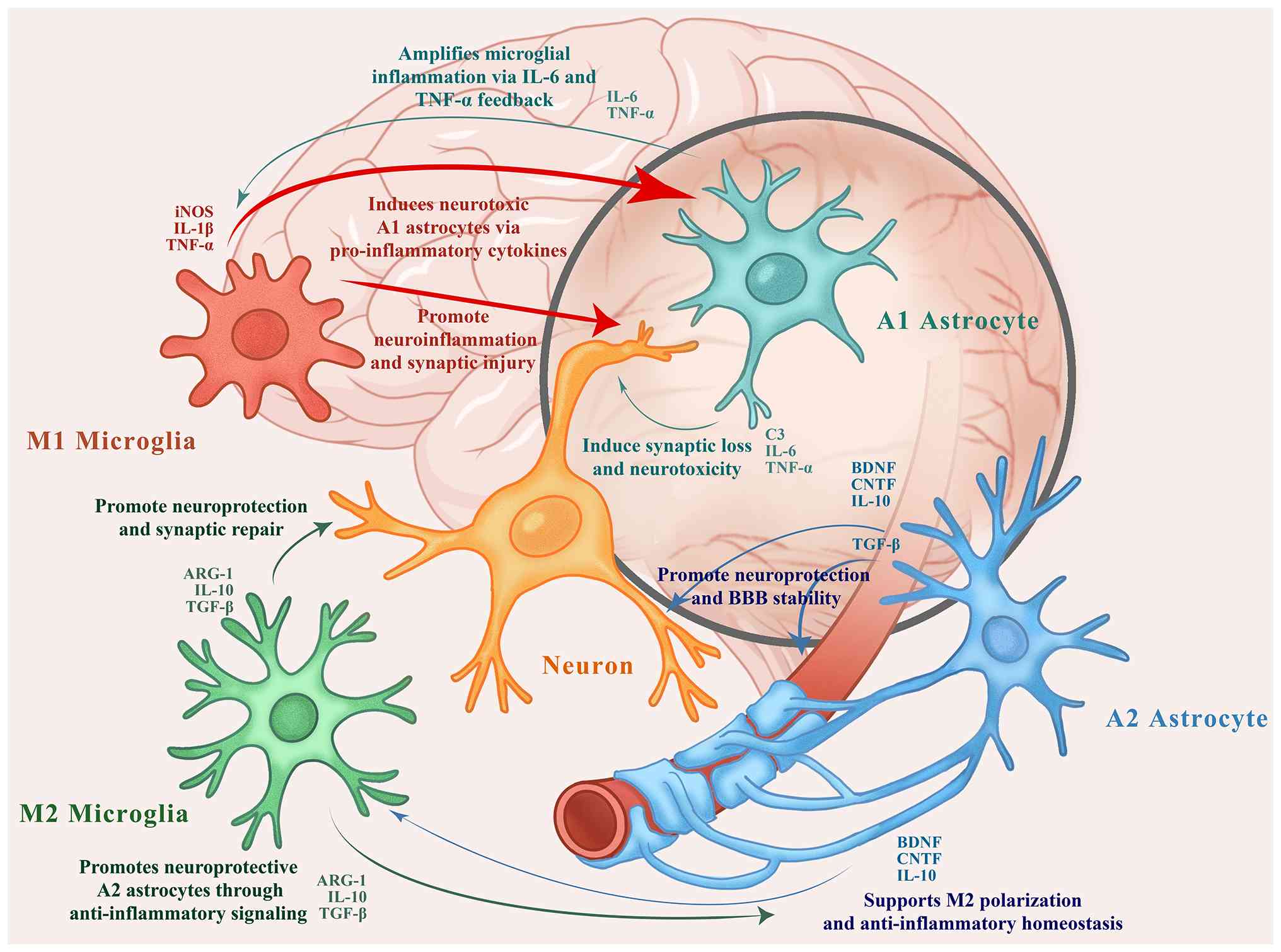
Fu JM, Satterstrom FK, Peng M, Brand H,
Collins RL, Dong S, Wamsley B, Klei L, Wang L, Hao SP, et al: Rare
coding variation provides insight into the genetic architecture and
phenotypic context of autism. Nat Genet. 54:1320–1331. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hirota T and King BH: Autism spectrum
disorder: A review. JAMA. 329:157–168. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Christensen J, Grønborg TK, Sørensen MJ,
Schendel D, Parner ET, Pedersen LH and Vestergaard M: Prenatal
valproate exposure and risk of autism spectrum disorders and
childhood autism. JAMA. 309:1696–1703. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zwaigenbaum L, Brian J and Ip A: Early
detection for autism spectrum disorder in young children. Paediatr
Child Health. 24:424–443. 2019.In English, French. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Robins DL, Casagrande K, Barton M, Chen
CMA, Dumont-Mathieu T and Fein D: Validation of the modified
checklist for Autism in toddlers, revised with follow-up
(M-CHAT-R/F). Pediatrics. 133:37–45. 2014. View Article : Google Scholar :
|
|
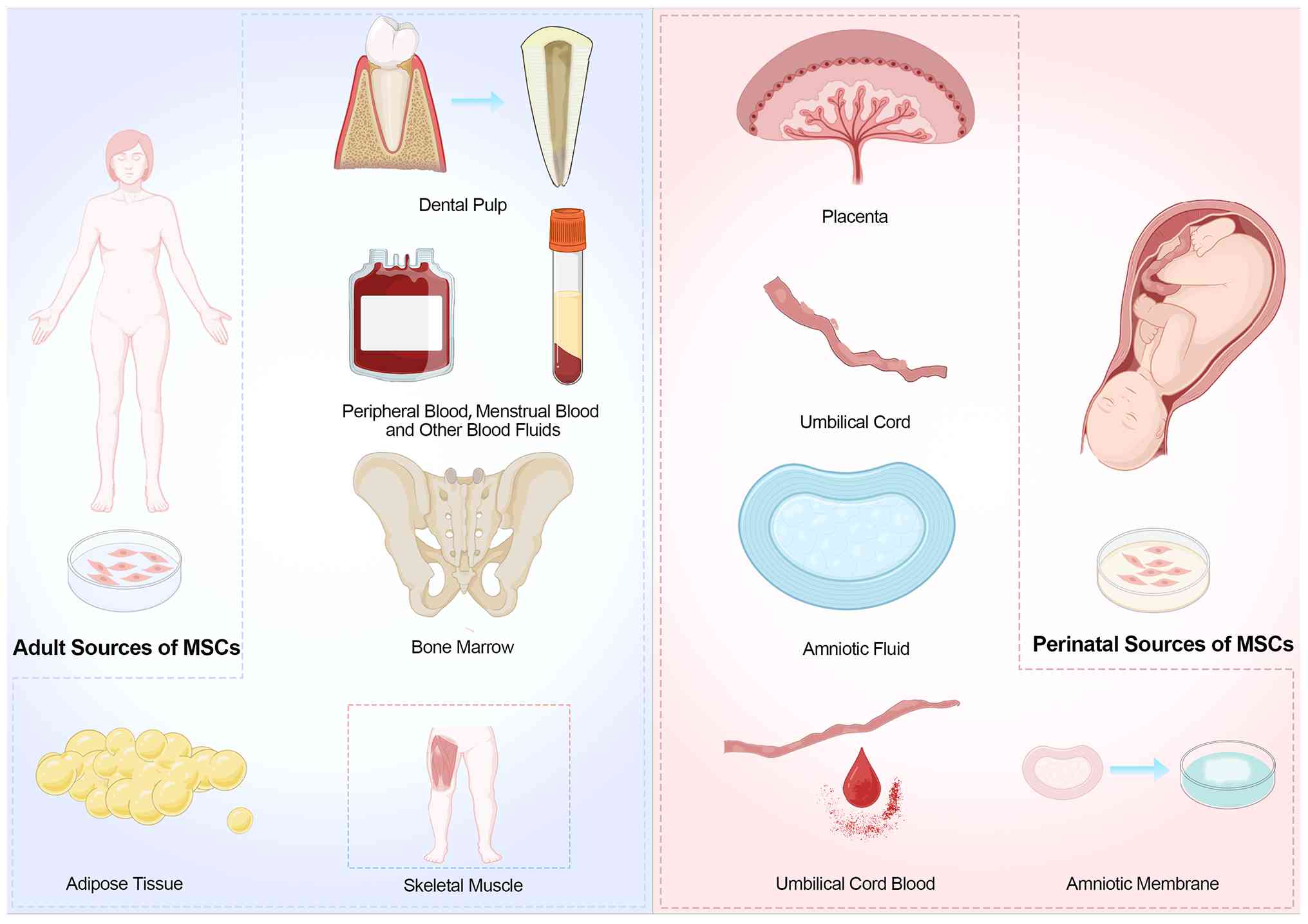
12
|
Volkmar F, Siegel M, Woodbury-Smith M,
King B, McCracken J and State M; American Academy of Child and
Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI):
Practice parameter for the assessment and treatment of children and
adolescents with autism spectrum disorder. J Am Acad Child Adolesc
Psychiatry. 53:237–257. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Song J, Reilly M and Reichow B: Overview
of meta-analyses on naturalistic developmental behavioral
interventions for children with autism spectrum disorder. J Autism
Dev Disord. 55:1–13. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
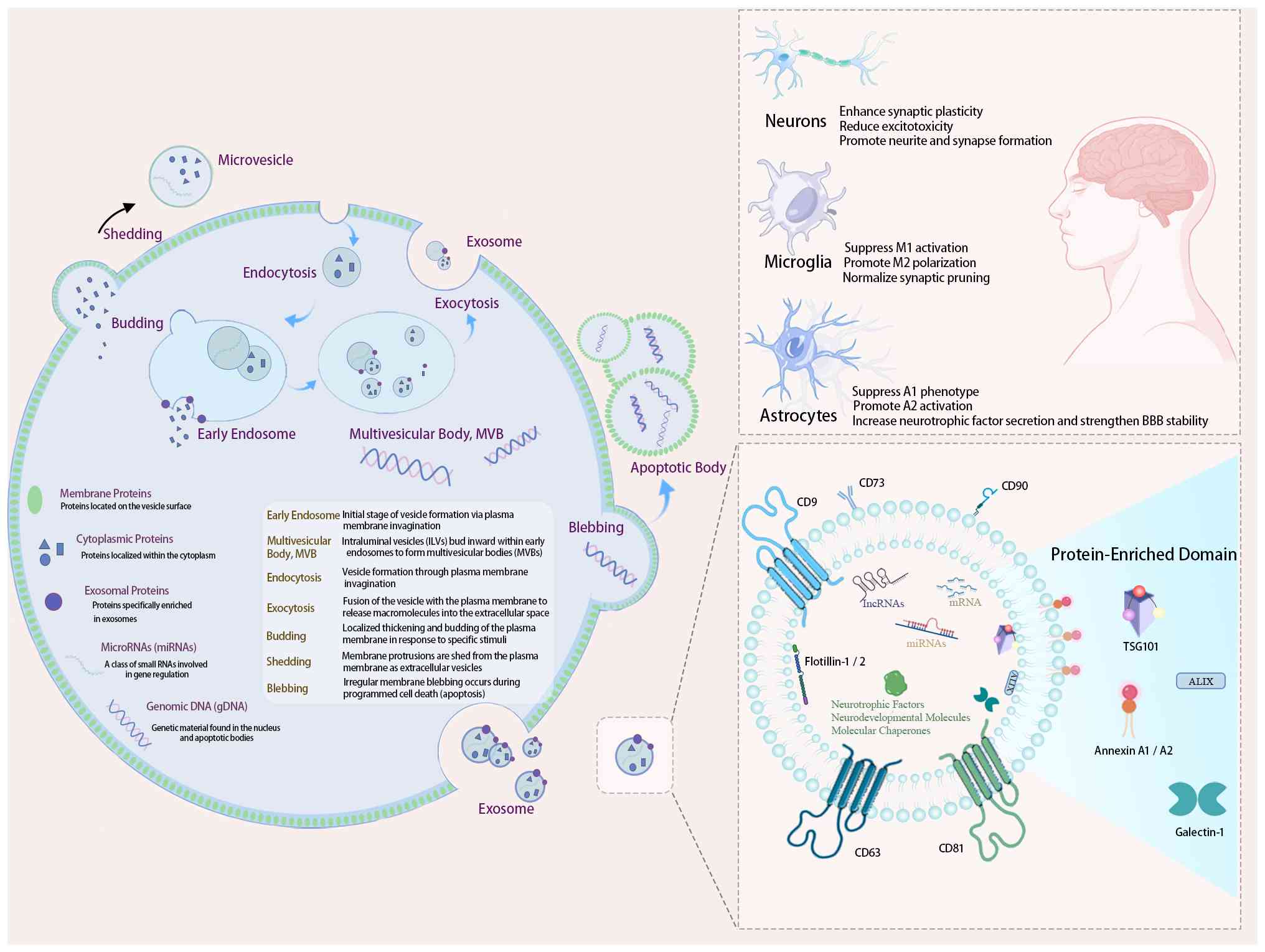
Dawson G, Rogers S, Munson J, Smith M,
Winter J, Greenson J, Donaldson A and Varley J: Randomized,
controlled trial of an intervention for toddlers with autism: The
early start denver model. Pediatrics. 125:e17–e23. 2010. View Article : Google Scholar
|
|
15
|
Wang Z, Loh S, Tian J and Chen QJ: A
meta-analysis of the effect of the early start denver model in
children with autism spectrum disorder. Int J Dev Disabil.
68:587–597. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fieiras C, Chen M, Liquitay CE, Meza N,
Rojas V, Franco J and Madrid E: Risperidone and aripiprazole for
autism spectrum disorder in children: an overview of systematic
reviews. BMJ Evid Based Med. 28:7–14. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Aglinskas A, Hartshorne J and Anzellotti
S: Contrastive machine learning reveals the structure of
neuroanatomical variation within autism. Science. 376:1070–1074.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Pizzano M, Shire S, Shih W, Levato L,
Landa R, Lord C, Smith T and Kasari C: Profiles of minimally verbal
autistic children: Illuminating the neglected end of the spectrum.
Autism Res. 17:1218–1229. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Konečná B, Radošinská J, Keményová P and
Repiská G: Detection of disease-associated microRNAs-application
for autism spectrum disorders. Rev Neurosci. 31:757–769. 2020.
View Article : Google Scholar
|
|
20
|
Yao TT, Chen L, Du Y, Jiang ZY and Cheng
Y: MicroRNAs as regulators, biomarkers, and therapeutic targets in
autism spectrum disorder. Mol Neurobiol. 62:5039–5056. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen W, Ren Q, Zhou J and Liu W:
Mesenchymal stem cell-induced neuroprotection in pediatric
neurological diseases: Recent update of underlying mechanisms and
clinical utility. Appl Biochem Biotechnol. 196:5843–5858. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Liang Y, Duan L, Xu X, Li X, Liu M, Chen
H, Lu J and Xia J: Mesenchymal stem cell-derived exosomes for
treatment of autism spectrum disorder. ACS Appl Bio Mater.
3:6384–6393. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hedayat M, Ahmadi M, Shoaran M and Rezaie
J: Therapeutic application of mesenchymal stem cells derived
exosomes in neurodegenerative diseases: A focus on non-coding RNAs
cargo, drug delivery potential, perspective. Life Sci.
320:1215662023. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Su R: Mesenchymal stem cell exosomes as
nanotherapeutic agents for neurodegenerative diseases. Highl Sci
Eng Technol. 2:7–14. 2022. View Article : Google Scholar
|
|
25
|
Tian MS and Yi XN: The role of mesenchymal
stem cell exosomes in the onset and progression of Alzheimer's
Disease. Biomed Sci. 10:6–13. 2024.
|
|
26
|
Ge Y, Wu J, Zhang L, Huang N and Luo Y: A
new strategy for the regulation of neuroinflammation: Exosomes
derived from mesenchymal stem cells. Cell Mol Neurobiol. 44:242024.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Elsherif R, Abdel-Hafez AM, Hussein O,
Sabry D, Abdelzaher L and Bayoumy AA: The potential ameliorative
effect of mesenchymal stem cells-derived exosomes on cerebellar
histopathology and their modifying role on PI3k-mTOR signaling in
rat model of autism spectrum disorder. J Mol Histol. 56:652025.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhao S, Zhong Y, Shen F, Cheng X, Qing X
and Liu J: Comprehensive exosomal microRNA profile and construction
of competing endogenous RNA network in autism spectrum disorder: A
pilot study. Biomol Biomed. 24:292–301. 2024. View Article : Google Scholar :
|
|
29
|
Perets N, Oron O, Herman S, Elliott E and
Offen D: Exosomes derived from mesenchymal stem cells improved core
symptoms of genetically modified mouse model of autism Shank3B. Mol
Autism. 11:1–13. 2020. View Article : Google Scholar
|
|
30
|
Ressa HJ, Newman BT, Jacokes Z, McPartland
JC, Kleinhans NM, Druzgal TJ, Pelphrey KA and Van Horn JD:
Widespread associations between behavioral metrics and brain
microstructure in ASD suggest age mediates subtypes of ASD.
BioRxiv. 28:2024.09.04.611183. 2024.
|
|
31
|
Almuqhim F and Saeed F: ASD-GResTM: Deep
learning framework for ASD classification using Gramian angular
field. Proceedings (IEEE Int Conf Bioinforma Biomed).
2023:2837–2843. 2023.
|
|
32
|
Tang X, Ran X, Liang Z, Zhuang H, Yan X,
Feng C, Qureshi A, Gao Y and Shen L: Screening biomarkers for
autism spectrum disorder using plasma proteomics combined with
machine learning methods. Clin Chim Acta. 565:1200182025.
View Article : Google Scholar
|
|
33
|
Herbrecht E, Lazari O, Notter M, Kievit E,
Schmeck K and Spiegel R: Short-term and highly intensive early
intervention FIAS: Two-year outcome results and factors of
influence. Front Psychiatry. 11:6872020. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Manohar H and Kandasamy P: Clinical
outcomes of children with ASD-preliminary findings from a 18 month
follow up study. Asian J Psychiatry. 64:1028162021. View Article : Google Scholar
|
|
35
|
Yuan B, Wang M, Wu X, Cheng P, Zhang R,
Zhang R, Yu S, Zhang J, Du Y, Wang X and Qiu Z: Identification of
de novo Mutations in the Chinese autism spectrum disorder cohort
via whole-exome sequencing unveils brain regions implicated in
autism. Neurosci Bull. 39:1469–1480. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Levy RJ and Paşca SP: What have organoids
and assembloids taught us about the pathophysiology of
neuropsychiatric disorders? Biol Psychiatry. 93:632–641. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Al-Beltagi M, Saeed NK, Bediwy AS, Bediwy
EA and Elbeltagi R: Decoding the genetic landscape of autism: A
comprehensive review. World J Clin Pediatr. 13:984682024.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hallmayer J, Cleveland S, Torres A,
Phillips J, Cohen B, Torigoe T, Miller J, Fedele A, Collins J,
Smith K, et al: Genetic heritability and shared environmental
factors among twin pairs with autism. Arch Gen Psychiatry.
68:1095–1102. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Tick B, Bolton P, Happé F, Rutter M and
Rijsdijk F: Heritability of autism spectrum disorders: A
meta-analysis of twin studies. J Child Psychol Psychiatry.
57:585–595. 2016. View Article : Google Scholar
|
|
40
|
Shaw KA, Bilder DA, McArthur D, Williams
AR, Amoakohene E, Bakian AV, Durkin MS, Fitzgerald RT, Furnier SM,
Hughes MM, et al: Early identification of autism spectrum disorder
among children aged 4 years-autism and developmental disabilities
monitoring network, 11 sites, United States, 2020. MMWR Surveill
Summ. 72:1–15. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Barnard RA, Pomaville MB and O'Roak BJ:
Mutations and modeling of the chromatin remodeler CHD8 define an
emerging autism etiology. Front Neurosci. 9:4772015. View Article : Google Scholar
|
|
42
|
Xu B, Ho Y, Fasolino M, Medina J, O'Brien
WT, Lamonica JM, Nugent E, Brodkin ES, Fuccillo MV, Bucan M and
Zhou Z: Allelic contribution of Nrxn1α to autism-relevant
behavioral phenotypes in mice. PLoS Genet. 19:e10106592023.
View Article : Google Scholar
|
|
43
|
Chiola S, Napan KL, Wang Y, Lazarenko RM,
Armstrong CJ, Cui J and Shcheglovitov A: Defective AMPA-mediated
synaptic transmission and morphology in human neurons with
hemizygous SHANK3 deletion engrafted in mouse prefrontal cortex.
Mol Psychiatry. 26:4670–4686. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Guo B, Chen J, Chen Q, Ren K, Feng D, Mao
H, Yao H, Yang J, Liu H, Liu Y, et al: Anterior cingulate cortex
dysfunction underlies social deficits in Shank3 mutant mice. Nat
Neurosci. 22:1223–1234. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Vogt D, Cho KKA, Shelton SM, Paul A, Huang
ZJ, Sohal VS and Rubenstein JLR: Mouse Cntnap2 and human CNTNAP2
ASD alleles cell autonomously regulate PV+ cortical interneurons.
Cereb Cortex. 28:3868–3879. 2018. View Article : Google Scholar
|
|
46
|
Kushima I, Nakatochi M, Aleksic B, Okada
T, Kimura H, Kato H, Morikawa M, Inada T, Ishizuka K, Torii Y, et
al: Cross-Disorder analysis of genic and regulatory copy number
variations in bipolar disorder, schizophrenia, and autism spectrum
disorder. Biol Psychiatry. 92:362–374. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Rein B and Yan Z: 16p11.2 copy number
variations and neurodevelopmental disorders. Trends Neurosci.
43:886–901. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zarrei M, Burton C, Engchuan W, Young EJ,
Higginbotham EJ, MacDonald JR, Trost B, Chan AJS, Walker S,
Lamoureux S, et al: A large data resource of genomic copy number
variation across neurodevelopmental disorders. NPJ Genomic Med.
4:262019. View Article : Google Scholar
|
|
49
|
Costain G, Walker S, Argiropoulos B,
Baribeau DA, Bassett AS, Boot E, Devriendt K, Kellam B, Marshall
CR, Prasad A, et al: Rare copy number variations affecting the
synaptic gene DMXL2 in neurodevelopmental disorders. J Neurodev
Disord. 11:32019. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Hauw JJ, Hausser-Hauw C and Barthélémy C:
Synapse and primary cilia dysfunctions in autism spectrum
disorders. Avenues to normalize these functions. Rev Neurol
(Paris). 180:1059–1070. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ferrucci L, Cantando I, Cordella F, Di
Angelantonio S, Ragozzino D and Bezzi P: Microglia at the
tripartite synapse during postnatal development: implications for
autism spectrum disorders and schizophrenia. Cells. 12:28272023.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Pagani M, Barsotti N, Bertero A, Trakoshis
S, Ulysse L, Locarno A, Miseviciute I, De Felice A, Canella C,
Supekar K, et al: mTOR-related synaptic pathology causes autism
spectrum disorder-associated functional hyperconnectivity. Nat
Commun. 12:60842021. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Giansante G, Marte A, Romei A, Prestigio
C, Onofri F, Benfenati F, Baldelli P and Valente P: Presynaptic
L-type Ca2+ channels increase glutamate release probability and
excitatory strength in the hippocampus during chronic
neuroinflammation. J Neurosci. 40:6825–6841. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Riekki R, Pavlov I, Tornberg J, Lauri S,
Airaksinen M and Taira T: Altered synaptic dynamics and hippocampal
excitability but normal long-term plasticity in mice lacking
hyperpolarizing GABA A receptor-mediated inhibition in CA1
pyramidal neurons. J Neurophysiol. 99:3075–3089. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Cast T, Boesch D, Smyth K, Shaw A,
Ghebrial M and Chanda S: An autism-associated mutation impairs
neuroligin-4 glycosylation and enhances excitatory synaptic
transmission in human neurons. J Neurosci. 41:392–407. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Amal H, Barak B, Bhat V, Gong G, Joughin
BA, Wang X, Wishnok JS, Feng G and Tannenbaum S: Shank3 mutation in
a mouse model of autism leads to changes in the S-nitroso-proteome
and affects key proteins involved in vesicle release and synaptic
function. Mol Psychiatry. 25:1835–1848. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Higa GSV, Viana FJC, Francis-Oliveira J,
Cruvinel E, Franchin TS, Marcourakis T, Ulrich H and De Pasquale R:
Serotonergic neuromodulation of synaptic plasticity.
Neuropharmacology. 257:1100362024. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Liu W, Chen QY, Li XH, Zhou Z and Zhuo M:
Cortical tagged synaptic long-term depression in the anterior
cingulate cortex of adult mice. J Neurosci. 44:e00282420242024.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Hagena H and Manahan-Vaughan D: Interplay
of hippocampal long-term potentiation and long-term depression in
enabling memory representations. Philos Trans R Soc Lond B Biol
Sci. 379:202302292024. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Cong J, Zhuang W, Liu Y, Yin S, Jia H, Yi
C, Chen K, Xue K, Li F, Yao D, et al: Altered default mode network
causal connectivity patterns in autism spectrum disorder revealed
by Liang information flow analysis. Hum Brain Mapp. 44:2279–2293.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Kember J, Patenaude P, Sweatman H, Van
Schaik L, Tabuenca Z and Chai X: Specialization of anterior and
posterior hippocampal functional connectivity differs in autism.
Autism Res. 17:1126–1139. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Grossberg S and Kishnan D: Neural dynamics
of autistic repetitive behaviors and fragile X syndrome: Basal
ganglia movement gating and mGluR-modulated adaptively timed
learning. Front Psychol. 9:2692018. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Xiao T, Wan J, Qu H and Li Y:
Tripartite-motif protein 21 knockdown extenuates LPS-triggered
neurotoxicity by inhibiting microglial M1 polarization via
suppressing NF-κB-mediated NLRP3 inflammasome activation. Arch
Biochem Biophys. 30:1089182021. View Article : Google Scholar
|
|
64
|
Zhou L, Wang D, Qiu X, Zhang W, Gong Z,
Wang Y and Xu X: DHZCP Modulates microglial M1/M2 polarization via
the p38 and TLR4/NF-κB signaling pathways in LPS-stimulated
microglial Cells. Front Pharmacol. 11:11262020. View Article : Google Scholar
|
|
65
|
Tao W, Hu Y, Chen Z, Dai Y, Hu Y and Qi M:
Magnolol attenuates depressive-like behaviors by polarizing
microglia towards the M2 phenotype through the regulation of
Nrf2/HO-1/NLRP3 signaling pathway. Phytomedicine. 91:1536922021.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Tsai C, Chen G, Chen YC, Shen CK, Lu DY,
Yang LY, Chen JH and Yeh WL: Regulatory effects of quercetin on
M1/M2 macrophage polarization and oxidative/antioxidative balance.
Nutrients. 14:672021. View Article : Google Scholar
|
|
67
|
Lehrman EK, Wilton DK, Litvina EY, Welsh
CA, Chang ST, Frouin A, Walker AJ, Heller MD, Umemori H, Chen C and
Stevens B: CD47 protects synapses from excess microglia-mediated
pruning during development. Neuron. 100:120–134.e6. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kobashi S, Terashima T, Katagi M, Nakae Y,
Okano J, Suzuki Y, Urushitani M and Kojima H: Transplantation of
M2-Deviated microglia promotes recovery of motor function after
spinal cord injury in mice. Mol Ther. 28:254–265. 2020. View Article : Google Scholar :
|
|
69
|
Li Y, Liu Z, Song Y, Pan JJ, Jiang Y, Shi
X, Liu C, Ma Y, Luo L, Mamtilahun M, et al: M2 microglia-derived
extracellular vesicles promote white matter repair and functional
recovery via miR-23a-5p after cerebral ischemia in mice.
Theranostics. 12:3553–3573. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Li Z, Xiao J, Xu X, Li W, Zhong R, Qi L,
Chen J, Cui G, Wang S, Zheng Y, et al: M-CSF, IL-6, and TGF-β
promote generation of a new subset of tissue repair macrophage for
traumatic brain injury recovery. Sci Adv. 7:eabb62602021.
View Article : Google Scholar
|
|
71
|
Ding X, Wang J, Huang M, Chen Z, Liu J,
Zhang Q, Zhang C, Xiang Y, Zen K and Li L: Loss of microglial SIRPα
promotes synaptic pruning in preclinical models of
neurodegeneration. Nat Commun. 12:20302021. View Article : Google Scholar
|
|
72
|
Penney J, Ralvenius WT, Loon A, Cerit O,
Dileep V, Milo B, Pao PC, Woolf H and Tsai LH: iPSC-derived
microglia carrying the TREM2 R47H/+ mutation are proinflammatory
and promote synapse loss. Glia. 72:452–469. 2024. View Article : Google Scholar
|
|
73
|
Nugent A, Lin K, Lengerich B, Lianoglou S,
Przybyla L, Davis SS, Llapashtica C, Wang J, Kim DJ, Xia D, et al:
TREM2 regulates microglial cholesterol metabolism upon chronic
phagocytic challenge. Neuron. 105:837–854. 2019. View Article : Google Scholar
|
|
74
|
Kong L, Li W, Chang E, Wang W, Shen N, Xu
X, Wang X, Zhang Y, Sun W, Hu W, et al: mtDNA-STING axis mediates
microglial polarization via IRF3/NF-κB signaling after ischemic
stroke. Front Immunol. 13:8609772022. View Article : Google Scholar
|
|
75
|
Diaz-Castro B, Bernstein AM, Coppola G,
Sofroniew MV and Khakh BS: Molecular and functional properties of
cortical astrocytes during peripherally induced neuroinflammation.
Cell Rep. 36:1095082021. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Chistyakov D, Gavrish G, Goriainov S,
Chistyakov V, Astakhova A, Azbukina N and Sergeeva M: Oxylipin
profiles as functional characteristics of acute inflammatory
responses in astrocytes pre-treated with IL-4, IL-10, or LPS. Int J
Mol Sci. 21:17802020. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Burmeister A, Johnson M, Yaemmongkol J and
Marriott I: Murine astrocytes produce IL-24 and are susceptible to
the immunosuppressive effects of this cytokine. J
Neuroinflammation. 16:552019. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Li D, Liu X, Liu T, Liu H, Tong L, Jia SW
and Wang YF: Neurochemical regulation of the expression and
function of glial fibrillary acidic protein in astrocytes. Glia.
68:878–897. 2020. View Article : Google Scholar
|
|
79
|
Wilhelmsson U, Pozo-Rodrigalvarez A, Kalm
M, de Pablo Y, Widestrand Å, Pekna M and Pekny M: The role of GFAP
and vimentin in learning and memory. Biol Chem. 400:1147–1156.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Ribot J, Breton R, Calvo C, Moulard J,
Ezan P, Zapata J, Samama K, Moreau M, Bemelmans AP, Sabatet V, et
al: Astrocytes close the mouse critical period for visual
plasticity. Science. 373:77–81. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Hasel P, Rose I, Sadick J, Kim R and
Liddelow S: Neuroinflammatory astrocyte subtypes in the mouse
brain. Nat Neurosci. 24:1475–1487. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Ziff O, Clarke B, Taha D, Crerar H,
Luscombe N and Patani R: Meta-analysis of human and mouse ALS
astrocytes reveals multi-omic signatures of inflammatory reactive
states. Genome Res. 32:71–84. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Liddelow SA, Guttenplan KA, Clarke LE,
Bennett FC, Bohlen CJ, Schirmer L, Bennett ML, Münch AE, Chung WS,
Peterson TC, et al: Neurotoxic reactive astrocytes are induced by
activated microglia. Nature. 541:481–487. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Versele R, Sevin E, Gosselet F, Fenart L
and Candela P: TNF-α and IL-1β modulate blood-brain barrier
permeability and decrease amyloid-β peptide efflux in a human
blood-brain barrier model. Int J Mol Sci. 23:102352022. View Article : Google Scholar
|
|
85
|
Takahashi K, Ishibashi Y, Chujo K, Suzuki
I and Sato K: Neuroprotective potential of L-glutamate transporters
in human induced pluripotent stem cell-derived neural cells against
excitotoxicity. Int J Mol Sci. 24:126052023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Luo Y, Yu Y, He H and Fan N: Acute
ketamine induces neuronal hyperexcitability and deficits in
prepulse inhibition by upregulating IL-6. Prog Neuropsychopharmacol
Biol Psychiatry. 130:1109132024. View Article : Google Scholar
|
|
87
|
Friedenstein AJ, Chailakhjan RK and
Lalykina KS: The development of fibroblast colonies in monolayer
cultures of guinea-pig bone marrow and spleen cells. Cell Tissue
Kinet. 3:393–403. 1970.PubMed/NCBI
|
|
88
|
Brown SE, Tong W and Krebsbach PH: The
derivation of mesenchymal stem cells from human embryonic stem
cells. Cells Tissues Organs. 189:256–260. 2009. View Article : Google Scholar :
|
|
89
|
Stefańska K, Němcová L, Blatkiewicz M, Zok
A, Kaczmarek M, Pieńkowski W, Mozdziak P, Piotrowska-Kempisty H and
Kempisty B: Expression profile of new marker genes involved in
differentiation of human Wharton's Jelly-derived mesenchymal stem
cells into chondrocytes, osteoblasts, adipocytes and neural-like
cells. Int J Mol Sci. 24:129392023. View Article : Google Scholar
|
|
90
|
Lee H, Kim SHL, Yoon H, Ryu J, Park HH,
Hwang NS and Park TH: Intracellular delivery of recombinant RUNX2
facilitated by cell-penetrating protein for the osteogenic
differentiation of hMSCs. ACS Biomater Sci Eng. 6:5202–5214. 2020.
View Article : Google Scholar
|
|
91
|
Zhang X, Liu L, Dou C, Cheng P, Liu L, Liu
H, Ren S, Wang C, Jia S, Chen L, et al: PPAR gamma-regulated
MicroRNA 199a-5p underlies bone marrow adiposity in aplastic
anemia. Mol Ther Nucleic Acids. 17:678–687. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Caron M, Eveque M, Cillero-Pastor B,
Heeren RMA, Housmans B, Derks K, Cremers A, Peffers MJ, van Rhijn
LW, van den Akker G and Welting TJM: Sox9 determines translational
capacity during early chondrogenic differentiation of ATDC5 cells
by regulating expression of ribosome biogenesis factors and
ribosomal proteins. Front Cell Dev Biol. 9:6860962021. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Yan Z, Shi X, Wang H, Si C, Liu Q and Du
Y: Neurotrophin-3 promotes the neuronal differentiation of BMSCs
and improves cognitive function in a rat model of Alzheimer's
disease. Front Cell Neurosci. 15:6293562021. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Chen QH, Wu F, Liu L, Chen HB, Zheng R,
Wang HL and Yu LN: Mesenchymal stem cells regulate the Th17/Treg
cell balance partly through hepatocyte growth factor in vitro. Stem
Cell Res Ther. 11:912020. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Chen L, Zhang Q, Chen QH, Ran FY, Yu LM,
Liu X, Fu Q, Song GY, Tang JM and Zhang T: Combination of G-CSF and
AMD3100 improves the anti-inflammatory effect of mesenchymal stem
cells on inducing M2 polarization of macrophages through
NF-κB-IL1RA signaling pathway. Front Pharmacol. 10:5792019.
View Article : Google Scholar
|
|
96
|
Soufihasanabad S, Mahmoudi M,
Taghavi-Farahabadi M, Mirsanei Z, Mahmoudi R, Abdallah JK, Babaei E
and Hashemi SM: In vivo polarization of M2 macrophages by
mesenchymal stem cell-derived extracellular vesicles: A novel
approach to macrophage polarization and its potential in treating
inflammatory diseases. Med Hypotheses. 187:1113532024. View Article : Google Scholar
|
|
97
|
Huaman O, Bahamonde J, Cahuascanco B,
Jervis M, Palomino J, Torres C and Peralta O: Immunomodulatory and
immunogenic properties of mesenchymal stem cells derived from
bovine fetal bone marrow and adipose tissue. Res Vet Sci.
124:212–222. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Yang S, Wei Y, Sun R, Lu W, Lv H, Xiao X,
Cao Y, Jin X and Zhao M: Umbilical cord blood-derived mesenchymal
stromal cells promote myeloid-derived suppressor cell proliferation
by secreting HLA-G to reduce acute graft-versus-host disease after
hematopoietic stem cell transplantation. Cytotherapy. 22:718–733.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
He J, Zhang N, Zhu Y, Jin R and Wu F: MSC
spheroids-loaded collagen hydrogels simultaneously promote neuronal
differentiation and suppress inflammatory reaction through PI3K-Akt
signaling pathway. Biomaterials. 265:1204482020. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Huang W, Wang C, Xie L, Wang X, Zhang L,
Chen C and Jiang B: Traditional two-dimensional mesenchymal stem
cells (MSCs) are better than spheroid MSCs on promoting retinal
ganglion cells survival and axon regeneration. Exp Eye Res.
185:1076992019. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Zavatti M, Gatti M, Beretti F, Palumbo C
and Maraldi T: Exosomes derived from human amniotic fluid
mesenchymal stem cells preserve microglia and neuron cells from Aβ.
Int J Mol Sci. 23:49672022. View Article : Google Scholar
|
|
102
|
Angeloni C, Gatti M, Prata C, Hrelia S and
Maraldi T: Role of mesenchymal stem cells in counteracting
oxidative stress-related neurodegeneration. Int J Mol Sci.
21:32992020. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Zeng CW: Multipotent mesenchymal stem
cell-based therapies for spinal cord injury: Current progress and
future prospects. Biology (Basel). 12:6532023.PubMed/NCBI
|
|
104
|
Sun S, Luo S, Chen J, Zhang O, Wu Q, Zeng
N, Bi J, Zheng C, Yan T, Li Z, et al: Human umbilical cord-derived
mesenchymal stem cells alleviate valproate-induced immune stress
and social deficiency in rats. Front Psychiatry. 15:14316892024.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Yang Y, Peng Y, Li Y, Shi T, Luan Y and
Yin C: Role of stem cell derivatives in inflammatory diseases.
Front Immunol. 14:11539012023. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Moghadasi S, Elveny M, Rahman H, Suksatan
W, Jalil AT, Abdelbasset WK, Yumashev AV, Shariatzadeh S, Motavalli
R, Behzad F, et al: A paradigm shift in cell-free approach: The
emerging role of MSCs-derived exosomes in regenerative medicine. J
Transl Med. 19:3022021. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Krylova S and Feng D: The machinery of
exosomes: Biogenesis, release, and uptake. Int J Mol Sci.
24:13372023. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Zheng D, Huo M, Li B, Wang W, Piao H, Wang
Y, Zhu Z, Li D, Wang T and Liu K: The role of exosomes and exosomal
MicroRNA in cardiovascular disease. Front Cell Dev Biol.
8:6161612021. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Tenchov R, Sasso J, Wang X, Liaw W, Chen
CA and Zhou Q: Exosomes-Nature's lipid nanoparticles, a rising star
in drug delivery and diagnostics. ACS Nano. 16:17802–17846. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Wu J, Li H, He J, Tian X, Luo S, Li J, Li
W, Zhong J, Zhang H, Huang Z, et al: Downregulation of
microRNA-9-5p promotes synaptic remodeling in the chronic phase
after traumatic brain injury. Cell Death Dis. 12:92021. View Article : Google Scholar :
|
|
111
|
Corradi E, Costa ID, Gavoci A, Iyer A,
Roccuzzo M, Otto TA, Oliani E, Bridi S, Strohbuecker S,
Santos-Rodriguez G, et al: Axonal precursor miRNAs hitchhike on
endosomes and locally regulate the development of neural circuits.
EMBO J. 39:e1025132020. View Article : Google Scholar
|
|
112
|
Li R, Zhao K, Ruan Q, Meng C and Yin F:
Bone marrow mesenchymal stem cell-derived exosomal microRNA-124-3p
attenuates neurological damage in spinal cord ischemia-reperfusion
injury by downregulating Ern1 and promoting M2 macrophage
polarization. Arthritis Res Ther. 22:752020. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Jiang D, Gong F, Ge X, Lv C, Huang C, Feng
S, Zhou Z, Rong Y, Wang J, Ji C, et al: Neuron-derived
exosomes-transmitted miR-124-3p protect traumatically injured
spinal cord by suppressing the activation of neurotoxic microglia
and astrocytes. J Nanobiotechnology. 18:1052020. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Song Y, Li Z, He T, Qu M, Jiang L, Li W,
Shi X, Pan J, Zhang L, Wang Y, et al: M2 microglia-derived exosomes
protect the mouse brain from ischemia-reperfusion injury via
exosomal miR-124. Theranostics. 9:2910–2923. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Cui Y, Yin Y, Xiao Z, Zhao Y, Chen B, Yang
B, Xu B, Song H, Zou Y, Ma X and Dai J: LncRNA Neat1 mediates
miR-124-induced activation of Wnt/β-catenin signaling in spinal
cord neural progenitor cells. Stem Cell Res Ther. 10:4002019.
View Article : Google Scholar
|
|
116
|
Han P, Sunada-Nara K, Kawashima N, Fujii
M, Wang S, Kieu TQ, Yu Z and Okiji T: MicroRNA-146b-5p suppresses
pro-inflammatory mediator synthesis via targeting TRAF6, IRAK1, and
RELA in lipopolysaccharide-stimulated human dental pulp cells. Int
J Mol Sci. 24:74332023. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Ho D, Lynd TO, Jun C, Shin J, Millican RC,
Estep BK, Chen J, Zhang X, Brott BC, Kim DW, et al: MiR-146a
encapsulated liposomes reduce vascular inflammatory responses
through decrease of ICAM-1 expression, macrophage activation, and
foam cell formation. Nanoscale. 15:3461–3474. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Venuti A, Musarra-Pizzo M, Pennisi R,
Tankov S, Medici MA, Mastino A, Rebane A and Sciortino M:
HSV-1\EGFP stimulates miR-146a expression in a NF-κB-dependent
manner in monocytic THP-1 cells. Sci Rep. 9:51572019. View Article : Google Scholar
|
|
119
|
Riazifar M, Mohammadi M, Pone E, Yeri A,
Lässer C, Segaliny AI, McIntyre LL, Shelke GV, Hutchins E, Hamamoto
A, et al: Stem cell-derived exosomes as nanotherapeutics for
autoimmune and neurodegenerative disorders. ACS Nano. 13:6670–668.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Long X, Yao X, Jiang QQ, Yang Y, He X,
Tian W, Zhao K and Zhang H: Astrocyte-derived exosomes enriched
with miR-873a-5p inhibit neuroinflammation via microglia phenotype
modulation after traumatic brain injury. J Neuroinflammation.
17:892020. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Wang QM, Lian GY, Sheng SM, Xu J, Ye LL,
Min C and Guo SF: Exosomal lncRNA NEAT1 inhibits NK-Cell activity
to promote multiple myeloma cell immune escape via an EZH2/PBX1
axis. Mol Cancer Res. 22:125–136. 2024. View Article : Google Scholar
|
|
122
|
Zhao F, Li Z, Dong Z, Wang Z, Guo P, Zhang
D and Li S: Exploring the potential of exosome-related LncRNA pairs
as predictors for immune microenvironment, survival outcome, and
microbiotain landscape in esophageal squamous cell carcinoma. Front
Immunol. 13:9181542022. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Zhang W, Yan Y, Peng J, Thakur A, Bai N,
Yang K and Xu Z: Decoding roles of exosomal lncRNAs in tumor-immune
regulation and therapeutic potential. Cancers (Basel). 15:2862022.
View Article : Google Scholar
|
|
124
|
Taha E, Ono K and Eguchi T: Roles of
extracellular HSPs as biomarkers in immune surveillance and immune
evasion. Int J Mol Sci. 20:45882019. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Montesinos JJ, López-García L,
Cortés-Morales VA, Arriaga-Pizano L, Valle-Ríos R, Fajardo-Orduña
GR and Castro-Manrreza ME: Human bone marrow mesenchymal
stem/stromal cells exposed to an inflammatory environment increase
the expression of ICAM-1 and release microvesicles enriched in this
adhesive molecule: Analysis of the participation of TNF-α and
IFN-γ. J Immunol Res. 2020:88396252020. View Article : Google Scholar
|
|
126
|
Wu D, Deng S, Li L, Liu T, Zhang T, Li J,
Yu Y and Xu Y: TGF-β1-mediated exosomal lnc-MMP2-2 increases
blood-brain barrier permeability via the miRNA-1207-5p/EPB41L5 axis
to promote non-small cell lung cancer brain metastasis. Cell Death
Dis. 12:7212021. View Article : Google Scholar
|
|
127
|
Cauvi D, Hawisher D, Derunes J, Rodriguez
E and De Maio A: Membrane phospholipids activate the inflammatory
response in macrophages by various mechanisms. FASEB J.
38:e236192024. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Zhou W, Silva M, Feng C, Zhao S, Liu L, Li
S, Zhong J and Zheng W: Exosomes derived from human placental
mesenchymal stem cells enhanced the recovery of spinal cord injury
by activating endogenous neurogenesis. Stem Cell Res Ther.
12:1742021. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Harrell CR, Volarevic A, Djonov V and
Volarevic V: Mesenchymal stem cell-derived exosomes as new remedy
for the treatment of neurocognitive disorders. Int J Mol Sci.
22:14332021. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Xun C, Ge L, Tang F, Wang L, Zhuo Y, Long
L, Qi J, Hu L, Duan D, Chen P and Lu M: Insight into the proteomic
profiling of exosomes secreted by human OM-MSCs reveals a new
potential therapy. Biomed Pharmacother. 131:1105842020. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Liu A, Li C, Wang C, Liang X and Zhang X:
Impact of mesenchymal stem cells on the gut microbiota and
microbiota associated functions in inflammatory bowel disease: A
systematic review of preclinical evidence on animal models. Curr
Stem Cell Res Ther. 19:981–992. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Ocansey D, Zhang Z, Xu X, Liu L, Amoah S,
Chen X, Wang B, Zhang X and Mao F: Mesenchymal stem cell-derived
exosome mitigates colitis via the modulation of the gut
metagenomics-metabolomics-farnesoid X receptor axis. Biomater Sci.
10:4822–4836. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Gu L, Ren F, Fang X, Yuan L, Liu G and
Wang S: Exosomal MicroRNA-181a derived from mesenchymal stem cells
improves gut microbiota composition, barrier function, and
inflammatory status in an experimental colitis model. Front Med
(Lausanne). 8:6606142021. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Alexandrov P, Zhai Y, Li W and Lukiw W:
Lipopolysaccharide-stimulated, NF-kB-, miRNA-146a- and
miRNA-155-mediated molecular-genetic communication between the
human gastrointestinal tract microbiome and the brain. Folia
Neuropathol. 57:211–219. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Geffen Y, Perets N, Horev R, Yudin D, Oron
O, Elliott E, Marom E, Danon U and Offen D: Exosomes derived from
adipose mesenchymal stem cells: A potential non-invasive intranasal
treatment for autism. Cytotherapy. 22:S492020.
|
|
136
|
Geffen Y, Horev R, Perets N, Marom E,
Danon U and Offen D: Immuno-modulation and neuroprotection mediate
the therapeutic effect of exosomes in mice model of autism.
Cytotherapy. 22:S49–S50. 2020.
|
|
137
|
Garcia G, Pinto S, Ferreira S, Lopes D,
Serrador MJ, Fernandes A, Vaz AR, Mendonça A, Edenhofer F, Malm T,
et al: Emerging role of miR-21-5p in neuron-glia dysregulation and
exosome transfer using multiple models of Alzheimer's disease.
Cells. 11:33772022. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Zhang Y, Zhang Y, Chopp M, Pang H, Zhang
Z, Mahmood A and Xiong Y: MiR-17-92 cluster-enriched exosomes
derived from human bone marrow mesenchymal stromal cells improve
tissue and functional recovery in rats after traumatic brain
injury. J Neurotrauma. 38:1535–1550. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Fan B, Chopp M, Zhang Z and Liu X:
Treatment of diabetic peripheral neuropathy with engineered
mesenchymal stromal cell-derived exosomes enriched with
microRNA-146a provide amplified therapeutic efficacy. Exp Neurol.
341:1136942021. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Chen Y, Tian Z, He L, Liu C, Wang N, Rong
L and Liu B: Exosomes derived from miR-26a-modified MSCs promote
axonal regeneration via the PTEN/AKT/mTOR pathway following spinal
cord injury. Stem Cell Res Ther. 12:2242021. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Perets N, Hertz S, London M and Offen D:
Intranasal administration of exosomes derived from mesenchymal stem
cells ameliorates autistic-like behaviors of BTBR mice. Mol Autism.
9:1–12. 2018. View Article : Google Scholar
|
|
142
|
Kabataş S, Civelek E, Savrunlu E,
Karaaslan U, Yıldız Ö and Karaöz E: Advances in the treatment of
autism spectrum disorder: Wharton jelly mesenchymal stem cell
transplantation. World J Methodol. 15:958572025. View Article : Google Scholar
|
|
143
|
Barmada A, Sharan J, Band N and Prodromos
C: Serious adverse events have not been reported with spinal
intrathecal injection of mesenchymal stem cells: A systematic
review. Curr Stem Cell Res Ther. 18:829–833. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Lv YT, Zhang Y, Liu M, Qiuwaxi JN, Ashwood
P, Cho SC, Huan Y, Ge RC, Chen XW, Wang ZJ, et al: Transplantation
of human cord blood mononuclear cells and umbilical cord-derived
mesenchymal stem cells in autism. J Transl Med. 11:1962013.
View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Shroff G: Human embryonic stem cells in
the treatment of autism: A case series. Innov Clin Neurosci.
14:12–16. 2017.PubMed/NCBI
|
|
146
|
Chez M, Lepage C, Parise C, Dang-Chu A,
Hankins A and Carroll M: Safety and observations from a
placebo-controlled, crossover study to assess use of autologous
umbilical cord blood stem cells to improve symptoms in children
with Autism. Stem Cells Transl Med. 7:333–341. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Simhal AK, Carpenter KLH, Nadeem S,
Kurtzberg J, Song A, Tannenbaum A, Sapiro G and Dawson G: Measuring
robustness of brain networks in autism spectrum disorder with Ricci
curvature. Sci Rep. 10:108192020. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Thanh LN, Nguyen HP, Ngo MD, Bui VA, Dam
PTM, Bui HTP, Ngo DV, Tran KT, Dang TTT, Duong BD, et al: Outcomes
of bone marrow mononuclear cell transplantation combined with
interventional education for autism spectrum disorder. Stem Cells
Transl Med. 10:14–26. 2021. View Article : Google Scholar
|
|
149
|
Al-Dhalimy A, Salim HM, Shather A, Naser
IH, Hizam M and Alshujery MK: The pathological and therapeutically
role of mesenchymal stem cell (MSC)-derived exosome in degenerative
diseases; Particular focus on LncRNA and microRNA. Pathol Res
Prract. 250:1547782023. View Article : Google Scholar
|
|
150
|
Dilsiz N: Mesenchymal Stem Cell-Derived
Exosomes in Clinical Trial. Pak BioMed J. 8:12025.
|
|
151
|
Hadizadeh A, Akbari-Asbagh R,
Heirani-Tabasi A, Soleimani M, Gorovanchi P, Daryani NE, Vahedi A,
Nazari H, Banikarimi SP, Dibavar MA, et al: Localized
administration of mesenchymal stem cell-derived exosomes for the
treatment of refractory perianal fistula in Crohn's disease
patients: A phase II clinical trial. Dis Colon Rectum.
67:1564–1575. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Fahlevie F, Apriningsih H, Sutanto Y,
Reviono R, Adhiputri A, Aphridasari J and Prasetyo W: Effects of
secretome supplementation on interleukin-6, tumor necrosis
factor-α, procalcitonin, and the length of stay in acute
exacerbation COPD patients. Narra J. 3:e1712023. View Article : Google Scholar
|
|
153
|
Xie M, Tao L, Zhang Z and Wang W:
Mesenchymal stem cells mediated drug delivery in tumor-targeted
therapy. Curr Drug Deliv. 18:876–891. 2020.PubMed/NCBI
|
|
154
|
Xu S, Liu B, Fan J, Xue C, Lu Y, Li C and
Cui D: Engineered mesenchymal stem cell-derived exosomes with high
CXCR4 levels for targeted siRNA gene therapy against cancer.
Nanoscale. 14:4098–4113. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Tang Y, Zhou Y and Li HJ: Advances in
mesenchymal stem cell exosomes: A review. Stem Cell Res Ther.
12:712021. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Abdelsalam M, Ahmed M, Osaid Z, Hamoudi R
and Harati R: Insights into exosome transport through the
blood-brain barrier and the potential therapeutical applications in
brain diseases. Pharmaceuticals (Basel). 16:5712023. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Mohamed-Ahmed S, Fristad I, Lie S, Suliman
S, Mustafa K, Vindenes H and Idris S: Adipose-derived and bone
marrow mesenchymal stem cells: A donor-matched comparison. Stem
Cell Res Ther. 9:1682018. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Gowen A, Shahjin F, Chand S, Odegaard KE
and Yelamanchili SV: Mesenchymal stem cell-derived extracellular
vesicles: Challenges in clinical applications. Front Cell Dev Biol.
8:1492020. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Li B, Chen X, Qiu W, Zhao R, Duan J, Zhang
S, Pan Z, Zhao S, Guo Q, Qi Y, et al: Synchronous disintegration of
ferroptosis defense axis via engineered exosome-conjugated magnetic
nanoparticles for glioblastoma therapy. Adv Sci (Weinh).
9:e21054512022. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Zhang M, Zhang R, Chen H, Zhang X, Zhang
Y, Liu H, Li C, Chen Y, Zeng Q and Huang G: Injectable
supramolecular hybrid hydrogel delivers IL-1β-stimulated exosomes
to target neuroinflammation. ACS Appl Mater Interfaces.
15:6486–6498. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Feng C, Xiong Z, Wang C, Xiao W, Xiao H,
Xie K, Chen K, Liang H, Zhang X and Yang H: Folic acid-modified
Exosome-PH20 enhances the efficiency of therapy via modulation of
the tumor microenvironment and directly inhibits tumor cell
metastasis. Bioact Mater. 6:963–974. 2021.
|
|
162
|
Zhan Q, Yi K, Qi H, Li S, Li X, Wang Q,
Wang Y, Liu C, Qiu M, Yuan X, et al: Engineering blood exosomes for
tumor-targeting efficient gene/chemo combination therapy.
Theranostics. 10:7889–7905. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Zhao Y, Gan YM, Xu G, Hua K and Liu D:
Exosomes from MSCs overexpressing microRNA-223-3p attenuate
cerebral ischemia through inhibiting microglial M1 polarization
mediated inflammation. Life Sci. 260:1184032020. View Article : Google Scholar : PubMed/NCBI
|