|
1
|
GBD 2017 Pancreatic Cancer Collaborators:
The global, regional, and national burden of pancreatic cancer and
its attributable risk factors in 195 countries and territories,
1990-2017: A systematic analysis for the global burden of disease
study 2017. Lancet Gastroenterol Hepatol. 4:934–947. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel RL, Giaquinto AN and Jemal A:
Cancer statistics, 2024. CA Cancer J Clin. 74:12–49.
2024.PubMed/NCBI
|
|
3
|
He J, Ahuja N, Makary MA, Cameron JL,
Eckhauser FE, Choti MA, Hruban RH, Pawlik TM and Wolfgang CL: 2564
resected periampullary adenocarcinomas at a single institution:
Trends over three decades. HPB (Oxford). 16:83–90. 2014. View Article : Google Scholar
|
|
4
|
Zeng L, Wu Z, Yang J, Zhou Y and Chen R:
Association of genetic risk and lifestyle with pancreatic cancer
and their age dependency: A large prospective cohort study in the
UK Biobank. BMC Med. 21:4892023. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li X and Liang Z: Causal effect of gut
microbiota on pancreatic cancer: A Mendelian randomization and
colocalization study. J Cell Mol Med. 28:e182552024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bhatt AP, Redinbo MR and Bultman SJ: The
role of the microbiome in cancer development and therapy. CA Cancer
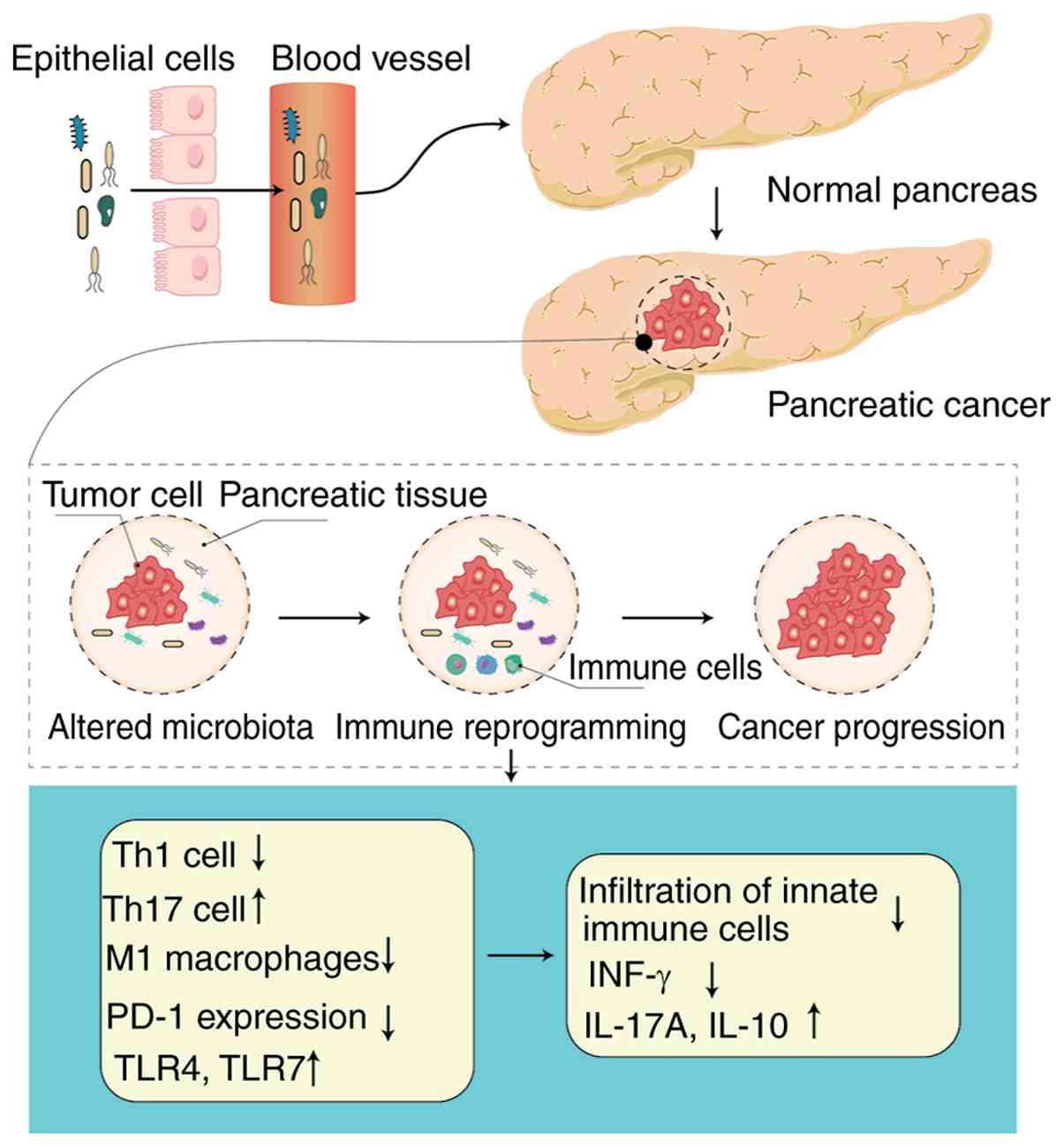
J Clin. 67:326–344. 2017.PubMed/NCBI
|
|
7
|
Li P, Shu Y and Gu Y: The potential role
of bacteria in pancreatic cancer: A systematic review.
Carcinogenesis. 41:397–404. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
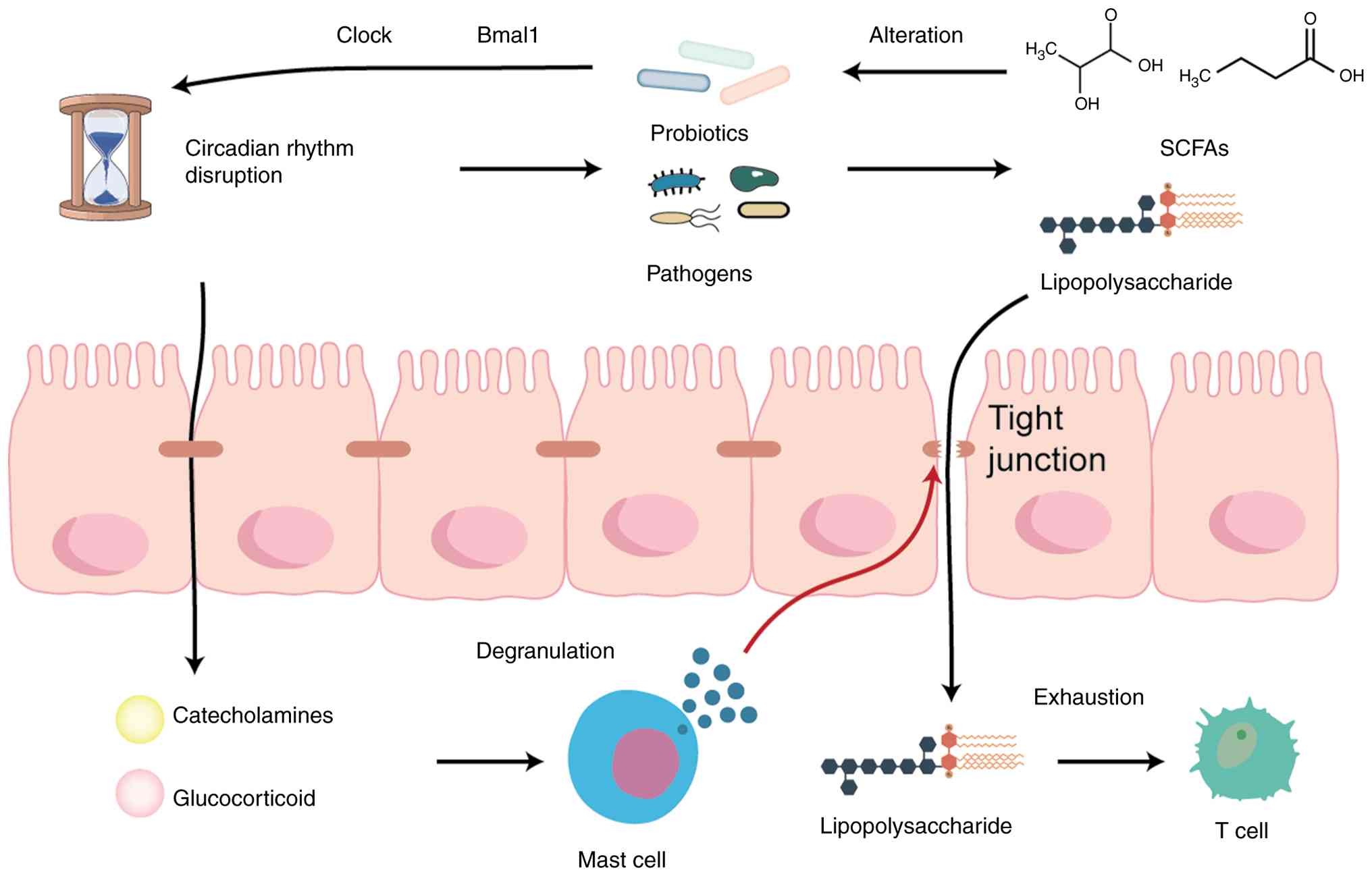
Bass J and Lazar MA: Circadian time
signatures of fitness and disease. Science. 354:994–999. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Allada R and Bass J: Circadian mechanisms
in medicine. N Engl J Med. 384:550–561. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li W, Liu L, Liu D, Lin S, Yang Y, Tang W
and Gong L: Decreased circadian component Bmal1 predicts tumor
progression and poor prognosis in human pancreatic ductal
adenocarcinoma. Biochem Biophys Res Commun. 472:156–162. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zarrinpar A, Chaix A, Yooseph S and Panda
S: Diet and feeding pattern affect the diurnal dynamics of the gut
microbiome. Cell Metab. 20:1006–1017. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Paulose JK, Wright JM, Patel AG and
Cassone VM: Human gut bacteria are sensitive to melatonin and
express endogenous circadian rhythmicity. PLoS One.
11:e01466432016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
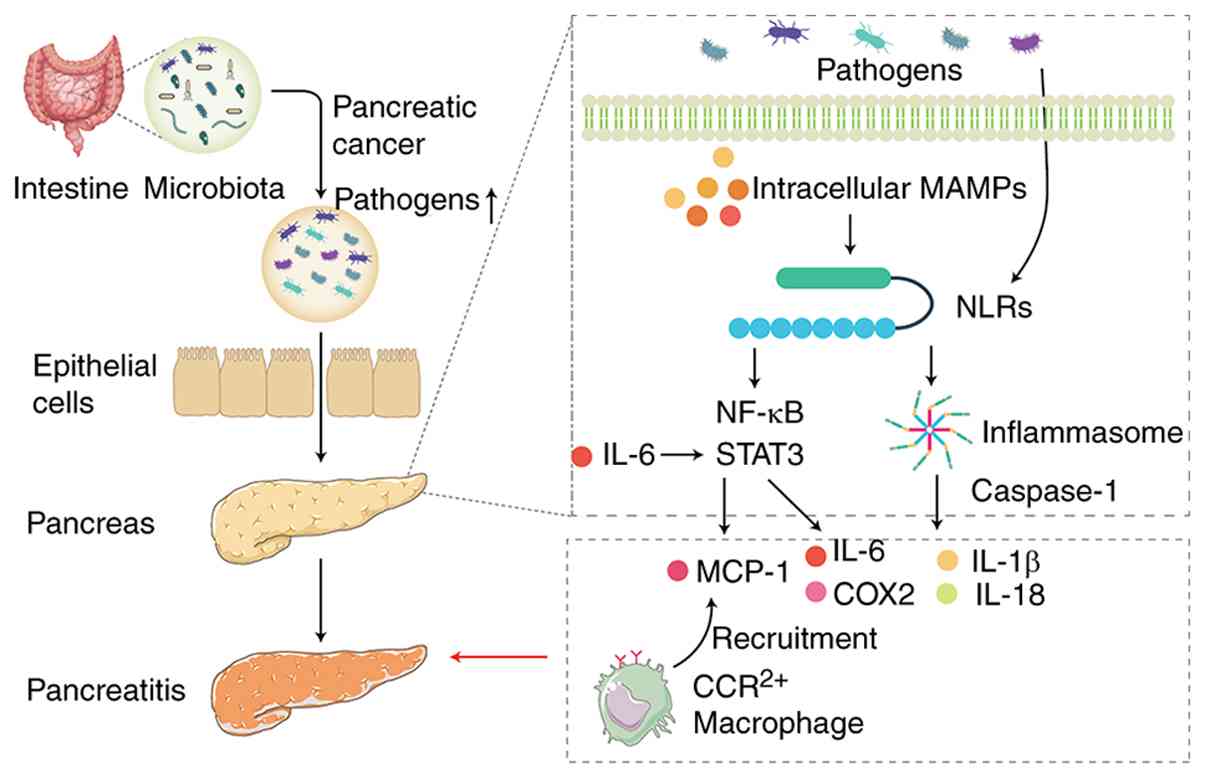
Bishehsari F, Voigt RM and Keshavarzian A:
Circadian rhythms and the gut microbiota: From the metabolic
syndrome to cancer. Nat Rev Endocrinol. 16:731–739. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Schwartz PB, Nukaya M, Berres ME,
Rubinstein CD, Wu G, Hogenesch JB, Bradfield CA and
Ronnekleiv-Kelly SM: The circadian clock is disrupted in pancreatic
cancer. PLoS Genet. 19:e10107702023. View Article : Google Scholar : PubMed/NCBI
|
|
15
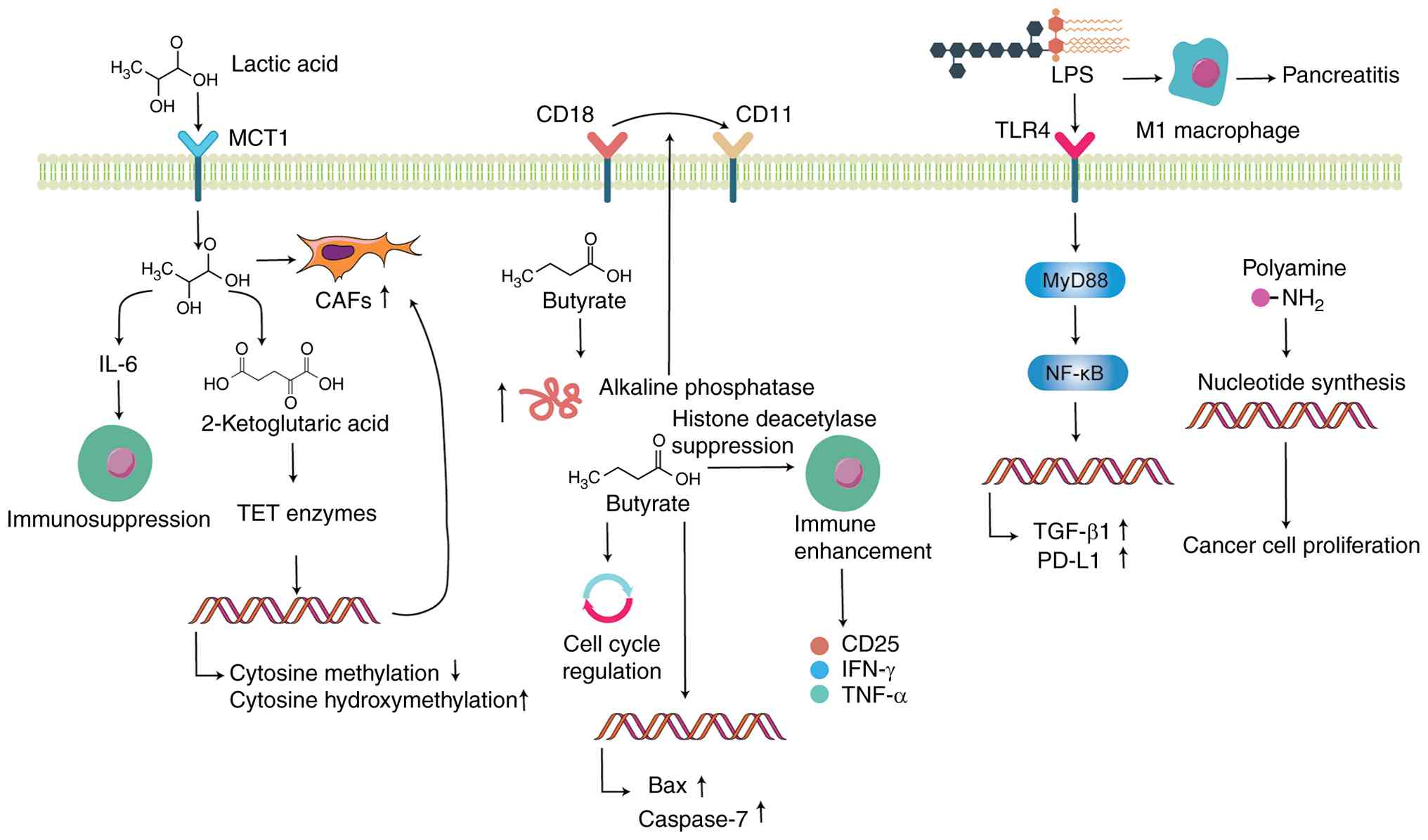
|
Amara S, Yang LV, Tiriveedhi V and
Muzaffar M: Complex role of microbiome in pancreatic tumorigenesis:
Potential therapeutic implications. Cells. 11:19002022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Subramanian SK, Brahmbhatt B,
Bailey-Lundberg JM, Thosani NC and Mutha P: Lifestyle medicine for
the prevention and treatment of pancreatitis and pancreatic cancer.
Diagnostics (Basel). 14:6142024. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
IARC Monographs Vol 124 group:
Carcinogenicity of night shift work. Lancet Oncol. 20:1058–1059.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gu F, Xu S, Devesa SS, Zhang F, Klerman
EB, Graubard BI and Caporaso NE: Longitude position in a time zone
and cancer risk in the United States. Cancer Epidemiol Biomarkers
Prev. 26:1306–1311. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Parent M, El-Zein M, Rousseau MC, Pintos J
and Siemiatycki J: Night work and the risk of cancer among men. Am
J Epidemiol. 176:751–759. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Xiao Q, Jones RR, James P and
Stolzenberg-Solomon RZ: Light at night and risk of pancreatic
cancer in the NIH-AARP diet and health study. Cancer Res.
81:1616–1622. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Titova OE, Michaëlsson K, Vithayathil M,
Mason AM, Kar S, Burgess S and Larsson SC: Sleep duration and risk
of overall and 22 site-specific cancers: A mendelian randomization
study. Int J Cancer. 148:914–920. 2021. View Article : Google Scholar
|
|
22
|
Loosen S, Krieg S, Krieg A, Leyh C, Luedde
T, Vetter C, Kostev K and Roderburg C: Are sleep disorders
associated with the risk of gastrointestinal cancer?-A case-control
study. J Cancer Res Clin Oncol. 149:11369–11378. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dun A, Zhao X, Jin X, Wei T, Gao X, Wang Y
and Hou H: Association between night-shift work and cancer risk:
Updated systematic review and meta-analysis. Front Oncol.
10:10062020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liang X, Bushman FD and FitzGerald GA:
Rhythmicity of the intestinal microbiota is regulated by gender and
the host circadian clock. Proc Natl Acad Sci USA. 112:10479–10484.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Thaiss CA, Zeevi D, Levy M,
Zilberman-Schapira G, Suez J, Tengeler AC, Abramson L, Katz MN,
Korem T, Zmora N, et al: Transkingdom control of microbiota diurnal
oscillations promotes metabolic homeostasis. Cell. 159:514–529.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li S, Duan Y, Luo S, Zhou F, Wu Q and Lu
Z: Short-chain fatty acids and cancer. Trends Cancer. 11:154–168.
2025. View Article : Google Scholar
|
|
27
|
Li Q, Xu T, Shao C, Gao W, Wang M, Dong Y,
Wang X, Lu F, Li D, Tan H, et al: Obstructive sleep apnea is
related to alterations in fecal microbiome and impaired intestinal
barrier function. Sci Rep. 13:7782023. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Summa KC, Voigt RM, Forsyth CB, Shaikh M,
Cavanaugh K, Tang Y, Vitaterna MH, Song S, Turek FW and
Keshavarzian A: Disruption of the circadian clock in mice increases
intestinal permeability and promotes alcohol-induced hepatic
pathology and inflammation. PLoS One. 8:e671022013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Everson CA and Toth LA: Systemic bacterial
invasion induced by sleep deprivation. Am J Physiol Regul Integr
Comp Physiol. 278:R905–R916. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Irwin M, Thompson J, Miller C, Gillin JC
and Ziegler M: Effects of sleep and sleep deprivation on
catecholamine and interleukin-2 levels in humans: Clinical
implications. J Clin Endocrinol Metab. 84:1979–1985.
1999.PubMed/NCBI
|
|
31
|
Jacob C, Yang PC, Darmoul D, Amadesi S,
Saito T, Cottrell GS, Coelho AM, Singh P, Grady EF, Perdue M and
Bunnett NW: Mast cell tryptase controls paracellular permeability
of the intestine. Role of protease-activated receptor 2 and
beta-arrestins. J Biol Chem. 280:31936–31948. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Spindler LRB, Luppi AI, Adapa RM, Craig
MM, Coppola P, Peattie ARD, Manktelow AE, Finoia P, Sahakian BJ,
Williams GB, et al: Dopaminergic brainstem disconnection is common
to pharmacological and pathological consciousness perturbation.
Proc Natl Acad Sci USA. 118:e20262891182021. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wang X, Wang Z, Cao J, Dong Y and Chen Y:
Gut microbiota-derived metabolites mediate the neuroprotective
effect of melatonin in cognitive impairment induced by sleep
deprivation. Microbiome. 11:172023. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Pollmächer T, Mullington J, Korth C,
Schreiber W, Hermann D, Orth A, Galanos C and Holsboer F: Diurnal
variations in the human host response to endotoxin. J Infect Dis.
174:1040–1045. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Silver AC, Buckley SM, Hughes ME, Hastings
AK, Nitabach MN and Fikrig E: Daily oscillations in expression and
responsiveness of Toll-like receptors in splenic immune cells.
Heliyon. 4:e005792018. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Curtis AM, Fagundes CT, Yang G,
Palsson-McDermott EM, Wochal P, McGettrick AF, Foley NH, Early JO,
Chen L, Zhang H, et al: Circadian control of innate immunity in
macrophages by miR-155 targeting Bmal1. Proc Natl Acad Sci USA.
112:7231–7236. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Tran L, Jochum SB, Shaikh M, Wilber S,
Zhang L, Hayden DM, Forsyth CB, Voigt RM, Bishehsari F,
Keshavarzian A and Swanson GR: Circadian misalignment by
environmental light/dark shifting causes circadian disruption in
colon. PLoS One. 16:e02516042021. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hu L, Li G, Shu Y, Hou X, Yang L and Jin
Y: Circadian dysregulation induces alterations of visceral
sensitivity and the gut microbiota in Light/Dark phase shift mice.
Front Microbiol. 13:9359192022. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Yin H, Pu N, Chen Q, Zhang J, Zhao G, Xu
X, Wang D, Kuang T, Jin D, Lou W and Wu W: Gut-derived
lipopolysaccharide remodels tumoral microenvironment and synergizes
with PD-L1 checkpoint blockade via TLR4/MyD88/AKT/NF-κB pathway in
pancreatic cancer. Cell Death Dis. 12:10332021. View Article : Google Scholar
|
|
40
|
Massoumi RL, Teper Y, Ako S, Ye L, Wang E,
Hines OJ and Eibl G: Direct effects of lipopolysaccharide on human
pancreatic cancer cells. Pancreas. 50:524–528. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wu X, Chen L, Zeb F, Huang Y, An J, Ren J,
Yang F and Feng Q: Regulation of circadian rhythms by NEAT1
mediated TMAO-induced endothelial proliferation: A protective role
of asparagus extract. Exp Cell Res. 382:1114512019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Liu A, Zhang Y, Xun S and Sun M:
Trimethylamine N-oxide promotes atherosclerosis via regulating the
enriched abundant transcript 1/miR-370-3p/signal transducer and
activator of transcription 3/flavin-containing monooxygenase-3
axis. Bioengineered. 13:1541–1553. 2022. View Article : Google Scholar :
|
|
43
|
Lynch SV and Pedersen O: The human
intestinal microbiome in health and disease. N Engl J Med.
375:2369–2379. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fan Y and Pedersen O: Gut microbiota in
human metabolic health and disease. Nat Rev Microbiol. 19:55–71.
2021. View Article : Google Scholar
|
|
45
|
Sethi V, Kurtom S, Tarique M, Lavania S,
Malchiodi Z, Hellmund L, Zhang L, Sharma U, Giri B, Garg B, et al:
Gut microbiota promotes tumor growth in mice by modulating immune
response. Gastroenterology. 155:33–37.e36. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Trikudanathan G, Philip A, Dasanu CA and
Baker WL: Association between Helicobacter pylori infection and
pancreatic cancer. A cumulative meta-analysis. JOP. 12:26–31.
2011.PubMed/NCBI
|
|
47
|
Schulte A, Pandeya N, Fawcett J, Fritschi
L, Risch HA, Webb PM, Whiteman DC and Neale RE: Association between
Helicobacter pylori and pancreatic cancer risk: A meta-analysis.
Cancer Causes Control. 26:1027–1035. 2015.PubMed/NCBI
|
|
48
|
Xiao M, Wang Y and Gao Y: Association
between Helicobacter pylori infection and pancreatic cancer
development: A meta-analysis. PLoS One. 8:e755592013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Risch HA: Pancreatic cancer: Helicobacter
pylori colonization, N-nitrosamine exposures, and ABO blood group.
Mol Carcinog. 51:109–118. 2012. View Article : Google Scholar
|
|
50
|
Malfertheiner P, Camargo MC, El-Omar E,
Liou JM, Peek R, Schulz C, Smith SI and Suerbaum S: Helicobacter
pylori infection. Nat Rev Dis Primers. 9:192023. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Abasse KS, Essien EE, Abbas M, Yu X, Xie
W, Sun J, Akter L and Cote A: Association between dietary nitrate,
nitrite intake, and site-specific cancer risk: A systematic review
and meta-analysis. Nutrients. 14:6662022. View Article : Google Scholar
|
|
52
|
Luo J, Nordenvall C, Nyrén O, Adami HO,
Permert J and Ye W: The risk of pancreatic cancer in patients with
gastric or duodenal ulcer disease. Int J Cancer. 120:368–372. 2007.
View Article : Google Scholar
|
|
53
|
Lindkvist B, Johansen D, Borgström A and
Manjer J: A prospective study of Helicobacter pylori in relation to
the risk for pancreatic cancer. BMC Cancer. 8:3212008. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Mitsuhashi K, Nosho K, Sukawa Y, Matsunaga
Y, Ito M, Kurihara H, Kanno S, Igarashi H, Naito T, Adachi Y, et
al: Association of Fusobacterium species in pancreatic cancer
tissues with molecular features and prognosis. Oncotarget.
6:7209–7220. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hayashi M, Ikenaga N, Nakata K, Luo H,
Zhong P, Date S, Oyama K, Higashijima N, Kubo A, Iwamoto C, et al:
Intratumor fusobacterium nucleatum promotes the progression of
pancreatic cancer via the CXCL1-CXCR2 axis. Cancer Sci.
114:3666–3678. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kohi S, Macgregor-Das A, Dbouk M, Yoshida
T, Chuidian M, Abe T, Borges M, Lennon AM, Shin EJ, Canto MI and
Goggins M: Alterations in the duodenal fluid microbiome of patients
with pancreatic cancer. Clin Gastroenterol Hepatol. 20:e196–e227.
2022. View Article : Google Scholar
|
|
57
|
Nejman D, Livyatan I, Fuks G, Gavert N,
Zwang Y, Geller LT, Rotter-Maskowitz A, Weiser R, Mallel G, Gigi E,
et al: The human tumor microbiome is composed of tumor
type-specific intracellular bacteria. Science. 368:973–980. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Pushalkar S, Hundeyin M, Daley D,
Zambirinis CP, Kurz E, Mishra A, Mohan N, Aykut B, Usyk M, Torres
LE, et al: The pancreatic cancer microbiome promotes oncogenesis by
induction of innate and adaptive immune suppression. Cancer Discov.
8:403–416. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
D'Antonio DL, Zenoniani A, Umme S,
Piattelli A and Curia MC: Intratumoral fusobacterium nucleatum in
pancreatic cancer: Current and future perspectives. Pathogens.
14:22024. View Article : Google Scholar
|
|
60
|
Kartal E, Schmidt TSB, Molina-Montes E,
Rodríguez-Perales S, Wirbel J, Maistrenko OM, Akanni WA, Alhamwe
BA, Alves RJ, Carrato K, et al: A faecal microbiota signature with
high specificity for pancreatic cancer. Gut. 71:1359–1372. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Half E, Keren N, Reshef L, Dorfman T,
Lachter I, Kluger Y, Reshef N, Knobler H, Maor Y, Stein A, et al:
Fecal microbiome signatures of pancreatic cancer patients. Sci Rep.
9:168012019. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ren Z, Jiang J, Xie H, Li A, Lu H, Xu S,
Zhou L, Zhang H, Cui G, Chen X, et al: Gut microbial profile
analysis by MiSeq sequencing of pancreatic carcinoma patients in
China. Oncotarget. 8:95176–95191. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Kharofa J, Haslam D, Wilkinson R, Weiss A,
Patel S, Wang K, Esslinger H, Olowokure O, Sohal D, Wilson G, et
al: Analysis of the fecal metagenome in long-term survivors of
pancreas cancer. Cancer. 129:1986–1994. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Riquelme E, Zhang Y, Zhang L, Montiel M,
Zoltan M, Dong W, Quesada P, Sahin I, Chandra V, San Lucas A, et
al: Tumor microbiome diversity and composition influence pancreatic
cancer outcomes. Cell. 178:795–806.e712. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Tan Q, Ma X, Yang B, Liu Y, Xie Y, Wang X,
Yuan W and Ma J: Periodontitis pathogen Porphyromonas gingivalis
promotes pancreatic tumorigenesis via neutrophil elastase from
tumor-associated neutrophils. Gut Microbes. 14:20737852022.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Gaiser RA, Halimi A, Alkharaan H, Lu L,
Davanian H, Healy K, Hugerth LW, Ateeb Z, Valente R, Moro CF, et
al: Enrichment of oral microbiota in early cystic precursors to
invasive pancreatic cancer. Gut. 68:2186–2194. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Dickson I: Microbiome promotes pancreatic
cancer. Nat Rev Gastroenterol Hepatol. 15:3282018. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Tojo R, Suárez A, Clemente MG, de los
Reyes-Gavilán CG, Margolles A, Gueimonde M and Ruas-Madiedo P:
Intestinal microbiota in health and disease: Role of bifidobacteria
in gut homeostasis. World J Gastroenterol. 20:15163–15176. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Sethi V, Vitiello GA, Saxena D, Miller G
and Dudeja V: The role of the microbiome in immunologic development
and its implication for pancreatic cancer immunotherapy.
Gastroenterology. 156:2097–2115.e2092. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Geller LT, Barzily-Rokni M, Danino T,
Jonas OH, Shental N, Nejman D, Gavert N, Zwang Y, Cooper ZA, Shee
K, et al: Potential role of intratumor bacteria in mediating tumor
resistance to the chemotherapeutic drug gemcitabine. Science.
357:1156–1160. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Nilsson HO, Stenram U, Ihse I and Wadstrom
T: Helicobacter species ribosomal DNA in the pancreas, stomach and
duodenum of pancreatic cancer patients. World J Gastroenterol.
12:3038–3043. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Takayama S, Takahashi H, Matsuo Y, Okada Y
and Manabe T: Effects of Helicobacter pylori infection on human
pancreatic cancer cell line. Hepatogastroenterology. 54:2387–2391.
2007.
|
|
73
|
Albillos A, de Gottardi A and Rescigno M:
The gut-liver axis in liver disease: Pathophysiological basis for
therapy. J Hepatol. 72:558–577. 2020. View Article : Google Scholar
|
|
74
|
Xu JH, Fu JJ, Wang XL, Zhu JY, Ye XH and
Chen SD: Hepatitis B or C viral infection and risk of pancreatic
cancer: A meta-analysis of observational studies. World J
Gastroenterol. 19:4234–4241. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Lanini S, Ustianowski A, Pisapia R, Zumla
A and Ippolito G: Viral hepatitis: Etiology, epidemiology,
transmission, diagnostics, treatment, and prevention. Infect Dis
Clin North Am. 33:1045–1062. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Fiorino S, Cuppini A, Castellani G,
Bacchi-Reggiani ML and Jovine E: HBV- and HCV-related infections
and risk of pancreatic cancer. JOP. 14:603–609. 2013.PubMed/NCBI
|
|
77
|
Yoshimura M, Sakurai I, Shimoda T, Abe K,
Okano T and Shikata T: Detection of HBsAg in the pancreas. Acta
Pathol Jpn. 31:711–717. 1981.PubMed/NCBI
|
|
78
|
Jin Y, Gao H, Chen H, Wang J, Chen M, Li
G, Wang L, Gu J and Tu H: Identification and impact of hepatitis B
virus DNA and antigens in pancreatic cancer tissues and adjacent
non-cancerous tissues. Cancer Lett. 335:447–454. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Taranto D, Carrato A, Romano M, Maio G,
Izzo CM and Del Vecchio Blanco C: Mild pancreatic damage in acute
viral hepatitis. Digestion. 42:93–97. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Ben Q, Li Z, Liu C, Cai Q, Yuan Y, Wang K,
Xiao L, Gao J and Zhang H: Hepatitis B virus status and risk of
pancreatic ductal adenocarcinoma: A case-control study from China.
Pancreas. 41:435–440. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Iloeje UH, Yang HI, Jen CL, Su J, Wang LY,
You SL, Lu SN and Chen CJ: Risk of pancreatic cancer in chronic
hepatitis B virus infection: Data from the REVEAL-HBV cohort study.
Liver Int. 30:423–429. 2010. View Article : Google Scholar
|
|
82
|
Wei XL, Qiu MZ, Chen WW, Jin Y, Ren C,
Wang F, Luo HY, Wang ZQ, Zhang DS, Wang FH, et al: The status of
HBV infection influences metastatic pattern and survival in Chinese
patients with pancreatic cancer. J Transl Med. 11:2492013.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Majumder S, Bockorny B, Baker WL and
Dasanu CA: Association between HBsAg positivity and pancreatic
cancer: A meta-analysis. J Gastrointest Cancer. 45:347–352. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Zhong S, Yeo W, Tang MW, Lin XR, Mo F, Ho
WM, Hui P and Johnson PJ: Gross elevation of TT virus genome load
in the peripheral blood mononuclear cells of cancer patients. Ann N
Y Acad Sci. 945:84–92. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Tomasiewicz K, Modrzewska R, Lyczak A and
Krawczuk G: TT virus infection and pancreatic cancer: Relationship
or accidental coexistence. World J Gastroenterol. 11:2847–2849.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Camargo CA Jr, Greig PD, Levy GA and
Clavien PA: Acute pancreatitis following liver transplantation. J
Am Coll Surg. 181:249–256. 1995.PubMed/NCBI
|
|
87
|
Demir M, Serin E, Göktürk S, Ozturk NA,
Kulaksizoglu S and Ylmaz U: The prevalence of occult hepatitis B
virus infection in type 2 diabetes mellitus patients. Eur J
Gastroenterol Hepatol. 20:668–673. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Brooks-Worrell B and Palmer JP: Immunology
in the clinic review series; focus on metabolic diseases:
Development of islet autoimmune disease in type 2 diabetes
patients: potential sequelae of chronic inflammation. Clin Exp
Immunol. 167:40–46. 2012. View Article : Google Scholar :
|
|
89
|
Chen Y, Bai X, Zhang Q, Wen L, Su W, Fu Q,
Sun X, Lou Y, Yang J, Zhang J, et al: The hepatitis B virus X
protein promotes pancreatic cancer through modulation of the
PI3K/AKT signaling pathway. Cancer Lett. 380:98–105. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Lowenfels AB, Maisonneuve P, Cavallini G,
Ammann RW, Lankisch PG, Andersen JR, Dimagno EP, Andrén-Sandberg A
and Domellöf L: Pancreatitis and the risk of pancreatic cancer.
International pancreatitis study group. N Engl J Med.
328:1433–1437. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Zambirinis CP, Pushalkar S, Saxena D and
Miller G: Pancreatic cancer, inflammation, and microbiome. Cancer
J. 20:195–202. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Sammallahti H, Kokkola A, Rezasoltani S,
Ghanbari R, Aghdaei HA, Knuutila S, Puolakkainen P and Sarhadi VK:
Microbiota alterations and their association with oncogenomic
changes in pancreatic cancer patients. Int J Mol Sci. 22:129782021.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Serra N, Di Carlo P, Gulotta G, d' Arpa F,
Giammanco A, Colomba C, Melfa G, Fasciana T and Sergi C: Bactibilia
in women affected with diseases of the biliary tract and pancreas.
A STROBE guidelines-adherent cross-sectional study in Southern
Italy. J Med Microbiol. 67:1090–1095. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Franchi L, Muñoz-Planillo R and Núñez G:
Sensing and reacting to microbes through the inflammasomes. Nat
Immunol. 13:325–332. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Hayward JA, Mathur A, Ngo C and Man SM:
Cytosolic recognition of microbes and pathogens: Inflammasomes in
action. Microbiol Mol Biol Rev. 82:e00015–e00018. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Chen GY and Núñez G: Inflammasomes in
intestinal inflammation and cancer. Gastroenterology.
141:1986–1999. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Hoque R, Sohail M, Malik A, Sarwar S, Luo
Y, Shah A, Barrat F, Flavell R, Gorelick F, Husain S and Mehal W:
TLR9 and the NLRP3 inflammasome link acinar cell death with
inflammation in acute pancreatitis. Gastroenterology. 141:358–369.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Tsuji Y, Watanabe T, Kudo M, Arai H,
Strober W and Chiba T: Sensing of commensal organisms by the
intracellular sensor NOD1 mediates experimental pancreatitis.
Immunity. 37:326–338. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Fukuda A, Wang SC, Morris JP IV, Folias
AE, Liou A, Kim GE, Akira S, Boucher KM, Firpo MA, Mulvihill SJ and
Hebrok M: Stat3 and MMP7 contribute to pancreatic ductal
adenocarcinoma initiation and progression. Cancer Cell. 19:441–455.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Lesina M, Kurkowski MU, Ludes K, Rose-John
S, Treiber M, Klöppel G, Yoshimura A, Reindl W, Sipos B, Akira S,
et al: Stat3/Socs3 activation by IL-6 transsignaling promotes
progression of pancreatic intraepithelial neoplasia and development
of pancreatic cancer. Cancer Cell. 19:456–469. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Yu H, Pardoll D and Jove R: STATs in
cancer inflammation and immunity: A leading role for STAT3. Nat Rev
Cancer. 9:798–809. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Schwabe RF and Jobin C: The microbiome and
cancer. Nat Rev Cancer. 13:800–812. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
De Monte L, Reni M, Tassi E, Clavenna D,
Papa I, Recalde H, Braga M, Di Carlo V, Doglioni C and Protti MP:
Intratumor T helper type 2 cell infiltrate correlates with
cancer-associated fibroblast thymic stromal lymphopoietin
production and reduced survival in pancreatic cancer. J Exp Med.
208:469–478. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Thomas RM, Gharaibeh RZ, Gauthier J,
Beveridge M, Pope JL, Guijarro MV, Yu Q, He Z, Ohland C, Newsome R,
et al: Intestinal microbiota enhances pancreatic carcinogenesis in
preclinical models. Carcinogenesis. 39:1068–1078. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Takeuchi O and Akira S: Pattern
recognition receptors and inflammation. Cell. 140:805–820. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Zambirinis CP, Ochi A, Barilla R, Greco S,
Deutsch M and Miller G: Induction of TRIF- or MYD88-dependent
pathways perturbs cell cycle regulation in pancreatic cancer. Cell
Cycle. 12:1153–1154. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Thomas RM and Jobin C: Microbiota in
pancreatic health and disease: The next frontier in microbiome
research. Nat Rev Gastroenterol Hepatol. 17:53–64. 2020. View Article : Google Scholar
|
|
108
|
Nicholson JK, Holmes E, Kinross J,
Burcelin R, Gibson G, Jia W and Pettersson S: Host-gut microbiota
metabolic interactions. Science. 336:1262–1267. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Chen D, Liu P, Lu X, Li J, Qi D, Zang L,
Lin J, Liu Y, Zhai S, Fu D, et al: Pan-cancer analysis implicates
novel insights of lactate metabolism into immunotherapy response
prediction and survival prognostication. J Exp Clin Cancer Res.
43:1252024. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Kitamura F, Semba T, Yasuda-Yoshihara N,
Yamada K, Nishimura A, Yamasaki J, Nagano O, Yasuda T, Yonemura A,
Tong Y, et al: Cancer-associated fibroblasts reuse cancer-derived
lactate to maintain a fibrotic and immunosuppressive
microenvironment in pancreatic cancer. JCI Insight. 8:e1630222023.
View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Bhagat TD, Von Ahrens D, Dawlaty M, Zou Y,
Baddour J, Achreja A, Zhao H, Yang L, Patel B, Kwak C, et al:
Lactate-mediated epigenetic reprogramming regulates formation of
human pancreatic cancer-associated fibroblasts. Elife.
8:e506632019. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Mullins TD, Kern HF and Metzgar RS:
Ultrastructural differentiation of sodium butyrate-treated human
pancreatic adenocarcinoma cell lines. Pancreas. 6:578–587. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Pellizzaro C, Speranza A, Zorzet S, Crucil
I, Sava G, Scarlata I, Cantoni S, Fedeli M and Coradini D:
Inhibition of human pancreatic cell line MIA PaCa2 proliferation by
HA-But, a hyaluronic butyric ester: A preliminary report. Pancreas.
36:e15–e23. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Kanika G, Khan S and Jena G: Sodium
butyrate ameliorates L-arginine-induced pancreatitis and associated
fibrosis in wistar rat: Role of inflammation and nitrosative
stress. J Biochem Mol Toxicol. 29:349–359. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Luu M, Riester Z, Baldrich A, Reichardt N,
Yuille S, Busetti A, Klein M, Wempe A, Leister H, Raifer H, et al:
Microbial short-chain fatty acids modulate CD8(+) T cell responses
and improve adoptive immunotherapy for cancer. Nat Commun.
12:40772021. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Avila-Calderón ED, Ruiz-Palma MDS,
Aguilera-Arreola MG, Velázquez-Guadarrama N, Ruiz EA, Gomez-Lunar
Z, Witonsky S and Contreras-Rodríguez A: Outer membrane vesicles of
gram-negative bacteria: An outlook on biogenesis. Front Microbiol.
12:5579022021. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Sivam HGP, Chin BY, Gan SY, Ng JH,
Gwenhure A and Chan EWL: Lipopolysaccharide (LPS) stimulation of
pancreatic ductal adenocarcinoma (PDAC) and macrophages activates
the NLRP3 inflammasome that influences the levels of
pro-inflammatory cytokines in a co-culture model. Cancer Biol Ther.
24:22848572023. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Peng C, Tu G, Wang J, Wang Y, Wu P, Yu L,
Li Z and Yu X: MLKL signaling regulates macrophage polarization in
acute pancreatitis through CXCL10. Cell Death Dis. 14:1552023.
View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Sun L, Xiu M, Wang S, Brigstock DR, Li H,
Qu L and Gao R: Lipopolysaccharide enhances TGF-β1 signalling
pathway and rat pancreatic fibrosis. J Cell Mol Med. 22:2346–2356.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Tofalo R, Cocchi S and Suzzi G: Polyamines
and gut microbiota. Front Nutr. 6:162019. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Arruabarrena-Aristorena A, Zabala-Letona A
and Carracedo A: Oil for the cancer engine: The cross-talk between
oncogenic signaling and polyamine metabolism. Sci Adv.
4:eaar26062018. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Matsumoto M and Benno Y: The relationship
between microbiota and polyamine concentration in the human
intestine: A pilot study. Microbiol Immunol. 51:25–35. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Mendez R, Kesh K, Arora N, Di Martino L,
McAllister F, Merchant N and Banerjee S and Banerjee S: Microbial
dysbiosis and polyamine metabolism as predictive markers for early
detection of pancreatic cancer. Carcinogenesis. 41:561–570. 2020.
View Article : Google Scholar :
|
|
124
|
Di Martino ML, Campilongo R, Casalino M,
Micheli G, Colonna B and Prosseda G: Polyamines: Emerging players
in bacteria-host interactions. Int J Med Microbiol. 303:484–491.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Blanco-Míguez A, Carloni S, Cardenas C,
Dioguardi CC, Lambroia L, Capretti G, Nappo G, Fugazza A, Capogreco
A, Armanini F, et al: Microbial composition associated with biliary
stents in patients undergoing pancreatic resection for cancer. NPJ
Biofilms Microbiomes. 10:352024. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Flemming HC, van Hullebusch ED, Neu TR,
Nielsen PH, Seviour T, Stoodley P, Wingender J and Wuertz S: The
biofilm matrix: Multitasking in a shared space. Nat Rev Microbiol.
21:70–86. 2023. View Article : Google Scholar
|
|
127
|
Chen L, Wang D, Liu W, Zhou S, Gu Q and
Zhou T: Immunomodulation of exopolysaccharide produced by
Lacticaseibacillus rhamnosus ZFM216 in cyclophosphamide-induced
immunosuppressed mice by modulating gut microbiota. Int J Biol
Macromol. 283:1376192024. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Jia K, Wei M, He Y, Wang Y, Wei H and Tao
X: Characterization of novel exopolysaccharides from enterococcus
hirae WEHI01 and its immunomodulatory activity. Foods. 11:35382022.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Itonaga M and Kitano M: Endoscopic biliary
drainage for distal bile duct obstruction due to pancreatic cancer.
Clin Endosc. 58:40–52. 2025. View Article : Google Scholar :
|
|
130
|
Vaishnavi C, Samanta J and Kochhar R:
Characterization of biofilms in biliary stents and potential
factors involved in occlusion. World J Gastroenterol. 24:112–123.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Lübbert C, Wendt K, Feisthammel J, Moter
A, Lippmann N, Busch T, Mössner J, Hoffmeister A and Rodloff AC:
Epidemiology and resistance patterns of bacterial and fungal
colonization of biliary plastic stents: A prospective cohort study.
PLoS One. 11:e01554792016. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Niemelä J, Kallio R, Ohtonen P, Saarnio J
and Syrjälä H: Impact of cholangitis on survival of patients with
malignant biliary obstruction treated with percutaneous
transhepatic biliary drainage. BMC Gastroenterol. 23:912023.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Di Martino P: Extracellular polymeric
substances, a key element in understanding biofilm phenotype. AIMS
Microbiol. 4:274–288. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Mulcahy H, Charron-Mazenod L and Lewenza
S: Extracellular DNA chelates cations and induces antibiotic
resistance in Pseudomonas aeruginosa biofilms. PLoS Pathog.
4:e10002132008. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Tetz GV, Artemenko NK and Tetz VV: Effect
of DNase and antibiotics on biofilm characteristics. Antimicrob
Agents Chemother. 53:1204–1209. 2009. View Article : Google Scholar :
|
|
136
|
Karygianni L, Attin T and Thurnheer T:
Treatment interferes with composition combined dnase and proteinase
and structural integrity of multispecies oral biofilms. J Clin Med.
9:9832020. View Article : Google Scholar
|
|
137
|
Gruszecka J and Filip R: Bacterial
biofilms-A threat to biliary stents, understanding their formation,
clinical consequences and management. Medicina (Kaunas).
61:5122025. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Zeng S, Pöttler M, Lan B, Grützmann R,
Pilarsky C and Yang H: Chemoresistance in pancreatic cancer. Int J
Mol Sci. 20:45042019. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Fu Y, Ricciardiello F, Yang G, Qiu J,
Huang H, Xiao J, Cao Z, Zhao F, Liu Y, Luo W, et al: The role of
mitochondria in the chemoresistance of pancreatic cancer cells.
Cells. 10:4972021. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Bengala C, Guarneri V, Giovannetti E,
Lencioni M, Fontana E, Mey V, Fontana A, Boggi U, Del Chiaro M,
Danesi R, et al: Prolonged fixed dose rate infusion of gemcitabine
with autologous haemopoietic support in advanced pancreatic
adenocarcinoma. Br J Cancer. 93:35–40. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Huang S, Li JY, Wu J, Meng L and Shou CC:
Mycoplasma infections and different human carcinomas. World J
Gastroenterol. 7:266–269. 2001. View Article : Google Scholar
|
|
142
|
Voorde VJ, Sabuncuoğlu S, Noppen S, Hofer
A, Ranjbarian F, Fieuws S, Balzarini J and Liekens S:
Nucleoside-catabolizing enzymes in mycoplasma-infected tumor cell
cultures compromise the cytostatic activity of the anticancer drug
gemcitabine. J Biol Chem. 289:13054–13065. 2014. View Article : Google Scholar
|
|
143
|
Weniger M, Hank T, Qadan M, Ciprani D,
Michelakos T, Niess H, Heiliger C, Ilmer M, D'Haese JG, Ferrone CR,
et al: Influence of Klebsiella pneumoniae and quinolone treatment
on prognosis in patients with pancreatic cancer. Br J Surg.
108:709–716. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Kesh K, Mendez R, Abdelrahman L and
Banerjee S and Banerjee S: Type 2 diabetes induced microbiome
dysbiosis is associated with therapy resistance in pancreatic
adenocarcinoma. Microb Cell Fact. 19:752020. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Udayasuryan B, Ahmad RN, Nguyen TTD, Umaña
A, Roberts LM, Sobol P, Jones SD, Munson JM, Slade DJ and Verbridge
SS: Fusobacterium nucleatum induces proliferation and migration in
pancreatic cancer cells through host autocrine and paracrine
signaling. Sci Signal. 15:eabn49482022. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Yu T, Guo F, Yu Y, Sun T, Ma D, Han J,
Qian Y, Kryczek I, Sun D, Nagarsheth N, et al: Fusobacterium
nucleatum promotes chemoresistance to colorectal cancer by
modulating autophagy. Cell. 170:548–563.e516. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Heshiki Y, Vazquez-Uribe R, Li J, Ni Y,
Quainoo S, Imamovic L, Li J, Sørensen M, Chow BKC, Weiss GJ, et al:
Predictable modulation of cancer treatment outcomes by the gut
microbiota. Microbiome. 8:282020. View Article : Google Scholar : PubMed/NCBI
|