1. Introduction
A redox disequilibrium has been recognized in recent
years as a specific vulnerability of various tumor cells (1–3). By
exacerbating the oxidative stress, pro-oxidant drugs achieve
antineoplastic activity in a multitude of cancer cells (1,4–6).
Non-malignant cells, with their high anti-oxidant capacity, are
largely resistant to the same degree of deviation from the redox
equilibrium resulting in a high selectivity of such drugs for tumor
cells (2,4–7). In
the present review, Taurolidine is described as a redox-directed
cancer therapeutic with a broad spectrum of antineoplastic action.
In first clinical application in surgical oncology, Taurolidine was
well tolerated in patients with glioblastoma and gastrointestinal
cancers (8–13). In support of the ROS stress pathway
being an effective target for broad antineoplastic action, the
anticancer activity of Piperlongumine, a plant-derived experimental
agent (14,15), is briefly outlined.
2. Redox-directed cancer therapeutics
Cancer arises through a multistep, mutagenic process
(‘oncogene dependency’) whereby cancer cells acquire a common set
of properties that enable tumor cells to proliferate and
disseminate metastases (16). As
an adaptive response, non-oncogenic pathways such as the oxidative
stress response pathways, are also affected (1,2).
Reactive oxygen species (ROS), the key mediators of cellular
oxidative stress involved in cancer initiation and progression,
have recently emerged as promising targets for anticancer drug
development. Cancer cells have been reported to harbor elevated
levels of ROS and the ability to cope with chronically elevated
levels of cellular stress is compromised in a multitude of cancer
cells (1–3,17).
This specific vulnerability of various tumor cells was termed
‘non-oncogene dependency’ or ‘non-oncogene addiction’ (1,4,14).
Importantly, this dependency may not be shared by many
non-transformed cells (3–5,7).
Their basal ROS levels are low and their anti-oxidant capacity is
robust due to the activation of Nrf2, the master regulator of
anti-oxidant responses which includes the induction of anti-oxidant
enzymes such as catalase or glutathione-S-transferase (3,5,7).
In keeping with this hypothesis, small molecular
weight pro-oxidant drugs, which enhance the oxidative stress in
tumor cells, are considered as potential antineoplastic agents
(2,3,6,15).
In contrast, due to the lower basal ROS levels and elevated
anti-oxidant capacity, the same pro-oxidant deviation from redox
homeostasis would be tolerated by non-malignant cells leading to
minimal side-effects (1–3,6,14).
In the age of molecularly targeted therapy, drugs
with pleiotropic actions such as redox-directed agents, frequently
find limited enthusiasm based on the expectation of off-target
toxic effects. However, as exemplified in this review, at least
some redox-directed agents appear to act selectively on tumor
cells. In addition, recent research suggests that it is exactly the
pleiotropic mode of action which seems to be uniquely tailored to
overcome cancer cell drug resistance originating from a redundancy
of oncogenic signaling and rapid mutation (3,6).
3. Broad-spectrum antineoplastic activity of
Taurolidine
Taurolidine, first synthesized in the 1970s
(18) as bis(1,1-
dioxoperhydro-1,2,4-thiadizinyl-4)methane, was originally known for
its antibacterial and anti-toxin (exo/endotoxin) activity and was
tested clinically in the 1980’s in the treatment of severe surgical
infections, abdominal sepsis and peritonitis (10,11,13).
Its antineoplastic activity became apparent in colony forming
assays, in which dissociated cells were seeded at very low density
and incubated for 2 to 4 weeks. Taurolidine potently prevented cell
proliferation (EC50, 1 to 7 μg/ml) as shown for glioma
cell lines (19–21) as well as ex vivo human
glioblastoma cells (19). In
addition, at higher concentrations, Taurolidine induced acute
cytotoxicity (EC50, 40 to 80 μg/ml), tested at 24–72 h
incubation, as shown for a multitude of cultured tumor cell lines
such as mesothelioma (22–24), prostate (21,25),
glioblastoma (19,20,26,27),
ovarian (21,28), leukemia (28), colon (21,29–36),
melanoma (21,37,38),
osteosarcoma (40,41), pancreatic (41), lung (21), esophageal (42) and fibrosarcoma (41,43)
as partly summarized by Jacobi et al (44). The effectiveness of Taurolidine
in vitro was largely confirmed in vivo using various
tumor cell lines as xenografts such as mesothelioma (23), prostate (25), ovarian (21,45),
colon (29–31,34,35)
and melanoma (37,46) as well as melanoma cells in a
metastatic tumor model (46).
4. ROS-dependent cytotoxicity of
Taurolidine
As first demonstrated in glioblastoma cells
(19), a ROS-dependent mechanism
of Taurolidine-induced cell death became apparent in many tumor
cell types. Taurolidine increased the level of ROS as shown in
glioblastoma (19) and
mesothelioma cells (22,24). The reducing agent N-acetylcysteine
(NAC) was able to block or strongly reduce the cytotoxicity in
nearly all tumor cells such as glioblastoma (20), mesothelioma cells (22,24),
colon carcinoma HT29 cells (47)
and Chang liver cells (47)
although not in fibrosarcoma HT1080 cells (47). Addition of glutathione similarly
prevented cytotoxicity as shown for mesothelioma cells (22). Conversely, a reduction of the
glutathione level with DL-buthionin-(S,R)-sulfoximine (BSO)
enhanced the ability of Taurolidine to induce cell death as shown
for glioblastoma cells (20) as
well as colon and pancreas carcinoma cells (47). These results underline the central
role of ROS in triggering the Taurolidine-induced programmed cell
death. Molecularly, Taurolidine may interfere with regulators of
redox and ROS homeostasis such as glutathione-S transferase 1.
5. Taurolidine and cancer stem cells
In most tumors, the hierarchical model of tumor
formation is thought to be operative with cancer stem cells (CSC)
contributing to self-renewal and regrowth after debulking of tumor
mass by surgery or radiation (16)
e.g., in glioblastoma (48).
Taurolidine exerted potent cytotoxic activity against murine and
human glioma CSCs with ED50, 12±2 μg/ml and
EC50, 13±2 μg/ml, respectively. The CSCs were isolated
by the formation of neurospheres from either the murine SMA 560
glioma cell line or from tissue resected from newly diagnosed WHO
grade IV glioblastoma patients (KF, unpublished data). These
results extend the effectiveness of redox-directed cytotoxicity to
CSCs and may strengthen the therapeutic potential of
Taurolidine.
6. Sparing of normal cells by
Taurolidine
Non-tumor cells in vitro such as bone marrow
cells (28), NIH-3T3 fibroblasts
(21), non-neoplastic mesothelial
cells (22) were not affected by
Taurolidine under conditions of tumor cell cytotoxicity. Similarly,
in vivo, physiological cell proliferation such as
leukopoiesis or erythropoiesis (28,31,44)
were practically not affected by Taurolidine. The apparent
selective induction of cytotoxicity in cancer cells distinguishes
Taurolidine from other molecules that partly affect ROS levels,
such as paclitaxel, bleomycin, cisplatin or the glutathione
synthesis inhibitor BSO (6,49–53).
7. Good tolerability of Taurolidine in
patients
Initially, Taurolidine was tested as an
intraperitoneal and intravenous adjunct in the treatment of severe
surgical infections (sepsis, peritonitis, pancreatitis), exploiting
its activity against antibiotic-resistant bacteria and bacterial
toxins. Taurolidine showed good tolerability (10,11,13).
In the first clinical experiences with cancer patients in surgical
oncology, Taurolidine was likewise well tolerated. In a first case
report, a patient with gastric cancer re-recurrence was
palliatively treated with 2% Taurolidine i.v. for 39 cycles, each
cycle consisting of 7 days of treatment per month (300 mg/kg body
weight per day). The patient was in good clinical condition as
shown by the relevant blood parameters which included an
undisturbed leukopoesis and thrombopoesis and no sign of toxicity
(9). In a clinical experience with
two patients with progressive, non-resectable glioblastoma and
conventional therapy, the neurological condition and the quality of
life improved in both patients with no sign of tumor progression
(‘partial remission’) following two cycles of 21 days each with 2%
Taurolidine i.v. (20 g/day) (8).
In 11 patients with progresssive metastatic melanoma,
co-administration of Taurolidine with high rIL-2 enhanced the
tolerability of this regime (54).
In a multicenter prospective randomized trial, patients with
different resectable gastrointestinal (GI) cancers (20 patients
each with colon, pancreas or stomach cancer) were treated with a
perioperative lavage (2×10 min) consisting of 0.5%
Taurolidine/heparin versus 0.25% povidone- iodine (control).
Taurolidine resulted in a reduction of inflammatory cytokines
(IL-1, IL-6, IL-10) at 2 and 6 h as measured in peritoneal fluid
compared to pre-resection levels (12). There was no change in serum
leukocytes and the perioperative complications did not differ. Up
to now, the number of GI cancer patients in each group has remained
insufficient for a statistical analysis of disease outcome
following Taurolidine treatment (12). Nevertheless, in these oncological
surgical interventions, Taurolidine did not interfere with
post-operative wound healing, which was also demonstrated in a
study on the use of Taurolidine in coronary artery bypass grafting
in 60 patients (55). These
findings confirmed previous findings in rats in which the scar
tissue biopsies were examined macroscopically and
histopathologically following Taurolidine treatment (56). The perioperative use of Taurolidine
solution (2%) in surgical oncology (57) promises to be of special benefit as
it is administered at the earliest possible therapeutic time
window. Perioperatively, circulating tumor cells, which correlate
negatively with disease free survival and overall survival
(58), would be the prime targets
for Taurolidine. By its ability to be cytotoxic to tumor cells and
tumor stem cells, perioperative Taurolidine promises to reduce
micrometastases and increase survival, as substantiated in a
pancreatic cancer model (59). The
majority of clinical studies relates to the intraperitoneal
administration of Taurolidine, especially in the setting of
peritonitis (11,13). In intravenous studies, vein
irritation at high doses has been experienced, necessitating direct
central administration or peripherally via a PICC line (57).
8. Potency of action and plasma levels in
patients
Due to its short half-life in man (60) Taurolidine is usually administered
by intravenous infusion (2% Taurolidine). When administered i.v.
intermittently to glioblastoma patients, Taurolidine reached a
maximal plasma level of 83±18 μg/ml (61), which is similar to peak values
obtained in acutely treated healthy volunteers (60). This plasma concentration is
expected to be clinically effective. It is about 20 times higher
than the antiproliferative effective concentration of Taurolidine
and is in the range of its cytotoxic potency.
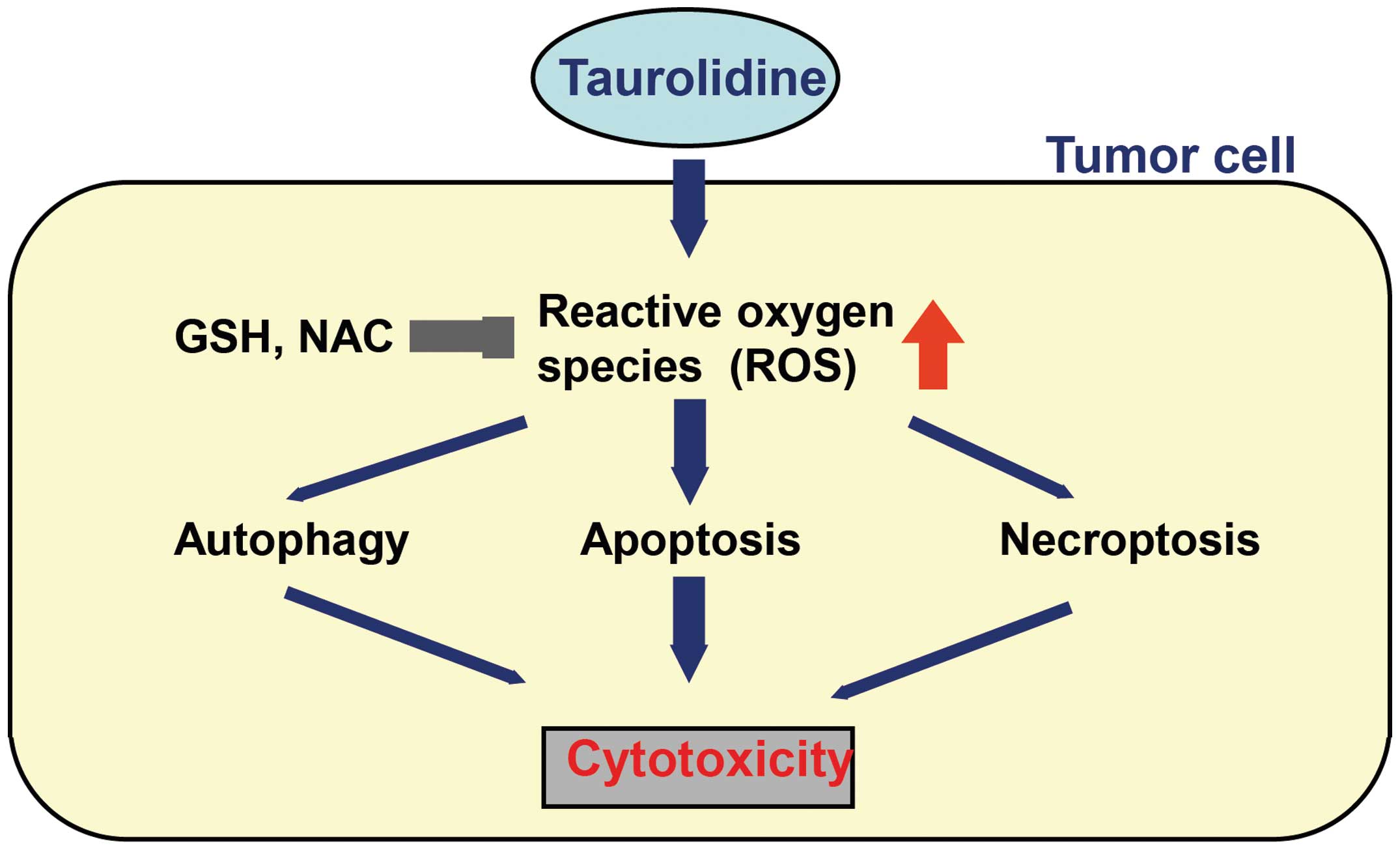
9. Mechanisms of antineoplastic action
The ROS-dependent induction of programmed cell death
by Taurolidine is based on a mixed type of cellular signaling, in
particular the induction of caspase-independent apoptosis but also
autophagy and programmed necrosis (necroptosis) (Fig. 1).
Apoptosis
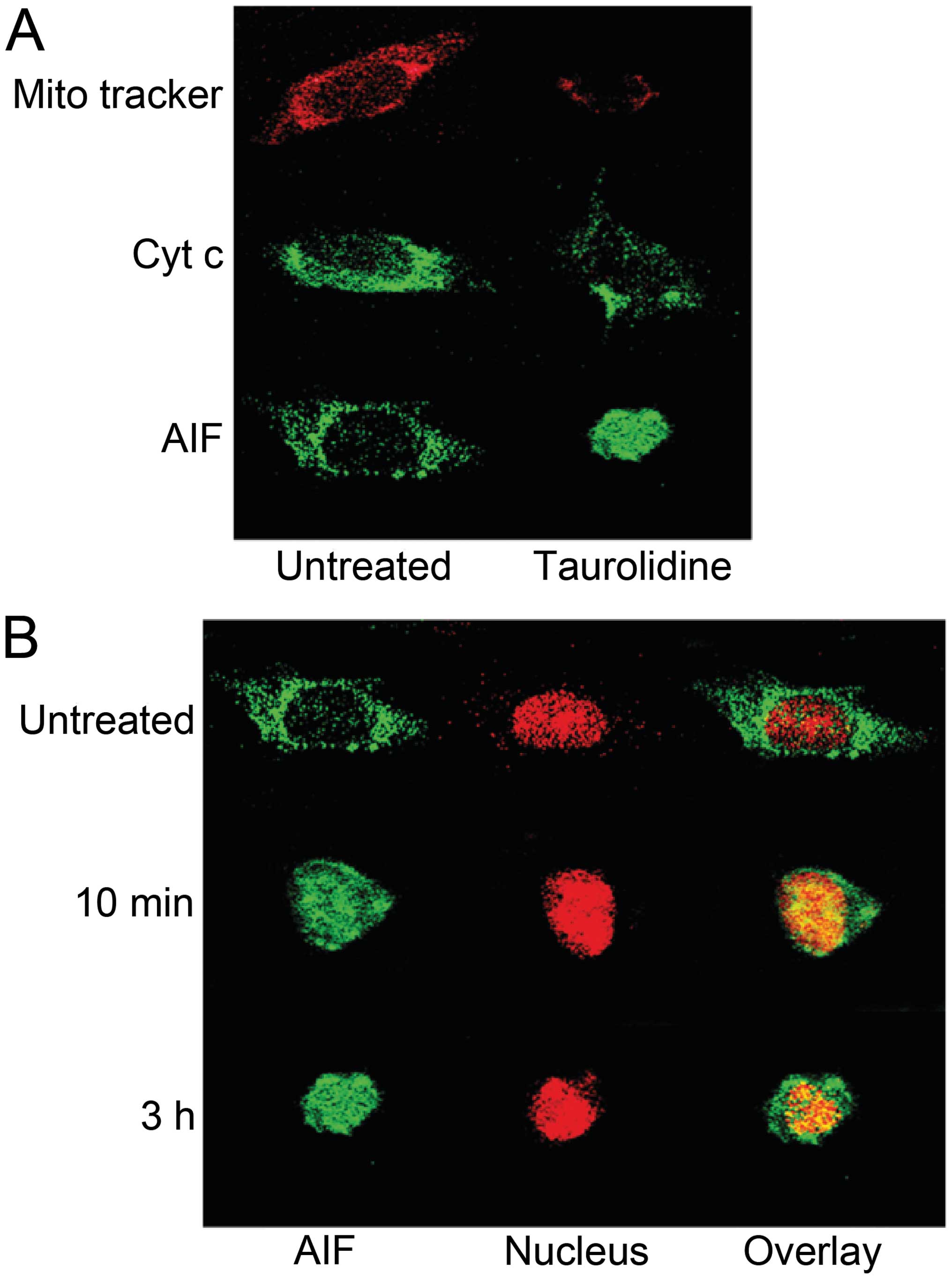
Induction of apoptosis by Taurolidine was first
shown in ovarian tumor cells (21), also in mesothelioma cells (1,24)
but was most extensively studied in glioma cells (19,20,26,27).
Within minutes of incubation with Taurolidine, the ROS-induced
mitochondrial stress signaling pathway was activated as shown by
the depolarization and permeabilisation of the mitochondrial
membrane of glioblastoma cells (Fig.
2). Concomitantly, as an inducer of apoptosis, the
mitochondrial apoptosis-inducing factor (AIF) was transduced from
the cytoplasm into the nucleus (Fig.
2) (19). In keeping with the
redox-directed mechanism, this process was completely blocked by
co-incubation with N-acetyl-cysteine (NAC) (19). This reducing agent prevented the
Taurolidine-induced cell death in practically all tumor cells
tested, as described above, supporting the view that induction of
apoptosis is the main mechanism of Taurolidine-induced cytotoxicity
(19,22,24,47).
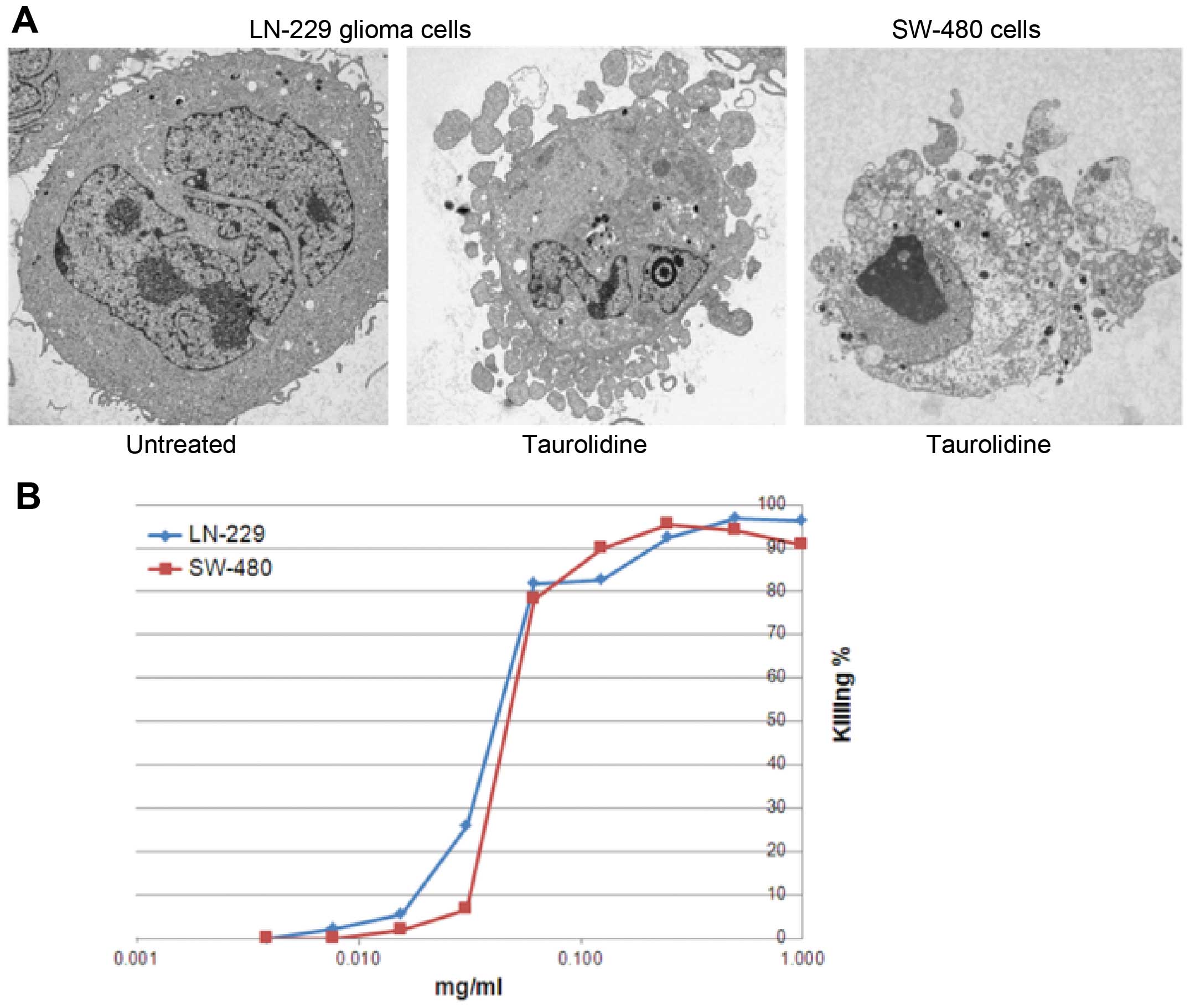
Other markers of apoptosis included condensation of chromatin,
fragmentation of DNA, externalization of phosphatidylserine and
blebbing of the plasma membrane (Fig.
3) (19–21,23,24,27).
On the molecular level, the signaling pathways
activated by Taurolidine, included the expression of pro-apoptotic
transcription factors, the downregulation of the anti-apoptotoc
regulator Bcl2, as well as the induction of genes involved in the
ER stress response, in protein ubiquitination and in mitochondrial
apoptotic pathways (42,62,63).
Akt (but not Erk1,2) was inhibited (22). Taurolidine acted synergistically
with TRAIL-induced apoptosis (42,63).
In keeping with the ROS-dependent mechanism of action, Taurolidine
was effective independent of whether p53 was mutated or not
(19,20). A significant effect on DNA repair
(PARP) was excluded, since PARP inhibition did not interfere with
the cytotoxicity of Taurolidine (19,20).
Caspase-dependent pathways of apoptosis played a
minor role. In glioblastoma cell lines, but not in ex vivo
glioma cells, cytochrome c translocation was observed only
to a very small extent (19,20).
Nevertheless, after long-term incubation with Taurolidine (up to 48
h), some cytochrome c-dependent caspase activation (caspase
8 and 9) was apparent in prostate, colon and mesothelioma tumor
cell lines since cytotoxicity was partly inhibited by a pan-caspase
inhibitor (23,41,45).
The primary molecular targets of Taurolidine remain to be
identified.
Autophagy
States of cellular stress, including ROS formation,
are known to be strong inducers of autophagy, a caspase-independent
process of cell death. In this lysosomal process, cytoplasm and
intracellular organelles are sequestered into autophagosomes and
delivered to lysosomes for degradation. In glioblastoma cells,
incubation with Taurolidine (6–24 h) induced autophagy in part of
the cells as visualized by the sequestration and lysosomal
degradation of intracellular oganelles using transmission electron
microscopy (20,41). Autophagosomes were also detected by
confocal microscopy (20).
Inhibition by 3-methyl-adenine is likewise in keeping with
autophagy (20). Autophagy
represents an alternative mechanism of cytotoxicity in particular
for apoptosis-resistant tumor cells (64).
Necrosis
The degree of Taurolidine-induced necrosis was
variable. It was negligible in glioma cells but appeared more
prevalent in pancreatic and fibrosarcoma cell lines (47). In glioma cell culture (LN229),
Taurolidine within 24 h killed 90% of the cells as shown by the
complete dissolution of the cell morphology (phase contrast
microscopy before Annexin-V and PI staining). Of these cells, 53%
were apoptotic, only 4.6% were necrotic (19,20).
The latter was largely due to programmed necrosis (necroptosis)
since pretreatment with necrostatin-1, a selective inhibitor of the
receptor-interacting protein kinase RIP1, had some protective
effect (about 40%) (20). The
large number of unstained glioma cells (42%) may point to effects
of Taurolidine beyond the induction of apoptosis and necrosis such
as autophagy, as described above.
10. Supportive anti-angiogenic and
anti-inflammatory activities of Taurolidine
Tumors are able to create a permissive
microenvironment which includes the ability to induce
neo-angiogenesis for maintaining the supply of oxygen and nutrients
(16). Besides the induction of
the programmed cell death, the antineoplastic activity of
Taurolidine includes the inhibition of neo-angiogenesis.
Taurolidine inhibited the adhesion of cultured endothelial cells
(65), reduced the synthesis of
VEGF but not of IL-6 (19,31) and potently inhibited the
VEGF-induced formation of new blood vessels from human endothelial
cells in vitro (lowest active concentration 1.25 μg/ml)
(65). It remains to be seen,
wether Taurolidine, besides its cytotoxic effect on tumor cells,
may interfere with the neovascularization of tumors in
vivo.
Taurolidine also showed anti-inflammatory activity
as demonstrated early on by the suppression of E. coli
endotoxin-induced endotoxemia (66) and the endotoxin-induced increase in
IL-1β and TNFα synthesis in human peripheral blood monocytes
(67) as well as the suppression
of the stimulated release of IL-1β from peritoneal macrophages
(34). There is a strong link
between chronic inflammation and cancer, and NFκB is implicated as
a key component in inflammation-induced tumorigenesis (68). In potentially attenuating this
process, Taurolidine upregulated the NFκB inhibitor NFκBIA in
fibrosarcoma and esophageal cancer cells (42,63).
NFκB also regulates the release of the proinflammatory mediators
IL-1, IL-6 and TNFα. The anti-inflammatory effect of Taurolidine
was proposed to contribute, at least partially, to the attenuation
of perioperative tumorigenesis by diminishing the surgery-related
inflammation as shown in a rat melanoma model (46,57).
11. Piperlongumine, a broad-spectrum
antineoplastic agent
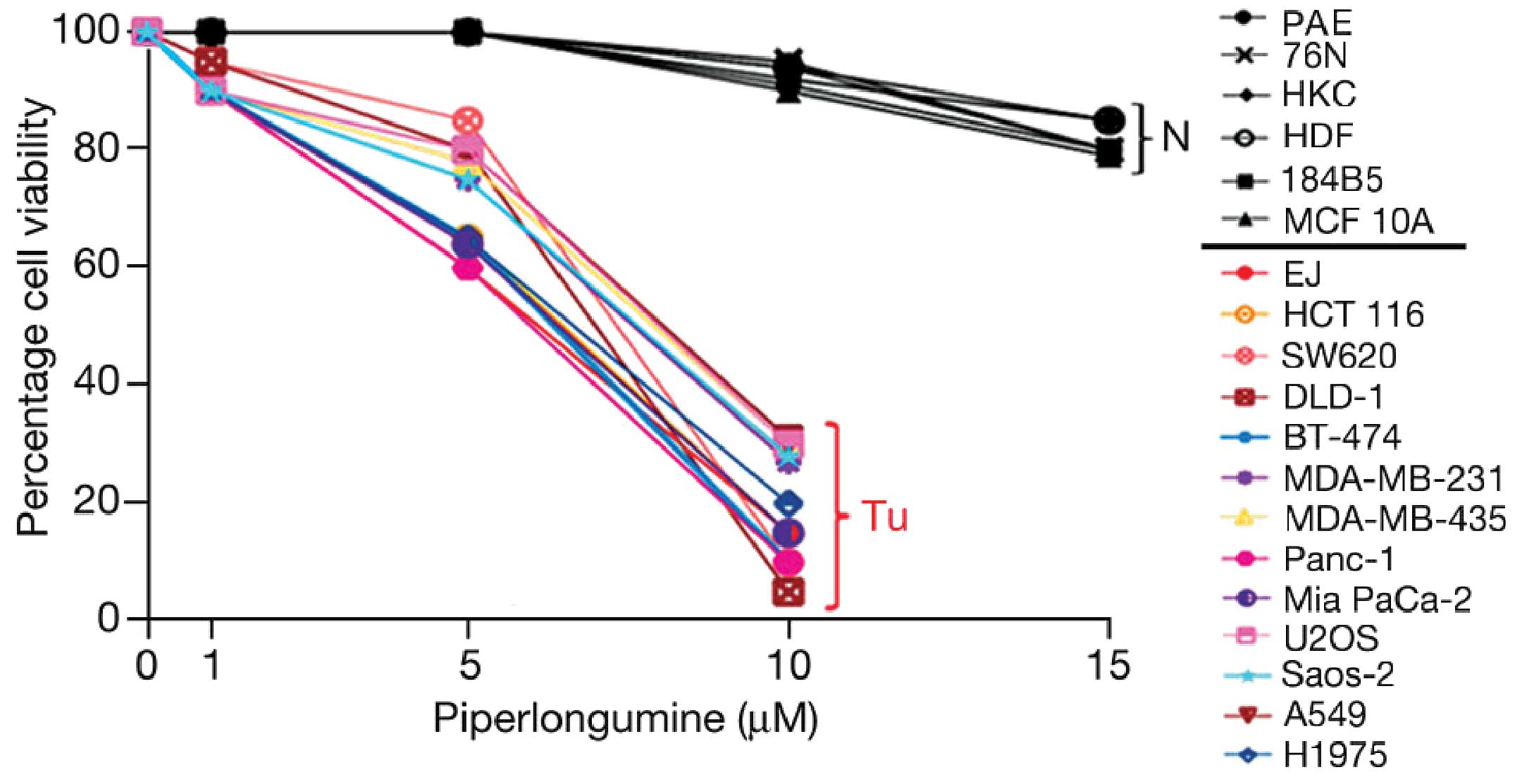
The plant alkaloid Piperlongumine (PL), which was
previously reported to have antibacterial properties (69), was recently shown to display broad
antineoplastic activity by targeting the ROS stress pathway in
tumor cells. PL caused a marked increase in ROS selectively in
cancer cells as shown in four cancer cell lines (incubation for 1
and 3 h) (14). PL
dose-dependently induced cytotoxicity in all 13 different tumor
cell lines tested with half maximal effects being reached at 6–8 μM
(Fig. 4) (14). The increase in ROS in tumor cells
and the cytotoxicity of PL was reduced by co-incubation with the
enzyme catalase or blocked by the addition of NAC (14). PL is thought to interfere with
redox and ROS homeostatic regulators such as glutathione-S
transferase 1 or carbonyl reductase (14). PL, under comparable conditions, did
not cause an increase of ROS or cytotoxicity in normal cells such
as endothelial cells, breast epithelial cells, keratinocytes and
skin fibroblasts (Fig. 4)
(14). The PL-induced killing of a
broad spectrum of tumor cell lines was based on a mixed type of
cellular signaling based largely on the induction of apoptosis
(70) but also of autophagy. The
latter was triggered via the p38 protein kinase ROS stress response
pathway (71). In prostate cells,
inhibition of proliferation included the downregulation of the
transcription factor NFκB (72).
Thus, PL is an interesting broad-spectrum, redox-directed
experimental antineoplastic agent.
12. Conclusions
Taurolidine is a representative of a novel class of
redox-directed, broad-spectrum antineoplastic agents with
tumor-selective cytotoxicity. It induces programmed cell death by
targeting the oxidative stress response pathway which is
compromised in many tumor cells. In initial applications in
surgical oncology, Taurolidine i.v. was largely free of significant
side-effects and merits further clinical evaluation. Applied
perioperatively, Taurolidine promises to reduce circulating tumor
cells, a negative predictor for disease-free survival. Taurolidine
also inhibits VEGF-induced neo-angiogenesis and may therefore
display a dual mode of antineoplastic action. Piperlongumine, an
experimental plant-derived agent, is another redox-directed
broad-spectrum antineoplastic agent with tumor cell
selectivity.
References
|
1
|
Luo J, Solimini NL and Elledge SJ:
Principles of cancer therapy: oncogene and non-oncogene addiction.
Cell. 136:823–837. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Trachootham D, Alexandre J and Huang P:
Targeting cancer cells by ROS-mediated mechanisms: a radical
therapeutic approach? Nat Rev Drug Discov. 8:579–591. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gorrini C, Harris IS and Mak TW:
Modulation of oxidative stress as an anticancer strategy. Nat Rev
Drug Discov. 12:931–947. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fruehauf JP and Meyskens FL Jr: Reactive
oxygen species: a breath of life or death? Clin Cancer Res.
13:789–794. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sporn MB and Liby KT: NRF2 and cancer: the
good, the bad and the importance of context. Nat Rev Cancer.
12:564–571. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wondrak GT: Redox-directed cancer
therapeutics: molecular merchanisms and opportunities. Antioxid
Redox Signal. 11:3013–3069. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kansanen E, Kuosmanen SM, Leinonen H and
Levonen AL: The Keap1-Nrf2 pathway: mechanism of activation and
dysregulation in cancer. Redox Biology. 1:45–49. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Stendel R, Picht T, Schilling A,
Heidenreich J, Loddenkemper C, Jänisch W and Brock M: Treatment of
glioblastoma with intravenous Taurolidine. First clinical
experience. Anticancer Res. 24:1143–1147. 2004.PubMed/NCBI
|
|
9
|
Braumann C, Winkler G, Rogalla P,
Menenakos C and Jacobi CA: Prevention of disease progression in a
patient with a gastric cancer-recurrence. Outcome after intravenous
treatment with the novel antineoplastic agent Taurolidine. Report
of a case. World J Surg Oncol. 4:342006. View Article : Google Scholar
|
|
10
|
McCartney AC and Browne MK: Clinical
studies on administration of taurolidine in severe sepsis: a
preliminary study. Progr Clin Biol Res. 272:361–371.
1988.PubMed/NCBI
|
|
11
|
Staubach KH: Adjuvant therapy of
peritonitis with taurolidine. Modulation of mediator liberation.
Langenbecks Arch Chir. 382:S26–S30. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Braumann C, Gutt CN, Scheele J, Menenakos
C, Willems W, Mueller JM and Jacobi CA: Taurolidine reduces the
tumor-stimulating cytokine IL 1beta in patients with resectable
gastrointestinal cancer: a multicenter prospective randomized
trial. World J Surg Oncol. 7:32–45. 2009. View Article : Google Scholar
|
|
13
|
Wesch G, Petermann C and Linder MM: Drug
therapy of peritonitis: 6-year experience with the chemotherapeutic
agent and anti-endotoxin Taurolin. Fortschr Med. 101:545–550.
1983.PubMed/NCBI
|
|
14
|
Raj L, Ide T, Gurkar AU, Foley M, Schenone
M, Li X, Tolliday NJ, Golub TR, Carr SA, Shamji AF, Stern AM,
Mandinova A, Schreiber SL and Lee SW: Selective killing of cancer
cells by a small molecule targeting the stress response to ROS.
Nature. 475:231–234. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Parkinson EI and Hergenrother PJ: Runaway
ROS as selective anticancer strategy. Chem Med Chem. 6:1957–1959.
2011. View Article : Google Scholar
|
|
16
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: the next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Szatrowski TP and Nathan CF: Production of
large amounts of hydrogen peroxide by human tumor cells. Cancer
Res. 51:794–798. 1991.PubMed/NCBI
|
|
18
|
Pfirrmann RW: Taurolin, ein neues Konzept
zur antimikrobiellen Chemotherapie chirurgischer Infektionen.
Brückner WL and Pfirrmann RW: Urban and Schwarzenberg Verlag; 1985,
(In German).
|
|
19
|
Rodak R, Kubota H, Ishihara H, Eugster HP,
Könü D, Möhler H, Yonekawa Y and Frei K: Induction of reactive
oxygen intermediates- dependent programmed cell death in human
malignant ex vivo glioma cells and inhibition of the vascular
endothelial growth factor production by Taurolidine. J Neurosurg.
102:1055–1068. 2005. View Article : Google Scholar
|
|
20
|
Stendel R, Biefer HR, Dékany M, Kubota H,
Münz C, Wang S, Möhler H, Yonekawa Y and Frei K: The antibacterial
substance Taurolidine exhibits anti-neoplastic action based on a
mixed type of programmed cell death. Autophagy. 5:194–210. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Calabresi P, Goulette FA and Darnowski JW:
Taurolidine: cytotoxic and mechanistic evaluation of a novel
antineoplastic agent. Cancer Res. 61:6816–6821. 2001.PubMed/NCBI
|
|
22
|
Aceto N, Bertino P, Barbone D, Tassi G,
Manzo L, Porta C, Mutti L and Gaudio G: Taurolidine and oxidative
stress: a rationale for local treatment of mesothelioma. Eur Respir
J. 34:1399–1407. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nici L, Monfils B and Calabresi P: The
effects of Taurolidine, a novel antineoplastic agent, on human
malignant mesothelioma. Clin Cancer Res. 10:7655–7661. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Opitz I, Sigrist B, Hillinger S, Lardinois
D, Stahel R, Weder W and Hopkins-Donaldson S: Taurolidine and
povidone-iodine induce different types of cell death in malignant
pleural mesothelioma. Lung Cancer. 56:327–336. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Darnowski JW, Goulette FA, Cousens LP,
Chatterjee D and Calabresi P: Mechanistic and antineoplastic
evaluation of Taurolidine in the DU145 model of human prostate
cancer. Cancer Chemother Pharmacol. 54:249–258. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Stendel R, Stoltenburg-Didinger G and
Brock M: Apoptotic changes in brain tumor cells induced by
Taurolidine. J Cancer Res Clin Oncol. 128:1502002.
|
|
27
|
Stendel R, Stoltenburg-Didinger G, Al
Keikh CL, Wattroth M and Brock M: The effect of Taurolidine on
brain tumor cells. Anticancer Res. 22:809–814. 2002.PubMed/NCBI
|
|
28
|
Ribizzi I, Darnowski JW, Goulette FA,
Akhtar MS, Chatterjee D and Calabresi P: Taurolidine: preclinical
evaluation of a novel, highly selective, agent for bone marrow
purging. Bone Marrow Transplant. 29:313–319. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
McCourt M, Wang JH, Sookhai S and Redmond
HP: Taurolidine inhibits tumor cell growth in vitro and in vivo.
Ann Surg Oncol. 7:685–691. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nestler G, Schulz HU, Schubert D, Krüger
S, Lippert H and Pross M: Impact of Taurolidine on the growth of
CC531 coloncarcinoma cells in vitro and in a laparoscopic animal
model in rats. Surg Endosc. 19:280–284. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Braumann C, Schoenbeck M, Menenakos C,
Kilian M and Jacobi CA: Effects of increasing doses of a bolus
injection and an intravenous long-term therapy of Taurolidine on
subcutaneous (metastic) tumor growth in rats. Clin Exp Metastasis.
22:77–83. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hoksch B, Rufer B, Gazdhar A, Bilici M,
Beshay M, Gugger M and Schmid RA: Taurolidine in the prevention and
therapy of lung metastases. Eur J Cardiothorac Surg. 36:1058–1063.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chromik AM, Daigeler A, Hilgert C, Bulut
D, Geisler A, Liu V, Otte JM, Uhl W and Mittelkötter U: Synergistic
effects in apoptosis induction by Taurolidine and TRAIL in HCT-15
colon carcinoma cells. J Investigat Surg. 20:339–348. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Jacobi C, Peter FJ, Wenger FA, Ordemann J
and Müller JM: New therapeutic strategies to avoid intra- and
extraperitoneal metastases during laparoscopy: results of a tumor
model in the rat. Dig Surg. 16:393–399. 1999. View Article : Google Scholar
|
|
35
|
Jacobi C, Sabat R, Ordemann J, Wenger F,
Volk H and Müller J: Peritoneal instillation of taurolidine and
heparin for preventing intraperitoneal tumor growth and trocar
metastases in laparoscopic operations in the rat model. Langenbecks
Arch Chir. 382:S31–S36. 1997. View Article : Google Scholar
|
|
36
|
Jacobi CA, Ordemann J, Böhm B, Zieren HU,
Sabat R and Müller JM: Inhibition of peritoneal tumor cell growth
and implantation in laparoscopic surgery in a rat model. Am J
Surgery. 174:359–363. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Braumann C, Jacobi CA, Rogalla S,
Menenakos C, Fuehrer K, Trefzer U and Hofmann M: The tumor
suppressive reagent Taurolidine inhibits growth of malignant
melanoma - a mouse model. J Surg Res. 143:372–378. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sun BS, Wang JH, Liu LL, Gong SL and
Redmond HP: Taurolidine induces apoptosis of murine melanoma cells
in vitro and in vivo by modulation of the Bcl-2 family proteins. J
Surg Oncol. 96:241–248. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Walters DK, Muff R, Langsam B, Gruberer P,
Born W and Fuchs B: Taurolidine: a novel anti-neoplastic agent
induces apoptosis of osterosarcoma cell lines. Invest New Drugs.
25:305–312. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Marley K, Helfand SC, Edris WA, Mata JE,
Gitelman AI, Medlock J and Séguin B: The effects of taurolidine
alone and in combination with doxorubicin or carboplatin in canine
osteosarcoma in vitro. BMC Veterinary Res. 9:15–24. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Chromik AM, Daigeler A, Bulut D, Flier A,
May C, Havati K, Roschinsky J, Sülberg D, Ritter PR, Mittelkötter
U, Hahn SA and Uhl W: Comparative analysis of cell death induction
by Taurolidine in different malignant human cancer cell lines. J
Exp Clin Cancer Res. 29:21–37. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Daigeler A, Chromik AM, Geisler A, Bulut
D, Hilgert C, Krieg A, Klein-Hitpass L, Lehnhardt M, Uhl W and
Mittelkötter U: Synergistic apoptotic effects of taurolidine and
TRAIL on squamous carcinoma cells of the esophagus. Int J Oncol.
32:1205–1220. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Daigeler A, Chromik AM, Haendschke K,
Emmelmann S, Siepmann M, Hensel K, Schmitz G, Klein-Hitpass L,
Steinau HU, Lehnhardt M and Hauser J: Synergistic effects of
sonoporation and taurolidin/TRAIL on apoptosis in human
fibrosarcoma. Ultrasound Med Biol. 36:1893–1906. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Jacobi CA, Menenakos C and Braumann C:
Taurolidine - a new drug with anti-tumor and anti-angiogenic
effects. Anticancer Drugs. 16:917–921. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Volz J, Volz-Köster S, Kanis S, Klee D,
Ahlert C and Melchert F: Modulation of tumor-induced lethality
after pneumoperitoneum in a mouse model. Cancer. 89:262–266. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Da Costa ML, Redmond HP and Bouchier-Hayes
DJ: Taurolidine improves survival by abrogating the accelerated
development and proliferation of solid tumors and development of
organ metastases from circulating tumor cells released following
surgery. J Surg Res. 101:111–119. 2001.
|
|
47
|
Chromik AM, Daigeler A, Bulut D, Flier A,
May C, Harti K, Roschinsky J, Sülberg D, Ritter PR, Mittelkötter U,
Hahn SA and Uhl W: Comparative analysis of cell death induction by
Taurolidine in different malignant human cancer cell lines. J Exp
Clin Res. 29:21–36. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Chen L, Li Y, Yu TS, McKay RM, Burns DK,
Kernie SG and Parada LF: A restricted cell population propagates
glioblastoma growth after chemotherapy. Nature. 488:522–526. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Trachootham D, Zhou Y, Zhang H, Demizu Y,
Chen Z, Pelicano H, Chiao PJ, Acxhanta G, Arlinghaus RB, Liu J and
Hunag P: Selective killing of oncogenically trandformed cells
through a ROS mediated mechanism by beta-phenylethyl
isothiocyanate. Cancer Cell. 10:241–252. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Huang P, Feng L, Oldham EA, Keating MJ and
Plunkett W: Superoxide dismutase as a target for killing of cancer
cells. Nature. 407:390–395. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Shaw AT, Winslow MM, Magendantz M, Ouyang
C, Dowdle J, Subramanian A, Lewis TA, Maglathin RL, Tolliday N and
Jacks T: Selective killing of K-ras mutant cancer cells by small
molecule inducers of oxidative stress. Proc Natl Acad Sci USA.
108:8773–8778. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Dolam S, Lessnick SL, Hahn WC and
Stockwell BR: Idebtificaton of genotype-selective antitumor agents
using syntheticchemical screening in engineered human tumor cells.
Cancer Cell. 3:285–296. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Guzman ML, Rossi RM, Neelakantan S, Li X,
Corbett CA, Hassane DC, Becker MW, Bennet JM, et al: An orally
bioavailable parthenolide analog selectively eradicates acute
myelogenous leukemia stem and progenitor cells. Blood.
110:4427–4435. 2007. View Article : Google Scholar
|
|
54
|
O’Brien G, Cahill R, Bouchier-Hayes D and
Redmond P: Co-immunotherapy with interleukin-2 and taurolidine for
progressive metastatic melanoma. Irish J Med Sci. 175:10–14.
2006.PubMed/NCBI
|
|
55
|
Doddakula KK, Neary PM, Wang JH, Sookhai
S, O’Donnel A, et al: The antioxidant agent taurolidine potentially
reduces ischemia/reperfusion injury through its metabolite taurine.
Surgery. 148:567–572. 2010. View Article : Google Scholar
|
|
56
|
Braumann C, Guenther N, Pohlenz J,
Pfirrmann RW and Menenakos C: Wound healing is not impaired in rats
undergoing perioperative treatment with the antineoplastic agent
taurolidine. Eur Surg Res. 42:91–96. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Neary PM, Hallihan P, Wang JH, Pfirrmann
R, Bouchier-Haves HP and Redmond HP: The evolving role of
Taurolidine in cancer therapy. Ann Surg Oncol. 17:1135–1143. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Liberko M, Kolostova K and Bobek V:
Essentials of circulating tumor cells for clinical research and
practice. Cirtic Rev Hematol Oncol. 88:338–356. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Kilian M, Gregor JI, Heukamp I, Braumann
C, Guski H, Schimke I, Walz MK, Jacobi CA and Wenger FA: Impact of
taurolidine and octreotide on liver metastasis and lipid
peroxidation after laparoscopy in chemical induced ductal
pancreatic cancer. Invest New Drugs. 23:157–164. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Gong L, Greenberg HE, Perhach JL, Waldman
SA and Kraft WK: The pharmacokinetics of Taurolidine metabolites in
healthy volunteers. J Clin Pharmacol. 47:697–703. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Stendel R, Scheurer L, Schlatterer K,
Stalder U, Pfirrmann R, Fiss I, Möhler H and Bigler L:
Pharmacokinetics of Taurolidine follwing repeated intravenous
infusions measured by HPLC-ESI-MS/MS of the derivatives Taurultame
and taurinamide in glioblastoma patients. Clin Pharmacokinetics.
46:513–524. 2007. View Article : Google Scholar
|
|
62
|
Chromik AM, Hahn SA, Daigeler A, Flier A,
Bulut D, May C, Harati K, Roschinsky J, Sülberg D, Weyhe D,
Mittelkötter U and Uhl W: Gene expression analysis of cell death
induction by taurolidine in different malignant cell lines. BMC
Cancer. 10:595–608. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Daigeler A, Brenzel Ch, Bulut D, Geisler
A, Hilgert C, Lehnhardt M, Steinau HU, Flier A, Steinsträsser L,
Klein-Hitpass L, Mittelkötter U, Uhl W and Chromik AM: TRAIL and
Taurolidine induce apoptosis and decrease proliferation in human
fibrosarcoma. J Exp Clin Cancer Res. 27:82–102. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Rubinsztein DC, Codogno P and Levine B:
Autophagy modulation as a potential therapeutic target for divers
diseases. Nature Rev Drug Disc. 11:709–730. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Möhler T, Willhauck-Fleckenstein M,
Schwartz-Albiez R, Merling A and Möhler H: Inhibition of
endothelial cell adhesion and in vitro angiogenesis by Taurolidine.
Cancer Ther. 6:623–628. 2008.
|
|
66
|
Egan BM, Bouchier-Hayes DJ, Condron C,
Kelly CJ and Abdih H: Taurolidine attenuates the hemodynamic and
respiratory changes associated with endotoxemia. Scock. 17:308–311.
2002.PubMed/NCBI
|
|
67
|
Bedrosian I, Sofia RD, Wolff SM and
Dinarello CA: Taurolidine, an analogue of the amino acid taurine,
suppresses interleukin 1 and tumor necrosis factor synthesis in
human peripheral blood mononuclear cells. Cytokine. 3:568–575.
1991. View Article : Google Scholar
|
|
68
|
Grivennikov SI, Greten FR and Karin M:
Immunity, inflammation and cancer. Cell. 140:883–899. 2010.
View Article : Google Scholar
|
|
69
|
Reddy PS, Jamil K, Madhusudhan P and
Anjani G: Antibacterial activity of isolates of from Piper
longum and Taxus baccata. Pharm Biol. 39:236–238. 2001.
View Article : Google Scholar
|
|
70
|
Adams DJ, Dai M, Pellegrino G, Wagner BK,
et al: Synthesis, cellular evaluation and mechanism of action of
piperlongumine anlogs. Proc Natl Acad Sci USA. 109:15115–15120.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Wang Y, Wang JW, Xiao X, Shan Y, Xue B,
Jiang G, He Q, Chen J, Xu HG, Zhao RX, Werle KD, Cui R, Liang J, Li
YL and Xu ZX: Piperlongumine induces autophagy by targeting p38.
Cell Death Dis. 4:e8242013. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Ginzburg S, Golovine KV, Makhov PB, Uzzo
RG, Kutikov A and Kolenko VM: Piperlongumine inhibits NFkappaB
activity and attenuates aggressive growth characteristics of
prostate cancer cells. Prostate. 73:1–10. 2013.PubMed/NCBI
|