Introduction
Hepatocellular carcinoma (HCC) is one of the most
common malignancies worldwide. Liver resection for HCC has the
highest local controllability among all local treatments; however,
the recurrence rates of HCC remain high even after curative
hepatectomy (1–3). Because of the high recurrence rate
and poor prognosis, the prognostic assessment and selection of
treatment strategy in HCC patients are quite important (4,5). In
particular, a precise stratification system for the prognosis of
HCC patients is required in parallel to the advent of effective
systemic treatment options (6).
It is well known that the prognosis of HCC depends
on both tumor factors (i.e., size and extent of primary tumor) and
host factors (i.e., liver function) (7); however, the latter is not integrated
in the tumor lymph node metastasis (TNM) staging system, which is
generally accepted as a standard approach for prognostication in
many cancer clinical staging systems. Even when primary HCC is
completely treated, recurrence is observed much more frequently in
the form of multicentric carcinogenesis in the residual cirrhotic
liver, because the potential for multicentric carcinogenesis
increases with the progression of chronic liver disease and liver
cirrhosis (2,3). Therefore, from the standpoint of
prognosis, a staging system based on information regarding both
tumor factors and host factors such as liver function are required
to accurately classify HCC patients undergoing various therapeutic
options. For this reason, many prognostic staging systems for HCC,
such as the Japan Integrated Staging score (JIS score), modified
JIS score, the Cancer of the Liver Italian Program (CLIP) score,
and the Tokyo score, have been proposed during the last two decades
(8–11). However, the prognostic ability of
these systems cannot be universally accepted because of the
variation in cohorts and/or subjects. It remains unclear which of
the staging systems is most accurate for predicting the prognosis
of HCC. Therefore, in the present study, we developed a new staging
system that had high accuracy in predicting the recurrence of HCC
by driving data for factors used in the known staging systems.
Patients and methods
Patients
We pooled data on the clinicopathological features
of 304 patients who underwent curative hepatectomy for HCC at
Yamaguchi University School of Medicine between 1985 and 2009. The
diagnoses of HCC were all confirmed pathologically. We defined
curative hepatectomy as complete resection of all tumor nodules
without involving any major branch of the portal or hepatic veins.
We excluded 29 patients who had follow-up periods <5 years, and
excluded 41 patients who had undergone treatment options such as
percutaneous ethanol injection therapy (PEIT), microwave
coagulation therapy (MCT), radiofrequency ablation (RFA), or
transcatheter arterial chemoembolization (TACE) prior to surgery.
Ultimately, 234 patients were enrolled in the study.
Data on tumor factors such as size of the main
tumor, number of tumors, tumor differentiation, and vascular
invasion were based on the final pathological findings of the
resected liver. Laboratory data, including albumin, bilirubin,
prothrombin activity, platelet count, indocyanine green retention
rate at 15 min (ICG-R15), α-fetoprotein (AFP), and positivity for
viral markers (hepatitis B surface antigen and anti-hepatitis C
antibody), were obtained before operation. The Child-Pugh
classification (12), the degree
of Liver Damage classification by the Liver Cancer Study Group of
Japan (LCSGJ) (13), TNM staging
system (LCSGJ), TNM staging system (Union for International Cancer
Control, UICC), JIS score, modified JIS score, CLIP score, and
Tokyo score were evaluated using these variables. All patients were
followed up after hepatectomy until death or the date of last
follow-up visit, and survival was censored in December 2013.
Development of predictive staging system
(PS score)
We attempted to identify tumor factors that were
closely related to the prognosis of HCC after surgery.
Subsequently, we constructed a novel multidimensional staging
system by combing the identified tumor factor and some host
factors.
By analyzing the variables and their combinations
that were used in the TNM staging system (data not shown), we found
that the mathematical product (NxS factor) of tumor number and size
(cm) had high accuracy in predicting recurrence of HCC. We next
determined the optimal cut-off values of the NxS factor at 4 and 9
in reference to the Milan criteria (single tumor ≤5 cm in size or
≤3 tumors each ≤3 cm in size) (14). The cut-off points of the NxS factor
at 4 and 9 classified the 234 patients into 3 groups. All HCC
patients with NxS factor <4 were within the Milan criteria and
had a low incidence of recurrence. Almost all patients with NxS
factor >9 were outside the Milan criteria and had a high
recurrence rate. The remaining HCC patients with NxS factor 4–9
were considered to be at intermediate risk for recurrence of HCC
(data not shown).
Among the host factors used in four staging systems
(JIS score, m-JIS score, CLIP score, and Tokyo score), we searched
for the factors with the highest prognostic probability in the
postoperative clinical course of HCC patients in combination with
the NxS factor.
Statistics
Disease-free survival (DFS) and overall survival
(OS) curves were plotted with the Kaplan-Meier method. Differences
in DFS and OS between the groups were compared by using a log-rank
test in univariate analysis. Variables that had statistical
significance (P<0.05) for DFS in the univariate analysis were
subsequently entered into a multivariate Cox proportional hazards
model. Then, we established a new prognostic scoring system (PS
score) by using the combination of factors that retained
significance in multivariate analysis.
To compare the prognostic ability of each staging
system, the Akaike information criterion (AIC) (15) within a Cox proportional hazards
regression model was used as a measure of relative goodness-of-fit.
The AIC statistic was defined by AIC = −2 log likelihood + 2 × the
number of parameters in the model and −2 log likelihood calculated
using the Cox model. Therefore, a smaller AIC value indicates a
more desirable model for predicting outcome (9,10,16–18).
For all tests, P<0.05 was considered significant. Statistical
analysis was performed using JMP version 9.0 (SAS Institute Japan,
Tokyo, Japan) and the Statistical Package for Social Sciences
version 11 (SPSS Japan, Tokyo, Japan).
Results
Patient characteristics
The baseline characteristics of the 234 HCC patients
are shown in Table I. The median
age of the patients was 63.2±0.57 [mean ± standard error (SE)]
years. Among them, 187 patients (79.9%) were males and 47 patients
(20.1%) were females. There were 146 patients who were positive for
antibodies to the hepatitis C virus (HCV), 44 patients positive for
hepatitis B surface (HBS) antigen, and 44 patients negative for
both HCV antibody and HBS antigen. In the present study, 206 and 28
patients were judged as A and B of the Child-Pugh classification,
respectively. There were 148 and 86 patients who were judged as A
and B of the degree of Liver Damage classification proposed by the
Liver Cancer Study Group of Japan, respectively. In the present
study, there were no patients classified with Child-Pugh C or Liver
Damage C.
 | Table IPatient profiles and tumor
characteristics. |
Table I
Patient profiles and tumor
characteristics.
| Variable | No. of
patients |
|---|
| Host factors |
| Age |
| Mean ± standard
error (years) | 63.2±0.57 |
| Gender |
| Male/female | 187/47 |
| Viral
infection |
|
HBV/HCV/non-BC | 44/146/44 |
| Platelet count
(x103/mm3) |
| <10/≥10 | 62/172 |
| Degree of liver
damage |
| A/B | 148/86 |
| Child-Pugh
classification |
| A/B | 206/28 |
| Tumor factors |
| Tumor size (cm)
(maximum diameter) | |
| <2/≥2,
<5/≥5 | 35/153/46 |
| Number of
tumors |
| 1/2–3/≥4 | 155/64/15 |
| The product of NxS
factor |
|
<4/4–9/>9 | 110/78/46 |
| Macroscopic portal
vein invasion |
|
Absent/present | 198/36 |
| Macroscopic
hepatic vein invasion |
|
Absent/present | 222/12 |
| Microscopic portal
vein invasion |
|
Absent/present | 177/57 |
| Microscopic
hepatic vein invasion |
|
Absent/present | 181/53 |
| AFP (ng/ml) |
| <400/≥400 | 179/55 |
|
Differentiation |
|
Well/moderate/poor | 46/153/35 |
| Anatomical
resection |
| Yes/no | 159/75 |
| Staging
systems |
| TNM stage
(LCSGJ) |
| I/II/III/IV | 25/87/85/37 |
| TNM stage
(UICC) |
| I/II/III/IV | 104/103/25/2 |
| JIS score |
| 0/1/2/3–4 | 20/84/81/49 |
| Modified JIS
score |
| 0/1/2/3–4 | 16/63/88/67 |
| CLIP |
| 0/1/2/3–5 | 109/78/32/15 |
| Tokyo score |
| 0/1/2/3/4–6 | 14/79/81/42/18 |
HCC recurrence and survival rates
Among the 234 patients, 164 experienced recurrence
of HCC within 5 years after hepatectomy. The disease-free median
survival time was 23.2 months [95% confidence interval (CI), 20.1
to 29.7 months], and the 1-, 3- and 5-year DFS rates were 75.6,
39.7 and 29.9%, respectively. The type of recurrence was mainly
intrahepatic [143 (87.2%) of 164 cases], not extrahepatic. Among
the 164 cases, 12 (7.3%) had both extrahepatic and intrahepatic
recurrences, and 9 (5.5%) had extrahepatic recurrence without
intrahepatic recurrence.
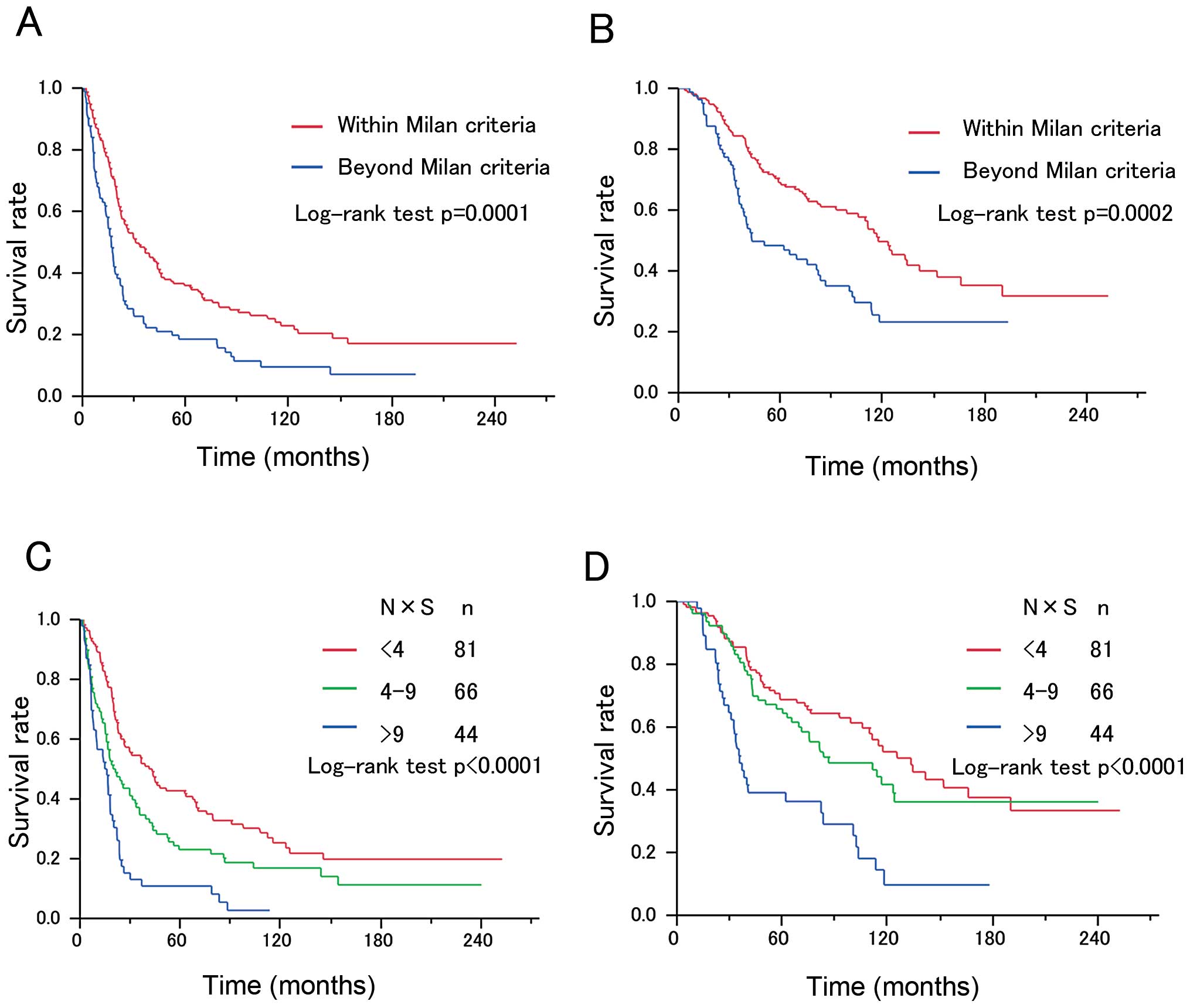
There were statistical differences in DFS and OS
between the two groups divided according to whether they fit the
Milan criteria (Fig. 1A and B).
The 1-year DFS rates were 88.2, 69.2 and 56.5%, the 3-year DFS
rates were 54.6, 34.6 and 13.0%, and the 5-year DFS rates were
42.7, 23.1 and 10.9% in patients with NxS factor <4, NxS factor
4–9 and NxS factor >9, respectively (Fig. 1C and D). There were statistical
differences in DFS and OS among the groups classified by NxS factor
(P<0.0001) (Fig. 1C and D).
Log-rank analysis for DFS identified NxS factor,
microscopic portal vein invasion, microscopic hepatic vein
invasion, Child-Pugh classification, and degree of Liver Damage as
significant prognostic factors (Table
II). DFS was not associated with tumor differentiation and
serum AFP levels. Multivariate analysis of the five variables that
achieved statistical significance in the univariate analysis for
DFS revealed that NxS factor and the degree of Liver Damage
classification were independent predictors (Table II). Notably, the hazard ratio (HR)
of the degree of Liver Damage classification showed higher values
(HR 1.93; 95%CI 1.37–2.70; P=0.0002) in comparison with other host
factors.
 | Table IIUnivariate analysis (log-rank test)
and multivariate analysis (Cox proportional hazards model) of
variables potentially predictive of disease-free survival in
patients with HCC (n=234). |
Table II
Univariate analysis (log-rank test)
and multivariate analysis (Cox proportional hazards model) of
variables potentially predictive of disease-free survival in
patients with HCC (n=234).
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|---|
| Variable | Median survival
(95% CI) (months) | P-value | HR (95% CI) | P-value |
|---|
| NxS factor | | <0.0001 | | |
| <4 | 42.3
(26.4–63.3) | | 1 | |
| 4–9 | 20.5
(15.4–33.1) | | 1.43
(1.02–2.00) | 0.0364 |
| >9 | 15.5
(8.1–18.2) | | 2.77
(1.83–4.17) | <0.0001 |
| Microscopic portal
vein invasion | | 0.0015 | | |
| Absent | 29.6
(21.9–39.3) | | 1 | |
| Present | 17.5
(9.4–22.9) | | 1.31
(0.91–1.86) | 0.1464 |
| Microscopic hepatic
vein invasion | | 0.0072 | | |
| Absent | 26.4
(21.0–36.5) | | 1 | |
| Present | 17.5
(9.3–23.5) | | 1.35
(0.92–1.94) | 0.1237 |
|
Differentiation | | 0.3236 | | |
| Well | 32.4
(22.5–56.1) | | | |
| Moderate | 21.0
(18.2–26.4) | | | |
| Poor | 22.9
(15.0–41.6) | | | |
| AFP | | 0.7067 | | |
| <400 | 24.4
(20.2–31.3) | | | |
| >400 | 19.2
(7.3–35.8) | | | |
| Child-Pugh | | 0.0281 | | |
| A | 24.1
(20.6–30.0) | | 1 | |
| B | 18.5
(9.2–36.5) | | 1.28
(0.79–2.04) | 0.3026 |
| Degree of liver
damage | | 0.0002 | | |
| A | 30.4
(22.4–43.6) | | 1 | |
| B | 18.9
(14.9–21.9) | | 1.93
(1.37–2.70) | 0.0002 |
PS score
Given that the NxS factor and the degree of Liver
Damage classification were independent risk factors for HCC
prognosis by multivariate analysis, we constructed the PS score by
combining the NxS factor with the degree of Liver Damage
classification. The score for the NxS factor can be easily obtained
by allocating NxS factor <4, 4–9 and >9 to Liver Damage
scores 0, 1 and 2, respectively (Table III). The score for the degree of
Liver Damage classification can be similarly obtained by allocating
Liver Damage A and B to scores 0 and 1, respectively (Table III).
 | Table IIIPS score. |
Table III
PS score.
| Score |
|---|
|
|
|---|
| 0 | 1 | 2 |
|---|
| NxS factor | <4 | 4–9 | >9 |
| Liver damage | A | B | |
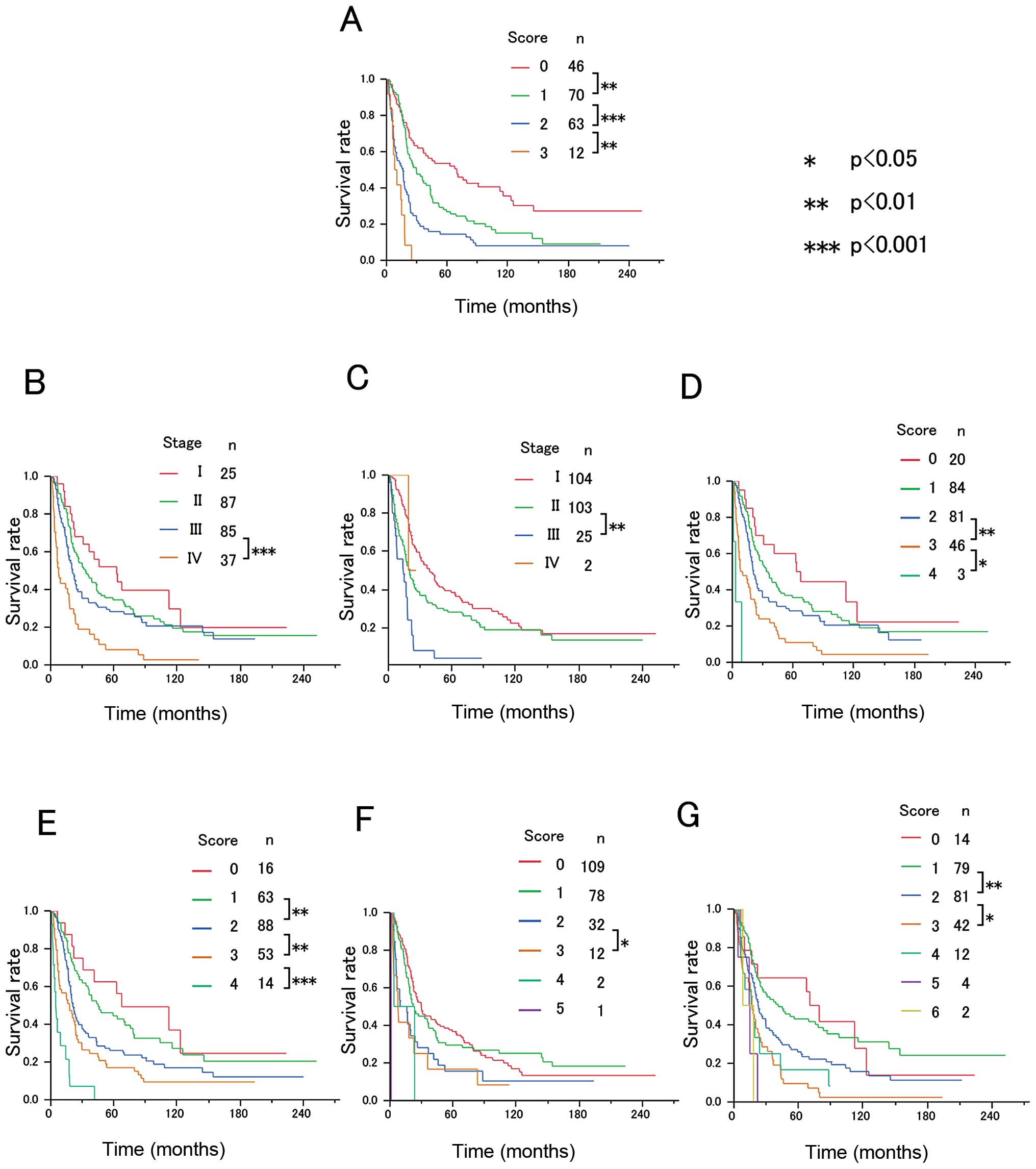
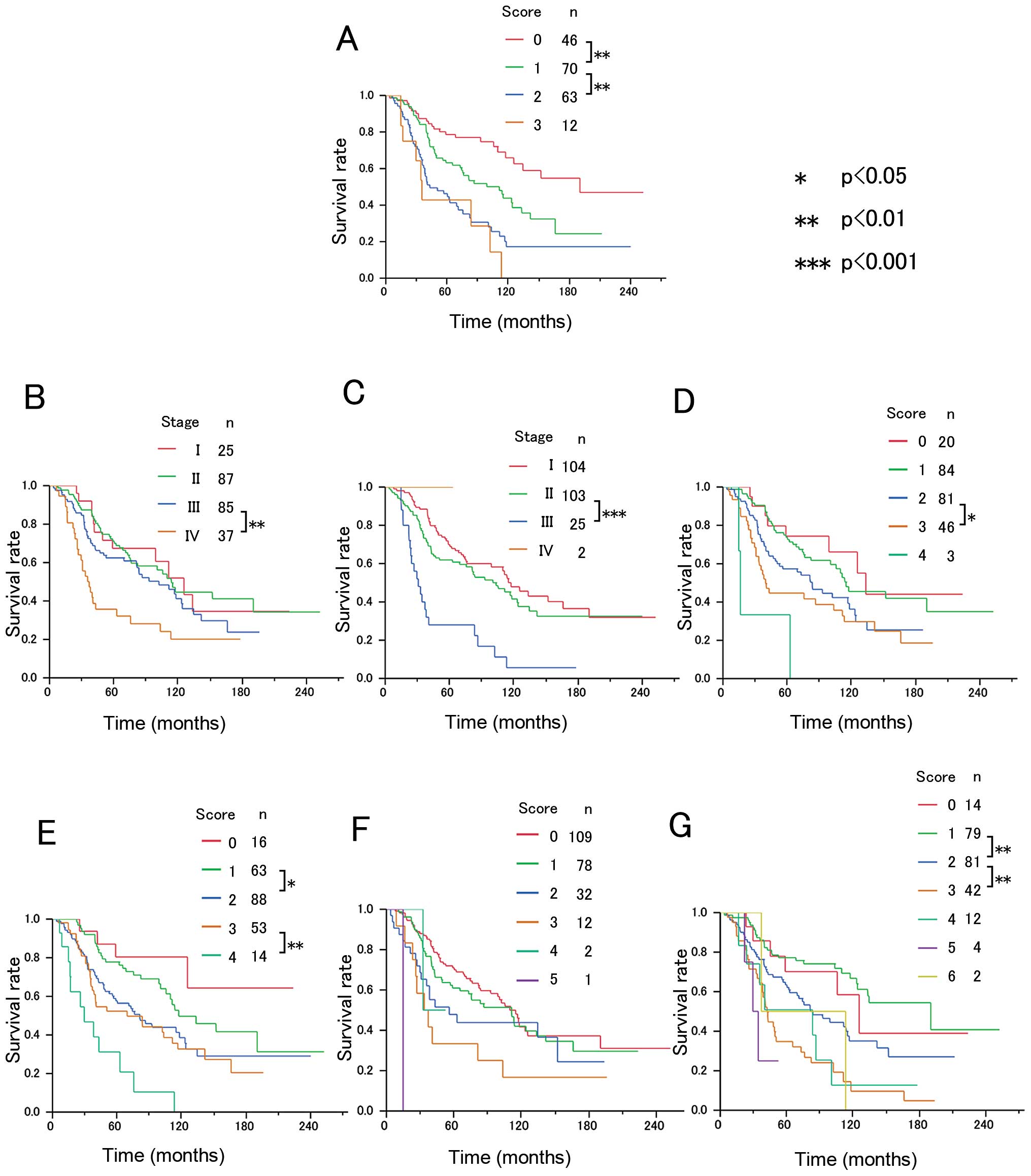
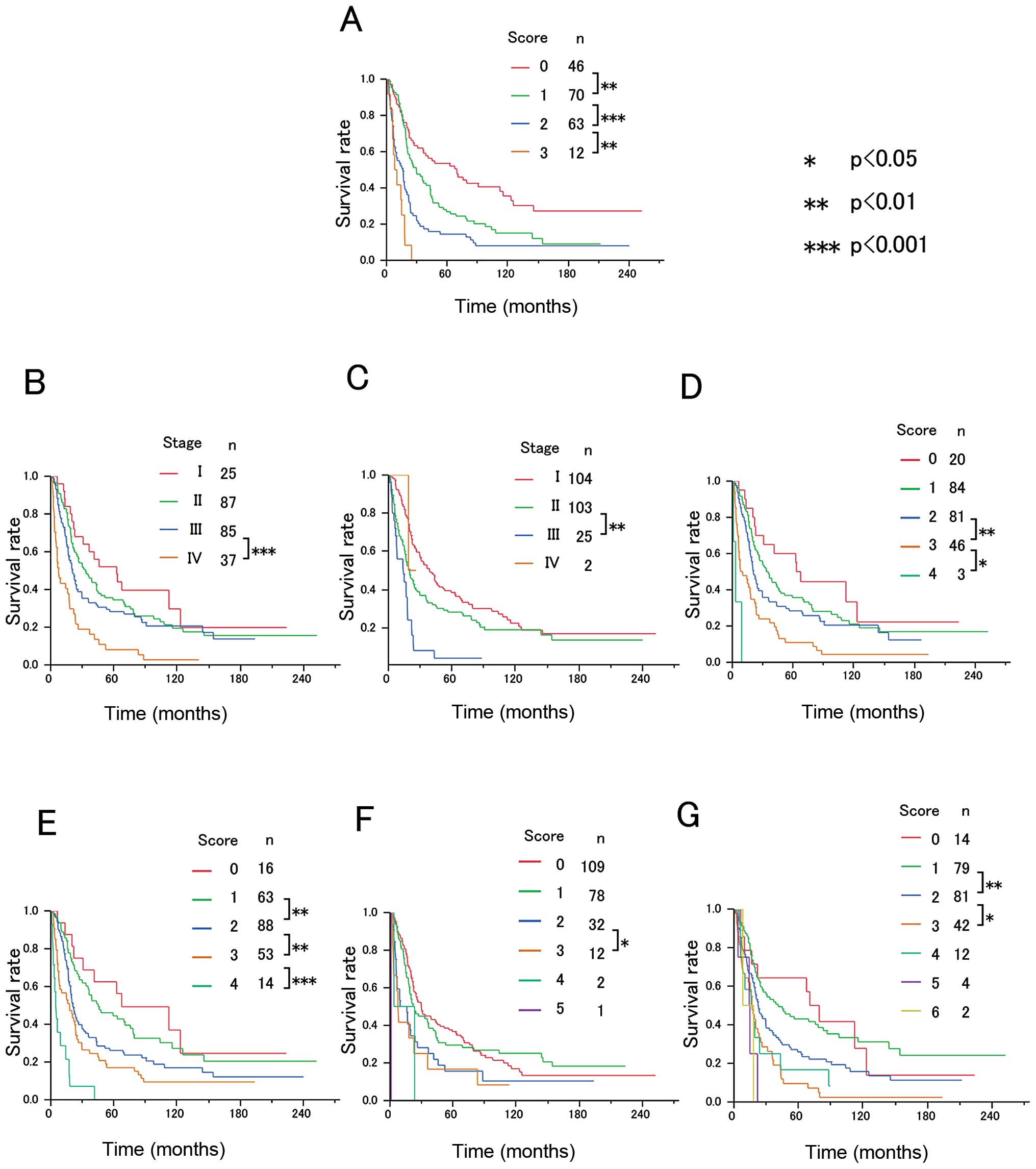
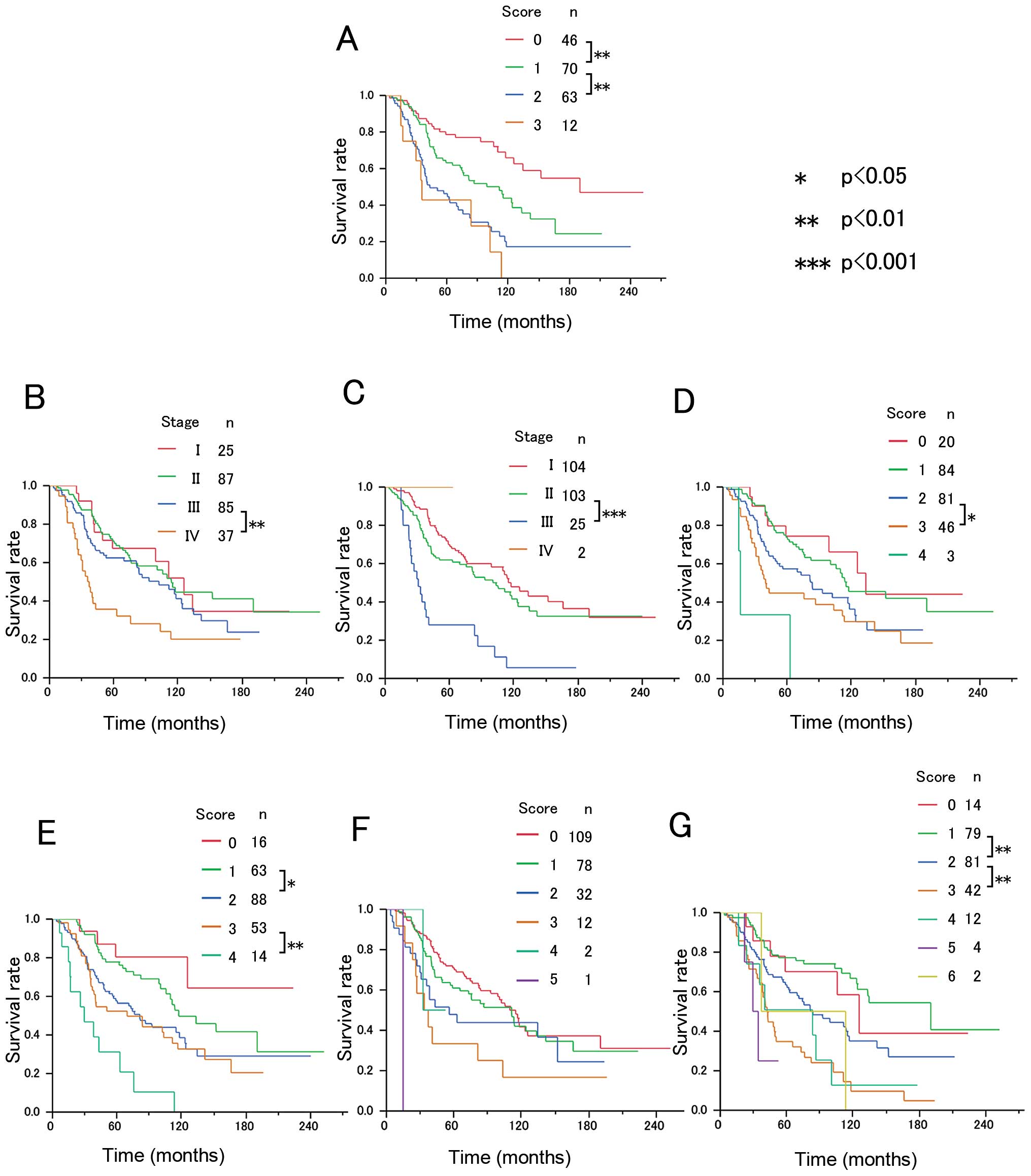
The Kaplan-Meier estimated DFS curves and OS curves
according to PS score, TNM staging system (LCSGJ), TNM staging
system (UICC), JIS score, modified JIS score, CLIP score, and Tokyo
score are depicted in Figs. 2 and
3, respectively. There were
significant differences (P<0.05) in both DFS and OS between
patients with different PS scores (PS score 0 vs. 1; PS score 1 vs.
2), and there was a significant difference in DFS, but not OS,
between patients with PS score 2 and those with PS score 3
(Figs. 2 and 3). Among the seven staging systems, only
the PS score demonstrated significant differences in DFS between
all adjacent strata.
 | Figure 2Comparison of disease-free survival
according to scoring systems: (A) PS score, (B) TNM (LCSGJ), (C)
TNM (UICC), (D) JIS, (E) M-JIS, (F) CLIP, and (G) Tokyo score. TNM,
tumor lymph node metastasis; LCSGJ, Liver Cancer Study Group of
Japan; UICC, Union for International Cancer Control; JIS, Japan
Integrated Staging score; m-JIS, modified Japan Integrated Staging
score; CLIP, Cancer of the Liver Italian Program. |
 | Figure 3Comparison of overall survival
according to scoring systems: (A) PS score, (B) TNM (LCSGJ), (C)
TNM (UICC), (D) JIS, (E) M-JIS, (F) CLIP, and (G) Tokyo score. TNM,
tumor lymph node metastasis; LCSGJ, Liver Cancer Study Group of
Japan; UICC, Union for International Cancer Control; JIS, Japan
Integrated Staging score; m-JIS, modified Japan Integrated Staging
score; CLIP, Cancer of the Liver Italian Program. |
Assessment of predictive ability of
staging systems
The PS score had smaller values of the Akaike
information criterion for both DFS and OS than any of the six
clinical staging systems [the TNM staging system (LSCGJ), TNM
staging system (UICC), CLIP score, JIS score, m-JIS score and Tokyo
score] (Table IV).
 | Table IVComparison of prognostic
stratification. |
Table IV
Comparison of prognostic
stratification.
| Component of the
score | AIC |
|---|
|
|
|
|---|
| Model | Tumor factor | Liver function | DFS | OS |
|---|
| PS score | (+) | (+) | 1791.19 | 1231.40 |
| TNM (LCSGJ) | (+) | (−) | 1810.51 | 1250.48 |
| TNM (UICC) | (+) | (−) | 1812.06 | 1242.38 |
| JIS | (+) | (+) | 1805.09 | 1249.85 |
| m-JIS | (+) | (+) | 1797.13 | 1240.21 |
| CLIP | (+) | (+) | 1816.89 | 1256.92 |
| Tokyo | (+) | (+) | 1811.63 | 1232.70 |
Discussion
We have developed a novel clinical scoring system,
the PS score, for accurate prediction of the outcome of HCC
patients after surgery by combining tumor factors and liver
function. The most important findings of the present study were
that there were significant differences in DFS between HCC patients
with different PS scores (score 0 vs 1; score 1 vs. 2; score 2 vs.
3), and the PS score had smaller values of the AIC for DFS than any
of the six well-known clinical staging systems. Such a precise
stratification for DFS in HCC patients after surgery will provide a
better understanding of the metastatic potentials of HCC, which
will become more and more essential in parallel with the advent of
effective systemic treatment options including molecular-targeted
agents (6).
Our successful result was largely due to the
integration of tumor number and the size of the largest tumor into
the NxS factor; tumor number and size of largest tumor were each
used as the main parameters in the TNM staging systems. The Milan
criteria (14) hinted that we
could increase the predictive power of the outcome of HCC patients
if we applied the Milan criteria to our system. We found that the
NxS factor had high accuracy in predicting HCC recurrence by
setting the optimal two cut-off values based on the Milan criteria.
Notably, the NxS factor can be obtained from modalities such as
computed tomography (CT) or magnetic resonance imaging (MRI).
Therefore, our newly-developed PS score is an easy-to-use
preoperative assessment tool because the information on
pathological vessel involvement is not needed, which is one of the
parameters for the conventional TNM staging systems and is
integrated into the JIS score and the modified JIS score (7,16,19).
Unsuccessful preoperative assessment causes a
potential limitation in these clinical staging systems due to
discrepancy between the pre- and postoperative status of HCC
patients (19). In this regard,
the PS score is fascinating because the score can be determined
preoperatively via several imaging modalities. HCC patients have
various backgrounds and divergent clinical courses, resulting in
the lower predictive power of many clinical staging systems
(20–22). In particular, liver function is
considered to be important from the viewpoint of multicentric
carcinogenesis and a necessity of additive surgical therapies
(23,24).
Recently, several staging systems for HCC based on
information of both tumor factors and liver function have been
proposed. The CLIP score has been successful in discriminating HCC
patients with regard to OS (11,25)
and has been well validated in predicting the prognosis of HCC
patients (26–28). Nevertheless, the CLIP score
functioned poorly in predicting OS and DFS in Japanese HCC patients
enrolled in the present study (Figs.
2F and 3F). One possible
explanation of this deficiency is that the criteria of 50% for
tumor extension in the liver used in the CLIP score system failed
to accurately capture features of HCC in Japan, where many smaller
tumors are detected based on the established screening system for
HCC.
To overcome the deficiency of the CLIP score, Kudo
et al developed the JIS score, composed of the Child-Pugh
classification and the TNM staging system of LCSGJ. Kudo et
al reported that this system had superior prognostic
capabilities regarding OS in HCC patients when compared with the
CLIP score (10,29). Thereafter, the JIS score gradually
came to be used for the evaluation of treatment modalities in
Japan.
In the present study, the JIS score worked poorly in
predicting DFS and OS of HCC patients undergoing hepatic resection
because most of them had Child-Pugh A disease. There was less
advantage with the JIS score, which was made by combining two
systems, the Child-Pugh classification and the TNM staging system
of the LCSGJ (8,16). Therefore, many Japanese liver
surgeons have not considered the JIS score to be effective in HCC
patients who have undergone hepatic resection (30).
More recently, Nanashima et al developed the
m-JIS score, which was constructed using the degree of Liver Damage
and the TNM staging system of the LCSGJ. These investigators showed
that the m-JIS score was a better predictor of prognosis than the
JIS score in HCC patients who underwent hepatic resection (8,16).
Ikai et al validated this system using the records of 42,269
HCC patients (31). In the present
study, the m-JIS score demonstrated better stratification for
prognosis after surgery and a smaller AIC value than did the JIS
score. This finding is supported by the concept that the assessment
of the degree of Liver Damage classification in the m-JIS score, in
which ICG-R15 was substituted for encephalopathy in the Child-Pugh
classification, could evaluate and classify liver function more
precisely than the Child-Pugh classification.
ICG-R15 (representing indocyanine green clearance)
has been used in the field of surgery routinely in Japan as a
useful marker of hepatic function and as a gauge for
decision-making regarding the permitted volume of hepatic resection
(32,33). Moreover, ICG-R15 is a significant
prognostic factor in HCC patients (34–36).
The substitution of ICG-R15 for encephalopathy in the PS score
might have reflected individual differences more accurately among
patients who underwent hepatic resection in the present study,
because none of them had any encephalopathy before operation.
In addition, the PS score had a smaller AIC value
than did the m-JIS score with respect to both DFS and OS. This
finding is supported by the concept that the NxS factor was more
prognostic than TNM staging by the LCSGJ for tumor characteristics.
The difference between the PS score and the m-JIS was confined to
the tumor factor because the degree of Liver Damage was
incorporated in both the PS score and the m-JIS score as liver
function.
The Tokyo score is a new prognostic scoring system
for patients who are candidates for radical therapy, such as
percutaneous ablation or surgical resection (9). This system consists of four factors:
tumor size, number of tumor nodules, serum albumin and bilirubin.
These factors can be obtained from laboratory data or images before
surgery. Although the Tokyo score can also become a clinical
staging system for HCC patients to predict their prognosis before
operation, this system has demonstrated poorer stratification than
did the PS score in the present study. The Tokyo score may have
been especially limited in its ability to stratify patients with an
advanced score (Tokyo scores 4–6) in the present study, because
most patients who had advanced cancer with poor liver function in
this study were not subjected to hepatic resection.
In the present study, we were unable to evaluate the
Barcelona Clinic Liver Cancer (BCLC) staging system (37), Chinese University Prognostic Index
(38), or other recently reported
systems (17, 39), because portal pressure, performance
status, and alkaline phosphatase levels were not fully recorded for
the patients enrolled in the present study. Although portal
hypertension is accepted as a strong predictor of poor prognosis
(40,41), formal measurement of hepatic venous
pressure gradient is a special examination that is not routinely
carried out in daily practice. However, all of the parameters used
by the PS score can be easily and safely obtained before the
operation.
In conclusion, the present study showed that the PS
score was superior to any of the well-known systems, including
CLIP, JIS, modified-JIS, and the Tokyo score in predicting the
prognosis of HCC patients.
There were several limitations in the present study:
it was a retrospective single-center study that enrolled only
patients who underwent curative hepatectomy. In this regard,
further studies will be needed to evaluate whether the robustness
of the PS score in predicting prognosis could be maintained in a
cohort in which the majority of the subjects were HCC patients who
received non-surgical treatment.
References
|
1
|
Forner A, Llovet JM and Bruix J:
Hepatocellular carcinoma. Lancet. 379:1245–1255. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Adachi E, Maeda T, Matsumata T, et al:
Risk factors for intra-hepatic recurrence in human small
hepatocellular carcinoma. Gastroenterology. 108:768–775. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ikeda K, Saitoh S, Tsubota A, et al: Risk
factors for tumor recurrence and prognosis after curative resection
of hepatocellular carcinoma. Cancer. 71:19–25. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Iizuka N, Hamamoto Y and Oka M: Predicting
individual outcomes in hepatocellular carcinoma. Lancet.
364:1837–1839. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Iizuka N, Oka M, Yamada-Okabe H, et al:
Oligonucleotide microarray for prediction of early intrahepatic
recurrence of hepatocellular carcinoma after curative resection.
Lancet. 361:923–929. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Llovet JM, Ricci S, Mazzaferro V, et al:
Sorafenib in advanced hepatocellular carcinoma. N Engl J Med.
359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Henderson JM, Sherman M, Tavill A,
Abecassis M, Chejfec G and Gramlich T: AHPBA/AJCC consensus
conference on staging of hepatocellular carcinoma: consensus
statement. HPB (Oxford). 5:243–250. 2003. View Article : Google Scholar
|
|
8
|
Nanashima A, Sumida Y, Morino S, et al:
The Japanese integrated staging score using liver damage grade for
hepatocellular carcinoma in patients after hepatectomy. Eur J Surg
Oncol. 30:765–770. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tateishi R, Yoshida H, Shiina S, et al:
Proposal of a new prognostic model for hepatocellular carcinoma: an
analysis of 403 patients. Gut. 54:419–425. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kudo M, Chung H, Haji S, et al: Validation
of a new prognostic staging system for hepatocellular carcinoma:
the JIS score compared with the CLIP score. Hepatology.
40:1396–1405. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
A new prognostic system for hepatocellular
carcinoma: a retrospective study of 435 patients: the Cancer of the
Liver Italian Program (CLIP) investigators. Hepatology. 28:751–755.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pugh RN, Murray-Lyon IM, Dawson JL,
Pietroni MC and Williams R: Transection of the oesophagus for
bleeding oesophageal varices. Br J Surg. 60:646–649. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
The general rules for the clinical and
pathological study of primary liver cancer. Kanehara; Tokyo:
2010
|
|
14
|
Mazzaferro V, Regalia E, Doci R, et al:
Liver transplantation for the treatment of small hepatocellular
carcinomas in patients with cirrhosis. N Engl J Med. 334:693–699.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Akaike H: A new look at the statistical
model identification. IEEE trans. Automatic Control. AC-19:716–723.
1974. View Article : Google Scholar
|
|
16
|
Nanashima A, Sumida Y, Abo T, et al:
Modified Japan Integrated Staging is currently the best available
staging system for hepatocellular carcinoma patients who have
undergone hepatectomy. J Gastroenterol. 41:250–256. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Omagari K, Honda S, Kadokawa Y, et al:
Preliminary analysis of a newly proposed prognostic scoring system
(SLiDe score) for hepatocellular carcinoma. J Gastroenterol
Hepatol. 19:805–811. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
OuYang PY, Su Z, Ma XH, Mao YP, Liu MZ and
Xie FY: Comparison of TNM staging systems for nasopharyngeal
carcinoma, and proposal of a new staging system. Br J Cancer.
109:2987–2997. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim BK, Han KH, Park YN, et al: Prediction
of microvascular invasion before curative resection of
hepatocellular carcinoma. J Surg Oncol. 97:246–252. 2008.
View Article : Google Scholar
|
|
20
|
Han KH, Kudo M, Ye SL, et al: Asian
consensus workshop report: expert consensus guideline for the
management of intermediate and advanced hepatocellular carcinoma in
Asia. Oncology. 81(Suppl 1): 158–164. 2011. View Article : Google Scholar
|
|
21
|
Pons F, Varela M and Llovet JM: Staging
systems in hepatocellular carcinoma. HPB (Oxford). 7:35–41. 2005.
View Article : Google Scholar
|
|
22
|
Chung H, Kudo M, Takahashi S, et al:
Review of current staging systems for hepatocellular carcinoma.
Hepatol Res. 37(Suppl 2): S210–S215. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Toyoda H, Kumada T, Kiriyama S, et al:
Comparison of the usefulness of three staging systems for
hepatocellular carcinoma (CLIP, BCLC, and JIS) in Japan. Am J
Gastroenterol. 100:1764–1771. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Toyama T, Hiramatsu N, Yakushijin T, et
al: A new prognostic system for hepatocellular carcinoma including
recurrent cases: a study of 861 patients in a single institution. J
Clin Gastroenterol. 42:317–322. 2008.PubMed/NCBI
|
|
25
|
Prospective validation of the CLIP score:
a new prognostic system for patients with cirrhosis and
hepatocellular carcinoma. The Cancer of the Liver Italian Program
(CLIP) Investigators. Hepatology. 31:840–845. 2000. View Article : Google Scholar
|
|
26
|
Hsu CY, Hsia CY, Huang YH, et al:
Selecting an optimal staging system for hepatocellular carcinoma:
comparison of 5 currently used prognostic models. Cancer.
116:3006–3014. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Shao YY, Lu LC, Lin ZZ, et al: Prognosis
of advanced hepatocellular carcinoma patients enrolled in clinical
trials can be classified by current staging systems. Br J Cancer.
107:1672–1677. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
op den Winkel M, Nagel D, Sappl J, et al:
Prognosis of patients with hepatocellular carcinoma. Validation and
ranking of established staging-systems in a large western
HCC-cohort. PLoS One. 7:e450662012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kudo M, Chung H and Osaki Y: Prognostic
staging system for hepatocellular carcinoma (CLIP score): its value
and limitations, and a proposal for a new staging system, the Japan
Integrated Staging Score (JIS score). J Gastroenterol. 38:207–215.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Luo KZ, Itamoto T, Amano H, et al:
Comparative study of the Japan Integrated Stage (JIS) and modified
JIS score as a predictor of survival after hepatectomy for
hepatocellular carcinoma. J Gastroenterol. 43:369–377. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ikai I, Takayasu K, Omata M, et al: A
modified Japan Integrated Stage score for prognostic assessment in
patients with hepatocellular carcinoma. J Gastroenterol.
41:884–892. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wakabayashi H, Ishimura K, Izuishi K,
Karasawa Y and Maeta H: Evaluation of liver function for hepatic
resection for hepatocellular carcinoma in the liver with damaged
parenchyma. J Surg Res. 116:248–252. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lau H, Man K, Fan ST, Yu WC, Lo CM and
Wong J: Evaluation of preoperative hepatic function in patients
with hepatocellular carcinoma undergoing hepatectomy. Br J Surg.
84:1255–1259. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Fukuda S, Itamoto T, Amano H, et al:
Clinicopathologic features of hepatocellular carcinoma patients
with compensated cirrhosis surviving more than 10 years after
curative hepatectomy. World J Surg. 31:345–352. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kim SH, Choi SB, Lee JG, et al: Prognostic
factors and 10-year survival in patients with hepatocellular
carcinoma after curative hepatectomy. J Gastrointest Surg.
15:598–607. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Matsuda M, Omata F, Fuwa S, et al:
Prognosis of patients with hepatocellular carcinoma treated solely
with transcatheter arterial chemoembolization: risk factors for
one-year recurrence and two-year mortality (preliminary data).
Intern Med. 52:847–853. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Llovet JM, Fuster J and Bruix J: The
Barcelona approach: diagnosis, staging, and treatment of
hepatocellular carcinoma. Liver Transpl. 10:S115–S120. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Leung TW, Tang AM, Zee B, et al:
Construction of the Chinese University Prognostic Index for
hepatocellular carcinoma and comparison with the TNM staging
system, the Okuda staging system, and the Cancer of the Liver
Italian Program staging system: a study based on 926 patients.
Cancer. 94:1760–1769. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kinoshita A, Onoda H, Imai N, et al: The
Glasgow Prognostic Score, an inflammation based prognostic score,
predicts survival in patients with hepatocellular carcinoma. BMC
Cancer. 13:522013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Boleslawski E, Petrovai G, Truant S, et
al: Hepatic venous pressure gradient in the assessment of portal
hypertension before liver resection in patients with cirrhosis. Br
J Surg. 99:855–863. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Hidaka M, Takatsuki M, Soyama A, et al:
Intraoperative portal venous pressure and long-term outcome after
curative resection for hepatocellular carcinoma. Br J Surg.
99:1284–1289. 2012. View Article : Google Scholar : PubMed/NCBI
|