Introduction
Pancreatic cancer is one of the most deadly
malignancies. In contrast to the stable or declining trends for
most other cancer types, incidence rates are increasing for cancers
of the pancreas (1). Despite the
use of multimodality treatment, the overall 5-year survival rate
for pancreatic cancer is only six percent because of its high
recurrence rate (1). Invasion and
metastasis are the major causes of the poor prognosis of pancreatic
cancer (2). The coordination of
intercellular adhesion, cell-matrix interaction, matrix
degradation, and cell migration is essential for cancer cell
invasion and metastasis, and a diverse variety of transmembrane
proteins regulate these cellular events (3–5).
Notably, proteins of the tetraspanin superfamily, such as Tspan8
(6), CD82 (7), CD9 (8), and CD151 (9) are important for the regulation of
tumor cell motility and the interaction between tumor cells and
their microenvironment. Therefore, tetraspanins may represent
promising diagnostic or prognostic markers and therapeutic targets
for tumor progression (10,11).
TM4SF1 is a member of the tetraspanin superfamily
(12). Tetraspanins are
characterized by four transmembrane domains delimiting two
extracytoplasmic regions of unequal size (13). Elevated expression of TM4SF1 has
been reported in several tumor types, and is implicated in cancer
cell migration and patient outcome, but it adopts different roles
that are dependent upon tumor type (14–17).
In addition, TM4SF1 is important for endothelial cell migration and
tumor angiogenesis (18,19), although the underlying mechanism of
its function is not clear, especially in pancreatic cancer.
In the present study, we investigated the role of
TM4SF1 in pancreatic ductal adenocarcinoma (PDAC). TM4SF1
expression in PDAC tissues was evaluated by immunohistochemistry,
and the correlation between clinicopathological characteristics and
TM4SF1 expression was assessed to determine its prognostic
significance in PDAC. To determine the biomolecular functions of
TM4SF1 in pancreatic cancer cells, we investigated changes in cell
migration and invasion in vitro using a siRNA knockdown
approach.
Materials and methods
Cell lines
The following six pancreatic cancer cell lines were
used: KP-2, SUIT-2 (Dr H. Iguchi, National Shikoku Cancer Center,
Matsuyama, Japan), MIA PaCa-2 (Japanese Cancer Resource Bank,
Tokyo, Japan), Capan-1, Capan-2 and Hs766T (American Type Culture
Collection, Manassas, VI, USA). The human immortalized pancreatic
ductal epithelial cell line (HPDE6-E6E7 clone 6) was kindly
provided by Dr Ming-Sound Tsao (University of Toronto, Toronto,
Canada). All cells were maintained as previously described
(20).
Pancreatic tissues
We analyzed TM4SF1 expression in 74 tissue samples
obtained from patients who underwent pancreatic resection for
pancreatic cancer at our institution between January 2000 and
August 2009. We also obtained normal pancreatic tissue samples from
intact pancreas resected for bile duct cancer as control tissues.
Survival was measured from the time of pancreatic resection, with
death as the end-point. Overall survival and disease-free survival
analyses were performed in February 2012. The median observation
time for overall survival and disease-free survival was 19 months
(range 2–137 months) and 11 months (range 1–137 months),
respectively. Forty-nine patients died during the follow-up. All
surviving patients were censored. Histological diagnosis of
specimens was in accordance with the criteria of the updated World
Health Organization classification (21). Tumor stage was assessed according
to the UICC classification, 7th edition (22). The clinicopathological
characteristics of all patients are summarized in Table I. The study was approved by the
Ethics Committee of Kyushu University and conducted according to
the Ethical Guidelines for Human Genome/Gene Research enacted by
the Japanese Government and the Helsinki Declaration.
 | Table IClinicopathological characteristics
of patients with PDAC (N=74). |
Table I
Clinicopathological characteristics
of patients with PDAC (N=74).
| Median age | 66.55 (range 36–86
years) |
|---|
| Gender
(male/female) | 46 (62.2%)/28
(37.8%) |
| pT category |
| T1 | 2 (2.7%) |
| T2 | 2 (2.7%) |
| T3 | 68 (91.9%) |
| T4 | 2 (2.7%) |
| pN category |
| pN0 | 16 (21.6%) |
| pN1 | 58 (78.4%) |
| UICC stage |
| I | 3 (4.1%) |
| II | 68 (91.8%) |
| III | 2 (2.7%) |
| IV | 1 (1.4%) |
| Residual tumor
category |
| R0 | 52 (70.3%) |
| R1 | 22 (29.7%) |
| Histologic
grade |
| Grade 1 | 13 (17.6%) |
| Grade 2 | 35 (47.3%) |
| Grade 3 | 26 (35.1%) |
| Vascular
invasion |
| Negative | 20 (27.3%) |
| Positive | 54 (72.7%) |
| Perineural
invasion |
| Negative | 6 (8.2%) |
| Positive | 68 (91.8%) |
| Lymphatic
invasion |
| Negative | 17 (23%) |
| Positive | 57 (77%) |
Quantitative reverse transcription
polymerase chain reaction (qRT-PCR)
One-step real-time qRT-PCR using gene-specific
primers was performed as described previously (23). Primer sequences were as follows:
TM4SF1 forward 5′-ATTGGAAT TGCAGGATCTGG-3′ and reverse
5′-GCCGAGGGAATCAA GACATA-3′; 18S rRNA forward 5′-GTAACCCGTTGAACC
CCATT-3′ and reverse 5′-CCATCCAATCGGTAGTAGCG-3′. BLAST searches
were performed to ensure the specificity of all primers. Primers
were purchased from Sigma Genosys (Tokyo, Japan).
Immunohistochemical procedures and
evaluation
Immunohistochemistry was performed using a Histofine
SAB-PO kit (Nichirei, Tokyo, Japan) (24). Sections were incubated with
anti-TM4SF1 antibody (HPA002823; Sigma-Aldrich, Tokyo, Japan)
overnight at 4°C. Carcinoma cells were identified according to
morphology and counted in at least 20 fields per section at ×200
magnification. The distribution of TM4SF1 staining was evaluated as
the percentage of stained cells, and was scored as follows: 0, no
staining or <10%; 1, 11–25%; 2, 26–50%; 3, 51–75%; or 4,
76–100%. Cells were also scored for staining intensity, which was
scored as 0, no staining; 1, weak; 2, moderate; or 3, strong. The
multiplication product (from 0–12) from these two scores was used
to assign patients into one of two groups according to TM4SF1
expression, where a score of 0–4 represented low expression and a
score of 6–12 represented high expression. All slides were
evaluated independently by two investigators who were unaware of
the clinical features of each case.
Silencing of TM4SF1 using small
interfering RNAs (siRNAs)
Gene silencing was carried out using siRNA (Qiagen,
MA, USA) directed against human TM4SF1. Sequences were as follows:
siRNA-1 (sense, 5′-ggaccacuaugucuugauutt-3′; antisense,
5′-aaucaagacauaguggucctt-3′); siRNA-2 (sense, 5′-cgaug
acugggcaagaagatt-3′; antisense, 5′-ucuucuugcccagucaucgta-3′).
Qiagen all-star siRNA was used as a negative control. Transfections
were performed as described previously (25). All cells were used in subsequent
experiments 48 h after transfection.
Matrigel invasion and migration
assays
Migration and invasion of cultured cancer cells were
assessed by counting the number of cells migrating or invading
through uncoated or Matrigel-coated transwell chambers (BD
Biosciences, Franklin Lakes, NJ, USA) as described previously
(20,26). Cells were maintained in 10%
FBS/DMEM during these assays. Cells were transfected with siRNAs 48
h prior to experimentation. Migration was determined after a 24-h
period, and invasiveness was determined after a 48-h period.
TGF-β1 treatment
SUIT-2 and Capan-2 cells were cultured in 6-well
plates (1×105 cells/well) in 1% FBS/DMEM with or without
10 ng/ml recombinant human TGF-β1 (R&D, Oxon, UK) for 24 and 48
h (27). At each time-point, total
RNA was extracted to evaluate TM4SF1 mRNA expression by qRT-PCR. To
evaluate TM4SF1 protein levels, cells were seeded in 90-mm dishes
at a density of 2×105 cells/dish and cultured in 1%
FBS/DMEM with or without 10 ng/ml TGF-β1 prior to cell lysis.
Western blot analysis
Western blotting was performed as described
previously (28). Antibodies used
in this study were as follows: anti-TM4SF1 (sc-103267; Santa Cruz,
CA, USA), anti-E-cadherin (no. 3195), anti-vimentin (no. 5741),
anti-N-cadherin (no. 4061), anti-claudin-1 (no. 4933) (Cell
Signaling Technology, Danvers, MA, USA) and anti-β actin (ab8227;
Abcam, Cambridge, MA, USA).
Statistical analysis
A χ2 test was used to analyze the
correlation between TM4SF1 expression and clinicopathological
characteristics. Survival analysis was performed using Kaplan-Meier
analysis and curves were compared using the log-rank test. For
in vitro experiments, values are expressed as means ±
standard deviation. Comparison between two groups was performed
using the Student’s t-test. Statistical significance was defined as
P<0.05. All statistical analyses were performed using JMP 9.0.2
software (SAS Institute, NC, USA).
Results
Pancreatic cancer cells express
TM4SF1
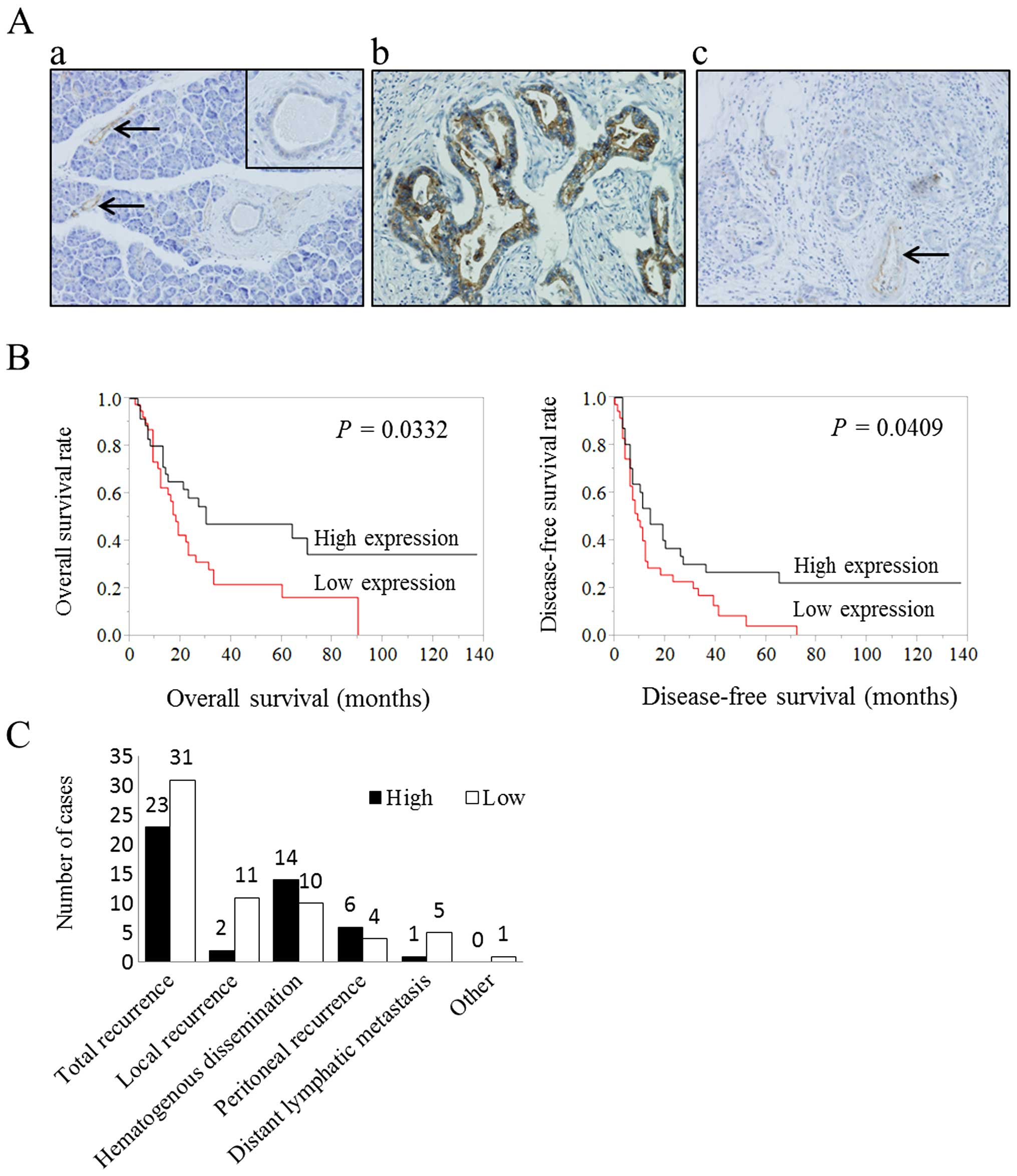
We first sought to determine the level of TM4SF1
expression in PDAC and normal pancreatic tissues. In normal
pancreatic tissues, weak-to-no staining was detected in pancreatic
ductal epithelial cells and TM4SF1 expression was not observed in
acinar cells or stroma. Blood vessels consistently stained positive
for TM4SF1, and were used as a positive control (Fig. 1A-a and -c). In tumor tissues,
strong luminal membrane surface staining and a weak-to-moderate
cytoplasmic staining was detected in cancer cells (Fig. 1A-b). In addition to tumor tissue
samples where moderate staining was observed, there were also tumor
tissue samples where little-to-no staining was observed (Fig. 1A-c).
Prognostic significance of TM4SF1
expression
Survival analysis was performed for patients with
PDAC. The high TM4SF1 expression group showed better survival
(P=0.0332; Fig. 1B) than the low
expression group, and there was an obvious difference in the
disease-free time between the groups (P=0.0409; Fig. 1B). Median survival was 30 months
for the high expression group and 17 months for the low expression
group (Table II). Next, we
performed multivariate analysis based on the Cox proportional
hazard model on all parameters that were found to be significant in
the univariate analyses. Overall survival was significantly
dependent on residual tumor (R1) status (relative risk = 2.732,
P=0.0017), vascular invasion (relative risk = 2.461, P=0.0101) and
low TM4SF1 expression (relative risk = 1.987, P=0.0196) (Table III).
 | Table IIUnivariate survival analysis of
conventional prognostic factors and TM4SF1 expression in PDAC
patient resections (N=74). |
Table II
Univariate survival analysis of
conventional prognostic factors and TM4SF1 expression in PDAC
patient resections (N=74).
|
Characteristics | No. of cases | Median survival
time (months) | 5-year survival
rate | P-value |
|---|
| TM4SF1
expression | | | | 0.0332 |
| High | 35 | 30 | 40.8 | |
| Low | 39 | 17 | 13.2 | |
| Age (years) | | | | 0.3099 |
| <65 | 27 | 23 | 38.0 | |
| ≥65 | 47 | 23 | 17.7 | |
| UICC stage | | | | 0.0774 |
| I/IIA | 15 | 60 | 44.1 | |
| IIB/III/IV | 59 | 19 | 18.6 | |
| Histological
grade | | | | 0.4285 |
| Grade 1/grade
2 | 48 | 23 | 30.8 | |
| Grade 3 | 26 | 19 | 14.2 | |
| Residual tumor | | | | 0.0001 |
| R0 | 52 | 30 | 36.8 | |
| R1 | 22 | 11 | 2.8 | |
| Vascular
invasion | | | | 0.0079 |
| Negative | 20 | 60 | 53.1 | |
| Positive | 54 | 17 | 14.0 | |
| Perineural
invasion | | | | 0.1458 |
| Negative | 6 | 90 | 60.3 | |
| Positive | 68 | 19 | 23.8 | |
| Lymphatic
invasion | | | | 0.0667 |
| Negative | 17 | 60 | 46.5 | |
| Positive | 57 | 19 | 21.0 | |
 | Table IIIMultivariate analysis of conventional
prognostic factors and TM4SF1 expression in PDAC patients
(N=74). |
Table III
Multivariate analysis of conventional
prognostic factors and TM4SF1 expression in PDAC patients
(N=74).
|
Characteristics | Relative risk | 95% confidence
interval | P-value |
|---|
| Low TM4SF1
expression | 1.987 | 1.116–3.632 | 0.0196 |
| R factor | 2.732 | 1.479–4.949 | 0.0017 |
| Vascular
invasion | 2.461 | 1.226–5.503 | 0.0101 |
The relationship between TM4SF1 expression and
clinicopathological factors of PDAC is shown in Table IV. There was no statistically
significant correlation between TM4SF1 expression and
clinicopathological factors possibly due to the relatively small
size of the patient cohort, although it appears that the patients
with low expression have a higher tumor grade and a more advanced
clinical stage. Because there was an obvious difference in the
disease-free time, we analyzed the site of first recurrence
(Fig. 1C) and found that the
locoregional recurrence rate in the low TM4SF1 expression group
(28.21%) was higher than in the high expression group (5.71%;
P=0.0079) although the total recurrence rates for the two patients
groups were similar (Table V). The
data suggest that tumors with low TM4SF1 expression undergo local
spread more frequently than those with high expression, and this
may contribute to the observed survival differences.
 | Table IVRelationship between TM4SF1
expression and various clinicopathological factors in patients with
PDAC (N=74). |
Table IV
Relationship between TM4SF1
expression and various clinicopathological factors in patients with
PDAC (N=74).
|
Characteristics | High expression
group
n=35 (47.3%) | Low expression
group
n=39 (52.7%) | P-value |
|---|
| Age (years) | | | 0.9115 |
| <65 | 13 (37.14) | 14 (35.90) | |
| ≥65 | 22 (62.86) | 25 (64.10) | |
| pT category | | | 0.9114 |
| pT1/pT2 | 2 (5.71) | 2 (5.13) | |
| pT3/pT4 | 33 (94.29) | 37 (94.87) | |
| pN Category | | | 0.4179 |
| pNo | 9 (25.71) | 7 (17.95) | |
| pN1 | 26 (74.29) | 32 (82.05) | |
| UICC stage | | | 0.6002 |
| I/IIA | 8 (22.86) | 7 (17.95) | |
| IIB/III/IV | 27 (77.14) | 32 (82.05) | |
| Histological
grade | | | 0.5263 |
| Grade 1/grade
2 | 24 (68.57) | 24 (61.54) | |
| Grade 3 | 11 (31.43) | 15 (38.46) | |
| Residual tumor
category | | | 0.8363 |
| R0 | 25 (71.43) | 27 (69.23) | |
| R1 | 10 (28.57) | 12 (30.77) | |
| Lymphatic
invasion | | | 0.9821 |
| Negative | 8 (22.86) | 9 (23.08) | |
| Positive | 27 (77.14) | 30 (76.92) | |
| Vascular
invasion | | | 0.8095 |
| Negative | 9 (25.71) | 11 (28.21) | |
| Positive | 26 (74.29) | 28 (71.79) | |
| Perineural
invasion | | | 0.3189 |
| Negative | 4 (11.43) | 2 (5.13) | |
| Positive | 31 (88.57) | 37 (94.87) | |
 | Table VRelationship between TM4SF1
expression and patterns of recurrence in patients with PDAC
(N=74). |
Table V
Relationship between TM4SF1
expression and patterns of recurrence in patients with PDAC
(N=74).
|
Characteristics | High expression
group
n=35 (47.3%) | Low expression
group
n=39 (52.7%) | P-value |
|---|
| Total
recurrence | | | 0.1823 |
| Negative | 12 (34.29) | 8 (20.51) | |
| Positive | 23 (65.71) | 31 (79.49) | |
| Local
recurrence | | | 0.0079 |
| Negative | 33 (94.29) | 28 (71.79) | |
| Positive | 2 (5.71) | 11 (28.21) | |
| Hematogenous
dissemination | | | 0.8363 |
| Negative | 21 (60.00) | 29 (74.36) | |
| Positive | 14 (40.00) | 10 (25.64) | |
| Peritoneal
recurrence | | | 0.3866 |
| Negative | 29 (82.86) | 35 (89.74) | |
| Positive | 6 (17.14) | 4 (10.26) | |
| Distant lymphatic
metastasis | | | 0.0647 |
| Negative | 34 (97.14) | 34 (87.18) | |
| Positive | 1 (2.86) | 5 (12.82) | |
Inhibition of TM4SF1 expression promotes
migration and invasion of pancreatic cancer cells
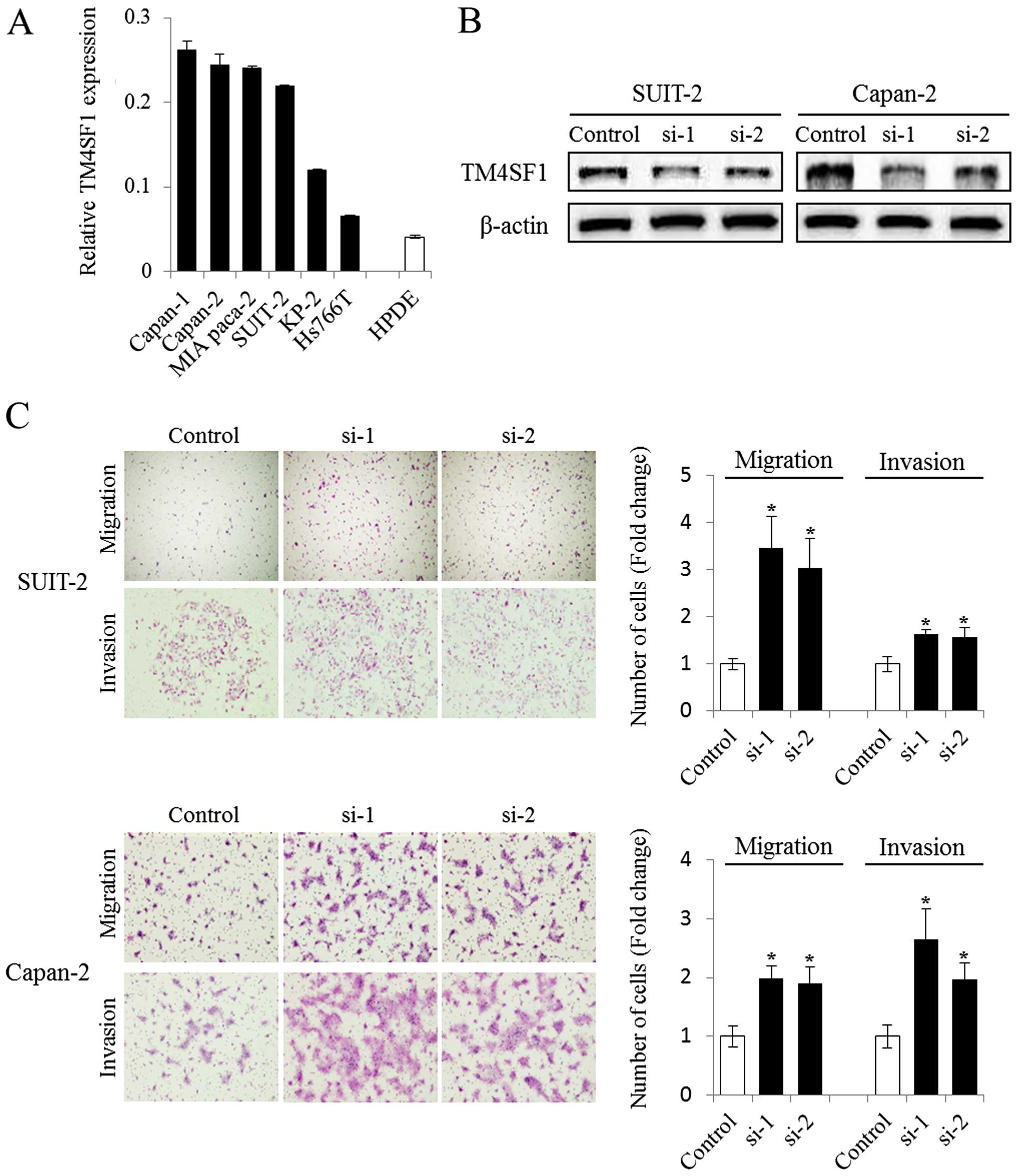
We also determined the level of TM4SF1 expression in
a variety of pancreatic cancer cell lines, and the level of TM4SF1
mRNA expression was found to be higher in pancreatic cancer cell
lines than in normal (HPDE) epithelial cells (Fig. 2A). Because local tumor invasion is
more likely in patients with low TM4SF1 tumor expression, and
because TM4SF1 has been reported to be involved in the migration of
cancer cells (14,15), we next performed migration and
invasion assays following knockdown of TM4SF1 in pancreatic cancer
cells. Decreased TM4SF1 protein expression was confirmed by western
blotting following transfection of cells with TM4SF1-specific siRNA
(Fig. 2B). The invasion and
migration of two cell lines studied, SUIT-2 and Capan-2, were
enhanced following siRNA-mediated knockdown of TM4SF1 (Fig. 2C). These suggest that TM4SF1 has an
inhibitory role in the invasion and migration of pancreatic cancer
cells.
E-cadherin expression is reduced in
pancreatic cancer cells following knockdown of TM4SF1
Because the process of cancer invasion requires
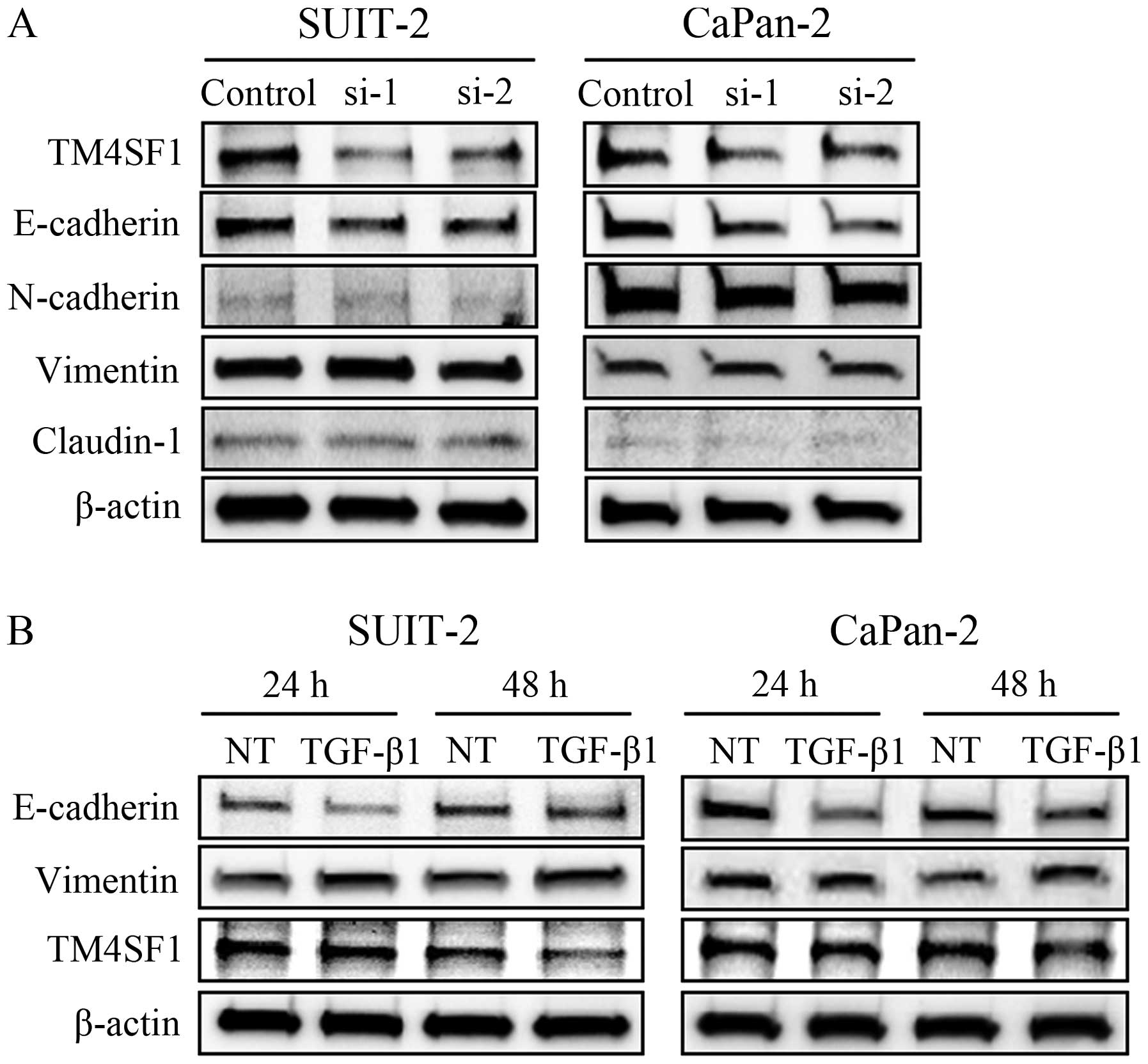
epithelial tumor cells to undergo epithelial to mesenchymal
transition (EMT) either transiently or stably (29), we examined the correlation between
the expression of TM4SF1 and EMT markers in vitro. We found
that E-cadherin expression was reduced after knockdown of TM4SF1,
but there were no changes in the expression of other makers
including vimentin, N-cadherin and claudin-1 (Fig. 3A). Changes in cell morphology,
however, were not observed after knockdown of TM4SF1 (data not
shown).
TGF-β1 negatively regulates TM4SF1
expression
TGF-β1 is a major inducer of EMT in a number of
cellular contexts (30), and plays
a pivotal role in driving EMT in the pathogenesis of pancreatic
cancer (27,31). To investigate whether TGF-β1
influences TM4SF1 expression, we performed additional in
vitro analyses on pancreatic cancer cells treated with TGF-β1.
Western blot analysis revealed that TGF-β1 treatment significantly
downregulated E-cadherin expression and upregulated vimentin
expression in both these cell lines. TM4SF1 protein levels were
also reduced following treatment with TGF-β1 for 48 h (Fig. 3B).
Discussion
TM4SF1 is a tumor-associated antigen that is
detected widely in human carcinomas (32), and it represents a promising target
for antibody-mediated immunotherapy (33). However, the exact role of TM4SF1 in
cancer remains controversial. TM4SF1 is reported to be a prognostic
marker in a number of malignant tumors. In lung (14) and colorectal cancer (34) patients, increased expression of
TM4SF1 was shown to be significantly associated with early
postoperative relapse and shorter survival. In contrast, our study
revealed that decreased expression of TM4SF1 was significantly
associated with shorter survival and early local spread in PDAC
patients, suggesting that TM4SF1 plays an inhibitory role in
pancreatic cancer relapse and tumor progression. These results are
consistent with those of a previous study of TM4SF1 in mesothelioma
patients (16). Furthermore,
serial analysis of gene expression in breast cancer tissues
revealed a negative correlation between TM4SF1 expression and
progression of breast carcinomas (17). These data suggest that TM4SF1 may
be a novel predictive marker of good prognosis in several tumors
including PDAC, although the clinical significance of TM4SF1
expression varies depending on tumor type.
With respect to the cellular functions of TM4SF1, it
has previously been reported that high expression of TM4SF1
increases the invasiveness of lung carcinoma cells (14) and the migration of prostate cancer
cells (15). Our study
demonstrates a contrasting function for TM4SF1 in pancreatic cancer
cells as cancer cell motility was enhanced following inhibition of
TM4SF1 expression, a finding which may account for the differences
in local recurrence rate and prognosis among PDAC patients.
Furthermore, we found that knockdown of TM4SF1 reduced E-cadherin
expression in pancreatic cancer cells (although other EMT markers
examined were unaffected) and that treatment with TGF-β1
downregulated TM4SF1 in these cells. E-cadherin is closely
implicated in the motility of cancer cells (35), and loss of E-cadherin expression is
associated with poor clinical outcome in several cancer types
(36,37) including pancreatic cancer (38). Our findings therefore suggest a
role for TM4SF1 in TGF-β1-induced EMT, and that TM4SF1 may alter
the migration of pancreatic cancer cells partially via regulating
E-cadherin expression. Targeting TM4SF1 expression may therefore
potentially lead to the development of promising therapies for
several types of tumor, including PDAC.
Previous reports indicate that tetraspanins, through
protein-protein and protein-lipid interactions, recruit various
transmembrane and cytoplasmic proteins to form tetraspanin-enriched
microdomains (TERM), functional complexes involved in cell
migration (39). Tetraspanins
interact with a variety of transmembrane proteins, participate in
various TERM formations, and can perform different functions in a
variety of cell types. For example, CD151, one of the tetraspanin
members, regulates cell migration in a cell type-specific manner
(40). The CD151-α6β4 complex is a
major component of hemidesmosomes in skin keratinocytes, structures
that oppose cell migration by stabilizing cell attachment to the
extracellular matrix (41).
However, in human cervical carcinoma cells, CD151 promotes tumor
cell migration but does not appear to affect cell adhesion to
matrix proteins (42). TM4SF1 is
also associated with TERM, and influences cell motility via
regulating the surface presentation and endocytosis of a number of
components of these complexes (43). Therefore, we speculate that in
diverse tissues or cell types, TM4SF1 may interact with different
transmembrane proteins (such as E-cadherin) and influence cell
migration by modulating the endocytosis and recycling of proteins
associated with motility.
In conclusion, our results suggest that TM4SF1 plays
an inhibitory role in the migration and invasion of pancreatic
cancer cells. Further investigation is now needed to elucidate the
mechanisms of interaction between TM4SF1 and either E-cadherin or
TGF-β1 in the migration and invasion of pancreatic cancer cells.
Furthermore, decreased expression of TM4SF1 is significantly
associated with shorter survival in PDAC patients, suggesting that
TM4SF1 is a promising prognostic biomarker in PDAC.
Acknowledgements
This study was supported by Grant-in-Aid from the
Ministry of Education, Culture, Sports, Science and Technology of
Japan (grant nos. 26293305 and 25293285). We are grateful to Emiko
Manabe and Miyuki Omori (Department of Surgery and Oncology, Kyushu
University) for skillful technical assistance, and thankful for
scholarships to Biao Zheng by China Scholarship Council (http://www.csc.edu.cn/).
References
|
1
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
DiMagno EP, Reber HA and Tempero MA;
American Gastroenterological Association. AGA technical review on
the epidemiology, diagnosis, and treatment of pancreatic ductal
adenocarcinoma. Gastroenterology. 117:1464–1484. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ellenrieder V, Adler G and Gress TM:
Invasion and metastasis in pancreatic cancer. Ann Oncol. 10(Suppl
4): S46–S50. 1999. View Article : Google Scholar
|
|
4
|
Boucheix C, Duc GH, Jasmin C and
Rubinstein E: Tetraspanins and malignancy. Expert Rev Mol Med.
2001:1–17. 2001.
|
|
5
|
Zöller M: Tetraspanins: Push and pull in
suppressing and promoting metastasis. Nat Rev Cancer. 9:40–55.
2009. View
Article : Google Scholar
|
|
6
|
Kanetaka K, Sakamoto M, Yamamoto Y,
Takamura M, Kanematsu T and Hirohashi S: Possible involvement of
tetraspanin CO-029 in hematogenous intrahepatic metastasis of liver
cancer cells. J Gastroenterol Hepatol. 18:1309–1314. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ruseva Z, Geiger PX, Hutzler P, Kotzsch M,
Luber B, Schmitt M, Gross E and Reuning U: Tumor suppressor KAI1
affects integrin alphavbeta3-mediated ovarian cancer cell adhesion,
motility, and proliferation. Exp Cell Res. 315:1759–1771. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Longo N, Yáñez-Mó M, Mittelbrunn M, de la
Rosa G, Muñoz ML, Sánchez-Madrid F and Sánchez-Mateos P: Regulatory
role of tetraspanin CD9 in tumor-endothelial cell interaction
during transendothelial invasion of melanoma cells. Blood.
98:3717–3726. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Novitskaya V, Romanska H, Dawoud M, Jones
JL and Berditchevski F: Tetraspanin CD151 regulates growth of
mammary epithelial cells in three-dimensional extracellular matrix:
Implication for mammary ductal carcinoma in situ. Cancer Res.
70:4698–4708. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Adachi M, Taki T, Ieki Y, Huang CL,
Higashiyama M and Miyake M: Correlation of KAI1/CD82 gene
expression with good prognosis in patients with non-small cell lung
cancer. Cancer Res. 56:1751–1755. 1996.PubMed/NCBI
|
|
11
|
Nakamoto T, Murayama Y, Oritani K,
Boucheix C, Rubinstein E, Nishida M, Katsube F, Watabe K, Kiso S,
Tsutsui S, et al: A novel therapeutic strategy with anti-CD9
antibody in gastric cancers. J Gastroenterol. 44:889–896. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Marken JS, Schieven GL, Hellström I,
Hellström KE and Aruffo A: Cloning and expression of the
tumor-associated antigen L6. Proc Natl Acad Sci USA. 89:3503–3507.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Maecker HT, Todd SC and Levy S: The
tetraspanin superfamily: molecular facilitators. FASEB J.
11:428–442. 1997.PubMed/NCBI
|
|
14
|
Kao YR, Shih JY, Wen WC, Ko YP, Chen BM,
Chan YL, Chu YW, Yang PC, Wu CW and Roffler SR: Tumor-associated
antigen L6 and the invasion of human lung cancer cells. Clin Cancer
Res. 9:2807–2816. 2003.PubMed/NCBI
|
|
15
|
Allioli N, Vincent S, Vlaeminck-Guillem V,
Decaussin-Petrucci M, Ragage F, Ruffion A and Samarut J: TM4SF1, a
novel primary androgen receptor target gene over-expressed in human
prostate cancer and involved in cell migration. Prostate.
71:1239–1250. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gordon GJ, Jensen RV, Hsiao LL, Gullans
SR, Blumenstock JE, Richards WG, Jaklitsch MT, Sugarbaker DJ and
Bueno R: Using gene expression ratios to predict outcome among
patients with mesothelioma. J Natl Cancer Inst. 95:598–605. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Abba MC, Drake JA, Hawkins KA, Hu Y, Sun
H, Notcovich C, Gaddis S, Sahin A, Baggerly K and Aldaz CM:
Transcriptomic changes in human breast cancer progression as
determined by serial analysis of gene expression. Breast Cancer
Res. 6:R499–R513. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zukauskas A, Merley A, Li D, Ang LH,
Sciuto TE, Salman S, Dvorak AM, Dvorak HF and Jaminet SC: TM4SF1: A
tetraspanin-like protein necessary for nanopodia formation and
endothelial cell migration. Angiogenesis. 14:345–354. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shih SC, Zukauskas A, Li D, Liu G, Ang LH,
Nagy JA, Brown LF and Dvorak HF: The L6 protein TM4SF1 is critical
for endothelial cell function and tumor angiogenesis. Cancer Res.
69:3272–3277. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ohuchida K, Mizumoto K, Murakami M, Qian
LW, Sato N, Nagai E, Matsumoto K, Nakamura T and Tanaka M:
Radiation to stromal fibroblasts increases invasiveness of
pancreatic cancer cells through tumor-stromal interactions. Cancer
Res. 64:3215–3222. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hruban RH, Klöppel G, Boffetta P, et al:
Ductal adenocarcinoma of the pancreas. WHO Classification of
Tumours of the Digestive System. World Health Organization; pp.
281–291. 2010
|
|
22
|
Edge SB, Byrd DR, Compton CC, et al:
Exocrine and Endocrine Pancreas, AJCC Cancer Staging Manual. 7th
edition. Springer; New York, NY: pp. 241–248. 2010
|
|
23
|
Cui L, Ohuchida K, Mizumoto K, Moriyama T,
Onimaru M, Nakata K, Nabae T, Ueki T, Sato N, Tominaga Y, et al:
Prospectively isolated cancer-associated CD10 (+) fibroblasts have
stronger interactions with CD133 (+) colon cancer cells than with
CD133 (−) cancer cells. PLoS One. 5:e121212010. View Article : Google Scholar
|
|
24
|
Ikenaga N, Ohuchida K, Mizumoto K, Cui L,
Kayashima T, Morimatsu K, Moriyama T, Nakata K, Fujita H and Tanaka
M: CD10+ pancreatic stellate cells enhance the
progression of pancreatic cancer. Gastroenterology. 139:1041–1051.
51 e1–8. 2010. View Article : Google Scholar
|
|
25
|
Moriyama T, Ohuchida K, Mizumoto K, Cui L,
Ikenaga N, Sato N and Tanaka M: Enhanced cell migration and
invasion of CD133+ pancreatic cancer cells cocultured
with pancreatic stromal cells. Cancer. 116:3357–3368. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Iwamoto Y, Tanaka K, Okuyama K, Sugioka Y
and Taniguchi S: In vitro assay of the invasive potential of
malignant bone and soft tissue tumours through basement membranes.
Int Orthop. 18:240–247. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ikenaga N, Ohuchida K, Mizumoto K, Akagawa
S, Fujiwara K, Eguchi D, Kozono S, Ohtsuka T, Takahata S and Tanaka
M: Pancreatic cancer cells enhance the ability of collagen
internalization during epithelial-mesenchymal transition. PLoS One.
7:e404342012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kozono S, Ohuchida K, Eguchi D, Ikenaga N,
Fujiwara K, Cui L, Mizumoto K and Tanaka M: Pirfenidone inhibits
pancreatic cancer desmoplasia by regulating stellate cells. Cancer
Res. 73:2345–2356. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
De Craene B and Berx G: Regulatory
networks defining EMT during cancer initiation and progression. Nat
Rev Cancer. 13:97–110. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
30
|
Moustakas A and Heldin CH: Induction of
epithelial-mesenchymal transition by transforming growth factor β.
Semin Cancer Biol. 22:446–454. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lou C, Zhang F, Yang M, Zhao J, Zeng W,
Fang X, Zhang Y, Zhang C and Liang W: Naringenin decreases
invasiveness and metastasis by inhibiting TGF-β-induced epithelial
to mesenchymal transition in pancreatic cancer cells. PLoS One.
7:e509562012. View Article : Google Scholar
|
|
32
|
Svensson HP, Frank IS, Berry KK and Senter
PD: Therapeutic effects of monoclonal antibody-beta-lactamase
conjugates in combination with a nitrogen mustard anticancer
prodrug in models of human renal cell carcinoma. J Med Chem.
41:1507–1512. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tu SH, Huang HI, Lin SI, Liu HY, Sher YP,
Chiang SK, Chong P, Roffler S, Tseng GC, Chen HW, et al: A novel
HLA-A2-restricted CTL epitope of tumor-associated antigen L6 can
inhibit tumor growth in vivo. J Immunother. 35:235–244. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Schiedeck TH, Wellm C, Roblick UJ, Broll R
and Bruch HP: Diagnosis and monitoring of colorectal cancer by L6
blood serum polymerase chain reaction is superior to
carcinoembryonic antigen-enzyme-linked immunosorbent assay. Dis
Colon Rectum. 46:818–825. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kang Y and Massagué J:
Epithelial-mesenchymal transitions: Twist in development and
metastasis. Cell. 118:277–279. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bringuier PP, Umbas R, Schaafsma HE,
Karthaus HF, Debruyne FM and Schalken JA: Decreased E-cadherin
immunoreactivity correlates with poor survival in patients with
bladder tumors. Cancer Res. 53:3241–3245. 1993.PubMed/NCBI
|
|
37
|
Endo K, Ueda T, Ueyama J, Ohta T and
Terada T: Immunoreactive E-cadherin, alpha-catenin, beta-catenin,
and gamma-catenin proteins in hepatocellular carcinoma:
Relationships with tumor grade, clinicopathologic parameters, and
patients’ survival. Hum Pathol. 31:558–565. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Shimamura T, Sakamoto M, Ino Y, Sato Y,
Shimada K, Kosuge T, Sekihara H and Hirohashi S: Dysadherin
overexpression in pancreatic ductal adenocarcinoma reflects tumor
aggressiveness: Relationship to e-cadherin expression. J Clin
Oncol. 21:659–667. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hemler ME: Tetraspanin proteins mediate
cellular penetration, invasion, and fusion events and define a
novel type of membrane microdomain. Annu Rev Cell Dev Biol.
19:397–422. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Berditchevski F: Complexes of tetraspanins
with integrins: More than meets the eye. J Cell Sci. 114:4143–4151.
2001.PubMed/NCBI
|
|
41
|
Sterk LM, Geuijen CA, Oomen LC, Calafat J,
Janssen H and Sonnenberg A: The tetraspan molecule CD151, a novel
constituent of hemidesmosomes, associates with the integrin
alpha6beta4 and may regulate the spatial organization of
hemidesmosomes. J Cell Biol. 149:969–982. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Testa JE, Brooks PC, Lin JM and Quigley
JP: Eukaryotic expression cloning with an antimetastatic monoclonal
antibody identifies a tetraspanin (PETA-3/CD151) as an effector of
human tumor cell migration and metastasis. Cancer Res.
59:3812–3820. 1999.PubMed/NCBI
|
|
43
|
Lekishvili T, Fromm E, Mujoomdar M and
Berditchevski F: The tumour-associated antigen L6 (L6-Ag) is
recruited to the tetraspanin-enriched microdomains: Implication for
tumour cell motility. J Cell Sci. 121:685–694. 2008. View Article : Google Scholar : PubMed/NCBI
|