Introduction
Programmed cell death-1 (PD-1/PDCD1), also known as
CD279, is a 288-amino acid cell surface protein that belongs to the
immunoglobulin superfamily. PD-1 is expressed by immune cells,
including T cells, B cells and macrophages (1). High-level expression of the PD-1
ligand (CD274 or B7-H1) in tumor cells has been found to be
associated with increased tumor aggressiveness and poor prognosis
(2,3). When PD-1 binds its ligand, immune
cell activation and effector function are attenuated (4,5). The
PD-1/programmed death-ligand 1 (PD-L1) pathway is associated with
cancer immune-evasion, autoimmunity, and Listeria
monocytogenes infection (6).
Previous studies have implicated PD-L1 interactions in
immune-attenuation at peripheral sites outside lymphatic organs
(7,8). As antibodies are natural antagonists,
inhibition of the PD-1/PD-L1 signaling pathway with antibodies may
improve host tumor clearance and restore the immune function of
lymphocytes. This presents a novel direction for antitumor
immunotherapy.
A number of monoclonal antibodies (mAbs) targeting
the PD-1/PD-L1 checkpoint are undergoing clinical trials, and have
thus far exhibited encouraging therapeutic effects (6,8,9).
However, the low response rate in a small number of cancer patients
limits their utilization (10–13).
In addition, adverse events have frequently been observed during
antibody treatment, such as antibody-dependent cell-mediated
cytotoxicity (14–16), which reduces the effectiveness of
the therapy and restricts clinical application. Therefore, it is
important to develop mAbs with reduced toxicity for the
immunotherapeutic treatment of patients with cancer, and to
determine how to maximize their efficacy.
PD-1/PD-L1-targeting therapy has been used in recent
years for the treatment of a variety of solid tumors, including
non-small cell lung cancer (17,18),
malignant melanoma (19,20), urothelial carcinoma (21,22),
triple-negative breast cancer (23), lymphoma (24) and head and neck cancer (25). However, the application of
PD-1/PD-L1 checkpoint inhibitors in hepatocellular carcinoma (HCC)
is not well reported. In addition, studies have demonstrated that
abnormal PD-L1 expression in tumor tissues is significantly
associated with the degree of tumor malignancy, poor prognosis and
low survival rates (26–30). However, the clinical significance
of PD-1 expression in HCC tissues is not well understood, and it
remains to be determined whether PD-1 may be used as a biomarker
for the immunotherapeutic treatment of HCC. Therefore, in the
present study, a novel PD-1 mAb (9E11) with the most sensitive
experimental effects in immunohistochemistry (IHC) was selected as
the primary antibody to detect the expression of PD-1 in HCC
tissues by IHC. In addition, the correlation between PD-1
expression in HCC tissues and the clinicopathological features of
patients was assessed, in order to explore the potency of an
anti-PD-1 monoclonal antibody as an immunotherapeutic agent for the
treatment of HCC. These results may facilitate the application of
anti-PD-1 monoclonal antibody in the immunotherapeutic treatment of
patients with HCC.
Materials and methods
Clinical specimens
HCC tissue specimens from 77 cases (64 males and 13
females), collected between January and December 2014 from the
Pathology Department of the Daping Hospital Third Military Medical
University (Chongqing, China), were fixed in formalin and embedded
in paraffin. All patients included in the analysis were diagnosed
with HCC following surgery and had received no adjuvant
radiotherapy, chemotherapy, biological therapy or other treatments.
HCC was staged according to the Union for International Cancer
Control/American Joint Committee On Cancer 2010 tumor, node and
metastasis (TNM) staging criteria. This project was conducted in
accordance with the Declaration of Helsinki and was approved by the
Ethics Committee of Daping Hospital and Research Institute of
Surgery, Third Military Medical University. Written informed
consent was obtained from the subjects for the entire research
process in this study. All specimens were anonymized and handled
according to the aforementioned ethical and legal standards.
Cells and animals
The mouse myeloma cell line SP2/0-Ag14 was obtained
from the American Type Culture Collection (cat. no. CRL-1581;
Manassas, VA, USA). Specific pathogen-free female BALB/c mice
(weight, 18–20 g; age, 6–7 weeks) were purchased from Charles River
Laboratories (Saint Constant, QC, Canada). Procedures involving
animals and their care were conducted at Yes Biotech Laboratories
registered animal facility (license no. 0107-01; Yes Biotech
Laboratories Ltd., Mississauga, ON, Canada) under the Animals for
Research Act and at the supervision of Ontario Ministry of
Agriculture, Food and Rural Affairs (Guelph, ON, Canada). The mice
were maintained at 20–23°C, with a humidity of 40–60% and exposed
to 12 h/12 h light-dark cycles. Mice were fed on Laboratory Rodent
Diet 5001 purchased from Ren’s Pets Depot (Oakville, ON, Canada).
The procedures and pain level assessments were reviewed and
approved by Yes Biotech Laboratories Animal Care Committee and
complied with the Animals for Research Act.
Chemicals and reagents
Freund’s complete adjuvant and Freund’s incomplete
adjuvant solutions were purchased from Sigma-Aldrich; Merck KGaA
(Darmstadt, Germany). Incomplete medium used for hybridoma
development consisted of base medium and supplements purchased from
Gibco; Thermo Fisher Scientific, Inc. (Waltham, MA, USA). The
incomplete medium contained 50% RPMI-1640 (cat. no. 11875-093), 50%
Dulbecco’s modified Eagle’s medium/F12 (cat. no. 11320-033), 1%
L-glutamine (200 mM; cat. no. 15039-027), 1% minimum essential
medium-non essential amino acids (cat. no. 11140-050), 0.1%
mercapotoethanol (cat. no. 21985-023), and 1%
Antibiotic-Antimycotic (cat. no. 15240-062). Complete medium
consisted of incomplete medium supplemented with 10% fetal bovine
serum (cat. no. 10091-148; Gibco, Thermo Fisher Scientific, Inc.).
Polyethylene glycol 1500 [PEG 1500; 50% (w/v)] was purchased from
Roche Diagnostics (Lavel, QC, Canada). Recombinant Human PD-1/PDCD1
protein was purchased from ACROBiosystems (Newark, DE, USA).
Control mouse anti-PD-1 monoclonal antibody (clone ID: UMAB199),
horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (cat.
no. ZB-2305) and diaminobenzidine (DAB) were purchased from OriGene
Technologies, Inc. (Beijing, China). Normal goat serum and neutral
gum were purchased from Wuhan Boster Biological Technology, Ltd.
(Wuhan, China). 4-chloro-1-naphthol substrate (cat. no. C8890) was
purchased from Sigma-Aldrich; Merck KGaA. The Mouse Typer
Sub-Isotyping kit was purchased from Bio-Rad Laboratories, Inc.
(Hercules, CA, USA).
Preparation of mAbs
The mAbs were prepared by Yes Biotech Laboratories
Ltd. A total of 4 BALB/c mice were used for this project. The mice
were divided into two equal groups, and were immunized using the
same procedure. The first immunization was performed subcutaneously
at multiple sites on the back of each mouse with 200 μl
emulsion consisting of phosphate-buffered saline (PBS) containing
25 μg recombinant PD-1 protein (cat. no. PD1-H5221;
ACROBiosystems) and 100 μl complete Freund’s adjuvant
solution. The immunization was boosted twice intraperitoneally (IP)
with an emulsion containing 25 μg PD-1 protein and 100
μl incomplete Freund’s adjuvant at 3-week intervals. At 10
days following the second booster injection, 4 μl blood was
collected from the tip of the mouse tail. The antibody titers in
the serum were assessed by indirect ELISA method using the
recombinant PD-1 (immunogen)-coated ELISA plates (developed
in-house by Yes Biotech Laboratories Ltd.). The negative control in
the indirect ELISA was PBS, which was the diluent for the mouse
serum samples. The blank control was substrate reading. A final
booster injection was performed with 25 μg PD-1 protein in
50 μl PBS (IP). At 4 days following the final booster
injection, the mice with the desired antibody titer
(>106) were sacrificed by cervical dislocation by a
trained animal technician. The spleen was removed and spleen cells
were isolated. A total of 108 cells were obtained from
each spleen of the immunized mice. The spleen cells were mixed with
the Sp2/0-Ag14 myeloma cells, which were pre-selected with
8-azaguanine (cat. no. A5284; Sigma-Aldrich; Merck KGaA) for fusion
in a sterile centrifuge tube in the presence of 50% PEG 1500 (cat.
no. 783641; Roche Applied Science), as previously described
(31,32). At 24 h following fusion, the
hybridomas were selected by adding 100 μl of complete medium
supplemented with 1% hypoxanthine-aminopterin-thymidine (cat. no.
31062-011; Gibco; Thermo Fisher Scientific, Inc.) to each well. At
8 days following fusion, the supernatants were tested for PD-1
antibody by indirect ELISA method using the recombinant PD-1
(immunogen)-coated plates. Cells whose supernatants exhibiting
strong reactivity with immunogen in the indirect ELISA were
subcloned by a limiting dilution procedure in complete medium
supplemented with 1% hypoxanthine-thymidine (cat. no. 11067-030;
Gibco; Thermo Fisher Scientific, Inc.).
Isotyping and antibody purification
The mAb isotypes secreted by the hybridomas were
determined using the Mouse Typer Sub-Isotyping kit (cat. no.
1722051; Bio-Rad Laboratories, Inc.) according to the
manufacturer’s instructions. This ELISA-based kit uses a panel of
ultrapure reagents to determine the mouse sub-isotypes IgG1, IgG2a,
IgG2b, IgG3, IgM, IgA, κ and λ chains. In the experiment, PD-1 was
coated onto an ELISA microplate, and then each specific anti-PD-1
monoclonal antibody was added to the respective columns. The
isotype antibodies were added to respective horizontal rows.
Immunoglobulin isotypes were then determined using goat anti-rabbit
(H+L) HRP conjugate (dilution, 1:2,000; cat. no. 172-1019; Bio-Rad
Laboratories, Inc.) and 3,3′,5,5′-tetramethylbenzidine substrate
(cat. no. 00-4201-56; Thermo Fisher Scientific, Inc.).
Subsequently, the mAbs were purified using GammaBind Plus sepharose
resin (cat. no. 17088602; GE Healthcare Life Sciences, Little
Chalfont, UK).
Measurement of mAb specificity by western
blot analysis
A 15% PAGE gel was prepared and SDS-PAGE was
performed as described previously (33) using recombinant PD-1 protein (cat.
no. PD1-H5221; ACROBiosystems) following denaturation for 10 min at
100°C. The PD-1 protein was loaded at 40 ng/lane. Following
electrophoresis, the protein was transferred to polyvinylidene
difluoride membranes (Merck KGaA) at 150 mA for 2 h in transfer
buffer at 4°C. The membranes were washed five times with PBS
containing 0.05% Tween -20 (PBST), and blocked with 3% gelatin in
PBS at room temperature for 2 h. The membranes were subsequently
cut into strips along the lane dividers. Each of the 14 prepared
PD-1 antibodies were quantified with a spectrophotometer by
measuring the absorbance of the antibody samples at 280 nm. The
antibodies were then diluted to 1 μg/ml in PBST, and
incubated with individual strips at room temperature for 2 h.
Following five washes with PBST, the strips were incubated with
HRP-conjugated goat anti-mouse IgG (Yes Biotech Laboratories Ltd.)
diluted to 1:1,000 in PBST with 1% bovine serum albumin (cat. no.
81-003-07; Merck KGaA) for 1 h at room temperature. The strips were
then washed five times with PBST. The 40-kD PD-1 bands were
visualized by incubating the membranes with 4-chloro-1-naphthol
substrate (cat. no. C8890; Sigma-Aldrich; Merck KGaA).
Measurement of mAb specificity for PD-1
in HCC specimens by IHC staining
The paraffin-embedded tissues specimens collected
from HCC patients were prepared and stored by the Pathology
Department of the Daping Hospital Third Military Medical
University. The 3-μm-thick tissue sections were dewaxed in
xylene, rehydrated in alcohol and immersed in 3% hydrogen peroxide
for 10 min at room temperature to suppress endogenous peroxidase
activity. Antigen retrieval was performed by heating each section
for 30 min in 0.01 mol/l sodium citrate buffer (pH 6.0) at 100°C.
Sections were then washed three times in PBS (each for 5 min).
After blocking any nonspecific binding with ready-to-use normal
goat serum for 30 min at 37°C, the sections were incubated in a
humidified chamber overnight at 4°C with each of the 14 prepared
PD-1 mAbs (diluted, 1:400). The commercial anti-PD-1 mAb (dilution,
1:400; cat. no. UMAB199) was used as the positive control, while
PBS was used as the negative control. The sections were then
incubated with HRP-conjugated goat anti-mouse IgG (diluted, 1:500;
cat. no. ZB-2305; OriGene Technologies, Inc.) for 30 min at room
temperature. Following three additional washes, peroxidase activity
was developed with DAB for 5 min at room temperature. The sections
were counterstained with 0.2% hematoxylin for 1 min at room
temperature. The optical density of the sections was quantitatively
analyzed using Image-Pro Plus 6.0 software (Media Cybernetics,
Inc., Rockville, MD, USA).
Assessing the correlation between PD-1
expression and clinical significance in HCC
The paraffin-embedded HCC tissues were stained with
0.2% hematoxylin for 5 min and counterstained with 0.5% eosin for 1
min at room temperature to identify the cancer tissues and the
adjacent normal regions. According to the results of the mAb
analyses, the highest-specificity PD-1 mAb (9E11) was selected to
detect the expression of PD-1 in HCC tissues, in order to assess
the correlation between the expression of PD-1 in the tumor tissues
and the clinicopathological features of patients, and to evaluate
the feasibility of utilizing an anti-PD-1 mAb in the treatment of
HCC. The IHC methods used were the same as those described
above.
Two experienced pathologists evaluated tissue
staining intensity and positive cell percentage scoring in a
double-blind manner (34,35). A total of five T lymphocyte
infiltration-dense regions were selected for counting the number of
PD-1+ T lymphocytes in each tissue section. The
expression levels of PD-1 were defined by a ‘quickscore’, which was
calculated according to the methods described previously (34,35).
Briefly, the proportion of positively stained cells throughout the
section was termed category A, and was assigned a score ranging
from 0 to 3 (0, 0–4%; 1, 5–24%; 2, 25–49%; 3, 50–100%). The entire
section was scanned at low microscopic power in order to gauge the
levels of staining intensity. The average intensity defined as
negative (colorless), weak (pale yellow), intermediate (pale
brown), or strong staining (dark brown) was assigned a score
ranging from 0 to 3, and termed category B. The product (A + B) was
recorded as the total score. Total scores <3 were considered to
indicate negative PD-1 expression, while total scores ≥3 were
considered to indicate positive PD-1 expression.
In addition to the aforementioned methods, the
number of positive cells per field of view was evaluated under a
high-powered microscope by two experienced pathologists as
described previously (36). A
total of five T lymphocyte infiltration-dense regions (at ×200
magnification) were selected for counting the number of PD-1
positive cells in each tissue section. PD-1 expression levels in
HCC tissues were determined by calculating the number of
PD-1+ T lymphocytes per field of view.
Statistical analysis
IBM SPSS Statistics software (version 23.0; IBM
Corp., Armonk, NY, USA) was used for statistical analysis. The
results were expressed as the mean ± standard deviation.
Differences among multiple groups were compared by one-way analysis
of variance followed by the Games-Howell post hoc test. The
χ2 and Fisher’s exact test were used for the comparison
of categorical variables. The Mann-Whitney U test was applied for
the comparison of ranked data. The evaluation of multiple factors
was performed by stepwise binary logistic regression. P<0.05 was
considered to indicate statistically significant difference.
Results
Immunized BALB/c mice meet the
requirements of cell fusion experiments
The recombinant human PD-1/PDCD1 protein was used as
an antigen to immunize BALB/c mice. Blood was collected from the
mice tail tips at 10 days following the final booster injection,
and the antibody titers in the serum were assessed by indirect
ELISA. As shown in Table I, serum
antibody titers reached 1:107, and the desired
immunization effect was therefore achieved for subsequent cell
fusion experiments.
 | Table IAntibody titers in the sera of the
immunized mice. |
Table I
Antibody titers in the sera of the
immunized mice.
| Group |
1:103 |
1:104 |
1:105 |
1:106 |
1:107 |
1:108 | Negative
control | Blank control |
|---|
| 1 | 2.642 | 1.722 | 0.699 | 0.386 | 0.201 | 0.063 | 0.052 | 0.040 |
| 2 | 2.944 | 2.327 | 0.973 | 0.332 | 0.148 | 0.090 | 0.041 | 0.039 |
Successful production of 14 specific PD-1
mAbs
Splenocytes from the immunized BALB/c mice were
fused with the mouse myeloma cell line Sp2/0-Ag14. PD-1 mAbs were
generated and assigned the following names: 1C4, 1H8, 2C4, 2H7,
3E5, 5B2, 5H7, 7C9, 7E5, 7G12, 9A5, 9B4, 9E11 and B1C4. Following
repeated serial culture in vitro, cryopreservation and
revival, the hybridomas maintained a normal morphology and
continuously secreted PD-1 mAbs (data not shown).
Identification of the mAb isotypes
The isotypes of the 14 mAbs were determined using a
Mouse Typer Sub-Isotyping kit. As shown in Table II, the heavy chains of 13 mAbs
were IgG1, while clone 9A5 was observed to be IgG2a. All 14 mAbs
were observed to contain κ light chains.
 | Table IIIsotype determination of mouse
anti-human programmed cell death-1 mAb. |
Table II
Isotype determination of mouse
anti-human programmed cell death-1 mAb.
| Subtype |
mAb clone
|
|---|
| IC4 | 1H8 | 2C4 | 2H7 | 3E5 | 5B2 | 5H7 | 7C9 | 7E5 | 7G12 | 9A5 | 9B4 | 9E11 | B1C4 |
|---|
| IgG1 | 2.91 | 2.85 | 2.49 | 1.82 | 2.56 | 1.96 | 2.23 | 2.89 | 2.08 | 2.15 | 0.08 | 2.02 | 2.02 | 2.45 |
| IgG2a | 0.99 | 0.47 | 0.21 | 0.13 | 0.14 | 0.31 | 0.18 | 0.23 | 0.11 | 0.16 | 1.49 | 0.21 | 0.20 | 0.22 |
| IgG2b | 0.82 | 0.15 | 0.08 | 0.08 | 0.04 | 0.20 | 0.06 | 0.17 | 0.05 | 0.05 | 0.08 | 0.08 | 0.06 | 0.09 |
| IgG3 | 0.62 | 0.13 | 0.05 | 0.12 | 0.12 | 0.19 | 0.05 | 0.15 | 0.04 | 0.04 | 0.04 | 0.06 | 0.05 | 0.05 |
| IgM | 0.12 | 0.20 | 0.11 | 0.17 | 0.06 | 0.27 | 0.06 | 0.17 | 0.05 | 0.11 | 0.05 | 0.06 | 0.14 | 0.11 |
| IgA | 0.05 | 0.09 | 0.06 | 0.16 | 0.06 | 0.21 | 0.04 | 0.05 | 0.04 | 0.04 | 0.05 | 0.04 | 0.05 | 0.05 |
| κ | 2.56 | 2.77 | 2.02 | 1.57 | 1.86 | 1.82 | 1.84 | 2.62 | 1.46 | 1.71 | 0.97 | 1.95 | 1.90 | 2.00 |
| λ | 0.09 | 0.13 | 0.07 | 0.09 | 0.06 | 0.19 | 0.11 | 0.08 | 0.05 | 0.05 | 0.07 | 0.01 | 0.05 | 0.07 |
Specificity of PD-1 mAbs for antigen
recognition as determined by western blot analysis
The 14 mAbs were used as primary antibodies in
western blot analysis to detect PD-1 protein. The molecular weight
of recombinant human PD-1/PDCD1 protein is 40 kDa. As shown in
Fig. 1, the 2C4, 5B2, 5H7, 7E5,
7G12, 9A5, 9B4, 9E11 and B1C4 mAbs demonstrated a high specificity
for PD-1, indicating that these antibodies may be used as detection
antibodies in western blotting. By contrast, a weak reaction was
observed for 1C4 and 2H7 mAbs, and no reaction was observed for the
7C9, 1H8 and 3E5 mAbs. This indicates that these five mAbs are
unsuitable for the detection of PD-1 by western blot analysis.
However, it remains unclear whether they would be useful for the
additional immunostaining experiments, such as IHC analysis.
 | Figure 1Specificity of mouse anti-human PD-1
mAbs by western blot analysis. The recombinant PD-1 protein (40
kDa) was subjected to SDS-PAGE and blotted with the 1C4, 1H8, 2C4,
2H7, 3E5, 5B2, 5H7, 7C9, 7E5, 7G12, 9A5, 9B4, 9E11 and B1C4 mAb
clones. PD-1, programmed cell death-1; mAb, monoclonal
antibody. |
PD-1 mAb 9E11 exhibited the strongest
specificity for antigen recognition in HCC tissues by IHC
analysis
The 14 mouse anti-human PD-1 mAbs were used for IHC
analysis of HCC tissues as primary antibodies. As shown in Fig. 2, the 9E11 and 2H7 mAbs exhibited
strong positive staining, particularly the 9E11 clone, which was
similar to the commercial antibody UMAB199 in detecting PD-1
expression (Fig. 2B). Using the
9E11 mAb, the staining was dark, the background of tissues was
clear and there was non-specific staining. By contrast, the B1C4
mAb exhibited lighter staining when compared with the UMAB199
positive control. The remaining 11 mAbs exhibited more non-specific
staining, as demonstrated by the staining pattern observed when the
7E5 mAb was used (Fig. 2); the
antibody bound to additional non-specific proteins on tumor cell
membranes. The results indicated that these mAbs demonstrate poor
specificity for PD-1 in HCC tissues. Therefore, the 9E11 mAb, which
exhibited the strongest specificity for PD-1, was used to
investigate the clinical significance of PD-1 expression in HCC
tissues for subsequent experiments.
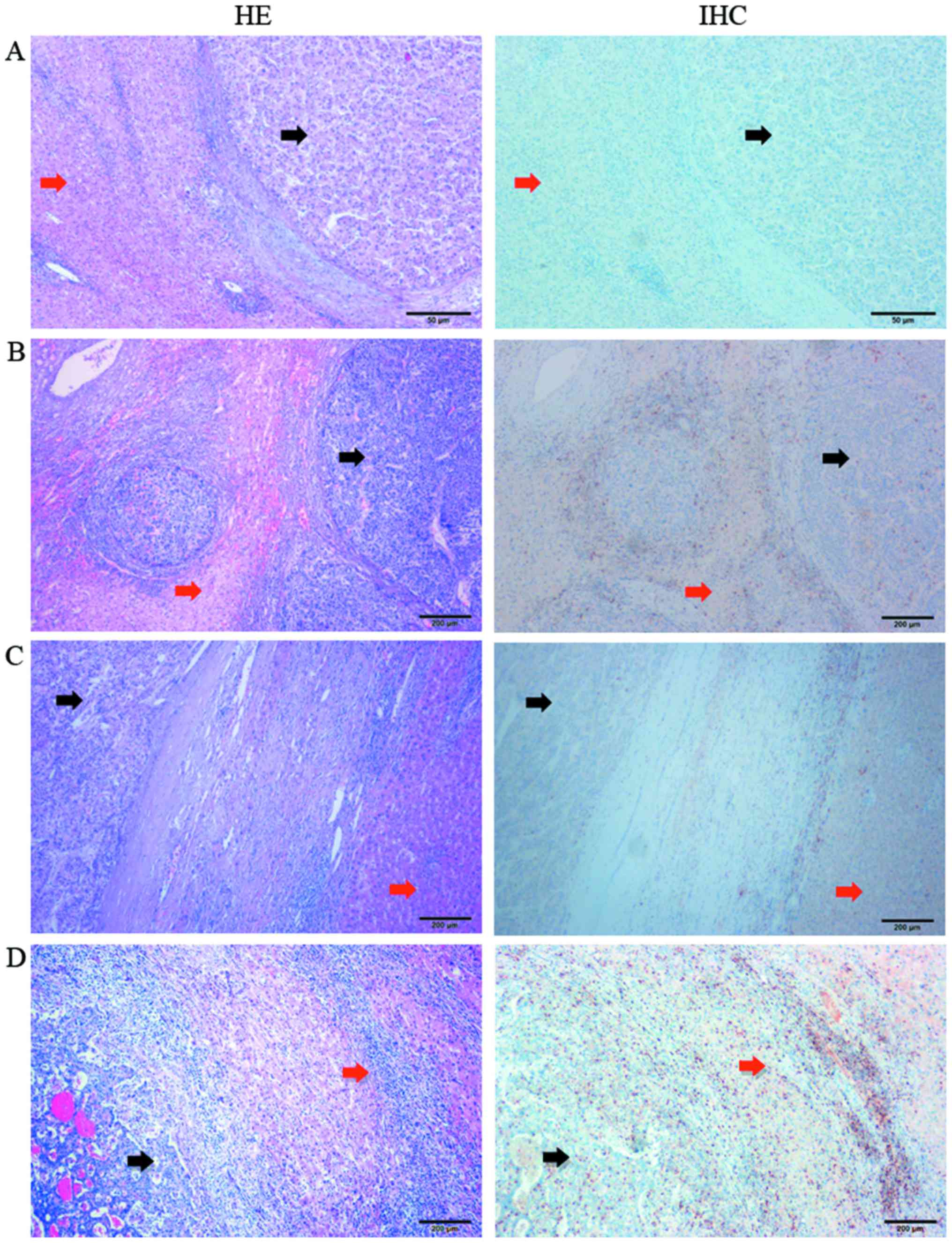
PD-1 is highly expressed in the
peritumoral tissues at the junction of tumors
A total of 77 HCC tumor specimens were examined by
IHC. The distribution of PD-1 expression in the HCC tissue samples
is presented in Figs. 3 and
4. The images in Fig. 3 display HE and IHC staining results
where the same HCC tissue sections were stained in tandem. The
tumor tissues (black arrows) and peritumoral tissues (red arrows)
were clearly distinguished by comparing the HE and IHC images of
the same HCC tissue section. A large number of T lymphocytes were
identified in the peritumoral tissues at the tumor-normal adjacent
tissue junction. The distribution of PD-1+ T lymphocytes
at different HCC tissue locations, as detected by IHC, is presented
in Fig. 4. An accumulation of a
small number of PD-1+ T lymphocytes was observed in the
nodular margin of the HCC tissue (Fig.
4A). A large number of T lymphocytes were present in the
peritumoral tissues at tumor-normal adjacent tissue junction
(Fig. 4B and C) and primarily in
the liver portal region (Fig. 4B).
In addition, due to the low degree of T lymphocyte infiltration in
the tumor interior, fewer PD-1+ T lymphocytes were
observed in this region (Fig. 4D).
Therefore, peritumoral tissues at the tumor-normal adjacent tissue
junction were selected to analyze the correlation between PD-1
expression in HCC and the clinical and pathological characteristics
of patients.
PD-1 expression level in HCC tissues is
closely associated with tumor size and the degree of
differentiation
Under a double-blind setting, the results of IHC
analysis for the 77 HCC cases (Table
III) were evaluated by two pathologists according to the
staining intensity of PD-1 combined with the ratio of PD-1-positive
cells. Using these results, the correlation between PD-1 expression
in the HCC tissues and the clinical and pathological
characteristics of patients were statistically evaluated. As
demonstrated in Table IV, PD-1
expression in HCC tissues was significantly associated with tumor
size, venous thrombosis and the degree of tumor differentiation.
The rate of positive PD-1 expression in HCC cases with a tumor size
≤5 cm was higher than that in tumors >5 cm in size (P<0.01).
The proportion of HCC tissue samples derived from patients with
venous thrombosis that were positive for PD-1 expression was higher
than in the proportion of patients positive for PD-1 expression
without venous thrombosis (P<0.05). In addition, the positive
rate of PD-1 in poorly differentiated (highly malignant) HCC was
significantly higher than in moderately and highly differentiated
HCC (P<0.01). The expression of PD-1 in HCC tissues was not
correlated with patient sex, median age, hepatic cirrhosis,
hepatitis B infection, TNM stage or tumor location (Table IV).
 | Table IIIClinical data of 77 patients with
hepatocellular carcinoma. |
Table III
Clinical data of 77 patients with
hepatocellular carcinoma.
| No. | Sex | Age (years) | Degree of
differentiation | Hepatic
cirrhosis | Hepatitis B | Tumor size >5
cm | Exact tumor
dimensions (cm) | Tumor location | Venous
thrombosis | PD-1 | Positive
lymphocytes (×200) | TNM stage |
|---|
| 1 | Male | 57 | Low | Yes | No | Yes | 8.0×6.0×6.0 | Left | No | + | 41 | III |
| 2 | Female | 49 | Middle | No | Yes | Yes | 9.0×8.0×7.0 | Right | No | − | 12 | IV |
| 3 | Male | 71 | Low | Yes | Yes | No | 3.0×3.0×3.0 | Right | Yes | ++ | 112 | III |
| 4 | Male | 56 | Low | Yes | Yes | Yes | 10.0×7.0×5.0 | Right | Yes | + | 49 | III |
| 5 | Male | 37 | Low | No | Yes | No | 2.5×2.5×2.5 | Left | No | + | 33 | I |
| 6 | Male | 41 | Middle | Yes | Yes | No | 2.5×2.0×2.0 | Right | No | ++ | 37 | I |
| 7 | Male | 59 | High | Yes | Yes | No | 3.0×2.5×2.0 | Left | No | − |
0 | I |
| 8 | Male | 47 | Middle | No | No | No | 4.0×4.0×4.0 | Right | No | + | 25 | I |
| 9 | Male | 60 | Middle | No | Yes | No | 4.0×3.0×3.0 | Right | No | +++ | 135 | I |
| 10 | Male | 50 | Middle | No | No | No | 3.5×3.5×3.0 | Right | No | + | 37 | I |
| 11 | Male | 59 | Middle | No | No | Yes | 11.0×8.0×8.0 | Right | No | − |
0 | I |
| 12 | Male | 42 | Middle | No | No | No | 1.5×1.5×1.5 | Right | No | − |
7 | I |
| 13 | Male | 57 | Middle | Yes | No | Yes | 6.5×5.5×3.5 | Right | No | ++ | 72 | IV |
| 14 | Female | 62 | Low | Yes | No | Yes | 6.0×6.0×5.0 | Right | No | ++ | 83 | I |
| 15 | Male | 36 | Middle | Yes | Yes | No | 3.0×3.0×2.0 | Right | No | + | 19 | II |
| 16 | Male | 41 | Middle | Yes | Yes | No | 4.0×4.0×3.0 | Right | Yes | + | 28 | III |
| 17 | Male | 46 | Middle | Yes | No | Yes | 9.0×8.0×8.0 | Right | No | − | 10 | I |
| 18 | Male | 49 | Middle | Yes | No | No | 1.8×1.5×1.0 | Right | No | + | 31 | I |
| 19 | Male | 63 | Middle | Yes | No | No | 5.0×3.5×3.5 | Left | Yes | + | 18 | III |
| 20 | Male | 51 | Middle | No | No | Yes | 5.5×5.0×4.5 | Right | No | − |
5 | I |
| 21 | Female | 64 | Middle | Yes | No | Yes | 6.0×5.0×4.0 | Right | Yes | + | 23 | III |
| 22 | Female | 61 | Middle | No | No | Yes | 7.5×7.0×7.0 | Left | No | − |
0 | I |
| 23 | Male | 60 | Middle | Yes | No | Yes | 6.0×5.5×5.0 | Right | Yes | + | 61 | III |
| 24 | Male | 69 | Low | No | No | Yes | 12.5×8.0×8.0 | Left | No | + | 46 | I |
| 25 | Male | 63 | Middle | Yes | No | Yes | 5.5×5.0×5.0 | Right | No | − |
0 | I |
| 26 | Male | 60 | Middle | Yes | No | Yes | 6.5×5.5×4.5 | Right | No | − |
4 | II |
| 27 | Male | 51 | Low | Yes | No | No | 3.5×3.5×3.0 | Right | No | ++ | 60 | II |
| 28 | Male | 28 | Middle | No | No | Yes | 7.0×6.0×6.0 | Right | No | − |
0 | III |
| 29 | Male | 57 | Low | Yes | No | Yes | 11.0×11.0×10.0 | Right | Yes | + | 34 | III |
| 30 | Female | 58 | Low | Yes | Yes | No | 5.0×4.0×3.0 | Left | Yes | ++ | 69 | III |
| 31 | Male | 54 | Middle | No | No | No | 5.0×4.0×3.5 | Right | No | + | 22 | III |
| 32 | Male | 42 | Middle | No | Yes | No | 1.2×1.2×0.7 | Left | No | + | 23 | I |
| 33 | Female | 44 | Middle | Yes | Yes | Yes | 6.5×4.5×3.5 | Left | No | − |
8 | I |
| 34 | Female | 43 | Middle | No | No | Yes | 9.0×6.0×6.0 | Right | No | − |
0 | II |
| 35 | Male | 55 | High | Yes | No | No | 2.0×1.5×1.5 | Left | No | + | 18 | I |
| 36 | Female | 27 | Middle | No | Yes | Yes | 11.0×10.0×6.0 | Left | No | − |
0 | I |
| 37 | Male | 57 | Middle | No | Yes | Yes | 8.0×6.0×5.5 | right | No | − |
0 | I |
| 38 | Male | 50 | High | Yes | Yes | No | 3.0×3.0×2.0 | Right | No | + | 28 | I |
| 39 | Male | 52 | Middle | Yes | No | No | 3.0×2.0×2.0 | Right | No | ++ | 40 | I |
| 40 | Female | 67 | High | No | No | Yes | 1.5×1.0×1.0 | Right | No | − |
0 | III |
| 41 | Female | 58 | Middle | Yes | Yes | No | 3.0×3.0×3.0 | Left | No | + | 25 | I |
| 42 | Male | 46 | Middle | No | No | No | 5.0×4.0×4.0 | Right | Yes | + | 29 | III |
| 43 | Male | 52 | Middle | Yes | No | No | <1.0 | Right | No | + | 41 | I |
| 44 | Male | 49 | Middle | Yes | Yes | No | 3.0×2.5×2.0 | Right | No | + | 38 | I |
| 45 | Male | 61 | Middle | No | Yes | No | 3.5×3.0×2.5 | Right | No | − |
0 | I |
| 46 | Male | 59 | Low | No | No | Yes | 8.0×7.0×5.5 | Right | No | + | 18 | III |
| 47 | Male | 49 | Low | Yes | No | Yes | 9.5×8.0×8.0 | Right | Yes | − |
8 | III |
| 48 | Male | 40 | Middle | Yes | No | Yes | 6.0×5.0×5.0 | Left | No | − |
0 | I |
| 49 | Male | 27 | Low | Yes | Yes | No | 4.0×3.0×3.0 | Right | No | + | 52 | I |
| 50 | Male | 60 | Low | Yes | Yes | No | 2.2×1.2×1.0 | Right | No | − |
3 | II |
| 51 | Female | 58 | Low | Yes | No | No | 4.0×3.0×3.0 | Right | No | +++ | 129 | I |
| 52 | Male | 43 | Low | Yes | Yes | No | 3.0×3.0×2.0 | Left | No | ++ | 82 | I |
| 53 | Male | 56 | Middle | No | Yes | Yes | 12.0×12.0×12.0 | Right | No | + | 24 | III |
| 54 | Female | 64 | Middle | No | No | No | 4.2×4.0×3.5 | Right | No | + | 53 | I |
| 55 | Male | 62 | Middle | Yes | No | No | 5.0×2.5×2.5 | Right | No | ++ | 89 | IV |
| 56 | Male | 61 | Middle | Yes | No | No | 3.0×2.0×2.0 | Right | No | + | 14 | I |
| 57 | Male | 68 | High | No | No | Yes | 7.0×4.5×4.0 | Left | No | − |
0 | I |
| 58 | Male | 41 | High | No | No | Yes | 7.0×6.5×6.0 | Right | No | − |
0 | I |
| 59 | Male | 32 | Middle | No | No | No | 4.0×4.0×4.0 | Right | No | ++ | 59 | I |
| 60 | Male | 51 | Middle | Yes | Yes | No | 2.5×2.5×1.0 | Right | No | − |
5 | I |
| 61 | Male | 50 | Low | Yes | No | Yes | 11.0×10.0×7.0 | Right | No | + | 35 | IV |
| 62 | Male | 51 | Middle | No | Yes | No | 5.0×4.0×4.0 | Right | No | + | 45 | I |
| 63 | Male | 50 | Low | Yes | No | No | 4.0×4.0×2.0 | Right | No | +++ | 101 | I |
| 64 | Female | 30 | Low | Yes | Yes | No | 5.0×5.0×4.0 | Left | Yes | + | 48 | III |
| 65 | Male | 51 | Middle | No | Yes | No | 3.0×2.5×2.0 | Left | No | + | 54 | I |
| 66 | Male | 41 | Low | Yes | Yes | Yes | 9.0×8.0×5.5 | Right | Yes | ++ | 59 | III |
| 67 | Male | 58 | Middle | Yes | No | No | 5.0×4.0×4.0 | Right | No | − |
0 | I |
| 68 | Male | 59 | High | No | No | No | 5.0×5.0×4.0 | Right | No | + | 64 | I |
| 69 | Male | 68 | Middle | Yes | No | No | 4.0×3.0×2.0 | Left | No | − |
0 | I |
| 70 | Male | 37 | Middle | No | No | Yes | 7.0×7.0×6.0 | Right | No | + | 25 | I |
| 71 | Male | 62 | Middle | Yes | Yes | Yes | 6.0×5.0×4.0 | Left | No | + | 29 | III |
| 72 | Male | 41 | Middle | Yes | No | No | 4.5×4.0×4.0 | Right | No | − |
3 | I |
| 73 | Male | 42 | Middle | No | No | Yes | 7.0×7.0×7.0 | Right | No | − |
8 | IV |
| 74 | Male | 65 | Middle | Yes | No | Yes | 7.5×5.5×4.5 | Right | No | − |
6 | II |
| 75 | Male | 50 | Low | Yes | No | No | 2.5×2.0×2.0 | Right | No | ++ | 85 | II |
| 76 | Male | 41 | Low | Yes | No | No | <1.0 | Left | No | + | 21 | IV |
| 77 | Male | 79 | Middle | Yes | No | No | 3.5×3.0×3.0 | Left | No | + | 32 | I |
 | Table IVAssociation between PD-1 expression
in hepatocellular carcinoma tissues and the clinicopathological
characteristics of patients based on the staining intensity
combined with the ratio of PD-1+ lymphocytes. |
Table IV
Association between PD-1 expression
in hepatocellular carcinoma tissues and the clinicopathological
characteristics of patients based on the staining intensity
combined with the ratio of PD-1+ lymphocytes.
| Variable | PD-1 expression
|
|---|
| No. | Positive | Negative | P-value |
|---|
| Sex | | | | |
| Male | 64 | 43 | 21 | 0.358 |
| Female | 13 | 7 | 6 | |
| Age (years) | | | | |
| ≤52 | 40 | 26 | 14 | 0.990 |
| >52 | 37 | 24 | 13 | |
| Tumor size
(cm) | | | | |
| ≤5 | 44 | 36 | 8 | <0.001 |
| >5 | 33 | 14 | 19 | |
| Hepatic
cirrhosis | | | | |
| Yes | 47 | 34 | 13 | 0.088 |
| No | 30 | 16 | 14 | |
| Hepatitis B | | | | |
| Yes | 28 | 20 | 8 | 0.367 |
| No | 49 | 30 | 19 | |
| Venous
thrombosis | | | | |
| Yes | 12 | 11 | 1 | 0.035 |
| No | 65 | 39 | 26 | |
| Degree of
differentiation | | | | |
| I | 21 | 19 | 2 | 0.004 |
| II/III | 56 | 31 | 25 | |
| TNM stage | | | | |
| I | 45 | 27 | 18 | 0.181 |
| II | 6 | 3 | 3 | |
| III | 20 | 16 | 4 | |
| IV | 6 | 4 | 2 | |
| Tumor location | | | | |
| Right | 56 | 36 | 20 | 0.845 |
| Left | 21 | 14 | 7 | |
The number of PD-1 positive cells in multiple fields
of view (×200 magnification) for each tissue section was then
determined (Fig. 5). The number of
PD-1+ T lymphocytes was closely correlated with tumor
size and differentiation (P<0.01; Fig. 5A and B). PD-1 expression was
significantly increased in tumors ≤5 cm in size or in poorly
differentiated tumors, which is consistent with the aforementioned
IHC results. By contrast, no correlation between the number of
PD-1+ T lymphocytes in HCC tissues and the presence of
venous thrombosis was observed (Fig.
5C).
The results indicate that PD-1 expression in HCC
tissues may be closely correlated with tumor size and the degree of
differentiation and moderately correlated with venous thrombosis.
However, PD-1 expression does not appear to be correlated with
additional clinical characteristics, including patient sex, age,
cirrhosis, hepatitis B infection, TNM stage or tumor location.
Discussion
Tumor cells are able to escape clearance by the host
immune system through a variety of mechanisms; one of which is the
PD-1/PD-L1 immune checkpoint that serves a crucial role in this
process (37). Tumor cells
recognize PD-1 proteins, which are expressed on effector T cells,
by overexpressing PD-L1. Activation of the PD-1/PD-L1 immune
checkpoint subsequently communicates immunosuppressive signals to T
cells, leading to evasion of tumor cell clearance by the host
immune system (6–8). Therefore, inhibition of the
PD-1/PD-L1 immune checkpoint has been widely investigated as a
promising strategy for antitumor immunotherapy, in an attempt to
reverse the immunological tolerance of tumor cells in the host.
Inhibitory antibodies targeting the PD-1/PD-L1
immune checkpoint have demonstrated substantial clinical effects in
patients with metastatic melanoma, renal cell carcinoma, non-small
cell lung cancer and a number of additional tumors (6,8,9).
However, reports concerning the curative effects of these
antibodies in patients with HCC are limited. It has been generally
recognized that HCC is a life-threatening malignancy with high
mortality rates and now ranks as the second cause of
cancer-associated death worldwide. This is particularly the case in
China, where the number of HCC cases accounts for 42.5% of the
total number of global cases (38). This indicates the broad potential
application of PD-1/PD-L1 immune checkpoint inhibitors in HCC
immunotherapy (17–20). Therefore, the development of novel
anti-PD-1 mAbs may be of great significance for the
immunotherapeutic treatment and diagnosis of HCC.
In the present study, the 9E11 mAb clone, which
demonstrated the highest specificity for PD-1 in HCC tissues, was
used to investigate PD-1 expression in HCC tissues by IHC. In HCC
tissues, PD-1+ T lymphocytes were primarily located in
the peritumoral tissues at the tumor-normal adjacent tissue
junction, while relatively few PD-1+ T lymphocytes were
identified in the tumor interior. In addition, although the number
of infiltrating T lymphocytes in the tumor interior was small, the
proportion of PD-1+ T lymphocytes out of the total
number of infiltrating T lymphocytes was large and not
significantly different from that in the peritumoral tissues. The
characteristics of PD-1 expression and distribution in the HCC
tissues were similar to those reported in the literature (39–41).
Shen et al (42) reported
that the proportion of PD-1+ CD3+ T
lymphocytes in HCC tumors was significantly higher when compared
with adjacent tissues. An additional previous study demonstrated
that the expression level of PD-1 on CD8+ tumor
infiltrating lymphocytes was significantly higher when compared
with non-tumor infiltrating lymphocytes (43).
In the present study, two methods were employed to
evaluate and analyze the results of IHC analysis. In a previous
report, Chang et al (44)
demonstrated that high PD-1 expression was significantly correlated
with several adverse clinicopathologic features including high TNM
stage, presence of vascular tumor emboli, and high pre-operative
serum α-fetoprotein levels, but not correlated with tumor size. The
results of the present study demonstrated that the expression of
PD-1 in HCC tissues was significantly correlated with tumor size
and the degree of differentiation, moderately correlated with
venous thrombosis, and not correlated with clinical
characteristics, including sex, age, cirrhosis, hepatitis B
infection, TNM stage or tumor location. Hepatitis B and C viruses
are major causes of HCC, although the underlying pathophysiological
mechanisms are unclear (45).
Notably, a previous study reported that the PD-1/PD-L1 signaling
pathway is associated with cytotoxic CD8+ T-cell
responses in virus-infected hosts, with reduced PD-1 expression
observed following treatment-induced suppression of HBV replication
in vivo (46). By contrast,
the present study did not observe an association between PD-1
expression and hepatitis B viral infection. These inconsistent
results may be due to the use of different sample sources, as well
as differences between epitopes and the structures of the
antibodies used.
There were several limitations of the present study.
Morphologically, HCC is highly heterogeneous, and therefore, small
tumor tissue samples are unlikely to represent an entire tumor.
Further research involving a large number of randomized samples may
enable researchers to investigate the practical application of
using PD-1 mAbs in the diagnosis and treatment of HCC. In addition,
the present study was unable to analyze the correlation between
PD-1 expression and patient prognosis, due to the short follow up
period. Furthermore, in addition to the biological characteristics
of tumors, a number of additional factors are known to affect
patient prognosis, such as liver function (47,48).
At present, the association between PD-1 expression and the
prognosis of HCC remains unclear; however, a number of studies have
demonstrated no significant correlation between PD-1 expression and
the postoperative survival rate of patients (48,49).
By contrast, Hersey et al (50) reported that the expression level of
PD-1 on CD8+ T lymphocytes in the peripheral blood of
patients with primary HCC was significantly higher than that
observed in the healthy subjects, chronic hepatitis B patients and
cirrhosis patients, suggesting that the expression of PD-1 on
CD8+ T lymphocytes was associated with primary liver
cancer progression. In a study involving 65 patients with HCC,
Gabrielson et al (51)
demonstrated that the relapse rate of patients with tumor tissues
containing a high density of CD3+ T and CD8+
T cells was lower (P=0.007) and exhibited longer recurrence-free
survival rates (P=0.002) when compared with the group with a low
number of infiltrating CD3+ T and CD8+ T
cells. The present study did not assess the correlation between
PD-1 expression and patient prognosis. However, the authors will
monitor the outcomes of HCC patients recruited to the current
study, and combine these observations with PD-1 expression in HCC
tissues in order to examine the association between PD-1 expression
and prognosis in a future study.
Previous studies have demonstrated that the
proliferation and antitumor activities of T lymphocytes are
inhibited when they express PD-1 (52), indicating that tumor-infiltrating T
lymphocytes will undergo the whole process of cell activation and
activity suppression until cell apoptosis (53). Therefore, PD-1 expression levels in
tumor tissues may switch from low to high, and then decline
according to alterations in T lymphocyte activity. This may explain
why PD-1 is present in poorly differentiated tumors, as well as in
well-differentiated tumors (52,53).
Nevertheless, the present study demonstrated that PD-1 expression
was significantly associated with the degree of tumor
differentiation.
In conclusion, this study investigated PD-1
expression in HCC tissues using a novel anti-PD-1 mAb (9E11) as an
alternative to commercially available antibodies (44,54).
The results indicated that high-level PD-1 expression may be an
important factor associated with the immune checkpoint pathway in
liver cancer, and that it may be a potential predictor of
therapeutic response in a clinical setting. This will enable
evaluation of the applicability of using a PD-1 inhibitor for the
treatment of patients with HCC. Notably, the results indicated that
patients with poorly differentiated tumors might benefit from
anti-PD-1 mAb-based immunotherapy. Further research, with a large
number of randomized samples to validate practical application is
required. In order to identify a functional monoclonal antibody
that inhibits HCC growth, future studies will continue to
investigate the inhibitory effect of the prepared PD-1 mAbs on
tumor cells and explore their antitumor mechanisms.
Acknowledgments
The authors gratefully acknowledge Yes Biotech
Laboratories Ltd. (Mississauga, ON, L5S 1V6, Canada) for their
technical assistance.
Funding
This project was supported by the Chongqing Program
for Application and Development (grant no. cstc2014yykfA110022) and
the Scientific and Technological Achievements Transformation Fund
of the Third Military Medical University (grant no. 2015XZH19). The
authors gratefully acknowledge the financial support received from
the Scientific Research Project supported by Medical Health Charity
Foundation of Beijing (grant no. YWJKJJHKYJJ-B16405 and
YWJKJJHKYJJ-TLG17102).
Availability of data and materials
The data sets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors’ contributions
ZL, BL and JC were responsible for the study design,
original article drafting and editing, data acquisition and data
analysis. ZL and BL were major experiment operators and
contributors in writing the manuscript. DP, HX and PL gave advice
on the experiments and writing of the manuscript. GW was
responsible for immunohistochemical evaluations and data analysis.
JW revised the manuscript and determined the isotype and titers of
the monoclonal antibodies. GY provided technical assistance for the
preparation of PD-1 mAbs. All authors read and provided final
approval for the submission.
Ethics approval and consent to
participate
The use of human tissues was approved by the Ethics
Committee of Daping Hospital and Research Institute of Surgery,
Third Military Medical University, and informed consent for
participation in the study or use of their tissues was obtained
from all participants. Procedures involving animals and their care
were conducted in Yes Biotech Laboratories registered animal
facility (License Number 0107-01) under the Animals for Research
Act at the supervision of Ontario Ministry of Agriculture, Food and
Rural Affair, Canada. The procedures and pain level assessment were
reviewed and approved by Yes Biotech Laboratories Animal Care
Committee and complied with the Animals for Research Act.
Consent for publication
Publication of the clinical datasets in this study
does not compromise anonymity or confidentiality or breach local
data protection laws.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Benson DM Jr, Bakan CE, Mishra A,
Hofmeister CC, Efebera Y, Becknell B, Baiocchi RA, Zhang J, Yu J,
Smith MK, et al: The PD-1/PD-L1 axis modulates the natural killer
cell versus multiple myeloma effect: A therapeutic target for
CT-011, a novel monoclonal anti-PD-1 antibody. Blood.
116:2286–2294. 2010. View Article : Google Scholar
|
|
2
|
Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ,
Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, et al:
Safety and activity of anti-PD-L1 antibody in patients with
advanced cancer. N Engl J Med. 366:2455–2465. 2012. View Article : Google Scholar
|
|
3
|
Tykodi SS, Brahmer JR, Hwu WJ, Chow LQ,
Topalian SL, Hwu P, Odunsi K, Camacho LH, Kauh JS, Pitot HC, et al:
PD-1/PD-L1 pathway as a target for cancer immunotherapy: Safety and
clinical activity of BMS-936559, an anti-PD-L1 antibody, in
patients with solid tumors. J Clin Oncol. 30:25102012.
|
|
4
|
Chen DS, Irving BA and Hodi FS: Molecular
pathways: Next-generation immunotherapy - inhibiting programmed
death-ligand 1 and programmed death-1. Clin Cancer Res.
18:6580–6587. 2012. View Article : Google Scholar
|
|
5
|
Horn L, Herbst RS, Spigel D, Gettinger SN,
Gordon MS, Hollebecque and Kowanetz M: An analysis of the
relationship of clinical activity to baseline EGFR status, PD-L1
expression and prior treatment history in patients with non-small
cell lung cancer (NSCLC) following PD-L1 blockade with MPDL3280A
(anti-PDL1). J Thorac Oncol. 8:S3642013.
|
|
6
|
Powles T, Eder JP, Fine GD, Braiteh FS,
Loriot Y, Cruz C, Bellmunt J, Burris HA, Petrylak DP, Teng SL, et
al: MPDL3280A (anti-PD-L1) treatment leads to clinical activity in
metastatic bladder cancer. Nature. 515:558–562. 2014. View Article : Google Scholar
|
|
7
|
Creelan BC: Update on immune checkpoint
inhibitors in lung cancer. Cancer Contr. 21:80–89. 2014. View Article : Google Scholar
|
|
8
|
Stewart R, Morrow M, Hammond SA, Mulgrew
K, Marcus D, Poon E, Watkins A, Mullins S, Chodorge M, Andrews J,
et al: Identification and characterization of MEDI4736, an
antagonistic anti-PD-L1 monoclonal antibody. Cancer Immunol Res.
3:1052–1062. 2015. View Article : Google Scholar
|
|
9
|
Massard C, Gordon MS, Sharma S, Rafii S,
Wainberg ZA, Luke J, Curiel TJ, Colon-Otero G, Hamid O, Sanborn RE,
et al: Safety and efficacy of durvalumab (MEDI4736), an
anti-programmed cell death ligand-1 immune checkpoint inhibitor, in
patients with advanced urothelial bladder cancer. J Clin Oncol.
34:3119–3125. 2016. View Article : Google Scholar
|
|
10
|
West EE, Jin HT, Rasheed AU,
Penaloza-Macmaster P, Ha SJ, Tan WG, Youngblood B, Freeman GJ,
Smith KA and Ahmed R: PD-L1 blockade synergizes with IL-2 therapy
in reinvigorating exhausted T cells. J Clin Invest. 123:2604–2615.
2013. View
Article : Google Scholar
|
|
11
|
Strome SE, Dong H, Tamura H, Voss SG,
Flies DB, Tamada K, Salomao D, Cheville J, Hirano F, Lin W, et al:
B7-H1 blockade augments adoptive T-cell immunotherapy for squamous
cell carcinoma. Cancer Res. 63:6501–6505. 2003.
|
|
12
|
Hamanishi J, Mandai M, Ikeda T, Minami M,
Kawaguchi A, Murayama T, Kanai M, Mori Y, Matsumoto S, Chikuma S,
et al: Efficacy and safety of anti-PD-1 antibody (nivolumab:
BMS-936558, ONO-4538) in patients with platinum-resistant ovarian
cancer. J Clin Oncol. 32:55112014.
|
|
13
|
Hodi FS, Sznol M, Kluger HM, Mcdermott DF,
Carvajal RD, Lawrence DP, Topalian SL, Atkins MB, Powderly JD,
Sharfman WH, et al: Long-term survival of ipilimumab-naive patients
(pts) with advanced melanoma (mel) treated with nivolumab
(anti-pd-1, bms-936558, ono-4538) in a phase I trial. J Clin Oncol.
25:374–393. 2014.
|
|
14
|
Dong H, Strome SE, Salomao DR, Tamura H,
Hirano F, Flies DB, Roche PC, Lu J, Zhu G, Tamada K, et al:
Tumor-associated B7-H1 promotes T-cell apoptosis: A potential
mechanism of immune evasion. Nat Med. 8:793–800. 2002. View Article : Google Scholar
|
|
15
|
Woo SR, Turnis ME, Goldberg MV, Bankoti J,
Selby M, Nirschl CJ, Bettini ML, Gravano DM, Vogel P, Liu CL, et
al: Immune inhibitory molecules LAG-3 and PD-1 synergistically
regulate T-cell function to promote tumoral immune escape. Cancer
Res. 72:917–927. 2012. View Article : Google Scholar
|
|
16
|
Mangsbo SM, Sandin LC, Anger K, Korman AJ,
Loskog A and Tötterman TH: Enhanced tumor eradication by combining
CTLA-4 or PD-1 blockade with CpG therapy. J Immunother. 33:225–235.
2010. View Article : Google Scholar
|
|
17
|
Steidl C, Shah SP, Woolcock BW, Rui L,
Kawahara M, Farinha P, Johnson NA, Zhao Y, Telenius A, Neriah SB,
et al: MHC class II transactivator CIITA is a recurrent gene fusion
partner in lymphoid cancers. Nature. 471:377–381. 2011. View Article : Google Scholar
|
|
18
|
Francisco LM, Salinas VH, Brown KE,
Vanguri VK, Freeman GJ, Kuchroo VK and Sharpe AH: PD-L1 regulates
the development, maintenance, and function of induced regulatory T
cells. J Exp Med. 206:3015–3029. 2009. View Article : Google Scholar
|
|
19
|
Inman BA, Sebo TJ, Frigola X, Dong H,
Bergstralh EJ, Frank I, Fradet Y, Lacombe L and Kwon ED: PD-L1
(B7-H1) expression by urothelial carcinoma of the bladder and
BCG-induced granulomata: Associations with localized stage
progression. Cancer. 109:1499–1505. 2007. View Article : Google Scholar
|
|
20
|
Ahmadzadeh M, Johnson LA, Heemskerk B,
Wunderlich JR, Dudley ME, White DE and Rosenberg SA: Tumor
antigen-specific CD8 T cells infiltrating the tumor express high
levels of PD-1 and are functionally impaired. Blood. 114:1537–1544.
2009. View Article : Google Scholar
|
|
21
|
Hirano F, Kaneko K, Tamura H, Dong H, Wang
S, Ichikawa M, Rietz C, Flies DB, Lau JS, Zhu G, et al: Blockade of
B7-H1 and PD-1 by monoclonal antibodies potentiates cancer
therapeutic immunity. Cancer Res. 65:1089–1096. 2005.
|
|
22
|
Okudaira K, Hokari R, Tsuzuki Y, Okada Y,
Komoto S, Watanabe C, Kurihara C, Kawaguchi A, Nagao S, Azuma M, et
al: Blockade of B7-H1 or B7-DC induces an anti-tumor effect in a
mouse pancreatic cancer model. Int J Oncol. 35:741–749. 2009.
|
|
23
|
Wong RM, Scotland RR, Lau RL, Wang C,
Korman AJ, Kast WM and Weber JS: Programmed death-1 blockade
enhances expansion and functional capacity of human melanoma
antigen-specific CTLs. Int Immunol. 19:1223–1234. 2007. View Article : Google Scholar
|
|
24
|
Curiel TJ, Wei S, Dong H, Alvarez X, Cheng
P, Mottram P, Krzysiek R, Knutson KL, Daniel B, Zimmermann MC, et
al: Blockade of B7-H1 improves myeloid dendritic cell-mediated
antitumor immunity. Nat Med. 9:562–567. 2003. View Article : Google Scholar
|
|
25
|
Zhang Y, Huang S, Gong D, Qin Y and Shen
Q: Programmed death-1 upregulation is correlated with dysfunction
of tumor-infiltrating CD8+ T lymphocytes in human
non-small cell lung cancer. Cell Mol Immunol. 7:389–395. 2010.
View Article : Google Scholar
|
|
26
|
Rupa P, Nakamura S, Katayama S and Mine Y:
Attenuation of allergic immune response phenotype by mannosylated
egg white in orally induced allergy in BALB/c mice. J Agric Food
Chem. 62:9479–9487. 2014. View Article : Google Scholar
|
|
27
|
Boyoglu-Barnum S, Chirkova T, Todd SO,
Barnum TR, Gaston KA, Jorquera P, Haynes LM, Tripp RA, Moore ML and
Anderson LJ: Prophylaxis with a respiratory syncytial virus (RSV)
anti-G protein monoclonal antibody shifts the adaptive immune
response to RSV rA2-line19F infection from Th2 to Th1 in BALB/c
mice. J Virol. 88:10569–10583. 2014. View Article : Google Scholar
|
|
28
|
Pali-Schöll I, Szöllösi H, Starkl P,
Scheicher B, Stremnitzer C, Hofmeister A, Roth-Walter F, Lukschal
A, Diesner SC, Zimmer A, et al: Protamine nanoparticles with
CpG-oligodeoxynucleotide prevent an allergen-induced Th2-response
in BALB/c mice. Eur J Pharm Biopharm. 85(3 Pt A): 656–664. 2013.
View Article : Google Scholar
|
|
29
|
Webster WS, Thompson RH, Harris KJ,
Frigola X, Kuntz S, Inman BA and Dong H: Targeting molecular and
cellular inhibitory mechanisms for improvement of antitumor memory
responses reactivated by tumor cell vaccine. J Immunol.
179:2860–2869. 2007. View Article : Google Scholar
|
|
30
|
Zhou Q, Xiao H, Liu Y, Peng Y, Hong Y,
Yagita H, Chandler P, Munn DH, Mellor A, Fu N, et al: Blockade of
programmed death-1 pathway rescues the effector function of
tumor-infiltrating T cells and enhances the antitumor efficacy of
lentivector immunization. J Immunol. 185:5082–5092. 2010.
View Article : Google Scholar
|
|
31
|
Marusich MF: Efficient hybridoma
production using previously frozen splenocytes. J Immunol Methods.
114:155–159. 1988. View Article : Google Scholar
|
|
32
|
Campbell AM: Monoclonal Antibody
Technology. Elsevier Science Publishers; Amsterdam: pp. 2641984
|
|
33
|
Laemmli UK: Cleavage of structural
proteins during the assembly of the head of bacteriophage T4.
Nature. 227:680–685. 1970. View Article : Google Scholar
|
|
34
|
Detre S, Saclani Jotti G and Dowsett M: A
‘quickscore’ method for immunohistochemical semiquantitation:
Validation for oestrogen receptor in breast carcinomas. J Clin
Pathol. 48:876–878. 1995. View Article : Google Scholar
|
|
35
|
Wang BJ, Bao JJ, Wang JZ, Wang Y, Jiang M,
Xing MY, Zhang WG, Qi JY, Roggendorf M, Lu MJ, et al:
Immunostaining of PD-1/PD-Ls in liver tissues of patients with
hepatitis and hepatocellular carcinoma. World J Gastroenterol.
17:3322–3329. 2011. View Article : Google Scholar
|
|
36
|
Shi F, Shi M, Zeng Z, Qi RZ, Liu ZW, Zhang
JY, Yang YP, Tien P and Wang FS: PD-1 and PD-L1 upregulation
promotes CD8(+) T-cell apoptosis and postoperative recurrence in
hepatocellular carcinoma patients. Int J Cancer. 128:887–896. 2011.
View Article : Google Scholar
|
|
37
|
Keir ME, Butte MJ, Freeman GJ and Sharpe
AH: PD-1 and its ligands in tolerance and immunity. Annu Rev
Immunol. 26:677–704. 2008. View Article : Google Scholar
|
|
38
|
Yuan F, Zhang LS, Li HY, Liao M, Lv M and
Zhang C: Influence of angiotensin I-converting enzyme gene
polymorphism on hepatocellular carcinoma risk in China. DNA Cell
Biol. 32:268–273. 2013. View Article : Google Scholar
|
|
39
|
Patel SP and Kurzrock R: PD-L1 Expression
as a predictive biomarker in cancer immunotherapy. Mol Cancer Ther.
14:847–856. 2015. View Article : Google Scholar
|
|
40
|
Robert C, Ribas A, Wolchok JD, Hodi FS,
Hamid O, Kefford R, Weber JS, Joshua AM, Hwu WJ, Gangadhar TC, et
al: Anti-programmed-death-receptor-1 treatment with pembrolizumab
in ipilimumab-refractory advanced melanoma: A randomised
dose-comparison cohort of a phase 1 trial. Lancet. 384:1109–1117.
2014. View Article : Google Scholar
|
|
41
|
Meng X, Huang Z, Teng F, Xing L and Yu J:
Predictive biomarkers in PD-1/PD-L1 checkpoint blockade
immunotherapy. Cancer Treat Rev. 41:868–876. 2015. View Article : Google Scholar
|
|
42
|
Shen MQ, Sun CY and Liu ZJ: Expression and
clinical significance of B7-H1 and PD-1 in primary hepatocellular
carcinoma tissues. WJCD. 16:3110–3113. 2008.
|
|
43
|
Zeng Z, Shi F and Zhang M: Significance of
PD-1 expression on CD8+ T lymphocytes from patients with
hepatocellular carcinoma. Infect Dis Info. 22:83–85. 2009.
|
|
44
|
Chang H, Jung W, Kim A, Kim HK, Kim WB,
Kim JH and Kim BH: Expression and prognostic significance of
programmed death protein 1 and programmed death ligand-1, and
cytotoxic T lymphocyte-associated molecule-4 in hepatocellular
carcinoma. APMIS. 125:690–698. 2017. View Article : Google Scholar
|
|
45
|
Di Bisceglie AM: Hepatitis B and
hepatocellular carcinoma. Hepatology. 49(Suppl): S56–S60. 2009.
View Article : Google Scholar
|
|
46
|
Evans A, Riva A, Cooksley H, Phillips S,
Puranik S, Nathwani A, Brett S, Chokshi S and Naoumov NV:
Programmed death 1 expression during antiviral treatment of chronic
hepatitis B: Impact of hepatitis B e-antigen seroconversion.
Hepatology. 48:759–769. 2008. View Article : Google Scholar
|
|
47
|
Joseph RW, Cappel M, Goedjen B, Gordon M,
Kirsch B, Gilstrap C, Bagaria S and Jambusaria-Pahlajani A:
Lichenoid dermatitis in three patients with metastatic melanoma
treated with anti-PD-1 therapy. Cancer Immunol Res. 3:18–22. 2015.
View Article : Google Scholar
|
|
48
|
Hamid O, Robert C, Daud A, Hodi FS, Hwu
WJ, Kefford R, Wolchok JD, Hersey P, Joseph RW, Weber JS, et al:
Safety and tumor responses with lambrolizumab (anti-PD-1) in
melanoma. N Engl J Med. 369:134–144. 2013. View Article : Google Scholar
|
|
49
|
Eto S, Yoshikawa K, Nishi M, Higashijima
J, Tokunaga T, Nakao T, Kashihara H, Takasu C, Iwata T and Shimada
M: Programmed cell death protein 1 expression is an independent
prognostic factor in gastric cancer after curative resection.
Gastric Cancer. 19:466–471. 2016. View Article : Google Scholar
|
|
50
|
Hersey P, Ribas A, Hodi FS, Kefford R,
Hamid O, Daud A, Wolchok JD, Hwu WJ, Gangadhar TC, Patnaik A, et
al: Efficacy and safety of the anti-PD-1 monoclonal antibody
MK-3475 in 411 patients (pts) with melanoma. Asia Pac J Clin Oncol.
10:48–49. 2014.
|
|
51
|
Gabrielson A, Wu Y, Kallakury B, Jiang J,
Wang H, Johnson LB, Island E, Fishbein T, Satoskar R, Jha R, et al:
A high density of tumor infiltrating CD3 and CD8 cells to predict
recurrence free survival in patient with hepatocellular carcinoma.
J Clin Oncol. 33(Suppl 3): 2802015. View Article : Google Scholar
|
|
52
|
Curran MA, Montalvo W, Yagita H and
Allison JP: PD-1 and CTLA-4 combination blockade expands
infiltrating T cells and reduces regulatory T and myeloid cells
within B16 melanoma tumors. Proc Natl Acad Sci USA. 107:4275–4280.
2010. View Article : Google Scholar
|
|
53
|
Keir ME, Liang SC, Guleria I, Latchman YE,
Qipo A, Albacker LA, Koulmanda M, Freeman GJ, Sayegh MH and Sharpe
AH: Tissue expression of PD-L1 mediates peripheral T cell
tolerance. J Exp Med. 203:883–895. 2006. View Article : Google Scholar
|
|
54
|
Zeng Z, Shi F, Zhou L, Zhang MN, Chen Y,
Chang XJ, Lu YY, Bai WL, Qu JH, Wang CP, et al: Upregulation of
circulating PD-L1/PD-1 is associated with poor post-cryoablation
prognosis in patients with HBV-related hepatocellular carcinoma.
PLoS One. 6:e236212011. View Article : Google Scholar
|