|
1
|
Arnold M, Sierra MS, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global patterns and trends in
colorectal cancer incidence and mortality. Gut. 66:683–691. 2017.
View Article : Google Scholar
|
|
2
|
Ricci-Vitiani L, Lombardi DG, Pilozzi E,
Biffoni M, Todaro M, Peschle C and De Maria R: Identification and
expansion of human colon-cancer-initiating cells. Nature.
445:111–115. 2007. View Article : Google Scholar
|
|
3
|
O'Brien CA, Pollett A, Gallinger S and
Dick JE: A human colon cancer cell capable of initiating tumour
growth in immunodeficient mice. Nature. 445:106–110. 2007.
View Article : Google Scholar
|
|
4
|
Chen X, Liao R, Li D and Sun J: Induced
cancer stem cells generated by radiochemotherapy and their
therapeutic implications. Oncotarget. 8:17301–17312. 2017.
|
|
5
|
Wang SS, Jiang J, Liang XH and Tang YL:
Links between cancer stem cells and epithelial-mesenchymal
transition. Onco Targets Ther. 8:2973–2980. 2015.PubMed/NCBI
|
|
6
|
Celià-Terrassa T and Kang Y: Distinctive
properties of metastasis-initiating cells. Genes Dev. 30:892–908.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hutchinson L and Kirk R: High drug
attrition rates--where are we going wrong? Nat Rev Clin Oncol.
8:189–190. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sant S and Johnston PA: The production of
3D tumor spheroids for cancer drug discovery. Drug Discov Today
Technol. 23:27–36. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Karlsson H, Fryknäs M, Larsson R and
Nygren P: Loss of cancer drug activity in colon cancer HCT-116
cells during spheroid formation in a new 3-D spheroid cell culture
system. Exp Cell Res. 318:1577–1585. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Olejniczak A, Szaryńska M and Kmieć Z: In
vitro characterization of spheres derived from colorectal cancer
cell lines. Int J Oncol. 52:599–612. 2018.
|
|
11
|
Costa EC, Moreira AF, de Melo-Diogo D,
Gaspar VM, Carvalho MP and Correia IJ: 3D tumor spheroids: An
overview on the tools and techniques used for their analysis.
Biotechnol Adv. 34:1427–1441. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Qureshi-Baig K, Ullmann P, Rodriguez F,
Frasquilho S, Nazarov PV, Haan S and Letellier E: What do we learn
from spheroid culture systems? Insights from tumorspheres derived
from primary colon cancer tissue. PLoS One. 11:e01460522016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim SY, Hong SH, Basse PH, Wu C, Bartlett
DL, Kwon YT and Lee YJ: Cancer stem cells protect non-stem cells
from anoikis: Bystander effects. J Cell Biochem. 117:2289–2301.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Paoli P, Giannoni E and Chiarugi P:
Anoikis molecular pathways and its role in cancer progression.
Biochim Biophys Acta. 1833:3481–3498. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Islam F, Gopalan V, Smith RA and Lam AK:
Translational potential of cancer stem cells: A review of the
detection of cancer stem cells and their roles in cancer recurrence
and cancer treatment. Exp Cell Res. 335:135–147. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Siddique HR and Saleem M: Role of BMI1, a
stem cell factor, in cancer recurrence and chemoresistance:
Preclinical and clinical evidences. Stem Cells. 30:372–378. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yan KS, Chia LA, Li X, Ootani A, Su J, Lee
JY, Su N, Luo Y, Heilshorn SC, Amieva MR, et al: The intestinal
stem cell markers Bmi1 and Lgr5 identify two functionally distinct
populations. Proc Natl Acad Sci USA. 109:466–471. 2012. View Article : Google Scholar
|
|
18
|
Manhas J, Bhattacharya A, Agrawal SK,
Gupta B, Das P, Deo SV, Pal S and Sen S: Characterization of cancer
stem cells from different grades of human colorectal cancer. Tumour
Biol. 37:14069–14081. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Butler SJ, Richardson L, Farias N,
Morrison J and Coomber BL: Characterization of cancer stem cell
drug resistance in the human colorectal cancer cell lines HCT116
and SW480. Biochem Biophys Res Commun. 490:29–35. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Szaryńska M, Olejniczak A, Kobiela J,
Spychalski P and Kmieć Z: Therapeutic strategies against cancer
stem cells in human colorectal cancer. Oncol Lett. 14:7653–7668.
2017.
|
|
21
|
Chan AT, Manson JE, Feskanich D, Stampfer
MJ, Colditz GA and Fuchs CS: Long-term aspirin use and mortality in
women. Arch Intern Med. 167:562–572. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thorat MA and Cuzick J: Role of aspirin in
cancer prevention. Curr Oncol Rep. 15:533–540. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Din FV, Valanciute A, Houde VP, Zibrova D,
Green KA, Sakamoto K, Alessi DR and Dunlop MG: Aspirin inhibits
mTOR signaling, activates AMP-activated protein kinase, and induces
autophagy in colorectal cancer cells. Gastroenterology.
142:1504–1515.e1503. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kaur J and Sanyal SN: PI3-kinase/Wnt
association mediates COX-2/PGE(2) pathway to inhibit apoptosis in
early stages of colon carcinogenesis: Chemoprevention by
diclofenac. Tumour Biol. 31:623–631. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Saha S, Mukherjee S, Khan P, Kajal K,
Mazumdar M, Manna A, Mukherjee S, De S, Jana D, Sarkar DK, et al:
Aspirin suppresses the acquisition of chemoresistance in breast
cancer by disrupting an NFkappaB-IL6 signaling axis responsible for
the generation of cancer stem cells. Cancer Res. 76:2000–2012.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kastrati I, Litosh VA, Zhao S, Alvarez M,
Thatcher GR and Frasor J: A novel aspirin prodrug inhibits NFκB
activity and breast cancer stem cell properties. BMC Cancer.
15:8452015. View Article : Google Scholar
|
|
27
|
Moon CM, Kwon JH, Kim JS, Oh SH, Jin Lee
K, Park JJ, Pil Hong S, Cheon JH, Kim TI and Kim WH: Nonsteroidal
anti-inflammatory drugs suppress cancer stem cells via inhibiting
PTGS2 (cyclooxygenase 2) and NOTCH/HES1 and activating PPARG in
colorectal cancer. Int J Cancer. 134:519–529. 2014. View Article : Google Scholar
|
|
28
|
Miyamoto Y, Suyama K and Baba H: Recent
advances in targeting the EGFR signaling pathway for the treatment
of metastatic colorectal cancer. Int J Mol Sci. 18:182017.
View Article : Google Scholar
|
|
29
|
Van Emburgh BO, Sartore-Bianchi A, Di
Nicolantonio F, Siena S and Bardelli A: Acquired resistance to
EGFR-targeted therapies in colorectal cancer. Mol Oncol.
8:1084–1094. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Goel A, Chang DK, Ricciardiello L, Gasche
C and Boland CR: A novel mechanism for aspirin-mediated growth
inhibition of human colon cancer cells. Clin Cancer Res. 9:383–390.
2003.PubMed/NCBI
|
|
31
|
Wang H, Liu B, Wang J, Li J, Gong Y, Li S,
Wang C, Cui B, Xue X, Yang M, et al: Reduction of NANOG mediates
the inhibitory effect of aspirin on tumor growth and stemness in
colorectal cancer. Cell Physiol Biochem. 44:1051–1063. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mhaidat N M and Bouk lihacene M:
5-Fluorouracil-induced apoptosis in colorectal cancer cells is
caspase-9-dependent and mediated by activation of protein kinase
C-δ. Oncol Lett. 8:699–704. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Virgone-Carlotta A, Lemasson M, Mertani
HC, Diaz JJ, Monnier S, Dehoux T, Delanoë-Ayari H, Rivière C and
Rieu JP: In-depth phenotypic characterization of multicellular
tumor spheroids: Effects of 5-Fluorouracil. PLoS One.
12:e01881002017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Martin-Villalba A, Llorens-Bobadilla E and
Wollny D: CD95 in cancer: Tool or target? Trends Mol Med.
19:329–335. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Chen L, Park SM, Tumanov AV, Hau A, Sawada
K, Feig C, Turner JR, Fu YX, Romero IL, Lengyel E, et al: CD95
promotes tumour growth. Nature. 465:492–496. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
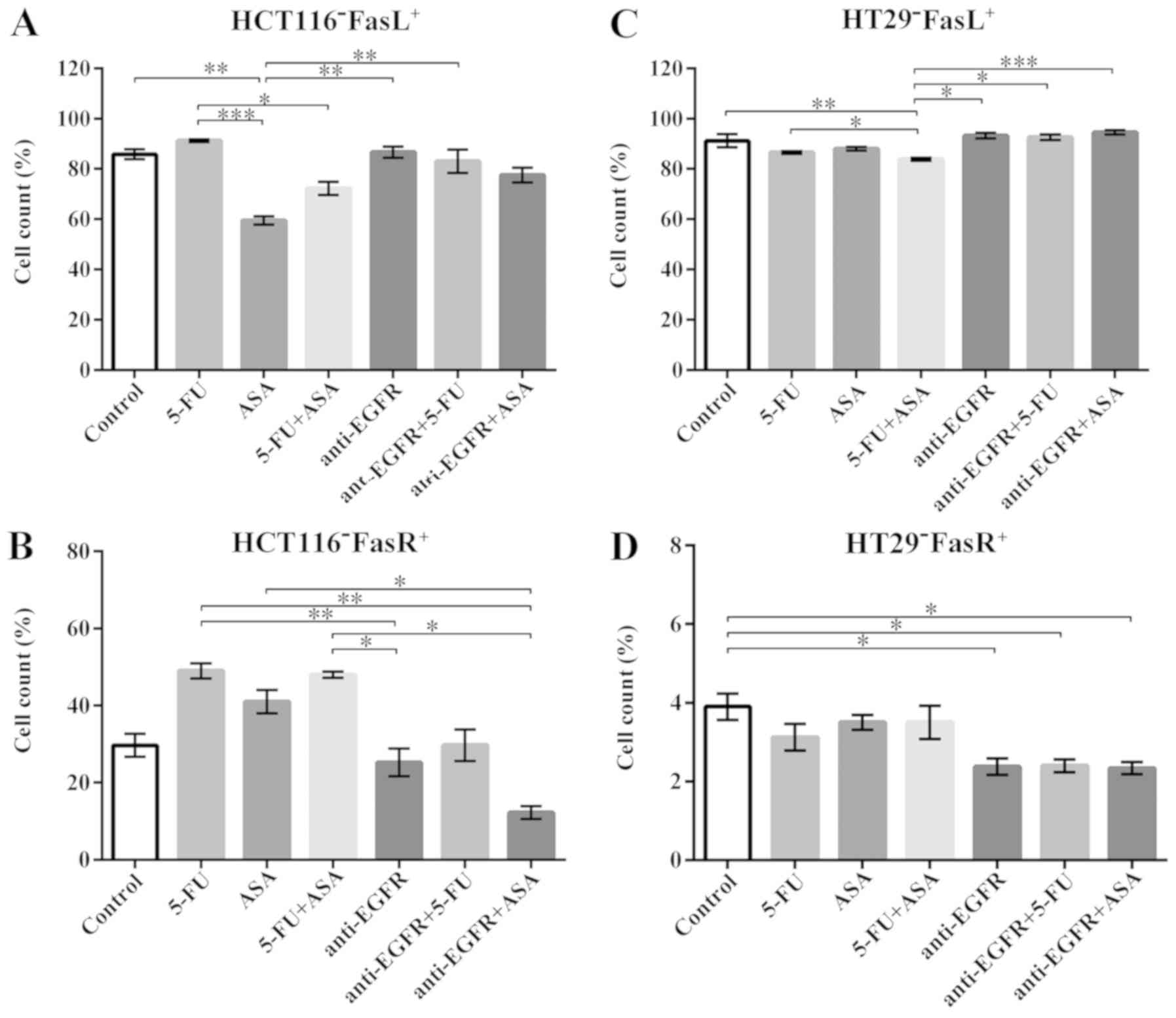
Szarynska M, Olejniczak A, Wierzbicki P,
Kobiela J, Laski D, Sledzinski Z, Adrych K, Guzek M and Kmiec Z:
FasR and FasL in colorectal cancer. Int J Oncol. 51:975–986. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ceppi P, Hadji A, Kohlhapp FJ, Pattanayak
A, Hau A, Liu X, Liu H, Murmann AE and Peter ME: CD95 and CD95L
promote and protect cancer stem cells. Nat Commun. 5:52382014.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Mancias JD and Kimmelman AC: Mechanisms of
selective autophagy in normal physiology and cancer. J Mol Biol.
428:1659–1680. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Vaiopoulos AG, Kostakis ID, Koutsilieris M
and Papavassiliou AG: Colorectal cancer stem cells. Stem Cells.
30:363–371. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Gao XL, Zhang M, Tang YL and Liang XH:
Cancer cell dormancy: Mechanisms and implications of cancer
recurrence and metastasis. OncoTargets Ther. 10:5219–5228. 2017.
View Article : Google Scholar
|
|
41
|
Takeishi S and Nakayama KI: To wake up
cancer stem cells, or to let them sleep, that is the question.
Cancer Sci. 107:875–881. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kreso A and Dick JE: Evolution of the
cancer stem cell model. Cell Stem Cell. 14:275–291. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Weiswald LB, Bellet D and Dangles-Marie V:
Spherical cancer models in tumor biology. Neoplasia. 17:1–15. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Szaryńska M, Olejniczak A, Kobiela J,
Łaski D, Śledziński Z and Kmieć Z: Cancer stem cells as targets for
DC-based immunotherapy of colorectal cancer. Sci Rep. 8:120422018.
View Article : Google Scholar
|
|
45
|
Drew DA, Cao Y and Chan AT: Aspirin and
colorectal cancer: The promise of precision chemoprevention. Nat
Rev Cancer. 16:173–186. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Valverde A, Peñarando J, Cañas A,
López-Sánchez LM, Conde F, Guil-Luna S, Hernández V, Villar C,
Morales-Estévez C, de la Haba-Rodríguez J, et al: The addition of
celecoxib improves the antitumor effect of cetuximab in colorectal
cancer: Role of EGFR-RAS-FOXM1-β- catenin signaling axis.
Oncotarget. 8:21754–21769. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Ahmed D, Eide PW, Eilertsen IA, Danielsen
SA, Eknæs M, Hektoen M, Lind GE and Lothe RA: Epigenetic and
genetic features of 24 colon cancer cell lines. Oncogenesis.
2:e712013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kleber S, Sancho-Martinez I, Wiestler B,
Beisel A, Gieffers C, Hill O, Thiemann M, Mueller W, Sykora J, Kuhn
A, et al: Yes and PI3K bind CD95 to signal invasion of
glioblastoma. Cancer Cell. 13:235–248. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Peter ME, Hadji A, Murmann AE, Brockway S,
Putzbach W, Pattanayak A and Ceppi P: The role of CD95 and CD95
ligand in cancer. Cell Death Differ. 22:885–886. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
De Roock W, Claes B, Bernasconi D, De
Schutter J, Biesmans B, Fountzilas G, Kalogeras KT, Kotoula V,
Papamichael D, Laurent-Puig P, et al: Effects of KRAS, BRAF, NRAS,
and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy
in chemotherapy-refractory metastatic colorectal cancer: A
retrospective consortium analysis. Lancet Oncol. 11:753–762. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Karapetis CS, Khambata-Ford S, Jonker DJ,
O'Callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD,
Robitaille S, et al: K-ras mutations and benefit from cetuximab in
advanced colorectal cancer. N Engl J Med. 359:1757–1765. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Gajate P, Sastre J, Bando I, Alonso T,
Cillero L, Sanz J, Caldés T and Díaz-Rubio E: Influence of KRAS
p.G13D mutation in patients with metastatic colorectal cancer
treated with cetuximab. Clin Colorectal Cancer. 11:291–296. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Misale S, Di Nicolantonio F,
Sartore-Bianchi A, Siena S and Bardelli A: Resistance to anti-EGFR
therapy in colorectal cancer: From heterogeneity to convergent
evolution. Cancer Discov. 4:1269–1280. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Allegra CJ, Jessup JM, Somerfield MR,
Hamilton SR, Hammond EH, Hayes DF, McAllister PK, Morton RF and
Schilsky RL: American Society of Clinical Oncology provisional
clinical opinion: Testing for KRAS gene mutations in patients with
metastatic colorectal carcinoma to predict response to
anti-epidermal growth factor receptor monoclonal antibody therapy.
J Clin Oncol. 27:2091–2096. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
De Roock W, Jonker DJ, Di Nicolantonio F,
Sartore-Bianchi A, Tu D, Siena S, Lamba S, Arena S, Frattini M,
Piessevaux H, et al: Association of KRAS p.G13D mutation with
outcome in patients with chemotherapy-refractory metastatic
colorectal cancer treated with cetuximab. JAMA. 304:1812–1820.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Tejpar S, Celik I, Schlichting M,
Sartorius U, Bokemeyer C and Van Cutsem E: Association of KRAS G13D
tumor mutations with outcome in patients with metastatic colorectal
cancer treated with first-line chemotherapy with or without
cetuximab. J Clin Oncol. 30:3570–3577. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Tveit KM, Guren T, Glimelius B, Pfeiffer
P, Sorbye H, Pyrhonen S, Sigurdsson F, Kure E, Ikdahl T, Skovlund
E, et al: Phase III trial of cetuximab with continuous or
intermittent fluorouracil, leucovorin, and oxaliplatin (Nordic
FLOX) versus FLOX alone in first-line treatment of metastatic
colorectal cancer: The NORDIC-VII study. J Clin Oncol.
30:1755–1762. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Guren TK, Thomsen M, Kure EH, Sorbye H,
Glimelius B, Pfeiffer P, Österlund P, Sigurdsson F, Lothe IM,
Dalsgaard AM, et al: Cetuximab in treatment of metastatic
colorectal cancer: Final survival analyses and extended RAS data
from the NORDIC-VII study. Br J Cancer. 116:1271–1278. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Maughan TS, Adams RA, Smith CG, Meade AM,
Seymour MT, Wilson RH, Idziaszczyk S, Harris R, Fisher D, Kenny SL,
et al: MRC COIN Trial Investigators: Addition of cetuximab to
oxali-platin-based first-line combination chemotherapy for
treatment of advanced colorectal cancer: Results of the randomised
phase 3 MRC COIN trial. Lancet. 377:2103–2114. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Roelofs HM, Te Morsche RH, van Heumen BW,
Nagengast FM and Peters WH: Overexpression of COX-2 mRNA in
colorectal cancer. BMC Gastroenterol. 14:12014. View Article : Google Scholar
|
|
61
|
Lin PC, Lin YJ, Lee CT, Liu HS and Lee JC:
Cyclooxygenase-2 expression in the tumor environment is associated
with poor prognosis in colorectal cancer patients. Oncol Lett.
6:733–739. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Xu F, Li M, Zhang C, Cui J, Liu J, Li J
and Jiang H: Clinicopathological and prognostic significance of
COX-2 immu-nohistochemical expression in breast cancer: A
meta-analysis. Oncotarget. 8:6003–6012. 2017.
|
|
63
|
Wang ZM, Liu J, Liu HB, Ye M, Zhang YF and
Yang DS: Abnormal COX2 protein expression may be correlated with
poor prognosis in oral cancer: A meta-analysis. BioMed Res Int.
2014:3642072014.PubMed/NCBI
|
|
64
|
Elder DJ, Halton DE, Crew TE and Paraskeva
C: Apoptosis induction and cyclooxygenase-2 regulation in human
colorectal adenoma and carcinoma cell lines by the
cyclooxygenase-2-selective non-steroidal anti-inflammatory drug
NS-398. Int J Cancer. 86:553–560. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Xu XT, Hu WT, Zhou JY and Tu Y: Celecoxib
enhances the radiosensitivity of HCT116 cells in a COX-2
independent manner by up-regulating BCCIP. Am J Transl Res.
9:1088–1100. 2017.PubMed/NCBI
|
|
66
|
Alfonso L, Ai G, Spitale RC and Bhat GJ:
Molecular targets of aspirin and cancer prevention. Br J Cancer.
111:61–67. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Cao S, Yan Y, Zhang X, Zhang K, Liu C,
Zhao G, Han J, Dong Q, Shen B, Wu A, et al: EGF stimulates
cyclooxygenase-2 expression through the STAT5 signaling pathway in
human lung adenocarcinoma A549 cells. Int J Oncol. 39:383–391.
2011.PubMed/NCBI
|
|
68
|
Lippman SM, Gibson N, Subbaramaiah K and
Dannenberg AJ: Combined targeting of the epidermal growth factor
receptor and cyclooxygenase-2 pathways. Clin Cancer Res.
11:6097–6099. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Choe MS, Zhang X, Shin HJ, Shin DM and
Chen ZG: Interaction between epidermal growth factor receptor- and
cyclooxygenase 2-mediated pathways and its implications for the
chemoprevention of head and neck cancer. Mol Cancer Ther.
4:1448–1455. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Huang CY and Yu LC: Pathophysiological
mechanisms of death resistance in colorectal carcinoma. World J
Gastroenterol. 21:11777–11792. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Kim YM, Park SY and Pyo H:
Cyclooxygenase-2 (COX-2) negatively regulates expression of
epidermal growth factor receptor and causes resistance to gefitinib
in COX-2-overexpressing cancer cells. Mol Cancer Res. 7:1367–1377.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Hu H, Han T, Zhuo M, Wu LL, Yuan C, Wu L,
Lei W, Jiao F and Wang LW: Elevated COX-2 expression promotes
angio-genesis through EGFR/p38-MAPK/Sp1-dependent signalling in
pancreatic cancer. Sci Rep. 7:4702017. View Article : Google Scholar
|
|
73
|
Shalini S, Dorstyn L, Dawar S and Kumar S:
Old, new and emerging functions of caspases. Cell Death Differ.
22:526–539. 2015. View Article : Google Scholar :
|
|
74
|
Fujita J, Crane AM, Souza MK, Dejosez M,
Kyba M, Flavell RA, Thomson JA and Zwaka TP: Caspase activity
mediates the differentiation of embryonic stem cells. Cell Stem
Cell. 2:595–601. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Janzen V, Fleming HE, Riedt T, Karlsson G,
Riese MJ, Lo Celso C, Reynolds G, Milne CD, Paige CJ, Karlsson S,
et al: Hematopoietic stem cell responsiveness to exogenous signals
is limited by caspase-3. Cell Stem Cell. 2:584–594. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
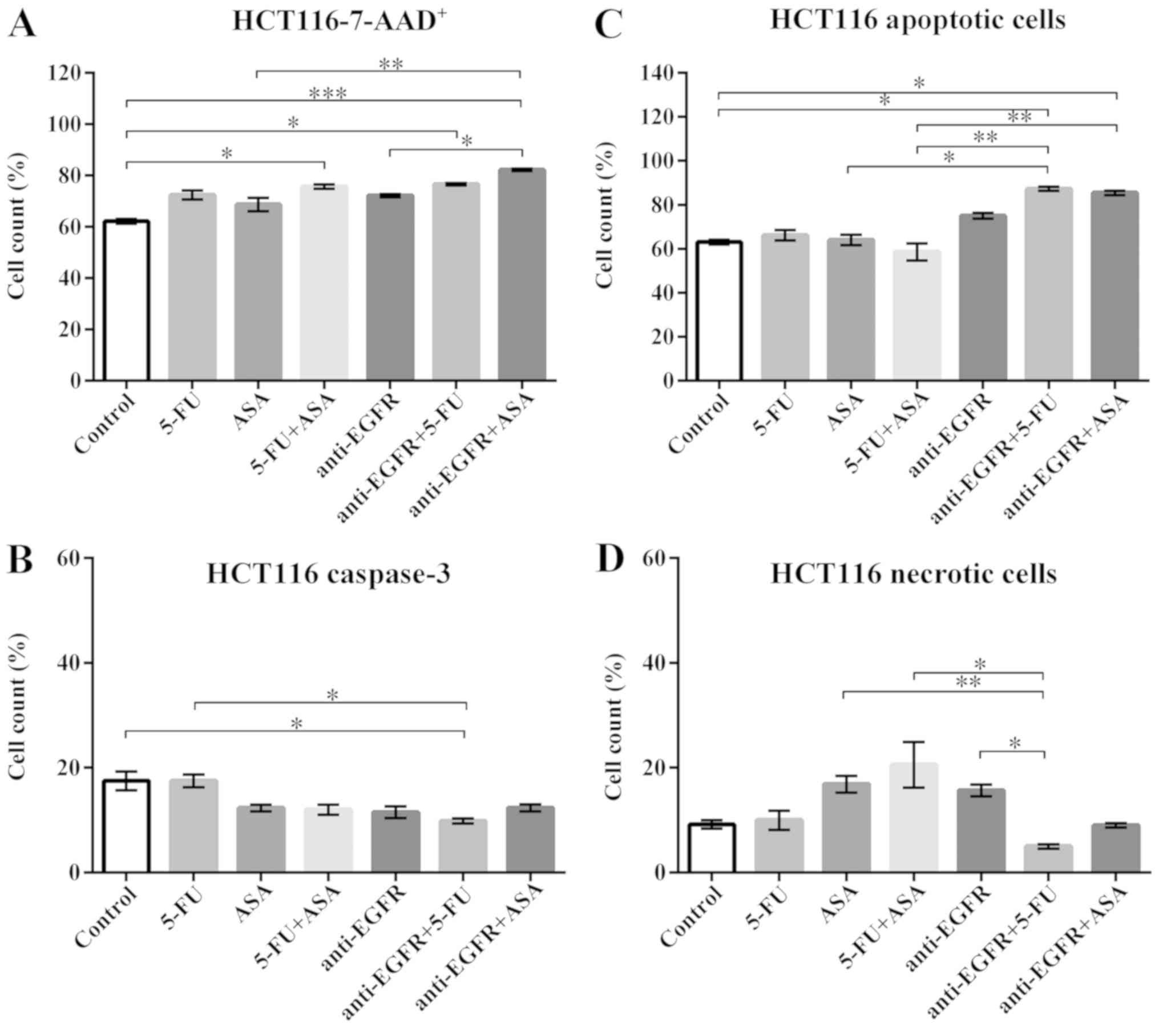
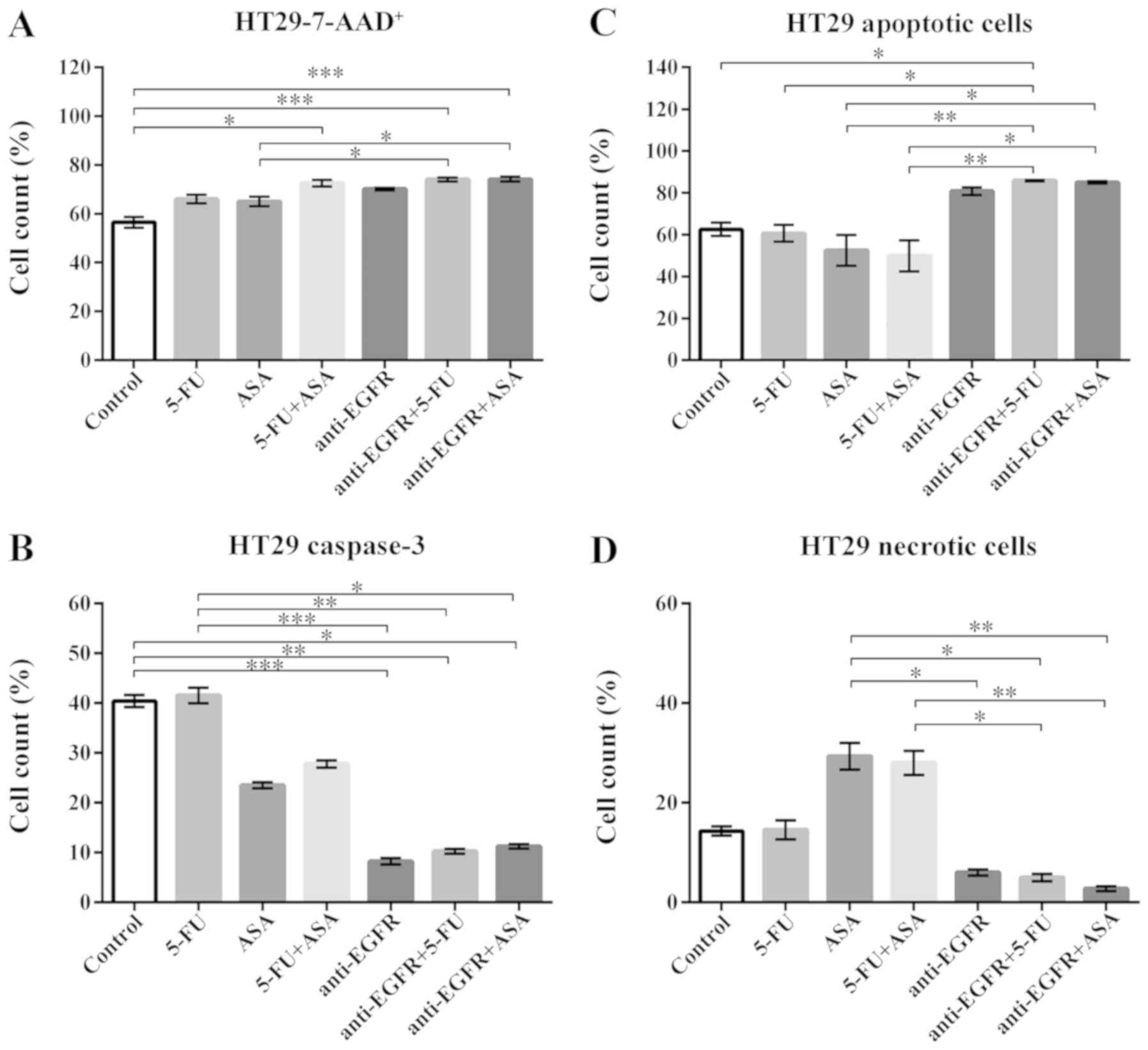
Flanagan L, Meyer M, Fay J, Curry S, Bacon
O, Duessmann H, John K, Boland KC, McNamara DA, Kay EW, et al: Low
levels of Caspase- 3 predict favourable response to 5FU-based
chemotherapy in advanced colorectal cancer: Caspase-3 inhibition as
a therapeutic approach. Cell Death Dis. 7:e20872016. View Article : Google Scholar
|
|
77
|
Liang Y, Yan C and Schor NF: Apoptosis in
the absence of caspase 3. Oncogene. 20:6570–6578. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Huang Q, Li F, Liu X, Li W, Shi W, Liu FF,
O'Sullivan B, He Z, Peng Y, Tan AC, et al: Caspase 3-mediated
stimulation of tumor cell repopulation during cancer radiotherapy.
Nat Med. 17:860–866. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Li F, Huang Q, Chen J, Peng Y, Roop DR,
Bedford JS and Li CY: Apoptotic cells activate the 'phoenix rising'
pathway to promote wound healing and tissue regeneration. Sci
Signal. 3:ra132010. View Article : Google Scholar
|
|
80
|
Pietilä M, Lehtonen S, Närhi M, Hassinen
IE, Leskelä HV, Aranko K, Nordström K, Vepsäläinen A and Lehenkari
P: Mitochondrial function determines the viability and osteogenic
potency of human mesenchymal stem cells. Tissue Eng Part C Methods.
16:435–445. 2010. View Article : Google Scholar
|
|
81
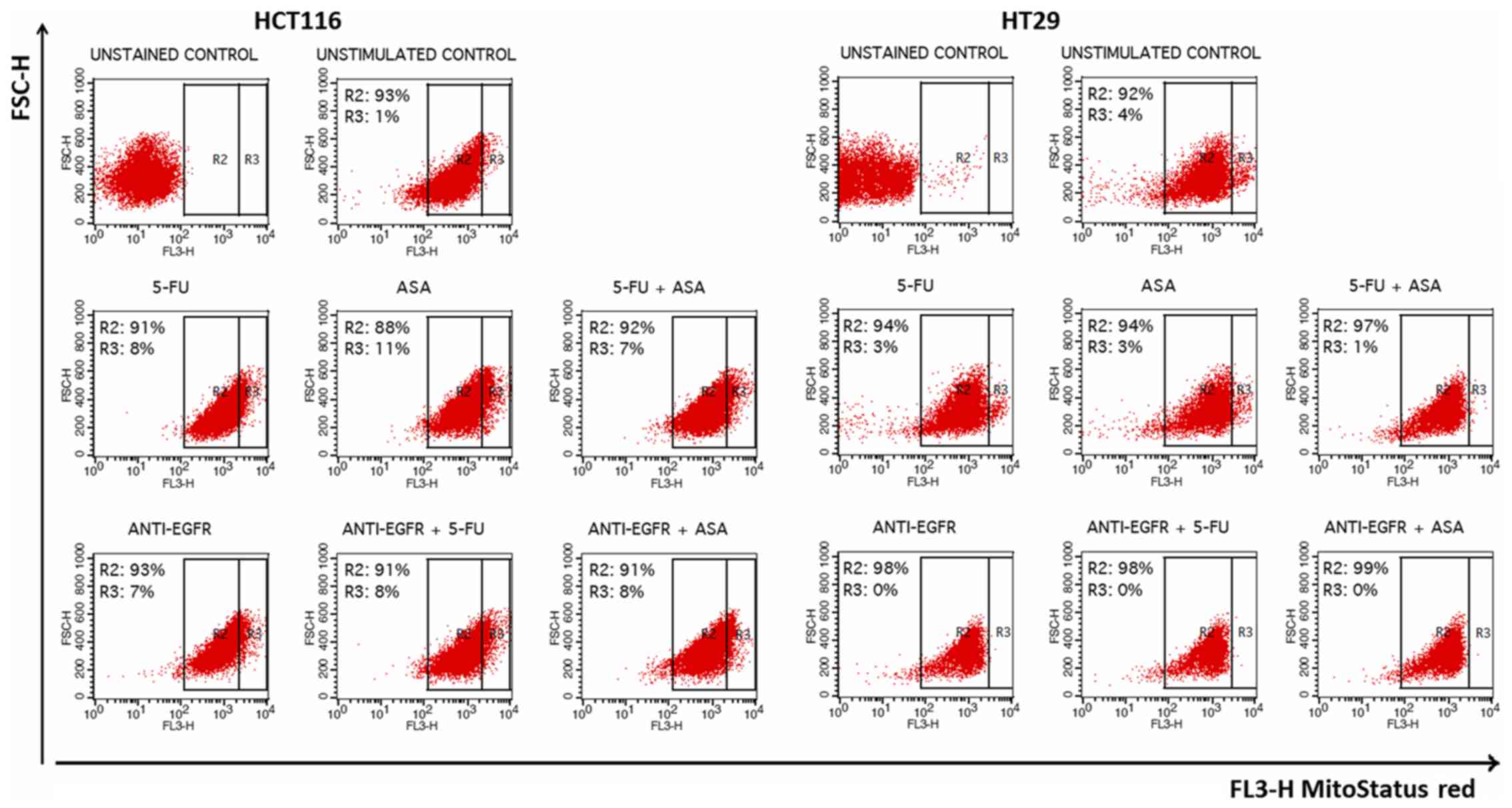
|
Heerdt BG, Houston MA, Wilson AJ and
Augenlicht LH: The intrinsic mitochondrial membrane potential
(Deltapsim) is associated with steady-state mitochondrial activity
and the extent to which colonic epithelial cells undergo
butyrate-mediated growth arrest and apoptosis. Cancer Res.
63:6311–6319. 2003.PubMed/NCBI
|
|
82
|
Heerdt BG, Houston MA and Augenlicht LH:
The intrinsic mitochondrial membrane potential of colonic carcinoma
cells is linked to the probability of tumor progression. Cancer
Res. 65:9861–9867. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Heerdt BG, Houston MA and Augenlicht LH:
Growth properties of colonic tumor cells are a function of the
intrinsic mitochondrial membrane potential. Cancer Res.
66:1591–1596. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Ye XQ, Li Q, Wang GH, Sun FF, Huang GJ,
Bian XW, Yu SC and Qian GS: Mitochondrial and energy
metabolism-related properties as novel indicators of lung cancer
stem cells. Int J Cancer. 129:820–831. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Michelakis ED, Sutendra G, Dromparis P,
Webster L, Haromy A, Niven E, Maguire C, Gammer TL, Mackey JR,
Fulton D, et al: Metabolic modulation of glioblastoma with
dichloroacetate. Sci Transl Med. 2:31ra342010. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Pastò A, Bellio C, Pilotto G, Ciminale V,
Silic-Benussi M, Guzzo G, Rasola A, Frasson C, Nardo G, Zulato E,
et al: Cancer stem cells from epithelial ovarian cancer patients
privilege oxidative phosphorylation, and resist glucose
deprivation. Oncotarget. 5:4305–4319. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Sun T, Ming L, Yan Y, Zhang Y and Xue H:
Beclin 1 acetylation impairs the anticancer effect of aspirin in
colorectal cancer cells. Oncotarget. 8:74781–74790. 2017.PubMed/NCBI
|
|
88
|
Morselli E, Galluzzi L, Kepp O, Vicencio
JM, Criollo A, Maiuri MC and Kroemer G: Anti- and pro-tumor
functions of autophagy. Biochim Biophys Acta. 1793:1524–1532. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Phi LT, Sari IN, Yang YG, Lee SH, Jun N,
Kim KS, Lee YK and Kwon HY: Cancer stem cells (CSCs) in drug
resistance and their therapeutic implications in cancer treatment.
Stem Cells Int. 2018:54169232018. View Article : Google Scholar : PubMed/NCBI
|