|
1
|
Orso F, Quirico L, Dettori D, Coppo R,
Virga F, Ferreira LC, Paoletti C, Baruffaldi D, Penna E and Taverna
D: Role of miRNAs in tumor and endothelial cell interactions during
tumor progression. Semin Cancer Biol. 60:214–224. 2020. View Article : Google Scholar
|
|
2
|
Iwakawa HO and Tomari Y: The functions of
MicroRNAs: mRNA decay and translational repression. Trends Cell
Biol. 25:651–665. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
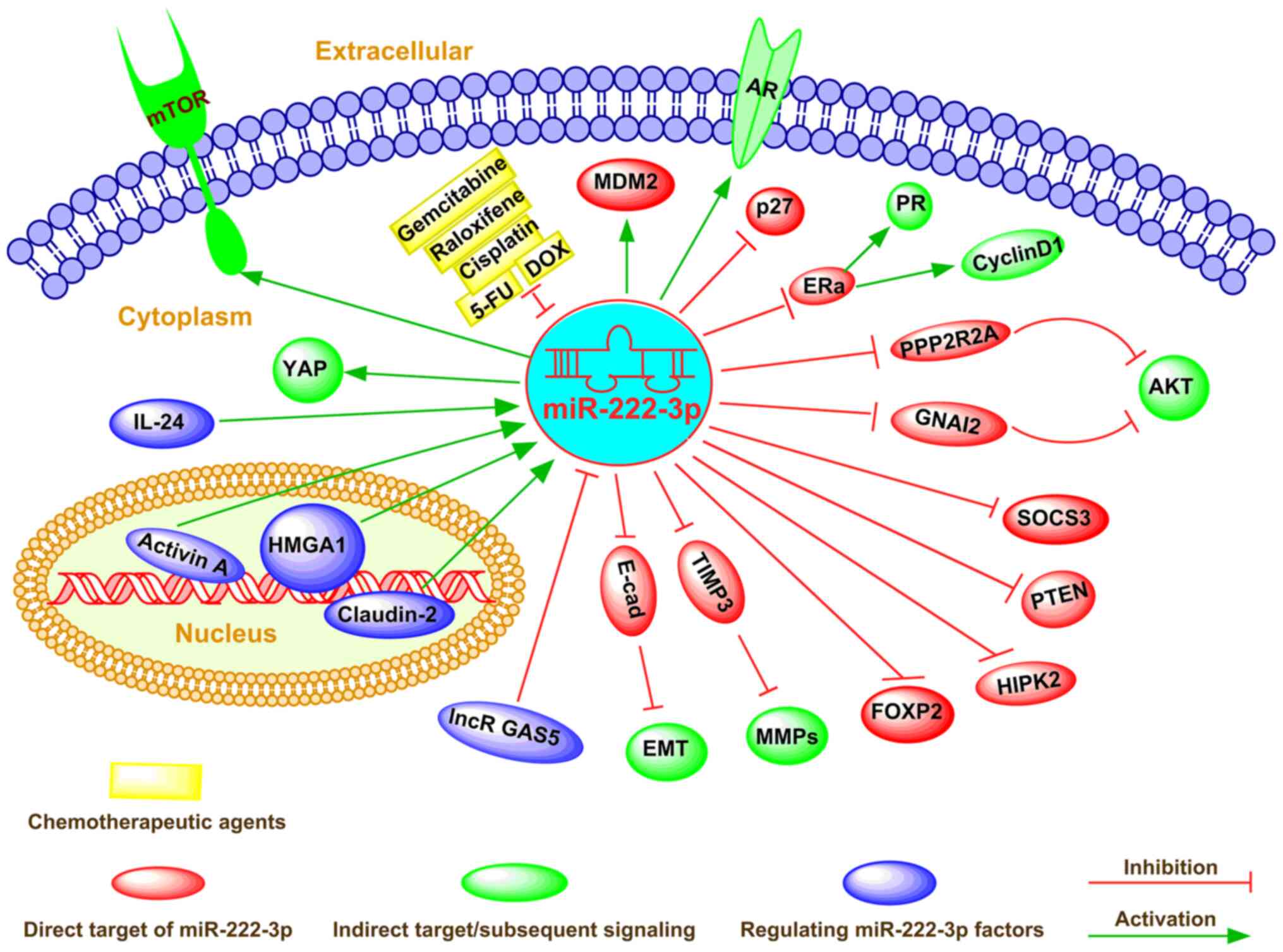
Wightman B, Ha I and Ruvkun G:
Posttranscriptional regulation of the heterochronic gene lin-14 by
lin-4 mediates temporal pattern formation in C. elegans. Cell.
75:855–862. 1993. View Article : Google Scholar : PubMed/NCBI
|
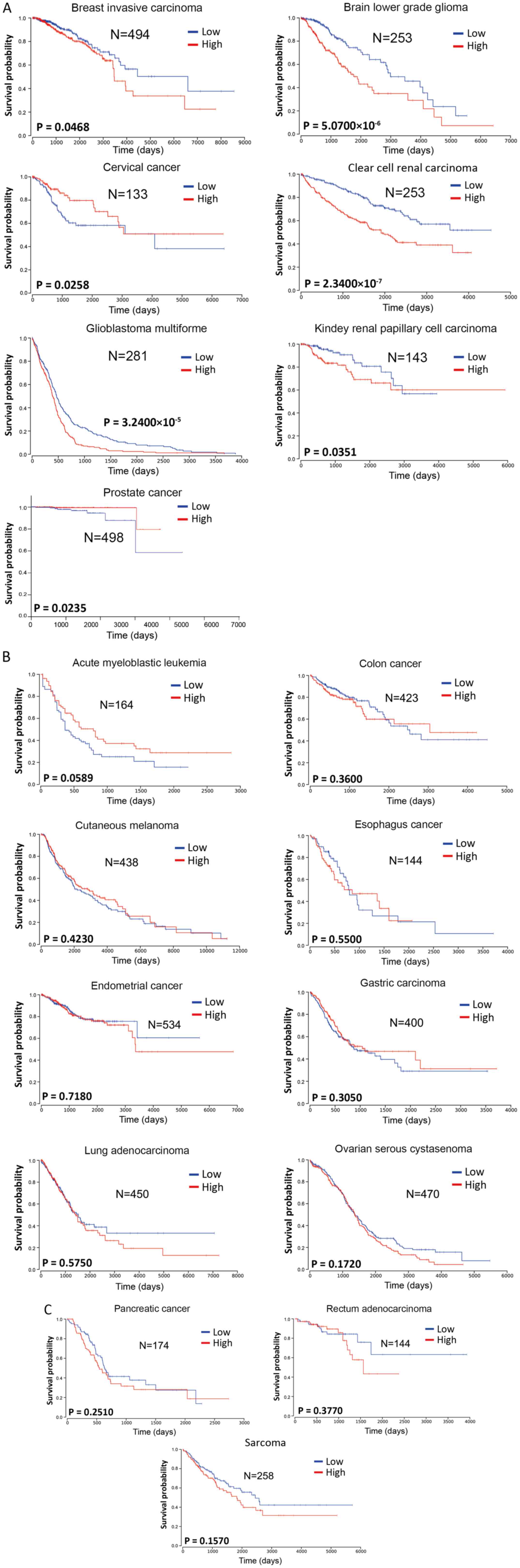
|
4
|
Rupaimoole R, Calin GA, Lopez-Berestein G
and Sood AK: miRNA deregulation in cancer cells and the tumor
microenvironment. Cancer Discov. 6:235–246. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gebert LFR and MacRae IJ: Regulation of
microRNA function in animals. Nat Rev Mol Cell Biol. 20:21–37.
2019. View Article : Google Scholar :
|
|
6
|
Treiber T, Treiber N and Meister G:
Regulation of microRNA biogenesis and its crosstalk with other
cellular pathways. Nat Rev Mol Cell Biol. 20:5–20. 2019. View Article : Google Scholar
|
|
7
|
Ha M and Kim VN: Regulation of microRNA
biogenesis. Nat Rev Mol Cell Biol. 15:509–524. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chendrimada TP, Gregory RI, Kumaraswamy E,
Norman J, Cooch N, Nishikura K and Shiekhattar R: TRBP recruits the
Dicer complex to Ago2 for microRNA processing and gene silencing.
Nature. 436:740–744. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhao JJ, Chu ZB, Hu Y, Lin J, Wang Z,
Jiang M, Chen M, Wang X, Kang Y, Zhou Y, et al: Targeting the
miR-221-222/PUMA/BAK/BAX pathway abrogates dexamethasone resistance
in multiple myeloma. Cancer Res. 75:4384–4397. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chang KW, Kao SY, Wu YH, Tsai MM, Tu HF,
Liu CJ, Lui MT and Lin SC: Passenger strand miRNA miR-31* regulates
the phenotypes of oral cancer cells by targeting RhoA. Oral Oncol.
49:27–33. 2013. View Article : Google Scholar
|
|
11
|
Ogawa T, Enomoto M, Fujii H, Sekiya Y,
Yoshizato K, Ikeda K and Kawada N: MicroRNA-221/222 upregulation
indicates the activation of stellate cells and the progression of
liver fibrosis. Gut. 61:1600–1609. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yasmeen S, Kaur S, Mirza AH, Brodin B,
Pociot F and Kruuse C: miRNA-27a-3p and miRNA-222-3p as novel
modulators of phosphodiesterase 3a (PDE3A) in cerebral
microvascular endothelial cells. Mol Neurobiol. 56:5304–5314. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gulluoglu S, Tuysuz EC, Kuskucu A, Ture U,
Atalay B, Sahin F and Bayrak OF: The potential function of microRNA
in chordomas. Gene. 585:76–83. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu C, Liu Z, Ma L, Pei C, Qin L, Gao N, Li
J and Yin Y: MiRNAs regulate oxidative stress related genes via
binding to the 3'UTR and TATA-box regions: A new hypothesis for
cataract pathogenesis. BMC Ophthalmol. 17:2–8. 2017. View Article : Google Scholar
|
|
15
|
Verjans R, Peters T, Beaumont FJ, van
Leeuwen R, van Herwaarden T, Verhesen W, Munts C, Bijnen M, Henkens
M, Diez J, et al: MicroRNA-221/222 family counteracts myocardial
fibrosis in pressure overload-induced heart failure. Hypertension.
71:280–288. 2018. View Article : Google Scholar
|
|
16
|
Wei F, Ma C, Zhou T, Dong X, Luo Q, Geng
L, Ding L, Zhang Y, Zhang L, Li N, et al: Exosomes derived from
gemcitabine-resistant cells transfer malignant phenotypic traits
via delivery of miRNA-222-3p. Mol Cancer. 16:132–147. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Coarfa C, Fiskus W, Eedunuri VK,
Rajapakshe K, Foley C, Chew SA, Shah SS, Geng C, Shou J, Mohamed
JS, et al: Comprehensive proteomic profiling identifies the
androgen receptor axis and other signaling pathways as targets of
microRNAs suppressed in metastatic prostate cancer. Oncogene.
35:2345–2356. 2016. View Article : Google Scholar
|
|
18
|
Liu L, Wang HJ, Meng T, Lei C, Yang XH,
Wang QS, Jin B and Zhu JF: lncRNA GAS5 inhibits cell migration and
invasion and promotes autophagy by targeting miR-222-3p via the
GAS5/PTEN-signaling pathway in CRC. Mol Ther Nucleic Acids.
17:644–656. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jafri MA, Al-Qahtani MH and Shay JW: Role
of miRNAs in human cancer metastasis: Implications for therapeutic
intervention. Semin Cancer Biol. 44:117–131. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Alves Dos Santos K, Clemente Dos Santos
IC, Santos Silva C, Gomes Ribeiro H, de Farias Domingos I and
Nogueira Silbiger V: Circulating exosomal miRNAs as biomarkers for
the diagnosis and prognosis of Colorectal Cancer. 22:3462020.
|
|
22
|
Fong M, Yan W, Ghassemian M, Wu X, Zhou X,
Cao M, Jiang L, Wang J, Liu X, Zhang J and Wang SJ: Cancer-secreted
miRNAs regulate amino-acid-induced mTORC1 signaling and fibroblast
protein synthesis. EMBO Rep. 22:e512392020.PubMed/NCBI
|
|
23
|
Wang X, Liao X, Huang K, Zeng X, Liu Z,
Zhou X, Yu T, Yang C, Yu L, Wang Q, et al: Clustered microRNAs
hsa-miR-221-3p/hsa-miR-222-3p and their targeted genes might be
prognostic predictors for hepatocellular carcinoma. J Cancer.
10:2520–2533. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wang H, Deng Z, Chen X, Cai J, Ma T, Zhong
Q, Li R, Li L and Li T: Downregulation of miR-222-3p reverses
doxorubicin-resistance in LoVo cells through upregulating forkhead
box protein P2 (FOXP2) protein. Med Sci Monit. 25:2169–2178. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Guo J, Liu Q, Li Z, Guo H, Bai C and Wang
F: miR-222-3p promotes osteosarcoma cell migration and invasion
through targeting TIMP3. Onco Targets Ther. 11:8643–8653. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liu B, Che Q, Qiu H, Bao W, Chen X, Lu W,
Li B and Wan X: Elevated MiR-222-3p promotes proliferation and
invasion of endometrial carcinoma via targeting ERalpha. PLoS One.
9:e875632014. View Article : Google Scholar
|
|
27
|
Ostenfeld MS, Jensen SG, Jeppesen DK,
Christensen LL, Thorsen SB, Stenvang J, Hvam ML, Thomsen A,
Mouritzen P, Rasmussen MH, et al: miRNA profiling of circulating
EpCAM(+) extracellular vesicles: Promising biomarkers of colorectal
cancer. J Extracell Vesicles. 5:3402–3417. 2016. View Article : Google Scholar
|
|
28
|
Korabecna M, Koutova L and Tesarova P: The
potential roles of vesicle-enclosed miRNAs in communication between
macrophages and cancer cells in tumor microenvironment. Neoplasma.
64:406–411. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gasparello J, Papi C, Allegretti M,
Giordani E, Carboni F, Zazza S, Pescarmona E, Romania P, Giacomini
P, Scapoli C, et al: A distinctive microRNA (miRNA) signature in
the blood of colorectal cancer (CRC) patients at surgery. Cancers
(Basel). 12:24102020. View Article : Google Scholar
|
|
30
|
Pudova E, Krasnov G, Nyushko K,
Kobelyatskaya A, Savvateeva M, Poloznikov A, Dolotkazin D, Klimina
K, Guvatova Z, Simanovsky S, et al: miRNAs expression signature
potentially associated with lymphatic dissemination in locally
advanced prostate cancer. BMC Med Genomics. 13(Suppl 8): S1292020.
View Article : Google Scholar
|
|
31
|
Jiang K, Li G, Chen W, Song L, Wei T, Li
Z, Gong R, Lei J, Shi H and Zhu J: Plasma exosomal miR-146b-5p and
miR-222-3p are potential biomarkers for lymph node metastasis in
papillary thyroid carcinomas. Onco Targets Ther. 13:1311–1319.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fredsoe J, Rasmussen AKI, Mouritzen P,
Borre M, Orntoft T and Sorensen KD: A five-microRNA model (pCaP)
for predicting prostate cancer aggressiveness using cell-free
urine. Int J Cancer. 145:2558–2567. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Cheng Y, Cheng T, Zhao Y and Qu Y: HMGA1
exacerbates tumor progression by activating miR-222 through
PI3K/Akt/MMP-9 signaling pathway in uveal melanoma. Cell Signal.
63:52019. View Article : Google Scholar
|
|
34
|
Zhang XF, Ye Y and Zhao SJ: LncRNA Gas5
acts as a ceRNA to regulate PTEN expression by sponging miR-222-3p
in papillary thyroid carcinoma. Oncotarget. 9:3519–3530. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tan X, Tang H, Bi J, Li N and Jia Y:
MicroRNA-222-3p associated with Helicobacter pylori targets HIPK2
to promote cell proliferation, invasion, and inhibits apoptosis in
gastric cancer. J Cell Biochem. 119:5153–5162. 2018. View Article : Google Scholar
|
|
36
|
Ma S, Kong S, Gu X, Xu Y, Tao M, Shen L,
Shen X and Ju S: As a biomarker for gastric cancer, circPTPN22
regulates the progression of gastric cancer through the EMT
pathway. Cancer Cell Int. 21:442021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Fu X, Li Y, Alvero A, Li J, Wu Q, Xiao Q,
Peng Y, Hu Y, Li X, Yan W, et al: MicroRNA-222-3p/GNAI2/AKT axis
inhibits epithelial ovarian cancer cell growth and associates with
good overall survival. Oncotarget. 7:80633–80654. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Rosignolo F, Memeo L, Monzani F, Colarossi
C, Pecce V, Verrienti A, Durante C, Grani G, Lamartina L, Forte S,
et al: MicroRNA-based molecular classification of papillary thyroid
carcinoma. Int J Oncol. 50:1767–1777. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Di Fazio P, Montalbano R, Neureiter D,
Alinger B, Schmidt A, Merkel AL, Quint K and Ocker M:
Downregulation of HMGA2 by the pan-deacetylase inhibitor
panobinostat is dependent on hsa-let-7b expression in liver cancer
cell lines. Exp Cell Res. 318:1832–1843. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jahanbani I, Al-Abdallah A, Ali RH,
Al-Brahim N and Mojiminiyi O: Discriminatory miRNAs for the
management of papillary thyroid carcinoma and noninvasive
follicular thyroid neoplasms with papillary-like nuclear features.
Thyroid. 28:319–327. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Denaro M, Ugolini C, Poma AM, Borrelli N,
Materazzi G, Piaggi P, Chiarugi M, Miccoli P, Vitti P and Basolo F:
Differences in miRNA expression profiles between wild-type and
mutated NIFTPs. Endocr Relat Cancer. 24:543–553. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Borrelli N, Denaro M, Ugolini C, Poma AM,
Miccoli M, Vitti P, Miccoli P and Basolo F: miRNA expression
profiling of 'noninvasive follicular thyroid neoplasms with
papillary-like nuclear features' compared with adenomas and
infiltrative follicular variants of papillary thyroid carcinomas.
Mod Pathol. 30:39–51. 2017. View Article : Google Scholar
|
|
43
|
de Conti A, Ortega JF, Tryndyak V, Dreval
K, Moreno FS, Rusyn I, Beland FA and Pogribny IP: MicroRNA
deregulation in nonalcoholic steatohepatitis-associated liver
carcinogenesis. Oncotarget. 8:88517–88528. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kim BH, Hong SW, Kim A, Choi SH and Yoon
SO: Prognostic implications for high expression of oncogenic
microRNAs in advanced gastric carcinoma. J Surg Oncol. 107:505–510.
2013. View Article : Google Scholar
|
|
45
|
Zhang L, Huang Z, Zhang H, Zhu M, Zhu W,
Zhou X and Liu P: Prognostic value of candidate microRNAs in
gastric cancer: A validation study. Cancer Biomark. 18:221–230.
2017. View Article : Google Scholar
|
|
46
|
Rinnerthaler G, Hackl H, Gampenrieder SP,
Hamacher F, Hufnagl C, Hauser-Kronberger C, Zehentmayr F, Fastner
G, Sedlmayer F, Mlineritsch B and Greil R: miR-16-5p is a
stably-expressed house-keeping MicroRNA in breast cancer tissues
from primary tumors and from metastatic sites. Int J Mol Sci.
17:156–167. 2016. View Article : Google Scholar
|
|
47
|
Fredsoe J, Rasmussen AKI, Thomsen AR,
Mouritzen P, Hoyer S, Borre M, Orntoft TF and Sorensen KD:
Diagnostic and prognostic MicroRNA biomarkers for prostate cancer
in cell-free urine. Eur Urol Focus. 4:825–833. 2018. View Article : Google Scholar
|
|
48
|
Fang R, Zhu Y, Hu L, Khadka VS, Ai J, Zou
H, Ju D, Jiang B, Deng Y and Hu X: Plasma MicroRNA pair panels as
novel biomarkers for detection of early stage breast cancer. Front
Physiol. 9:1879–1880. 2018. View Article : Google Scholar
|
|
49
|
Fu Z, Qian F, Yang X, Jiang H, Chen Y and
Liu S: Circulating miR-222 in plasma and its potential diagnostic
and prognostic value in gastric cancer. Med Oncol. 31:164–175.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Chang YA, Weng SL, Yang SF, Chou CH, Huang
WC, Tu SJ, Chang TH, Huang CN, Jong YJ and Huang HD: A
Three-MicroRNA signature as a potential biomarker for the early
detection of oral cancer. Int J Mol Sci. 19:7582018. View Article : Google Scholar
|
|
51
|
Fredsoe J, Rasmussen AKI, Laursen EB, Cai
Y, Howard KA, Pedersen BG, Borre M, Mouritzen P, Orntoft T and
Sorensen KD: Independent validation of a diagnostic noninvasive
3-MicroRNA ratio model (uCaP) for prostate cancer in cell-free
urine. Clin Chem. 65:540–548. 2019. View Article : Google Scholar
|
|
52
|
Uchino K, Takeshita F, Takahashi RU,
Kosaka N, Fujiwara K, Naruoka H, Sonoke S, Yano J, Sasaki H, Nozawa
S, et al: Therapeutic effects of microRNA-582-5p and -3p on the
inhibition of bladder cancer progression. Mol Ther. 21:610–619.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Tan X, Tang H, Bi J, Li N and Jia Y:
MicroRNA-222-3p associated with Helicobacter pylori targets HIPK2
to promote cell proliferation, invasion, and inhibits apoptosis in
gastric cancer. J Cell Biochem. 119:5153–5162. 2018. View Article : Google Scholar
|
|
54
|
Rosignolo F, Sponziello M, Giacomelli L,
Russo D, Pecce V, Biffoni M, Bellantone R, Lombardi CP, Lamartina
L, Grani G, et al: Identification of thyroid-associated serum
microRNA profiles and their potential use in thyroid cancer
follow-up. J Endocr Soc. 1:3–13. 2017.PubMed/NCBI
|
|
55
|
Ulivi P, Petracci E, Marisi G, Baglivo S,
Chiari R, Billi M, Canale M, Pasini L, Racanicchi S, Vagheggini A,
et al: Prognostic role of circulating miRNAs in Early-stage
non-small cell lung cancer. J Clin Med. 8:131–142. 2019. View Article : Google Scholar :
|
|
56
|
Wang Y, Yin W, Lin Y, Yin K, Zhou L, Du Y,
Yan T and Lu J: Downregulated circulating microRNAs after surgery:
Potential noninvasive biomarkers for diagnosis and prognosis of
early breast cancer. Cell Death Discov. 4:2–8. 2018. View Article : Google Scholar
|
|
57
|
Kara M, Yumrutas O, Ozcan O, Celik OI,
Bozgeyik E, Bozgeyik I and Tasdemir S: Differential expressions of
cancer-associated genes and their regulatory miRNAs in colorectal
carcinoma. Gene. 567:81–86. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Spindler KL, Pallisgaard N, Vogelius I and
Jakobsen A: Quantitative cell-free DNA, KRAS, and BRAF mutations in
plasma from patients with metastatic colorectal cancer during
treatment with cetuximab and irinotecan. Clin Cancer Res.
18:1177–1185. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Domingo E, Camps C, Kaisaki PJ, Parsons
MJ, Mouradov D, Pentony MM, Makino S, Palmieri M, Ward RL, Hawkins
NJ, et al: Mutation burden and other molecular markers of prognosis
in colorectal cancer treated with curative intent: Results from the
QUASAR 2 clinical trial and an Australian community-based series.
Lancet Gastroenterol Hepatol. 3:635–643. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Zhao H, Shen J, Hodges TR, Song R, Fuller
GN and Heimberger AB: Serum microRNA profiling in patients with
glioblastoma: A survival analysis. Mol Cancer. 16:59–70. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Cooper J and Giancotti FG: Integrin
signaling in cancer: Mechanotransduction, stemness, epithelial
plasticity, and therapeutic resistance. Cancer Cell. 35:347–367.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Friedmann Angeli JP, Krysko DV and Conrad
M: Ferroptosis at the crossroads of cancer-acquired drug resistance
and immune evasion. Nat Rev Cancer. 19:405–414. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Tooker P, Yen WC, Ng SC, Negro-Vilar A and
Hermann TW: Bexarotene (LGD1069, Targretin), a selective retinoid X
receptor agonist, prevents and reverses gemcitabine resistance in
NSCLC cells by modulating gene amplification. Cancer Res.
67:4425–4433. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Alvarez-Garcia I and Miska EA: MicroRNA
functions in animal development and human disease. Development.
132:4653–4662. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Lu J, Getz G, Miska EA, Alvarez-Saavedra
E, Lamb J, Peck D, Sweet-Cordero A, Ebert BL, Mak RH, Ferrando AA,
et al: MicroRNA expression profiles classify human cancers. Nature.
435:834–838. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Garofalo M, Romano G, Di Leva G, Nuovo G,
Jeon YJ, Ngankeu A, Sun J, Lovat F, Alder H, Condorelli G, et al:
EGFR and MET receptor tyrosine kinase-altered microRNA expression
induces tumorigenesis and gefitinib resistance in lung cancers. Nat
Med. 18:74–82. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Liu S, Sun X, Wang M, Hou Y, Zhan Y, Jiang
Y, Liu Z, Cao X, Chen P, Chen X, et al: A microRNA 221- and
222-mediated feedback loop maintains constitutive activation of
NFκB and STAT3 in colorectal cancer cells. Gastroenterology.
147:847–859.e11. 2014. View Article : Google Scholar
|
|
68
|
Ladeiro Y, Couchy G, Balabaud C,
Bioulac-Sage P, Pelletier L, Rebouissou S and Zucman-Rossi J:
MicroRNA profiling in hepatocellular tumors is associated with
clinical features and oncogene/tumor suppressor gene mutations.
Hepatology. 47:1955–1963. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Li Z, Yu Z, Meng X, Zhou S, Xiao S, Li X,
Liu S and Yu P: Long noncoding RNA GAS5 impairs the proliferation
and invasion of endometrial carcinoma induced by high glucose via
targeting miR-222-3p/p27. Am J Transl Res. 11:2413–2421.
2019.PubMed/NCBI
|
|
70
|
Paquet-Fifield S, Koh SL, Cheng L, Beyit
LM, Shembrey C, Molck C, Behrenbruch C, Papin M, Gironella M,
Guelfi S, et al: Tight junction protein Claudin-2 promotes
Self-renewal of human colorectal cancer Stem-like cells. Cancer
Res. 78:2925–2938. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Polk DB and Peek RM Jr: Helicobacter
pylori: Gastric cancer and beyond. Nat Rev Cancer. 10:403–414.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Ishiguro H, Kimura M and Takeyama H: Role
of microRNAs in gastric cancer. World J Gastroenterol.
20:5694–5699. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Ebert MS and Sharp PA: Roles for microRNAs
in conferring robustness to biological processes. Cell.
149:515–524. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Zhao JJ, Lin J, Yang H, Kong W, He L, Ma
X, Coppola D and Cheng JQ: MicroRNA-221/222 negatively regulates
estrogen receptor alpha and is associated with tamoxifen resistance
in breast cancer. J Biol Chem. 291:31079–31086. 2016. View Article : Google Scholar
|
|
75
|
Garofalo M, Di Leva G, Romano G, Nuovo G,
Suh SS, Ngankeu A, Taccioli C, Pichiorri F, Alder H, Secchiero P,
et al: miR-221&222 regulate TRAIL resistance and enhance
tumorigenicity through PTEN and TIMP3 downregulation. Cancer Cell.
16:498–509. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Sun K, Wang W, Zeng JJ, Wu CT, Lei ST and
Li GX: MicroRNA-221 inhibits CDKN1C/p57 expression in human
colorectal carcinoma. Acta Pharmacol Sin. 32:375–384. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Zhang Y, Ma T, Yang S, Xia M, Xu J, An H,
Yang Y and Li S: High-mobility group A1 proteins enhance the
expression of the oncogenic miR-222 in lung cancer cells. Mol Cell
Biochem. 357:363–371. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Ying SY, Chang DC, Miller JD and Lin SL:
The microRNA: Overview of the RNA gene that modulates gene
functions. Methods Mol Biol. 342:1–18. 2006.PubMed/NCBI
|
|
79
|
Fuse M, Kojima S, Enokida H, Chiyomaru T,
Yoshino H, Nohata N, Kinoshita T, Sakamoto S, Naya Y, Nakagawa M,
et al: Tumor suppressive microRNAs (miR-222 and miR-31) regulate
molecular pathways based on microRNA expression signature in
prostate cancer. J Hum Genet. 57:691–699. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Ottley EC, Nicholson HD and Gold EJ:
Activin A regulates microRNAs and gene expression in LNCaP cells.
Prostate. 76:951–963. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Tong AW, Fulgham P, Jay C, Chen P, Khalil
I, Liu S, Senzer N, Eklund AC, Han J and Nemunaitis J: MicroRNA
profile analysis of human prostate cancers. Cancer Gene Ther.
16:206–216. 2009. View Article : Google Scholar
|
|
82
|
Ottley EC, Nicholson HD and Gold EJ:
Activin A regulates microRNAs and gene expression in LNCaP cells.
Prostate. 76:951–963. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Xu G, Wu J, Zhou L, Chen B, Sun Z, Zhao F
and Tao Z: Characterization of the small RNA transcriptomes of
androgen dependent and independent prostate cancer cell line by
deep sequencing. PLoS One. 5:e155192010. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Rihani A, Van Goethem A, Ongenaert M, De
Brouwer S, Volders PJ, Agarwal S, De Preter K, Mestdagh P, Shohet
J, Speleman F, et al: Genome wide expression profiling of p53
regulated miRNAs in neuroblastoma. Sci Rep. 5:9027–9044. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Narrandes S and Xu W: Gene expression
detection assay for cancer clinical use. J Cancer. 9:2249–2265.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Bourboulia D and Stetler-Stevenson WG:
Matrix metalloproteinases (MMPs) and tissue inhibitors of
metalloproteinases (TIMPs): Positive and negative regulators in
tumor cell adhesion. Semin Cancer Biol. 20:161–168. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Liu W, Wang X, Wang Y, Dai Y, Xie Y, Ping
Y, Yin B, Yu P, Liu Z, Duan X, et al: SGK1 inhibition-induced
autophagy impairs prostate cancer metastasis by reversing. EMT J
Exp Clin Cancer Res. 37:732018. View Article : Google Scholar
|
|
88
|
Liu W, Wang X, Liu Z, Wang Y, Yin B, Yu P,
Duan X, Liao Z, Chen Y, Liu C, et al: SGK1 inhibition induces
autophagy-dependent apoptosis via the mTOR-Foxo3a pathway. Br J
Cancer. 117:1139–1153. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Indran IR, Tufo G, Pervaiz S and Brenner
C: Recent advances in apoptosis, mitochondria and drug resistance
in cancer cells. Biochim Biophys Acta. 1807:735–745. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Mavrogiannis A, Kokkinopoulou I, Kontos C
and Sideris DJ: Effect of vinca alkaloids on the expression levels
of microRNAs targeting apoptosis-related genes in breast cancer
cell lines. Curr Pharm Biotechnol. 19:1076–1086. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Jacob H, Stanisavljevic L, Storli KE,
Hestetun KE, Dahl O and Myklebust MP: Identification of a
sixteen-microRNA signature as prognostic biomarker for stage II and
III colon cancer. Oncotarget. 8:87837–87847. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Tan HY, Wang N, Lam W, Guo W, Feng Y and
Cheng YC: Targeting tumour microenvironment by tyrosine kinase
inhibitor. Mol Cancer. 17:43–52. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Vuong L, Kotecha RR, Voss MH and Hakimi
AA: Tumor microenvironment dynamics in clear-cell renal cell
carcinoma. Cancer Discov. 9:1349–1357. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Vitale I, Manic G, Coussens LM, Kroemer G
and Galluzzi L: Macrophages and metabolism in the tumor
microenvironment. Cell Metab. 30:36–50. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Zhou S, Liu R, Yuan K, Yi T, Zhao X, Huang
C and Wei Y: Proteomics analysis of tumor microenvironment:
Implications of metabolic and oxidative stresses in tumorigenesis.
Mass Spectrom Rev. 32:267–311. 2013. View Article : Google Scholar
|
|
96
|
Ying X, Wu Q, Wu X, Zhu Q and Wang X,
Jiang L, Chen X and Wang X: Epithelial ovarian cancer-secreted
exosomal miR-222-3p induces polarization of tumor-associated
macro-phages. Oncotarget. 7:43076–43087. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Cabibbo G, Celsa C, Calvaruso V, Petta S,
Cacciola I, Cannavo MR, Madonia S, Rossi M, Magro B, Rini F, et al:
Direct-acting antivirals after successful treatment of early
hepatocellular carcinoma improve survival in HCV-cirrhotic
patients. J Hepatol. 71:265–273. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Degasperi E, D'Ambrosio R, Iavarone M,
Sangiovanni A, Aghemo A, Soffredini R, Borghi M, Lunghi G, Colombo
M and Lampertico P: Factors associated with increased risk of de
novo or recurrent hepatocellular carcinoma in patients with
cirrhosis treated with direct-acting antivirals for HCV infection.
Clin Gastroenterol Hepatol. 17:1183–1191.e7. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Santangelo L, Bordoni V, Montaldo C,
Cimini E, Zingoni A, Battistelli C, D'Offizi G, Capobianchi MR,
Santoni A, Tripodi M and Agrati C: Hepatitis C virus direct-acting
antivirals therapy impacts on extracellular vesicles microRNAs
content and on their immunomodulating properties. Liver Int.
38:1741–1750. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Varchetta S, Mele D, Mantovani S, Oliviero
B, Cremonesi E, Ludovisi S, Michelone G, Alessiani M, Rosati R,
Montorsi M and Mondelli MU: Impaired intrahepatic natural killer
cell cytotoxic function in chronic hepatitis C virus infection.
Hepatology. 56:841–849. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
van der Meer AJ, Feld JJ, Hofer H, Almasio
PL, Calvaruso V, Fernandez-Rodriguez CM, Aleman S, Ganne-Carrie N,
D'Ambrosio R, Pol S, et al: Risk of cirrhosis-related complications
in patients with advanced fibrosis following hepatitis C virus
eradication. J Hepatol. 66:485–493. 2017. View Article : Google Scholar
|
|
102
|
Fugier E, Marche H, Thélu MA, Macek
Jilková Z, Van Campenhout N, Dufeu-Duchesne T, Leroy V, Zarski JP,
Sturm N, Marche PN and Jouvin-Marche E: Functions of liver natural
killer cells are dependent on the severity of liver inflammation
and fibrosis in chronic hepatitis C. PLoS One. 9:e956142014.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Tölle A, Jung K, Friedersdorff F, Maxeiner
A, Lein M, Fendler A and Stephan C: The discriminative ability of
Prostate Health Index to detect prostate cancer is enhanced in
combination with miR-222-3p. Cancer Biomark. Dec 15–2020.Epub ahead
of print. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Ryu K, Lee J, Choi M, Yoon S, Cho J, Ko Y,
Shim J, Kim W, Park C and Kim SJ: Serum-derived exosomal MicroRNA
profiles can predict poor survival outcomes in patients with
extranodal natural Killer/T-cell lymphoma. Cancers (Basel).
12:35482020. View Article : Google Scholar
|
|
105
|
Zhai S, Xu Z, Xie J, Zhang J, Wang X, Peng
C, Li H, Chen H, Shen B and Deng X: Epigenetic silencing of LncRNA
LINC00261 promotes c-myc-mediated aerobic glycolysis by regulating
miR-222-3p/HIPK2/ERK axis and sequestering IGF2BP1. Oncogene.
40:277–291. 2021. View Article : Google Scholar :
|
|
106
|
Lu B, Sheng Y, Zhang J, Zheng Z and Ji L:
The altered microRNA profile in andrographolide-induced inhibition
of hepatoma tumor growth. Gene. 588:124–133. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Gumbiner BM and Kim NG: The Hippo-YAP
signaling pathway and contact inhibition of growth. J Cell Sci.
127:709–717. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Panneerselvam J, Srivastava A,
Muralidharan R, Wang Q, Zheng W, Zhao L, Chen A, Zhao YD, Munshi A
and Ramesh R: IL-24 modulates the high mobility group (HMG)
A1/miR222/AKT signaling in lung cancer cells. Oncotarget.
7:70247–70263. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Ignacio C, Mooney SM and Middleton FA:
Effects of acute prenatal exposure to ethanol on microRNA
expression are ameliorated by social enrichment. Front Pediatr.
2:1032014. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Théry C, Zitvogel L and Amigorena S:
Exosomes: Composition, biogenesis and function. Nat Rev Immunol.
2:569–579. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
111
|
Pant S, Hilton H and Burczynski ME: The
multifaceted exosome: Biogenesis, role in normal and aberrant
cellular function, and frontiers for pharmacological and biomarker
opportunities. Biochem Pharmacol. 83:1484–1494. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Kalluri R: The biology and function of
exosomes in cancer. J Clin Invest. 126:1208–1215. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Sun Z, Shi K, Yang S, Liu J, Zhou Q, Wang
G, Song J, Li Z, Zhang Z and Yuan W: Effect of exosomal miRNA on
cancer biology and clinical applications. Mol Cancer. 17:1472018.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Han Z, Li Y, Zhang J, Guo C, Li Q, Zhang
X, Lan Y, Gu W, Xing Z, Liang L, et al: Tumor-derived circulating
exosomal miR-342-5p and miR-574-5p as promising diagnostic
biomarkers for early-stage Lung Adenocarcino. Int J Med Sci.
17:1428–1438. 2020. View Article : Google Scholar :
|
|
115
|
Ortega MM and Bouamar H: Guidelines on
designing MicroRNA sponges: From construction to stable cell line.
Methods Mol Biol. 1509:221–233. 2017. View Article : Google Scholar
|
|
116
|
Wang Z: The guideline of the design and
validation of MiRNA mimics. Methods Mol Biol. 676:211–223. 2011.
View Article : Google Scholar
|
|
117
|
Arroyo J, Gallichotte E and Tewari M:
Systematic design and functional analysis of artificial microRNAs.
Nucleic Acids Res. 42:6064–6077. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Ganju A, Khan S, Hafeez BB, Behrman SW,
Yallapu MM, Chauhan SC and Jaggi M: miRNA nanotherapeutics for
cancer. Drug Discov Today. 22:424–432. 2017. View Article : Google Scholar :
|
|
119
|
Chen Y, Gao DY and Huang L: In vivo
delivery of miRNAs for cancer therapy: challenges and strategies.
Adv Drug Deliv Rev. 81:128–141. 2015. View Article : Google Scholar
|
|
120
|
Bofill-De Ros X and Gu S: Guidelines for
the optimal design of miRNA-based shRNAs. Methods. 103:157–166.
2016. View Article : Google Scholar : PubMed/NCBI
|