|
1
|
Gantt CL: Red blood cells for patients
with cancer. Lancet. 2:3631981. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Parmiani G, Fossati G and Della Porta G:
The undefined relationship between tumor antigens and
histocompatibility antigens on cancer cells. Ric Clin Lab.
10:481–492. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jiang XB, Zhang LP, Wang YJ and Ma C:
Research advance on clinical blood transfusion and tumor therapy.
Zhongguo Shi Yan Xue Ye Xue Za Zhi. 18:1092–1095. 2010.(In
Chinese). PubMed/NCBI
|
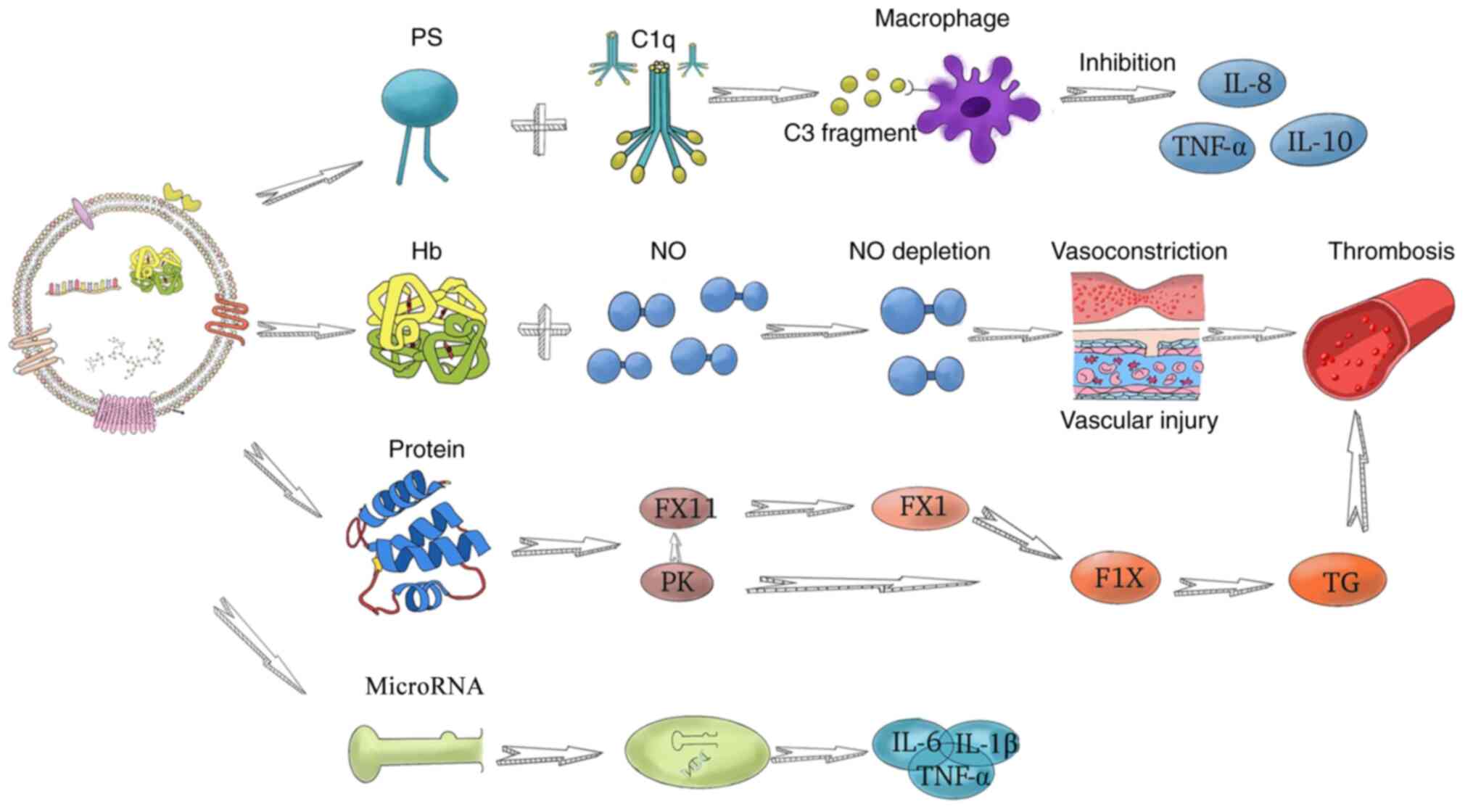
|
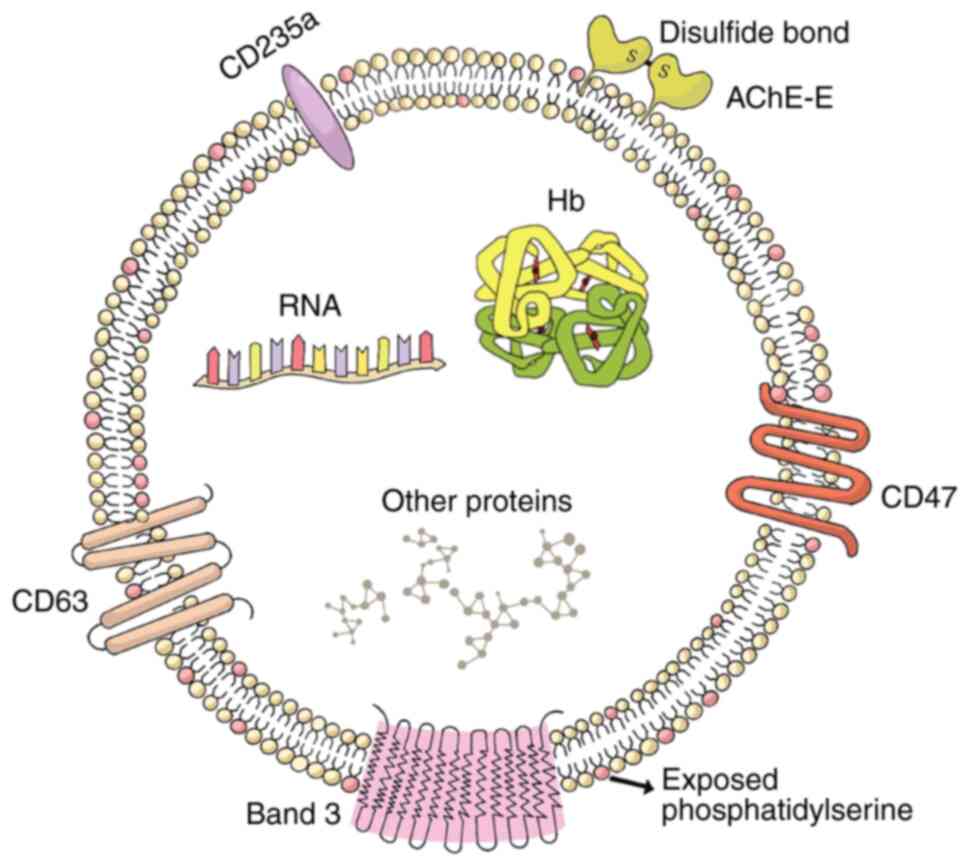
4
|
Kenar G, Köksoy EB, Ürün Y and Utkan G:
Prevalence, etiology and risk factors of anemia in patients with
newly diagnosed cancer. Support Care Cancer. 28:5235–5242. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Owusu C, Cohen HJ, Feng T, Tew W, Mohile
SG, Klepin HD, Gross CP, Gajra A, Lichtman SM and Hurria A; Cancer
Aging Research Group (CARG), . Anemia and functional disability in
older adults with cancer. J Natl Compr Canc Netw. 13:1233–1239.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Watkins T, Surowiecka MK and McCullough J:
Transfusion indications for patients with cancer. Cancer Control.
22:38–46. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dicato M, Plawny L and Diederich M: Anemia
in cancer. Ann Oncol. 21 (Suppl 7):vii167–vii172. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shortt J, Polizzotto MN, Waters N, Borosak
M, Moran M, Comande M, Devine A, Jolley DJ and Wood EM: Assessment
of the urgency and deferability of transfusion to inform emergency
blood planning and triage: The bloodhound prospective audit of red
blood cell use. Transfusion. 49:2296–2303. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tzounakas VL, Seghatchian J, Grouzi E,
Kokoris S and Antonelou MH: Red blood cell transfusion in surgical
cancer patients: Targets, risks, mechanistic understanding and
further therapeutic opportunities. Transfus Apher Sci. 56:291–304.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Al-Refaie WB, Parsons HM, Markin A, Abrams
J and Habermann EB: Blood transfusion and cancer surgery outcomes:
A continued reason for concern. Surgery. 152:344–354. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Aguilar-Nascimento JE, Zampieri-Filho JP
and Bordin JO: Implications of perioperative allogeneic red blood
cell transfusion on the immune-inflammatory response. Hematol
Transfus Cell Ther. 43:58–64. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Connor JP, O'Shea A, McCool K, Sampene E
and Barroilhet LM: Peri-operative allogeneic blood transfusion is
associated with poor overall survival in advanced epithelial
ovarian cancer; potential impact of patient blood management on
cancer outcomes. Gynecol Oncol. 151:294–298. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Goubran H, Sheridan D, Radosevic J,
Burnouf T and Seghatchian J: Transfusion-related immunomodulation
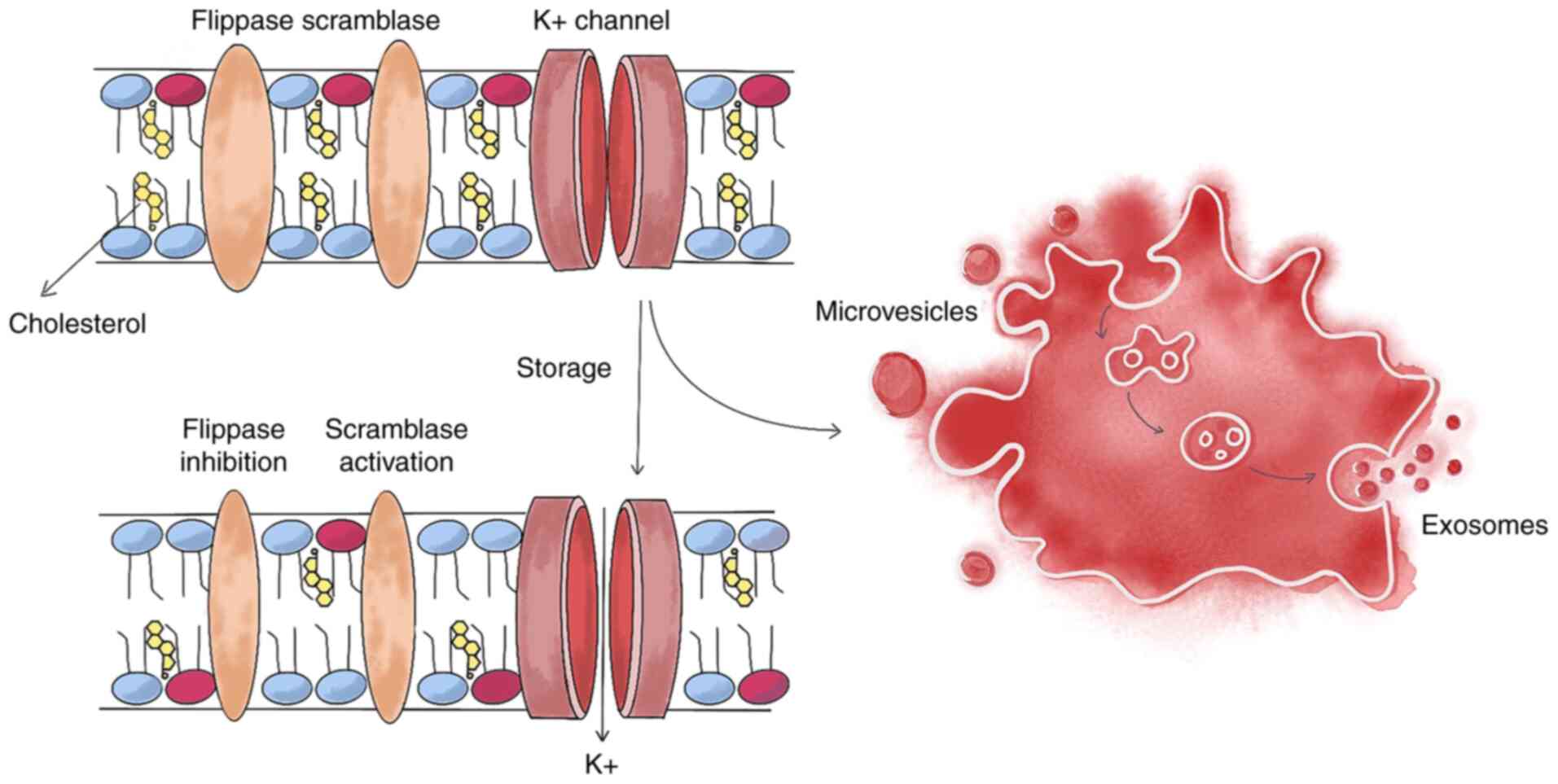
and cancer. Transfus Apher Sci. 56:336–340. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Remy KE, Hall MW, Cholette J, Juffermans
NP, Nicol K, Doctor A, Blumberg N, Spinella PC, Norris PJ, Dahmer
MK, et al: Mechanisms of red blood cell transfusion-related
immunomodulation. Transfusion. 58:804–815. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
D'Alessandro A, Kriebardis AG, Rinalducci
S, Antonelou MH, Hansen KC, Papassideri IS and Zolla L: An update
on red blood cell storage lesions, as gleaned through biochemistry
and omics technologies. Transfusion. 55:205–219. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Laurén E, Tigistu-Sahle F, Valkonen S,
Westberg M, Valkeajärvi A, Eronen J, Siljander P, Pettilä V, Käkelä
R, Laitinen S and Kerkelä E: Phospholipid composition of packed red
blood cells and that of extracellular vesicles show a high
resemblance and stability during storage. Biochim Biophys Acta Mol
Cell Biol Lipids. 1863:1–8. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Antonelou MH and Seghatchian J: Insights
into red blood cell storage lesion: Toward a new appreciation.
Transfus Apher Sci. 55:292–301. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hoehn RS, Jernigan PL, Chang AL, Edwards
MJ and Pritts TA: Molecular mechanisms of erythrocyte aging. Biol
Chem. 396:621–631. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nieuwland R, Falcon-Perez JM, Soekmadji C,
Boilard E, Carter D and Buzas EI: Essentials of extracellular
vesicles: Posters on basic and clinical aspects of extracellular
vesicles. J Extracell Vesicles. 7:15482342018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
van der Pol E, Böing AN, Harrison P, Sturk
A and Nieuwland R: Classification, functions, and clinical
relevance of extracellular vesicles. Pharmacol Rev. 64:676–705.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
van Niel G, D'Angelo G and Raposo G:
Shedding light on the cell biology of extracellular vesicles. Nat
Rev Mol Cell Biol. 19:213–228. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Danesh A, Inglis HC, Jackman RP, Wu S,
Deng X, Muench MO, Heitman JW and Norris PJ: Exosomes from red
blood cell units bind to monocytes and induce proinflammatory
cytokines, boosting T-cell responses in vitro. Blood. 123:687–696.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kriebardis AG, Antonelou MH, Stamoulis KE,
Economou-Petersen E, Margaritis LH and Papassideri IS: RBC-derived
vesicles during storage: Ultrastructure, protein composition,
oxidation, and signaling components. Transfusion. 48:1943–1953.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Azarov I, Liu C, Reynolds H, Tsekouras Z,
Lee JS, Gladwin MT and Kim-Shapiro DB: Mechanisms of slower nitric
oxide uptake by red blood cells and other hemoglobin-containing
vesicles. J Biol Chem. 286:33567–33579. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bosman GJ, Lasonder E, Luten M,
Roerdinkholder-Stoelwinder B, Novotný VM, Bos H and De Grip WJ: The
proteome of red cell membranes and vesicles during storage in blood
bank conditions. Transfusion. 48:827–835. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Huang H, Zhu J, Fan L, Lin Q, Fu D, Wei B
and Wei S: MicroRNA profiling of exosomes derived from red blood
cell units: Implications in transfusion-related immunomodulation.
Biomed Res Int. 2019:20459152019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Saas P, Angelot F, Bardiaux L, Seilles E,
Garnache-Ottou F and Perruche S: Phosphatidylserine-expressing cell
by-products in transfusion: A pro-inflammatory or an
anti-inflammatory effect? Transfus Clin Biol. 19:90–97. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Deeb AP, Aquina CT, Monson JRT, Blumberg
N, Becerra AZ and Fleming FJ: Allogeneic leukocyte-reduced red
blood cell transfusion is associated with postoperative infectious
complications and cancer recurrence after colon cancer resection.
Dig Surg. 37:163–170. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tamini N, Deghi G, Gianotti L, Braga M and
Nespoli L: Colon cancer surgery: Does preoperative blood
transfusion influence short-term postoperative outcomes? J Invest
Surg. 34:974–978. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Qiu L, Wang DR, Zhang XY, Gao S, Li XX,
Sun GP and Lu XB: Impact of perioperative blood transfusion on
immune function and prognosis in colorectal cancer patients.
Transfus Apher Sci. 54:235–241. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Acheson AG, Brookes MJ and Spahn DR:
Effects of allogeneic red blood cell transfusions on clinical
outcomes in patients undergoing colorectal cancer surgery: A
systematic review and meta-analysis. Ann Surg. 256:235–244. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liu X, Ma M, Huang H and Wang Y: Effect of
perioperative blood transfusion on prognosis of patients with
gastric cancer: A retrospective analysis of a single center
database. BMC Cancer. 18:6492018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Benson D and Barnett CC Jr: Perioperative
blood transfusions promote pancreas cancer progression. J Surg Res.
166:275–279. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Churchhouse AM, Mathews TJ, McBride OM and
Dunning J: Does blood transfusion increase the chance of recurrence
in patients undergoing surgery for lung cancer? Interact Cardiovasc
Thorac Surg. 14:85–90. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Seon DY, Kwak C, Kim HH, Ku JH and Kim HS:
Impact of perioperative blood transfusion on oncologic outcomes in
patients with nonmetastatic renal cell carcinoma treated with
curative nephrectomy: A retrospective analysis of a large,
single-institutional cohort. Investig Clin Urol. 61:136–145. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Nizri E, Kusamura S, Fallabrino G, Guaglio
M, Baratti D and Deraco M: Dose-dependent effect of red blood cells
transfusion on perioperative and long-term outcomes in peritoneal
surface malignancies treated with cytoreduction and HIPEC. Ann Surg
Oncol. 25:3264–3270. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Cata JP, Wang H, Gottumukkala V, Reuben J
and Sessler DI: Inflammatory response, immunosuppression, and
cancer recurrence after perioperative blood transfusions. Br J
Anaesth. 110:690–701. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wu HL, Tai YH, Lin SP, Chan MY, Chen HH
and Chang KY: The impact of blood transfusion on recurrence and
mortality following colorectal cancer resection: A propensity score
analysis of 4,030 patients. Sci Rep. 8:133452018. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Grasso M, Pacella G, Sangiuliano N, De
Palma M and Puzziello A: Gastric cancer surgery: clinical outcomes
and prognosis are influenced by perioperative blood transfusions.
Updates Surg. 71:439–443. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Gunka I, Dostalik J, Martinek L, Gunkova P
and Mazur M: Impact of blood transfusions on survival and
recurrence in colorectal cancer surgery. Indian J Surg. 75:94–101.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Halabi WJ, Jafari MD, Nguyen VQ,
Carmichael JC, Mills S, Pigazzi A and Stamos MJ: Blood transfusions
in colorectal cancer surgery: Incidence, outcomes, and predictive
factors: An American college of surgeons national surgical quality
improvement program analysis. Am J Surg. 206:1024–1033. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Baguena G, Pellino G, Frasson M, Escrig J,
Marinello F, Espí A, García-Granero A, Roselló S, Cervantes A and
García-Granero E: Impact of perioperative transfusions and sepsis
on long-term oncologic outcomes after curative colon cancer
resection. A retrospective analysis of a prospective database.
Gastroenterol Hepatol. 43:63–72. 2020.(In English, Spanish).
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Tarantino I, Ukegjini K, Warschkow R,
Schmied BM, Steffen T, Ulrich A and Müller SA: Blood transfusion
does not adversely affect survival after elective colon cancer
resection: A propensity score analysis. Langenbecks Arch Surg.
398:841–849. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Hunsicker O, Gericke S, Graw JA, Krannich
A, Boemke W, Meyer O, Braicu I, Spies C, Sehouli J, Pruß A and
Feldheiser A: Transfusion of red blood cells does not impact
progression-free and overall survival after surgery for ovarian
cancer. Transfusion. 59:3589–3600. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Zaw AS, Kantharajanna SB, Maharajan K, Tan
B, Vellayappan B and Kumar N: Perioperative blood transfusion: Does
it influence survival and cancer progression in metastatic spine
tumor surgery? Transfusion. 57:440–450. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Chang CC, Lee TC, Su MJ, Lin HC, Cheng FY,
Chen YT, Yen TH and Chu FY: Transfusion-associated adverse
reactions (TAARs) and cytokine accumulations in the stored blood
components: The impact of prestorage versus poststorage
leukoreduction. Oncotarget. 9:4385–4394. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Chalfin HJ, Liu JJ, Gandhi N, Feng Z,
Johnson D, Netto GJ, Drake CG, Hahn NM, Schoenberg MP, Trock BJ, et
al: Blood transfusion is associated with increased perioperative
morbidity and adverse oncologic outcomes in bladder cancer patients
receiving neoadjuvant chemotherapy and radical cystectomy. Ann Surg
Oncol. 23:2715–2722. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Carson JL, Guyatt G, Heddle NM, Grossman
BJ, Cohn CS, Fung MK, Gernsheimer T, Holcomb JB, Kaplan LJ, Katz
LM, et al: Clinical practice guidelines from the AABB: Red blood
cell transfusion thresholds and storage. JAMA. 316:2025–2035. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Alkhalid Y, Lagman C, Sheppard JP, Nguyen
T, Prashant GN, Ziman AF and Yang I: Restrictive transfusion
threshold is safe in high-risk patients undergoing brain tumor
surgery. Clin Neurol Neurosurg. 163:103–107. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Boone JD, Kim KH, Marques M and Straughn
JM: Compliance rates and outcomes associated with a restrictive
transfusion policy in gynecologic oncology patients. Gynecol Oncol.
132:227–230. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Syan-Bhanvadia S, Drangsholt S, Shah S,
Cai J, Miranda G, Djaladat H and Daneshmand S: Restrictive
transfusion in radical cystectomy is safe. Urol Oncol.
35:528.e15–528.e21. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Wehry J, Agle S, Philips P, Cannon R,
Scoggins CR, Puffer L, McMasters KM and Martin RC: Restrictive
blood transfusion protocol in malignant upper gastrointestinal and
pancreatic resections patients reduces blood transfusions with no
increase in patient morbidity. Am J Surg. 210:1197–1205. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Prescott LS, Taylor JS, Lopez-Olivo MA,
Munsell MF, VonVille HM, Lairson DR and Bodurka DC: How low should
we go: A systematic review and meta-analysis of the impact of
restrictive red blood cell transfusion strategies in oncology.
Cancer Treat Rev. 46:1–8. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Ozben V, Stocchi L, Ashburn J, Liu X and
Gorgun E: Impact of a restrictive vs liberal transfusion strategy
on anastomotic leakage and infectious complications after
restorative surgery for rectal cancer. Colorectal Dis. 19:772–780.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Bergamin FS, Almeida JP, Landoni G, Galas
FRBG, Fukushima JT, Fominskiy E, Park CHL, Osawa EA, Diz MPE,
Oliveira GQ, et al: Liberal versus restrictive transfusion strategy
in critically Ill oncologic patients: The transfusion requirements
in critically Ill oncologic patient randomized controlled trial.
Crit Care Med. 45:766–773. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Crawford TM, Andersen CC and Stark MJ:
Effect of repeat transfusion exposure on plasma cytokine and
markers of endothelial activation in the extremely preterm neonate.
Transfusion. 60:2217–2224. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Muszynski JA, Spinella PC, Cholette JM,
Acker JP, Hall MW, Juffermans NP, Kelly DP, Blumberg N, Nicol K,
Liedel J, et al: Transfusion-related immunomodulation: Review of
the literature and implications for pediatric critical illness.
Transfusion. 57:195–206. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Opelz G, Sengar DP, Mickey MR and Terasaki
PI: Effect of blood transfusions on subsequent kidney transplants.
Transplant Proc. 5:253–259. 1973.PubMed/NCBI
|
|
59
|
Carpenter CB: Blood transfusion effects in
kidney transplantation. Yale J Biol Med. 63:435–443.
1990.PubMed/NCBI
|
|
60
|
Abdolmohammadi K, Mahmoudi T,
Jafari-Koshki T, Hassan ZM and Pourfathollah AA: Immunomodulatory
effects of blood transfusion on tumor size, metastasis, and
survival in experimental fibrosarcoma. Indian J Hematol Blood
Transfus. 34:697–702. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Atzil S, Arad M, Glasner A, Abiri N,
Avraham R, Greenfeld K, Rosenne E, Beilin B and Ben-Eliyahu S:
Blood transfusion promotes cancer progression: A critical role for
aged erythrocytes. Anesthesiology. 109:989–997. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Sugita S, Sasaki A, Iwaki K, Uchida H, Kai
S, Shibata K, Ohta M and Kitano S: Prognosis and postoperative
lymphocyte count in patients with hepatocellular carcinoma who
received intraoperative allogenic blood transfusion: A
retrospective study. Eur J Surg Oncol. 34:339–345. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Chen G, Zhang FJ, Gong M and Yan M: Effect
of perioperative autologous versus allogeneic blood transfusion on
the immune system in gastric cancer patients. J Zhejiang Univ Sci
B. 8:560–565. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Tao CJ, Chen YY, Jiang F, Feng XL, Jin QF,
Jin T, Piao YF and Chen XZ: A prognostic model combining CD4/CD8
ratio and N stage predicts the risk of distant metastasis for
patients with nasopharyngeal carcinoma treated by intensity
modulated radiotherapy. Oncotarget. 7:46653–46661. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Sparrow RL: Red blood cell storage and
transfusion-related immunomodulation. Blood Transfus. 8 (Suppl
3):s26–s30. 2010.PubMed/NCBI
|
|
66
|
Clark DA, Gorczynski RM and Blajchman MA:
Transfusion-related immunomodulation due to peripheral blood
dendritic cells expressing the CD200 tolerance signaling molecule
and alloantigen. Transfusion. 48:814–821. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Teicher BA: Transforming growth
factor-beta and the immune response to malignant disease. Clin
Cancer Res. 13:6247–6251. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Pinheiro MK, Tamagne M, Elayeb R, Andrieu
M, Pirenne F and Vingert B: Blood microparticles are a component of
immune modulation in red blood cell transfusion. Eur J Immunol.
50:1237–1240. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Ghio M, Contini P, Ubezio G, Mazzei C,
Puppo F and Indiveri F: Immunomodulatory effects of blood
transfusions: The synergic role of soluble HLA Class I free
heavy-chain molecules detectable in blood components. Transfusion.
48:1591–1597. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Contini P, Ghio M, Poggi A, Filaci G,
Indiveri F, Ferrone S and Puppo F: Soluble HLA-A,-B,-C and -G
molecules induce apoptosis in T and NK CD8+ cells and inhibit
cytotoxic T cell activity through CD8 ligation. Eur J Immunol.
33:125–134. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Ottonello L, Ghio M, Contini P, Bertolotto
M, Bianchi G, Montecucco F, Colonna M, Mazzei C, Dallegri F and
Indiveri F: Nonleukoreduced red blood cell transfusion induces a
sustained inhibition of neutrophil chemotaxis by stimulating in
vivo production of transforming growth factor-beta1 by neutrophils:
Role of the immunoglobulinlike transcript 1, sFasL, and sHLA-I.
Transfusion. 47:1395–1404. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Baumgartner JM, Silliman CC, Moore EE,
Banerjee A and McCarter MD: Stored red blood cell transfusion
induces regulatory T cells. J Am Coll Surg. 208:110–119. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Zhuang Y, Zhang T, Wei C, Pan JC, Wang SF,
Zhang AQ and Wang DQ: Effect of leukoreduction on tumor-associated
cytokine accumutation in supernatant of stored packed red cells and
its effect on tumor cell proliferation in vitro. Zhongguo Shi Yan
Xue Ye Xue Za Zhi. 23:217–221. 2015.(In Chinese). PubMed/NCBI
|
|
74
|
Baumgartner JM, Nydam TL, Clarke JH,
Banerjee A, Silliman CC and McCarter MD: Red blood cell supernatant
potentiates LPS-induced proinflammatory cytokine response from
peripheral blood mononuclear cells. J Interferon Cytokine Res.
29:333–338. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Long K, Meier C, Ward M, Williams D,
Woodward J and Bernard A: Immunologic profiles of red blood cells
using in vitro models of transfusion. J Surg Res. 184:567–571.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Ohue Y and Nishikawa H: Regulatory T
(Treg) cells in cancer: Can Treg cells be a new therapeutic target?
Cancer Sci. 110:2080–2089. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Almizraq RJ, Holovati JL and Acker JP:
Characteristics of extracellular vesicles in red blood concentrates
change with storage time and blood manufacturing method. Transfus
Med Hemother. 45:185–193. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Menocha S and Muszynski JA:
Transfusion-related immune modulation: Functional consequence of
extracellular vesicles? Transfusion. 59:3553–3555. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Almizraq RJ, Seghatchian J and Acker JP:
Extracellular vesicles in transfusion-related immunomodulation and
the role of blood component manufacturing. Transfus Apher Sci.
55:281–291. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Sut C, Tariket S, Chou ML, Garraud O,
Laradi S, Hamzeh-Cognasse H, Seghatchian J, Burnouf T and Cognasse
F: Duration of red blood cell storage and inflammatory marker
generation. Blood Transfus. 15:145–152. 2017.PubMed/NCBI
|
|
81
|
Sadallah S, Eken C and Schifferli JA:
Erythrocyte-derived ectosomes have immunosuppressive properties. J
Leukoc Biol. 84:1316–1325. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Straat M, van Hezel ME, Böing A, Tuip-De
Boer A, Weber N, Nieuwland R, van Bruggen R and Juffermans NP:
Monocyte-mediated activation of endothelial cells occurs only after
binding to extracellular vesicles from red blood cell products, a
process mediated by β-integrin. Transfusion. 56:3012–3020. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Cole SW: Chronic inflammation and breast
cancer recurrence. J Clin Oncol. 27:3418–3419. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Nakagawa K, Sho M, Akahori T, Nagai M,
Nakamura K, Takagi T, Tanaka T, Nishiofuku H, Ohbayashi C,
Kichikawa K and Ikeda N: Significance of the inflammation-based
prognostic score in recurrent pancreatic cancer. Pancreatology.
19:722–728. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Guo D, Zhang J, Jing W, Liu J, Zhu H, Fu
L, Li M, Kong L, Yue J and Yu J: Prognostic value of systemic
immune-inflammation index in patients with advanced non-small-cell
lung cancer. Future Oncol. 14:2643–2650. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Matsubara D, Arita T, Nakanishi M, Kuriu
Y, Murayama Y, Kudou M, Konishi H, Komatsu S, Shiozaki A and Otsuji
E: The impact of postoperative inflammation on recurrence in
patients with colorectal cancer. Int J Clin Oncol. 25:602–613.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Yoshida D, Minami K, Sugiyama M, Ota M,
Ikebe M, Morita M, Matsukuma A and Toh Y: Prognostic impact of the
neutrophil-to-lymphocyte ratio in stage I–II rectal cancer
patients. J Surg Res. 245:281–287. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Acker JP, Almizraq RJ, Millar D and
Maurer-Spurej E: Screening of red blood cells for extracellular
vesicle content as a product quality indicator. Transfusion.
58:2217–2226. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Almizraq RJ, Seghatchian J, Holovati JL
and Acker JP: Extracellular vesicle characteristics in stored red
blood cell concentrates are influenced by the method of detection.
Transfus Apher Sci. 56:254–260. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Donadee C, Raat NJ, Kanias T, Tejero J,
Lee JS, Kelley EE, Zhao X, Liu C, Reynolds H, Azarov I, et al:
Nitric oxide scavenging by red blood cell microparticles and
cell-free hemoglobin as a mechanism for the red cell storage
lesion. Circulation. 124:465–476. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Almizraq RJ, Norris PJ, Inglis H, Menocha
S, Wirtz MR, Juffermans N, Pandey S, Spinella PC, Acker JP and
Muszynski JA: Blood manufacturing methods affect red blood cell
product characteristics and immunomodulatory activity. Blood Adv.
2:2296–2306. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Richter JR, Sutton JM, Hexley P,
Johannigman TA, Lentsch AB and Pritts TA: Leukoreduction of packed
red blood cells attenuates proinflammatory properties of
storage-derived microvesicles. J Surg Res. 223:128–135. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Bicalho B, Pereira AS and Acker JP: Buffy
coat (top/bottom)- and whole-blood filtration (top/top)-produced
red cell concentrates differ in size of extracellular vesicles. Vox
Sang. 109:214–220. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Gamonet C, Desmarets M, Mourey G, Biichle
S, Aupet S, Laheurte C, François A, Resch E, Bigey F, Binda D, et
al: Processing methods and storage duration impact extracellular
vesicle counts in red blood cell units. Blood Adv. 4:5527–5539.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Yoshida T, Prudent M and D'Alessandro A:
Red blood cell storage lesion: Causes and potential clinical
consequences. Blood Transfus. 17:27–52. 2019.PubMed/NCBI
|
|
96
|
Kozlova E, Chernysh A, Moroz V, Kozlov A,
Sergunova V, Sherstyukova E and Gudkova O: Two-step process of
cytoskeletal structural damage during long-term storage of packed
red blood cells. Blood Transfus. 19:124–134. 2021.PubMed/NCBI
|
|
97
|
Kaczmarska M, Grosicki M, Bulat K, Mardyla
M, Szczesny-Malysiak E, Blat A, Dybas J, Sacha T and Marzec KM:
Temporal sequence of the human RBCs' vesiculation observed in
nano-scale with application of AFM and complementary techniques.
Nanomedicine. 28:1022212020. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Bicalho B, Holovati JL and Acker JP:
Phospholipidomics reveals differences in glycerophosphoserine
profiles of hypothermically stored red blood cells and
microvesicles. Biochim Biophys Acta. 1828:317–326. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
McVey MJ, Kuebler WM, Orbach A, Arbell D,
Zelig O, Barshtein G and Yedgar S: Reduced deformability of stored
red blood cells is associated with generation of extracellular
vesicles. Transfus Apher Sci. 59:1028512020. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Burger P, Kostova E, Bloem E,
Hilarius-Stokman P, Meijer AB, van den Berg TK, Verhoeven AJ, de
Korte D and van Bruggen R: Potassium leakage primes stored
erythrocytes for phosphatidylserine exposure and shedding of
pro-coagulant vesicles. Br J Haematol. 160:377–386. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Arashiki N and Takakuwa Y: Maintenance and
regulation of asymmetric phospholipid distribution in human
erythrocyte membranes: Implications for erythrocyte functions. Curr
Opin Hematol. 24:167–172. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Wesseling MC, Wagner-Britz L, Nguyen DB,
Asanidze S, Mutua J, Mohamed N, Hanf B, Ghashghaeinia M, Kaestner L
and Bernhardt I: Novel insights in the regulation of
phosphatidylserine exposure in human red blood cells. Cell Physiol
Biochem. 39:1941–1954. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Nguyen DB, Wagner-Britz L, Maia S, Steffen
P, Wagner C, Kaestner L and Bernhardt I: Regulation of
phosphatidylserine exposure in red blood cells. Cell Physiol
Biochem. 28:847–856. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Tanaka Y and Schroit AJ: Insertion of
fluorescent phosphatidylserine into the plasma membrane of red
blood cells. Recognition by autologous macrophages. J Biol Chem.
258:11335–11343. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Orbach A, Zelig O, Yedgar S and Barshtein
G: Biophysical and biochemical markers of red blood cell fragility.
Transfus Med Hemother. 44:183–187. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Sudnitsyna J, Skverchinskaya E, Dobrylko
I, Nikitina E, Gambaryan S and Mindukshev I: Microvesicle formation
induced by oxidative stress in human erythrocytes. Antioxidants
(Basel). 9:9292020. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Prudent M, Delobel J, Hübner A, Benay C,
Lion N and Tissot JD: Proteomics of stored red blood cell membrane
and storage-induced microvesicles reveals the association of
flotillin-2 with band 3 complexes. Front Physiol. 9:4212018.
View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Willekens FL, Werre JM, Groenen-Döpp YA,
Roerdinkholder-Stoelwinder B, de Pauw B and Bosman GJ: Erythrocyte
vesiculation: A self-protective mechanism? Br J Haematol.
141:549–556. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Tissot JD, Rubin O and Canellini G:
Analysis and clinical relevance of microparticles from red blood
cells. Curr Opin Hematol. 17:571–577. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Wagner-Britz L, Wang J, Kaestner L and
Bernhardt I: Protein kinase Cα and P-type Ca channel CaV2.1 in red
blood cell calcium signalling. Cell Physiol Biochem. 31:883–891.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Cloos AS, Ghodsi M, Stommen A, Vanderroost
J, Dauguet N, Pollet H, D'Auria L, Mignolet E, Larondelle Y,
Terrasi R, et al: Interplay between plasma membrane lipid
alteration, oxidative stress and calcium-based mechanism for
extracellular vesicle biogenesis from erythrocytes during blood
storage. Front Physiol. 11:7122020. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Shao H, Im H, Castro CM, Breakefield X,
Weissleder R and Lee H: New technologies for analysis of
extracellular vesicles. Chem Rev. 118:1917–1950. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Nguyen DB, Ly TB, Wesseling MC, Hittinger
M, Torge A, Devitt A, Perrie Y and Bernhardt I: Characterization of
microvesicles released from human red blood cells. Cell Physiol
Biochem. 38:1085–1099. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Noubouossie DF, Henderson MW, Mooberry M,
Ilich A, Ellsworth P, Piegore M, Skinner SC, Pawlinski R, Welsby I,
Renné T, et al: Red blood cell microvesicles activate the contact
system, leading to factor IX activation via 2 independent pathways.
Blood. 135:755–765. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
van der Pol E, Coumans F, Varga Z, Krumrey
M and Nieuwland R: Innovation in detection of microparticles and
exosomes. J Thromb Haemost. 11 (Suppl 1):S36–S45. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Lawrie AS, Albanyan A, Cardigan RA, Mackie
IJ and Harrison P: Microparticle sizing by dynamic light scattering
in fresh-frozen plasma. Vox Sang. 96:206–212. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Théry C, Witwer KW, Aikawa E, Alcaraz MJ,
Anderson JD, Andriantsitohaina R, Antoniou A, Arab T, Archer F,
Atkin-Smith GK, et al: Minimal information for studies of
extracellular vesicles 2018 (MISEV2018): A position statement of
the international society for extracellular vesicles and update of
the MISEV2014 guidelines. J Extracell Vesicles. 7:15357502018.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Muszynski JA, Bale J, Nateri J, Nicol K,
Wang Y, Wright V, Marsh CB, Gavrilin MA, Sarkar A, Wewers MD and
Hall MW: Supernatants from stored red blood cell (RBC) units, but
not RBC-derived microvesicles, suppress monocyte function in vitro.
Transfusion. 55:1937–1945. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Turpin D, Truchetet ME, Faustin B, Augusto
JF, Contin-Bordes C, Brisson A, Blanco P and Duffau P: Role of
extracellular vesicles in autoimmune diseases. Autoimmun Rev.
15:174–183. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Vasconcelos MH, Caires HR, Ābols A, Xavier
CPR and Linē A: Extracellular vesicles as a novel source of
biomarkers in liquid biopsies for monitoring cancer progression and
drug resistance. Drug Resist Updat. 47:1006472019. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Naito Y, Yoshioka Y, Yamamoto Y and Ochiya
T: How cancer cells dictate their microenvironment: Present roles
of extracellular vesicles. Cell Mol Life Sci. 74:697–713. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Zecher D, Cumpelik A and Schifferli JA:
Erythrocyte-derived microvesicles amplify systemic inflammation by
thrombin-dependent activation of complement. Arterioscler Thromb
Vasc Biol. 34:313–320. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Liu C, Zhao W, Christ GJ, Gladwin MT and
Kim-Shapiro DB: Nitric oxide scavenging by red cell microparticles.
Free Radic Biol Med. 65:1164–1173. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Kim-Shapiro DB, Lee J and Gladwin MT:
Storage lesion: Role of red blood cell breakdown. Transfusion.
51:844–851. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Said AS and Doctor A: Influence of red
blood cell-derived microparticles upon vasoregulation. Blood
Transfus. 15:522–534. 2017.PubMed/NCBI
|
|
126
|
Kamm A, Przychodzen P, Kuban-Jankowska A,
Jacewicz D, Dabrowska AM, Nussberger S, Wozniak M and
Gorska-Ponikowska M: Nitric oxide and its derivatives in the cancer
battlefield. Nitric Oxide. 93:102–114. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Oliveira GP Jr, Zigon E, Rogers G,
Davodian D, Lu S, Jovanovic-Talisman T, Jones J, Tigges J, Tyagi S
and Ghiran IC: Detection of extracellular vesicle RNA using
molecular beacons. iScience. 23:1007822020. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Miyashita Y, Ishikawa K, Fukushima Y,
Kouwaki T, Nakamura K and Oshiumi H: Immune-regulatory microRNA
expression levels within circulating extracellular vesicles
correspond with the appearance of local symptoms after seasonal flu
vaccination. PLoS One. 14:e02195102019. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Okamoto M, Fukushima Y, Kouwaki T, Daito
T, Kohara M, Kida H and Oshiumi H: MicroRNA-451a in extracellular,
blood-resident vesicles attenuates macrophage and dendritic cell
responses to influenza whole-virus vaccine. J Biol Chem.
293:18585–18600. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Liu Z, Miao T, Feng T, Jiang Z, Li M, Zhou
L and Li H: miR-451a inhibited cell proliferation and enhanced
tamoxifen sensitive in breast cancer via macrophage migration
inhibitory factor. Biomed Res Int. 2015:2076842015.PubMed/NCBI
|
|
131
|
Yamada Y, Arai T, Sugawara S, Okato A,
Kato M, Kojima S, Yamazaki K, Naya Y, Ichikawa T and Seki N: Impact
of novel oncogenic pathways regulated by antitumor miR-451a in
renal cell carcinoma. Cancer Sci. 109:1239–1253. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Nobre CC, de Araújo JM, Fernandes TA,
Cobucci RN, Lanza DC, Andrade VS and Fernandes JV: Macrophage
migration inhibitory factor (MIF): Biological activities and
relation with cancer. Pathol Oncol Res. 23:235–244. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Almizraq RJ, Kipkeu BJ and Acker JP:
Platelet vesicles are potent inflammatory mediators in red blood
cell products and washing reduces the inflammatory phenotype.
Transfusion. 60:378–390. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Nelson KA, Aldea GS, Warner P, Latchman Y,
Gunasekera D, Tamir A, Gernsheimer T, Bolgiano D and Slichter SJ:
Transfusion-related immunomodulation: Gamma irradiation alters the
effects of leukoreduction on alloimmunization. Transfusion.
59:3396–3404. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Sanchez R, Lee TH, Wen L, Montalvo L,
Schechterly C, Colvin C, Alter HJ, Luban NL and Busch MP: Absence
of transfusion-associated microchimerism in pediatric and adult
recipients of leukoreduced and gamma-irradiated blood components.
Transfusion. 52:936–945. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Bohlius J, Bohlke K, Castelli R,
Djulbegovic B, Lustberg MB, Martino M, Mountzios G, Peswani N,
Porter L, Tanaka TN, et al: Management of cancer-associated anemia
with erythropoiesis-stimulating agents: ASCO/ASH clinical practice
guideline update. Blood Adv. 3:1197–1210. 2019. View Article : Google Scholar : PubMed/NCBI
|