|
1
|
Carey L, Winer E, Viale G, Cameron D and Gianni L: Triple-negative breast cancer: Disease entity or title of convenience? Nat Rev Clin Oncol. 7:683–692. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gluz O, Liedtke C, Gottschalk N, Pusztai L, Nitz U and Harbeck N: Triple-negative breast cancer-current status and future directions. Ann Oncol. 20:1913–1927. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sharma S, Barry M, Gallagher DJ, Kell M and Sacchini V: An overview of triple negative breast cancer for surgical oncologists. Surg Oncol. 24:276–283. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vagia E, Mahalingam D and Cristofanilli M: The landscape of targeted therapies in TNBC. Cancers (Basel). 12:9162020. View Article : Google Scholar
|
|
5
|
Farkona S, Diamandis EP and Blasutig IM: Cancer immunotherapy: The beginning of the end of cancer? BMC Med. 14:732016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jia H, Truica CI, Wang B, Wang Y, Ren X, Harvey HA, Song J and Yang JM: Immunotherapy for triple-negative breast cancer: Existing challenges and exciting prospects. Drug Resist Updat. 32:1–15. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kurozumi S, Fujii T, Matsumoto H, Inoue K, Kurosumi M, Horiguchi J and Kuwano H: Significance of evaluating tumor-infiltrating lymphocytes (TILs) and programmed cell death-ligand 1 (PD-L1) expression in breast cancer. Med Mol Morphol. 50:185–194. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li Z, Qiu Y, Lu W, Jiang Y and Wang J: Immunotherapeutic interventions of triple negative breast cancer. J Transl Med. 16:1472018. View Article : Google Scholar : PubMed/NCBI
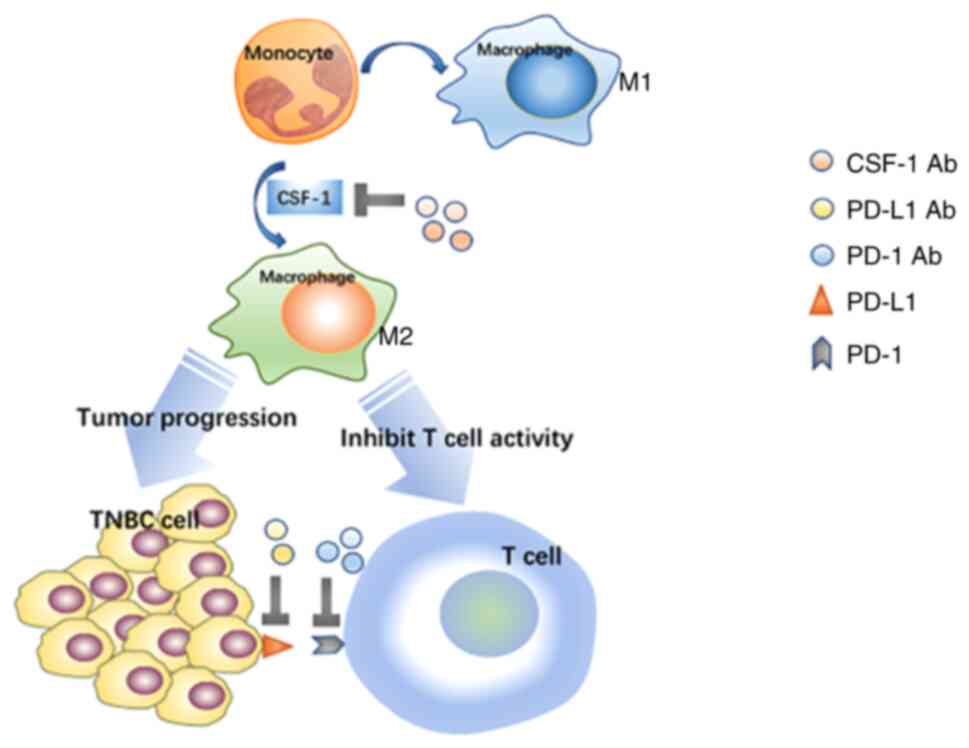
|
|
9
|
Tomioka N, Azuma M, Ikarashi M, Yamamoto M, Sato M, Watanabe KI, Yamashiro K and Takahashi M: The therapeutic candidate for immune checkpoint inhibitors elucidated by the status of tumor-infiltrating lymphocytes (TILs) and programmed death ligand 1 (PD-L1) expression in triple negative breast cancer (TNBC). Breast Cancer. 25:34–42. 2018. View Article : Google Scholar
|
|
10
|
Meléndez B, Van Campenhout C, Rorive S, Remmelink M, Salmon I and D'Haene N: Methods of measurement for tumor mutational burden in tumor tissue. Transl Lung Cancer Res. 7:661–667. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chalmers ZR, Connelly CF, Fabr izio D, Gay L, Ali SM, Ennis R, Schrock A, Campbell B, Shlien A, Chmielecki J, et al: Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9:342017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chan TA, Yarchoan M, Jaffee E, Swanton C, Quezada SA, Stenzinger A and Peters S: Development of tumor mutation burden as an immunotherapy biomarker: Utility for the oncology clinic. Ann Oncol. 30:44–56. 2019. View Article : Google Scholar :
|
|
13
|
Alva AS, Mangat PK, Garrett-Mayer E, Halabi S, Hansra D, Calfa CJ, Khalil MF, Ahn ER, Cannon TL, Crilley P, et al: Pembrolizumab in patients with metastatic breast cancer with high tumor mutational Burden: Results from the targeted agent and profiling utilization registry (TAPUR) study. J Clin Oncol. 39:2443–2451. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bertucci F, Ng CKY, Patsouris A, Droin N, Piscuoglio S, Carbuccia N, Soria JC, Dien AT, Adnani Y, Kamal M, et al: Genomic characterization of metastatic breast cancers. Nature. 569:560–564. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Haricharan S, Bainbridge MN, Scheet P and Brown PH: Somatic mutation load of estrogen receptor-positive breast tumors predicts overall survival: An analysis of genome sequence data. Breast Cancer Res Treat. 146:211–220. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
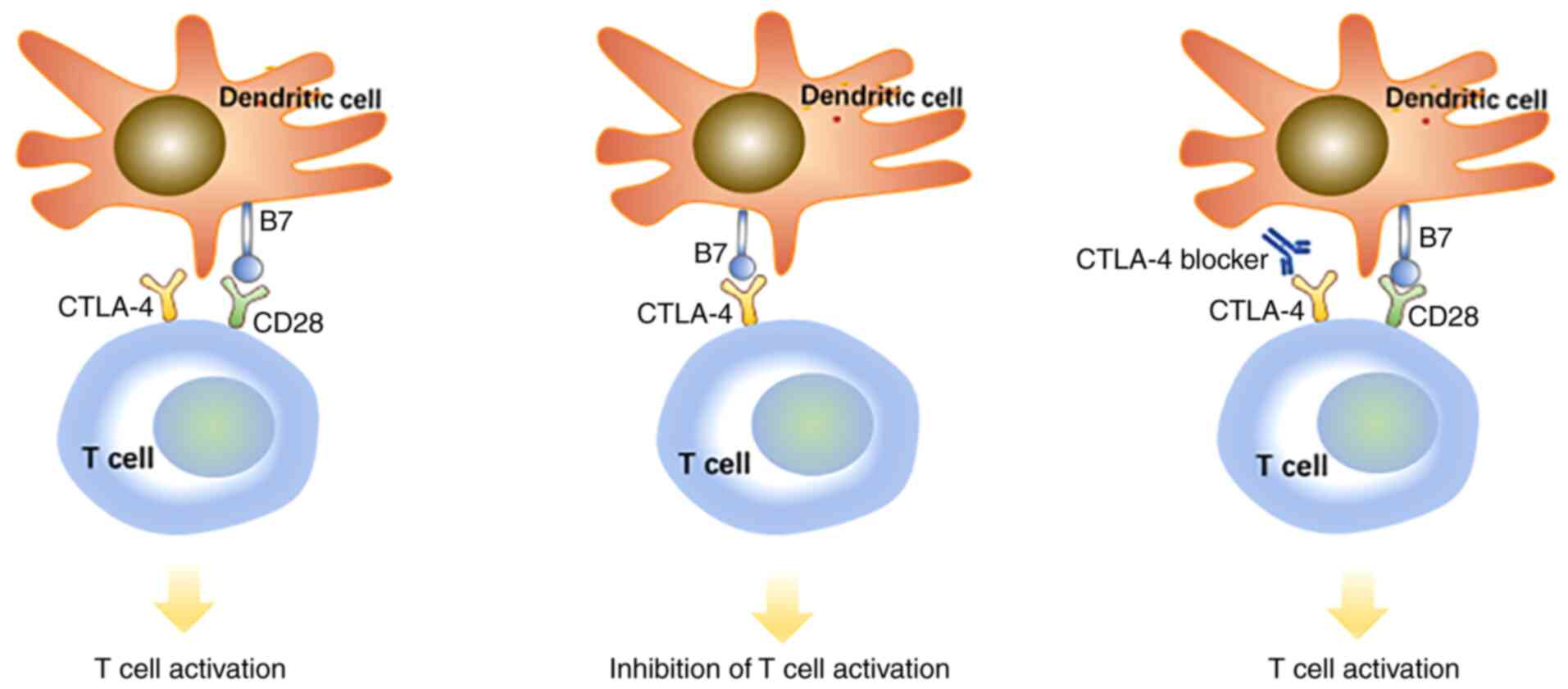
Shah SP, Roth A, Goya R, Oloumi A, Ha G, Zhao Y, Turashvili G, Ding J, Tse K, Haffari G, et al: The clonal and mutational evolution spectrum of primary triple-negative breast cancers. Nature. 486:395–399. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Barroso-Sousa R, Jain E, Cohen O, Kim D, Buendia-Buendia J, Winer E, Lin N, Tolaney SM, Wagle N, et al: Prevalence and mutational determinants of high tumor mutation burden in breast cancer. Ann Oncol. 31:387–394. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Huang RSP, Haberberger J, McGregor K, Mata DA, Decker B, Hiemenz MC, Lechpammer M, Danziger N, Schiavone K, Creeden J, et al: Clinicopathologic and genomic landscape of breast carcinoma brain metastases. Oncologist. 26:835–844. 2021. View Article : Google Scholar : PubMed/NCBI
|
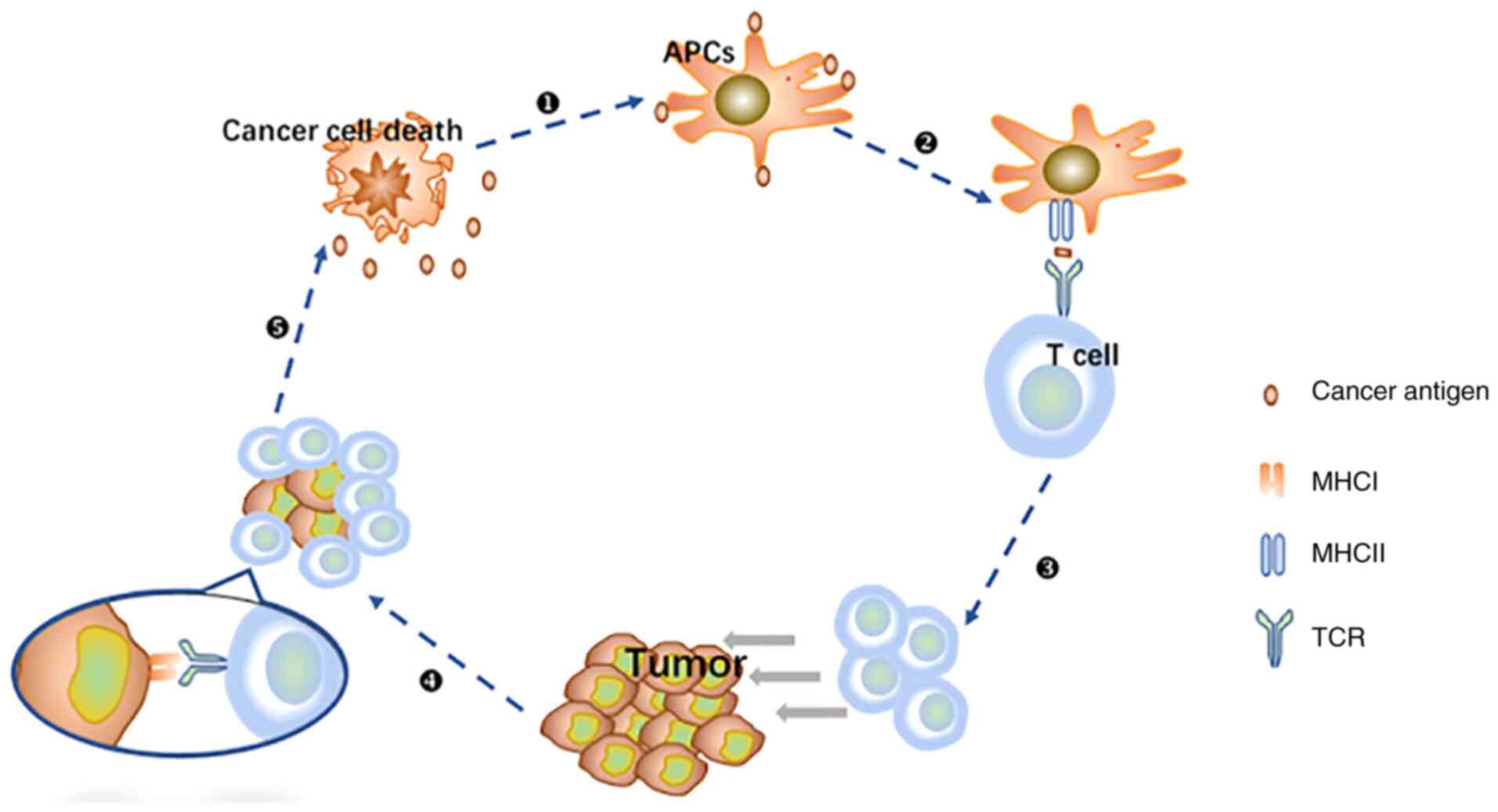
|
19
|
Cortes J, Cescon DW, Rugo HS, Nowecki Z, Im SA, Yusof MM, Gallardo C, Lipatov O, Barrios CH, Holgado E, et al: Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): A randomised, placebo-controlled, double-blind, phase 3 clinical trial. Lancet. 396:1817–1828. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Schmid P, Rugo HS, Adams S, Schneeweiss A, Barrios CH, Iwata H, Diéras V, Henschel V, Molinero L, Chui SY, et al: Atezolizumab plus nab-paclitaxel as first-line treatment for unresectable, locally advanced or metastatic triple-negative breast cancer (IMpassion130): Updated efficacy results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 21:44–59. 2020. View Article : Google Scholar
|
|
21
|
Adams S, Loi S, Toppmeyer D, Cescon DW, De Laurentiis M, Nanda R, Winer EP, Mukai H, Tamura K, Armstrong A, et al: Pembrolizumab monotherapy for previously untreated, PD-L1-positive, metastatic triple-negative breast cancer: Cohort B of the phase II KEYNOTE-086 study. Ann Oncol. 30:405–411. 2019. View Article : Google Scholar
|
|
22
|
Hutchinson KE, Yost SE, Chang CW, Johnson RM, Carr AR, McAdam PR, Halligan DL, Chang CC, Schmolze D, Liang J and Yuan Y: Comprehensive profiling of poor-risk paired primary and recurrent triple-negative breast cancers reveals immune phenotype shifts. Clin Cancer Res. 26:657–668. 2020. View Article : Google Scholar
|
|
23
|
Guo S and Deng CX: Effect of stromal cells in tumor microenvironment on metastasis initiation. Int J Biol Sci. 14:2083–2093. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chen F, Zhuang X, Lin L, Yu P, Wang Y, Shi Y, Hu G and Sun Y: New horizons in tumor microenvironment biology: Challenges and opportunities. BMC Med. 13:452015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Paijens ST, Vledder A, de Bruyn M and Nijman HW: Tumor-infiltrating lymphocytes in the immunotherapy era. Cell Mol Immunol. 18:842–859. 2021. View Article : Google Scholar :
|
|
26
|
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, Martino S, Wang M, Jones VE, Saphner TJ, et al: Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol. 32:2959–2966. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Blackley EF and Loi S: Targeting immune pathways in breast cancer: Review of the prognostic utility of TILs in early stage triple negative breast cancer (TNBC). Breast. 48(Suppl 1): S44–S48. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Denkert C, Liedtke C, Tutt A and von Minckwitz G: Molecular alterations in triple-negative breast cancer-the road to new treatment strategies. Lancet. 389:2430–2442. 2017. View Article : Google Scholar
|
|
29
|
Mahmoud SM, Paish EC, Powe DG, Macmillan RD, Grainge MJ, Lee AH, Ellis IO and Green AR: Tumor-infiltrating CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin Oncol. 29:1949–1955. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Pruneri G, Vingiani A, Bagnardi V, Rotmensz N, De Rose A, Palazzo A, Colleoni AM, Goldhirsch A and Viale G: Clinical validity of tumor-infiltrating lymphocytes analysis in patients with triple-negative breast cancer. Ann Oncol. 27:249–256. 2016. View Article : Google Scholar
|
|
31
|
Stanton SE and Disis ML: Clinical significance of tumor-infiltrating lymphocytes in breast cancer. J Immunother Cancer. 4:592016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Denkert C, von Minckwitz G, Brase JC, Sinn BV, Gade S, Kronenwett R, Pfitzner BM, Salat C, Loi S, Schmitt WD, et al: Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol. 33:983–991. 2015. View Article : Google Scholar
|
|
33
|
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, Rouas G, Francis P, Crown JP, Hitre E, et al: Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol. 31:860–867. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Stanton SE, Adams S and Disis ML: Variation in the incidence and magnitude of tumor-infiltrating lymphocytes in breast cancer subtypes: A systematic review. JAMA Oncol. 2:1354–1360. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Dieci MV, Mathieu MC, Guarneri V, Conte P, Delaloge S, Andre F and Goubar A: Prognostic and predictive value of tumor-infiltrating lymphocytes in two phase III randomized adjuvant breast cancer trials. Ann Oncol. 26:1698–1704. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Denkert C, von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, Budczies J, Huober J, Klauschen F, Furlanetto J, et al: Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: A pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 19:40–50. 2018. View Article : Google Scholar
|
|
37
|
Czystowska M, Han J, Szczepanski MJ, Szajnik M, Quadrini K, Brandwein H, Hadden JW, Signorelli K and Whiteside TL: IRX-2, a novel immunotherapeutic, protects human T cells from tumor-induced cell death. Cell Death Differ. 16:708–718. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Page DB, Pucilowska J, Sanchez KG, Conrad VK, Conlin AK, Acheson AK, Perlewitz KS, Imatani JH, Aliabadi-Wahle S, Moxon N, et al: A phase Ib study of preoperative, locoregional IRX-2 cytokine immunotherapy to prime immune responses in patients with early-stage breast cancer. Clin Cancer Res. 26:1595–1605. 2020. View Article : Google Scholar
|
|
39
|
Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S, Gordon S, Hamilton JA, Ivashkiv LB, Lawrence T, et al: Macrophage activation and polarization: Nomenclature and experimental guidelines. Immunity. 41:14–20. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Vitale I, Manic G, Coussens LM, Kroemer G and Galluzzi L: Macrophages and metabolism in the tumor microenvironment. Cell Metab. 30:36–50. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Pixley FJ and Stanley ER: CSF-1 regulation of the wandering macrophage: Complexity in action. Trends Cell Biol. 14:628–638. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Hume DA and MacDonald KP: Therapeutic applications of macrophage colony-stimulating factor-1 (CSF-1) and antagonists of CSF-1 receptor (CSF-1R) signaling. Blood. 119:1810–1820. 2012. View Article : Google Scholar
|
|
43
|
Wei S, Lightwood D, Ladyman H, Cross S, Neale H, Griffiths M, Adams R, Marshall D, Lawson A, McKnight AJ and Stanley ER: Modulation of CSF-1-regulated post-natal development with anti-CSF-1 antibody. Immunobiology. 210:109–119. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Lin W, Xu D, Austin CD, Caplazi P, Senger K, Sun Y, Jeet S, Young J, Delarosa D, Suto E, et al: Function of CSF1 and IL34 in macrophage homeostasis, inflammation, and cancer. Front Immunol. 10:20192019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Autio KA, Klebanoff CA, Schaer D, Kauh JSW, Slovin SF, Adamow M, Blinder VS, Brahmachary M, Carlsen M, Comen E, et al: Immunomodulatory activity of a colony-stimulating factor-1 receptor inhibitor in patients with advanced refractory breast or prostate cancer: A phase I study. Clin Cancer Res. 26:5609–5620. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Peranzoni E, Lemoine J, Vimeux L, Feuillet V, Barrin S, Kantari-Mimoun C, Bercovici N, Guérin M, Biton J, Ouakrim H, et al: Macrophages impede CD8 T cells from reaching tumor cells and limit the efficacy of anti-PD-1 treatment. Proc Natl Acad Sci USA. 115:E4041–E4050. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
U.S. National Library of Medicine: Cabiralizumab in Combination With Nivolumab and Neoadjuvant Chemotherapy in Patients With Localized Triple-negative Breast Cancer. ClinicalTrials.gov Identifier: NCT04331067. April 02, 2020. https://clinicaltrials.gov/.
|
|
48
|
Zheng H, Siddharth S, Parida S, Wu X and Sharma D: Tumor microenvironment: Key players in triple negative breast cancer immunomodulation. Cancers (Basel). 13:33572021. View Article : Google Scholar
|
|
49
|
Gruosso T, Gigoux M, Manem VSK, Bertos N, Zuo D, Perlitch I, Saleh SMI, Zhao H, Souleimanova M, Johnson RM, et al: Spatially distinct tumor immune microenvironments stratify triple-negative breast cancers. J Clin Invest. 129:1785–1800. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Pardoll DM: The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 12:252–264. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Gubin MM, Zhang X, Schuster H, Caron E, Ward JP, Noguchi T, Ivanova Y, Hundal J, Arthur CD, Krebber WJ, et al: Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature. 515:577–581. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yang Y: Cancer immunotherapy: Harnessing the immune system to battle cancer. J Clin Invest. 125:3335–3337. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Tarantino P, Gandini S, Trapani D, Criscitiello C and Curigliano G: Immunotherapy addition to neoadjuvant chemotherapy for early triple negative breast cancer: A systematic review and meta-analysis of randomized clinical trials. Crit Rev Oncol Hematol. 159:1032232021. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Li Y, Li F, Jiang F, Lv X, Zhang R, Lu A and Zhang G: A mini-review for cancer immunotherapy: Molecular understanding of PD-1/PD-L1 pathway & translational blockade of immune Checkpoints. Int J Mol Sci. 17:11512016. View Article : Google Scholar :
|
|
55
|
Zak KM, Grudnik P, Magiera K, Dömling A, Dubin G and Holak TA: Structural biology of the immune checkpoint receptor PD-1 and its ligands PD-L1/PD-L2. Structure. 25:1163–1174. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Zhang J, Dang F, Ren J and Wei W: Biochemical Aspects of PD-L1 regulation in cancer immunotherapy. Trends Biochem Sci. 43:1014–1032. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Jiang Y, Chen M, Nie H and Yuan Y: PD-1 and PD-L1 in cancer immunotherapy: Clinical implications and future considerations. Hum Vaccin Immunother. 15:1111–1122. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Sun S, Fei X, Mao Y, Wang X, Garfield DH, Huang O, Wang J, Yuan F, Sun L, Yu Q, et al: PD-1(+) immune cell infiltration inversely correlates with survival of operable breast cancer patients. Cancer Immunol Immunother. 63:395–406. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Mittendorf EA, Philips AV, Meric-Bernstam F, Qiao N, Wu Y, Harrington S, Su X, Wang Y, Gonzalez-Angulo AM, Akcakanat A, et al: PD-L1 expression in triple-negative breast cancer. Cancer Immunol Res. 2:361–370. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Son S, Shin S, Rao NV, Um W, Jeon J, Ko H, Deepagan VG, Kwon S, Lee JY and Park JH: Anti-Trop2 antibody-conjugated bioreducible nanoparticles for targeted triple negative breast cancer therapy. Int J Biol Macromol. 110:406–415. 2018. View Article : Google Scholar
|
|
61
|
Meng Q, Meng J, Ran W, Wang J, Zhai Y, Zhang P and Li Y: Light-activated core-shell nanoparticles for spatiotemporally specific treatment of metastatic triple-negative breast cancer. ACS Nano. 12:2789–2802. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Nanda R, Chow LQ, Dees EC, Berger R, Gupta S, Geva R, Pusztai L, Pathiraja K, Aktan G, Cheng JD, et al: Pembrolizumab in patients with advanced triple-negative breast cancer: Phase Ib KEYNOTE-012 study. J Clin Oncol. 34:2460–2467. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Winer EP, Lipatov O, Im SA, Goncalves A, Muñoz-Couselo E, Lee KS, Schmid P, Tamura K, Testa L, Witzel I, et al: Pembrolizumab versus investigator-choice chemotherapy for metastatic triple-negative breast cancer (KEYNOTE-119): A randomised, open-label, phase 3 trial. Lancet Oncol. 22:499–511. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Emens LA, Cruz C, Eder JP, Braiteh F, Chung C, Tolaney SM, Kuter I, Nanda R, Cassier PA, Delord JP, et al: Long-term clinical outcomes and biomarker analyses of atezolizumab therapy for patients with metastatic triple-negative breast cancer: A phase 1 study. JAMA Oncol. 5:74–82. 2019. View Article : Google Scholar :
|
|
65
|
Ali MA, Aiman W, Shah SS, Hussain M and Kashyap R: Efficacy and safety of pembrolizumab based therapies in triple-negative breast cancer: A systematic review of clinical trials. Crit Rev Oncol Hematol. 157:1031972021. View Article : Google Scholar
|
|
66
|
Schmid P, Salgado R, Park YH, Muñoz-Couselo E, Kim SB, Sohn J, Im SA, Foukakis T, Kuemmel S, Dent R, et al: Pembrolizumab plus chemotherapy as neoadjuvant treatment of high-risk, early-stage triple-negative breast cancer: Results from the phase 1b open-label, multicohort KEYNOTE-173 study. Ann Oncol. 31:569–581. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Nanda R, Liu MC, Yau C, Shatsky R, Pusztai L, Wallace A, Chien AJ, Forero-Torres A, Ellis E, Han H, et al: Effect of pembrolizumab plus neoadjuvant chemotherapy on pathologic complete response in women with early-stage breast cancer: An analysis of the ongoing phase 2 adaptively randomized I-SPY2 trial. JAMA Oncol. 6:676–684. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Cetin B and Gumusay O: Pembrolizumab for early triple-negative breast cancer. N Engl J Med. 382:e1082020. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Sang M, Han L, Luo R, Qu W, Zheng F, Zhang K, Liu F, Xue J, Liu W, Feng F, et al: CD44 targeted redox-triggered self-assembly with magnetic enhanced EPR effects for effective amplification of gambogic acid to treat triple-negative breast cancer. Biomater Sci. 8:212–223. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Schmid P, Cortes J, Dent R, Pusztai L, McArthur H, Kümmel S, Bergh J, Denkert C, Park YH, Hui R, et al: Event-free survival with pembrolizumab in early triple-negative breast cancer. N Engl J Med. 386:556–567. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Adams S, Diéras V, Barrios CH, Winer EP, Schneeweiss A, Iwata H, Loi S, Patel S, Henschel V, Chui SY, et al: Patient-reported outcomes from the phase III IMpassion130 trial of atezolizumab plus nab-paclitaxel in metastatic triple-negative breast cancer. Ann Oncol. 31:582–589. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Gianni L, Huang CS, Egle D, Bermejo B, Zamagni C, Thill M, Anton A, Zambelli S, Bianchini G and Russo S: Pathologic complete response (pCR) to neoadjuvant treatment with or without atezolizumab in triple negative, early high-risk and locally advanced breast cancer. NeoTRIPaPDL1 Michelangelo randomized study. Ann Oncol. 33:534–543. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, Diéras V, Hegg R, Im SA, Shaw Wright G, et al: Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 379:2108–2121. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Miles D, Gligorov J, André F, Cameron D, Schneeweiss A, Barrios C, Xu B, Wardley A, Kaen D, Andrade L, et al: Primary results from IMpassion131, a double-blind, placebo-controlled, randomised phase III trial of first-line paclitaxel with or without atezolizumab for unresectable locally advanced/metastatic triple-negative breast cancer. Ann Oncol. 32:994–1004. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Dameri M, Ferrando L, Cirmena G, Vernieri C, Pruneri G, Ballestrero A and Zoppoli G: Multi-gene testing overview with a clinical perspective in metastatic triple-negative breast cancer. Int J Mol Sci. 22:71542021. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Mittendorf EA, Zhang H, Barrios CH, Saji S, Jung KH, Hegg R, Koehler A, Sohn J, Iwata H, Telli ML, et al: Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): A randomised, double-blind, phase 3 trial. Lancet. 396:1090–1100. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Loibl S, Untch M, Burchardi N, Huober J, Sinn BV, Blohmer JU, Grischke EM, Furlanetto J, Tesch H, Hanusch C, et al: A randomised phase II study investigating durvalumab in addition to an anthracycline taxane-based neoadjuvant therapy in early triple-negative breast cancer: Clinical results and biomarker analysis of GeparNuevo study. Ann Oncol. 30:1279–1288. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Leach DR, Krummel MF and Allison JP: Enhancement of antitumor immunity by CTLA-4 blockade. Science. 271:1734–1736. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Allison JP: Immune checkpoint blockade in cancer therapy: The 2015 Lasker-DeBakey clinical medical research award. JAMA. 314:1113–1114. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Peggs KS, Quezada SA, Korman AJ and Allison JP: Principles and use of anti-CTLA4 antibody in human cancer immunotherapy. Curr Opin Immunol. 18:206–213. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Fife BT and Bluestone JA: Control of peripheral T-cell tolerance and autoimmunity via the CTLA-4 and PD-1 pathways. Immunol Rev. 224:166–182. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T, Miyara M, Fehervari Z, Nomura T and Sakaguchi S: CTLA-4 control over Foxp3+ regulatory T cell function. Science. 322:271–275. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Nobel Prizes 2018. Angew Chem Int Ed Engl. 57:146832018. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Chen LQ, Zhang ZM, Huang W, Gao ZG, Fang WS, Jin MJ and Yu L: Inhibiting the proliferation, migration and invasion of triple negative breast cancer cells through anti-tumor human serum albumin nanoparticles loading aziditaxel as a novel taxane derivative. Pharmazie. 72:152–160. 2017.
|
|
85
|
Kern R and Panis C: CTLA-4 expression and its clinical significance in breast cancer. Arch Immunol Ther Exp (Warsz). 69:162021. View Article : Google Scholar
|
|
86
|
Peng Z, Su P, Yang Y, Yao X, Zhang Y, Jin F and Yang B: Identification f CTLA-4 associated with tumor microenvironment and competing interactions in triple negative breast cancer by co-expression network analysis. J Cancer. 11:6365–6375. 2020. View Article : Google Scholar :
|
|
87
|
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, Schadendorf D, Dummer R, Smylie M, Rutkowski P, et al: Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 373:23–34. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Gourd E: Nivolumab plus ipilimumab in metastatic colorectal cancer. Lancet Oncol. 19:e1392018. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Weber J, Mandala M, Del Vecchio M, Gogas HJ, Arance AM, Cowey CL, Dalle S, Schenker M, Chiarion-Sileni V, Marquez-Rodas I, et al: Adjuvant nivolumab versus ipilimumab in resected stage III or IV melanoma. N Engl J Med. 377:1824–1835. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Chen DS and Mellman I: Oncology meets immunology: The cancer-immunity cycle. Immunity. 39:1–10. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Garg AD, More S, Rufo N, Mece O, Sassano ML, Agostinis P, Zitvogel L, Kroemer G and Galluzzi L: Trial watch: Immunogenic cell death induction by anticancer chemotherapeutics. Oncoimmunology. 6:e13868292017. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Bezu L, Gomes-de-Silva LC, Dewitte H, Breckpot K, Fucikova J, Spisek R, Galluzzi L, Kepp O and Kroemer G: Combinatorial strategies for the induction of immunogenic cell death. Front Immunol. 6:1872015.PubMed/NCBI
|
|
93
|
Hanoteau A and Moser M: Chemotherapy and immunotherapy: A close interplay to fight cancer? Oncoimmunology. 5:e11900612016. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Chow MT, Sceneay J, Paget C, Wong CS, Duret H, Tschopp J, Möller A and Smyth MJ: NLRP3 suppresses NK cell-mediated responses to carcinogen-induced tumors and metastases. Cancer Res. 72:5721–5732. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Kershaw MH, Jackson JT, Haynes NM, Teng MW, Moeller M, Hayakawa Y, Street SE, Cameron R, Tanner JE, Trapani JA, et al: Gene-engineered T cells as a superior adjuvant therapy for metastatic cancer. J Immunol. 173:2143–2150. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Gao M, Wang T, Ji L, Bai S, Tian L and Song H: Therapy with carboplatin and Anti-PD-1 antibodies before surgery demonstrates sustainable anti-tumor effects for secondary cancers in mice with triple-negative breast cancer. Front Immunol. 11:3662020. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Wu FTH, Xu P, Chow A, Man S, Krüger J, Khan KA, Paez-Ribes M, Pham E and Kerbel RS: Pre- and post-operative anti-PD-L1 plus anti-angiogenic therapies in mouse breast or renal cancer models of micro- or macro-metastatic disease. Br J Cancer. 120:196–206. 2019. View Article : Google Scholar :
|
|
98
|
Sternschuss M, Yerushalmi R, Saleh RR, Amir E and Goldvaser H: Efficacy and safety of neoadjuvant immune checkpoint inhibitors in early-stage triple-negative breast cancer: A systematic review and meta-analysis. J Cancer Res Clin Oncol. 147:3369–3379. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Bommareddy PK, Shettigar M and Kaufman HL: Integrating oncolytic viruses in combination cancer immunotherapy. Nat Rev Immunol. 18:498–513. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Kaufman HL, Kohlhapp FJ and Zloza A: Oncolytic viruses: A new class of immunotherapy drugs. Nat Rev Drug Discov. 14:642–662. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Liu Z, Ravindranathan R, Kalinski P, Guo ZS and Bartlett DL: Rational combination of oncolytic vaccinia virus and PD-L1 blockade works synergistically to enhance therapeutic efficacy. Nat Commun. 8:147542017. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Marabelle A, Tselikas L, de Baere T and Houot R: Intratumoral immunotherapy: Using the tumor as the remedy. Ann Oncol. 28(suppl_12): xii33–xii43. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Bourgeois-Daigneault MC, Roy DG, Aitken AS, El Sayes N, Martin NT, Varette O, Falls T, St-Germain LE, Pelin A, Lichty BD, et al: Neoadjuvant oncolytic virotherapy before surgery sensitizes triple-negative breast cancer to immune checkpoint therapy. Sci Transl Med. 10:eaao16412018. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Hong WX, Haebe S, Lee AS, Westphalen CB, Norton JA, Jiang W and Levy R: Intratumoral immunotherapy for early-stage solid tumors. Clin Cancer Res. 26:3091–3099. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Zamarin D, Holmgaard RB, Subudhi SK, Park JS, Mansour M, Palese P, Merghoub T, Wolchok JD and Allison JP: Localized oncolytic virotherapy overcomes systemic tumor resistance to immune checkpoint blockade immunotherapy. Sci Transl Med. 6:226ra322014. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Chaurasiya S, Yang A, Kang S, Lu J, Kim SI, Park AK, Sivanandam V, Zhang Z, Woo Y, Warner SG and Fong Y: Oncolytic poxvirus CF33-hNIS-ΔF14.5 favorably modulates tumor immune microenvironment and works synergistically with anti-PD-L1 antibody in a triple-negative breast cancer model. Oncoimmunology. 9:17293002020. View Article : Google Scholar
|
|
107
|
Camilio KA, Wang MY, Mauseth B, Waagene S, Kvalheim G, Rekdal Ø, Sveinbjørnsson B and Mælandsmo GM: Combining the oncolytic peptide LTX-315 with doxorubicin demonstrates therapeutic potential in a triple-negative breast cancer model. Breast Cancer Res. 21:92019. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Desrichard A, Snyder A and Chan TA: Cancer neoantigens and applications for immunotherapy. Clin Cancer Res. 22:807–812. 2016. View Article : Google Scholar
|
|
109
|
Vinay DS, Ryan EP, Pawelec G, Talib WH, Stagg J, Elkord E, Lichtor T, Decker WK, Whelan RL, Kumara HMCS, et al: Immune evasion in cancer: Mechanistic basis and therapeutic strategies. Semin Cancer Biol. 35:S185–S198. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Safavi A, Kefayat A, Mahdevar E, Ghahremani F, Nezafat N and Modarressi MH: Efficacy of co-immunization with the DNA and peptide vaccines containing SYCP1 and ACRBP epitopes in a murine triple-negative breast cancer model. Hum Vaccin Immunother. 17:22–34. 2021. View Article : Google Scholar :
|
|
111
|
Liu L, Wang Y, Miao L, Liu Q, Musetti S, Li J and Huang L: Combination immunotherapy of MUC1 mRNA Nano-vaccine and CTLA-4 blockade effectively inhibits growth of triple negative breast cancer. Mol Ther. 26:45–55. 2018. View Article : Google Scholar :
|
|
112
|
Gibney GT, Weiner LM and Atkins MB: Predictive biomarkers for checkpoint inhibitor-based immunotherapy. Lancet Oncol. 17:e542–e551. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Charoentong P, Finotello F, Angelova M, Mayer C, Efremova M, Rieder D, Hackl H and Trajanoski Z: Pan-cancer immunogenomic analyses reveal genotype-immunophenotype relationships and predictors of response to checkpoint blockade. Cell Rep. 18:248–262. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Bindea G, Mlecnik B, Tosolini M, Kirilovsky A, Waldner M, Obenauf AC, Angell H, Fredriksen T, Lafontaine L, Berger A, et al: Spatiotemporal dynamics of intratumoral immune cells reveal the immune landscape in human cancer. Immunity. 39:782–795. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Miao YR, Zhang Q, Lei Q, Luo M, Xie GY, Wang H and Guo AY: ImmuCellAI : A unique method for comprehensive T-cell subsets abundance prediction and its application in cancer immunotherapy. Adv Sci (Weinh). 7:19028802020. View Article : Google Scholar
|
|
116
|
Peng Y, Yu H, Jin Y, Qu F, Ren H, Tang Z, Zhang Y, Qu C, Zong B and Liu S: Construction and validation of an immune infiltration-related gene signature for the prediction of prognosis and therapeutic response in breast cancer. Front Immunol. 12:6661372021. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Wang K, Li HL, Xiong YF, Shi Y, Li ZY, Li J, Zhang X and Li HY: Development and validation of nomograms integrating immune-related genomic signatures with clinicopathologic features to improve prognosis and predictive value of triple-negative breast cancer: A gene expression-based retrospective study. Cancer Med. 8:686–700. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
He Y, Jiang Z, Chen C and Wang X: Classification of triple-negative breast cancers based on Immunogenomic profiling. J Exp Clin Cancer Res. 37:3272018. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Pauken KE, Dougan M, Rose NR, Lichtman AH and Sharpe AH: Adverse events following cancer immunotherapy: Obstacles and opportunities. Trends Immunol. 40:511–523. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Haanen JBAG, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J and Jordan K: ESMO Guidelines Committee: Management of toxicities from immunotherapy: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 28(suppl_4): iv119–iv142. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Postow MA, Sidlow R and Hellmann MD: Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med. 378:158–168. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Wang DY, Salem JE, Cohen JV, Chandra S, Menzer C, Ye F, Zhao S, Das S, Beckermann KE, Ha L, et al: Fatal toxic effects associated with immune checkpoint inhibitors: A systematic review and meta-analysis. JAMA Oncol. 4:1721–1728. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
de Filette J, Andreescu CE, Cools F, Bravenboer B and Velkeniers B: A systematic review and meta-analysis of endocrine-related adverse events associated with immune checkpoint inhibitors. Horm Metab Res. 51:145–156. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Cappelli LC, Gutierrez AK, Bingham CO III and Shah AA: Rheumatic and musculoskeletal immune-related adverse events due to immune checkpoint inhibitors: A systematic review of the literature. Arthritis Care Res (Hoboken). 69:1751–1763. 2017. View Article : Google Scholar
|
|
125
|
Arbour KC, Mezquita L, Long N, Rizvi H, Auclin E, Ni A, Martínez-Bernal G, Ferrara R, Lai WV, Hendriks LEL, et al: Impact of baseline steroids on efficacy of programmed cell Death-1 and programmed death-ligand 1 blockade in patients with non-small-cell lung cancer. J Clin Oncol. 36:2872–2878. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Szekely B, Bossuyt V, Li X, Wali VB, Patwardhan GA, Frederick C, Silber A, Park T, Harigopal M, Pelekanou V, et al: Immunological differences between primary and metastatic breast cancer. Ann Oncol. 29:2232–2239. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Adams S, Gatti-Mays ME, Kalinsky K, Korde LA, Sharon E, Amiri-Kordestani L, Bear H, McArthur HL, Frank E, Perlmutter J, et al: Current landscape of immunotherapy in breast cancer: A review. JAMA Oncol. 5:1205–1214. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y and Pietenpol JA: Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest. 121:2750–2767. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Ramos-Casals M, Brahmer JR, Callahan MK, Flores-Chávez A, Keegan N, Khamashta MA, Lambotte O, Mariette X, Prat A and Suárez-Almazor ME: Immuneelated adverse events of checkpoint inhibitors. Nat Rev Dis Primers. 6:382020. View Article : Google Scholar
|
|
130
|
Kanjanapan Y, Day D, Butler MO, Wang L, Joshua AM, Hogg D, Leighl NB, Razak ARA, Hansen AR, Boujos S, et al: Delayed immune-related adverse events in assessment for dose-limiting toxicity in early phase immunotherapy trials. Eur J Cancer. 107:1–7. 2019. View Article : Google Scholar
|
|
131
|
Eun Y, Kim IY, Sun JM and Lee J, Cha HS, Koh EM and Lee J: Risk factors for immune-related adverse events associated with anti-PD-1 pembrolizumab. Sci Rep. 9:140392019. View Article : Google Scholar : PubMed/NCBI
|