|
1
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263.
2024.PubMed/NCBI
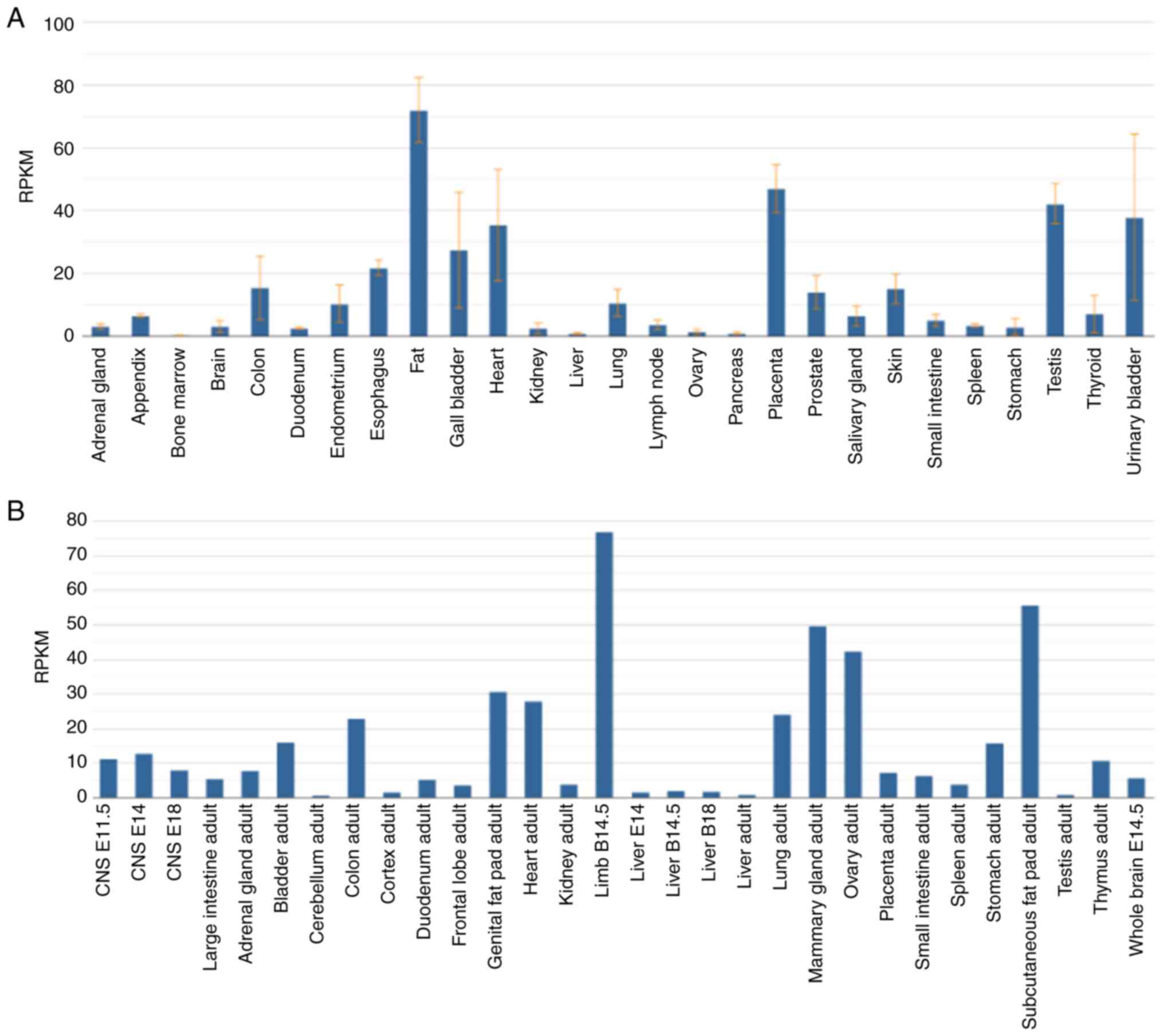
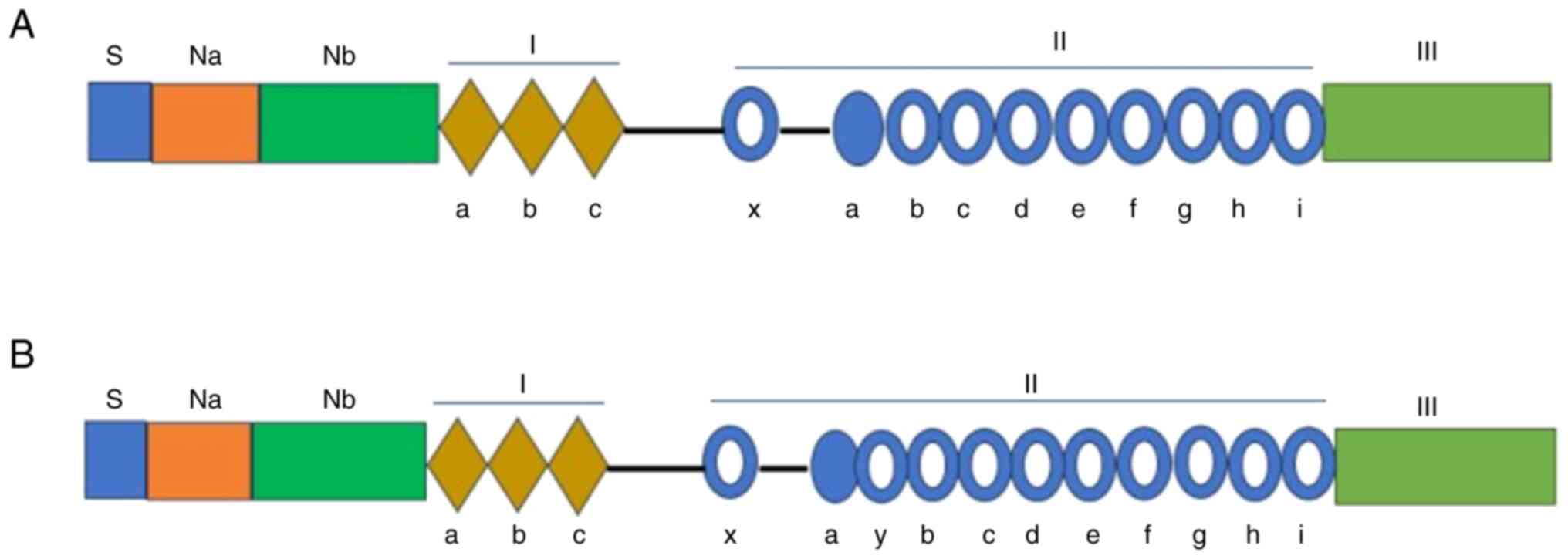
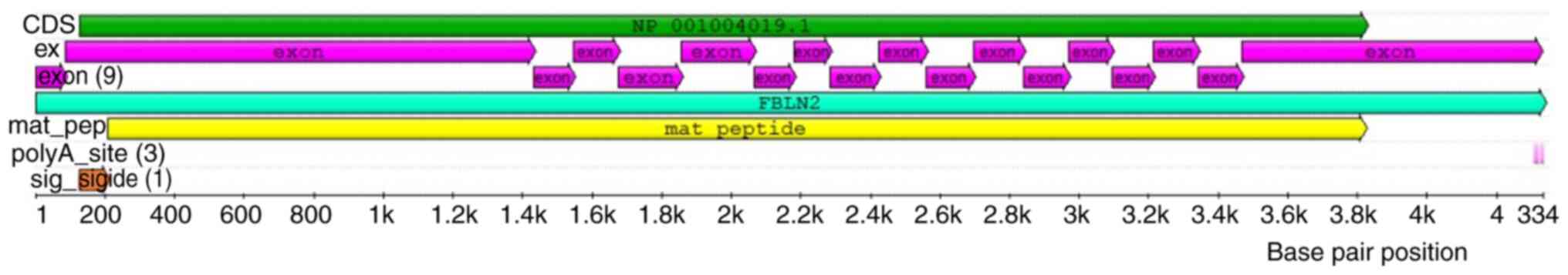
|
|
2
|
Bray F, Laversanne M, Weiderpass E and
Soerjomataram I: The ever-increasing importance of cancer as a
leading cause of premature death worldwide. Cancer. 127:3029–3030.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siegel RL, Kratzer TB, Giaquinto AN, Sung
H and Jemal A: Cancer statistics, 2025. CA Cancer J Clin. 75:10–45.
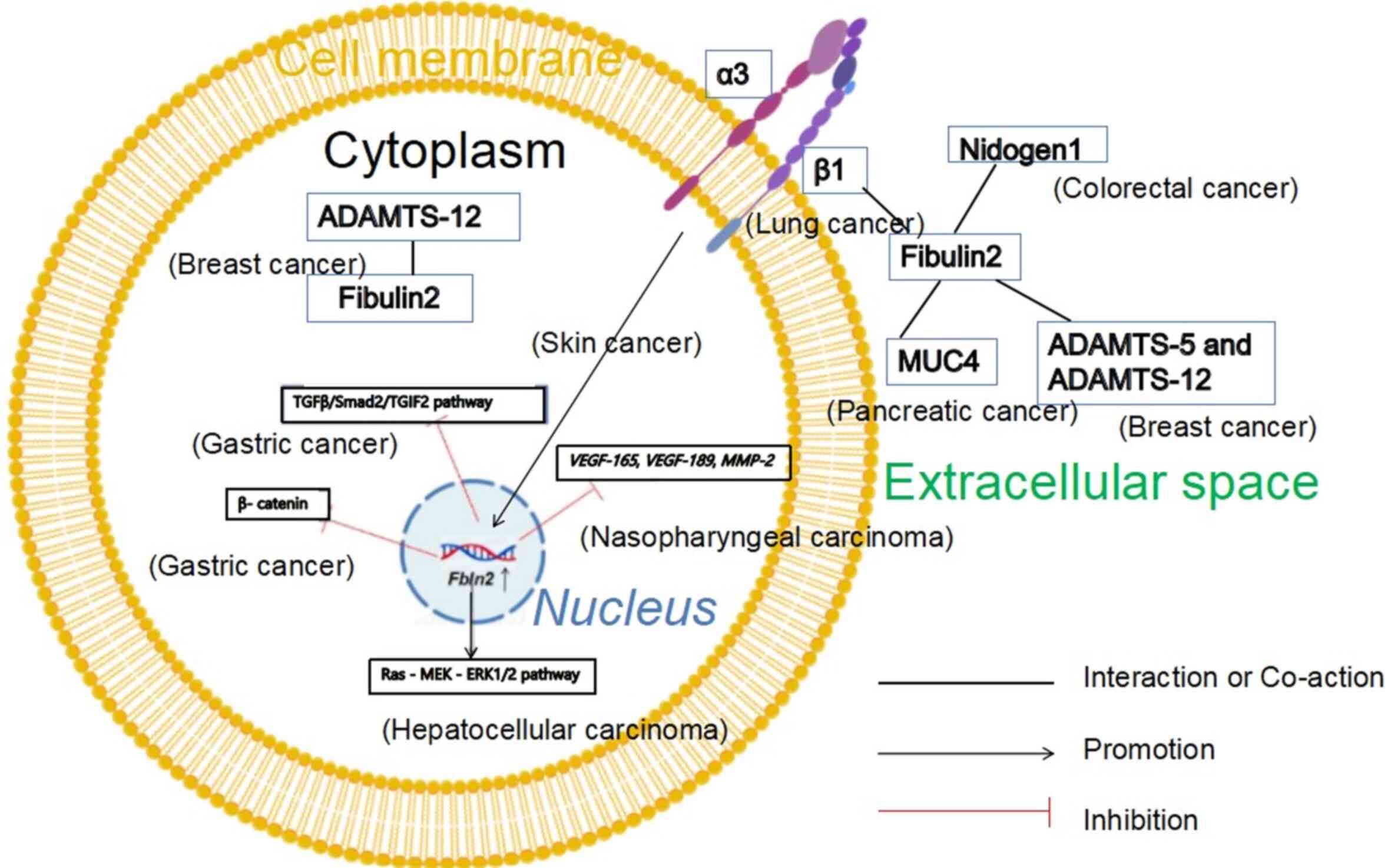
2025.PubMed/NCBI
|
|
4
|
Takakura D, Ohashi S, Kobayashi N,
Tokuhisa M, Ichikawa Y and Kawasaki N: Targeted O-glycoproteomics
for the development of diagnostic markers for advanced colorectal
cancer. Front Oncol. 13:11049362023. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sofela AA, Hilton DA, Ammoun S, Baiz D,
Adams CL, Ercolano E, Jenkinson MD, Kurian KM, Teo M, Whitfield PC,
et al: Fibulin-2: A novel biomarker for differentiating grade II
from grade I meningiomas. Int J Mol Sci. 22:5602021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sofela AA, McGavin L, Whitfield PC and
Hanemann CO: Biomarkers for differentiating grade II meningiomas
from grade I: A systematic review. Br J Neurosurg. 35:696–702.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ren T, Lin S, Wang Z and Shang A:
Differential proteomics analysis of low- and high-grade of
astrocytoma using iTRAQ quantification. Onco Targets Ther.
9:5883–5895. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pan TC, Sasaki T, Zhang RZ, Fässler R,
Timpl R and Chu ML: Structure and expression of fibulin-2, a novel
extracellular matrix protein with multiple EGF-like repeats and
consensus motifs for calcium binding. J Cell Biol. 123:1269–1277.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang H, Hui D and Fu X: Roles of
Fibulin-2 in carcinogenesis. Med Sci Monit.
26:e9180992020.PubMed/NCBI
|
|
10
|
Baird BN, Schliekelman MJ, Ahn YH, Chen Y,
Roybal JD, Gill BJ, Mishra DK, Erez B, O'Reilly M, Yang Y, et al:
Fibulin-2 is a driver of malignant progression in lung
adenocarcinoma. PLoS One. 8:e670542013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang RZ, Pan TC, Zhang ZY, Mattei MG,
Timpl R and Chu ML: Fibulin-2 (FBLN2): Human cDNA sequence, mRNA
expression, and mapping of the gene on human and mouse chromosomes.
Genomics. 22:425–430. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brown JC, Sasaki T, Göhring W, Yamada Y
and Timpl R: The C-terminal domain V of perlecan promotes beta1
integrin-mediated cell adhesion, binds heparin, nidogen and
fibulin-2 and can be modified by glycosaminoglycans. Eur J Biochem.
250:39–46. 1997. View Article : Google Scholar
|
|
13
|
Hopf M, Göhring W, Kohfeldt E, Yamada Y
and Timpl R: Recombinant domain IV of perlecan binds to nidogens,
laminin-nidogen complex, fibronectin, fibulin-2 and heparin. Eur J
Biochem. 259:917–925. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sasaki T, Göhring W, Mann K, Brakebusch C,
Yamada Y, Fässler R and Timpl R: Short arm region of laminin-5
gamma2 chain: Structure, mechanism of processing and binding to
heparin and proteins. J Mol Biol. 314:751–763. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Talts JF, Andac Z, Göhring W, Brancaccio A
and Timpl R: Binding of the G domains of laminin alpha1 and alpha2
chains and perlecan to heparin, sulfatides, alpha-dystroglycan and
several extracellular matrix proteins. EMBO J. 18:863–870. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sasaki T, Wiedemann H, Matzner M, Chu ML
and Timpl R: Expression of fibulin-2 by fibroblasts and deposition
with Fibronectin into a fibrillar matrix. J Cell Sci. 109(Pt 12):
2895–2904. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sasaki T, Fukai N, Mann K, Göhring W,
Olsen BR and Timpl R: Structure, function and tissue forms of the
C-terminal globular domain of collagen XVIII containing the
angiogenesis inhibitor endostatin. EMBO J. 17:4249–4256. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Olin AI, Mörgelin M, Sasaki T, Timpl R,
Heinegård D and Aspberg A: The proteoglycans aggrecan and Versican
form networks with fibulin-2 through their lectin domain binding. J
Biol Chem. 276:1253–1261. 2001. View Article : Google Scholar
|
|
19
|
Friedrich MV, Göhring W, Mörgelin M,
Brancaccio A, David G and Timpl R: Structural basis of
glycosaminoglycan modification and of heterotypic interactions of
perlecan domain V. J Mol Biol. 294:259–270. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Utani A, Nomizu M and Yamada Y: Fibulin-2
binds to the short arms of laminin-5 and laminin-1 via conserved
amino acid sequences. J Biol Chem. 272:2814–2820. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
de Vega S, Iwamoto T and Yamada Y:
Fibulins: Multiple roles in matrix structures and tissue functions.
Cell Mol Life Sci. 66:1890–1902. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Law EW, Cheung AK, Kashuba VI, Pavlova TV,
Zabarovsky ER, Lung HL, Cheng Y, Chua D, Kwong DLK, Tsao SW, et al:
Anti-angiogenic and tumor-suppressive roles of candidate
tumor-suppressor gene, Fibulin-2, in nasopharyngeal carcinoma.
Oncogene. 31:728–738. 2012. View Article : Google Scholar
|
|
23
|
Alcendor DJ, Knobel S, Desai P, Zhu WQ and
Hayward GS: KSHV regulation of fibulin-2 in Kaposi's sarcoma:
Implications for tumorigenesis. Am J Pathol. 179:1443–1454. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang X, Duan L, Zhang Y, Zhao H, Yang X
and Zhang C: Correlation of Fibulin-2 expression with
proliferation, migration and invasion of breast cancer cells. Oncol
Lett. 20:1945–1951. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hu X, Liu T, Li L, Gan H, Wang T, Pang P
and Mao J: Fibulin-2 facilitates malignant progression of
hepatocellular carcinoma. Turk J Gastroenterol. 34:635–644. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ma H, Lian C and Song Y: Fibulin-2
inhibits development of gastric cancer by downregulating β-catenin.
Oncol Lett. 18:2799–2804. 2019.PubMed/NCBI
|
|
27
|
Zhou M, Mao X, Shen K, Zhan Q, Ni H, Liu
C, Huang Z and Li R: FBLN2 inhibits gastric cancer proliferation
and metastasis via the TGFβ/TGIF2 pathway. Pathol Res Pract.
269:1558992025. View Article : Google Scholar
|
|
28
|
Missan DS, Chittur SV and DiPersio CM:
Regulation of fibulin-2 gene expression by integrin α3β1
contributes to the invasive phenotype of transformed keratinocytes.
J Invest Dermatol. 134:2418–2427. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang MR, Chen RJ, Zhao F, Zhang HH, Bi QY,
Zhang YN, Zhang YQ, Wu ZC and Ji XM: Effect of Wenxia Changfu
formula combined with cisplatin reversing non-small cell lung
cancer cell adhesion-mediated drug resistance. Front Pharmacol.
11:5001372020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
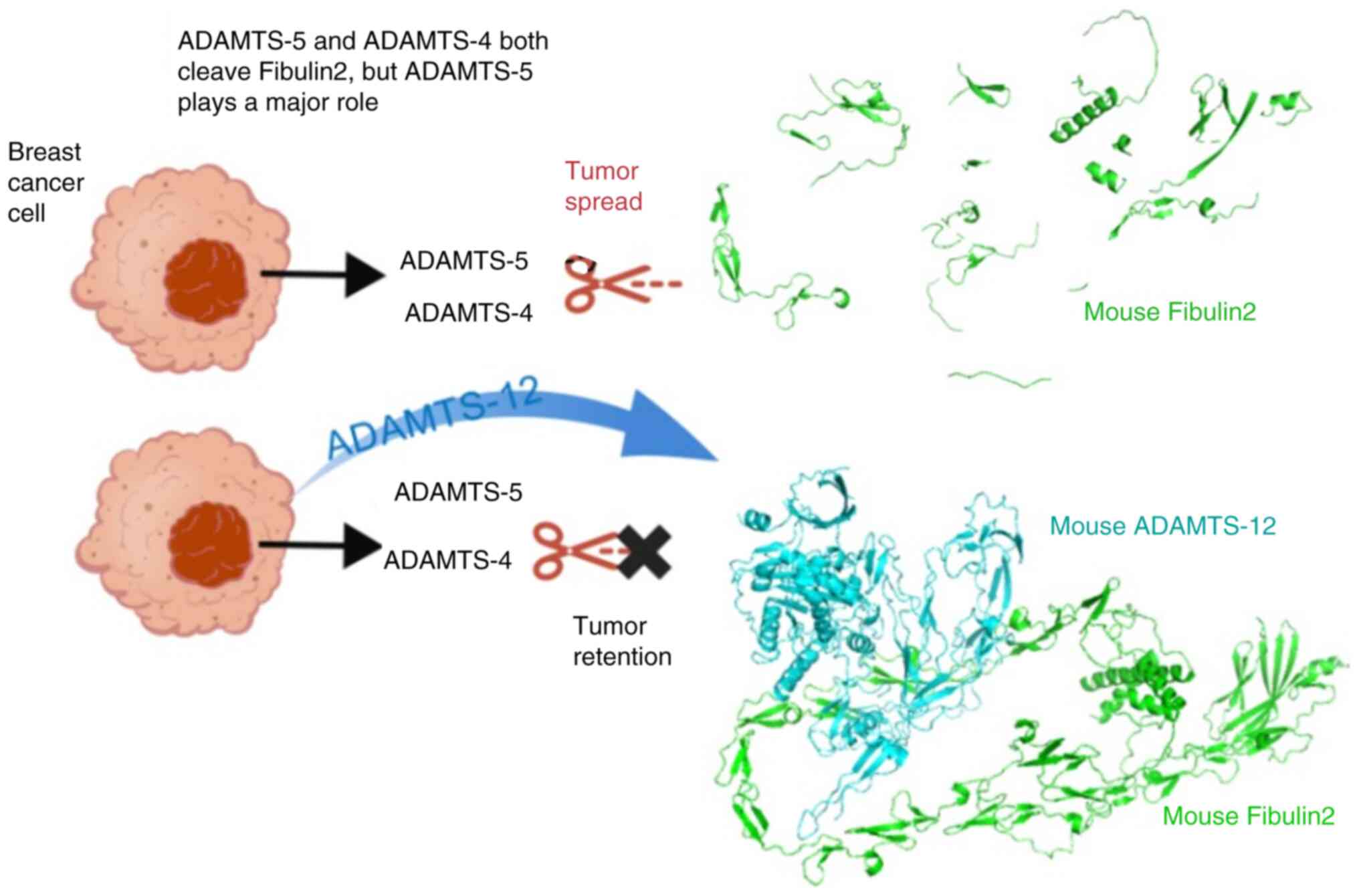
Fontanil T, Álvarez-Teijeiro S, Villaronga
MÁ, Mohamedi Y, Solares L, Moncada-Pazos A, Vega JA, García-Suárez
O, Pérez-Basterrechea M, García-Pedrero JM, et al: Cleavage of
Fibulin-2 by the aggrecanases ADAMTS-4 and ADAMTS-5 contributes to
the tumorigenic potential of breast cancer cells. Oncotarget.
8:13716–13729. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
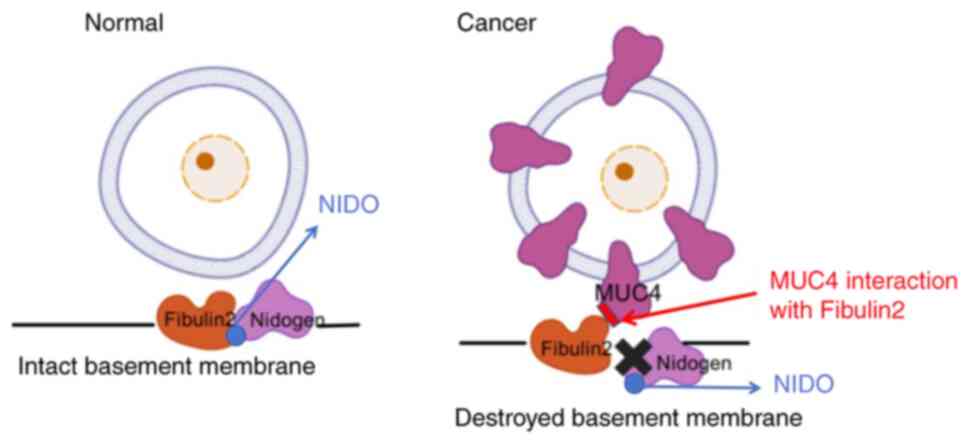
Vaes N, Schonkeren SL, Rademakers G,
Holland AM, Koch A, Gijbels MJ, Keulers TG, de Wit M, Moonen L, Van
der Meer JRM, et al: Loss of enteric neuronal Ndrg4 promotes
colorectal cancer via increased release of Nid1 and Fbln2. EMBO
Rep. 22:e519132021. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Senapati S, Gnanapragassam VS, Moniaux N,
Momi N and Batra SK: Role of MUC4-NIDO domain in the MUC4-mediated
metastasis of pancreatic cancer cells. Oncogene. 31:3346–3356.
2012. View Article : Google Scholar :
|
|
33
|
Melotte V, Lentjes MH, van den Bosch SM,
Hellebrekers DM, de Hoon JP, Wouters KA, Daenen KL,
Partouns-Hendriks IE, Stessels F, Louwagie J, et al: N-Myc
downstream-regulated gene 4 (NDRG4): A candidate tumor suppressor
gene and potential biomarker for colorectal cancer. J Natl Cancer
Inst. 101:916–927. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
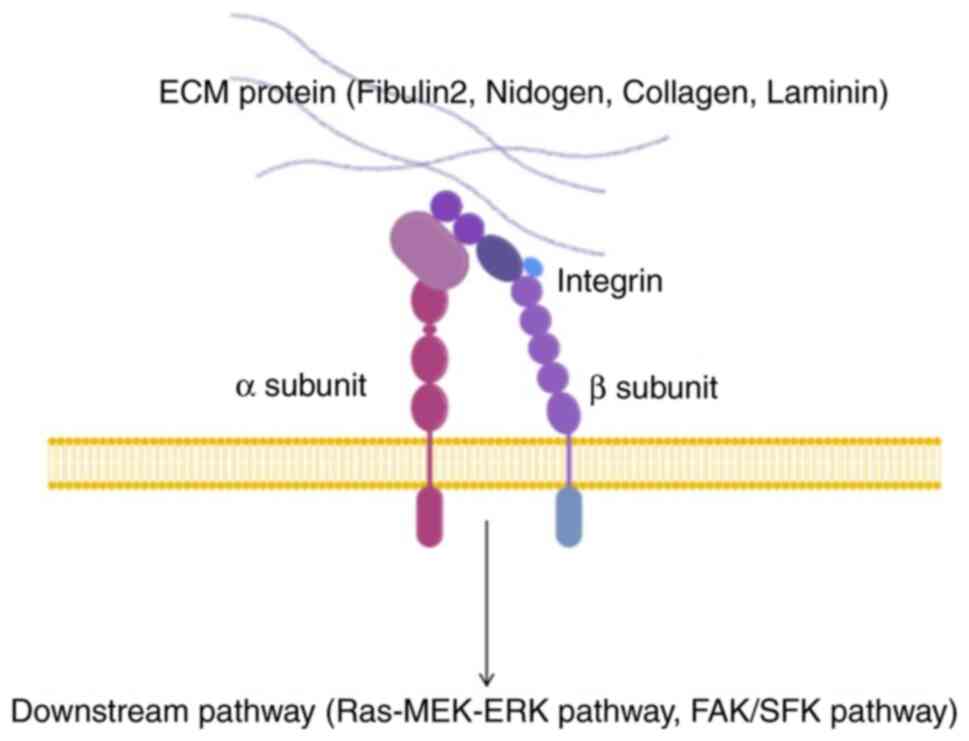
Barczyk M, Carracedo S and Gullberg D:
Integrins. Cell Tissue Res. 339:269–280. 2010. View Article : Google Scholar
|
|
35
|
Cooper J and Giancotti FG: Integrin
signaling in cancer: Mechanotransduction, stemness, epithelial
plasticity, and therapeutic resistance. Cancer Cell. 35:347–367.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Nobre LT, Vidal AA, Almeida-Lima J,
Oliveira RM, Paredes-Gamero EJ, Medeiros VP, Trindade ES, Franco
CR, Nader HB and Rocha HA: Fucan effect on CHO cell proliferation
and migration. Carbohydr Polym. 98:224–232. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Fischer C, Sanchez-Ruderisch H, Welzel M,
Wiedenmann B, Sakai T, André S, Gabius HJ, Khachigian L, Detjen KM
and Rosewicz S: Galectin-1 interacts with the {alpha}5{beta}1
fibronectin receptor to restrict carcinoma cell growth via
induction of p21 and p27. J Biol Chem. 280:37266–37277. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hynes RO: Integrins: Bidirectional,
allosteric signaling machines. Cell. 110:673–687. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hamidi H and Ivaska J: Every step of the
way: Integrins in cancer progression and metastasis. Nat Rev
Cancer. 18:533–548. 2019. View Article : Google Scholar :
|
|
40
|
Humphries JD, Byron A and Humphries MJ:
Integrin ligands at a glance. J Cell Sci. 119:3901–3903. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Springer TA and Wang JH: The
three-dimensional structure of integrins and their ligands, and
sconformational regulation of cell adhesion. Adv Protein Chem.
68:29–63. 2004. View Article : Google Scholar
|
|
42
|
Arnaout MA, Mahalingam B and Xiong JP:
Integrin structure, allostery, and bidirectional signaling. Annu
Rev Cell Dev Biol. 21:381–410. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Erler JT, Bennewith KL, Nicolau M,
Dornhofer N, Kong C, Le QT, Chi JT, Jeffrey SS and Giaccia AJ:
Lysyl oxidase is essential for hypoxia-induced metastasis. Nature.
440:1222–1226. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Levental KR, Yu H, Kass L, Lakins JN,
Egeblad M, Erler JT, Fong SF, Csiszar K, Giaccia A, Weninger W, et
al: Matrix crosslinking forces tumor progression by enhancing
integrin signaling. Cell. 139:891–906. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Couillard J, Demers M, Lavoie G and
St-Pierre Y: The role of DNA hypomethylation in the control of
stromelysin gene expression. Biochem Biophys Res Commun.
342:1233–1239. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Hanson JA, Gillespie JW, Grover A, Tangrea
MA, Chuaqui RF, Emmert-Buck MR, Tangrea JA, Libutti SK, Linehan WM
and Woodson KG: Gene promoter methylation in prostate
tumor-associated stromal cells. J Natl Cancer Inst. 98:255–261.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Lin HJ, Zuo T, Lin CH, Kuo CT,
Liyanarachchi S, Sun S, Shen R, Deatherage DE, Potter D, Asamoto L,
et al: Breast cancer-associated fibroblasts confer AKT1-mediated
epigenetic silencing of Cystatin M in epithelial cells. Cancer Res.
68:10257–10266. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Hanahan D and Coussens LM: Accessories to
the crime: Functions of cells recruited to the tumor
microenvironment. Cancer Cell. 21:309–322. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ostman A and Augsten M: Cancer-associated
fibroblasts and tumor growth-bystanders turning into key players.
Curr Opin Genet Dev. 19:67–73. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Micallef L, Vedrenne N, Billet F, Coulomb
B, Darby IA and Desmoulière A: The myofibroblast, multiple origins
for major roles in normal and pathological tissue repair.
Fibrogenesis Tissue Repair. 5(Suppl 1): S52012. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kalluri R: The biology and function of
fibroblasts in cancer. Nat Rev Cancer. 16:582–598. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Neuzillet C, Tijeras-Raballand A, Cros J,
Faivre S, Hammel P and Raymond E: Stromal expression of SPARC in
pancreatic adenocarcinoma. Cancer Metastasis Rev. 32:585–602. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Rønnov-Jessen L, Petersen OW and Bissell
MJ: Cellular changes involved in conversion of normal to malignant
breast: Importance of the stromal reaction. Physiol Rev. 76:69–125.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Chiquet-Ehrismann R, Mackie EJ, Pearson CA
and Sakakura T: Tenascin: An extracellular matrix protein involved
in tissue interactions during fetal development and oncogenesis.
Cell. 47:131–139. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kyutoku M, Taniyama Y, Katsuragi N,
Shimizu H, Kunugiza Y, Iekushi K, Koibuchi N, Sanada F, Oshita Y
and Morishita R: Role of periostin in cancer progression and
metastasis: Inhibition of breast cancer progression and metastasis
by anti-periostin antibody in a murine model. Int J Mol Med.
28:181–186. 2011.PubMed/NCBI
|
|
56
|
Mackie EJ, Chiquet-Ehrismann R, Pearson
CA, Inaguma Y, Taya K, Kawarada Y and Sakakura T: Tenascin is a
stromal marker for epithelial malignancy in the mammary gland. Proc
Natl Acad Sci USA. 84:4621–4625. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Ouyang G, Liu M, Ruan K, Song G, Mao Y and
Bao S: Upregulated expression of periostin by hypoxia in
non-small-cell lung cancer cells promotes cell survival via the
Akt/PKB pathway. Cancer Lett. 281:213–219. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Ruan K, Bao S and Ouyang G: The
multifaceted role of periostin in tumorigenesis. Cell Mol Life Sci.
66:2219–2230. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Boire A, Covic L, Agarwal A, Jacques S,
Sherifi S and Kuliopulos A: PAR1 is a matrix metalloprotease-1
receptor that promotes invasion and tumorigenesis of breast cancer
cells. Cell. 120:303–313. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Sternlicht MD, Lochter A, Sympson CJ, Huey
B, Rougier JP, Gray JW, Pinkel D, Bissell MJ and Werb Z: The
stromal proteinase MMP3/stromelysin-1 promotes mammary
carcinogenesis. Cell. 98:137–146. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Hotary KB, Allen ED, Brooks PC, Datta NS,
Long MW and Weiss SJ: Membrane type I matrix metalloproteinase
usurps tumor growth control imposed by the three-dimensional
extracellular matrix. Cell. 114:33–45. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Valkenburg KC, de Groot AE and Pienta KJ:
Targeting the tumour stroma to improve cancer therapy. Nat Rev Clin
Oncol. 15:366–381. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Nusse R and Clevers H: Wnt/β-catenin
signaling, disease, and emerging therapeutic modalities. Cell.
169:985–999. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Melnik S, Dvornikov D, Müller-Decker K,
Depner S, Stannek P, Meister M, Warth A, Thomas M, Muley T, Risch
A, et al: Cancer cell specific inhibition of Wnt/β-catenin
signaling by forced intracellular acidification. Cell Discov.
4:372018. View Article : Google Scholar
|
|
65
|
Deng YZ, Yao F, Li JJ, Mao ZF, Hu PT, Long
LY, Li G, Ji XD, Shi S, Guan DX, et al: RACK1 suppresses gastric
tumorigenesis by stabilizing the β-catenin destruction complex.
Gastroenterology. 142:812–823.e15. 2012. View Article : Google Scholar
|
|
66
|
Austinat M, Dunsch R, Wittekind C,
Tannapfel A, Gebhardt R and Gaunitz F: Correlation between
beta-catenin mutations and expression of Wnt-signaling target genes
in hepatocellular carcinoma. Mol Cancer. 7:212008. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Brenner KA, Corbett SA and Schwarzbauer
JE: Regulation of fibronectin matrix assembly by activated Ras in
transformed cells. Oncogene. 19:3156–3163. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Werbajh SE, Urtreger AJ, Puricelli LI, de
Lustig ES, de Kier Joffé E and Kornblihtt AR: Downregulation of
fibronectin transcription in highly metastatic adenocarcinoma
cells. FEBS Lett. 440:277–281. 1998. View Article : Google Scholar
|
|
69
|
Seo JY, Lee SH, Youn CS, Choi HR, Rhie GE,
Cho KH, Kim KH, Park KC, Eun HC and Chung JH: Ultraviolet radiation
increases Tropoelastin mRNA expression in the epidermis of human
skin in vivo. J Invest Dermatol. 116:915–919. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Taddese S, Weiss AS, Jahreis G, Neubert RH
and Schmelzer CE: In vitro degradation of human tropoelastin by
MMP-12 and the generation of matrikines from domain 24. Matrix
Biol. 28:84–91. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Yan L, Wang Y, Feng J, Ni Y, Zhang T, Cao
Y, Zhou M and Zhao C: Mechanism and application of fibrous proteins
in diabetic wound healing: A literature review. Front Endocrinol
(Lausanne). 15:14305432024. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Giaquinto AN, Sung H, Newman LA, Freedman
RA, Smith RA, Star J, Jemal A and Siegel RL: Breast cancer
statistics 2024. CA Cancer J Clin. 74:477–495. 2024.PubMed/NCBI
|
|
73
|
Yi CH, Smith DJ, West WW and Hollingsworth
MA: Loss of fibulin-2 expression is associated with breast cancer
progression. Am J Pathol. 170:1535–1545. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Ibrahim AM, Sabet S, El-Ghor AA, Kamel N,
Anis SE, Morris JS and Stein T: Fibulin-2 is required for basement
membrane integrity of mammary epithelium. Sci Rep. 8:141392018.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Longmate WM, Monichan R, Chu ML, Tsuda T,
Mahoney MG and DiPersio CM: Reduced fibulin-2 contributes to loss
of basement membrane integrity and skin blistering in mice lacking
Integrin α3β1 in the epidermis. J Invest Dermatol. 134:1609–1617.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Klingen TA, Chen Y, Aas H, Wik E and
Akslen LA: Fibulin-2 expression associates with vascular invasion
and patient survival in breast cancer. PLoS One. 16:e02497672021.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Cal S and López-Otín C: ADAMTS proteases
and cancer. Matrix Biol. 44-46:77–85. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Noël A, Gutiérrez-Fernández A, Sounni NE,
Behrendt N, Maquoi E, Lund IK, Cal S, Hoyer-Hansen G and López-Otín
C: New and paradoxical roles of matrix metalloproteinases in the
tumor microenvironment. Front Pharmacol. 3:1402012. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Luan Y, Kong L, Howell DR, Ilalov K,
Fajardo M, Bai XH, Di Cesare PE, Goldring MB, Abramson SB and Liu
CJ: Inhibition of ADAMTS-7 and ADAMTS-12 degradation of cartilage
oligomeric matrix protein by alpha-2-macroglobulin. Osteoarthritis
Cartilage. 16:1413–1420. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Fontanil T, Rúa S, Llamazares M,
Moncada-Pazos A, Quirós PM, García-Suárez O, Vega JA, Sasaki T,
Mohamedi Y, Esteban MM, et al: Interaction between the ADAMTS-12
metalloprotease and fibulin-2 induces tumor-suppressive effects in
breast cancer cells. Oncotarget. 5:1253–1264. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Kelwick R, Desanlis I, Wheeler GN and
Edwards DR: The ADAMTS (A DisIntegrin and Metalloproteinase with
Thrombospondin motifs) family. Genome Biol. 16:1132015. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Yu Y, Xiao CH, Tan LD, Wang QS, Li XQ and
Feng YM: Cancer-associated fibroblasts induce
epithelial-mesenchymal transition of breast cancer cells through
paracrine TGF-β signaling. Br J Cancer. 110:724–732. 2014.
View Article : Google Scholar
|
|
83
|
Cuffaro D, Ciccone L, Rossello A, Nuti E
and Santamaria S: Targeting Aggrecanases for osteoarthritis
therapy: From zinc chelation to exosite inhibition. J Med Chem.
65:13505–13532. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Niland S, Riscanevo AX and Eble JA: Matrix
metalloproteinases shape the tumor microenvironment in cancer
progression. Int J Mol Sci. 23:1462021. View Article : Google Scholar
|
|
85
|
Ghalehbandi S, Yuzugulen J, Pranjol MZI
and Pourgholami MH: The role of VEGF in cancer-induced angiogenesis
and research progress of drugs targeting VEGF. Eur J Pharmacol.
949:1755862023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Reddy RA, Varshini MS and Kumar RS: Matrix
metalloproteinase-2 (MMP-2): As an essential factor in cancer
progression. Recent Pat Anticancer Drug Discov. 20:26–44. 2025.
View Article : Google Scholar
|
|
87
|
Hergeth SP, Aicher WK, Essl M, Schreiber
TD, Sasaki T and Klein G: Characterization and functional analysis
of osteoblast-derived fibulins in the human hematopoietic stem cell
niche. Exp Hematol. 36:1022–1034. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Rashid ZA and Bardaweel SK: Novel matrix
metalloproteinase-9 (MMP-9) inhibitors in cancer treatment. Int J
Mol Sci. 24:121332023. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Astudillo P: Extracellular matrix
stiffness and Wnt/β-catenin signaling in physiology and disease.
Biochem Soc Trans. 48:1187–1198. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Henderson NC, Rieder F and Wynn TA:
Fibrosis: From mechanisms to medicines. Nature. 587:555–566. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Caligiuri G and Tuveson DA: Activated
fibroblasts in cancer: Perspectives and challenges. Cancer Cell.
41:434–449. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Bhowmick NA, Chytil A, Plieth D, Gorska
AE, Dumont N, Shappell S, Washington MK, Neilson EG and Moses HL:
TGF-beta signaling in fibroblasts modulates the oncogenic potential
of adjacent epithelia. Science. 303:848–851. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Cruz-Munoz W and Khokha R: The role of
tissue inhibitors of metalloproteinases in tumorigenesis and
metastasis. Crit Rev Clin Lab Sci. 45:291–338. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Bloomston M, Shafii A, Zervos EE and
Rosemurgy AS: TIMP-1 overexpression in pancreatic cancer attenuates
tumor growth, decreases implantation and metastasis, and inhibits
angiogenesis. J Surg Res. 102:39–44. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Chen J and Khalil RA: Matrix
metalloproteinases in normal pregnancy and preeclampsia. Prog Mol
Biol Transl Sci. 148:87–165. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Murphy G: Tissue inhibitors of
metalloproteinases. Genome Biol. 12:2332011. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Shimoda M, Jackson HW and Khokha R: Tumor
suppression by stromal TIMPs. Mol Cell Oncol. 3:e9750822016.
View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Zhai LL, Cai CY, Wu Y and Tang ZG:
Correlation and prognostic significance of MMP-2 and TFPI-2
differential expression in pancreatic carcinoma. Int J Clin Exp
Pathol. 8:682–691. 2015.PubMed/NCBI
|
|
99
|
Song G, Xu S, Zhang H, Wang Y, Xiao C,
Jiang T, Wu L, Zhang T, Sun X, Zhong L, et al: TIMP1 is a
prognostic marker for the progression and metastasis of colon
cancer through FAK-PI3K/AKT and MAPK pathway. J Exp Clin Cancer
Res. 35:1482016. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Shimoda M, Principe S, Jackson HW, Luga V,
Fang H, Molyneux SD, Shao YW, Aiken A, Waterhouse PD, Karamboulas
C, et al: Loss of the Timp gene family is sufficient for the
acquisition of the CAF-like cell state. Nat Cell Biol. 16:889–901.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Tjomsland V, Pomianowska E, Aasrum M,
Sandnes D, Verbeke CS and Gladhaug IP: Profile of MMP and TIMP
expression in human pancreatic stellate cells: Regulation by IL-1α
and TGFβ and implications for migration of pancreatic cancer cells.
Neoplasia. 18:447–456. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
https://gdt.gradepro.org/app/handbook/handbook.html#h.9rdbelsnu4iy.
Accessed 22 Jul 2023
|
|
103
|
Whiteaker JR, Zhang H, Zhao L, Wang P,
Kelly-Spratt KS, Ivey RG, Piening BD, Feng LC, Kasarda E, Gurley
KE, et al: Integrated pipeline for mass spectrometry-based
discovery and confirmation of biomarkers demonstrated in a mouse
model of breast cancer. J Proteome Res. 6:3962–3975. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Avsar M, Tambas M, Yalniz Z, Akdeniz D,
Tuncer SB, Kilic S, Erdogan OS, Ciftci R, Dagoglu N, Vatansever S
and Yazici H: The expression level of fibulin-2 in the circulating
RNA (ctRNA) of epithelial tumor cells of peripheral blood and tumor
tissue of patients with metastatic lung cancer. Mol Biol Rep.
46:4001–4008. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
WalyEldeen AA, Sabet S, Anis SE, Stein T
and Ibrahim AM: FBLN2 is associated with basal cell markers Krt14
and ITGB1 in mouse mammary epithelial cells and has a preferential
expression in molecular subtypes of human breast cancer. Breast
Cancer Res Treat. 208:6872024. View Article : Google Scholar
|
|
106
|
Setiawati Y, Alimuddin T, Mulyani H and
Kamelia M: The prognostic role of fibulin-2 and Ki-67 index in
patients with meningioma: A study among minangkabau ethnicity.
Asian Pac J Cancer Prev. 25:2735–2742. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Ibrahim AM, Roshdy M, Elshorbagy S, Hosny
M, Halawa S, Yehia D, Elfawy HA, Eldessouki A, Mohamed F, Ellithy
A, et al: An investigation of fibulin-2 in hypertrophic
cardiomyopathy. Int J Mol Sci. 21:71762020. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Li S, Jiang H, Xing W, Wang S, Zhang Y, Li
Y, Mao C, Zeng D, Lan P, Tang D, et al: A clinical diagnostic
study: Fibulin-2 is a novel promising biomarker for predicting
infection. Infect Dis Ther. 11:1057–1073. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Knittel T, Kobold D, Piscaglia F, Saile B,
Neubauer K, Mehde M, Timpl R and Ramadori G: Localization of liver
myofibroblasts and hepatic stellate cells in normal and diseased
rat livers: Distinct roles of (myo-)fibroblast subpopulations in
hepatic tissue repair. Histochem Cell Biol. 112:387–401. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Li SD, Xing W, Wang SC, Li YB, Jiang H,
Zheng HX, Li XM, Yang J, Guo DB, Xie XY, et al: Fibulin2: A
negative regulator of BMSC osteogenic differentiation in infected
bone fracture healing. Exp Mol Med. 55:443–456. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Papon MA, Le Feuvre Y, Barreda-Gómez G,
Favereaux A, Farrugia F, Bouali-Benazzouz R, Nagy F,
Rodríguez-Puertas R and Landry M: Spinal inhibition of GABAB
receptors by the extracellular matrix protein fibulin-2 in
neuropathic rats. Front Cell Neurosci. 14:2142020. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Ghorbani S, Li C, Lozinski BM, Moezzi D,
D'Mello C, Dong Y, Visser F, Li H, Silva C, Khakpour M, et al:
Fibulin-2 is an extracellular matrix inhibitor of oligodendrocytes
relevant to multiple sclerosis. J Clin Invest. 134:e1769102024.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Sicot FX, Tsuda T, Markova D, Klement JF,
Arita M, Zhang RZ, Pan TC, Mecham RP, Birk DE and Chu ML: Fibulin-2
is dispensable for mouse development and elastic fiber formation.
Mol Cell Biol. 28:1061–1067. 2008. View Article : Google Scholar :
|
|
114
|
Zhang H, Wu J, Dong H, Khan SA, Chu ML and
Tsuda T: Fibulin-2 deficiency attenuates angiotensin II-induced
cardiac hypertrophy by reducing transforming growth factor-β
signaling. Clin Sci (Lond). 126:275–288. 2014. View Article : Google Scholar
|
|
115
|
Tsuda T, Wu J, Gao E, Joyce J, Markova D,
Dong H, Liu Y, Zhang H, Zou Y, Gao F, et al: Loss of fibulin-2
protects against progressive ventricular dysfunction after
myocardial infarction. J Mol Cell Cardiol. 52:273–282. 2012.
View Article : Google Scholar :
|
|
116
|
Fässler R, Sasaki T, Timpl R, Chu ML and
Werner S: Differential regulation of fibulin, tenascin-C, and
nidogen expression during wound healing of normal and
glucocorticoid-treated mice. Exp Cell Res. 222:111–116. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Kida Y, Asahina K, Inoue K, Kawada N,
Yoshizato K, Wake K and Sato T: Characterization of vitamin
A-storing cells in mouse fibrous kidneys using Cygb/STAP as a
marker of activated stellate cells. Arch Histol Cytol. 70:95–106.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Piscaglia F, Dudás J, Knittel T, Di Rocco
P, Kobold D, Saile B, Zocco MA, Timpl R and Ramadori G: Expression
of ECM proteins fibulin-1 and -2 in acute and chronic liver disease
and in cultured rat liver cells. Cell Tissue Res. 337:449–462.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Zhang Y, Zhang W, Zhang R and Xia Y:
Knockdown of FBLN2 suppresses TGF-β1-induced MRC-5 cell migration
and fibrosis by downregulating VTN. Tissue Cell. 81:1020052023.
View Article : Google Scholar
|
|
120
|
Li S, Jiang H, Wang S, Li Y, Guo D, Zhan
J, Li Q, Meng H, Chen A, Chen L, et al: Fibulin-2: A potential
regulator of immune dysfunction after bone trauma. Immun Inflamm
Dis. 11:e8462023. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Radice PD, Mathieu P, Leal MC, Farías MI,
Ferrari C, Puntel M, Salibe M, Chernomoretz A and Pitossi FJ:
Fibulin-2 is a key mediator of the pro-neurogenic effect of
TGF-beta1 on adult neural stem cells. Mol Cell Neurosci. 67:75–83.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Patel MR and Weaver AM: Astrocyte-derived
small extracellular vesicles promote synapse formation via
fibulin-2-mediated TGF-β signaling. Cell Rep. 34:1088292021.
View Article : Google Scholar
|
|
123
|
Bois PR and Grosveld GC: FKHR (FOXO1a) is
required for myotube fusion of primary mouse myoblasts. EMBO J.
22:1147–1157. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Lehka L and Rędowicz MJ: Mechanisms
regulating myoblast fusion: A multilevel interplay. Semin Cell Dev
Biol. 104:81–92. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Chan CY, Masui O, Krakovska O, Belozerov
VE, Voisin S, Ghanny S, Chen J, Moyez D, Zhu P, Evans KR, et al:
Identification of differentially regulated secretome components
during skeletal myogenesis. Mol Cell Proteomics.
10:M110.0048042011. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Ström A, Olin AI, Aspberg A and
Hultgårdh-Nilsson A: Fibulin-2 is present in murine vascular
lesions and is important for smooth muscle cell migration.
Cardiovasc Res. 69:755–763. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Ball K, Dovedi SJ, Vajjah P and Phipps A:
Strategies for clinical dose optimization of T cell-engaging
therapies in oncology. MAbs. 15:21810162023. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Gueorguieva I, Cleverly AL, Stauber A,
Pillay NS, Rodon JA, Miles CP, Yingling JM and Lahn MM: Defining a
therapeutic window for the novel TGF-β inhibitor LY2157299
monohydrate based on a pharmacokinetic/pharmacodynamic model. Br J
Clin Pharmacol. 77:796–807. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Ou FS, Michiels S, Shyr Y, Adjei AA and
Oberg AL: Biomarker discovery and validation: Statistical
considerations. J Thorac Oncol. 16:537–545. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Kraus VB: Biomarkers as drug development
tools: Discovery, validation, qualification and use. Nat Rev
Rheumatol. 14:354–362. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Zhang Z, Wu H, Chong W, Shang L, Jing C
and Li L: Liquid biopsy in gastric cancer: Predictive and
prognostic biomarkers. Cell Death Dis. 13:9032022. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Galarini R, Diana F, Moretti S, Puppini B,
Saluti G and Persic L: Development and validation of a new
qualitative ELISA screening for multiresidue detection of
sulfonamides in food and feed. Food Control. 35:300–310. 2014.
View Article : Google Scholar
|
|
133
|
Wang S, Xu B, Zhang Y and He JX:
Development of enzyme-linked immunosorbent assay (ELISA) for the
detection of neomycin residues in pig muscle, chicken muscle, egg,
fish, milk and kidney. Meat Sci. 82:53–58. 2009. View Article : Google Scholar
|
|
134
|
Petz M: Recent applications of surface
plasmon resonance biosensors for analyzing residues and
contaminants in food. Monatshefte für Chemie-Chemical Monthly.
140:953–964. 2009. View Article : Google Scholar
|
|
135
|
Ahirwar R, Bhattacharya A and Kumar S:
Unveiling the underpinnings of various non-conventional ELISA
variants: A review article. Expert Rev Mol Diagn. 22:761–774. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Moreno BH and Ribas A: Anti-programmed
cell death protein-1/ligand-1 therapy in different cancers. Br J
Cancer. 112:1421–1427. 2015. View Article : Google Scholar
|
|
137
|
Boutros C, Tarhini A, Routier E, Lambotte
O, Ladurie FL, Carbonnel F, Izzeddine H, Marabelle A, Champiat S,
Berdelou A, et al: Safety profiles of anti-CTLA-4 and anti-PD-1
antibodies alone and in combination. Nat Rev Clin Oncol.
13:473–486. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Moreno V, Hernandez T, de Miguel M, Doger
B and Calvo E: Adoptive cell therapy for solid tumors: Chimeric
antigen receptor T cells and beyond. Curr Opin Pharmacol. 59:70–84.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Yang J, Xu J, Wang W, Zhang B, Yu X and
Shi S: Epigenetic regulation in the tumor microenvironment:
Molecular mechanisms and therapeutic targets. Signal Transduct
Target Ther. 8:2102023. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Yu H, Han R, Su J, Chen H and Li D:
Multi-marker diagnosis method for early hepatocellular carcinoma
based on surface plasmon resonance. Clin Chim Acta. 502:9–14. 2020.
View Article : Google Scholar
|
|
141
|
Yuan W, Tang W, Xie Y, Wang S, Chen Y, Qi
J, Qiao Y and Ma J: New combined microRNA and protein plasmatic
biomarker panel for pancreatic cancer. Oncotarget. 7:80033–80045.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Ginghina O, Hudita A, Zamfir M, Spanu A,
Mardare M, Bondoc I, Buburuzan L, Georgescu SE, Costache M, Negrei
C, et al: Liquid biopsy and artificial intelligence as tools to
detect signatures of colorectal malignancies: A modern approach in
patient's stratification. Front Oncol. 12:8565752022. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Weng X, Gaur G and Neethirajan S: Rapid
detection of food allergens by microfluidics ELISA-based optical
sensor. Biosensors (Basel). 6:242016. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Cheng CM, Martinez AW, Gong J, Mace CR,
Phillips ST, Carrilho E, Mirica KA and Whitesides GM: Paper-based
ELISA. Angew Chem Int Ed Engl. 49:4771–4774. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Kudłak B and Wieczerzak M: Aptamer based
tools for environmental and therapeutic monitoring: A review of
developments, applications, future perspectives. Crit Rev Environ
Sci Technol. 50:816–867. 2020. View Article : Google Scholar
|
|
146
|
Bauer M, Strom M, Hammond DS and Shigdar
S: Anything you can do, I can do better: Can aptamers replace
antibodies in clinical diagnostic applications? Molecules.
24:43772019. View Article : Google Scholar : PubMed/NCBI
|