Introduction
Minimally invasive techniques for thyroidectomy have
applied various endoscopic approaches, such as through two or more
holes (1), the
axillo-bilateral-breast approach (2)
and the anterior chest wall approach (3) after the first endoscopic
parathyroidectomy in 1996. MIVAT, originally described by Miccoli,
has gradually been accepted due to its advantages, such as better
cosmetic results compared with traditional procedures and better
postoperative outcome, as well as lower medical cost (4–6). The range
of applications of MIVAT has expanded rapidly from benign disease
to malignancy.
However, the MIVAT procedure has been associated
with certain disadvantages, such as limited operative space, use of
a thick rubber drainage tube and keloid formation. To address these
issues, effective surgical techniques have been investigated; for
example, a better operative space may be provided by using a
modified retractor. Moreover, placement of a smaller drainage tube
of moderate hardness has replaced thick rubber tubes for routine
drainage; in addition to carefully selecting the operative incision
and suturing every layer inwards and crosswise, sticky dressing was
applied for tension-free repair.
The aim of this study was to retrospectively compare
the results between patients who underwent MMST and those who
underwent MIVAT, in order to establish the safety, feasibility and
aesthetic superiority of MMST.
Patients and methods
Patients and criteria
A total of 70 consecutive patients who underwent
MIVAT between April, 2008 and May, 2012 and 127 patients who
underwent MMTS between September, 2011 and October, 2014 were
enrolled in this study. The eligibility and exclusion criteria were
as previously described (7).
Preoperative preparations
All the patients underwent thyroid ultrasound and
functional examinations in order to exclude hyperthyroidism,
hypothyroidism and hyperactive adenoma. A methoxyisobutylisonitrile
scan and enhanced computed tomography were also performed to
exclude any suspected lymph node metastasis or local invasion. In
all the cases, an intraoperative frozen section examination was
performed and the paraffin-embedded sections were routinely
examined postoperatively.
Modified surgical techniques
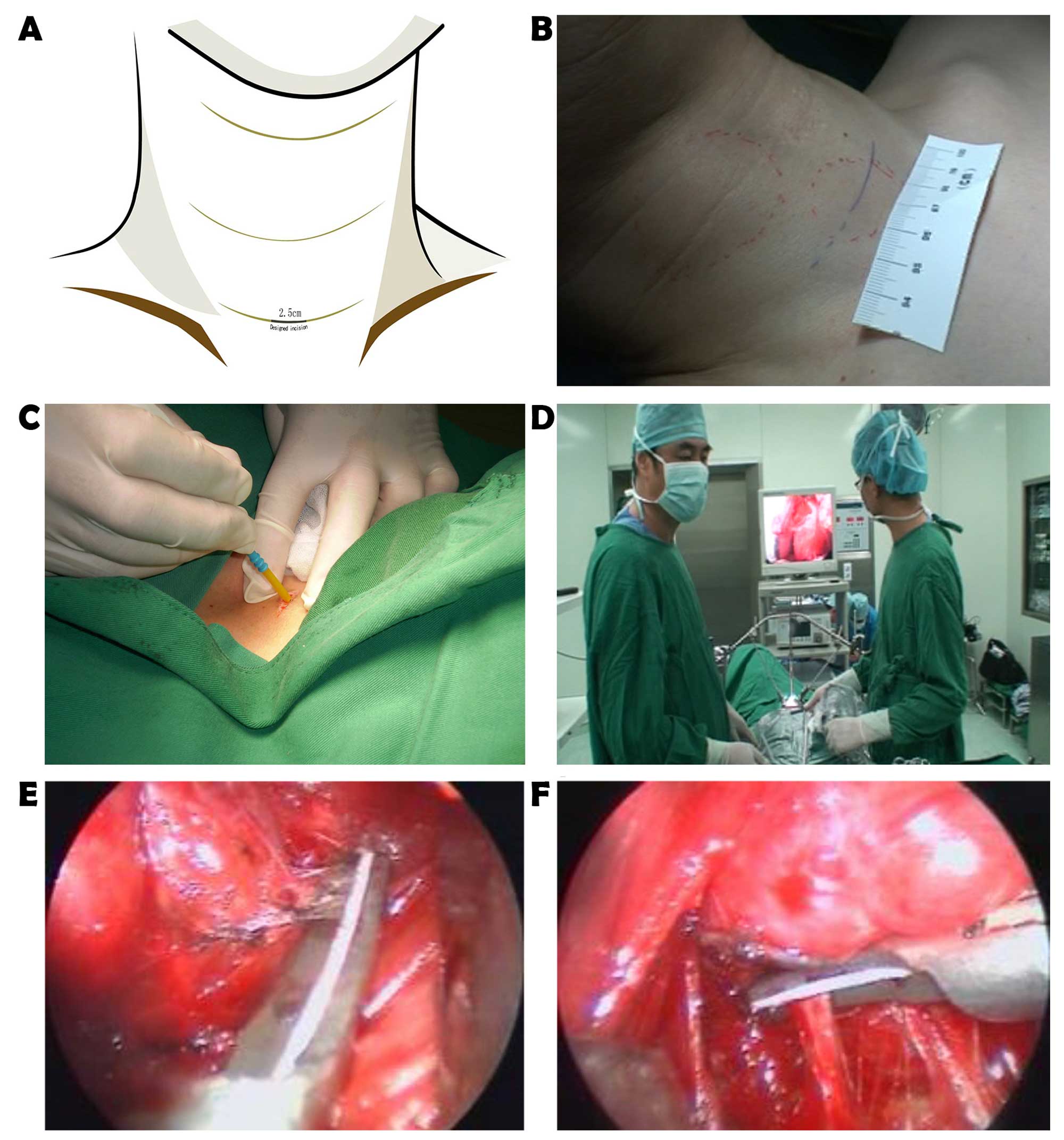
Selecting the operative incision
The incision was routinely designed in detail to
coincide with last prominent line of Langer (Fig. 1A and B), ~3.0 cm or two fingers above
the sternal notch. The primary requirement of the designed incision
was to move symmetrically along the last prominent line of Langer
(Fig. 1C).
Expanding the operative space
A gasless lifting system with modified retractors
was installed, suspended and fixed in an orderly manner (Fig. 1D). Sufficient working space was
created through a 30° (5 mm) endoscope. The procedure was performed
under endoscopic vision, with an amplified video (Fig. 1E and F) to help discriminate between
different anatomical structures.
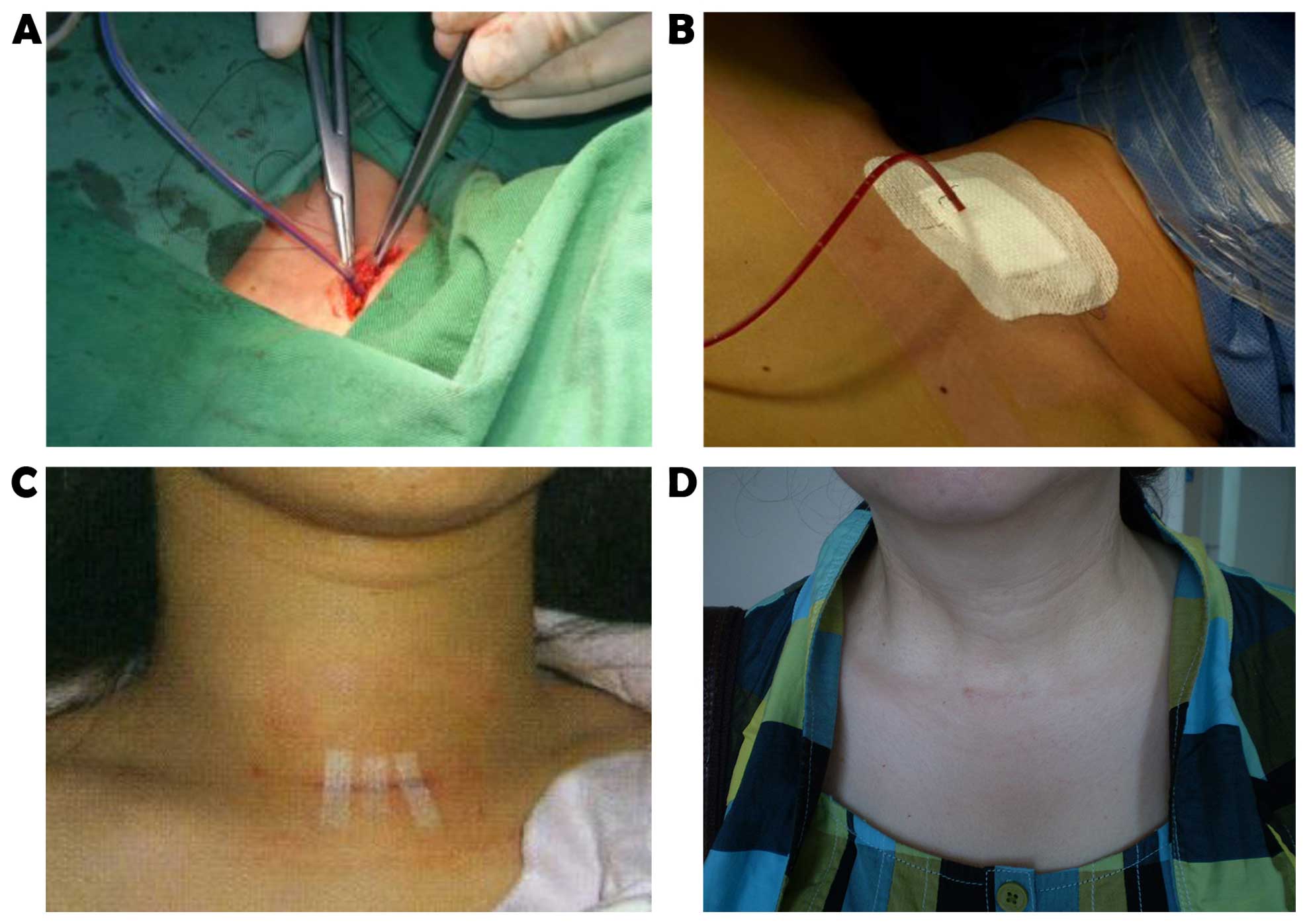
Suturing each layer inwards and crosswise
The Hunter line, fascia, platysma and subcutaneous
tissue were tightly sutured inwards and crosswise (Fig. 2A) following conventional check-up. The
skin was closed through subcuticular suturing and sticky dressing
was applied to achieve tension-free repair (Fig. 2B). The joined points of the adjacent
layers were not in the same perpendicular line, but rather
crosswise-positioned.
Placement of the drainage tube in situ
A small tube of moderate hardness, connected to a
compressible oval bulb, partly used to maintain an air-free state
for effective drainage, was carefully embedded in situ. The
steps were similar to those during conventional procedures.
Measuring cervical motion
The method for measuring the precise cervical range
of motion was previously reported by our team (7).
Statistical analysis
All the data are presented as means ± standard
deviation. Group data from the MIVAT and MMTS groups were analyzed.
The non-parametric Mann-Whitney test was used to compare the means
of the parameters. A value of P<0.01 was considered to indicate
a statistically significant difference.
Results
Patients
A consecutive series of 70 patients, including 54
benign and 16 malignant cases, initially underwent MIVAT between
April, 2008 and May, 2012, whereas 127 patients, including 98
benign and 29 malignant cases, subsequently underwent MMTS between
September, 2011 and October, 2014. The preoperative characteristics
were similar between the MMTS and MIVAT groups (Table I).
 | Table I.Clinical characteristics of all the
patients undergoing thyroid surgery. |
Table I.
Clinical characteristics of all the
patients undergoing thyroid surgery.
| Characteristics | MIVAT (n=70) | MMST (n=127) |
|---|
| Gender |
|
|
| F%
(F/M) | 77.14 (54/16) | 77.95 (99/28) |
| Age (years) |
|
|
| Mean ±
SD | 45±9 | 46±10 |
|
Range | 22–60 | 22–65 |
| Max tumor diameter
(cm) |
|
|
| Mean ±
SD | 1.8±0.9 | 1.8±0.8 |
|
Range | 0.2–3.5 | 0.2–3.5 |
| Location of
tumors |
|
|
| L%
(R/L) | 54.29 (38/32) | 53.54 (68/59) |
Surgical results
General anesthesia was applied to all the patients
and no cases were converted to conventional thyroidectomy. All the
MMTS and MIVAT procedures were performed by the same surgeon. The
surgical parameters, including operative time, blood loss,
postoperative drainage, peak angle of cervical rotation, length of
hospitalization and cosmetic satisfaction, are listed in Table II. Two cases of recurrent laryngeal
nerve palsy and 1 case of transient hypocalcemia at the beginning
of MIVAT recovered following symptomatic treatment. A 12-month
follow-up was required, including thyroid ultrasonography and
function. The serum thyroglobulin level was measured in patients
with malignant lesions. The cosmetic results of MMTS were visible
on the 3rd day (Fig. 2C) and the 1st
month (Fig. 2D) postoperatively.
 | Table II.Intraoperative and follow-up data. |
Table II.
Intraoperative and follow-up data.
| Surgical
parameters | MIVAT (n=70) | MMST (n=127) | P-value |
|---|
| Operative time
(min) | 82±29 | 102±36 | <0.01 |
| Blood loss (ml) | 32.3±12.6 | 20.3±11.3 | <0.01 |
| Postoperative
drainage (ml) | 50.48±23.2 | 42.77±15.2 | <0.01 |
| Peak angle of
cervical rotation (°) | 35.3±3.8° | 38.6±4.1° | 0.25 |
| Length of
hospitalization (days) | 4.51±1.30 | 4.25±1.08 | 0.52 |
| Cosmetic satisfaction
(%) | 88.9±2.7 | 94.6±3.5 | <0.01 |
Discussion
Although MIVAT has several advantages, including
less postoperative pain, shorter hospital stay, more attractive
cosmetic results and reduced distress (8) through transforming growth factor-β serum
levels, as well as no additional risks of rupturing the capsule
with subsequent cancer cell dissemination (9) and and other thyroidectomy complications,
it also has certain disadvantages, such as narrow operative space,
use of a thick rubber drainage tube and keloid formation. Based on
MIVAT, MMST uses modified surgical techniques to achieve better
results and cosmetic satisfaction.
The issue of the thyroidectomy incision was
investigated several decades prior. Desault first initiated an
anterior median longitudinal incision; next, a similarly lateral
incision but parallel to the inner border of the
sternocleidomastoid muscle was planned by Billroth; his junior,
Kocher, established an 8–10 cm collar incision that became popular
in the 20th century (10). Recently,
Miccoli introduced the MIVAT procedure (11), which revolutionized minimally invasive
thyroidectomy. A 1.5-cm horizontal incision placed 2 cm above the
sternal notch is associated with less trauma, compared to other
approaches. However, the standards of the incision have not been
clearly determined, except for a study reporting that, if placed
<2 cm or one fingerbreadth away from the sternal notch,
particularly on the manubrium, the incision may result in a
hypertrophic scar or keloid (12). In
addition, a precise measurable approach was introduced to determine
optimal incision placement between the cricoid cartilage and the
sternal notch (13). By contrast,
another previous study indicated that the incision migrates in
different positions (14). Of note,
migration of the incision of ~9 mm downwards was observed during
postoperative follow-up when changing the body position from
upright to supine in a preliminary study (15). Furthermore, cosmetic principles
suggest that the remaining incision may result in a hypertrophic
scar or keloid when deviating away from the Langer's line and
recommend using pre-existing neck creases to better hide the
incisions. Therefore, the incision in our department was designed
to coincide with the last prominent Langer's line, between the
cricoid cartilage and the sternal notch, and was individualized as
required.
In practice, cervical motion is considered to be
negatively correlated with postoperative pain, and may be a useful
parameter to monitor functional recovery; however, this is not a
simple and rapid way to evaluate drainage, incision length and
duration of hospitalization in clinical practice and only a limited
number of studies consider this parameter. The quantifiable angle
from the submental area to the maximal degree bilaterally was noted
after our patients were encouraged to move their heads, which may
be used to measure injuries directly.
Despite the possibility of drainage tube-related
damage to the laryngeal nerve and tube blocking by clots, drainage
is crucial for preventing hematoma formation from the slow
extravasation of blood and lymph fluid in a closed and narrow
space. Placing a smaller drainage tube in the thyroid bed is now
routinely practiced. Moreover, the air-free state of the smaller
tube makes drainage more effective from each layer.
Finally, as an independent indicator reported by
Sabuncuoglu et al (16), scar
tissue formation of <3 cm is important for cosmetic
satisfaction. Therefore, it is crucial for clinicians to study the
characteristics of keloid formation.
In conclusion, MMTS is feasible and safe for the
treatment of benign and/or malignant thyroid nodules, similar to
MIVAT. Furthermore, MMST is associated with less trauma and higher
cosmetic satisfaction compared with MIVAT. However, further
investigation is required to confirm the long-term outcome and more
attention should be focused on keloid formation.
References
|
1
|
Pai SI and Tufano RP: Central compartment
neck dissection for thyroid cancer. Technical considerations. ORL J
Otorhinolaryngol Relat Spec. 70:292–297. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bärlehner E and Benhidjeb T: Cervical
scarless endoscopic thyroidectomy: Axillo-bilateral-breast approach
(ABBA). Surg Endosc. 22:154–157. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nakano S, Kijima Y, Owaki T, Shirao K,
Baba M and Aikou T: Anterior chest wall approach for video-assisted
thyroidectomy using a modifed neck skin lifting method. Biomed
Pharmacother. 56 (Suppl 1):96S–99S. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Timon C and Miller IS: Minimally invasive
video-assisted thyroidectomy: Indications and technique.
Laryngoscope. 116:1046–1049. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lombardi CP, Raffaelli M, Princi P, De
Crea C and Bellantone R: Video-assisted thyroidectomy: Report on
the experience of a single center in more than four hundred cases.
World J Surg. 30:794–801. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miccoli B, Berti P, Bendinelli C, Conte M,
Fasolini F and Martino E: Minimally invasive video-assisted surgery
of the thyroid: A preliminary report. Lange becks Arch Surg.
385:261–264. 2000. View Article : Google Scholar
|
|
7
|
Yu JJ, Bao SL, Yu SL, Zhang DQ, Loo WT,
Chow LW, Su L, Cui Z, Chen K, Ma LQ, et al: Minimally invasive
video-assisted thyroidectomy for the early-stage differential
thyroid carcinoma. J Transl Med. 10 (Suppl 1):S132012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Elaraj DM and Clark OH: Changing
management in patients with papillary thyroid cancer. Curr Treat
Options Oncol. 8:305–313. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Miccoli P, Berti P, Raffaelli M, Materazzi
G, Baldacci S and Rossi G: Comparison between minimally invasive
video-assisted thyroidectomy and conventional thyroidectomy: A
prospective randomized study. Surgery. 130:1039–1043. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Thompson NW, Olsenn WR and Hoffman GL: The
continuing development of the technique of thyroidectomy. Surgery.
73:913–927. 1973.PubMed/NCBI
|
|
11
|
Pinchot S, Chen H and Sippel R: Incisions
and exposure of the neck for thyroidectomy and parathyroidectomy.
Operat Tech Gen Surg. 10:63–76. 2008. View Article : Google Scholar
|
|
12
|
Scott-Conner CE and Dawson DL: Operative
anatomy. 1st. JB Lippincott Company; Philadelphia, PA: pp.
388–1993
|
|
13
|
Xiao GZ and Gao L: A simple method for
determining an optimal incision for minimally invasive
video-assisted thyroidectomy. Surg Endosc. 22:2100–2101. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jancewicz S, Sidhu S, Jalaludin B and
Campbell P: Optimal position for a cervical collar incision: A
prospective study. ANZ J Surg. 72:15–17. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yu H, Yang YZ, Zhang DQ, Cui Z and Yu JJ:
Analysis of cervical dermatoglyph and related factors. Chin Arch
Gen Surg. 4:571–572. 2010.
|
|
16
|
Sabuncuoglu MZ, Sabuncuoglu A, Sozen I,
Benzin MF, Cakir T and Cetin R: Minimally invasive surgery using
mini anterior incision for thyroid diseases: A prospective cohort
study. Int J Clin Exp Med. 7:3404–3409. 2014.PubMed/NCBI
|