Introduction
Over several years, the majority of studies on
breast carcinoma have focused only on the epithelial component;
however, the tumor-associated stroma and particularly the
cancer-associated fibroblasts (CAFs) have been found to play a
crucial role in cancer pathogenesis (1,2).
We previously demonstrated that the majority of
these CAFs were smooth muscle actin (SMA)-positive, with a
myofibroblastic-like phenotype, and that the presence of these
peritumoral myofibroblasts (PMYs) is crucial for in situ and
invasive breast carcinoma of no special type (NST), as well in
metastatic disease (3,4). The origin of PMYs remains debatable, but
we previously demonstrated that the resident CD34-positive breast
fibroblasts are able to acquire SMA myofibroblastic characteristics
under the control of the transforming growth factor β-1 pathway
(3). It was suggested that these PMYs
promote tumor invasion, growth and angiogenesis through paracrine
factors and/or direct cell-cell crosstalk (5). Therefore, it was suggested that
CAFs/PMYs potentially secrete various proteins, particularly matrix
metalloproteinase 2 (MMP2), to facilitate tumor invasion (6,7). To
elucidate this issue, we immunohistochemically analyzed the
expression of MMP2 in normal breast stromal fibroblasts and in
CAFs/PMYs present in invasive breast carcinoma of NST, according to
clinicopathological variables. Our data were reviewed according to
the highlights of the recent literature.
Materials and methods
Specimens
Formalin-fixed, paraffin-embedded postsurgical
specimens from human breast carcinomas were retrieved from the
archives of the Department of Pathology, Erasme University
Hospital-Université Libre de Bruxelles (Brussels, Belgium). A total
of 155 patients with invasive breast carcinoma of NST, who
underwent surgery between 1997 and 2004, were randomly selected. A
total of 20 specimens of normal breast tissue obtained from women
who underwent resection for plastic surgery were also included in
the study as controls. This study was approved by the Ethics
Committee of Erasme University Hospital (reference no. P2014/418).
The pathological stage and grade were defined according to the 2014
criteria of the World Heath Organization (8). A clinically positive test for estrogen
and progesterone nuclear receptors (ER and PR, respectively) was
defined as nuclear staining in ≥1% of the tumor cells, as
previously described (9). Human
epidermal growth factor receptor 2 (HER2) immunoreactivity was
performed using the Oracle HER2 test (clone CB11; Leica
Microsystems GmbH, Wetzlar, Germany) according to the
manufacturer's instructions, and scoring was performed according to
the recommendations of the American Society of Clinical Oncology
(10). All HER2 scores of 2+ and 3+
were analyzed using the fluorescent in situ hybridization
(FISH) PathVysion HER2 DNA test (Abbott Laboratories, Abbott Park,
IL, USA) according to the manufacturer's instructions. Signal
ratios (HER2/chromosome 17 centromere) of ≥2 were classified as
amplified. In the present study, only 2+ and 3+ tumors with HER2
FISH amplification were considered as positive. A subtype
immunohistochemical classification, as previously described with
certain modifications (11), was
adopted to characterize the tumors as follows: Luminal A (either
one or both ER and PR present, HER2-negative and Ki-67 ≤14%);
luminal B (one or both ER and PR present, HER2-negative and Ki-67
>14%); luminal-HER2 (one or both ER and PR present,
HER2-positive, irrespective of the Ki-67 index); HER2-positive (ER
and PR absent, HER2-positive, irrespective of the Ki-67 index); and
triple-negative (ER and PR absent and HER2-negative).
Immunostaining for MMP2 (clone 17B11, dilution 1:30;
Leica Microsystems GmbH) was performed using a fully automated
immunohistochemical system (Autostainer Link A48; Dako, Glostrup,
Denmark).
A two-grade system was used to score the stromal
expression of MMP2, which was classified as positive or negative
according to a cut-off of 10%.
Statistical analysis
The Chi-square or Fisher's exact tests were used to
statistically compare the clinicopathological variables described
in the Table I. P<0.05 was
considered to indicate a statistically significant difference.
 | Table I.Clinicopathological chracateristics of
the 155 patients included in the study. |
Table I.
Clinicopathological chracateristics of
the 155 patients included in the study.
| Characteristics | Total cases, no. (%)
(n=155) |
|---|
| Age (years) |
|
|
<50 | 46
(30) |
| ≥50 | 109 (70) |
| Tumor size (mm) |
|
| ≤20 | 90
(58) |
|
>20 | 65
(42) |
| Lymph node
status |
|
|
Negative | 87
(56) |
|
Positive | 68
(44) |
| Histological
grade |
|
| 1 | 27
(17) |
| 2 | 63
(41) |
| 3 | 65
(42) |
| ER status |
|
|
Negative | 21
(14) |
|
Positive | 134 (86) |
| PR status |
|
|
Negative | 37
(24) |
|
Positive | 118 (76) |
| HER2 status |
|
|
Negative | 126 (81) |
|
Positive | 29
(19) |
| Ki-67 |
|
|
<15% | 35
(23) |
| ≥15% | 120 (77) |
| Molecular
subtypes |
|
| Luminal
A | 34
(22) |
| Luminal
B | 86
(55) |
|
Luminal-HER2 | 19
(12) |
|
HER2-enriched | 10 (7) |
|
Triple-negative | 6
(4) |
Results
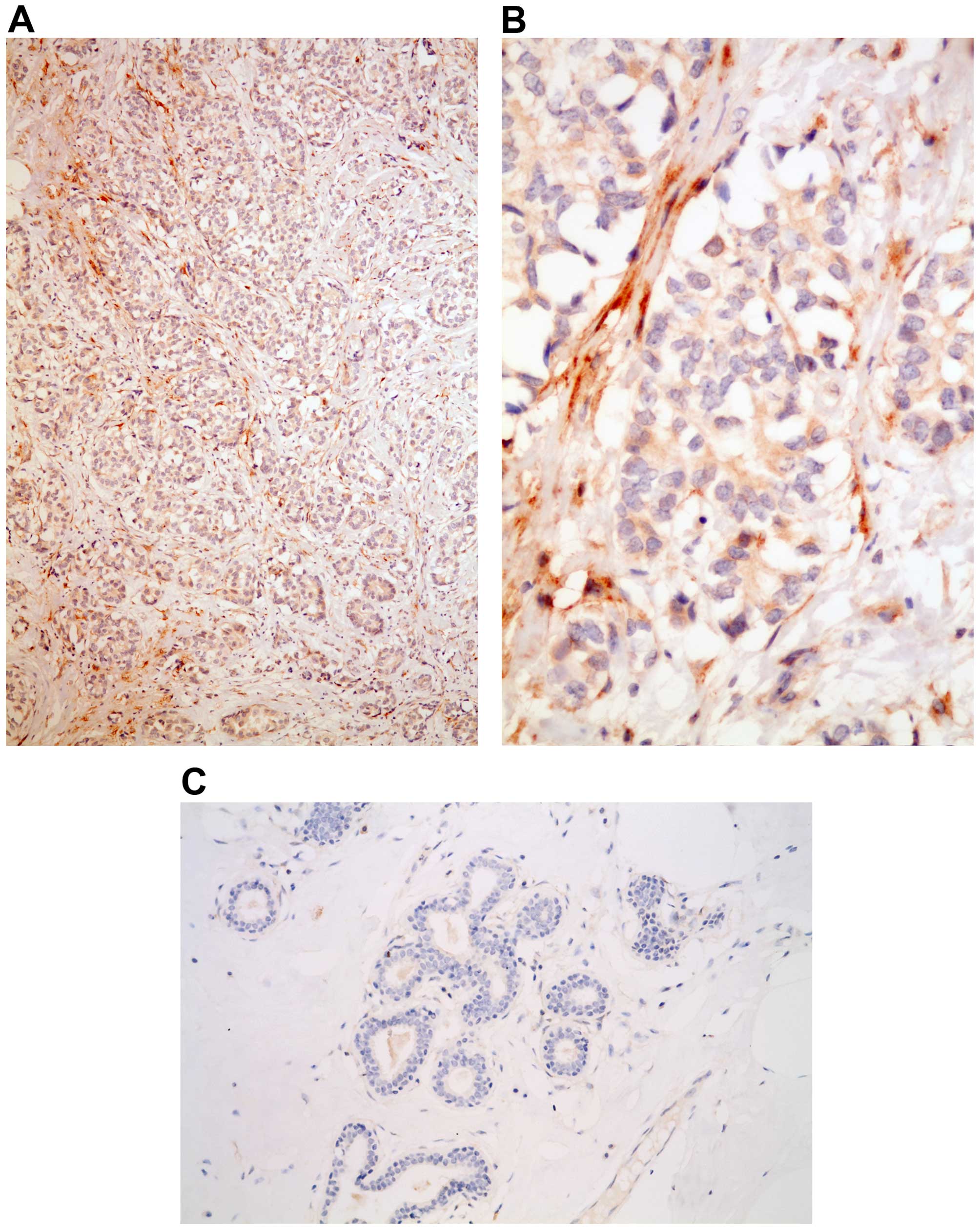
Stromal MMP2 expression
No MMP2 expression was observed in the stroma
surrounding normal breast acini or ductal units (Fig. 1). By contrast, MMP2 expression was
present in the peritumoral stroma in 24 of the 155 cases (15%) of
invasive breast carcinoma (Fig. 1).
According to the different clinical parameters, there was no
correlation between MMP2 stromal expression and patient age,
histological grade, lymph node involvement, ER/PR positivity, or
Ki-67 index. Conversely, MMP2 stromal expression was statistically
significantly different in tumors sized ≤20 mm (21% positivity)
compared with tumors >20 mm (8% positivity) (P=0.02). In
addition, stromal expression in HER2-positive carcinomas was more
frequent compared with that in in HER2-negative tumors (35 vs. 12%,
respectively; P=0.002). Finally, according to the subtype
immunohistochemical classification surrogates of molecular classes,
MMP2 stromal expression appeared more frequently by decreasing
order in luminal-HER2 (37%), HER2-enriched (30%), triple-negative
(17%), luminal B (13%) and luminal A (6%) tumors (P=0.025)
(Table II).
 | Table II.MMP2 stromal expression according to
the different clinicopathological characteristics. |
Table II.
MMP2 stromal expression according to
the different clinicopathological characteristics.
|
| MMP2 expression,
no. |
|
|---|
|
|
|
|
|---|
| Characteristics | Positive | Negative | P-value |
|---|
| Age (years) |
|
| 0.95 |
| ≤50 | 7 | 39 |
|
|
>50 | 17 | 92 |
|
| Tumor size (mm) |
|
| 0.02 |
| ≤20 | 19 | 71 |
|
|
>20 | 5 | 60 |
|
| Lymph node
status |
|
| 0.11 |
|
Negative | 17 | 70 |
|
|
Positive | 7 | 61 |
|
| Histological
grade |
|
| 0.17 |
| 1 | 2 | 25 |
|
| 2 | 8 | 55 |
|
| 3 | 14 | 51 |
|
| ER status |
|
| 0.075 |
|
Negative | 6 | 15 |
|
|
Positive | 18 | 116 |
|
| PR status |
|
| 0.09 |
|
Negative | 9 | 28 |
|
|
Positive | 15 | 103 |
|
| HER2 status |
|
| 0.002 |
|
Negative | 14 | 112 |
|
|
Positive | 10 | 19 |
|
| Ki-67 |
|
| 0.45 |
|
<15% | 4 | 31 |
|
| ≥15% | 20 | 100 |
|
| Molecular
subtypes |
|
| 0.025 |
| Luminal
A | 2 | 32 |
|
| Luminal
B | 11 | 75 |
|
|
Luminal-HER2 | 7 | 12 |
|
|
HER2-enriched | 3 |
7 |
|
|
Triple-negative | 1 |
5 |
|
Discussion
Several recent studies support the hypothesis that,
in invasive breast carcinoma, the gene expression profile of the
epithelial component and, therefore, the immunohistochemical
profile surrogates of molecular classes, represent biologically
distinct diseases with different response to therapy and clinical
outcome (12,13). In addition to the epithelial cell
autonomous processes, it has been hypothesized that the tumor
microenvironment, and particularly CAFs, are able to promote tumor
cell proliferation, angiogenesis and metastasis (3,4,14). Certain breast CAFs, which are
characterized by SMA expression and are referred to as PMYs, appear
to play an important role in metastasis, including lymph node
metastasis (3,4). Therefore, similar to the epithelial
counterpart, it was hypothesized that the tumor's aggressiveness
may be affected by the stromal composition, as well as the stroma's
own biological properties (‘stromal signature’) (15,16). In
the present study, we demonstrated that the stromal expression of
MMP2, which is known to promote cancer invasion and metastasis by
degrading various components of the extracellular matrix, varies
according to the different tumor subtypes. In particular, in
HER2-positive (luminal-HER2 and HER2-enriched) and triple-negative
tumors, stromal expression of MMP2 was more frequently detected
compared with the luminal subtypes (Table II). Of note, it was recently
indicated that, on multivariate analysis, luminal-HER2,
HER2-enriched and triple-negative tumors are associated with a
higher rate of distant metastasis, including brain, liver and lung
metastases (13,17). Therefore, the metastatic potential may
be determined by the intrinsic properties of the epithelial
component of the different breast tumor subtypes, as well as by the
stromal properties of the microenvironment, as in the present case,
by expressing different MMP2 levels, which have been implicated in
the degradation of extracellular matrix and the enhancement of
tumor cell motility (18,19,7,20). In conclusion, different stromal
properties, such as MMP2 expression, may predispose the different
histological breast tumor subtypes to different metastatic
outcomes. Further studies are in progress, with the aim to
accurately characterize stromal properties based on breast cancer
subtype classification.
References
|
1
|
Luo H, Tu G, Liu Z and Liu M:
Cancer-associated fibroblasts: A multifaceted driver of breast
cancer progression. Cancer Lett. 361:155–163. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Han Y, Zhang Y, Jia T and Sun Y: Molecular
mechanism underlying the tumor-promoting functions of
carcinoma-associated fibroblasts. Tumour Biol. 36:1385–1394. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Catteau X, Simon P and Noël JC:
Myofibroblastic stromal reaction and lymph node status in invasive
breast carcinoma: Possible role of the TGF-β1/TGF-βR1 pathway. BMC
Cancer. 14:4992014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Catteau X, Simon P and Noël JC:
Myofibroblastic reaction is a common event in metastatic disease of
breast carcinoma: A descriptive study. Diagn Pathol. 9:1962014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kohlhapp FJ, Mitra AK, Lengyel E and Peter
ME: MicroRNAs as mediators and communicators between cancer cells
and the tumor microenvironment. Oncogene April. 13:2015.(Epub ahead
of print).
|
|
6
|
Hassona Y, Cirillo N, Heesom K, Parkinson
EK and Prime SS: Senescent cancer-associated fibroblasts secrete
active MMP-2 that promotes keratinocyte dis-cohesion and invasion.
Br J Cancer. 111:1230–1237. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jezierska A and Motyl T: Matrix
metalloproteinase-2 involvement in breast cancer progression: A
mini-review. Med Sci Monit. 15:RA32–RA40. 2009.PubMed/NCBI
|
|
8
|
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH
and van de Vijver MJ: Invasive breast carcinoma: Introduction and
general features. WHO Classification of Tumours. 4:(4th). (Lyon).
IARC Press. 19–22. 2012.
|
|
9
|
Hammond ME, Hayes DF, Dowsett M, Allred
DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS,
Hayes M, et al: American Society of Clinical Oncology/College of
American Pathologists guideline recommendations for
immunohistochemical testing of estrogen and progesterone receptors
in breast cancer. J Clin Oncol. 28:2784–2795. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wolff AC, Hammond ME, Hicks DG, Dowsett M,
McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M,
Fitzgibbons P, et al: Recommendations for human epidermal growth
factor receptor 2 testing in breast cancer: American Society of
Clinical Oncology/College of American Pathologists clinical
practice guideline update. J Clin Oncol. 31:3997–4013. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Preat F, Simon P and Noel JC: Differences
in breast carcinoma immunohistochemical subtypes between immigrant
Arab and European women. Diagn Pathol. 9:262014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sihto H, Lundin J, Lundin M, Lehtimäki T,
Ristimäki A, Holli K, Sailas L, Kataja V, Turpeenniemi-Hujanen T,
Isola J, et al: Breast cancer biological subtypes and protein
expression predict for the preferential distant metastasis sites: A
nationwide cohort study. Breast Cancer Res. 13:R872011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kennecke H, Yerushalmi R, Woods R, Cheang
MC, Voduc D, Speers CH, Nielsen TO and Gelmon K: Metastatic
behavior of breast cancer subtypes. J Clin Oncol. 28:3271–3277.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
De Wever O, Demetter P, Mareel M and
Bracke M: Stromal myofibroblasts are drivers of invasive cancer
growth. Int J Cancer. 123:2229–2238. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Finak G, Bertos N, Pepin F, Sadekova S,
Souleimanova M, Zhao H, Chen H, Omeroglu G, Hallett M and Park M:
Stromal gene expression predicts clinical outcome in breast cancer.
Nat Med. 14:518–527. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Farmer P, Bonnefoi H, Anderle P, Cameron
D, Wirapati P, Becette V, André S, Piccart M, Campone M, Brain E,
et al: A stroma-related gene signature predicts resistance to
neoadjuvant chemotherapy in breast cancer. Nat Med. 15:68–74. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gupta GP and Massagué J: Cancer
metastasis: Building a framework. Cell. 127:679–695. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Duffy MJ, Maguire TM, Hill A, McDermott E
and O'Higgins N: Metalloproteinases: Role in breast carcinogenesis,
invasion and metastasis. Breast Cancer Res. 2:252–257. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jones JL, Glynn P and Walker RA:
Expression of MMP-2 and MMP-9, their inhibitors and the activator
MT1-MMP in primary breast carcinomas. J Pathol. 189:161–168. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Thompson EW, Yu M, Bueno J, Jin L, Maiti
SN, Palao-Marco FL, Pulyaeva H, Tamborlane JW, Tirgari R and Wapnir
I: Collagen induced MMP-2 activation in human breast cancer. Breast
Cancer Res Treat. 31:357–370. 1994. View Article : Google Scholar : PubMed/NCBI
|