Introduction
Endometriosis is defined as the presence of
endometrial glands and stroma outside the uterine cavity.
Endometriosis is a common disease affecting ~10% of women of
reproductive age. The lesions are mainly located in the ovaries,
peritoneal cavity, recto-uterine pouch and extrapelvic areas.
Malignant transformation is a rare complication of endometriosis,
occurring in 0.6–0.8% of all cases (1). Clinical characteristics of
endometriosis-associated ovarian cancer (EAOC) are frequently
observed in ovarian endometrioma (OE). Ovarian clear cell carcinoma
is the most frequent form of EAOC in Japan, followed by
endometrioid carcinoma (2).
Ultrasound remains the initial and most useful imaging method for
the detection of ovarian cancer, while magnetic resonance imaging
(MRI) is the second-line imaging modality. However, MRI is the most
optimal imaging method to distinguish between benign and malignant
ovarian cystic lesions (3). MR
criteria for the diagnosis of EAOC include the presence of a large
ovarian cyst with hemorrhagic fluid, various solid portions, mural
nodules, papillary projections, thick septations or significant
vascularization, as assessed by contrast medium administration. The
features of imaging modalities, including dynamic contrast-enhanced
imaging, high signal intensity of diffusion-weighted images and low
apparent diffusion coefficient values facilitate the diagnosis of
EAOC (4). To the best of our
knowledge, the only effective treatment to treat EAO consists in
the extensive excision of the tumor.
In addition to oncological outcomes, the management
of nulliparous women who have high risk of EAOC represents a
challenge, due to the potential impact of EAOC on their fertility.
When the patients select fertility-preserving alternatives, surgeon
must carefully consider each indication (5). In general, MRI can facilitate the
correct preoperative characterization of the lesion. However, in a
study by Tanase et al (4), it
was shown that a part of the benign mass can exhibit increased
mural nodules and solid components. For at-risk populations, MR
relaxometry is an emerging radiological technique that may improve
the prediction of EAOC occurrence (6). In a study by Yoshimoto et al
(6) transverse relaxation rate (R2)
was determined using a single-voxel, multi-echo MR sequence (HISTO)
using a 3 Tesla (3T)-MR system, and it was reported that
preoperative MR relaxometry is a useful tool for distinguishing
EAOC from benign OE.
The present study reported the case of a 42-year-old
nulliparous woman who was suspected of EAOC but desired a
fertility-sparing surgery, such as laparoscopic endometrioma
cystectomy. MR relaxometry was performed, and the MR relaxometry
results confirmed the diagnosis of EAOC.
Case presentation
The patient was a 42-year-old nulliparous woman with
a history of OE that occurred 4 years prior to admission to our
hospital. She presented mild cyclic pelvic pain, which required
admission to another clinic. She underwent hysteroscopic resection
of benign endometrial polyps 3 years prior to admission to our
hospital. The patient was admitted to the Nara Medical University
Hospital in April 2017 for the analysis of a complex bilateral
adnexal mass identified by sonographic examination. Physical
examination indicated right adnexal tenderness. The carbohydrate
antigen (CA) 125 and CA 19-9 levels at presentation were 50.4 U/ml
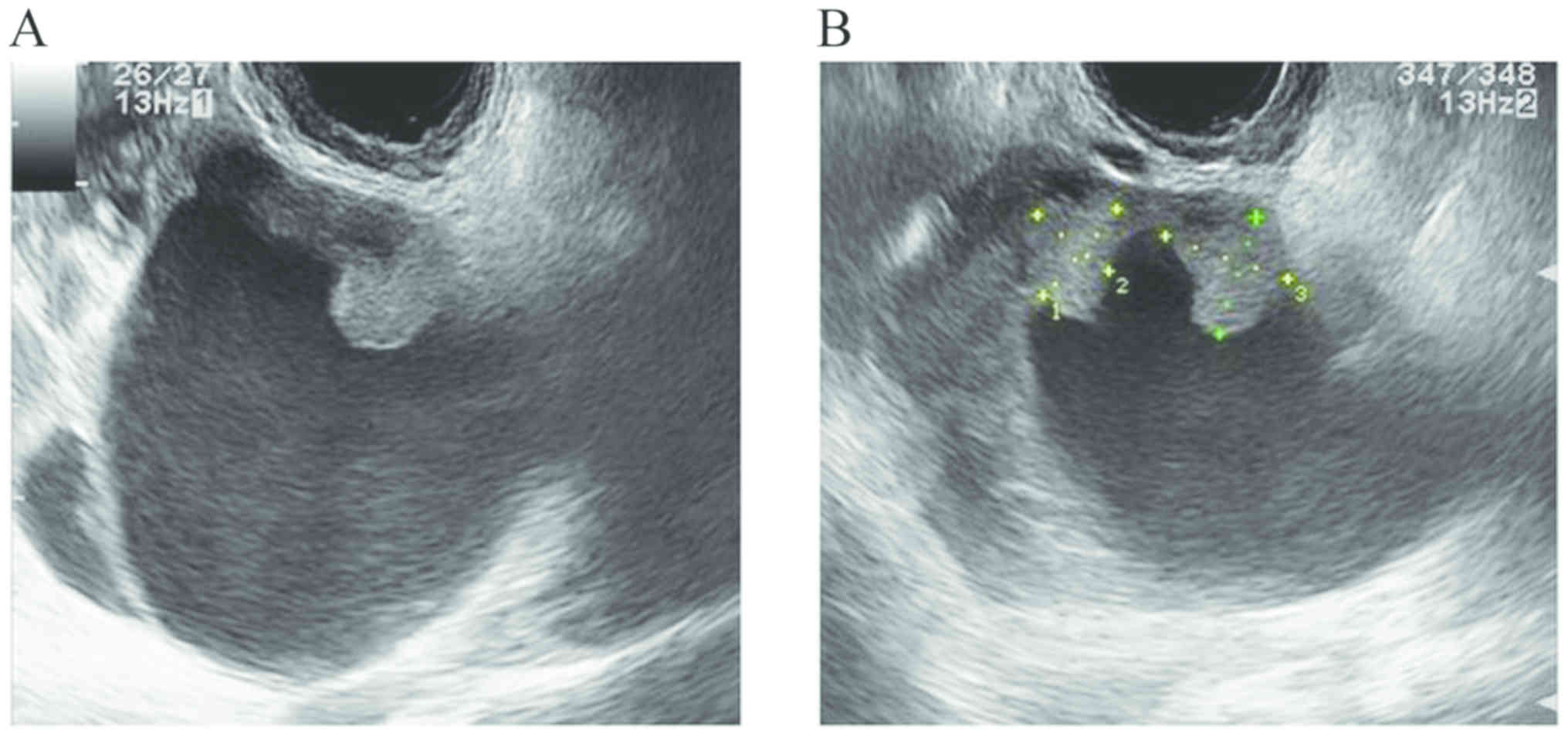
and 26.1 U/ml, respectively. Transvaginal ultrasonography, which
was performed in Kyoto University Hospital in May 2017, identified
a multilocular cystic mass with a size of ~64×52 mm in the right
ovary (Fig. 1), and one cystic mass
with a size of ~42×24 mm in the left ovary, accompanied with solid
mural nodules in the right adnexa with diameters of 12 mm. The
present findings were consistent with those of bilateral OE. The
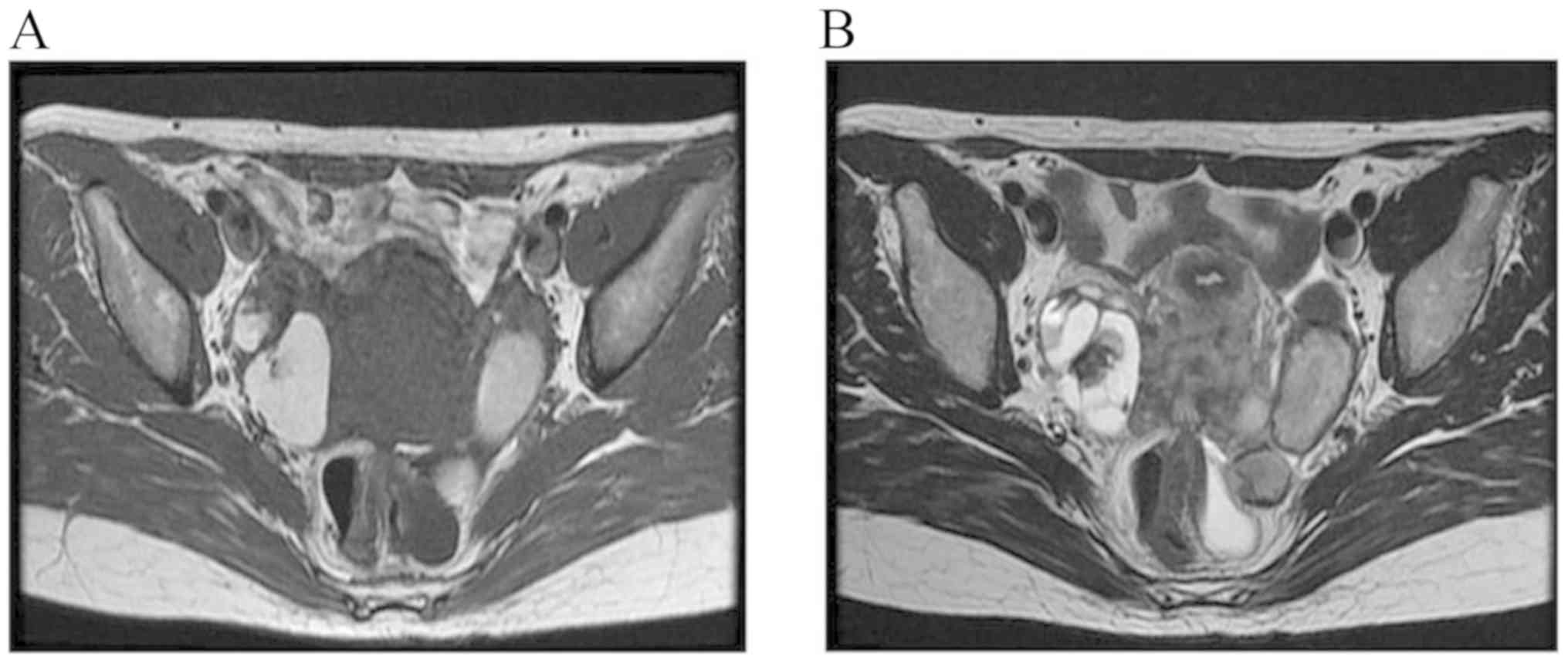
patient underwent routine MRI using T1-weighted (T1W) and
T2-weighted (T2W) sequences. The tumor exhibited areas of high
signal intensity using both T1W imaging (T1WI) and T2WI, suggestive
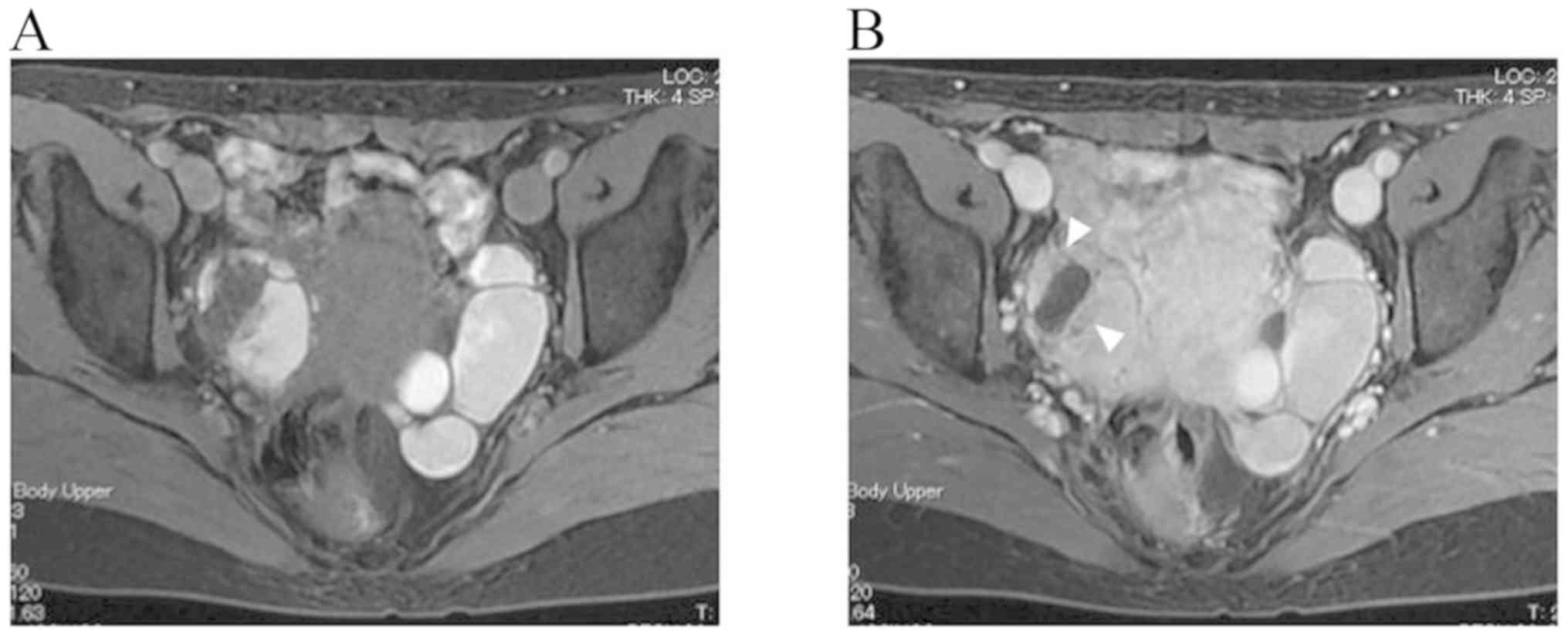
of subacute intra-cystic hemorrhage (Fig. 2). MR images of the pelvis revealed
bilateral multilocular cystic masses suggestive of mural nodules,
which showed heterogeneous enhancement on the post-contrast
fat-saturated T1WI, due to the increased vascularity in the right
adnexal mass (Fig. 3). Collectively,
these features were suggestive of a malignant transformation of
endometriosis.
The patient desired to preserve her fertility
despite the oncological hazards. A surgery that included staging,
right salpingo-oophorectomy, left cystectomy, omentectomy,
peritoneal washings and biopsies were suggested in order to perform
an accurate diagnosis, followed by retroperitoneal lymph node
dissection. However, the patient refused this treatment.
Gynecologic oncologists and radiologists advised the patient to
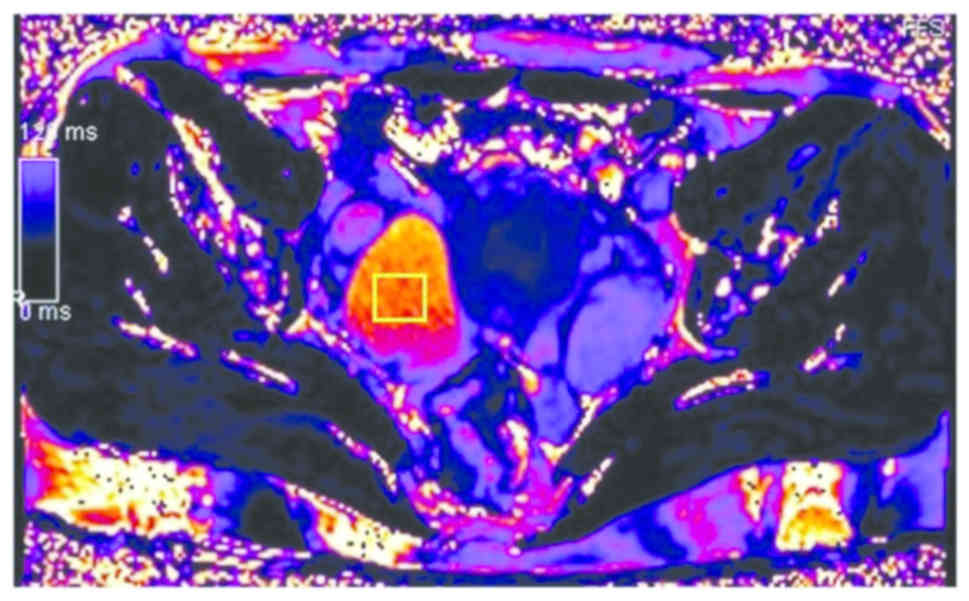
undergo MR relaxometry (MAGNETOM Skyra; 3T MRI; Siemens Healthcare
GmbH) of the pelvis. After routine MRI, the patient underwent MR
relaxometry using a single-voxel spectroscopy, a stimulated echo
acquisition mode sequence at multiple echoes, and fitting of an
exponential decay to the amplitude at each echo (6). The R2 value parameter was calculated
using a high-speed T2*-corrected HISTO using a 3T-MR system, as
previously described (6). MR
relaxometry identified an R2 value of 7.98 s−1 in the
right cyst, which suggested a malignant transformation of OE
(Fig. 4). Malignant potential was
identified by MRI only on the right side, and evaluation with MR
relaxometory on the left ovary was not performed because malignant
potential was not identified by MRI. Following MRI and MR
relaxometry, EAOC was pre-operatively diagnosed. Computed
tomography (CT) scan was performed in the previous hospital, and no
metastasis was identified. Based on these findings,
fertility-sparing surgery was contraindicated in this patient. She
underwent right salpingo-oophorectomy, left cystectomy,
omentectomy, peritoneal biopsies and retroperitoneal
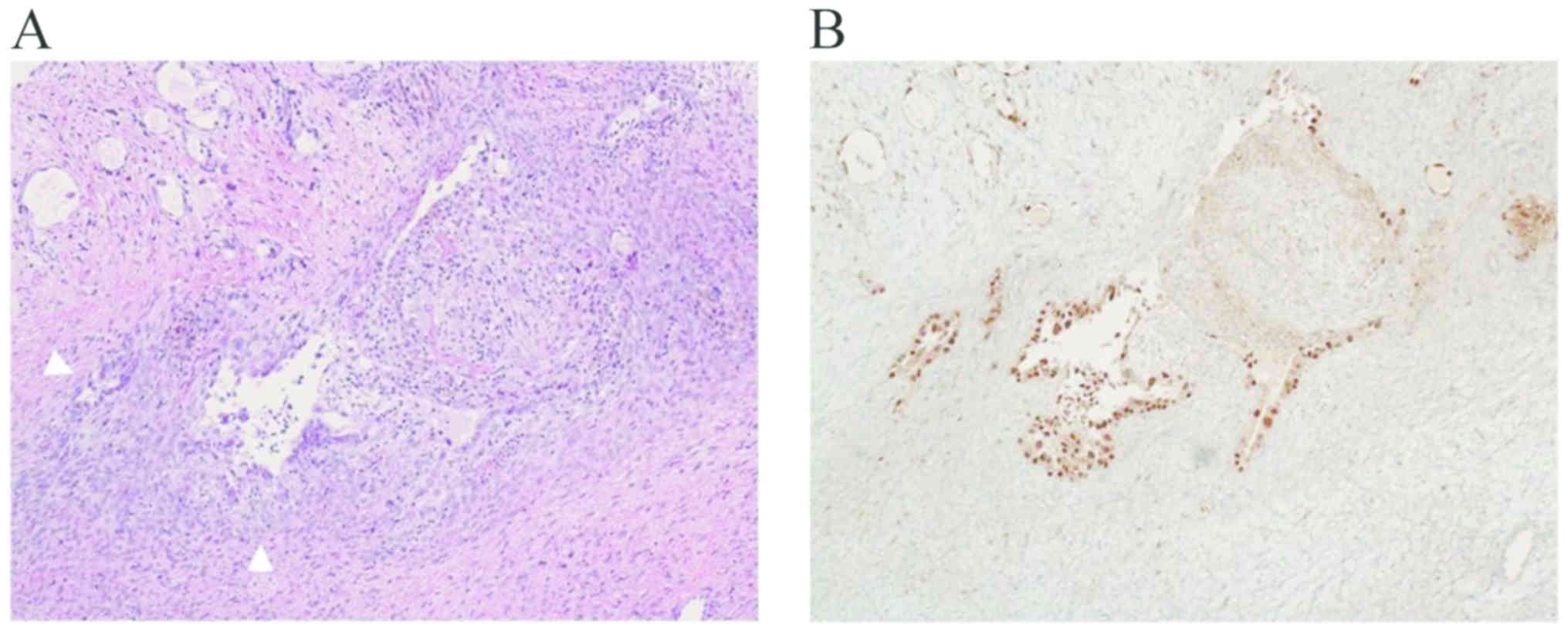
lymphadenectomy. The histopathological results identified clear
cell carcinoma arising from endometriosis (Fig. 5) at International Federation of
Gynecology and Obstetrics stage IC1 (7). The carcinoma did not extend to the
solid components within the cyst and remained limited to non-solid
regions in the cyst. Peritoneal washing results were negative for
malignant cells. Adjuvant chemotherapy was recommended, but the
patient refused it. The patient was asymptomatic without recurrence
or metastasis at the 2-year follow-up examination, which was
performed at another hospital.
Immunohistochemistry
Tissues were fixed with 10% neutral buffered
formalin-fixed at 20°C for 24 h, and paraffin-embedded tissues were
cut into 4-µm-thick sections. The slides were deparaffinized in
xylene at 20°C for 30 min and rehydrated in a graded alcohol
series. Endogenous peroxidase was inactivated with 3% hydrogen
peroxide at 20°C for 10 min. Tissue sections were incubated in 0.1
M citrate buffer (pH 6.0) and placed in an autoclave during antigen
retrieval at 125°C for 5 min. The sections were blocked with 1% BSA
diluted in PBS at 20°C for 10 min, and then incubated with a
primary antibody anti-hepatocyte nuclear factor-1β (1:500;
Sigma-Aldrich; Merck; cat. no. MABE971) at 4°C overnight and
incubated with secondary antibody hydrogen peroxidase-conjugated
(1:150; Sigma-Aldrich; Merck; cat. no. A9917) at 20°C for 60 min.
Sections were subjected to the peroxidase reaction using 0.02%
3,3′-diaminobenzidine tetrahydrochloride at 20°C for 10 min,
followed by counterstaining with hematoxylin at 20°C for 5 min.
Sections were visualized using a light microscope (magnification,
×200).
Discussion
The present case study suggested that preoperative
MR relaxometry may be a useful tool for distinguishing EAOC from
benign OE. The R2 value could guide patient selection prior to
conservative management, including fertility-sparing surgery, and
may serve as an effective parameter for the diagnosis of EAOC.
MRI has high accuracy in differentiating between
benign and malignant endometriosis (4). Malignant transformation is a rare
complication of endometriosis, affecting 0.6–0.8% of all cases of
OE (1). In Japan, clear cell
carcinoma is not uncommon and is the second most frequently
occurring type of EAOC, accounting for >20% of all EAOC cases
(8). In the present case report,
transvaginal ultrasonographic findings revealed a large pelvic mass
and solid echogenic loculi. Furthermore, based on the MRI results,
a reliable characterization of the malignant nature of the mass was
performed. Malignant transformation of endometriosis demonstrated
hemorrhage and solid projections as enhancement on postcontrast
T1WIs (9). The presence of an
enhanced soft-tissue component within a blood-filled ovarian cystic
mass was an evidence of malignant transformation. Dynamic
contrast-enhanced MRI has been shown to be useful in
differentiating malignancies from benign tumors (10). A previous study, however, has
reported that 21.4% of patients with benign OE have enhancing mural
nodules, whose pathologies include atypical endometriosis,
adenofibroma, fibrothecoma and papillary proliferation of the
epithelium (4). Therefore,
enhancement of the soft-tissue elements on dynamic
contrast-enhanced MRI would not always predict the diagnosis of
ovarian malignancy.
In addition, ovarian cancer exhibits solid mural
nodular lesions with enhancement after the intravenous
administration of a contrast medium. Pre-treatment assessment by CT
or MRI is helpful to identify patients who might benefit from
neoadjuvant chemotherapy prior to surgical management. In contrast,
a new imaging modality, MR relaxometry, can be used to
qualitatively differentiate between benign and malignant lesions.
MR relaxometry is a non-invasive, powerful tool for the direct
detection of cystic fluid iron concentration. Yoshimoto et
al (6) demonstrated that
patients with EAOC had much lower levels of iron in the cystic
fluid compared with patients with benign OE, and iron concentration
was a significant biomarker for the diagnosis of EAOC. An R2 value
<12.1 s−1 is predictive of malignancy (6). The R2 values exhibit excellent accuracy
in distinguishing between EAOC and benign OE, with 86% sensitivity
and 94% specificity (6). MR
relaxometry can allow the distinction between benign OE with an
enhancing soft-tissue component and EAOC. As malignant tissue was
identified in a location different from the solid component found
by MRI, diagnosis with MR relaxometry may present advantages
compared with MRI. Therefore, MR relaxometry can facilitate the
selection of patients who desire fertility-sparing surgery.
Notably, in case of ovarian hemorrhage, an R2 value <12.1
s−1 can be insufficient to diagnose ovarian cancer (data
not shown). In addition, limitations may be present in case of
multicenter collaborations.
In conclusion, conventional MRI and MR relaxometry
were used to examine a case of clear cell carcinoma arising from OE
where the patient desired fertility-preserving treatments. MR
relaxometry may improve the accuracy and reduce the overdiagnosis
of malignant transformations identified by MRI.
Acknowledgements
The authors would like to thank Dr Yuki Yamada
(Department of Obstetrics and Gynecology, Nara Medical University)
for technical assistance.
Funding
No funding was received.
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SM, DS, TW, AY, TM and MI collected, analyzed and
interpreted the clinical data. AH, RM, NH and MM interpreted the
pathological data. NK, CY and HK conceived the study. HK designed
the study and interpreted clinical and pathological data. All
authors read and approved the final version of the manuscript.
Ethical approval and consent to
participate
The present study was approved by The Ethics
Committee of the Nara Medical University.
Patient consent for publication
The patient signed a written informed consent.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
EAOC
|
endometriosis-associated ovarian
cancer
|
|
OE
|
ovarian endometrioma
|
|
MR
|
magnetic resonance
|
|
MRI
|
MR imaging
|
|
T1WI
|
T1-weighted image
|
|
T2WI
|
T2-weighted image
|
|
CA
|
carbohydrate antigen
|
References
|
1
|
Kobayashi H, Sumimoto K, Kitanaka T,
Yamada Y, Sado T, Sakata M, Yoshida S, Kawaguchi R, Kanayama S,
Shigetomi H, et al: Ovarian endometrioma-risks factors of ovarian
cancer development. Eur J Obstet Gynecol Reprod Biol. 138:187–193.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ogawa S, Kaku T, Amada S, Kobayashi H,
Hirakawa T, Ariyoshi K, Kamura T and Nakano H: Ovarian
endometriosis associated with ovarian carcinoma: A
clinicopathological and immunohistochemical study. Gynecol Oncol.
77:298–304. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Park SB and Lee JB: MRI features of
ovarian cystic lesions. J Magn Reson Imaging. 40:503–515. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tanase Y, Kawaguchi R, Takahama J and
Kobayashi H: Factors that differentiate between
endometriosis-associated ovarian cancer and benign ovarian
endometriosis with mural nodules. Magn Reson Med Sci. 17:231–237.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee S, Kim SK, Hwang KJ, Kim T and Kim SH:
Fertility preservation for patients with gynecologic malignancies:
The Korean Society for Fertility Preservation clinical guidelines.
Clin Exp Reprod Med. 44:175–180. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yoshimoto C, Takahama J, Iwabuchi T,
Uchikoshi M, Shigetomi H and Kobayashi H: Transverse relaxation
rate of cyst fluid can predict malignant transformation of ovarian
endometriosis. Magn Reson Med Sci. 16:137–145. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Prat J; FIGO Committee on Gynecologic
Oncology, : FIGO's staging classification for cancer of the ovary,
fallopian tube, and peritoneum: Abridged republication. J Gynecol
Oncol. 26:87–89. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kobayashi H: Screening, epidemiology,
molecular biology, and treatment strategies for
endometriosis-associated ovarian cancer. Reprod Med Biol. 9:17–22.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Takeuchi M, Matsuzaki K, Uehara H and
Nishitani H: Malignant transformation of pelvic endometriosis: MR
imaging findings and pathologic correlation. Radiographics.
26:407–417. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li HM, Feng F, Qiang JW, Zhang GF, Zhao
SH, Ma FH, Li YA and Gu WY: Quantitative dynamic contrast-enhanced
MR imaging for differentiating benign, borderline, and malignant
ovarian tumors. Abdom Radiol (NY). 43:3132–3141. 2018. View Article : Google Scholar : PubMed/NCBI
|