Introduction
Intracholecystic papillary neoplasm (ICPN) of the
gallbladder is a relatively new concept and suspected to share
clinicopathologic features with intraductal papillary mucinous
neoplasm (IPMN) of the pancreas and intraductal papillary neoplasm
of the bile duct (IPNB) (1,2). Because of its rarity, the imaging
characteristics of ICPN have not yet been definitively
standardized. Herein, we report a unique case of ICPN of the
gallbladder extending to the common bile duct (CBD) without
superficial spread.
Case report
A 58-year-old woman with no significant medical
history presented with fever lasting for three days. Her physical
examination was unremarkable. Laboratory analysis showed elevations
in C-reactive protein (2.1 mg/dl; normal range: <0.2 mg/dl),
aspartate aminotransferase (44 IU/l; 13–33 IU/l), alanine
aminotransferase (169 IU/l; 8–42 IU/l), alkaline phosphatase (1675
IU/l; 115–359 IU/l), and gamma-glutamyl transpeptidase (757 IU/l;
8–42 IU/l). Her leukocyte count and serum levels of total
bilirubin, carcinoembryonic antigen, and carbohydrate antigen 19-9
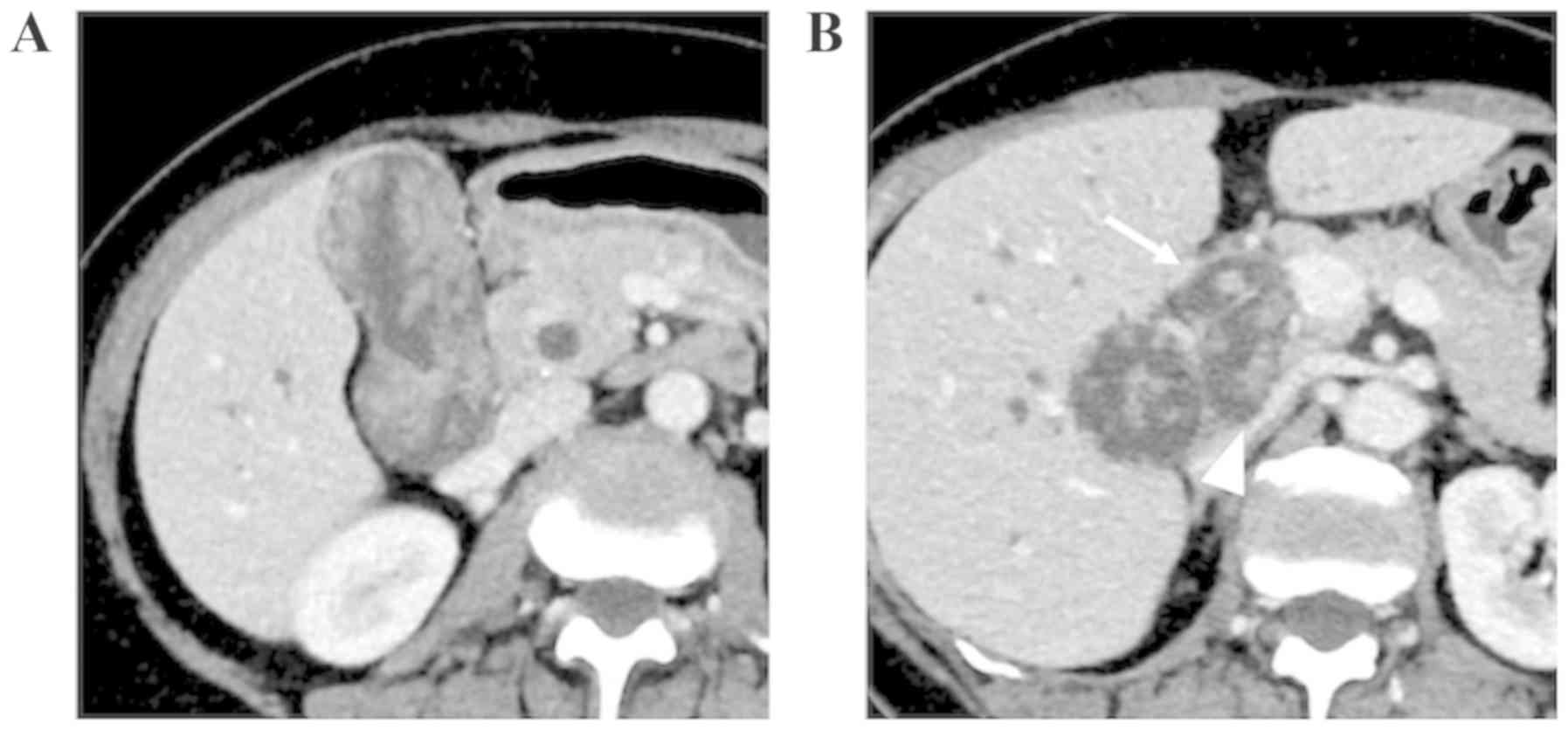
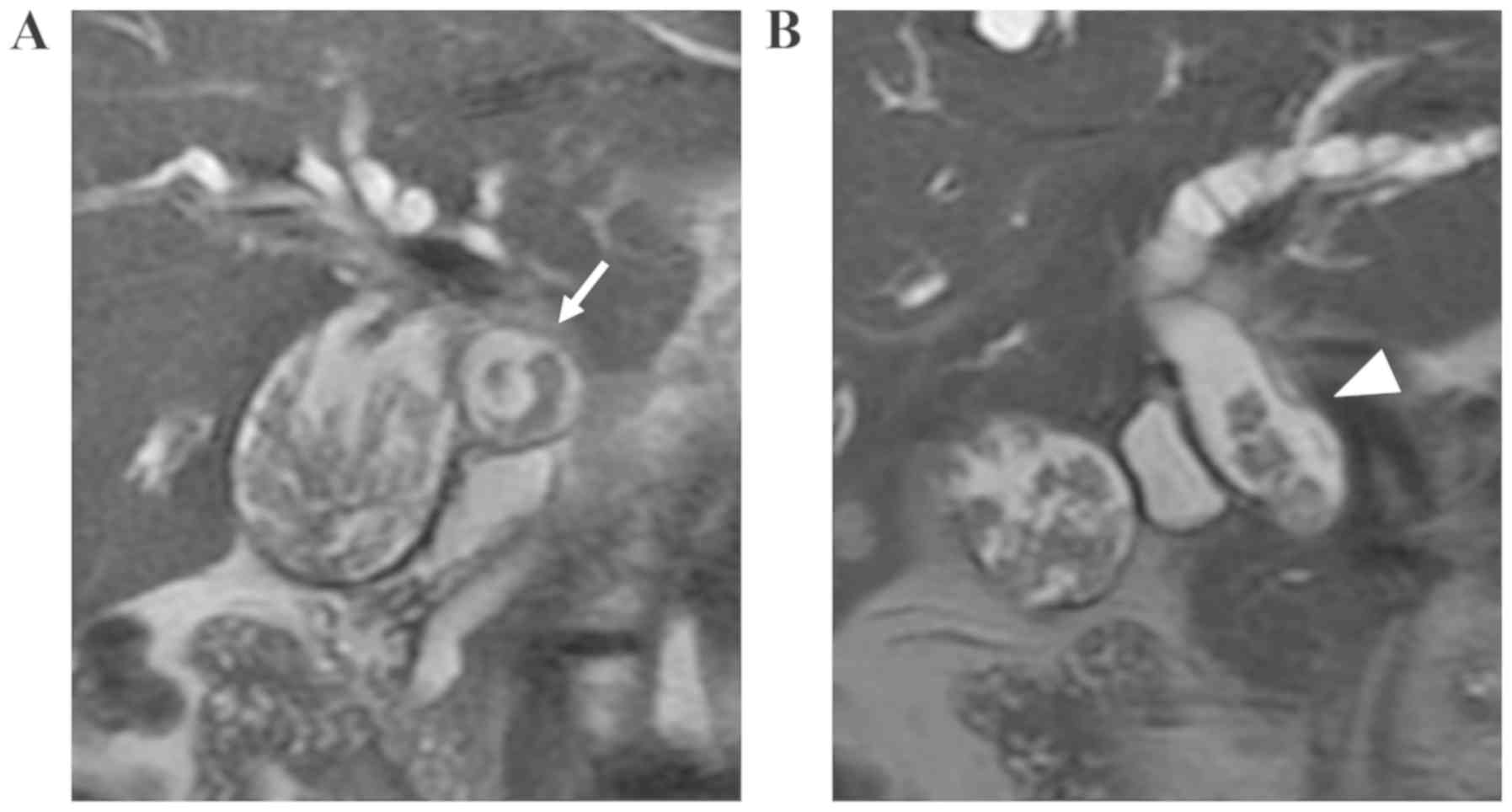
were within normal ranges. Contrast-enhanced computed tomography
(CT) and T2-weighted magnetic resonance imaging (MRI) showed an
enlarged gallbladder filled with a polypoid, papillary lesion. The
CBD was also dilated with a similar intraluminal papillary tumor,
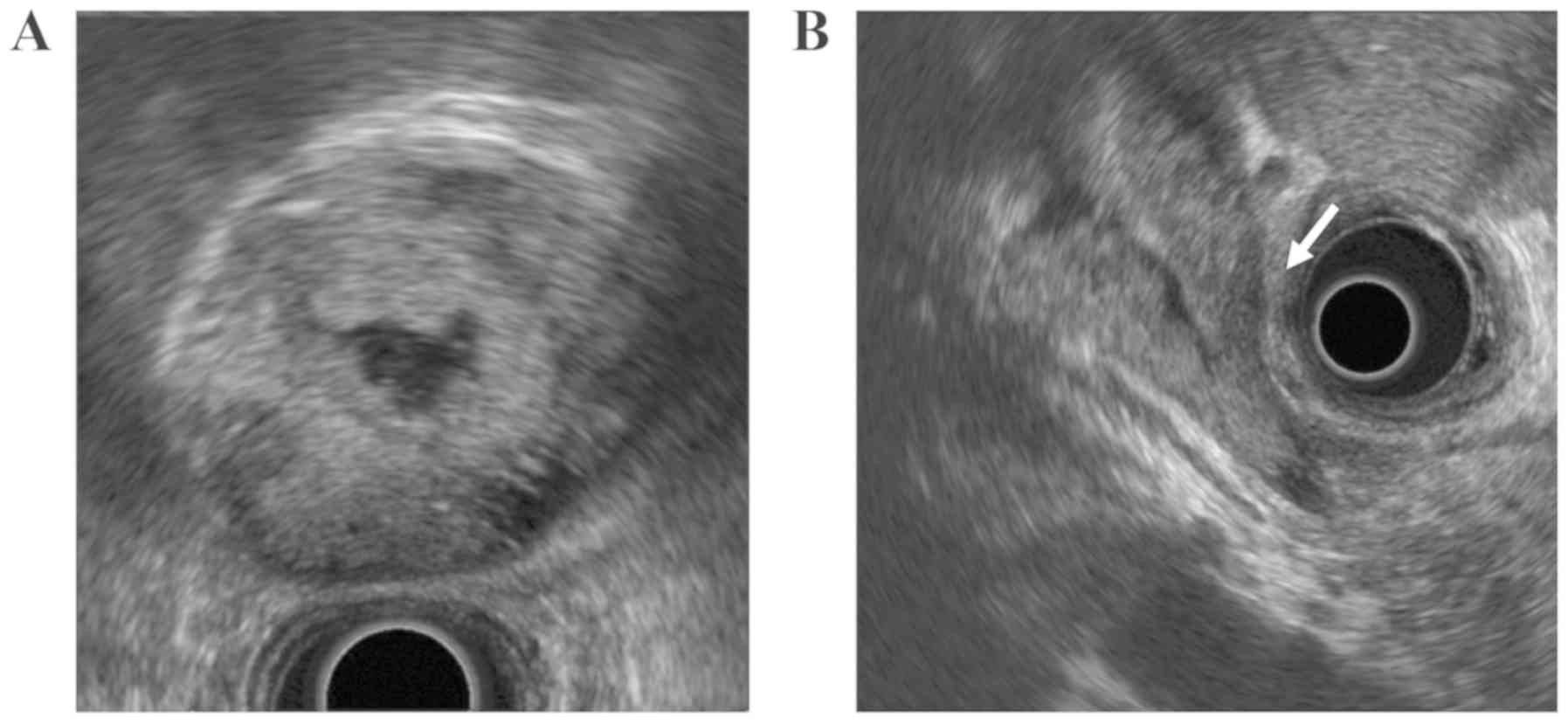
suggesting superficial spread of the gallbladder neoplasm (Figs. 1 and 2). Endoscopic ultrasonography showed the
polypoid lesion spreading from the gallbladder into the CBD without
signs of stromal invasion (Fig. 3).
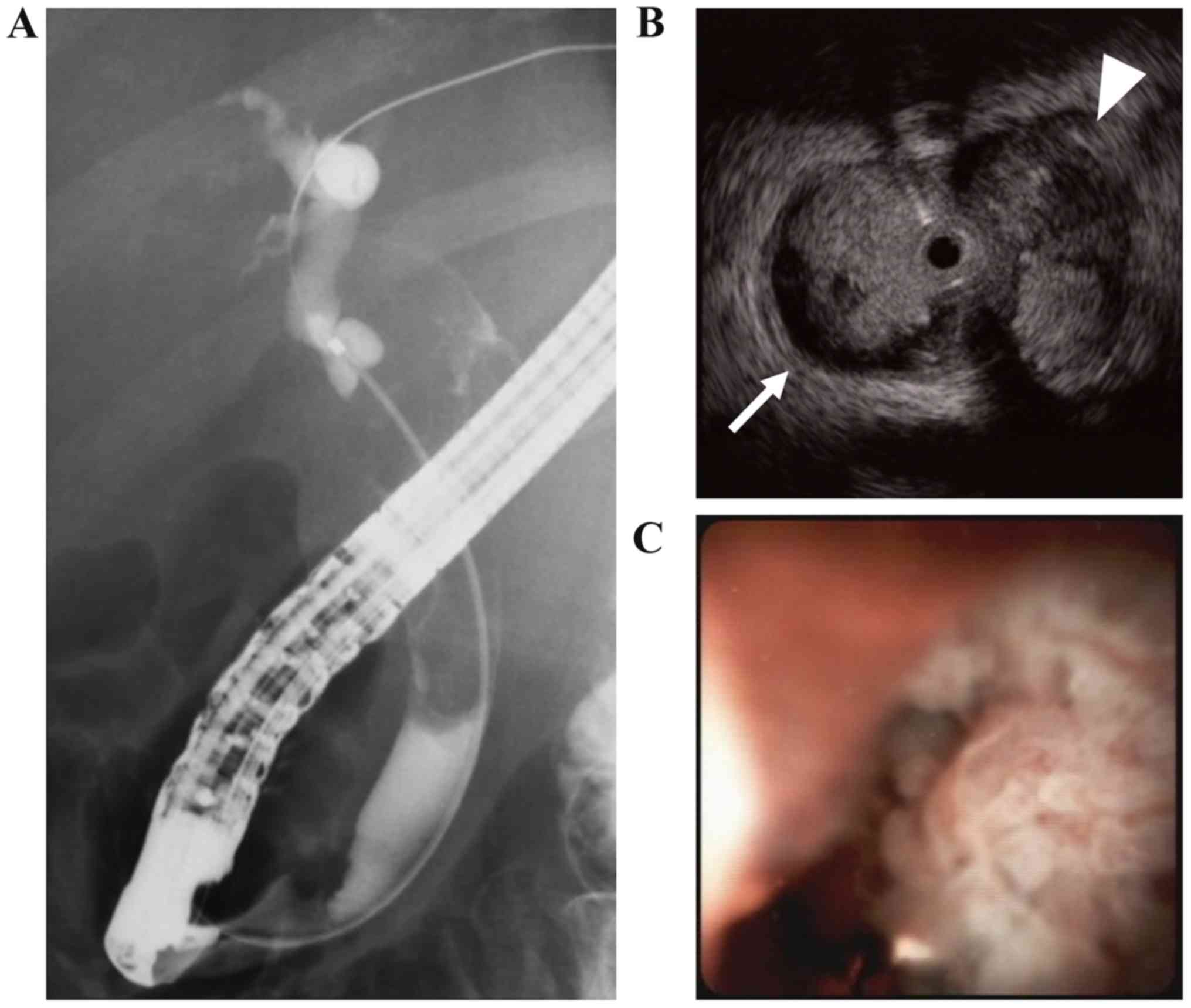
She also underwent endoscopic retrograde cholangiography, which
showed filling defects within the CBD, but the gallbladder and
cystic duct could not be visualized (Fig. 4A). Endoscopic examination with
intraductal ultrasound revealed a papillary lesion extending from
the cystic duct orifice to the lower CBD (Fig. 4B). Furthermore, peroral
cholangioscopy demonstrated a mucin-producing papillary tumor at
the same site, while the confluence of hepatic ducts was tumor-free
(Fig. 4C). The biopsy specimen taken
from the papillary tumor and bile cytology showed atypical
glandular cells consistent with adenocarcinoma. Based on the
diagnosis of ICPN with spread into the CBD, she underwent subtotal
stomach-preserving pancreaticoduodenectomy (SSPPD) and gallbladder
bed resection.
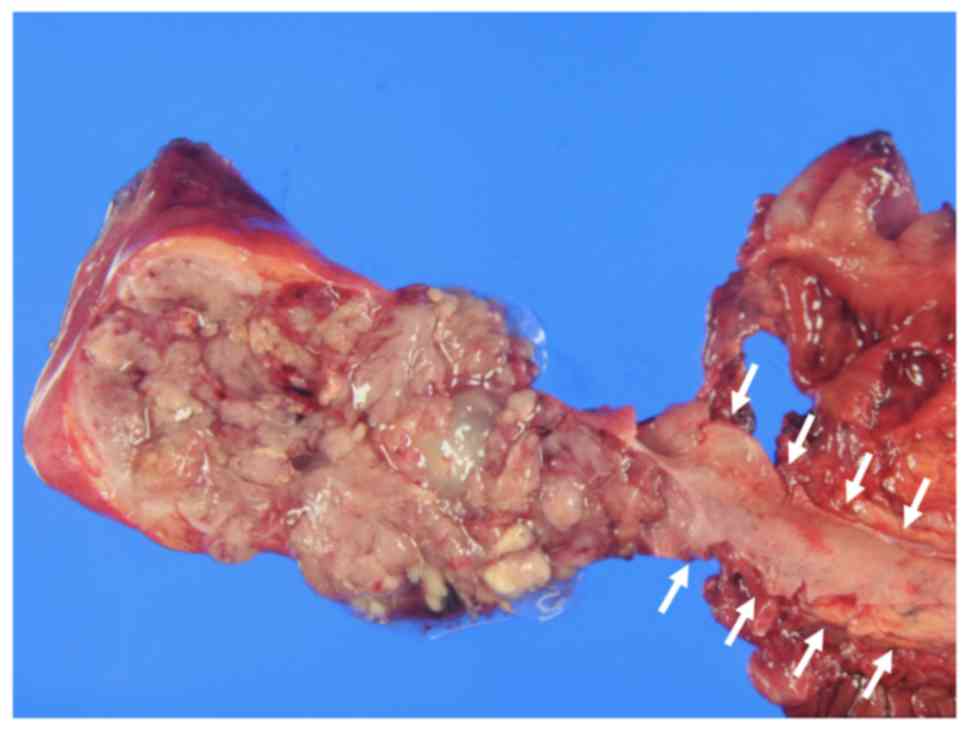
Gross examination showed an enlarged gallbladder and
dilated cystic duct, which were filled with significant amounts of
mucus as well as the papillary neoplasm. However, the mucosa of the
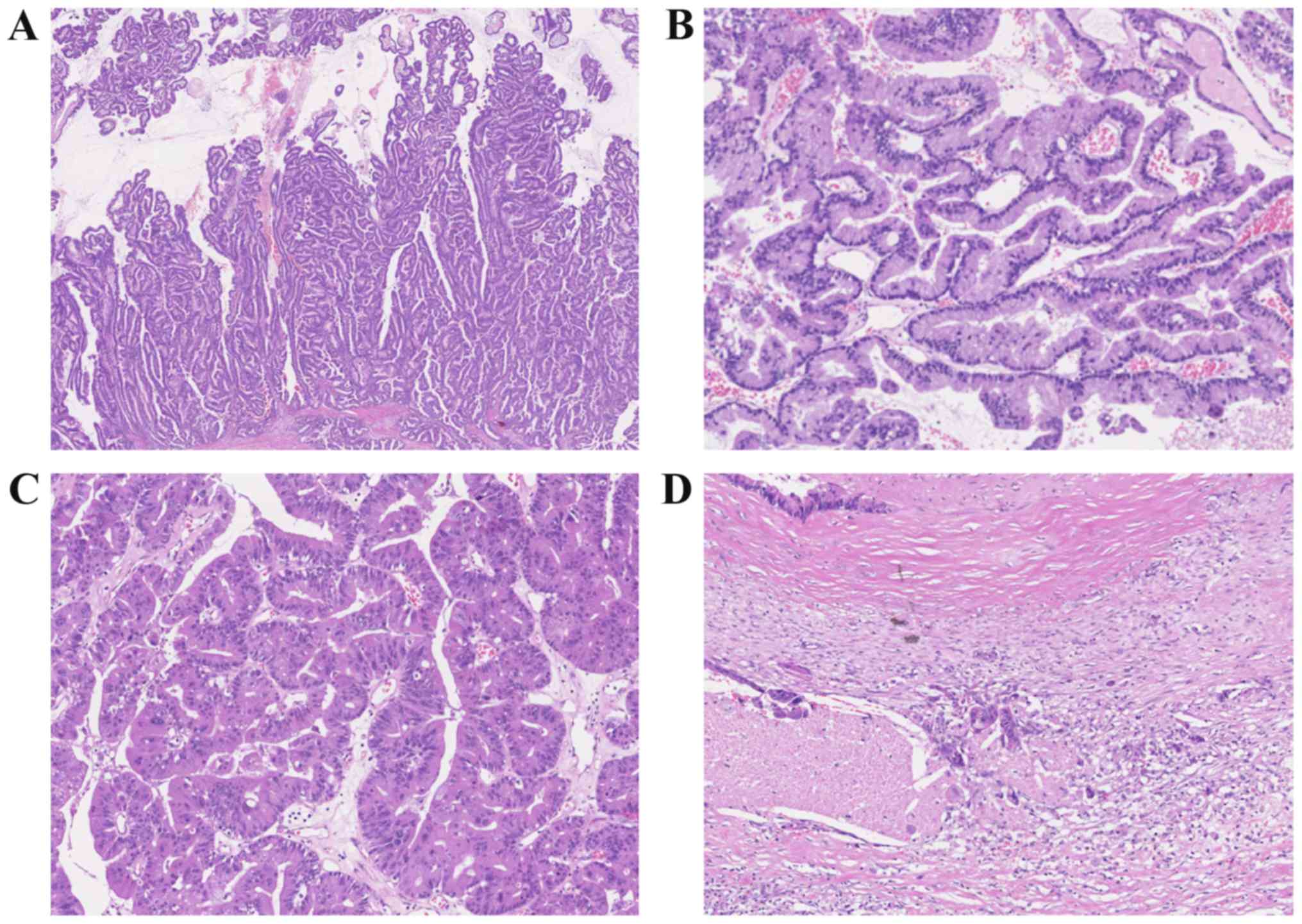
CBD was unremarkable with no tumor identified (Fig. 5). Microscopically, the gallbladder
neoplasm consisted of atypical glandular epithelium arranged in a
highly papillary architecture along fibrovascular stalks. The tumor
showed extensive superficial spread along the gallbladder mucosa,
and also into the Rokitansky-Aschoff sinus. Most tumor cells had
gastric-type features such as intracytoplasmic mucus, round nuclei,
and clear cytoplasms. Small foci consisting of highly eosinophilic
cells with centrally located round nuclei, consistent with the
oncocytic-type, were also present. The tumor was mostly
non-invasive, but there was a small focus (<1 cm) of stromal
invasion in the subserosal layer (Fig.
6).
On immunostaining, the cells were diffusely positive
for MUC1, MUC5AC, and MUC6, and negative for MUC2. On the basis of
the histologic findings, the tumor was diagnosed as a gastric-type
ICPN with an associated adenocarcinoma. Although the patient
refused adjuvant chemotherapy, the post-operative course was
uneventful with no recurrence observed at 6 months of
follow-up.
Discussion
ICPN is a comparatively new entity, first described
in the 2010 World Health Organization classification (1). Adsay et al (2) defined ICPN as an exophytic intramucosal
gallbladder mass (>1.0 cm) composed of dysplastic cells forming
a lesion distinct from the adjacent mucosa. However, this
definition is suspected of being excessively lax, and papillary
invasive carcinomas or intraductal tubular neoplasms (e.g., pyloric
gland adenoma) may also meet the criteria.
It has been reported that ICPNs are more common in
women older than 60 years and that they are present in <0.5% of
gallbladders removed for cholelithiasis or chronic cholecystitis
(2,3). These rare tumors present with an
intramucosal papillary or polypoid mass, often associated with
overproduction of mucin. ICPN is suspected to share characteristics
with IPMN and IPNB; however, they differ in some aspects. Low-grade
lesions and GNAS mutations were markedly less common in
IPNBs and ICPNs than in IPMNs of the pancreas (4–6).
Although 50% of patients with ICPN have invasive
malignant components, the prognosis of ICPN is reportedly
favorable. The 1-, 3- and 5-year survival rates of patients with
noninvasive ICPN were 90, 90 and 78%, respectively. Even patients
with associated invasive carcinoma have a significantly better
clinical outcome than those with ordinary invasive gallbladder
cancer (2). The difference in
prognosis can be at least partly explained by the exophytic growth
of ICPN, which increases the chances of diagnosis at an early stage
and curative resection.
In the present case, multimodality imaging studies
suggested superficial spread to the CBD, requiring SSPPD. However,
no tumor was found in the CBD, suggesting that the papillary mass
observed inside the bile duct was a prolapsed gallbladder neoplasm.
This discrepancy highlights the challenge in determining the degree
of lateral extension of ICPNs. Distinguishing tumor protrusion
without surface invasion from ordinary tumor extension is
difficult. Repeated CT and/or MRI may play an important role in
telling them apart in the case of a tumor moving easily between the
gallbladder and the CBD. Intraoperative ultrasonography may also be
useful for determining the degree of lateral tumor extension.
Another discrepancy between the imaging interpretations and
pathological diagnosis was the presence of stromal invasion. Small
foci of stromal invasion are difficult to identify on imaging, as
in the case of IPNB and IPMN of the pancreas. Considering this
limitation of the imaging studies, gallbladder bed resection was
performed.
Almost 50% of patients with ICPN present with right
upper outer quadrant pain, whereas the remaining 50% are found to
have a tumor incidentally without any associated symptoms (2). The fever in our patient was likely due
to cholangitis, suggesting that prolapsed ICPN can cause
cholangitis even without true bile duct involvement. In addition to
the tumor, the large amount of thick mucus might have also caused
the cholangitis. In contrast, obstructive jaundice is unusual in
the context of ICPN with only 2 reported cases presenting with
biliary obstruction to our knowledge (7,8). In both
cases, the tumors were present in the CBD mucosa as well. To the
best of our knowledge, this is the first study to suggest that ICPN
may protrude into the CBD without superficial spread.
In conclusion, when ICPNs increase in size, they may
protrude into the CBD due to the increased intracholecystic
pressure, which increases the risk of overestimation of tumor
extension and may result in unnecessary additional bile duct
resection.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MY acquired the data and wrote the manuscript. KH,
AS, TM, RH, TA and HA acquired the data and contributed clinical
advice. SY and YZ interpreted the pathological data. YZ revised the
manuscript. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
A written consent for publication was obtained from
the patient.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ICPN
|
intracholecystic papillary
neoplasm
|
|
CBD
|
common bile duct
|
|
IPMN
|
intraductal papillary mucinous
neoplasm
|
|
IPNB
|
intraductal papillary neoplasm of the
bile duct
|
|
CT
|
computed tomography
|
|
MRI
|
magnetic resonance imaging
|
|
SSPPD
|
subtotal stomach-preserving
pancreaticoduodenectomy
|
|
EUS
|
endoscopic ultrasonography
|
|
ERC
|
endoscopic retrograde
cholangiography
|
|
IDUS
|
intraductal ultrasound
|
|
POCS
|
peroral cholangioscopy
|
References
|
1
|
Albores-Saavedra J, Adsay NV, Crawford JM,
Klimstra DS, Klöppel G, Sripa B, Tsui WMS, Paradis V; Carcinoma of
the gallbladder and extrahepatic ducts, ; Bosman FT, Carneiro F,
Hruban RH and Theise ND: WHO classification of tumors of the
digestive system4th. Lyon: Int Agency Res Cancer. pp. 266–273.
2010
|
|
2
|
Adsay V, Jang KT, Roa JC, Dursun N, Ohike
N, Bagci P, Basturk O, Bandyopadhyay S, Cheng JD, Sarmiento JM, et
al: Intracholecystic papillary-tubular neoplasms (ICPN) of the
gallbladder (neoplastic polyps, adenomas, and papillary neoplasms
that are ≥1.0 cm): Clinicopathologic and immunohistochemical
analysis of 123 cases. Am J Surg Pathol. 36:1279–1301. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Klöppel G, Adsay V, Konukiewitz B, Kleeff
J, Schlitter AM and Esposito I: Precancerous lesions of the biliary
tree. Best Pract Res Clin Gastroenterol. 27:285–297. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zen Y, Fujii T, Itatsu K, Nakamura K,
Minato H, Kasashima S, Kurumaya H, Katayanagi K, Kawashima A,
Masuda S, et al: Biliary papillary tumors share pathological
features with intraductal papillary mucinous neoplasm of the
pancreas. Hepatology. 44:1333–1343. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Furukawa T, Kuboki Y, Tanji E, Yoshida S,
Hatori T, Yamamoto M, Shibata N, Shimizu K, Kamatani N and
Shiratori K: Whole-exome sequencing uncovers frequent GNAS
mutations in intraductal papillary mucinous neoplasms of the
pancreas. Sci Rep. 1:1612011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Matthaei H, Wu J, Dal Molin M, Debeljak M,
Lingohr P, Katabi N, Klimstra DS, Adsay NV, Eshleman JR, Schulick
RD, et al: GNAS codon 201 mutations are uncommon in intraductal
papillary neoplasms of the bile duct. HPB (Oxford). 14:677–683.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hashimoto S, Horaguchi J, Fujita N, Noda
Y, Kobayashi G, Ito K, Koshida S, Kanno Y, Ogawa T and Masu K:
Intracholecystic papillary-tubular neoplasm of the gallbladder
presenting with jaundice. Intern Med. 53:2313–2317. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sakai A, Masuda A, Shiomi H, Zen Y and
Ajiki T: Intracholecystic papillary neoplasm of the gallbladder
protruding into the common bile duct. Gastrointest Endosc.
88:405–406. 2018. View Article : Google Scholar : PubMed/NCBI
|