Introduction
Distal pancreatectomy (DP) is the standard procedure
for tumors located in the body or tail of the pancreas, such as
pancreatic carcinoma, intraductal papillary mucinous neoplasm,
neuroendocrine neoplasm, and invasive carcinomas from other organ
carcinomas including stomach and colon (1). A common complication of DP is
postoperative pancreatic fistula (POPF). Despite advances in
surgical techniques and devices, incidence of POPF over the last
few decades have been 24-40% (2,3).
Moreover, perioperative morbidity rates associated with POPF of 30%
have been reported (4). POPF has the
potential to cause lethal intra-abdominal abscess and bleeding
(4). POPF increases medical costs
and prolong hospital stays. Peng et al reported that body
mass index (BMI), blood transfusion, intraoperative blood loss, and
prolonged operative time are clinical predictors of POPF in
patients who undergo DP (5). The
geriatric nutritional risk index (GNRI) is a tool that has been
proposed to evaluate nutrition-related risks in elderly patients
(6) and can be easily calculated
from body weight, height, and serum albumin levels. Due to the
intimate relationship between preoperative body weight and POPF
(5), we examined whether GNRI is a
potential tool to predict POPF in patients who undergo DP.
Patients and methods
Patients
Between January 2007 and June 2018, 37 patients
underwent DP for pancreatic tumors or invasive gastric cancer at
the Kawaguchi Municipal Medical Center (Kawaguchi, China). We
retrospectively analyzed the records of these patients. The
exclusion criteria were as follows: i) invasion to celiac artery;
ii) peritoneal dissemination and iii) difficulty of radical
resection by DP. The present study protocol was reviewed and
approved by the Ethics Committee of the Kawaguchi Municipal Medical
Center in 2016. All patients or their guardians consented to the
use of their medical information for scientific research (ethics
approval no. KMMC2017-27). The requirement for informed consent
from all participants was waived because of the retrospective
nature of the present study. They had all undergone DP with
splenectomy, and the pancreatic remnant had been closed with a
stapler.
Clinicopathological data
Data collected from the medical records included the
occurrence of POPF, demographic variables (sex and age),
anthropometric parameters (height, weight, and BMI), comorbidities,
American Society of Anesthesiologist (ASA)'s physical status
classification, blood transfusions, estimated blood loss, operative
time, and serum albumin levels. POPF was classified according to
the International Study Group of Pancreatic Fistula definition and
grading (A, B, or C) (7). Grade A
indicates asymptomatic POPF, whereas, grades B and C are
symptomatic and require intervention, such as antibiotics therapies
and/or drainage for grade B, and resuscitation and/or exploratory
laparotomy for grade C fistulas. Drain amylase was monitored on
post-operative day 1, 3, 5, and 7.
Nutritional assessment using GNRI
Preoperative nutritional status was assessed with
GNRI, which was calculated as GNRI=[14.89 x serum albumin (g/l)]
+ [41.7 x actual/ideal body weight (kg)]. Ideal body weight was
calculated as ideal body weight = the patient's height (m) x
height (m) x 22 (BMI). When the actual body weight was higher
than the ideal weight, the ratio was set to 1.
These heights are all actual height. This formula
was used for male and female in the same way.
Statistical analysis
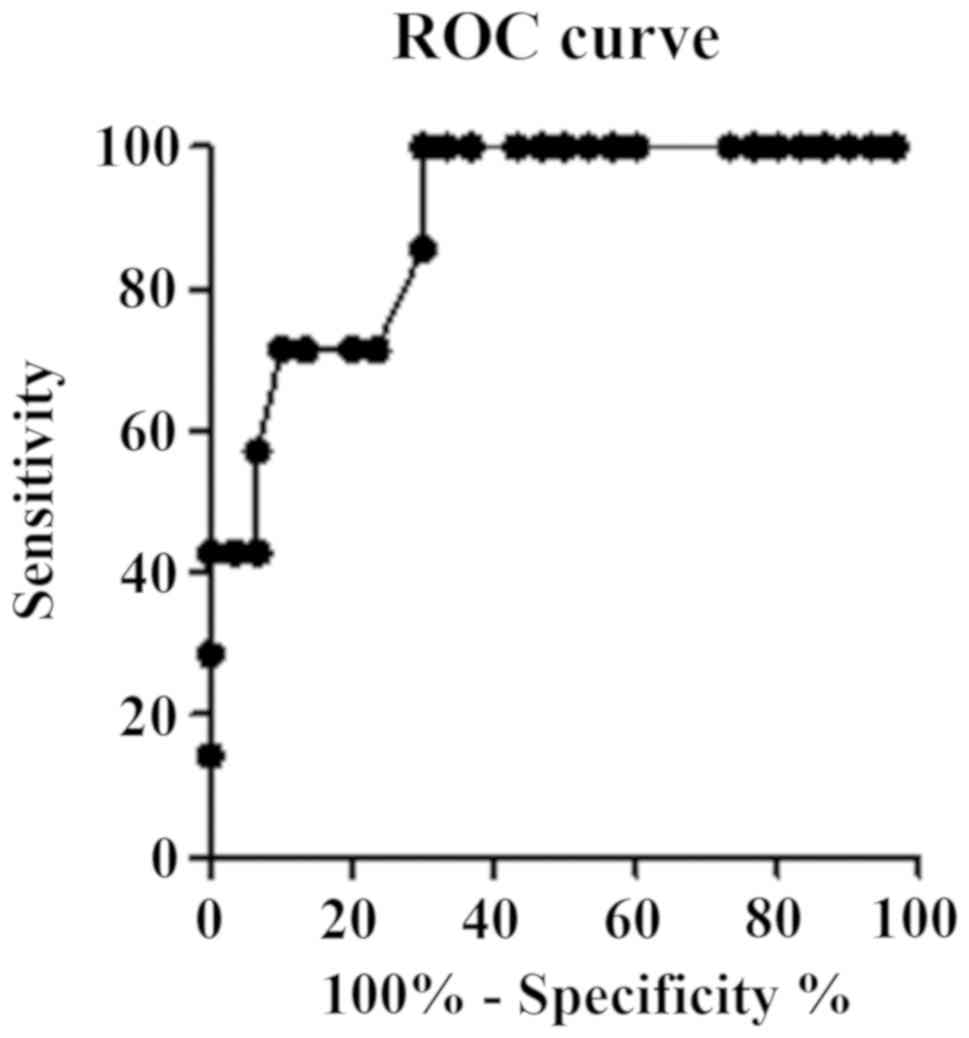
All statistical analyses were performed using
Graphpad Prism v5.0 (Graphpad Software Inc.) and StatView (Abacus
Concepts, Inc.). Differences between the patients with and without
POPF were compared using the Fisher's exact test or Chi-square
test. The optimal cut-off value of GNRI was determined using a
receiver operating characteristic (ROC) curve. The potential risk
factors of POPF were evaluated using univariate and multivariate
analyses. Univariate analysis was conducted using the Chi-square or
Fisher's exact test, followed by multivariate analysis using a
logistic regression to identify the risk factors of POPF. Results
are shown as odds ratios and 95% confidence intervals. P<0.05
was considered to indicate a statistically significant
difference.
Results
Patient characteristics
Of the 37 patients that were reviewed, 22 were men
and 15 were women. The median age was 73 (range 35-82) years. POPF
occurred in seven (19%) patients (grade B in all). There were no
statistically significant differences between patients with POPF
and those without POPF with respect to sex, age, BMI, diabetes
mellitus history, operative time, estimated blood loss, blood
transfusions, or the presence of soft pancreas. In addition,
malignant tumor did not affect risk of POPF (Table I). However, preoperative serum
albumin levels and GNRI were significantly lower in patients with
POPF than those without POPF (P<0.001, for both variables).
 | Table IPatients were divided by presence of
absence of POPF. The data exhibited a higher incidence of POPF in
GNRI <96 compared with GNRI ≥96 patients. |
Table I
Patients were divided by presence of
absence of POPF. The data exhibited a higher incidence of POPF in
GNRI <96 compared with GNRI ≥96 patients.
| Characteristics | POPF group, n=7 | Non-POPF group,
n=30 | P-value |
|---|
| Male/female | 3/4 | 17/13 | 0.68 |
| Age, years | 72.0±1.8 | 70.3±1.9 | 0.67 |
| BMI | 22.7±1.8 | 22.4±1.9 | 0.88 |
| Diabetes mellitus:
Yes (%) | 4 (57.1) | 13 (43.3) | 0.68 |
| Preoperative albumin,
g/l | 3.2±0.3 | 4.2±0.1 | <0.001 |
| GNRI | 85.8±6.8 | 103.5±1.2 | <0.001 |
|
<96 | 5 | 4 | 0.005 |
|
≥96 | 2 | 26 | |
| Malignant/benign
tumor | 6/1 | 31/8 | 0.15 |
| Time of operation,
min | 342.4±17.7 | 318.8±12.7 | 0.40 |
| Estimated blood loss,
ml | 814.3±216.6 | 1414.0±282.1 | 0.32 |
| Blood transfusion:
Yes (%) | 1 (14.3) | 12 (40.0) | 0.22 |
| Soft pancreas: Yes
(%) | 5 (71.4) | 27 (90.0) | 0.23 |
| SSIs: Yes (%) | 7 (100.0) | 2 (6.7) | <0.001 |
Calculation of optimal GNRI cut-off
value
The area under the curve (ROC) was 0.90 (Fig. 1). A GNRI of 96 was determined using
Youden index as the appropriate cut-off value that had a
sensitivity of 71.4%, a specificity of 86.7% and a likelihood ratio
of 5.36. Patients were categorized into two groups: Group A (GNRI
≥96, n=28) and group B (GNRI <96, n=9). POPF was observed in
7.1% of patients in group A and 55.6% of patients in group B.
Univariate and multivariable
analyses
Univariate analysis was performed to evaluate
factors predicting the risk of POPF after DP. Compared with
patients with GNRI ≥96, the incidence of POPF was significantly
higher in patients with GNRI <96 (P=0.005). Similarly, logistic
regression analysis revealed that a GNRI <96 was an independent
predictor of POPF (P=0.005; Table
II).
 | Table IIMultivariate analysis by logistical
regression demonstrated that GNRI <96 was an independent risk
factor to predict POPF following DP. |
Table II
Multivariate analysis by logistical
regression demonstrated that GNRI <96 was an independent risk
factor to predict POPF following DP.
| Characteristics | Odds ratio | 95% CI | P-value |
|---|
| BMI | 0.99 | 0.83-1.18 | 0.87 |
| Preoperative albumin,
g/l | 19.9 | 2.41-165.25 | 0.006 |
| GNRI <96 | 0.062 | 0.009-0.43 | 0.005 |
Discussion
POPFs remain a major pancreas-specific postoperative
complication after pancreatic resection, occurring in approximately
30-40% of patients after DP (3). A
number of risk factors of POPF following pancreatic resection have
been recognized, including a soft pancreas, obesity, blood
transfusion, age, sex, diabetes mellitus history, preoperative
serum albumin levels, extended lymphadenectomy, substantial
intraoperative blood loss, and longer operative time (8). At the tissue level, substantial
inflammatory activity, indicated by high levels of proinflammatory
cytokines and matrix metalloproteinases, and marked chronic
inflammatory infiltrates are reportedly associated with a lower
incidence of fistula (9). A
meta-analysis indicated that a soft pancreas, high BMI, blood
transfusion, intraoperative blood loss, and operative time were
clinical predictors of POPF (5). Of
these variables, a higher than normal BMI is the most common risk
factor of POPF after DP and pancreaticoduodenectomy (PD) (5,10,11).
Therefore, preoperative body weight including nutritional status
should be improved to avoid postoperative complications. As POPFs
are associated with a prolonged hospital stay, ultimately leading
to higher medical costs, surgeons should promptly identify at-risk
patients prior to surgery. Considering this, several methods of
nutritional assessment including body weight have been developed
and validated: The malnutrition inflammation score, nutritional
risk index (NRI), prognostic nutritional index (PNI), and GNRI
(6,12-14).
Among them, GNRI was originally developed to evaluate malnutrition
and related morbidity and mortality in elderly patients (6). Our previous study showed that a low
GNRI was associated with wound infections and POPF in patients who
undergo PD (15). Therefore, we
hypothesized that GNRI could be predictive of POPF following DP. In
the present study, 19% of the 37 patients developed POPF following
DP at our hospital. Malignant tumors did not affect the risk of
POPF as with Sierzega et al who reported that malnutirition
was associated with POPF risk (16).
For these patients, GNRI <96 was strongly associated with a
higher risk of POPF, suggesting that correcting nutrition before
the operation might decrease the risk. In addition, POPF is also a
potential predictor of surgical site infection and is intimately
related particularly to organ/space infections. Parikh et al
reported that 55% of POPFs contributed to the occurrence of
intra-abdominal abscess (17). In
our data, all patients with POPF had surgical site infections, with
85.7% having organ/space infections. However, in present study,
blood transfusion was not associated with POPF. We estimated the
reason why were that our sample was small, and criteria of
judgement for transfusion were different according to
anesthesiologists in our hospital.
Our findings are consistent with those of previous
studies, in which NRI was associated with POPF following DP
(16). Moreover, Sato et al
concluded that low PNI was significantly more common in patients
with grade B or C POPF (18). Our
study has several limitations. The results should be regarded with
caution because of the relatively sample size. A further limitation
is the retrospective nature of this study. Therefore, a larger
prospective study should be conducted to validate the present
findings. In conclusions, the present study revealed that a GNRI
score of <96 may be a risk factor of POPF in patients who
undergo DP.
Acknowledgements
The authors would like to thank Dr Noriko Funamizu
(Department of Internal Medicine, Hirose Hospital) for their advice
and discussion.
Funding
No funding was received
Availability of data and materials
The datasets used and analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
NF carried out the experimental studies, and drafted
and completed the manuscript. NF and KK participated in the design
of the study. YN performed the surgical procedure with NF and
revised the manuscript. NF conceived the study and performed the
statistical analysis. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was conducted based on the
Declaration of Helsinki after receiving approval from the review
board of the Kawaguchi Municipal Medical Center (ethics approval
no. KMMC2017-27). The requirement for informed consent from the
participants was waived because of the retrospective nature of the
present study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Parikh PY and Lillemoe KD: Surgical
management of pancreatic cancer-distal pancreatectomy. Semin Oncol.
42:110–122. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
van Hilst J, de Pastena M, de Rooij T,
Alseidi A, Busch OR, van Dieren S, van Eijck CH, Giovinazzo F,
Groot Koerkamp B, Marchegiani G, et al: Clinical impact of the
updated international postoperative pancreatic fistula definition
in distal pancreatectomy. HPB (Oxford). 20:1044–1050.
2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Diener MK, Knaebel HP, Witte ST, Rossion
I, Kieser M, Buchler MW and Seiler CM: DISPACT Trial Group. DISPACT
trial: A randomized controlled trial to compare two different
surgical techniques of DIStal PAnCreaTectomy-study rationale and
design. Clin Trials. 5:534–545. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Diener MK, Seiler CM, Rossion I, Kleeff J,
Glanemann M, Butturini G, Tomazic A, Bruns CJ, Busch OR, Farkas S,
et al: Efficacy of stapler versus hand-sewn closure after distal
pancreatectomy (DISPACT): A randomised, controlled multicentre
trial. Lancet. 377:1514–1522. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Peng YP, Zhu XL, Yin LD, Zhu Y, Wei JS, Wu
JL and Miao Y: Risk factors of postoperative pancreatic fistula in
patients after distal pancreatectomy: A systematic review and
meta-analysis. Sci Rep. 7(185)2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bouillanne O, Morineau G, Dupont C,
Coulombel I, Vincent JP, Nicolis I, Benazeth S, Cynober L and
Aussel C: Geriatric nutritional risk index: A new index for
evaluating at-risk elderly medical patients. Am J Clin Nutr.
82:777–783. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Bassi C, Dervenis C, Butturini G,
Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W
and Buchler M: International Study Group on Pancreatic Fistula
Definition. Postoperative pancreatic fistula: An international
study group (ISGPF) definition. Surgery. 138:8–13. 2005.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Goh BK, Tan YM Chung YF, Cheow PC, Ong HS,
Chan WH, Chow PK, Soo KC, Wong WK and Ooi LL: Critical appraisal of
232 consecutive distal pancreatectomies with emphasis on risk
factors, outcome, and management of the postoperative pancreatic
fistula: A 21-year experience at a single institution. Arch Surg.
143:956–965. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Felix K, Schuck A, Gaida MM, Hinz U,
Dovzhanskiy D and Werner J: Objective parameters aid the prediction
of fistulas in pancreatic surgery. Exp Ther Med. 8:719–726.
2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kimura W, Miyata H, Gotoh M, Hirai I,
Kenjo A, Kitagawa Y, Shimada M, Baba H, Tomita N, Nakagoe T, et al:
A pancreaticoduodenectomy risk model derived from 8575 cases from a
national single-race population (Japanese) using a web-based data
entry system: The 30-day and in-hospital mortality rates for
pancreaticoduodenectomy. Ann Surg. 259:773–780. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sell NM, Pucci MJ, Gabale S, Leiby BE,
Rosato EL, Winter JM, Yeo CJ and Lavu H: The influence of
transection site on the development of pancreatic fistula in
patients undergoing distal pancreatectomy: A review of 294
consecutive cases. Surgery. 157:1080–1087. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kalantar-Zadeh K, Kopple JD, Block G and
Humphreys MH: A malnutrition-inflammation score is correlated with
morbidity and mortality in maintenance hemodialysis patients. Am J
Kidney Dis. 38:1251–1263. 2001.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Adejumo OL, Koelling TM and Hummel SL:
Nutritional risk index predicts mortality in hospitalized advanced
heart failure patients. J Heart Lung Transplant. 34:1385–1389.
2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hu Q, Wang G, Ren J, Ren H, Li G, Wu X, Gu
G, Li R, Guo K, Deng Y, et al: Preoperative prognostic nutritional
index predicts postoperative surgical site infections in
gastrointestinal fistula patients undergoing bowel resections.
Medicine (Baltimore). 95(e4084)2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Funamizu N, Nakabayashi Y, Iida T and
Kurihara K: Geriatric nutritional risk index predicts surgical site
infection after pancreaticoduodenectomy. Mol Clin Oncol. 9:274–278.
2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sierzega M, Niekowal B, Kulig J and
Popiela T: Nutritional status affects the rate of pancreatic
fistula after distal pancreatectomy: A multivariate analysis of 132
patients. J Am Coll Surg. 205:52–59. 2007.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Parikh JA, Beane JD, Kilbane EM, Milgrom
DP and Pitt HA: Is American college of surgeons NSQIP organ space
infection a surrogate for pancreatic fistula? J Am Coll Surg.
219:1111–1116. 2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sato N, Mori Y, Minagawa N, Tamura T,
Shibao K, Higure A and Yamaguchi K: Rapid postoperative reduction
in prognostic nutrition index is associated with the development of
pancreatic fistula following distal pancreatectomy. Pancreatology.
14:216–220. 2014.PubMed/NCBI View Article : Google Scholar
|