Introduction
Leiomyosarcomas (LMS) constitute rare mesenchymal
tumors of smooth muscle origin. LMS of the adrenal gland are
retroperitoneal tumors in the suprarenal region with less than 50
cases described in the English literature. They are thought to
derive from the adrenal vein and/or its branches (1). Adrenal LMS are diagnosed
postoperatively after pathologic examination of the surgical
specimen; they have no specific clinical or imaging characteristics
nor biomarkers and are usually discovered after they have reached a
large size due to compressive phenomena (2). The aim of this report is to describe
the case of an adrenal LMS in a 62-year-old male patient discovered
incidentally.
Case report
An asymptomatic 62-year-old Caucasian male presented
to our unit for the investigation of an incidentally found left
suprarenal mass, discovered during his annual sonographic follow-up
for nephrolithiasis. From his medical history, except for the
nephrolithiasis, the patient had diabetes mellitus type II,
dyslipidaemia and an appendicectomy performed 30 years ago.
Physical examination and laboratory testing revealed no abnormal
findings and we proceeded with a computed tomography (CT) of the
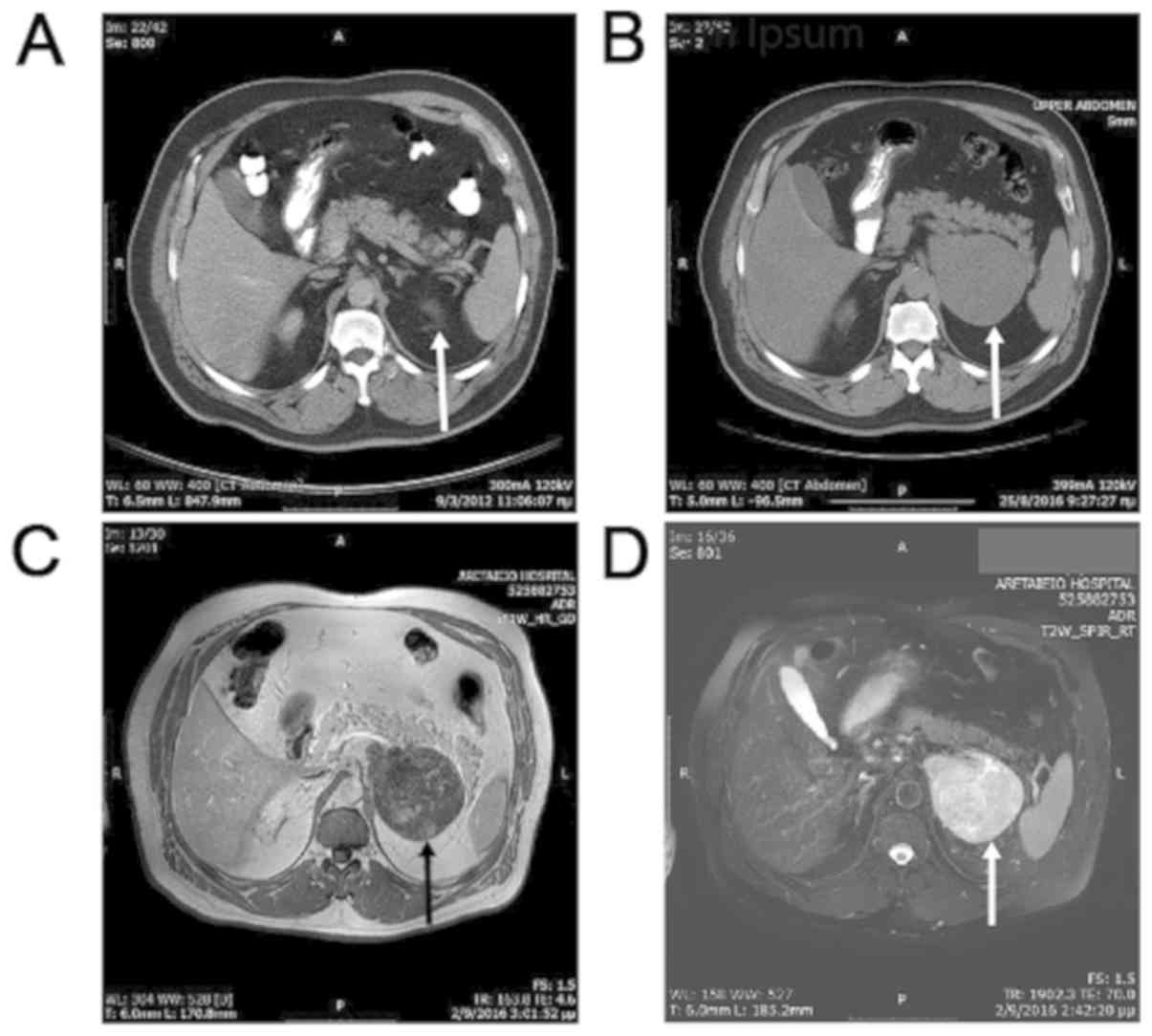
abdomen with intravenous (IV) and oral contrast agent. CT revealed
a low-density mass measuring 10.3x8.5x8.4 cm originating from the
left adrenal gland with minor contrast uptake, suspicious of
malignancy. The subsequent adrenal protocol magnetic resonance
imaging (MRI) revealed a 10x8.2 cm mass with low-signal-intensity
on T1-weighted (T1W) images and intermediately
high-signal-intensity on T2-weighted images (T2W), with
heterogeneous contrast uptake, without loss of signal-intensity in
out-of-phase gradient recalled echo (GRE) T1W sequence (Fig. 1). The medial border of the tumor
appeared to have the morphology of confluent nodules that were
possibly representing infiltrated lymph nodes. The mass was
rendered as highly suspicious of adrenal malignancy, most probably
of adrenocortical carcinoma. We thereafter performed a chest CT
scan to exclude the presence of pulmonary metastases, as well as a
biochemical evaluation of the patient for hormonal hypersecretion
to exclude the possibility of a hormonally active adrenal tumor.
Laboratory results were as follows: 24 h urine collection for
metanephrine: 62 mcg/24 h [reference range (r.r.) 52-341 mcg/24 h],
24 h urine collection for normetanephrine: 367 mcg/24 h (r.r.
88-444 mcg/24 h), dehydroepiandrosterone sulphate (S-DHEA): 186
mcg/dl (r.r. 51.7-295 mcg/dl), plasma renin activity (PRA): 0.21
ng/ml/h (r.r. 0.2-1.4 ng/ml/h), cortisol: 11.9 mcg/dl (r.r.
6.2-19.4 mcg/dl), adrenocorticotropic hormone (ACTH): 39.0 pg/ml
(r.r. 7.0-64 pg/ml), aldosterone: 5.11 ng/dl (r.r. 1.0-16 ng/dl),
dexamethasone suppression test: cortisol: 0.4 mcg/dl. Blood sample
collection was performed on September 27th, 2016.
The patient underwent left open radical
adrenalectomy due to the high possibility of the tumor being a
non-secretory adrenocortical carcinoma on account of imaging
characteristics and its size. The extent of the resection included
the tumor and all peri tumoral fat and para-aortic lymphatic tissue
from the diaphragm to the level of the left renal vein. The
postoperative course was uneventful and the patient was discharged
on day 6 after surgery.
Histopathology
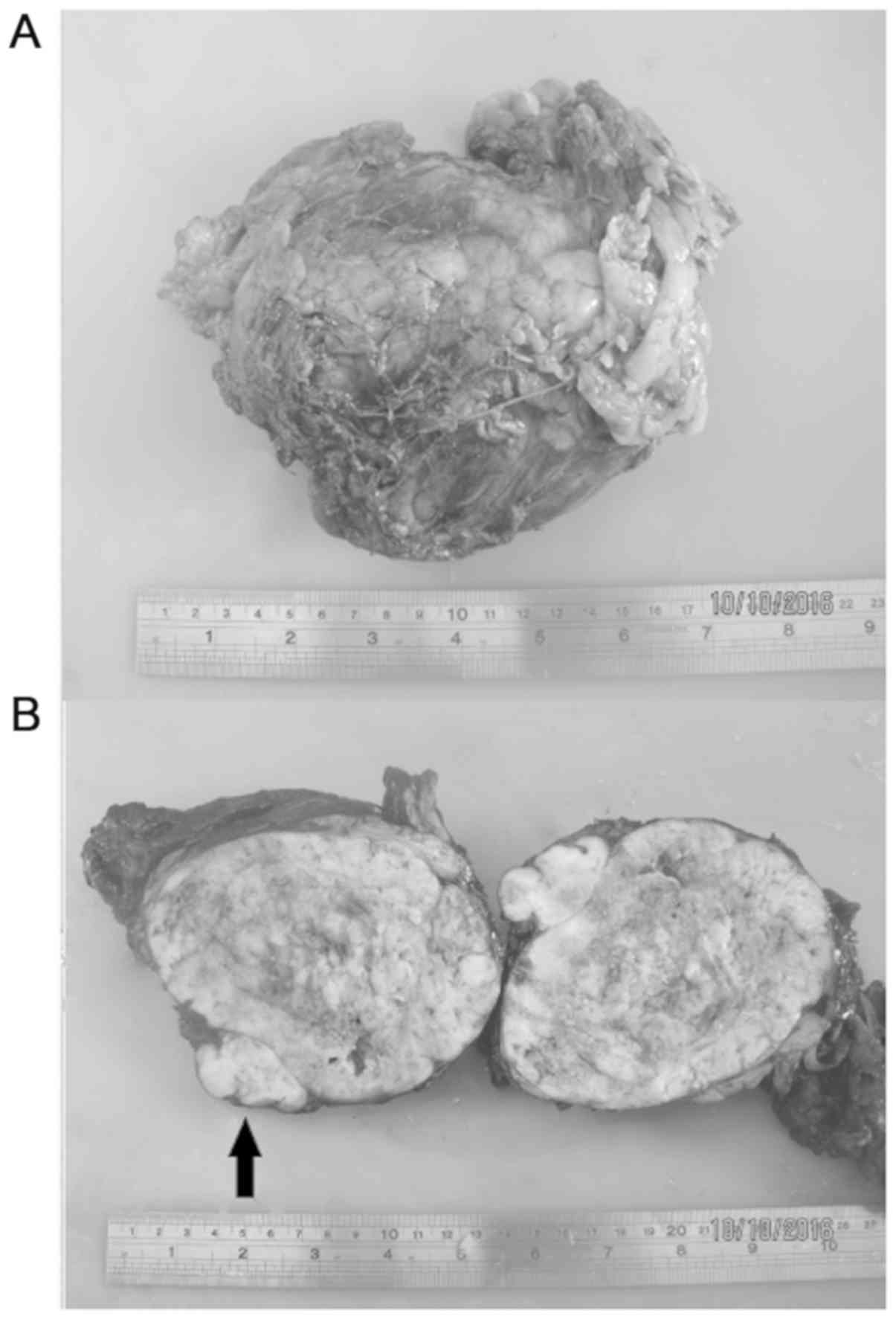
The surgical specimen was collected on October 7th,
2016. On gross pathological examination the specimen measured
13x11x6.5 cm and weighted 594 g (Fig.
2). The mass had lobulated appearance, showed areas of cystic
degeneration and necrosis in cross section and residual adrenal
tissue was identifiable on its outer surface. The tumor was
surrounded by fibroadipose tissue measuring 11x8x2 cm.
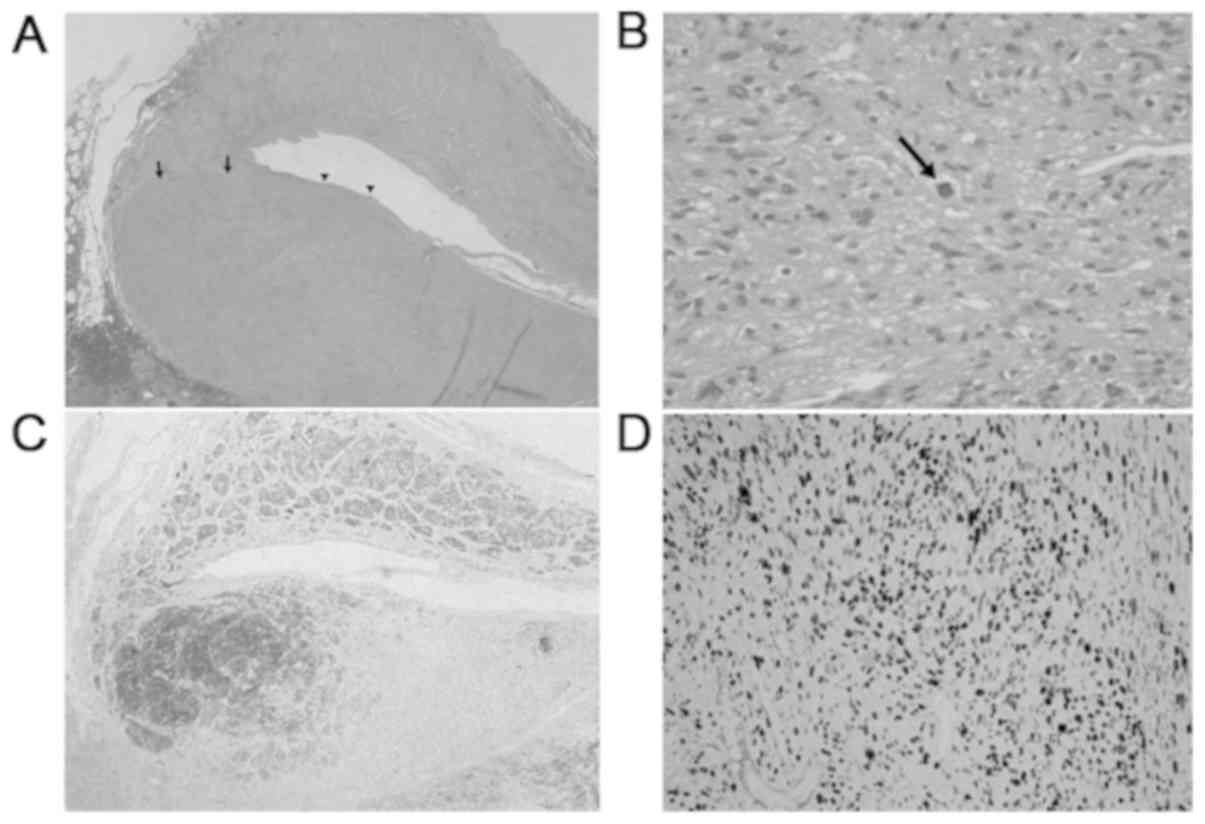
Microscopic examination revealed a spindle cell
tumor with intermediate nuclear atypia, significant mitotic
activity [7 mitoses/10 high power fields (HPF)] and small areas of
ischaemic necrosis. In certain sections the tumor was observed to
have grown in the wall of a large vein, most probably the central
adrenal vein and in the circumference of the mass adrenal tissue
residue was identifiable. Neoplastic cells were also present in the
periadrenal fibroadipose tissue with the form of discrete
circumscribed nodules.
Immunohistochemistry
Tumor cells were found to be positive for desmin,
smooth muscle actin (SMA) and negative for S-100 protein,
synaptophysin, chromogranin, pan-cytokeratin (PAN CK), calretinin.
The proliferating index Ki-67 was found to be approximately 75%
(Fig. 3).
The final diagnosis of the pathological analysis was
well-differentiated leiomyosarcoma of the left adrenal gland with
maximum diameter being 13 cm. There were no infiltrated lymph nodes
found. What were thought to be infiltrated lymph nodes in the
preoperative MRI was neoplastic infiltration of the periadrenal
fibroadipose tissue in the form of satellite nodules.
Following the pathological examination report, the
Multidisciplinary Oncology Council of our hospital decided the
regular follow-up of the patient with image studies, which in 3
months postoperatively showed a metastatic lesion in the 10th
thoracic vertebra (retroperitoneal MRI, thoracic spine MRI). The
patient was then treated with radiation therapy in the region of
the 9th-12th thoracic vertebrae; he received a total dose of 20 Gy,
with the daily dose being 4 Gy. The following chest and abdomen CT
performed at 7 months postoperatively were negative for pulmonary
metastases, but showed metastases in the hepatic parenchyma. The
patient was subsequently integrated in the Oncology Department of
our Hospital for the initiation of IV chemotherapy treatment with
gemcitabine and docetaxel. During this treatment the patient
exhibited progression of the disease, developing pulmonary
metastases 11 months postoperatively and his chemotherapy regimen
was changed to AIM (doxorubicin, ifosfamide, mesna) at 16 months
postoperatively, due to radiological evidence of bone, liver and
pulmonary metastases growing in number and in size (chest and
abdomen CT, skeletal scintigraphy with 99mTc-HDP). The
patient continues to receive IV chemotherapy treatment and is alive
with metastatic disease 31 months after surgery.
Discussion
Adrenal LMS are non-functional mesenchymal tumors of
the adrenal gland, with smooth muscle differentiation, which are
thought to derive from the adrenal vein or its branches. They are
usually found in image studies as large heterogeneous masses with
no specific characteristics, which makes them undistinguishable
from other adrenal tumors (3). The
pathogenesis of adrenal leiomyosarcoma remains unknown, but there
might be a correlation with Epstein-Barr Virus infection in
patients with acquired immunodeficiency syndrome (AIDS) (4). The treatment of choice is surgical
resection with negative margins, after the evaluation of the tumor
secretion to exclude the diagnosis of a functional tumor. Their
diagnosis is rendered after pathological examination of the
specimen, which is observed microscopically as a spindle cell
neoplasia with nuclear atypia or pleomorphism, high mitotic
activity and necrotic foci and immunohistochemically is found
positive for smooth muscle stains, although there have been
described cases with pleomorphic presentation of the tumor
(5).
Chemotherapy and radiation therapy have been
proposed for locally advanced or metastatic disease but these
treatments are yet to be proved beneficial (6). Biopsy of the tumor can provide the
necessary histological diagnosis before chemo/radiation therapy if
the patient is deemed inoperable (7). Adrenal LMS are usually diagnosed after
they have reached a large size due to their lack of specific signs
and symptoms, and in many cases the tumor is found to have extended
to the inferior vena cava (IVC) upon diagnosis, or to have spread
to distant organs (8). In addition,
patterns of recurrent disease and metastatic spread render the
behavior of this tumor rather aggressive, with longest patient
survival being reported as three years after surgery (9).
In conclusion, adrenal LMS are rare tumors found in
the suprarenal region, usually diagnosed having reached a large
size or after having provoked symptoms due to applying pressure to
adjacent structures, or by extending directly to the IVC. Their
usual diagnosis in an advanced stage contributes to the poor
prognosis of these patients. Their radiological characteristics are
similar to those of other adrenal tumors and therefor they should
be considered in the differential diagnosis of a suprarenal
non-secreting mass with malignant characteristics. The gold
standard of treatment is surgical excision, with chemotherapy and
radiation therapy being reserved for advanced disease.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used during the present study are
available from the corresponding author on reasonable request.
Authors' contributions
CN, AD and EG contributed to the conception and
design of the study. MS, DD and MT acquired, analyzed and
interpreted the data. MS, TT and EG drafted the manuscript. CN and
TT revised the manuscript. All authors read and approved the final
version of this manuscript.
Ethics approval and consent to
participate
Oral patient consent was obtained for participation
in this study.
Patient consent for publication
Informed consent was obtained for the publication of
patient data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zetler PJ, Filipenko JD, Bilbey JH and
Schmidt N: Primary adrenal leiomyosarcoma in a man with acquired
immunodeficiency syndrome (AIDS). Further evidence for an increase
in smooth muscle tumors related to Epstein-Barr infection in AIDS.
Arch Pathol Lab Med. 119:1164–1167. 1995.PubMed/NCBI
|
|
2
|
Onishi T, Yanagihara Y, Kikugawa T, Miura
N, Noda T, Kakuda T, Kitazawa R and Tanji N: Primary adrenal
leiomyosarcoma with lymph node metastasis: A case report. World J
Surg Oncol. 14(176)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Karaosmanoglu AD and Gee MS: Sonographic
findings of an adrenal leiomyosarcoma. J Ultrasound Med.
29:1369–1373. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Nagaraj V, Mustafa M, Amin E, Ali W, Naji
Sarsam S and Darwish A: Primary adrenal leiomyosarcoma in an arab
male: A rare case report with immunohistochemistry study. Case Rep
Surg. 2015(702541)2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Deshmukh SD, Babanagare SV, Anand M, Pande
DP and Yavalkar P: Primary adrenal leiomyosarcoma: A case report
with immunohistochemical study and review of literature. J Cancer
Res Ther. 9:114–116. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mohanty SK, Balani JP and Parwani AV:
Pleomorphic leiomyosarcoma of the adrenal gland: Case report and
review of the literature. Urology. 70(591.e57)2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mulani SR, Stoner P, Schlachterman A,
Ghayee HK, Lu L and Gupte A: First reported case of endoscopic
ultrasound-guided core biopsy yielding diagnosis of primary adrenal
leiomyosarcoma. Case Rep Gastrointest Med.
2018(8196051)2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhou Y, Tang Y, Tang J, Deng F, Gong G and
Dai Y: Primary adrenal leiomyosarcoma: A case report and review of
literature. Int J Clin Exp Pathol. 8:4258–4263. 2015.PubMed/NCBI
|
|
9
|
Quildrian S, Califano I, Carrizo F,
Daffinoti A and Calónico N: Primary adrenal leiomyosarcoma treated
by laparoscopic adrenalectomy. Endocrinol Nutr. 62:472–473.
2015.PubMed/NCBI View Article : Google Scholar
|