|
1
|
Ferris RL, Blumenschein G Jr, Fayette J,
Guigay J, Colevas AD, Licitra L, Harrington K, Kasper S, Vokes EE,
Even C, et al: Nivolumab for recurrent squamous-cell carcinoma of
the head and neck. N Engl J Med. 375:1856–1867. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Burtness B, Harrington KJ, Greil R,
Soulières D, Tahara M, de Castro G Jr, Psyrri A, Basté N, Neupane
P, Bratland Å, et al: Pembrolizumab alone or with chemotherapy
versus cetuximab with chemotherapy for recurrent or metastatic
squamous cell carcinoma of the head and neck (KEYNOTE-048): A
randomised, open-label, phase 3 study. Lancet. 394:1915–1928.
2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cohen EEW, Soulieres D, Le Tourneau C,
Dinis J, Licitra L, Ahn MJ, Soria A, Machiels JP, Mach N, Mehra R,
et al: Pembrolizumab versus methotrexate, docetaxel, or cetuximab
for recurrent or metastatic head-and-neck squamous cell carcinoma
(KEYNOTE-040): A randomised, open-label, phase 3 study. Lancet.
393:156–167. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
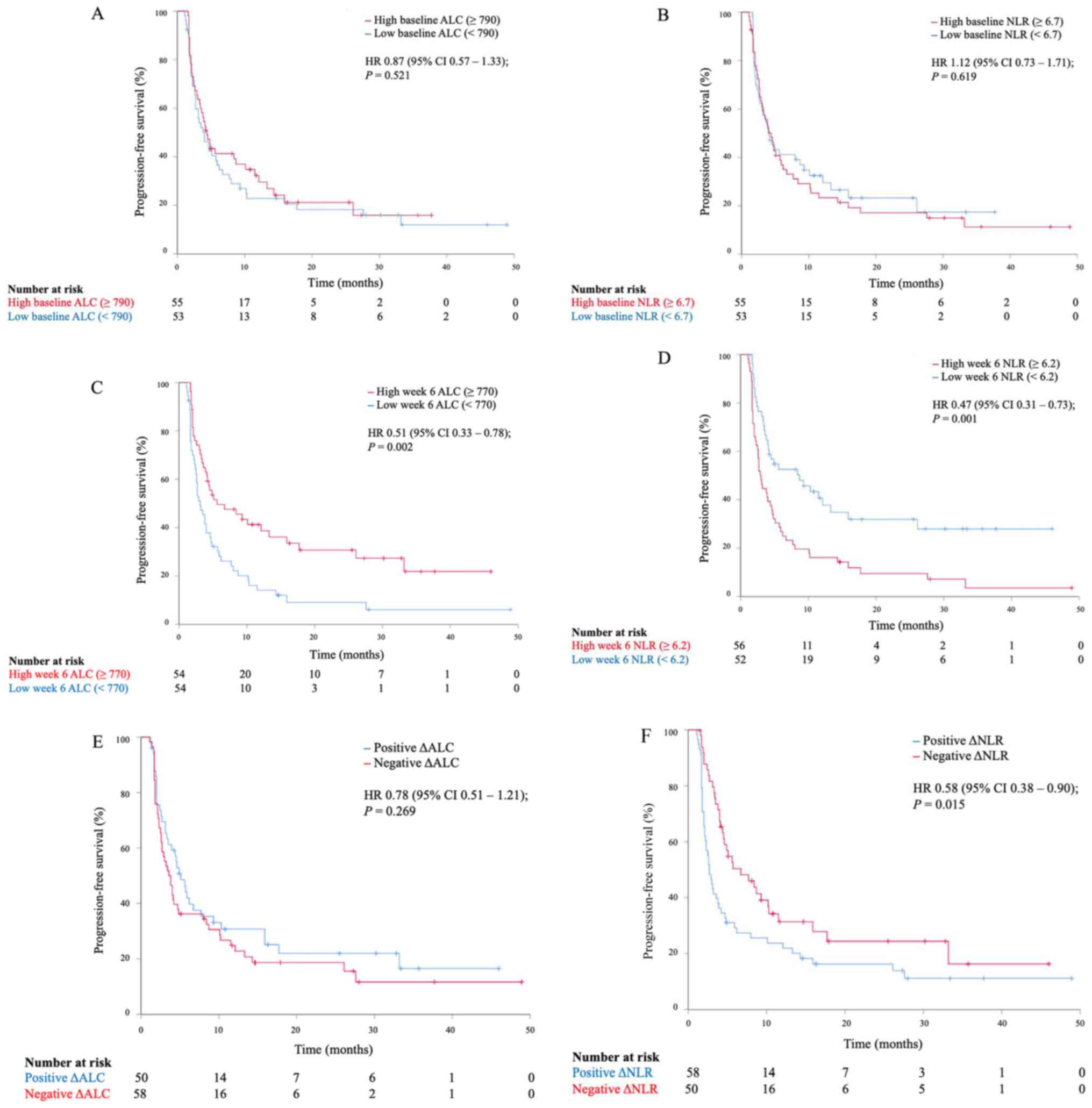
Ho WJ, Yarchoan M, Hopkins A, Mehra R,
Grossman S and Kang H: Association between pretreatment lymphocyte
count and response to PD1 inhibitors in head and neck squamous cell
carcinomas. J Immunother Cancer. 6(84)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ameratunga M, Chénard-Poirier M, Candilejo
IM, Pedregal M, Lui A, Dolling D, Aversa C, Garces AI, Ang EJ,
Banerji U, et al: Neutrophil-lymphocyte ratio kinetics in patients
with advanced solid tumours on phase I trials of PD-1/PD-L1
inhibitors. Eur J Cancer. 89:56–63. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Huemer F, Lang D, Westphal T, Gampenrieder
SP, Hutarew G, Weiss L, Hackl H, Lamprecht B, Rinnerthaler G and
Greil R: Baseline absolute lymphocyte count and ECOG performance
score are associated with survival in advanced non-small cell lung
cancer undergoing PD-1/PD-L1 blockade. J Clin Med.
8(1014)2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Maltese M, Panni S, Lazzarelli S,
Brighenti M, Negri F and Ratti M: High baseline lymphocyte count is
a predictive biomarker of prolonged time to progression in patients
with advanced solid tumors receiving checkpoint inhibitors. J Clin
Oncol. 35 (Suppl 15):e14532. 2017.
|
|
8
|
Zer A, Sung MR, Walia P, Khoja L, Maganti
M, Labbe C, Shepherd FA, Bradbury PA, Feld R, Liu G, et al:
Correlation of neutrophil to lymphocyte ratio and absolute
neutrophil count with outcomes with PD-1 axis inhibitors in
patients with advanced non-small-cell lung cancer. Clin Lung
Cancer. 19:426–434. e421. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lalani AKA, Xie W, Martini DJ, Steinharter
JA, Norton CK, Krajewski KM, Duquette A, Bossé D, Bellmunt J, Van
Allen EM, et al: Change in neutrophil-to-lymphocyte ratio (NLR) in
response to immune checkpoint blockade for metastatic renal cell
carcinoma. J Immunother Cancer. 6(5)2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bennati C, Mazza V, D'Arcangelo M, Minuti
G, Vecchiarelli S, Attilia L, Gili A, Montanari M, Landi L and
Cappuzzo F: E5Integrating programmed cell death ligand 1 (PD-L1)
and neutrophil to lymphocyte ratio (NLR) as predictive panel of
response to nivolumab in non-small cell lung cancer (NSCLC). Ann
Oncol 28 (Suppl_6): doi: 10.1093/annonc/mdx426.004.
|
|
11
|
Capone M, Giannarelli D, Mallardo D,
Madonna G, Festino L, Grimaldi AM, Vanella V, Simeone E, Paone M,
Palmieri G, et al: Baseline neutrophil-to-lymphocyte ratio (NLR)
and derived NLR could predict overall survival in patients with
advanced melanoma treated with nivolumab. J Immunother Cancer.
6(74)2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Moschetta M, Uccello M, Kasenda B, Mak G,
McClelland A, Boussios S, Forster M and Arkenau HT: Dynamics of
neutrophils-to-lymphocyte ratio predict outcomes of PD-1/PD-L1
blockade. Biomed Res Int. 2017(1506824)2017.PubMed/NCBI View Article : Google Scholar
|