Introduction
Dermatofibrosarcoma was first described as
progressive recurrent dermatofibroma in 1924 by Darier and Ferrand.
Subsequently, in 1925 Hoffmann referred to the disease as
dermatofibrosarcoma protuberans (DFSP) (1). It is a very rare neoplasm of the
breast. Dermatofibrosarcoma of the breast presents with a slow
growing pattern, initially in the dermis and then invading the
subcutaneous tissue (2). Usually,
DFSP is characterized as low to intermediate grade neoplasm with
high recurrence rate but rarely metastasises (3). The majority of DFSP presents as
low-grade tumours, but in 5-10% of cases the tumour contains
fibrosarcomatosous cells that upgrade the neoplasm in intermediate
grade with a higher aggressivity (4). Mainly affects young and middle-aged
patients 20 to 50 years old and as the lesion progresses, it
appears more and more protuberant (1). Surgery is the Gold Standard with
particular attention to obtain free margins in order to reduce the
recurrence rate (5). Wide local
excision (WLE) with minimum 3 cm free margins or Mohs micrographic
surgery (MMS) are recommended. We present a rare case of
dermatofibrosarcoma protuberans in the right breast of a
52-year-old female patient.
Case report
A 52-year-old patient presented to our Breast Unit
due to a skin lesion of her right breast that had slow but
persistent growth during the past 15 years. The physical
examination revealed a light-reddish, delineated exophytic, nodular
cutaneous mass 3x4 cm in the upper outer quadrant of the right
breast. No other finding from the breasts or axillary
lymphadenopathy was noted. She had an unremarkable personal and
family history.
Mammography revealed a dense, broad-based, well
circumscribed, cutaneous lesion. There was no associated
intramammary mass or microcalcifications. The lesion was evident on
previous mammograms, presenting a small growth rate.
In order to establish a diagnosis, a core-needle
biopsy was suggested which the patient denied. Subsequently, she
underwent surgical excision under local anesthesia. On gross
examination, there was a firm, grey-like mass 3.5 cm in diameter,
with irregular borders and extension into the subcutaneous tissue.
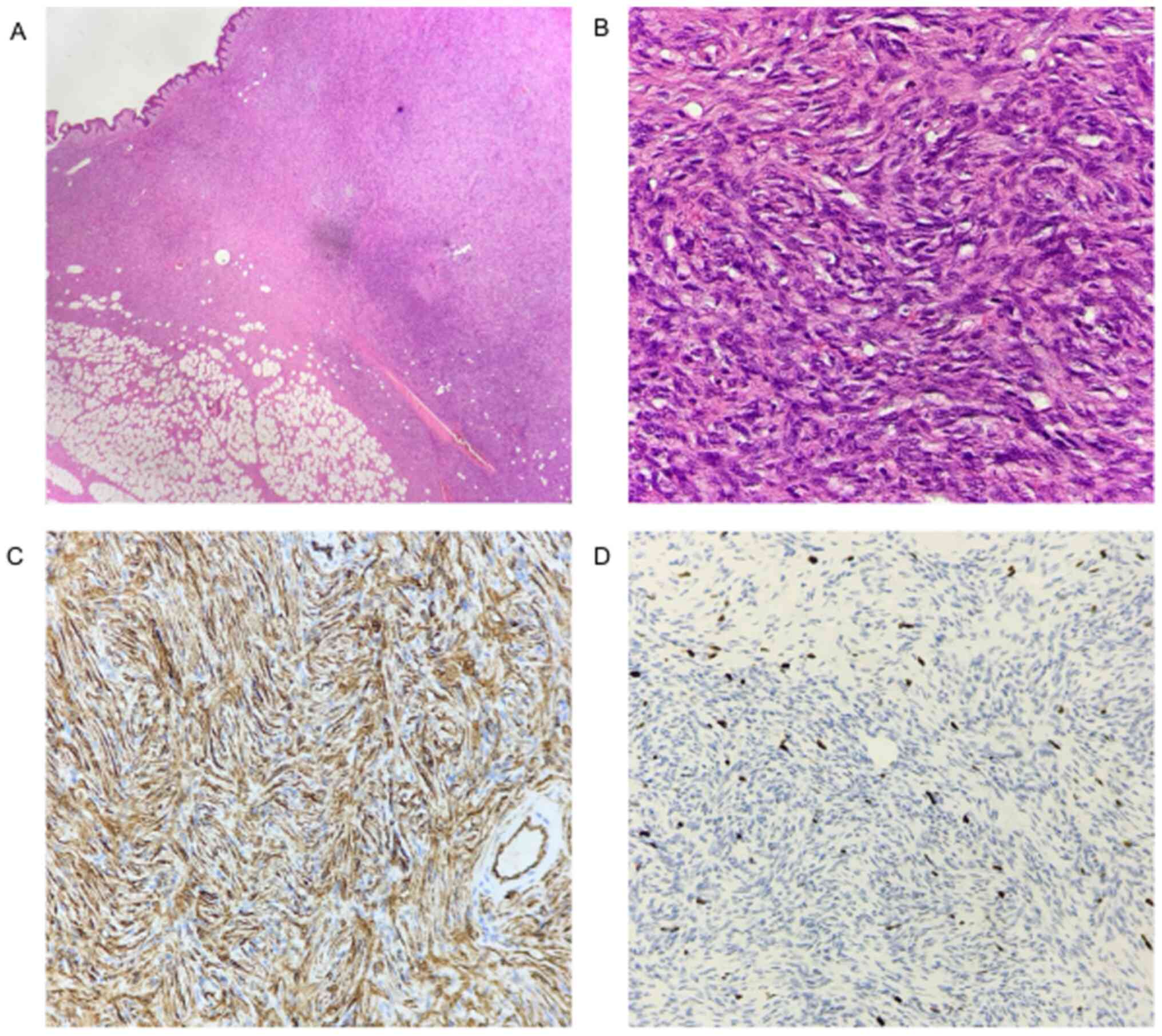
On microscopic examination, the tumor consisted of monomorphic
spindle-like cells arranged in storiform architectural pattern. The
nuclei were hyperchromatic, elongated, with little pleomorphism and
low mitotic activity (Fig. 1A and
1B). Immunohistochemically as
Fig. 1C and 1D show, the tumor cells showed diffuse
staining for CD34 and negative staining for CD68, while Ki67 was
15%.
Based on histological and immunohistochemical
findings, the mass was eventually diagnosed as dermatofibrosarcoma
protuberans. As the lateral and deep margins were focally involved
and in order to minimize the chance of local recurrence, a wide
re-excision of 3 cm healthy margins was performed.
Discussion
Dermatofibrosarcoma protuberans typically presents
as a painless, skin-coloured or yellow to brown nodular, exophytic,
nodular cutaneous mass (6,7). It tends to be well-circumscribed or
has subtle areas of microlobulation, while it can vary in size
(0.5->5 cm) (8). The lesion is
usually centered in the dermis, but it can invade the subcutaneous
tissue (9). It has an indolent
clinical course typically for years before the patients seek for
medical assistance.
Mammographically, DFSP presents as a dense mass.
Preoperative ultrasound examination or MRI offer limited
information about the degree of subcutaneous infiltration and can
be helpful only in selected cases (6,10).
Diagnosis is made histologically, either with a core-needle or an
excisional biopsy (7,10).
DFSP may appear histopathological similar to benign
fibrous histiocytoma but arises as a subcutaneous mass,
infiltrating and spreading along the surrounding tissue and fascia
with radial extensions of tumor in large distances (2). This growth pattern might be confusing
since both advanced breast cancer and squamous skin cancer follow
the same pattern. However, it rarely disseminates systematically
and metastasizes (3).
The etiology is not completely known. A history of
previous trauma has been suggested as predisposing factor in
approximately 10-20% of the cases. The reported cases included
lesions in surgical scars, burns, tattoo skin regions and even
bacillus Calmette-Guerin vaccination scar (11). But, the vast majority of cases arise
from the rearrangement of chromosomes 17 and 22, creating a
supernumerary ring chromosome composed of hybrid material derived
from t (17;22). This translocation leads to a continuous activation
of platelet derived growth factor receptor β-protein tyrosine
kinase due to a fusion of PDGFB gene with collagen Type Ia1 gene
(COL1A1) (12). Interestingly, this
PDGFB continuous loop is thought to be the main reason for the
sensitivity that this tumor has to imatinib, which is a tyrosine
kinase inhibitor. What this rearrangement fails to predict is the
metastatic potential of the tumor. There is increasing evidence
that positive immunoreactivity with CD34 and D2-40 antibody might
be the most accurate predictor for the latter (13). Moreover, increased age, high mitotic
index and increased cellularity are predictors of poor clinical
outcome (2). In our case, the
patient had no previous scar or trauma in the right breast and
immunochemistry showed a positive staining with CD34 and a low
mitotic index.
As far as treatment is concerned, surgical excision
is the standard of care, since DFSPs are resistant to chemotherapy
and radiotherapy (5). The exact
margin of resection is still unknown, but due to histologically
tumour-free margins varying significantly from clinically-free
ones, an excision with no less than 2-3 cm with skin, subcutaneous
tissue and fascia included is wide accepted. Mohs Micrographic
Surgery allows the extent of excision to be customized to the
microscopic extent of tumour and results in better tridimensional
margin control. In a series of 29 patients, this technique resulted
in 93.4% cure rate after the first surgery and low recurrence rates
at least short-term (14). MMS
offers lower but comparable local recurrence rates compared to WLE
(5,15). As a result, MMS is currently advised
as the method of choice for the treatment of DFSP (7,15).
Setbacks of this procedure include longer operative time, more
complex defect closure techniques and limited surgical expertise
(7,15,16).
However, MMS has yet to be widely diffused and many
centers-including ours-use as a primary mode of treatment standard
surgical techniques (WLE) and histopathological procedures
(7,17). Elective lymph node resection has no
additional benefit in prognosis of the disease (18). Adjuvant external irradiation is used
in cases with adverse prognostic factors such as high mitotic index
and positive margins.
DFSP tends to be locally aggressive (19). Systemic dissemination is rare (1-4%)
and usually occurs after multiple local recurrences (20,21).
Metastases are hematogenous, with the lungs being the most common
site (21). Extensive initial
staging workup is not done routinely and is essential only for
patients with suspected systemic disease (21). As there have been recurrences
reported after 5 years from the initial diagnosis, a long-term
follow-up is warranted. Diagnosis of DFSP in breast is challenging
because it is rare and imitates a wide range of benign and
malignant breast lesions and requires an increased readiness for
differentiating and managing it properly. We present this case to
recommend that obstetricians and gynecologists should be aware of
it and refer to a breast unit. Though a few treatments have been
suggested, wide local excision or Mohs micrographic surgery remain
the standard of care. To minimize recurrences, a personalized
follow-up plan should be applied due to the lack of an existing
evidence-based guideline.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contribution
DD and IB were major contributors in writing the
manuscript. AP was a major contributor in manuscript writing and
figure editing. NK performed the histological examination. DB and
KS performed the literature review. FD and IM contributed to
manuscript editing. All authors read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient gave a written informed consent allowing
the publication of histological findings and case presentation as
long as anonymity is preserved.
Competing interests
The authors declare that the they have no competing
interests.
References
|
1
|
Cottier O, Fiche M, Meuwly JY and Delaloye
JF: Dermatofibrosarcoma presenting as a nodule in the breast of a
75-year-old woman: A case report. J Med Case Rep.
5(503)2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bowne WB, Antonescu CR, Leung DH, Katz SC,
Hawkins WG, Woodruff JM, Brennan MF and Lewis JJ:
Dermatofibrosarcoma protuberans: A clinicopathologic analysis of
patients treated and followed at a single institution. Cancer.
88:2711–2720. 2000.PubMed/NCBI
|
|
3
|
Dragoumis DM, Katsohi LA, Amplianitis IK
and Tsiftsoglou AP: Late local recurrence of dermatofibrosarcoma
protuberans in the skin of female breast. World J Surg Oncol.
8(48)2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Woo KJ, Bang SI, Mun GH, Oh KS, Pyon JK
and Lim SY: Long-term outcomes of surgical treatment for
dermatofibrosarcoma protuberans according to width of gross
resection margin. J Plast Reconstr Aesthet Surg. 69:395–401.
2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Loghdey MS, Varma S, Rajpara SM, Al-Rawi
H, Perks G and Perkins W: Mohs micrographic surgery for
dermatofibrosarcoma protuberans (DFSP): A single-centre series of
76 patients treated by frozen-section Mohs micrographic surgery
with a review of the literature. J Plast Reconstr Aesthet Surg.
67:1315–1321. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lee SJ, Mahoney MC and Shaughnessy E:
Dermatofibrosarcoma protuberans of the breast: Imaging features and
review of the literature. AJR Am J Roentgenol. 193:W64–W69.
2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Saiag P, Grob JJ, Lebbe C, Malvehy J, del
Marmol V, Pehamberger H, Peris K, Stratigos A, Middelton M, Basholt
L, et al: Diagnosis and treatment of dermatofibrosarcoma
protuberans. European consensus-based interdisciplinary guideline.
Eur J Cancer. 51:2604–2608. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Taylor HB and Helwig EB:
Dermatofibrosarcoma protuberans. A study of 115 cases. Cancer.
15:717–725. 1962.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bague S and Folpe AL: Dermatofibrosarcoma
protuberans presenting as a subcutaneous mass: A
clinicopathological study of 15 cases with exclusive or
near-exclusive subcutaneous involvement. Am J Dermatopathol.
30:327–232. 2008.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ugurel S, Kortmann RD, Mohr P, Mentzel T,
Garbe C and Breuninger H: Short German guidelines:
Dermatofibrosarcoma protuberans. J Dtsch Dermatol Ges. 6 (Suppl
1):S17–S18. 2008.PubMed/NCBI View Article : Google Scholar : (In English,
German).
|
|
11
|
Stamatakos M, Fyllos A, Siafogianni A,
Ntzeros K, Tasiopoulou G, Rozis M and Kontzoglou K:
Dermatofibrosarcoma protuberans: A rare entity and review of the
literature. J Buon. 19:34–41. 2014.PubMed/NCBI
|
|
12
|
Nakanishi G, Lin SN, Asagoe K, Suzuki N,
Matsuo A, Tanaka R, Makino E, Fujimoto W and Iwatsuki K: A novel
fusion gene of collagen type I alpha 1 (exon 31) and
platelet-derived growth factor B-chain (exon 2) in
dermatofibrosarcoma protuberans. Eur J Dermatol. 17:217–219.
2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sadullahoglu C, Dere Y, Atasever TR, Oztop
MT and Karaaslan O: The Role of CD34 and D2-40 in the
differentiation of dermatofibroma and dermatofibrosarcoma
protuberans. Turk Patoloji Derg. 1:223–227. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Snow SN, Gordon EM, Larson PO, Bagheri MM,
Bentz ML and Sable DB: Dermatofibrosarcoma protuberans: A report on
29 patients treated by Mohs micrographic surgery with long-term
follow-up and review of the literature. Cancer. 101:28–38.
2004.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Malan M, Xuejingzi W and Quan SJ: The
efficacy of Mohs micrographic surgery over the traditional wide
local excision surgery in the cure of dermatofibrosarcoma
protuberans. Pan Afr Med J. 33(297)2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Meguerditchian AN, Wang J, Lema B,
Kraybill WG, Zeitouni NC and Kane JM III: Wide excision or Mohs
micrographic surgery for the treatment of primary
dermatofibrosarcoma protuberans. Am J Clin Oncol. 33:300–303.
2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Maji S, Paul MJ and Sen S:
Dermatofibrosarcoma protuberans of the breast-a rare entity. Indian
J Surg Oncol. 9:351–354. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Llombart B, Serra-Guillen C, Monteagudo C,
Lopez Guerrero JA and Sanmartin O: Dermatofibrosarcoma protuberans:
A comprehensive review and update on diagnosis and management.
Semin Diagn Pathol. 30:13–28. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Popov P, Bohling T, Asko-Seljavaara S and
Tukiainen E: Microscopic margins and results of surgery for
dermatofibrosarcoma protuberans. Plast Reconstr Surg.
119:1779–1784. 2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Pohlodek K, Meciarova I, Grossmann P and
Kinkor Z: Dermatofibrosarcoma protuberans of the breast: A case
report. Oncol Lett. 14:993–998. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Rutgers EJ, Kroon BB, Albus-Lutter CE and
Gortzak E: Dermatofibrosarcoma protuberans: Treatment and
prognosis. Eur J Surg Oncol. 18:241–248. 1992.PubMed/NCBI
|