Introduction
Locally advanced thyroid carcinoma can involve the
larynx (1,2). In such cases, partial laryngotracheal
resection is often performed as surgical treatment. Successful
reconstruction is required to avoid palliative stenting or
permanent tracheostomy. An important aspect of laryngotracheal
reconstruction is the establishment of skeletal support in order to
resist airway pressure changes (3).
Although there are several surgical techniques for performing
laryngotracheal reconstruction, surgeons occasionally find it
difficult to maintain an appropriate laryngeal and/or tracheal
shape.
Anaplastic thyroid carcinoma (ATC) is a rare but
highly aggressive malignant tumour that accounts for 1-2% of all
thyroid malignancies (4). Although
ATC is treated with a multidisciplinary approach that includes
surgery, radiotherapy, and chemotherapy, its prognosis is extremely
poor. Lenvatinib, a tyrosine kinase inhibitor, has been approved
for use in patients with unresectable or metastatic thyroid
carcinoma. The use of post-operative lenvatinib therapy has not yet
been established, and further studies are required to confirm the
efficacy of this therapy.
It is known that ATC may not only originate de
novo but also arise as a conversion of differentiated thyroid
carcinoma (5). Head and neck
surgeons may sometimes encounter ATC incidentally when treating
patients with locally advanced differentiated thyroid carcinomas
(6).
We report a case of incidental ATC that invaded the
larynx, with long-term survival with lenvatinib therapy and
post-operative preservation of laryngeal function.
Case report
Case presentation
A 71-year-old woman visited Nara Medical University
Hospital with complaints of hoarseness and a left-sided neck mass
(45x30 mm) in October 2018. Left vocal cord paralysis was confirmed
endoscopically. The larynx was displaced to the right by a
slow-growing left thyroid lobe tumour. We were unable to identify
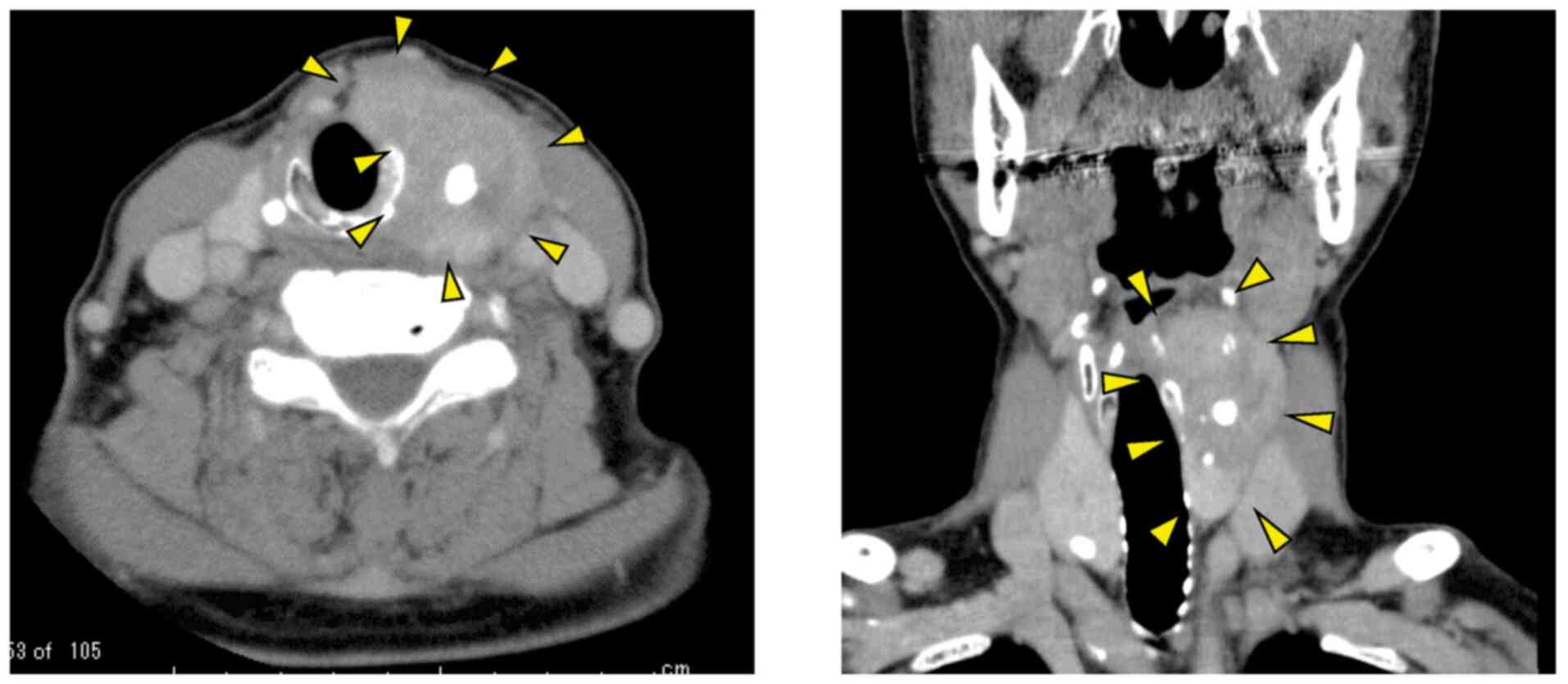
the border between the larynx and the tumour. Computed tomography
showed a calcified thyroid tumour extending from the left side of
the thyroid cartilage to the upper part of the cricoid cartilage
(Fig. 1). Positron emission
tomography/computed tomography showed no evidence of distant
metastasis. The tumour was histologically diagnosed as papillary
thyroid carcinoma (PTC) with no evidence of poorly differentiated
carcinoma or ATC. Subsequently, the patient was diagnosed with PTC
(cT4aN1bM0, stage III).
Surgery
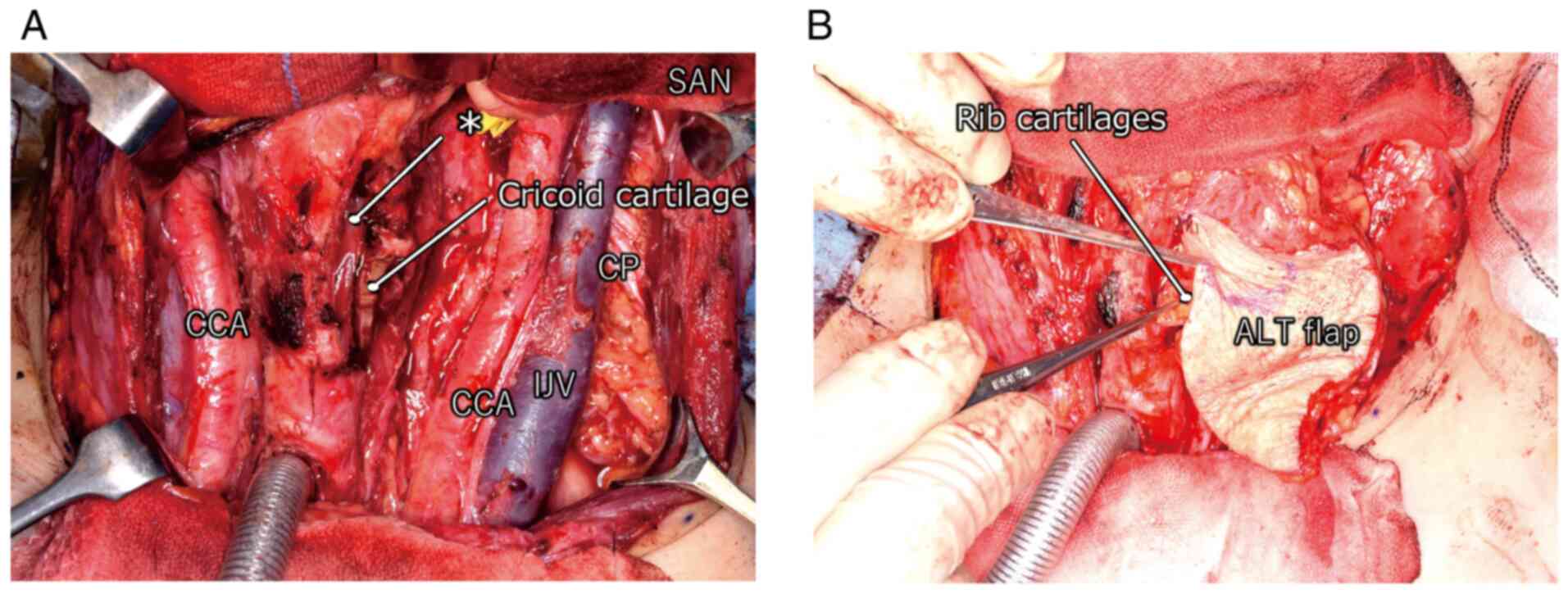
Total thyroidectomy with hemi-laryngectomy and neck
dissection was performed. The laryngeal defect was reconstructed
using a prefabricated anterolateral thigh (ALT) flap and free rib
cartilage grafts in order to maintain laryngeal function.
After tumour excision, bilateral paratracheal and
left lateral neck dissection was performed. The dissected tissues
were gathered toward the thyroid, and the thyroid was dissected
from the trachea with relative ease. We resected from the thyroid
cartilage to the superior edge of the cricoid cartilage in order to
complete en bloc extirpation of the lesion because the tumour
involved these structures. We resected approximately 40% of the
laryngeal defect, which would have resulted in loss of airway and
phonatory function. To compensate the laryngeal defect, grafting
using an ALT flap and free rib cartilage was performed as follows:
First, the left ALT flap (15x7 cm) was harvested and laid over the
surgical defect, and microscopic vascular anastomoses were
established. The flap had two perforators based on the left lateral
circumflex femoral artery descending branch. The left superior
thyroid artery was used as the recipient artery and the branch of
the left external jugular vein was used as the recipient vein.
Subsequently, small pieces of rib cartilage were harvested from the
left side of the chest. The cartilage pieces were placed in the
subcutaneous burrow under the ALT flap (Fig. 2). This tissue and the laryngeal
remnant constituted the reconstructed larynx that was fully
functional.
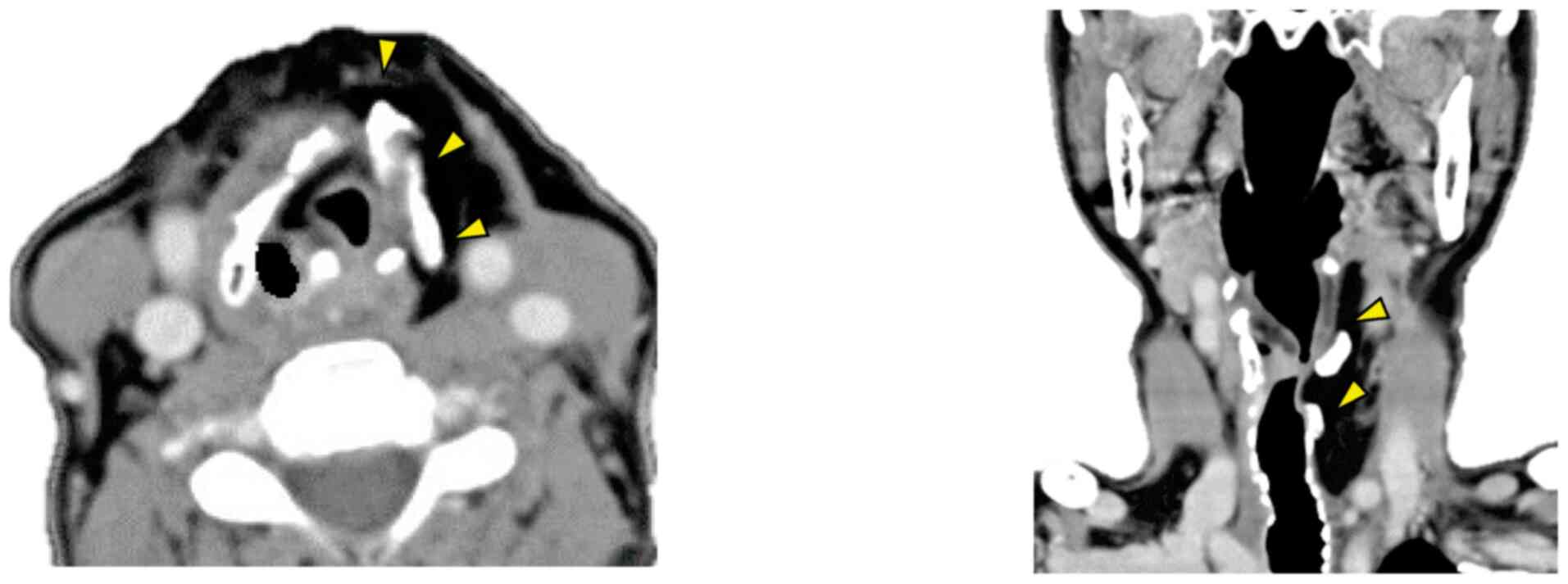
On the sixth post-operative day, the patient started
oral intake based on videofluorography findings. On the seventh
post-operative day, she was able to phonate with a speech cannula.
Four months later, the patient was decannulated, and the stoma
spontaneously closed. Consequently, one-stage reconstruction was
successfully accomplished (Fig.
3).
Outcome and follow-up
Post-operative histopathological examination of the
tumour revealed that the tumour was a PTC with focal anaplastic
changes. The surgical margin was negative. Lymph node metastases
were detected in the central, left lateral, left lateral
retropharyngeal, and superior mediastinal regions. Consequently,
the patient was diagnosed with ATC (pT4aN1bM0, stage IVB).
Following the histopathological diagnosis, positron emission
tomography/computed tomography was performed two months
post-operatively, and early recurrence in the left posterior neck
was detected. Considering the properties of ATC and the location of
the recurrence, the new lesion was determined to be unresectable.
Therapeutic modalities such as chemotherapy, radiotherapy,
chemoradiotherapy, and tyrosine kinase inhibitors were considered.
Finally, lenvatinib therapy was selected with the expectation of
prolonging survival and maintaining good flap condition. Three
months post-operatively, daily administration of 24 mg of
lenvatinib was started.
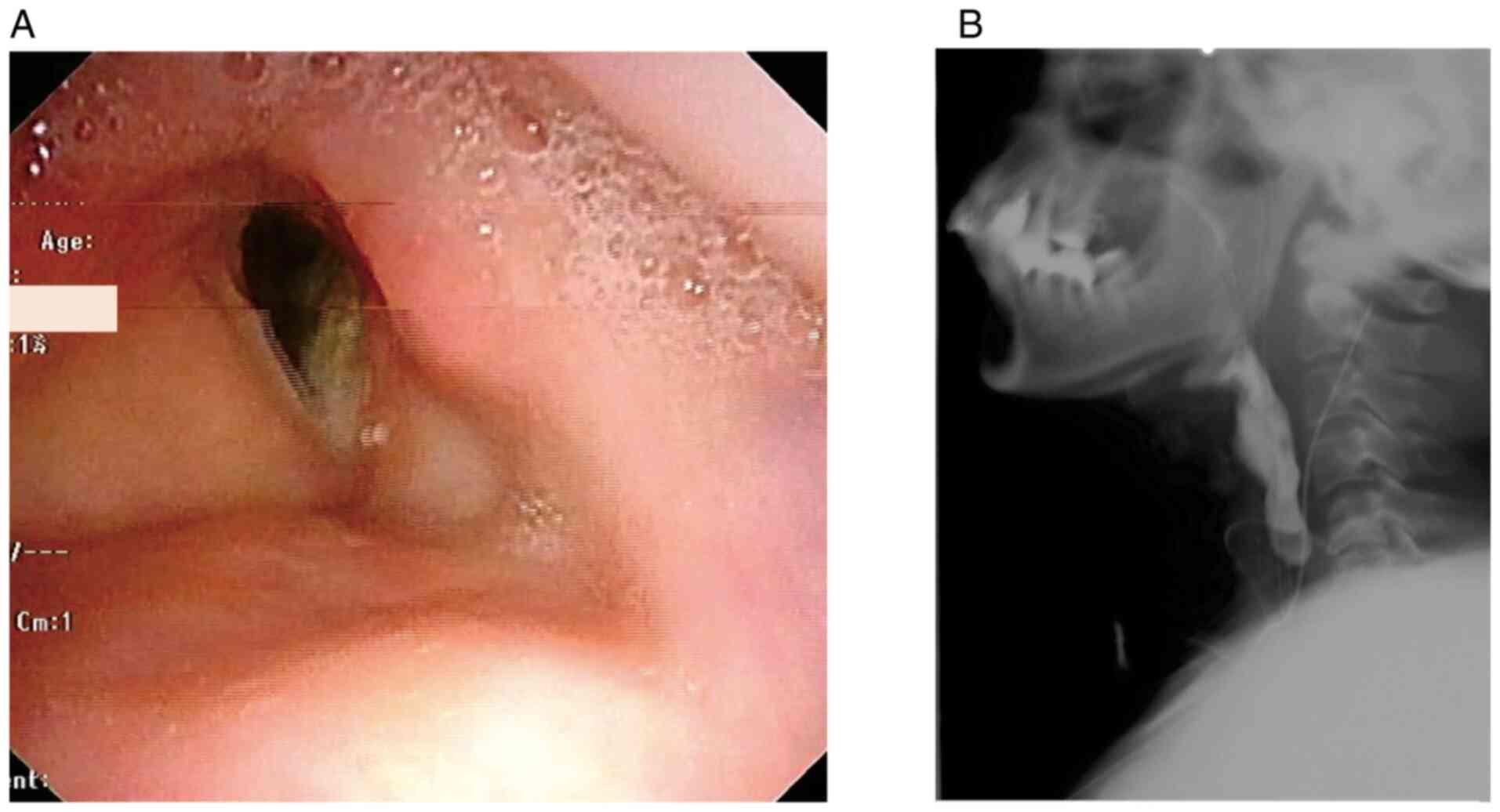
Twenty-six months after surgery, the patient's good
condition had been maintained without any noteworthy adverse
effects due to lenvatinib. Positron emission tomography/computed
tomography was performed, and we detected no sign of the tumour in
the left posterior neck. Post-operative lenvatinib therapy was
highly effective and her speech and swallowing functions were
approximately the same as those pre-operatively (Fig. 4).
Discussion
The larynx not only has a complex anatomy but is
also involved in multiple functions, such as breathing, speech, and
swallowing. It may be directly invaded by carcinomas of the
oesophagus or thyroid. It is said that 1-7% of thyroid carcinomas
invade the trachea and/or larynx. Advanced thyroid carcinoma
occasionally causes tracheal obstruction, leading to death
(1,2). Surgical management is thought to be
effective in resectable advanced thyroid carcinoma (7,8).
However, it involves partial laryngotracheal resection. Our
patient's tumour extended beyond the thyroid capsule, that is, from
the left wing of the thyroid cartilage to the cricoid cartilage.
Therefore, the laryngeal defect was reconstructed after total
thyroidectomy and hemi-laryngectomy. Many authors have described
the technique of laryngotracheal reconstruction (3,9-12).
We used an ALT flap and rib cartilage grafts. An ALT flap is often
used as material for head and neck reconstruction. However, there
are few reports on its application in laryngeal reconstruction. An
ALT flap has adequate size and volume to cover laryngeal defects.
In our patient, we were able to use it to sufficiently compensate
for a 40% defect of the larynx. It is also easy to harvest in the
supine position. Moreover, the post-operative scar at the donor
site is hidden behind the patient's clothes, making it relatively
inconspicuous in daily life. However, follow-up of the patient's
thigh condition is important. Post-operatively, older patients
should undergo early rehabilitation to maintain independence in
their activities of daily living.
Various materials such as the clavicle, rib
cartilage, auricular cartilage, and nasal septum cartilage are used
to reinforce the laryngeal lumen in case of reconstruction. We used
rib cartilage because it is rigid and easy to harvest and mould.
The donor site scar can be easily hidden behind the patient's
clothes, similarly to that of an ALT flap. We performed laryngeal
reconstruction to maintain airway patency. We vertically inserted
the rib cartilage into a pocket immediately below the dermis of the
skin flap. Kubo reported the effectiveness of this procedure using
a forearm flap (13). As an ALT
flap is soft, it is easy to mould it to the irregularly shaped
larynx and place trimmed cartilage grafts inside it. Additionally,
placement of the graft immediately below the dermis makes it adhere
easily and helps to maintain the shape of the reconstructed larynx
and trachea. Neck flexibility is also important. Movement of the
cartilage pieces makes the neck more flexible. On the other hand,
prevention of necrosis or leakage is important.
Although numerous techniques of laryngeal
reconstruction have been reported, most of them involve stepwise
procedures and palliative stenting. A one-stage procedure could
reduce patient burden and help to avoid multiple surgeries. This
procedure may lead to early healing of the surgical wound, which
may improve patients' quality of life. Post-operative management,
including monitoring for signs of infection and inflammation, is
important. In our patient, post-operative computed tomography and
laryngoscopy showed a reconstructed larynx with sufficient
function. Twenty-six months post-operatively, the patient
maintained an excellent airway and her larynx functioned
adequately.
ATC is a fatal disease for which various therapeutic
modalities have been unsuccessfully tried. Moreover, it has been
reported that 20-50% of patients with ATC have distant metastasis
at initial presentation, and the recurrence rate after treatment is
nearly 40% (14,15). This worsens the prognosis. Sugitani
et al (16,17) devised a prognostic index for ATC
based on four unfavourable prognostic factors: Acute symptoms
(duration of severe symptoms such as dysphonia, dysphagia,
dyspnoea, and rapid tumour growth in <1 month), leukocytosis
(leukocyte count 10,000/mm3), tumour size >5 cm, and
distant metastasis. They recommended attempting multimodal
treatment for patients with a prognostic index of ≤1. Our patient
did not have any unfavourable prognostic factors.
Our patient experienced recurrence after laryngeal
reconstruction using an ALT flap and rib cartilage grafts. While
treating the recurrence, we had to focus on the condition of these
flaps, which needed sufficient blood supply. Radiotherapy often
damages tissues and induces inflammatory responses, such as
arteritis and thrombosis in small vessels (18-20).
Gessert et al (21) reported
that the incidence of laryngeal chondroradionecrosis in patients
with laryngeal cancer treated with radiotherapy is 2.4%. It is
necessary to avoid these complications, maintain the flaps in good
condition, and assume that chondroradionecrosis may occur following
radiotherapy to the neck (22,23).
Radiotherapy can also inhibit post-operative wound healing.
Considering these problems and the post-operative
histopathological diagnosis of ATC, a multidisciplinary team
consisting of medical oncologists, radiologists, and head and neck
surgeons decided to avoid post-operative radiotherapy and to treat
the patient with systematic administration of lenvatinib rather
than local therapy. This decision led to good outcomes with respect
to preservation of laryngeal function and improvement of
survival.
Her condition has been maintained at 26 months after
the initial treatment. She has good laryngeal function, and we will
continue to regularly follow her progress.
In conclusion, one-stage laryngeal reconstruction is
highly useful as a treatment for advanced thyroid carcinoma
invading the larynx. This procedure could be effective in reducing
patient burden and improving quality of life. The use of an ALT
flap with free rib cartilage grafts resulted in maintained
laryngeal function and neck flexibility. Lenvatinib may be an
option for the treatment of early recurrence of ATC after
reconstructive surgery with a free flap.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AT made substantial contributions to conception and
acquisition of data, and drafted the manuscript. HU, TM, SK, YY,
MK, TY and TK provided cancer-related scientific inputs and
collected clinical data. GM and CO made the pathological diagnosis
and provided histopathological diagnosis-related scientific inputs.
HU, TM, TY and TK critically revised the manuscript. AT and TM
confirm the authenticity of all the raw data. All authors have
accepted responsibility for the entire content of this manuscript
and have approved the submission. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Djalilian M, Beahrs OH, Devine KD, Weiland
LH and DeSanto LW: Intraluminal involvement of the larynx and
trachea by thyroid cancer. Am J Surg. 128:500–504. 1974.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lawson W, Som HL and Biller HF: Papillary
adenocarcinoma of the thyroid invading the upper air passages. Ann
Otol Rhinol Laryngol. 86 (6 Pt 1):751–755. 1977.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Yu P, Clayman GL and Walsh GL: Long-term
outcomes of microsurgical reconstruction for large tracheal
defects. Cancer. 117:802–808. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hundahl SA, Fleming ID, Fremgen AM and
Menck HR: A national cancer data base report on 53,856 cases of
thyroid carcinoma treated in the U.S., 1985-1995 [see comments].
Cancer. 83:2638–2648. 1998.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hsu KT, Yu XM, Audhya AW, Jaume JC, Lloyd
RV, Miyamoto S, Prolla TA and Chen H: Novel approaches in
anaplastic thyroid cancer therapy. Oncologist. 19:1148–1155.
2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Are C and Shaha AR: Anaplastic thyroid
carcinoma: Biology, pathogenesis, prognostic factors, and treatment
approaches. Ann Surg Oncol. 13:453–464. 2006.PubMed/NCBI View Article : Google Scholar
|
|
7
|
McCarty TM, Kuhn JA, Williams WL Jr,
Ellenhorn JD, O'Brien JC, Preskitt JT, Lieberman ZH, Stephens J,
Odom-Maryon T, Clarke KG and Wagman LD: Surgical management of
thyroid cancer invading the airway. Ann Surg Oncol. 4:403–408.
1997.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kanazawa S and Kammori M: Case report:
84-month disease-free survival after surgery for anaplastic thyroid
carcinoma. J Nippon Med Sch. 86:38–42. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Eliachar I, Roberts JK, Welker KB and
Tucker HM: Advantages of the rotary door flap in laryngotracheal
reconstruction: Is skeletal support necessary? Ann Otol Rhinol
Laryngol. 98 (1 Pt 1):37–40. 1989.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Detwiller KY, Schindler JS, Schneider DS
and Lindau R: Complex adult laryngotracheal reconstruction with a
prefabricated flap: A case series. Head Neck. 35:E376–E380.
2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Den Hondt M and Vranckx JJ: Reconstruction
of defects of the trachea. J Mater Sci Mater Med.
28(24)2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Teng MS, Malkin BD and Urken ML:
Prefabricated composite free flaps for tracheal reconstruction: A
new technique. Ann Otol Rhinol Laryngol. 114:822–826.
2005.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kubo T, Kurita T, Tashima H, Suzuki M,
Uemura H, Fujii T, Seike S, Inohara H and Hosokawa K: Immediate
tracheal reconstruction with forearm flap and bone graft.
Microsurgery. 39:46–52. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
O'Neill JP and Shaha AR: Anaplastic
thyroid cancer. Oral Oncol. 49:702–706. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Corrigan KL, Williamson H, Range DE,
Niedzwiecki D, Brizel DM and Mowery YM: Treatment outcomes in
anaplastic thyroid cancer. J Thyroid Res.
2019(8218949)2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sugitani I, Kasai N, Fujimoto Y and
Yanagisawa A: Prognostic factors and therapeutic strategy for
anaplastic carcinoma of the thyroid. World J Surg. 25:617–622.
2001.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sugitani I, Onoda N, Ito KI and Suzuki S:
Management of anaplastic thyroid carcinoma: The fruits from the ATC
research consortium of Japan. J Nippon Med Sch. 85:18–27.
2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chandler JR: Radiation fibrosis and
necrosis of the larynx. Ann Otol Rhinol Laryngol. 88:509–514.
1979.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Filntisis GA, Moon RE, Kraft KL, Farmer
JC, Scher RL and Piantadosi CA: Laryngeal radionecrosis and
hyperbaric oxygen therapy: Report of 18 cases and review of the
literature. Ann Otol Rhinol Laryngol. 109:554–562. 2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Berger G, Freeman JL, Briant TD, Berry M
and Noyek AM: Late post radiation necrosis and fibrosis of the
larynx. J Otolaryngol. 13:160–164. 1984.PubMed/NCBI
|
|
21
|
Gessert TG, Britt CJ, Maas AMW, Wieland
AM, Harari PM and Hartig GK: Chondroradionecrosis of the larynx:
24-year university of Wisconsin experience. Head Neck.
39:1189–1194. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Alraiyes AH, Alraies MC and Abbas A:
Radiation-associated airway necrosis. Ochsner J. 13:273–275.
2013.PubMed/NCBI
|
|
23
|
Cukurova I and Cetinkaya EA: Radionecrosis
of the larynx: Case report and review of the literature. Acta
Otorhinolaryngol Ital. 30(205)2010.PubMed/NCBI
|