Introduction
Malignant tumors of the maxillary sinus are rare
neoplasms that account for ~3% of head and neck cancers and 0.5% of
all malignant diseases. The annual incidence of maxillary sinus
cancer is 0.5-1 case per 100,000 of the population (1). Squamous cell carcinoma is the most
common histologic type, accounting for ~70-80% of maxillary sinus
cancer (1). Most patients with
maxillary sinus cancer have no symptoms in the early stage and,
therefore, many of these patients are diagnosed in the advanced
stage of the disease (2). At the
time of diagnosis, 70-80% of maxillary sinus carcinomas present
with local extension and are classified as T3 or T4 using the
American Joint Committee on Cancer staging system (3,4).
Maxillary sinus squamous cell carcinoma is an
aggressive tumor and treatment includes surgery, radiation therapy,
or a combination of both. Nevertheless, for more advanced stages,
both surgery and radiotherapy have their limitations (5). Locally advanced carcinoma of the
maxillary sinus has been reported to have a poor prognosis
(6). Induction chemotherapy may be
effective for locally advanced and technically unresectable
maxillary sinus cancers resulting in successful surgery in a
significant proportion of patients (6).
Immunotherapy is another possible treatment for
maxillary sinus cancer. Immune checkpoint blockade has emerged as a
promising treatment option. Numerous anti-PD-1 and anti-PD-L1
antibodies are under investigation, and two of them (nivolumab and
pembrolizumab) were approved by the Food and Drug Administration
(FDA) in 2016 for sinonasal cancers (7). PD-1 and its ligands (PD-L1 and PD-L2)
are mainly involved in the modulation of T-cell activity. Tumors
upregulate PD-L1 to mediate immune tolerance. Blocking the PD-1
pathway enhances T-cell-mediated tumor cell killing (8).
There have been numerous studies on the use of the
combination of chemotherapy and radiotherapy for maxillary sinus
cancer investigating the effect of the combination of immunotherapy
and radiotherapy on maxillary sinus cancer (8,9).
However, to date, no study has investigated the combination of
chemotherapy and immunotherapy for maxillary sinus cancer.
The case of a patient with advanced maxillary sinus
cancer who refused surgery and radiotherapy is presented. After
discussion, the patient elected a combination of chemotherapy and
immunotherapy as initial palliative treatment. A marked regression
of the tumor including orbital invasion with stable condition was
noted at the follow-up of one year.
Case report
A 59-year-old man with a history of nasopharyngeal
carcinoma was treated with concurrent chemoradiotherapy in 2004.
The patient experienced right maxillary swelling for several weeks
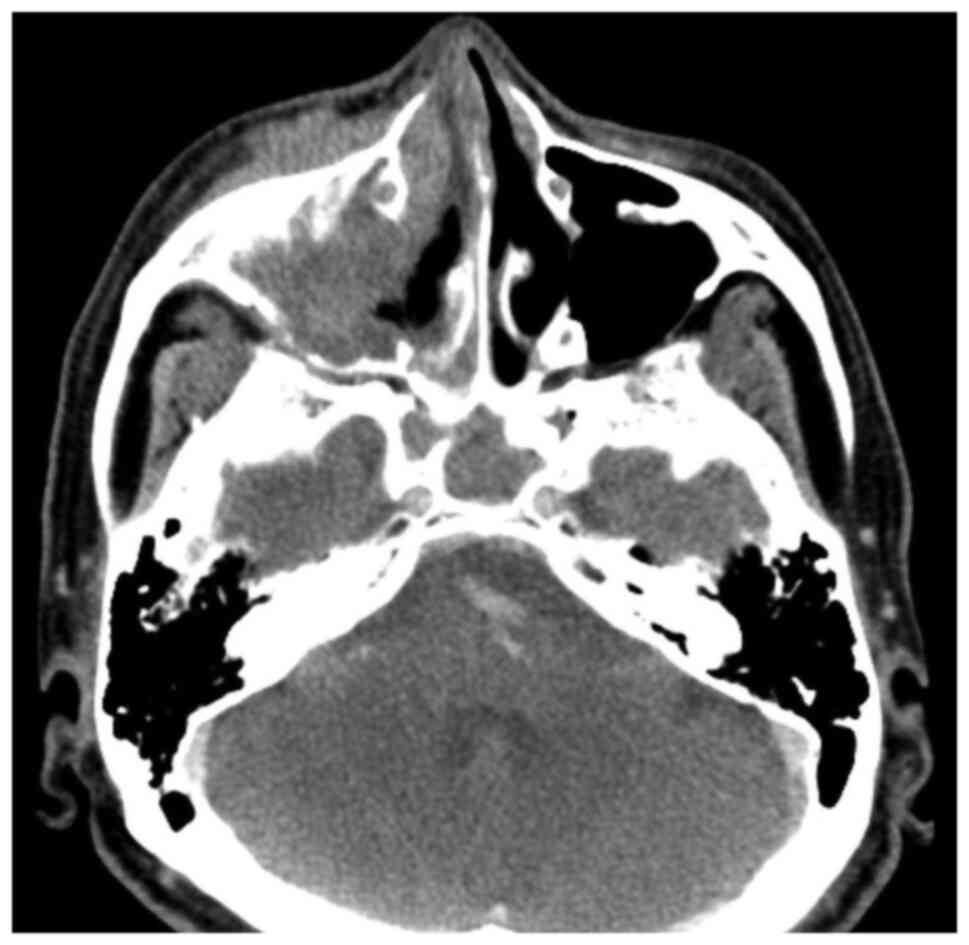
with blurred vision in the right eye since February 2019. Computed
tomography performed on March 29, 2019 revealed a suspicious soft
tissue mass involving the right maxillary sinus, right nasal
cavity, inferior extraconal space of the right eye, right cheek,
and right hard palate with extension into the right pterygopalatine
fossa (Figs. 1 and 2). The patient underwent biopsy through
endoscopic sinus surgery at Chi-Mei Medical Center (Tainan,
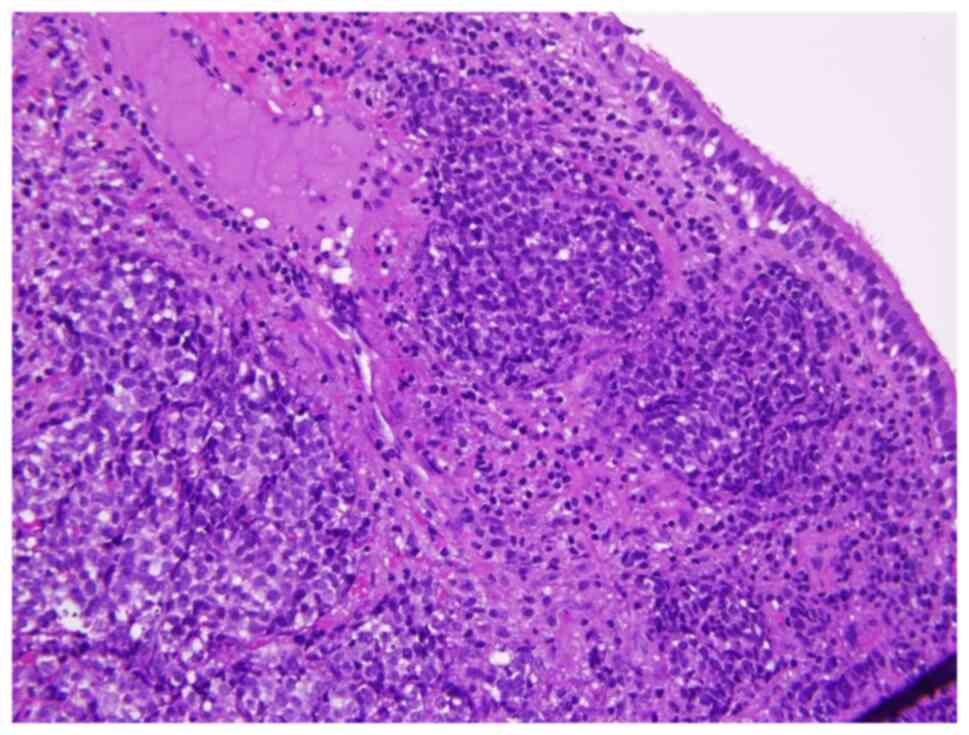
Taiwan). Pathology revealed infiltrative sheets of neoplastic cells
featuring a syncytial growth pattern and positive for p40 but
negative for CD56, synaptophysin, or chromogranin-A, consistent
with invasive carcinoma with squamous differentiation (Fig. 3). The patient was diagnosed and
staged as right maxillary sinus carcinoma with invasion of the
right orbital fossa, cT4aN0M0 (stage IVA).
The patient declined surgery and radiotherapy but
received a combination of chemotherapy and immunotherapy as
palliative treatment. Based on his height (169 cm) and weight (68
kg), the patient received a combination regimen of immunotherapy
(pembrolizumab 200 mg on day 1) and chemotherapy (cisplatin ~120 mg
on day 1; fluorouracil ~1,740 mg on days 1-3) from April 15 to
September 30, 2019 for eight cycles. The patient tolerated
treatment well despite experiencing mild dizziness occasionally.
Right maxillary swelling and right eye blurred vision gradually
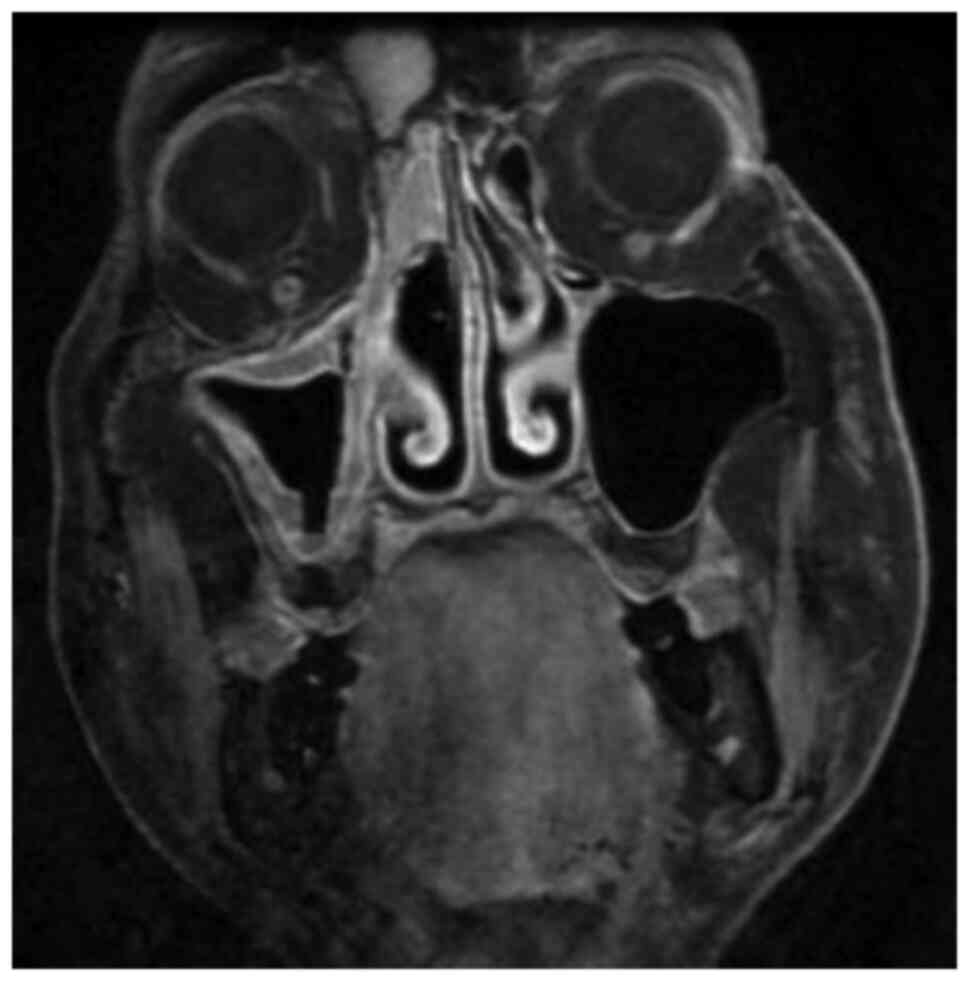
disappeared. Magnetic resonance imaging (MRI) performed on January
6, 2020 revealed marked regression of the tumor including right
orbital invasion (Fig. 4).
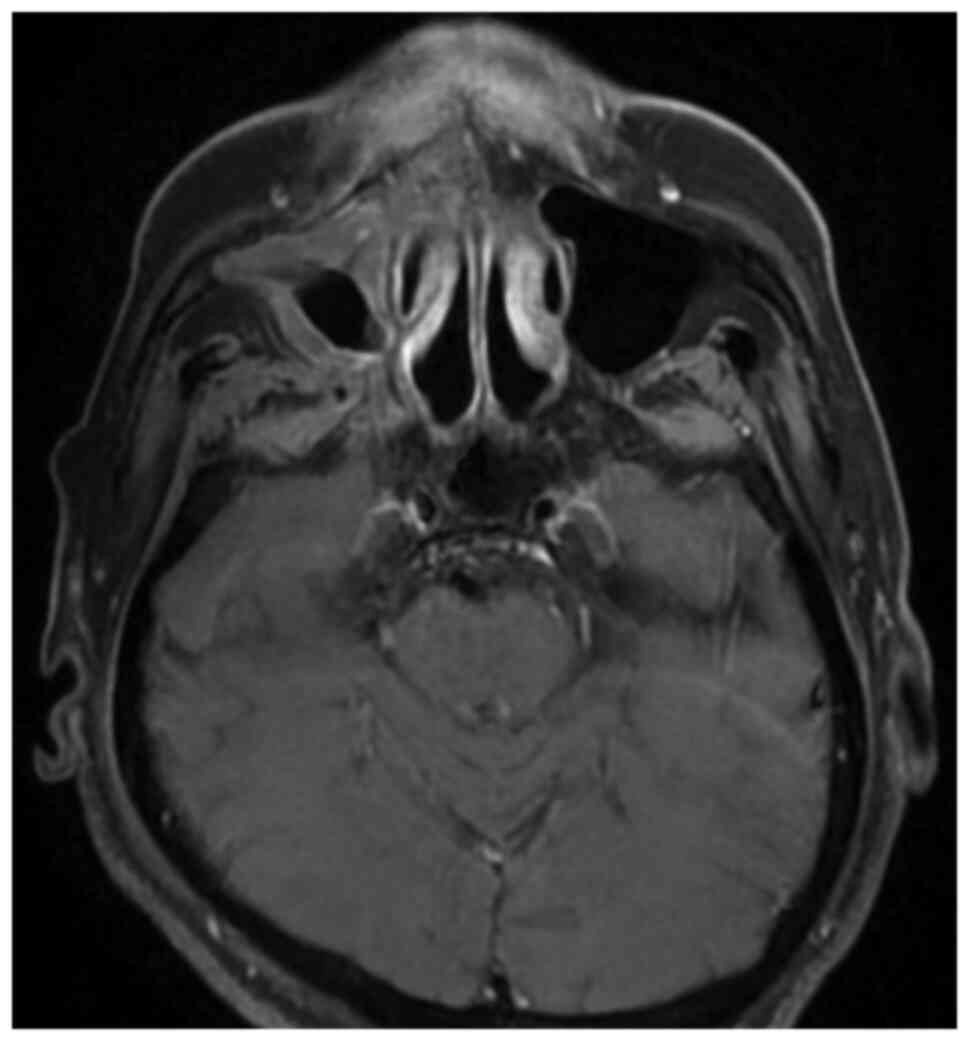
However, stable enhancing lesions were still present in the right
pterygopalatine fossa, right foramen rotundum and right medial and
lateral pterygoid plates. A residual tumor was suspected in the
enhancing lesions (Fig. 5). The
follow-up of Epstein-Barr virus viral load is presented in Table I. On the 1-year follow-up visit,
the patient was in stable condition. MRIs were planned for this
patient in future follow-ups.
 | Table IEpstein-Barr virus viral load
(IU/ml). |
Table I
Epstein-Barr virus viral load
(IU/ml).
| 2019/5/30 | 2019/9/5 | 2019/11/12 | 2020/2/18 | 2020/5/12 |
|---|
| Not detected | Not detected | Not detected | Not detected | Not detected |
Discussion
The main treatment options for maxillary sinus
cancer include surgery, radiation therapy, and a combination of
both. Since the patient in our case refused surgery and
radiotherapy, other possibilities were discussed with him. The
patient decided to undergo the combination of chemotherapy and
immunotherapy as palliative treatment. There have been limited
studies in the literature on the combination of chemotherapy and
immunotherapy for advanced maxillary sinus. Thus, it is valuable to
investigate its effects.
Concurrent chemoradiation was not used due to the
patient's history of nasopharyngeal cancer treated with
radiotherapy. Radiation toxicity was considered. According to the
evaluation of the radiation oncologist, blindness of the right eye
from cancer radiotherapy could occur.
Numerous anti-PD-1 and anti-PD-L1 antibodies are
under investigation, and two of them (nivolumab and pembrolizumab)
were approved by the FDA in 2016 for sinonasal cancers (8). Blocking the PD-1 pathway enhances T
cell-mediated killing of tumor cells (8). The results of the immunohistochemical
analysis of the tumor of the patient revealed that it was positive
for PD-L1 and the tumor proportion score was 10%. It is known that
high PD-L1 expression levels and a high mutational burden are
correlated with higher response rates to PD-1-based immunotherapies
(8). Previous studies have
revealed the effect of combining immunotherapy and radiotherapy on
maxillary sinus cancer (8,9) indicating favorable responses. Thus,
it may be used as an alternative for this patient if he elected
radiotherapy, despite that radiation toxicity must be considered
due to the history of the patient with radiotherapy for
nasopharyngeal cancer.
There are other examples of combination of
chemotherapy and immunotherapy for other tumors. One example is
gemcitabine and cisplatin plus pembrolizumab as neoadjuvant therapy
before radical cystectomy in patients with muscle-invasive bladder
cancer (10). Another example is
pembrolizumab plus chemotherapy in metastatic non-small cell lung
cancer (11). The combination of
chemotherapy and immunotherapy can achieve additive or synergistic
clinical activity. Two major means through which chemotherapy
promotes tumor immunity are by inducing immunogenic cell death as
part of its intended therapeutic effect and by disrupting
strategies that tumors use to evade immune recognition (12).
It was noted that induction chemotherapy for locally
advanced maxillary sinus cancer increased the possibility of
complete resection with orbital preservation as well as tumor
downstaging. The MRI of the patient on January 6, 2020 still showed
a stable enhancing lesion in the right pterygopalatine fossa, right
foramen rotundum, and right medial and lateral pterygoid plates. A
residual tumor was suspected and considered technically
unresectable due to the involvement of the pterygoid plates.
However, regression of advanced maxillary sinus cancer including
right orbital invasion was observed. The effect of the combination
of chemotherapy and immunotherapy may play a role in downstaging
tumors, although further investigation is required.
In conclusion, marked regression of advanced
maxillary sinus cancer with orbital invasion through the
combination of chemotherapy and immunotherapy was observed in this
one-year follow-up case. Further investigation is still needed on
the effect of the combination of chemotherapy and immunotherapy on
advanced maxillary sinus cancer.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used during the present study are
available from the corresponding author on reasonable request.
Authors' contributions
CSL performed the surgical procedures. CSL and YHK
conceived the study, wrote the manuscript and confirm the
authenticity of all the raw data. Both authors read and approved
the manuscript and agree to be accountable for all aspects of the
research in ensuring that the accuracy or integrity of any part of
the work are appropriately investigated and resolved.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Won HS, Chun SH, Kim BS, Chung SR, Yoo
IeR, Jung CK, Kim YS, Sun DI, Kim MS and Kang JH: Treatment outcome
of maxillary sinus cancer. Rare Tumours. 1(e36)2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Praveena NM and Maragathavalli G:
Carcinoma of the maxillary antrum: A case report. Cureus.
10(e2614)2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Dulguerov P, Jacobsen MS, Allal AS,
Lehmann W and Calcaterra T: Nasal and paranasal sinus carcinoma:
Are we making progress? A series of 220 patients and a systematic
review. Cancer. 92:3012–3029. 2001.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Dooley L and Shah J: Management of the
neck in maxillary sinus carcinomas. Curr Opin Otolaryngol Head Neck
Surg. 23:107–114. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ashraf M, Biswas J, Dam A, Bhowmick A, Jha
Sing V and Nayak S: Results of treatment of squamous cell carcinoma
of maxillary sinus: A 26-year experience. World J Oncol. 1:28–34.
2010.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Noronha V, Patil VM, Joshi A, Krishna MV,
Dhumal S, Juvekar S, Pai P, Chatturvedi P, Chaukar DA, Agarwal JP,
et al: Induction chemotherapy in technically unresectable locally
advanced carcinoma of maxillary sinus. Chemother Res Pract.
2014(487872)2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Xiang JJ, Uy NF, Minja FJ, Verter EE and
Burtness BA: Hyperprogression after one dose of nivolumab in
sinonasal cancer: A case report. Laryngoscope. 130:907–910.
2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yazici G, Gullu I, Cengiz M, Elmali A,
Yilmaz MT, Aksoy S, Yuce Sari S and Ozyigit G: The synergistic
effect of immune checkpoint blockade and radiotherapy in
recurrent/metastatic sinonasal cancer. Cureus.
10(e3519)2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Guram K, Nunez M, Einck J, Mell LK, Cohen
E, Sanders PD, Miyauchi S, Weihe E, Kurzrock R, Boles S and Sharabi
AB: Radiation therapy combined with checkpoint blockade
immunotherapy for metastatic undifferentiated pleomorphic sarcoma
of the maxillary sinus with a complete response. Front Oncol.
8(435)2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Rose TL, Harrison MR, Deal AM, Ramalingam
S, Whang YE, Brower B, Dunn M, Osterman CK, Heiling HM, Bjurlin MA,
et al: Phase II study of gemcitabine and split-dose cisplatin plus
pembrolizumab as neoadjuvant therapy before radical cystectomy in
patients with muscle-invasive bladder cancer. J Clin Oncol.
39:3140–3148. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Gandhi L, Rodríguez-Abreu D, Gadgeel S,
Esteban E, Felip E, De Angelis F, Domine M, Clingan P, Hochmair MJ,
Powell SF, et al: Pembrolizumab plus chemotherapy in metastatic
non-small-cell lung cancer. N Engl J Med. 378:2078–2092.
2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Emens LA and Middleton G: The interplay of
immunotherapy and chemotherapy: Harnessing potential synergies.
Cancer Immunol Res. 3:436–443. 2015.PubMed/NCBI View Article : Google Scholar
|