|
1
|
Skírnisdóttir I, Garmo H, Wilander E and
Holmberg L: Borderline ovarian tumors in Sweden 1960-2005: Trends
in incidence and age at diagnosis compared to ovarian cancer. Int J
Cancer. 123:1897–1901. 2008.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Abascal-Saiz A, Sotillo-Mallo L, de
Santiago J and Zapardiel I: Management of borderline ovarian
tumours: A comprehensive review of the literature.
Ecancermedicalscience. 17(403)2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Niu L, Tian H, Xu Y, Cao J, Zhang X, Zhang
J, Hou J, Lv W, Wang J, Xin L, et al: Recurrence characteristics
and clinicopathological results of borderline ovarian tumors. BMC
Womens Health. 21(134)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
National Comprehensive Cancer Network.
Ovarian cancer. (Version 1.2022) http//www.nccn.org/professionals/physician_gls/pdf/ovarian.pdf.
Accessed January 29, 2022.
|
|
5
|
Cianci S, Perrone E, Rossitto C, Fanfani
F, Tropea A, Biondi A, Scambia G and Gueli Alletti S:
Percutaneous-assisted vs mini-laparoscopic hysterectomy: Comparison
of ultra-minimally invasive approaches. Updates Surg. 73:2347–2354.
2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Song T, Kim MK, Jung YW, Yun BS, Seong SJ,
Choi CH, Kim TJ, Lee JW, Bae DS and Kim BG: Minimally invasive
compared with open surgery in patients with borderline ovarian
tumors. Gynecol Oncol. 145:508–512. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Perrone E, Rossitto C, Fanfani F, Cianci
S, Fagotti A, Uccella S, Vizzielli G, Vascone C, Restaino S, Fedele
C, et al: Percutaneous-assisted versus laparoscopic hysterectomy: A
prospective comparison. Gynecol Obstet Invest. 85:318–326.
2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cianci S, Rosati A, Rumolo V, Gueli
Alletti S, Gallotta V, Turco LC, Corrado G, Vizzielli G, Fagotti A,
Fanfani F, et al: Robotic Single-Port platform in general,
urologic, and gynecologic surgeries: A systematic review of the
literature and Meta-analysis. World J Surg. 43:2401–2419.
2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kumari S, Kumar S, Bhatla N, Mathur S,
Thulkar S and Kumar L: Oncologic and reproductive outcomes of
borderline ovarian tumors in Indian population. Gynecol Oncol Rep.
36(100756)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Johansen G, Dahm-Kähler P, Staf C, Flöter
Rådestad A and Rodriguez-Wallberg KA: Reproductive and obstetrical
outcomes with the overall survival of fertile-age women treated
with fertility-sparing surgery for borderline ovarian tumors in
Sweden: A prospective nationwide population-based study. Fertil
Steril. 115:157–163. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Uzan C, Nikpayam M, Ribassin-Majed L, Gouy
S, Bendifallah S, Cortez A, Rey A, Duvillard P, Darai E and Morice
P: Influence of histological subtypes on the risk of an invasive
recurrence in a large series of stage I borderline ovarian tumor
including 191 conservative treatments. Ann Oncol. 25:1312–1319.
2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Giampaolino P, Della Corte L, Foreste V,
Vitale SG, Chiofalo B, Cianci S, Zullo F and Bifulco G: Unraveling
a difficult diagnosis: The tricks for early recognition of ovarian
cancer. Minerva Med. 110:279–291. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Qi Y, Wang M, Yang Y, Zeng Z and Zhou Y:
Analysis of factors influencing relapse and pregnancy in patients
with borderline ovarian tumors. J Cancer. 12:5275–5285.
2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Fang C, Zhao L, Chen X, Yu A, Xia L and
Zhang P: The impact of clinicopathologic and surgical factors on
relapse and pregnancy in young patients (≤40 years old) with
borderline ovarian tumors. BMC Cancer. 18(1147)2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chen RF, Li J, Zhu TT, Yu HL and Lu X:
Fertility-sparing surgery for young patients with borderline
ovarian tumors (BOTs): Single institution experience. J Ovarian
Res. 9(16)2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sozen H, Vatansever D, Topuz S, Iyibozkurt
C, Kandemir H, Yalçin I, Onder S, Yavuz E and Salihoglu Y:
Clinicopathological analysis of borderline ovarian tumours and risk
factors related to recurrence: Experience of single institution. J
Obstet Gynaecol. 39:253–258. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ayhan A, Guvendag Guven ES, Guven S and
Kucukali T: Recurrence and prognostic factors in borderline ovarian
tumors. Gynecol Oncol. 98:439–445. 2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
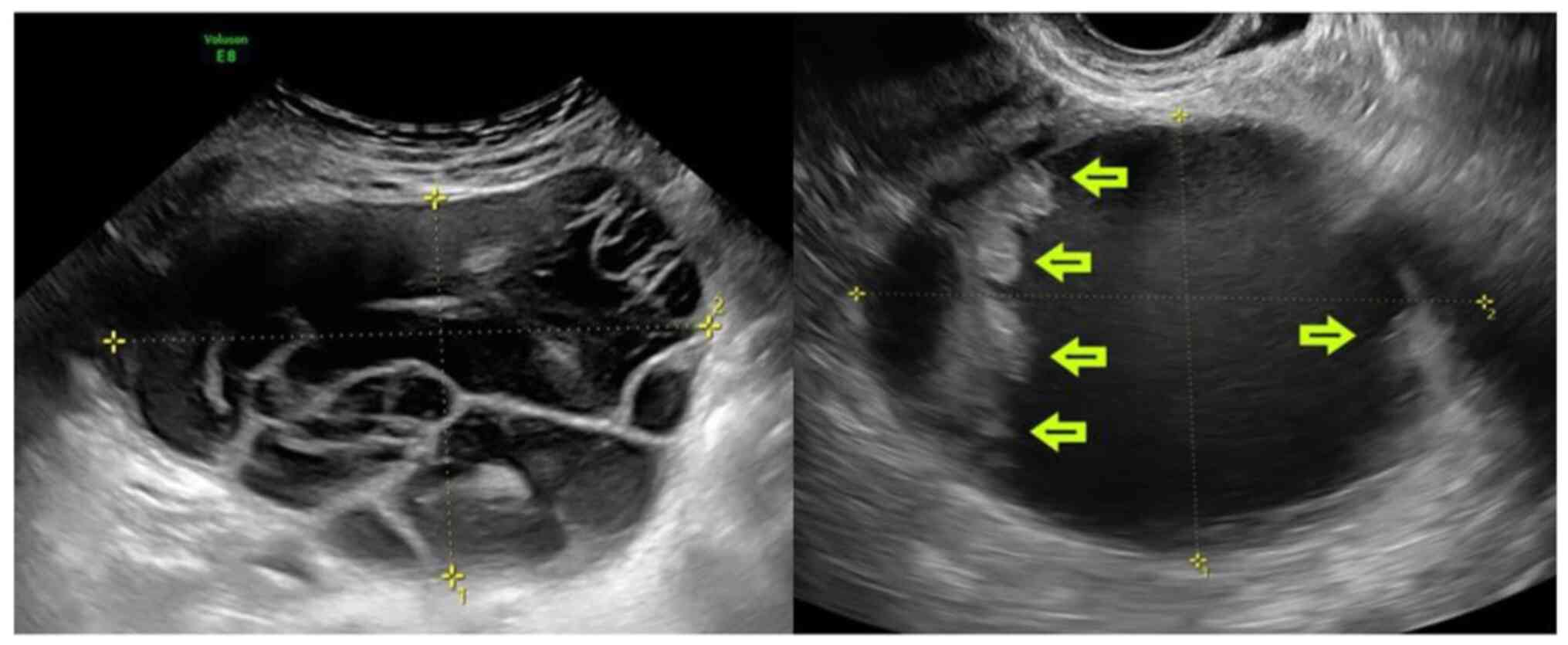
Timmerman D, Van Calster B, Testa A,
Savelli L, Fischerova D, Froyman W, Wynants L, Van Holsbeke C,
Epstein E, Franchi D, et al: Predicting the risk of malignancy in
adnexal masses based on the Simple Rules from the International
Ovarian Tumor Analysis group. Am J Obstet Gynecol. 214:424–437.
2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Watanabe E, Tanaka K, Takeda N, Takayasu
H, Yokota K and Watanabe M: Surgical technique to prevent spillage
of cyst fluid during operation for cystic ovarian tumors. Pediatr
Surg Int. 29:645–649. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Gueli Alletti S, Rossitto C, Perrone E,
Cianci S, De Blasis I, Fagotti A and Scambia G: Needleoscopic
conservative staging of borderline ovarian tumor. J Minim Invasive
Gynecol. 24:529–530. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kobayashi H, Sumimoto K, Kitanaka T,
Yamada Y, Sado T, Sakata M, Yoshida S, Kawaguchi R, Kanayama S,
Shigetomi H, et al: Ovarian endometrioma-risks factors of ovarian
cancer development. Eur J Obstet Gynecol Reprod Biol. 138:187–193.
2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Romagnolo C, Gadducci A, Sartori E, Zola P
and Maggino T: Management of borderline ovarian tumors: Results of
an Italian multicenter study. Gynecol Oncol. 101:255–260.
2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Karataşlı V, Can B, Çakır İ, Erkılınç S,
Karabulut A, Ayaz D, Kuru O, Gökçü M and Sancı M: Effect of tumor
size on the accuracy of frozen section in the evaluation of
mucinous borderline ovarian tumors. J Gynecol Obstet Hum Reprod.
49(101765)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Timmerman D, Testa AC, Bourne T, Ameye L,
Jurkovic D, Van Holsbeke C, Paladini D, Van Calster B, Vergote I,
Van Huffel S and Valentin L: Simple ultrasound-based rules for the
diagnosis of ovarian cancer. Ultrasound Obstet Gynecol. 31:681–690.
2008.PubMed/NCBI View
Article : Google Scholar
|
|
25
|
Franchi D, Boveri S, Fruscio R, Fischerova
D, Guerriero S, Moruzzi MC, Colombo N, Timmerman D, Valentin L and
Testa AC: Imaging in gynecological disease (8): Ultrasound
characteristics of recurrent borderline ovarian tumors. Ultrasound
Obstet Gynecol. 41:452–458. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zanetta G, Rota S, Lissoni A, Meni A,
Brancatelli G and Buda A: Ultrasound, physical examination, and CA
125 measurement for the detection of recurrence after conservative
surgery for early borderline ovarian tumors. Gynecol Oncol.
81:63–66. 2001.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Gizzo S, Berretta R, Di Gangi S, Guido M,
Zanni GC, Franceschetti I, Quaranta M, Plebani M, Nardelli GB and
Patrelli TS: Borderline ovarian tumors and diagnostic dilemma of
intraoperative diagnosis: Could preoperative He4 assay and ROMA
score assessment increase the frozen section accuracy? A
multicenter case-control study. Biomed Res Int.
2014(803598)2014.PubMed/NCBI View Article : Google Scholar
|