Introduction
Periampullary adenocarcinoma encompasses neoplasms
arising from the epithelium of four distinct anatomic sites:
ampullary adenocarcinoma, distal cholangiocarcinoma, duodenal
adenocarcinoma, and pancreatic head adenocarcinoma (1). Pancreatic cancer is the most common
periampullary adenocarcinoma and the fourth leading cause of cancer
deaths in the United States (2).
By the year 2030, it is estimated that 70% of all cancer cases and
85% of all cancer-related deaths are likely to occur in patients
older than 65 years (3). Moreover,
the older population in the European Union (EU) is rapidly growing.
EU total population on January 1st 2018 was estimated at 512.4
million, 19.7% of which constitute people aged 65 or over.
Interestingly, the subgroup of the very old (aged 85 years or more)
is growing at a faster pace than any other age group. Between 2018
and 2050, the oldest population in the EU is estimated to more than
double, up 130.3%. Across the EU member states, the highest share
of persons aged 65 or older in the total population in 2018 was
observed in Italy (22.6%) and Greece (21.8%), while the lowest
share was observed in Ireland (13.8%) (4,5). It
is well known that the incidence of solid tumor malignancy rises
with age, becoming progressively much more common in the older
brackets of the population.
As the percentage of patients in the older brackets
increases, more patients seek surgical care as a chance to cure.
Denying patients resection based on age alone seems unsustainable.
In fact, designing a patient centered personalized treatment plan
will require a better understanding of how these elderly patients
perform after major pancreatic resections. Surgical resection and
most specifically pancreaticoduodenectomy (PD) or Whipple procedure
remains the standard of treatment for periampullary adenocarcinoma
(6). Despite decades of
improvement in surgical technique and postoperative care, this
procedure still carries a high rate of post-operative morbidity and
mortality (7,8). Systematic reviews about PD in elderly
patients (older than 65 years) show controversial results regarding
post-operative morbidity and mortality (9,10).
Nonetheless, studies on patients older than 80 undergoing a PD
report either a similar profile of morbidity and mortality or a
slight increase, albeit non prohibitive (11,12).
In this context, in our tertiary referral center, we have observed
a trend in performing PD more frequently on octogenarians during
the last decade. To understand our unique population's
characteristics, we opted to study the short-term outcomes and
long-term survival after a PD for periampullary tumors in patients
older than 80 years in our center and compare these to their
younger counterparts.
Materials and methods
We retrospectively reviewed all consecutive patients
who underwent a Whipple procedure from January 2010 until December
2019 at the largest tertiary, academic hospital in Greece (Attikon
University Hospital). All the procedures were coordinated by
Professor Vasileios Smyrniotis, while all involved surgeons were
equally exposed to pancreatic surgery. Over the years, all
periampullary cancer patients referred to our facility are
evaluated by a multidisciplinary team; treatment is then
personalized according to stage and pathological features of the
tumor as well as to patient's comorbidities. Typically, patients
with resectable disease undergo surgical procedure; patients who
are deemed borderline resectable receive neoadjuvant chemotherapy
and are reevaluated for possible resection. Concerning older
patients, the performance status score was useful; patients with a
score 3 or 4 in ECOG scale may be discouraged of surgical treatment
(13). Other than that, there were
no specific selection or exclusion criteria.
Complete data from all patients were obtained from
hospital charts and included patient demographics, comorbidities,
medical history, tumor type, stage and histopathological features,
perioperative events and complications, and status of disease at
follow-up. Pathological staging of malignant tumors was performed
according to the Tenth Edition of the Cancer Staging Manual edited
by the American Joint Committee on Cancer (AJCC). Thirty-day
mortality was defined as death within 30 days from operation.
Overall survival was determined from date of operation until date
of death from any cause.
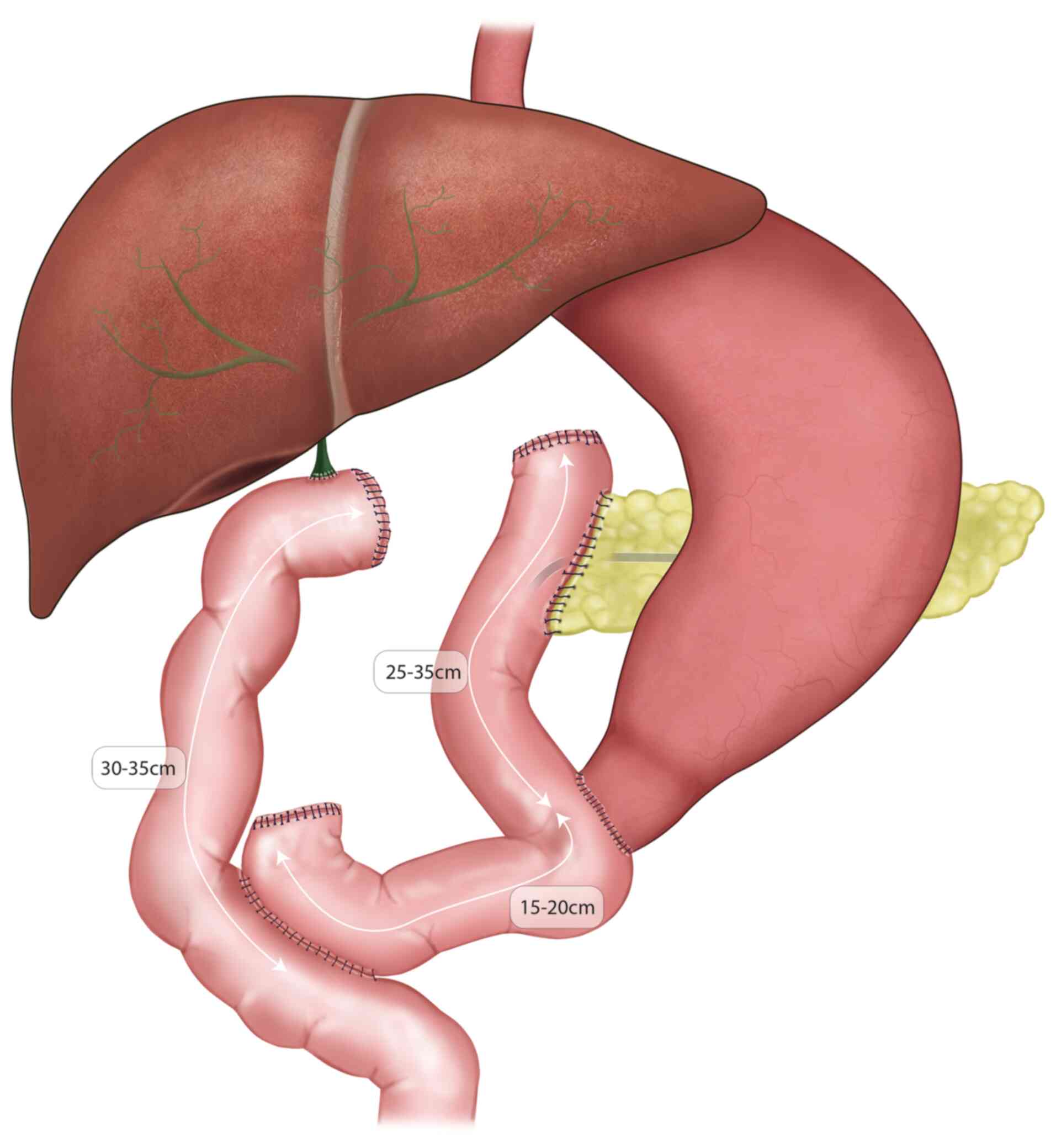
Patients undergo epidural and general anesthesia
before PD in our institution, unless it is contraindicated. Most
patients were operated on with Pylorus Preserving PD and the
restoration of the visceral continuity was achieved over a
Roux-en-Y configuration: the short limb was used for
pancreatico-jejunostomy and gastroenterostomy and the long limb for
the hepatico-jejunostomy (Fig. 1).
While the rest of the patients were operated on with the classical
technique and the restoration was achieved through a single jejunal
loop.
The patients identified were categorized into two
groups, according to age at the time of surgery: Group Y
(<80-year-old) and Group O (≥80-year-old). Variables analyzed in
the two groups included demographics, intra- and post-operative
outcomes. Sample characteristics were summarized through absolute
(N) and relative (%) frequencies (categorical variables) or median
and interquartile range-IQR (continuous variables). Summary
statistics were given by age group (<80 or 80+ years) and
overall. P-values in the respective tables were based on Fisher's
exact test for categorical variables and non-parametric
Mann-Whitney U-test for continuous variables. Analysis of the
overall mortality was based on survival methods. More specifically,
survival probabilities over time by group were estimated and
graphically presented using the Kaplan-Meier method whereas for the
respective between groups comparison the log-rank test was used.
All statistics performed were two-sided and declared at the 5%
significance level. The key study endpoints were length of stay,
overall morbidity, perioperative mortality and median survival.
There were no experiments performed for the purposes of this study.
All methods were carried out in accordance with relevant guidelines
and regulations. The study received ethical approval and was
conducted with permission of the Institutional Review Board and
Ethics Committee of Attikon University Hospital
(47929/16.12.16).
Results
Between 2010 and 2019, 218 patients underwent a
Whipple procedure at the department of surgery at Attikon
University Hospital. Of these, 20 (9.1%) were 80 years or older.
The study population included 117 men and 101 women with a median
age of 67 years (range 25-88) at the time of surgery. The median
age of the Y group was 66 (range 25-79) and of the O group was 81.5
(range 80-88). Table I describes
the demographics and comorbidities of the two study groups as well
as whether they received neoadjuvant therapy or not. There were no
differences in terms of gender composition (male 55.6 vs. 35.0%,
P=0.100) or Body Mass Index (BMI) status (P=0.478). American
Society of Anesthesiology (ASA) scores were worse in the
octogenarian group (ASA 3-4: 31.3 vs. 65%, P=0.018), as were the
Charlson Comorbidity Index (CCI) scores (CCI >6: 21.7 vs. 90%,
P<0.05). However, there were no major differences in the
incidence of patients' comorbidities, except for hypertension (49.5
vs. 80%, P=0.007).
 | Table ISample characteristics by age group (Y
group age, 25-79; O group age, 80-89). |
Table I
Sample characteristics by age group (Y
group age, 25-79; O group age, 80-89).
| Variable | Y group (n=198) | O group (n=20) | P-value |
|---|
| Male sex, n (%) | 110 (55.6) | 7 (35.0) | 0.100 |
| Smoking status, n
(%) | | | 0.068 |
|
Smoker | 82 (41.4) | 5 (25.0) | |
|
Non-smoker | 79 (39.9) | 13 (65.0) | |
|
Ex-smoker | 35 (17.7) | 1 (5.0) | |
|
N/A | 2 (1.0) | 1 (5.0) | |
| Hypertension, n
(%) | 98 (49.5) | 16 (80.0) | 0.007 |
| Diabetes mellitus, n
(%) | 47 (23.7) | 9 (45.0) | 0.077 |
| Coronary artery
disease, n (%) | 30 (15.2) | 6 (30.0) | 0.100 |
| Dyslipidemia, n
(%) | 54 (27.3) | 9 (45.0) | 0.110 |
| Personal history of
solid malignancy, n (%) | 20 (10.1) | 1 (5.0) | 0.590 |
| Arrythmias, n
(%) | 14 (7.1) | 2 (10.0) | 0.630 |
| Pulmonary morbidity,
n (%) | 9 (4.5) | 1 (5.0) | 0.990 |
| Hypothyroidism, n
(%) | 25 (12.6) | 2 (10.0) | 0.990 |
| Hyperthyroidism, n
(%) | 3 (1.5) | 0 (0.0) | 0.990 |
| Previous abdominal
surgery, n (%) | 96 (48.5) | 12 (60.0) | 0.337 |
| ASA score, n (%) | | | 0.018 |
|
I | 20 (10.1) | 0 (0.0) | |
|
II | 110 (55.6) | 6 (30.0) | |
|
III | 60 (30.3) | 13 (65.0) | |
|
IV | 2 (1.0) | 0 (0.0) | |
|
N/A | 6 (3.0) | 1 (5.0) | |
| Charlson Comorbidity
Index (CCI), n (%) | | | <0.05 |
|
0 | 1 (0.5) | 0 (0) | |
|
1 | 1 (0.5) | 0 (0) | |
|
2 | 13 (6.6) | 0 (0) | |
|
3 | 32 (16.2) | 0 (0) | |
|
4 | 49 (24.7) | 1(5) | |
|
5 | 59 (29.8) | 1(5) | |
|
6 | 34 (17.2) | 7(35) | |
|
7 | 7 (3.5) | 7(35) | |
|
8 | 2(1) | 4(20) | |
| Neoadjuvant
therapy | 4 (2.0) | 0 (0.0) | |
| BMI, kg/m2
(IQR) | 25.39 | 25.15 | 0.478 |
| | (23.38, 28.89) | (21.83, 27.46) | |
Intra-operative outcomes
Table II describes
intra-operative outcomes and hospitalization days for the two study
groups. No differences were noted in terms of operative time, rate
of portal vein resection and reconstruction, type of anesthesia or
analgesia and number of units of blood transfused.
 | Table IIIntra-operative outcomes by age group
(Y group age, 25-79; O group age, 80-89). |
Table II
Intra-operative outcomes by age group
(Y group age, 25-79; O group age, 80-89).
| Variable | Y group
(n=198) | O group (n=20) | P-value |
|---|
| Operation duration,
min (IQR) | 228 (185, 325) | 255 (180.0,
342.5) | 0.745 |
| RBC, n (%) | 0 (0, 2) | 1 (1, 2) | 0.084 |
| FFP, n (%) | 0 (0, 2) | 0 (0, 0) | 0.406 |
| Epidural anesthesia
and analgesia, n (%) | 132 (66.7) | 12 (60.0) | 0.799 |
| Vein
reconstruction, n (%) | 2 (1.0) | 0 (0.0) | >0.999 |
Pathology
Most neoplasms were adenocarcinoma of the pancreas
in both groups (61.1 vs. 65%) followed by ampullary adenocarcinoma
(12.4%), distal cholangiocarcinoma (10.1%) and Intraductal
Papillary Mucinous Neoplasm (IPMN) (6%). Most cancers were stage II
and III in group Y, while stage I and II in group O (Table III).
 | Table IIIPathology findings, by age group (Y
group age, 25-79; O group age, 80-89). |
Table III
Pathology findings, by age group (Y
group age, 25-79; O group age, 80-89).
| Variable | Y group
(n=198) | O group (n=20) | P-value |
|---|
| Histological type
(grouped), n (%) | | | 0.452 |
|
IPMN | 12 (6.1) | 1 (5.0) | |
|
Pancreatic
NET | 7 (3.5) | 0 (0.0) | |
|
Adenocarcinoma | | | |
|
Pancreas | 121 (61.1) | 13(65) | |
|
Ampullary | 25 (12.6) | 2(10) | |
|
Distal bile
duct | 21 (10.6) | 1(5) | |
|
Duodenal | 4(2) | 1(5) | |
|
Other | 8 (4.1) | 2(10) | |
| Stage, n (%) | | | 0.008 |
|
I/IA | 9 (4.5) | 1 (5.0) | |
|
IB | 25 (12.6) | 9 (45.0) | |
|
II/IIA | 30 (15.2) | 1 (5.0) | |
|
IIB | 67 (33.8) | 4 (20.0) | |
|
III/IIIA/IIIB | 49 (24.7) | 2 (10.0) | |
|
Unclassified | 18 (9.1) | 3 (15.0) | |
Post-operative outcomes
Overall morbidity (Clavien-Dindo≥3) was equally
distributed between the two groups (26.8 vs. 25%, P=0.895). No
differences were noted in terms of pancreatic fistula, hemorrhage,
delayed gastric emptying (DGE) or reoperation rates. Length of
hospitalization was not significantly different between younger and
older patients (14 days vs. 16 days, P=0.307), neither was the
30-day mortality [12 patients (6.1%) vs. 1 patient (5%),
P>0.99]. Follow-up was available for 214 patients (98.2% of our
population). Mean follow-up time was 30.6 months for Group Y and
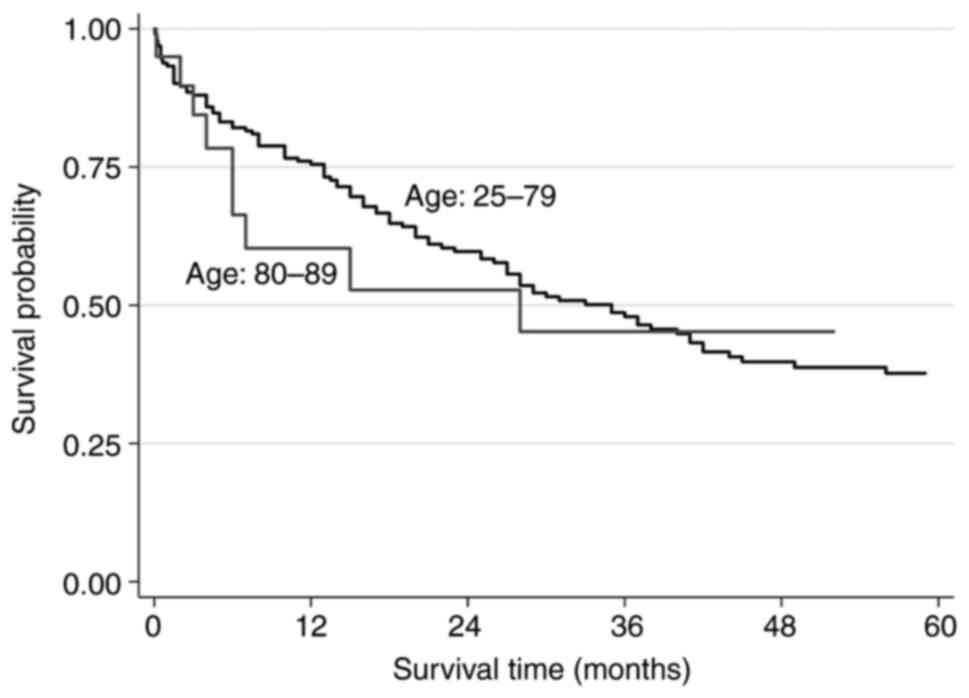
16.3 months for Group O. The 1-, 2- and 5-year survival rate was
75.5, 59.7 and 37.7% for Group Y and 60.3, 52.8 and 45.2% for Group
O respectively (Fig. 2). Median
overall survival (OS) was 35 months for patients younger than 80
years and 28 months for the octogenarians (log-rank test P=0.577)
(Table IV).
 | Table IVPost-operative outcomes, by age group
(Y group age, 25-79; O group age, 80-89). |
Table IV
Post-operative outcomes, by age group
(Y group age, 25-79; O group age, 80-89).
| Variable | Y group
(n=198) | O group (n=20) | P-value |
|---|
| Pancreatic fistula,
n (%) | | | 0.399 |
|
No
fistula | 148 (74.7) | 16 (80.0) | |
|
A | 20 (10.1) | 1 (5.0) | |
|
B | 15 (7.6) | 3 (15.0) | |
|
C | 15 (7.6) | 0 (0.0) | |
| Post-operative
hemorrhage, n (%) | 22 (11.1) | 1 (5.0) | 0.703 |
| Delayed gastric
emptying, n (%) | 44 (22.2) | 5 (25.0) | 0.781 |
| Re-exploration,
(%) | 22 (11.1) | 1 (5.0) | 0.703 |
| Morbidity, n
(%) | | | |
|
Clavien-Dindo
Grade I | 26 (13.1) | 4 (20.0) | |
|
Clavien-Dindo
Grade II | 33 (16.7) | 4 (20.0) | |
|
Clavien-Dindo
Grade IIIa | 18 (9.1) | 2 (10.0) | |
|
Clavien-Dindo
Grade IIIb | 4 (2.0) | 0 (0.0) | |
|
Clavien-Dindo
Grade Iva | 13 (6.6) | 2 (10.0) | |
|
Clavien-Dindo
Grade IVb | 0 (0.0) | 0 (0.0) | |
|
Clavien-Dindo
Grade V | 18 (9.1) | 1 (5.0) | |
| Post-operative need
for ICU care, n (%) | 25 (12.6) | 3 (15.0) | 0.728 |
| 30-day mortality, n
(%) | 12 (6.1) | 1 (5.0) | 0.990 |
| Length of stay,
days (IQR) | 14 (10, 22) | 16 (10.5,
23.0) | 0.307 |
| Median survival
time, months (IQR) | 35 (26, 42) | 28 (6,
non-estimable) | 0.577 |
Discussion
PD is a complex procedure, associated with high
rates of morbidity. However, it remains the standard treatment for
patients with periampullary neoplasms and especially for head
pancreatic adenocarcinoma (7).
Advanced age seems to be a risk factor regarding pancreatic cancer
(2).
As the segment of the Greek population over age 80
has grown in the last several years, similar to other EU member
states, in our tertiary referral center we have seen the portion of
octogenarians presenting with a periampullary malignancy and
receiving a PD increase as well. This study shows that patients
over the age of 80 can safely undergo a PD. These patients can
expect a profile of perioperative morbidity and mortality that does
not differ from their younger counterparts'. In fact, we have found
that octogenarians cared for in our center can expect a fair
oncologic outcome with an overall median survival higher than two
years after successfully undergoing their operation, without the
implementation of specific steps to reduce morbidity and mortality.
Α bigger portion of the octogenarians were operated on, in a more
favorable stage (45%-Stage IB) than the younger patients. That may
be explained because by the slower progress of cancer in elderly
and the frequent imaging studies of older patients due to other
comorbidities.
Previous studies have analyzed the outcomes of PD in
patients older than 80 years. Among them, studies have reported
that octogenarians are more prone to morbidity, and when serious
morbidity occurs, they are more prone to mortality (14-22).
Conclusively, octogenarians can safely undergo a complex
gastrointestinal operation, albeit being more fragile, they seem to
tolerate complications with less resilience than their younger
counterparts. In our study, even if octogenarians had more
postoperative complications than younger patients, there was no
significant difference in 30-day mortality and OS. This is probably
due to the small sample and it is not representative.
Regardless, authors appear to agree that PD is a
safe option for elderly patients as long as there is careful
selection depending on their preoperative workup (14-21).
In these series, age appears to be less important than physiologic
ability. Adding to that, some authors have proposed specific
criteria for elderly patients which quantifies this physiologic
ability, by assessment of cardiac and pulmonary function,
nutritional status, daily activity status as well as psychological
and independence status (21).
Although specific scores were not used regularly during the past
time period, the multidisciplinary team after the results of this
study selects patients to receive surgical treatment, with careful
consideration of Frailty index, Performance status score and CCI.
Frailty index could be a reliable tool to assess the physiologic
ability of older patients.
Performing a pancreatectomy in octogenarians with
pancreatic cancer has been challenged recently: a 2015
multi-institutional study from Japan which compared a group of
octogenarians who were operated for pancreatic malignancy with a
group of elderly patients who were treated only with chemotherapy
and possibly radiation showed no superiority of surgery in
comparison to chemo and radiotherapy, although the patients who
completed both resection and adjuvant chemotherapy had the best
overall survival (23). The same
group has also published in 2016 their experience in pancreatic
resection comparing their octogenarians vs. their younger patients
and found that the prognosis of octogenarians was poorer than that
of younger patients for both resectable and borderline resectable
tumors; importantly, there were few long-term survivors in their
elderly group, especially among those with borderline resectable
pancreatic cancer (24). These
results clearly showcase the importance of careful patient
selection especially in the extreme of age, and it also underscores
the importance of referring these patients to a tertiary level
center of excellence.
This study has several potential limitations. The
main limitation is the retrospective nature of our review. We
employed methodological strategies to minimize the difficulties in
accurately gathering the retrospective morbidity data. First,
complications such as pneumonia, urinary tract infection or wound
infection (all regarded as Clavien-Dindo classifications <3)
that could have been under documented in our patients' medical
records charting system over the years were excluded. We were also
not able to record some preoperative parameters such as biliary
stenting, bilirubin levels, presence of cholangitis, hemoglobin
levels, serum albumin levels. On the other hand, overall morbidity
was accurately captured, for our discharge summary specifies
whether the post-operative course of each patient was uneventful or
not. Secondly, since the date of the operation and date of
discharge from the hospital are always delineated in the electronic
medical record, the hospitalization days were used as an additional
quality measure of assessing for under reported postoperative
morbidity. Our results show similar length of stay for elderly
patients (14 days vs. 16 days), which supports the fact that there
was no significant difference in patients' morbidity. We showed
herein that our octogenarians had a worse overall ASA score than
our younger patients. Patients that either received adjuvant
chemotherapy or were not operated or denied surgical treatment,
even being fully informed, were not recorded. It would be
interesting to compare the results of this study with the
aforementioned group of patients. Lastly it is worth to mention
that we have added a small number of patients in both our groups
who had IPMN, a premalignant entity, as well as some adenomas which
tips the scales to a better median survival for both groups. The
grade of IPMN was not recorded in our study.
It is important to highlight that the population
will continue to grow older, and as such more patients in the
extreme of age will present with periampullary pathology and
malignancy. We have shown in our study that undergoing a PD is safe
and renders a significant survival benefit in octogenarians.
Patients should not be denied a curative surgical option for
periampullary disease, solely based on advanced age. Future
studies, using larger and prospective databases, should include
preoperative parameters and specific selection criteria, as careful
and detailed preoperative assessment is deemed crucial to choose PD
as a safe therapeutic option in octogenarians.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SP, TS, PK and VN acquired the data and drafted the
first edition of manuscript. NP was responsible for the statistical
analysis and, together with PV, PM and IM, interpreted the data and
critically revised the manuscript. NA, VS and IH conceived and
designed the study, revised the draft and formed the final edition
of the manuscript. SP, VN and TS confirm the authenticity of all
the raw data. All authors approve the final edition of the
manuscript.
Ethics approval and consent to
participate
This retrospective study involving human
participants was in accordance with the ethical standards of the
institutional and national research committee and with the 1964
Helsinki Declaration and its later amendments or comparable ethical
standards. Ethical approval was waived by the local Ethics
Committee of Attikon University Hospital in view of the
retrospective nature of the study and all the procedures being
performed were part of the routine care. The study protocol
including patients' consent was approved by Institutional Review
Board and Ethics Committee of Attikon University Hospital (approval
no. 47929/16.12.16).
Patient consent for publication
Written informed consent regarding publishing data
was obtained from all individual participants included in the
study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hester CA, Dogeas E, Augustine MM, Mansour
JC, Polanco PM, Porembka MR, Wang SC, Zeh HJ and Yopp A: Incidence
and comparative outcomes of periampullary cancer: A
population-based analysis demonstrating improved outcomes and
increased use of adjuvant therapy from 2004 to 2012. J Surg Oncol.
119:303–317. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ilic M and Ilic I: Epidemiology of
pancreatic cancer. World J Gastroenterol. 22:9694–9705.
2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Higuera O: Management of pancreatic cancer
in the elderly. World J Gastroenterol. 22:764–775. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Eurostat: Ageing Europe-statistics on
population developments-Statistics Explained. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Ageing_Europe_-_statistics_on_population_developments.
Accessed Apr 4, 2020.
|
|
5
|
Eurostat: Population structure and
ageing-Statistics Explained. https://ec.europa.eu/eurostat/statistics-explained/index.php/Population_structure_and_ageing.
Accessed Apr 4, 2020.
|
|
6
|
Wiltberger G, Krenzien F, Atanasov G, Hau
HM, Schmelzle M, Bartels M and Benzing C: Pancreaticoduodenectomy
for periampullary cancer: Does the tumour entity influence
perioperative morbidity and long-term outcome? Acta Chir. Belg.
118:341–347. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Karim SAM, Abdulla KS, Abdulkarim QH and
Rahim FH: The outcomes and complications of pancreaticoduodenectomy
(Whipple procedure): Cross sectional study. Int J Surg. 52:383–387.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cameron JL and He J: Two thousand
consecutive pancreaticoduodenectomies. J Am Coll Surg. 220:530–536.
2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Pędziwiatr M, Małczakab P, Mizera M,
Witowski J, Torbicz G, Major P, Pisarska M, Wysocki M, Jankowski M,
Rubinkiewicz M, et al: Pancreatoduodenectomy for pancreatic head
tumors in the elderly-systematic review and meta-analysis. Surg
Oncol. 27:346–364. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Miyazaki Y, Kokudo T, Amikura K, Kageyama
Y, Takahashi A, Ohkohchi N and Sakamoto H: Age does not affect
complications and overall survival rate after
pancreaticoduodenectomy: Single-center experience and systematic
review of literature. Biosci Trends. 10:300–306. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Casadei R, Ricci C, Lazzarini E,
Taffurelli G, D'Ambra M, Mastroroberto M, Morselli-Labate AM and
Minni F: Pancreatic resection in patients 80 years or older: A
meta-analysis and systematic review. Pancreas. 43:1208–1218.
2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kim SY, Weinberg L, Christophi C and
Nikfarjam M: The outcomes of pancreaticoduodenectomy in patients
aged 80 or older: A systematic review and meta-analysis. HPB
(Oxford). 19:475–482. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
West H and Jin JO: Performance status in
patients with cancer. JAMA Oncol. 1(998)2015.
|
|
14
|
Langan RC, Huang CC, Mao WR, Harris K,
Chapman W, Fehring C, Oza K, Jackson PG, Jha R, Haddad N, et al:
Pancreaticoduodenectomy hospital resource utilization in
octogenarians. Am J Surg. 211:70–75. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Liang DH, Shirkey BA, Rosenberg WR and
Martinez S: Clinical outcomes of pancreaticoduodenectomy in
octogenarians: A surgeon's experience from 2007 to 2015. J
Gastrointest Oncol. 7:540–546. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sugimachi K, Iguchi T, Mano Y, Nishijima
T, Nakanoko T, Uehara H, Sugiyama M, Ohta M, Ikebe M, Morita M and
Toh Y: The impact of immunonutritional and physical status on
surgical outcome after pancreaticoduodenectomy in elderly patients.
Anticancer Res. 39:6347–6353. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Oguro S, Shimada K, Kishi Y, Nara S, Esaki
M and Kosuge T: Perioperative and long-term outcomes after
pancreaticoduodenectomy in elderly patients 80 years of age and
older. Langenbecks Arch Surg. 398:531–538. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Langan RC, Zheng C, Harris K, Verstraete
R, Al-Refaie WB and Johnson LB: Hospital-level resource use by the
oldest-old for pancreaticoduodenectomy at high-volume hospitals.
Surgery. 158:366–372. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Melis M, Marcon F, Masi A, Pinna A, Sarpel
U, Miller G, Moore H, Cohen S, Berman R, Pachter HL and Newman E:
The safety of a pancreaticoduodenectomy in patients older than 80
years: Risk vs. benefits. HPB (Oxford). 14:583–588. 2012.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lee DY, Schwartz JA, Wexelman B, Kirchoff
D, Yang KC and Attiyeh F: Outcomes of pancreaticoduodenectomy for
pancreatic malignancy in octogenarians: An American college of
surgeons national surgical quality improvement program analysis. Am
J Surg. 207:540–548. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Shiozawa S, Usui T, Kuhara K, Tsuchiya A,
Miyauchi T, Kono T, Shimojima Y, Asaka S, Yamaguchi K, Yokomizo H,
et al: Eligibility criteria specific to pancreaticoduodenectomy for
octogenarians: Single-center opinion. Anticancer Res. 37:2037–2043.
2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hatzaras I, Schmidt C, Klemanski D,
Muscarella P, Melvin WS, Ellison EC and Bloomston M: Pancreatic
resection in the octogenarian: A safe option for pancreatic
malignancy. J Am Coll Surg. 212:373–377. 2011.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kinoshita S, Sho M, Yanagimoto H, Satoi S,
Akahori T, Nagai M, Nishiwada S, Yamamoto T, Hirooka S, Yamaki S,
et al: Potential role of surgical resection for pancreatic cancer
in the very elderly. Pancreatology. 15:240–246. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sho M, Murakami Y, Kawai M, Motoi F, Satoi
S, Matsumoto I, Honda G, Uemura K, Yanagimoto H, Kurata M, et al:
Prognosis after surgical treatment for pancreatic cancer in
patients aged 80 years or older: A multicenter study. J
Hepatobiliary Pancreat Sci. 23:188–197. 2016.PubMed/NCBI View
Article : Google Scholar
|