Introduction
Prostate cancer is the most common genitourinary
cancer in men. In 2020, 1,414,259 new cases and 375,304 deaths were
estimated worldwide (1).
Similarly, the incidence of prostate cancer is also the highest of
male cancers in Japan, with the projected number of patients in
2021 being 95,400(2). Serum
prostate-specific antigen (PSA) testing is the most important
clinical test for the early detection of prostate cancer. Due to
its simplicity, PSA testing is used to screen men for prostate
cancer risk, with numerous industrialized countries having
developed organized population-based PSA screening models. The
European Randomized Study of Screening for Prostate Cancer (ERSPC)
and the Prostate, Lung, Colorectal, and Ovarian Cancer Screening
Trial (PLCO) were large randomized controlled trials of PSA-based
screening that were announced simultaneously in 2009 (3,4).
Nine years of follow-up led to the mortality rate ratio in the
screening group being reduced by 20% in the ERSPC trial. However, a
difference in mortality rate ratios was not observed between
screened or unscreened groups after 11.5 years of follow-up in the
PLCO trial. Currently, population-screening for prostate cancer
remains one of the controversial issues in this field (5).
In Japan, organized population-based PSA screening
has been carried out since the early 1990s (6). However, by 2000, only 14.3% of
municipalities in Japan ran screening programs. Nevertheless, by
2015, according to a Japanese Foundation for Prostate Research
(JFPR) survey, population-based PSA screening systems could be
found in 83.0% of municipalities (7). Currently, a population-based PSA
screening system is present in over half of all cities and towns in
all prefectures of Japan, except for Shiga Prefecture. According to
the JFPR survey, in 2015, the implementation rate for organized PSA
mass-screening in Shiga Prefecture was lowest (6.7% of
municipalities). Moreover, the last city, Kusatsu, terminated
population-based screening in 2017. Therefore, since 2018, no local
governments in Shiga Prefecture have offered PSA screening, a
situation that is quite exceptional in Japan.
Features of newly-diagnosed patients with prostate
cancer in Shiga Prefecture were previously reported. A total of 97%
of the patients were discovered through opportunistic PSA testing
and showed worse clinical features than those patients diagnosed
via an organized population-based screening (8). In the present study, a subanalysis
was conducted to compare the characteristics of patients diagnosed
with prostate cancer in 2012 and 2017 in Kusatsu City (Japan), the
only municipality in Shiga Prefecture that implemented an organized
population-based PSA screening, with those of patients in other
municipalities in the prefecture.
Materials and methods
Patients
As a multicenter observational study, this
investigation was conducted in 14 hospitals in Shiga Prefecture,
Japan, as previously reported (8).
Briefly, in 2012 and 2017, patients diagnosed with prostate cancer
were surveyed. Cases were only included if they were pathologically
diagnosed via prostate biopsy due to elevated serum PSA. Patients
were excluded if they were incidentally diagnosed with T1a-b
prostate cancer when operated on for benign prostate
hyperplasia.
Data acquisition
Clinicopathological data of patients were extracted
from their medical records by attending physicians in each
hospital. In this survey, such data were collected, including
patient's age, reasons for PSA measurement, initial PSA levels,
Gleason score of prostate biopsy specimens, primary treatments
selected, clinical stage (TNM classification 2009), and their place
of residence. The reasons for PSA measurement were classified into
six groups as follows: i) testing in general practice clinics, ii)
testing in urologic clinics, iii) a repeat test due to elevated PSA
earlier, iv) community-based PSA screening, v) investigation for
metastatic disease of unknown origin, and vi) others. Risk
classification was defined according to Arnsrud Godtman et
al (9) as follows: Low
risk=T1, not N1 or M1, with a Gleason score ≤6, and PSA <10
ng/ml. Intermediate risk=T1-2, not N1 or M1, with a Gleason score
≤7 and/or PSA <20 ng/ml. High risk=T1-4, not N1 or M1, with a
Gleason score ≥8 and/or PSA <100 ng/ml. Advanced=N1 and/or M1
and/or PSA ≥100 ng/ml.
Approval (approval no. R2018-010) for the present
study was granted by the Ethics Committee of Shiga University of
Medical Science (Otsu, Japan) and by the ethics committee at each
study center. The study was undertaken according to the provisions
of the Declaration of Helsinki. Informed consent was obtained in
the form of opt-out, and those who rejected were excluded.
Organized population-based PSA
screening in Kusatsu City, Shiga
Kusatsu City initiated an annual prostate cancer
screening program using serum PSA tests in 2004. The target
population was limited to men ≥50 years old. Recommendations for
prostate cancer screening were made to eligible persons by mail.
The study participants visited family physicians or nearby
hospitals with a recommendation letter and underwent a serum PSA
test. The PSA cutoff value in this screening was set at 4.0 ng/ml.
Kusatsu City collected final reports from hospitals where further
prostate examinations were performed. This cancer screening program
ceased in 2018 according to Kusatsu City policy. Data from this PSA
screening program in Kusatsu City from 2004 to 2017 was kindly
provided by the Division of Health Promotion, the Department of
Health and Welfare, Kusatsu City, Japan.
Statistical analysis
We compared the clinical data of patients in Kusatsu
City to those of other municipalities in Shiga Prefecture. IBM SPSS
for Windows version 22.0 (IBM Corp.) was used to carry out
statistical analyses. Differences between groups were analyzed
using a Mann-Whitney U test and Fisher's exact test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Demographics of patients
Within the institutions surveyed, 984 patients in
total were diagnosed with prostate cancer made up of 431 in 2012
and 553 in 2017. According to the cancer registries of Shiga
Prefecture, the number of cases of newly diagnosed prostate cancer
were 616 and 896 in 2012 and 2017, respectively (10). Thus, the present study covered more
than 60% of the total patient population. Since the community-based
PSA screening program in Shiga Prefecture was similar between 2012
and 2017, data from the two years were combined and analyzed as a
single group. The study population was divided into two groups
according to the place of residence: Kusatsu City and other
municipalities. Demographics of patients are shown in Table I.
 | Table IDemographics of patients. |
Table I
Demographics of patients.
| | Total | Kusatsu city | Other
municipalities | P-value |
|---|
| Number of
patients | 984 | 93 | 891 | |
| Median age,
years | 72 (44-92) | 70 (50-88) | 73 (44-92) | 0.015 |
| Median initial PSA
(ng/ml) | 11.27
(1.15-8684) | 7.70
(3.488-8684) | 11.80
(1.15-8138) | <0.001 |
| Gleason score | | | | |
|
<8 | 596 (61%) | 70 (75%) | 526 (59%) | 0.002 |
|
≥8 | 388 (39%) | 23 (25%) | 365 (41%) | |
| T stage | | | | |
|
T1c | 263 (27%) | 26 (28%) | 237 (27%) | <0.001 |
|
T2 | 457 (46%) | 56 (60%) | 401 (45%) | |
|
T3 | 200 (21%) | 9 (10%) | 191 (21%) | |
|
T4 | 56 (6%) | 0 | 56 (6%) | |
|
Unknown | 8 (1%) | 2 (2%) | 6 (1%) | |
| N stage | | | | |
|
N0 | 860 (87%) | 87 (94%) | 773 (87%) | 0.047 |
|
N1 | 119 (12%) | 5 (5%) | 114 (13%) | |
|
Unknown | 5 (1%) | 1 (1%) | 4 (1%) | |
| M stage | | | | |
|
M0 | 846 (86%) | 88 (95%) | 758 (85%) | 0.011 |
|
M1 | 130 (13%) | 4 (4%) | 126 (14%) | |
|
Unknown | 8 (1%) | 1 (1%) | 7 (1%) | |
The median age of patients in Kusatsu City was
significantly younger than in other municipalities (70 vs. 73
years, P=0.015). The median initial PSA values of patients in
Kusatsu City were also significantly lower than those of other
municipalities (7.70 vs. 11.80 ng/ml, P<0.001). Worse prognostic
factors, including a high Gleason Score (P=0.002), higher T-stage
(P<0.001), higher rates of nodal (P=0.047) and distant
metastasis (P=0.011), were found in other municipalities.
Differences in reasons for PSA
measurements
The reasons for PSA measurements in each group are
summarized in Table II. In
Kusatsu City, 93 patients were diagnosed with prostate cancer in
two sample years. A total of 26 men (28.0%) were diagnosed through
community-based PSA screening. In comparison, in the other
municipalities, only three of 891 patients (0.3%) were diagnosed
via organized PSA screening (P=0.011). In other municipalities, the
most common reason for PSA measurement was examination by general
practitioners (42%). The specific reasons for why general
physicians measured PSA in some patients could not be precisely
identified because the referral forms showed incomplete
information.
 | Table IIReasons for PSA measurements. |
Table II
Reasons for PSA measurements.
| Reasons for PSA
measurements | Kusatsu City
(%) | Other
municipalities (%) | P-value |
|---|
| Overall | 93(100) | 891(100) | |
| Organized screening
(Community-based PSA screening) | 26(28) | 3 (0.3) | 0.011 |
| General practice
clinic | 13(14) | 375(42) | |
| Urologic
clinic | 24(26) | 251(28) | |
| Repetitive
measurement due to previous elevated PSA | 15(16) | 137(15) | |
| Investigation for
metastatic disease of unknown origin | 2(2) | 36(4) | |
| Others | 13(14) | 89(10) | |
Clinicopathological differences
between organized community-based PSA screening and opportunistic
PSA measurement in patients of Kusatsu City
Of the patients in Kusatsu City, cases screened by
opportunistic PSA test presented with a significantly higher median
initial PSA value (P=0.01) and than values for those who underwent
organized screening (Table III).
In addition, a trend was noted toward more patients with higher T
stage, nodal and distant metastases in the opportunistic screening
group, although no statistically significant differences were
evident.
 | Table IIIClinicopathological differences by
reasons for PSA measurement: Kusatsu City. |
Table III
Clinicopathological differences by
reasons for PSA measurement: Kusatsu City.
| | Organized
screening | Opportunistic
measurement | P-value |
|---|
| Overall | 26 | 67 | |
| Median age | 70 (61-80) | 70 (50-88) | 0.748 |
| Median initial PSA
(ng/ml) | 5.16
(3.791-27.3) | 9.1
(3.488-8684) | 0.010 |
| Initial PSA
(ng/ml) | | | |
|
<4 | 1 (4%) | 1 (1%) | 0.607 |
|
4-10 | 19 (73%) | 41 (61%) | |
|
10-20 | 5 (19%) | 16 (26%) | |
|
20-100 | 1 (4%) | 5 (7%) | |
|
≥100 | 0 | 4 (6%) | |
| Gleason score | | | |
|
<8 | 20 (77%) | 50 (75%) | 1 |
|
≥8 | 6 (23%) | 17 (25%) | |
| T stage | | | |
|
<T3 | 26 (100%) | 56 (86%) | 0.056 |
|
≥T3 | 0 | 9 (14%) | |
| N stage | | | |
|
N0 | 26 (100%) | 61 (93%) | 0.317 |
|
N1 | 0 | 5 (7%) | |
| M stage | | | |
|
M0 | 26 (100%) | 62 (94%) | 0.574 |
|
M1 | 0 | 4 (6%) | |
| Risk
classification | | | |
|
Low
risk | 3 (12%) | 8 (12%) | 0.479 |
|
Intermediate
risk | 17 (65%) | 36 (54%) | |
|
High
risk | 6 (23%) | 14 (21%) | |
|
Advanced | 0 | 7 (10%) | |
|
Unknown | 0 | 2 (3%) | |
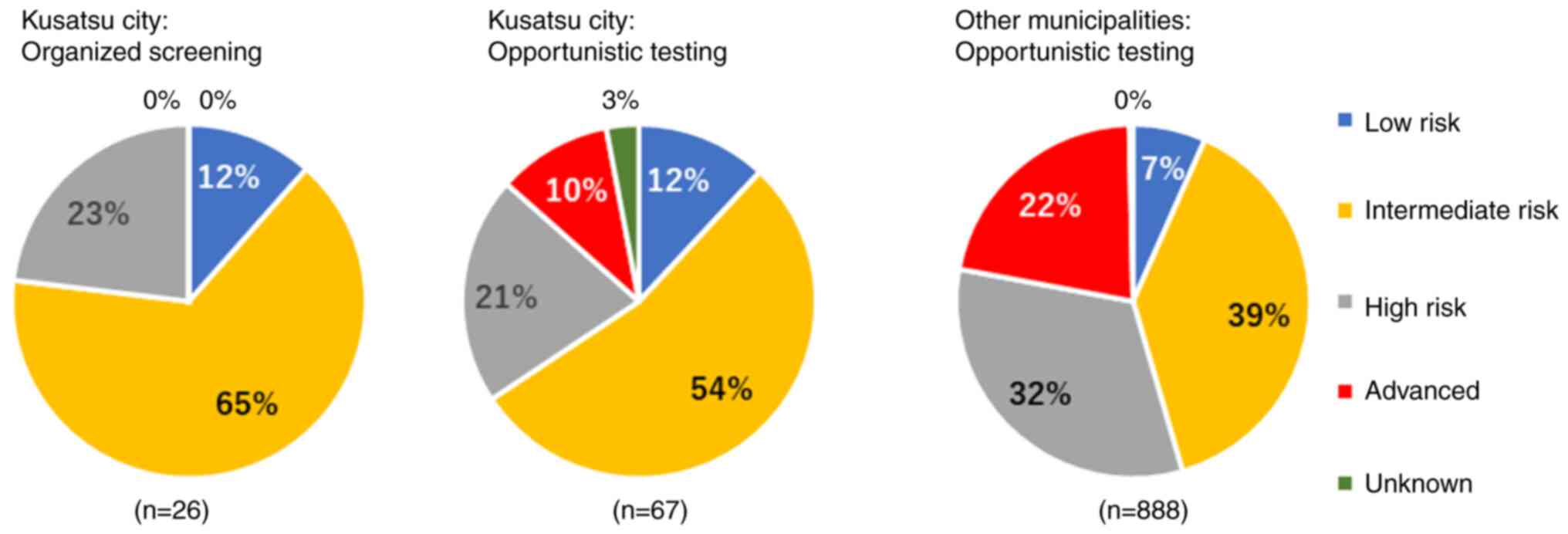
Clinicopathological features in
patients diagnosed through opportunistic PSA measurement
The characteristics of patients diagnosed
opportunistically, excluding through organized PSA screening
programs, were compared between Kusatsu and other municipalities in
Table IV. Patients in Kusatsu
were diagnosed at a younger age than in other municipalities
(P=0.034). A lower median PSA value was revealed in the Kusatsu
group compared with other municipalities (P=0.001). The proportion
of worse risk classification (high to advanced risk) in the other
municipality group was more prominent than in Kusatsu City
(P<0.001; Fig. 1).
 | Table IVClinicopathological features in
patients diagnosed by an opportunistic PSA measurement. |
Table IV
Clinicopathological features in
patients diagnosed by an opportunistic PSA measurement.
| | Kusatsu City | Other
municipalities | P-value |
|---|
| Overall | 67 | 888 | |
| Median age | 70 (50-88) | 73 (44-92) | 0.034 |
| Median initial PSA
(ng/ml) | 9.1
(3.488-8684) | 11.8
(1.15-8138) | 0.001 |
| Initial PSA
(ng/ml) | | | |
|
<4 | 1 (1%) | 10 (11%) | 0.003 |
|
4-10 | 41 (61%) | 370 (42%) | |
|
10-20 | 16 (26%) | 195 (22%) | |
|
20-100 | 5 (7%) | 175 (20%) | |
|
≥100 | 4 (6%) | 138 (15%) | |
| Gleason score | | | |
|
<8 | 50 (75%) | 523 (59%) | 0.014 |
|
≥8 | 17 (25%) | 365 (41%) | |
| T stage | | | |
|
<T3 | 56 (86%) | 635 (72%) | 0.013 |
|
≥T3 | 9 (14%) | 247 (28%) | |
| N stage | | | |
|
N0 | 61 (93%) | 770 (87%) | 0.250 |
|
N1 | 5 (7%) | 114 (13%) | |
| M stage | | | |
|
M0 | 62 (94%) | 755 (86%) | 0.064 |
|
M1 | 4 (6%) | 126 (14%) | |
| Risk
classification | | | |
|
Low
risk | 8 (12%) | 59 (7%) | <0.001 |
|
Intermediate
risk | 36 (54%) | 345 (39%) | |
|
High
risk | 14 (21%) | 288 (32%) | |
|
Advanced | 7 (10%) | 193 (22%) | |
|
Unknown | 2 (3%) | 3 (0.3%) | |
Discussion
Screening for PSA is helpful for the early detection
of asymptomatic prostate cancer, although controversy still exists
as to whether this reduces the rate of prostate cancer mortality.
In the U.S., the PLCO Cancer Screening Trial has been performed
since the 1990s (4). The PLCO
Trial randomly assigned 76,693 men to undergo either annual
screening (annual PSA testing for six years) or the usual care as
control. After follow-up for 7 to 10 years, the death rate from
prostate cancer was very low and showed no significant difference
between the two study groups. Extended follow-up over a median of
15 years also indicated no difference in reduction in prostate
cancer mortality between intervention and control arms (11). Due to these results, the U.S.
Preventive Services Task Force (USPSTF) recommended against
PSA-based screening for prostate cancer in 2012. In contrast to the
PLCO Trial, a statistically significant reduction (20%) was noted
for prostate cancer mortality in the ERSPC study (3). After a 16-year follow-up, a
significant reduction in cancer mortality continued, and the number
of men required to be screened to prevent one prostate cancer death
was reduced compared with that of previous reports from ERSPC
(12). However, the PLCO Trial was
flawed with a high contamination rate in the control arm (13). After a detailed review of various
reports, USPSTF revised the recommendation that undergoing periodic
PSA-based screening for prostate cancer is left to individual men
aged from 55 to 69 years (14).
With the spread of PSA testing in clinical use, population-based
PSA screening has expanded in Japan as well as the U.S. and Europe
(6). In 2015, 1,189 of 1,432
(83.0%) municipalities in Japan had systems in place for
population-based PSA screening according to a report by the JFPR
(7). Despite this high
implementation rate in Japan, only one city in Shiga Prefecture,
Kusatsu City, undertook population-based PSA screening during our
survey years.
In our study, patients in Kusatsu City who were
detected not only by an organized population-based screening but
also through opportunistic PSA testing showed a lower risk of
prostate cancer than those in other municipalities. An exact
explanation for this interesting result is not obvious but a
possible reason may be related to the exposure rate of PSA
screening. Organized mass screening using a serum PSA test by
Kusatsu City was undertaken for 14 years (2004-2017). A summary of
the data from PSA mass screenings in Kusatsu City are presented in
Table V. A total of ~20,000 men,
50 years or older, were invited to the mass screening program each
year, with uptake rates of 8.4-13.8%. Okihara et al
(15) reported on the findings and
quality control of prostate cancer screening performed serially for
a decade in the Otokuni area, Kyoto, Japan. In the Otokuni program,
candidates were part of a male population, 55 years or older, and
the program involved ~22,000 men per year. In Otokuni, 39,213 men
attended primary PSA screening over 10 years; thus, the mean yearly
number of men screened was ~3,900. It was hypothesized by the
authors that the exposure rate for PSA screening in the Otokuni
area was 65%. The number of candidates for organized PSA screening
in the Otokuni area was similar to that of Kusatsu City, but the
rate of men attending PSA screening was two to three-fold that of
Kusatsu City. Although we cannot calculate precisely the exposure
rate for PSA screening in the men of Kusatsu City, it was assumed
to be ~30%, which apparently seemed higher than that of other
municipalities in Shiga Prefecture. Therefore, it was hypothesized
that the higher exposure rates were caused by stage migration in
newly diagnosed patients in Kusatsu City, even though this was
opportunistic PSA testing, which is less effective compared with
organized screening.
 | Table VThe results of PSA mass screenings
organized by Kusatsu City (2004-2017). |
Table V
The results of PSA mass screenings
organized by Kusatsu City (2004-2017).
| | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|
| Male population of
aged 50-years or older (A) | 18,756 | 19,133 | 19,454 | 19,796 | 20,072 | 20,448 | 20,722 | 21,060 | 21,460 | 21,852 | 22,193 | 22,671 | 23,214 | 23,685 |
| Number of men
screened for PSA (B) | 1,593 | 2,514 | 2,633 | 2,734 | 2,434 | 2,411 | 2,371 | 2,308 | 2,422 | 2,366 | 2,428 | 2,001 | 1,977 | 2,001 |
| PSA screening rates
(B/A, %) | 8.5 | 13.1 | 13.5 | 13.8 | 12.1 | 11.8 | 11.4 | 11.0 | 11.3 | 10.8 | 10.9 | 8.8 | 8.5 | 8.4 |
| Number of people
with elevated PSA levels, 4.0 ng/ml or higher (C) | 198 | 207 | 215 | 236 | 222 | 201 | 217 | 176 | 164 | 160 | 174 | 132 | 113 | 73 |
| Positive PSA test
rates (C/B, %) | 12.4 | 8.2 | 8.2 | 8.6 | 9.1 | 8.3 | 9.2 | 7.6 | 6.8 | 6.8 | 7.2 | 6.6 | 5.7 | 3.6 |
| Number of people
who visited clinics for further examination (D) | 84 | 76 | 58 | 78 | 91 | 94 | 113 | 105 | 99 | 99 | 118 | 93 | 82 | 45 |
| Visiting rates for
further examination (D/C, %) | 42.4 | 36.7 | 27.0 | 33.1 | 41.0 | 46.8 | 52.1 | 59.7 | 60.4 | 61.9 | 67.8 | 70.5 | 72.6 | 61.6 |
| Number of patients
who were diagnosed with prostate cancer (E) | 33 | 27 | 12 | 13 | 21 | 17 | 10 | 21 | 13 | 14 | 20 | 17 | 14 | 4 |
| Cancer detection
rates (E/B, %) | 2.07 | 1.07 | 0.46 | 0.48 | 0.86 | 0.71 | 0.42 | 0.91 | 0.54 | 0.59 | 0.82 | 0.85 | 0.71 | 0.20 |
Further speculation relates to the awareness about
prostate cancer screening using PSA measurements in general
physicians as well as residents in Kusatsu City. Invitation letters
were sent to individuals who were eligible for PSA screening.
Therefore, this information may influence not only the response
rate of PSA screening, but also awareness about prostate cancer and
PSA testing in men in Kusatsu City. Furthermore, general physicians
in Kusatsu may also tend to perform opportunistic PSA testing more
frequently than in other municipalities in Shiga Prefecture.
However, it is too difficult to prove this hypothesis in the
present study.
The exact reason for the termination of the
organized screening program for detecting prostate cancer by the
Kusatsu City government is unknown. In Japan, prostate cancer is
not included in cancer screening as a national program under the
Health Promotion Act. The national committee in the Ministry of
Health, Labor and Welfare do not recommend PSA-based screening for
prostate cancer due to insufficient evidence of a reduction in
mortality (16). According to a
questionnaire by the JFPR, most cities and towns in Shiga
Prefecture responded that they did not provide cancer screening
because there is no legal basis for it (7). The present study showed not only the
direct effects of cancer screening but also the indirect effects.
In areas where cancer screening programs were continuously
implemented, even patients who underwent opportunistic PSA testing
were detected at an earlier stage than those in areas where cancer
screening was not conducted. On basis of these results, the
resumption of PSA screening in Kusatsu is appealing. Furthermore,
it is considered that it is important to disseminate these data to
other municipalities in Shiga Prefecture so that they consider
initiating PSA screening to diagnose cancer in its early
stages.
There are several limitations to the present study.
First, these results only apply to a limited area in Japan and may
not be applicable to other areas. Second, the present study could
not prove the effectiveness of PSA mass screening with respect to
cancer-specific mortality. Since the USPSTF recommended against
PSA-based prostate cancer screening for all men in 2012, there has
been a significant increase in the rate of metastatic disease at
diagnosis in U.S. (17). After 20
years of a steady decline, prostate cancer mortality in the U.S.
has also ticked upwards in the last few years (18). Based on the current situation in
the U.S., it is possible that discontinuation of PSA screening in
Kusatsu City may lead to a worsening of the mortality rate in
prostate cancer. It is planned by the authors to conduct a new
study on survival outcomes. Third, comments cannot be made on the
prevalence of overdiagnosing by PSA testing since individual
attending physicians likely have differing policies on diagnosis
and treatment. Current progress in the development of
multi-parametric magnetic resonance imaging (MRI) has played a
major role in the diagnosis of prostate cancer. The PRECISION study
showed that a multi-parametric MRI-based pathway increased the
detection rate of clinically significant prostate cancer from 26 to
38% and decreased the detection rate of clinically insignificant
cancer from 22 to 9%, compared with 12-core transrectal
ultrasound-guided biopsy (19). In
the near future, prostate-specific membrane antigen imaging may add
value to the detection of clinically significant localized prostate
cancer (20). Such diagnostic
efforts should reduce overdiagnosis. However, in spite of such
limitations, the present study yielded important information on the
indirect influence of population-based PSA screening.
In conclusion, organized PSA screening leads to an
increase in the number of men diagnosed with early-stage prostate
cancer. Furthermore, population-based mass screening may indirectly
affect early detection, even by opportunistic PSA testing in the
community. Although the results of the present study were derived
only from a small area, similar trends will likely be observed in
more communities with continuous organized PSA screening.
Acknowledgements
The authors appreciate the help of Professor Koji
Okihara (North Medical Center, Kyoto Prefectural University of
Medicine) for numerous helpful discussions and advice. The authors
would also like to thank the staff of the Division of Health
Promotion, the Department of Health and Welfare, Kusatsu City for
providing data. The authors would also like to acknowledge Dr
Etsuji Nakano (Nakano clinic) and Dr Tatsuhiro Yoshiki (Kyoto
Pharmaceutical University), founders of the organized PSA screening
system of Kusatsu City.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request. The data are not publicly available due to privacy or
ethical restrictions.
Authors' contributions
SK, YO, KN, ToY, SI, YaS and CJK designed the study.
SK and YO confirm the authenticity of all the raw data, analyzed
the data and drafted the manuscript. TI, RY, YA, ZN, HS, HU, YuS,
YN, AW, MaN, TeY, MiN performed acquisition of clinical data. AK
interpreted the data and supervised the study. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study was approved (approval no.
R2018-010) by the Ethics Committee of Shiga University of Medical
Science (Otsu, Japan) and by the ethics committee at each study
center. The present study was undertaken according to the
provisions of the Declaration of Helsinki. The participants were
informed of the study by public notice using posters or websites.
Informed consent was obtained in the form of opt-out, and those who
rejected were excluded.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
National Cancer Center Japan: Projected
cancer incidence in 2021. National Cancer Center Japan, Tokyo,
2021. https://ganjoho.jp/reg_stat/statistics/stat/short_pred_en.html.
Accessed April 17, 2022.
|
|
3
|
Schröder FH, Hugosson J, Roobol MJ,
Tammela TL, Ciatto S, Nelen V, Kwiatkowski M, Lujan M, Lilja H,
Zappa M, et al: Screening and prostate-cancer mortality in a
randomized European study. N Engl J Med. 360:1320–1328.
2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Andriole GL, Crawford ED, Grubb RL III,
Buys SS, Chia D, Church TR, Fouad MN, Gelmann EP, Kvale PA, Reding
DJ, et al: Mortality results from a randomized prostate-cancer
screening trial. N Engl J Med. 360:1310–1319. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Etzioni R, Gulati R, Cooperberg MR, Penson
DM, Weiss NS and Thompson IM: Limitations of basing screening
policies on screening trials: The US preventive services task force
and prostate cancer screening. Med Care. 51:295–300.
2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ito K, Oki R, Sekine Y, Arai S, Miyazawa
Y, Shibata Y, Suzuki K and Kurosawa I: Screening for prostate
cancer: History, evidence, controversies and future perspectives
toward individualized screening. Int J Urol. 26:956–970.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
The Japanese Foundation for Prostate
Research: Implementation status of prostate cancer screening by
municipality (MAP diagram)-Survey in June 2015. The Japanese
Foundation for Prostate Research, Tokyo, 2015. http://www.jfpr.or.jp/publish/pub21.html. Accessed
April 17, 2022.
|
|
8
|
Okinaka Y, Kageyama S, Nishizawa K,
Yoshida T, Ishitoya S, Shichiri Y, Kim CJ, Iwata T, Yokokawa R,
Arai Y, et al: Clinical, pathological, and therapeutic features of
newly diagnosed prostate cancer predominantly detected by
opportunistic PSA screening: A survey of Shiga Prefecture, Japan.
Prostate. 81:1172–1178. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Arnsrud Godtman R, Holmberg E, Lilja H,
Stranne J and Hugosson J: Opportunistic testing organized
prostate-specific antigen screening: Outcome after 18 years in
versus the Göteborg randomized population-based prostate cancer
screening trial. Eur Urol. 68:354–360. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Shiga Prefectural Government: Cancer
Registry. https://www.pref.shiga.lg.jp/ippan/kenkouiryouhukushi/iryo/15264.html.
Accessed April 17, 2022.
|
|
11
|
Pinsky PF, Prorok PC, Yu K, Kramer BS,
Black A, Gohagan JK, Crawford ED, Grubb RL and Andriole GL:
Extended mortality results for prostate cancer screening in the
PLCO trial with median follow-up of 15 years. Cancer. 123:592–569.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hugosson J, Roobol MJ, Månsson M, Tammela
TLJ, Zappa M, Nelen V, Kwiatkowski M, Lujan M, Carlsson SV, Talala
KM, et al: A 16-yr follow-up of the European randomized study of
screening for prostate cancer. Eur Urol. 76:43–51. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Shoag JE, Mittal S and Hu JC: Reevaluating
PSA testing rates in the PLCO trial. N Engl J Med. 374:1795–1796.
2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
U.S. Preventive Service Task Force: Final
Recommendation Statement. Screening for Prostate Cancer: May 08,
2018. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/prostate-cancer-screening.
Accessed April 17, 2022.
|
|
15
|
Okihara K, Kitamura K, Okada K, Mikami K,
Ukimura O and Miki T: Ten year trend in prostate cancer screening
with high prostate-specific antigen exposure rate in Japan. Int J
Urol. 15:156–160. 2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hamashima C: Cancer screening guidelines
and policy making: 15 Years of experience in cancer screening
guideline development in Japan. Jpn J Clin Oncol. 48:278–286.
2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Desai MM, Cacciamani GE, Gill K, Zhang J,
Liu L, Abreu A and Gill IS: Trends in incidence of metastatic
prostate cancer in the US. JAMA Netw Open.
5(e222246)2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Klotz L: Overdiagnosis in urologic cancer:
For world journal of urology symposium on active surveillance in
prostate and renal cancer. World J Urol. 40:1–8. 2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kasivisvanathan V, Rannikko AS, Borghi M,
Panebianco V, Mynderse LA, Vaarala MH, Briganti A, Budäus L,
Hellawell G, Hindley RG, et al: MRI-targeted or standard biopsy for
prostate-cancer diagnosis. N Engl J Med. 378:1767–1777.
2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Amin A, Blazevski A, Thompson J, Scheltema
MJ, Hofman MS, Murphy D, Lawrentschuk N, Sathianathen N, Kapoor J,
Woo HH, et al: Protocol for the PRIMARY clinical trial, a
prospective, multicentre, cross-sectional study of the additive
diagnostic value of gallium-68 prostate-specific membrane antigen
positron-emission tomography/computed tomography to multiparametric
magnetic resonance imaging in the diagnostic setting for men being
investigated for prostate cancer. BJU Int. 125:515–524.
2020.PubMed/NCBI View Article : Google Scholar
|