Introduction
Intravesical immunotherapy using bacillus
Calmette-Guerin (BCG) is recommended for patients with
intermediate- to high-risk non-muscle invasive bladder cancer after
transurethral resection of bladder tumor (TURBT) (1,2).
Carcinoma in situ (CIS) cannot be cured by tumor resection
alone and is usually followed by intravesical BCG therapy.
Induction BCG is also used to reduce the risk of intravesical
recurrence and progression. Although this treatment is effective,
many adverse effects have been reported and monitoring after
treatment is crucial. Common adverse effects that occur shortly
after BCG instillation include fever, dysuria, and hematuria due to
a systemic or local immune response (3). Severe adverse effects are related to
BCG infection or systemic immune reaction and can occur in any
structure-one possible manifestation is Reiter syndrome-but it is
rare for bladder tuberculosis (TB) to manifest several years after
BCG treatment. Bladder TB is also difficult to diagnose because the
symptoms are similar to those of cystitis or cancer and BCG
infection cannot be proven by urinalysis or urine culture. We
present our experience with a patient who had chronic cystitis due
to bladder TB after BCG treatment, resulting in voiding dysfunction
and hydronephrosis.
Case report
A 73-year-old man was referred to the Urology
Department of Okayama University Hospital (Okayama, Japan) in March
2016 because of nocturia and a positive urine cytology. Cystoscopy
showed a nonpapillary lesion on the posterior bladder wall;
computed tomography (CT) revealed no evidence of metastasis or
upper urinary tract tumor, and magnetic resonance imaging (MRI)
showed no sign of muscle-invasive bladder cancer. TURBT pathology
revealed high grade urothelial carcinoma at or above stage pT1.
Second TURBT 6 weeks after the initial resection revealed CIS. The
patient subsequently underwent intravesical BCG treatment (80 mg
once a week for 8 doses) without any complications.
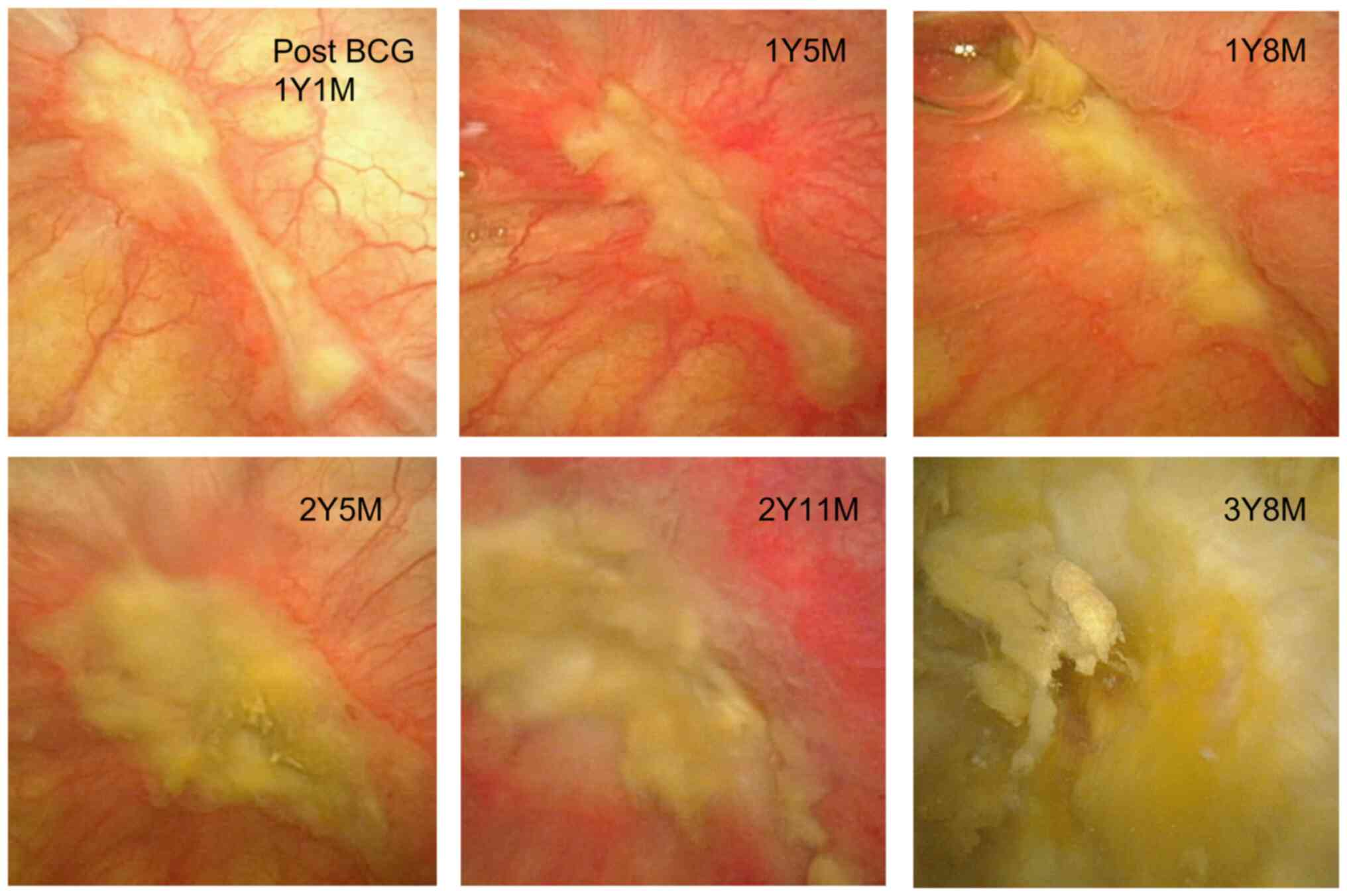
The patient underwent routine postoperative
follow-up. At 1 year and 5 months after BCG therapy, cystoscopy
showed an ulcerative lesion surrounded by edematous red patches at
the resection site in the bladder dome. This lesion was followed
with serial cystoscopy and observed to gradually spread. The
ulcerative lesion was gradually replaced with necrotic debris
(Fig. 1); although this was
suspicious of intravesical cancer recurrence, serial urine cytology
showed no signs of malignancy. At 3 years and 8 months after BCG
therapy, dysuria, pollakiuria and urge urinary incontinence
occurred. Antibiotic treatment had no effect on his symptoms or
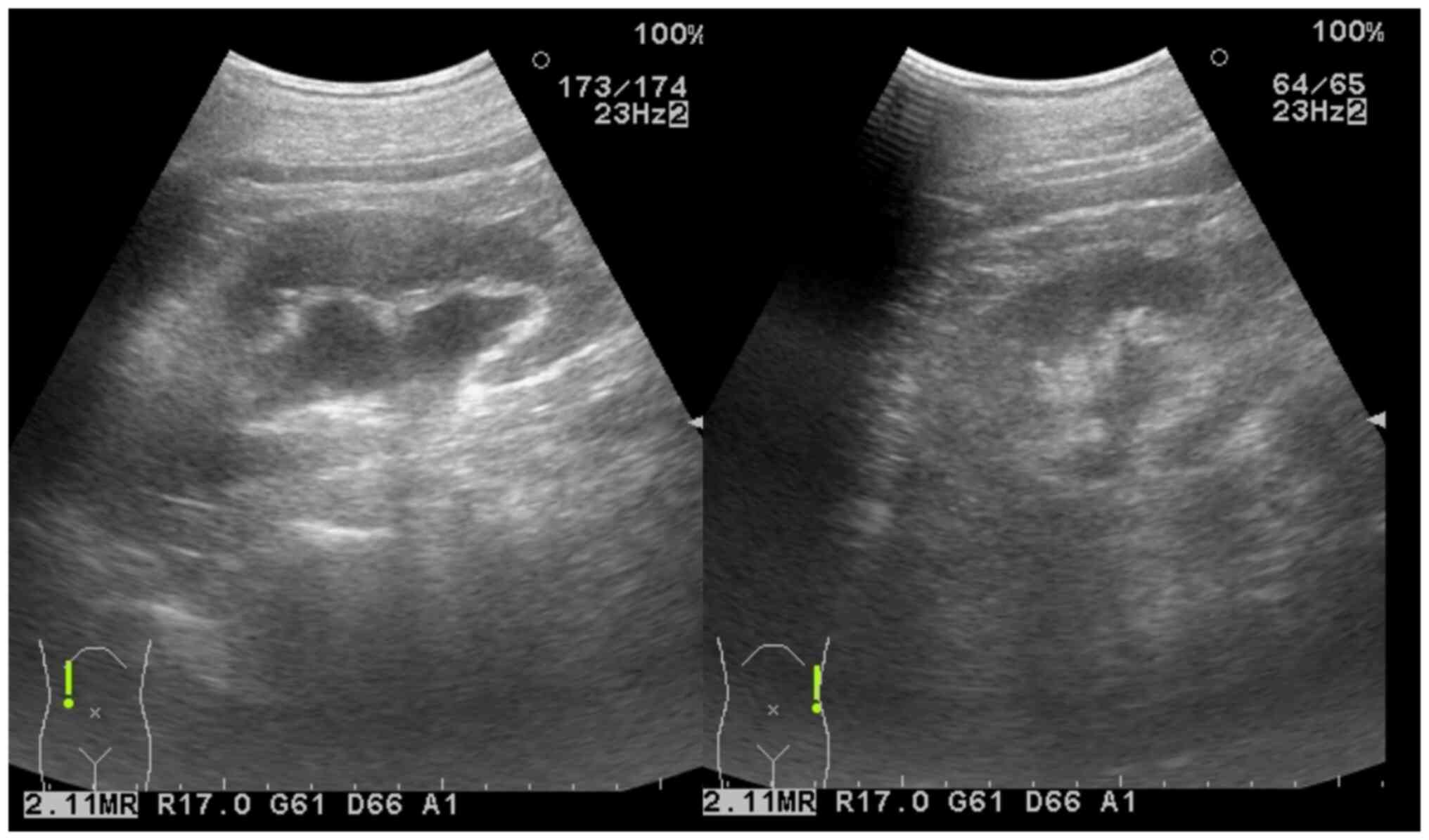
cystoscopy findings. Although a repeat TURBT performed 4 years
after BCG treatment revealed no malignancy, ultrasonography showed
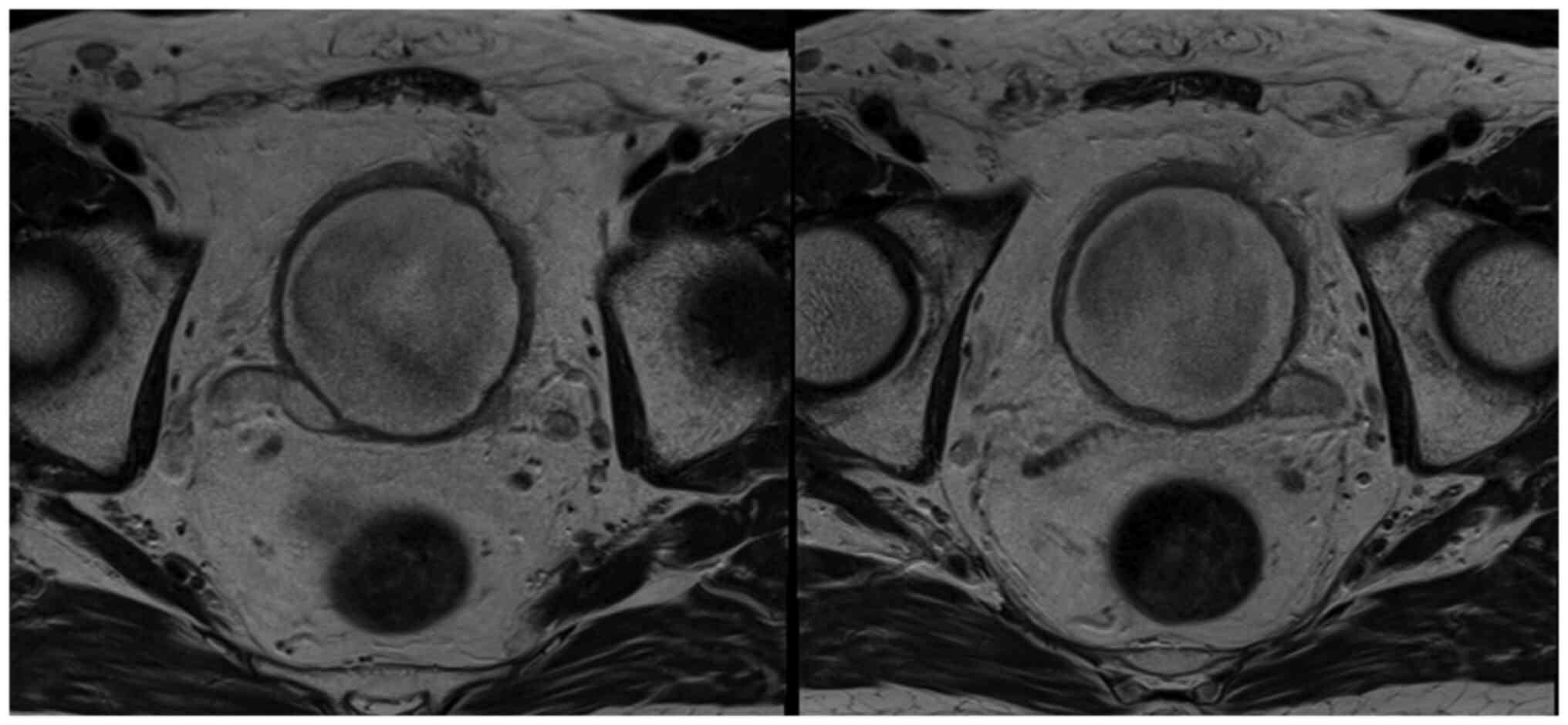
bilateral hydronephrosis (Fig. 2),
and MRI revealed a postvoid urine residual volume >100 ml and
bilateral distal ureteral dilation, suggesting a ureterovesical
junction obstruction (Fig. 3). We
placed a right ureteral stent but were unable to detect the left
ureteral orifice to place a left ureteral stent.
Four years and 3 months after BCG therapy,
Mycobacterium tuberculosis complex (MBTC) was detected by
mycobacterial urine culture. The urine nitrate reduction test was
negative, but urine polymerase chain reaction (PCR), which was
carried out by other researchers than us who belong to the
department of clinical laboratory in our hospital, was positive for
M. bovis. Therefore, we reached a diagnosis of bladder TB
caused by M. bovis. We placed a left ureteral stent by an
antegrade approach and started antitubercular treatment with 300 mg
isoniazid, 450 mg rifampicin, and 1,000 mg ethambutol daily. We
initially planned to continue the regimen for 3 months; however, 2
months after treatment started, the patient experienced drug
eruption over his back and both legs, which quickly spread over his
entire body [grade 2 according to the Common Terminology Criteria
for Adverse Events (CTCAE) version 5.0]. The discoloration
gradually improved after discontinuation of ethambutol. One month
later, the patient developed a persistent cough productive of
sputum. Chest CT revealed consolidation and a ground glass
appearance in both lungs. A pulmonologist diagnosed drug-induced
pneumonia after close inspection via bronchoscopy (CTACE grade 2).
We then discontinued the other 2 drugs. In total, he took
ethambutol for 76 days and isoniazid and rifampicin for 83
days.
Despite the interruption in TB treatment, repeat
urine testing revealed no evidence of MBTC and PCR was negative.
There was no evidence of intravesical cancer recurrence or
metastasis. His pneumonia gradually improved with corticosteroid
treatment. Six months after completing TB treatment, the patient
still had voiding dysfunction, so we started clean intermittent
catheterization (postvoid residual urine volume 150-180 ml). One
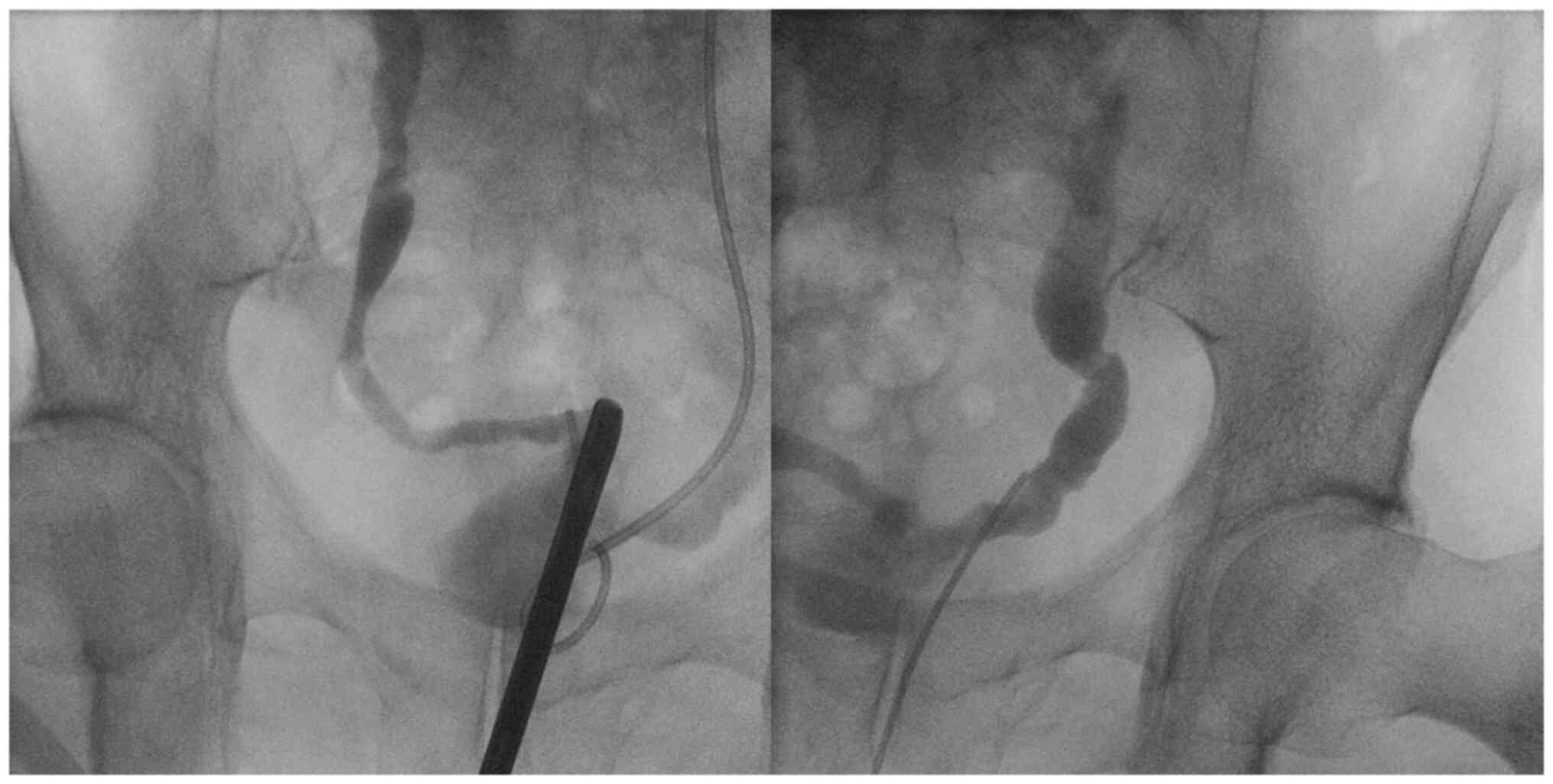
year after TB treatment, retrograde pyelography showed improvement
in his bilateral ureteral strictures (Fig. 4). After removal of both stents, he
was followed up with bilateral grade 1-2 hydronephrosis and voiding
dysfunction by ultrasonography.
Discussion
We present our experience with a patient who had
chronic cystitis with bilateral ureteral strictures and voiding
dysfunction caused by bladder TB resulting from intravesical BCG
therapy for CIS 4 years prior. When the patient initially presented
with continuous episodes of cystitis, we strongly suspected an
intravesical carcinoma recurrence; this presumption resulted in
delayed detection of his bladder TB.
Intravesical BCG instillation is standard therapy
after TURBT for CIS of the bladder (4). Previous studies have shown that the
therapy significantly reduces the risk of short- and long-term
treatment failure compared with intravesical chemotherapy (5). Instillation of BCG for intermediate-
or high-risk non-muscle invasive bladder cancer is an option to
decrease the rate of recurrence (6-8).
However, there are various adverse effects associated with
treatment, so close follow-up is crucial.
Approximately 1% of patients develop BCG infection
after bladder instillation; the median time to develop symptoms
from first BCG instillation is 170 days (in our patient, it was 3
years and 8 months) (9). A
contracted bladder and ureteral strictures can occur in patients
with TB cystitis as a result of the granulomatous inflammation and
edematous mucosa associated with infection (10,11),
presumably because of thickening of the ureteral and bladder
mucosae as a reaction to inflammation. Infection with BCG can cause
bladder ulcers; the increased risk of this manifestation was found
to be associated with male sex and certain tumor characteristics
(e.g., high grade and T1 stage) (11). Bladder TB cannot be distinguished
from other etiologies of cystitis using standard urinalysis and
urine culture; it requires specialized testing (mycobacterial urine
culture, PCR, biopsy, etc.). Clinicians should bear in mind the
possibility of bladder TB during follow-up after intravesical BCG
therapy, and they should remain vigilant for symptoms or cystoscopy
findings suspicious for TB.
Drug-susceptible TB is treated with a standard
6-month regimen of 4 antitubercular drugs: isoniazid, rifampicin,
ethambutol, and pyrazinamide (M. bovis is treated in the
same manner as M. tuberculosis) (10,12).
However, short courses may be feasible for genitourinary TB.
Although our patient's planned 3-month treatment period could not
be completed because of treatment-related adverse effects (drug
eruption and interstitial pneumonia), his mycobacterial urine
culture was negative after his truncated course of treatment. He
initially needed bilateral ureteral stenting for stricture, but the
stents were successfully removed after TB treatment. In some
patients, ureteral stricture and contracted bladder caused by TB
are irreversible and require surgical repair (10,13,14).
Therefore, early detection of bladder TB and proper intervention is
essential.
Bladder TB can occur several years after
intravesical BCG instillation. It is important to bear in mind the
possibility of BCG infection when patients experience persistent
cystitis with bladder ulceration after BCG instillation, even if
the treatment was long ago. The essence of our report is to warn
urologists not to miss the opportunity to diagnose bladder TB after
BCG therapy. We believe that our findings will be beneficial to
detect bladder TB at an early stage and reduce complications.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YT and MF wrote the manuscript (equally
contributed). TS was a major contributor to the conception and
design of the study. YT, MF and KW performed the patient's
examination. TS, SK, TI and SN confirm the authenticity of all the
raw data. YT, KB, KE, TK, YK, KW and MA performed the patient's
surgery and acquired the data. YT, MF, KK, YM and MA analyzed and
interpreted the data. SK, TI, SN, KB, KE, TK, YK, KK, YM, KW and MA
critically revised the manuscript for intellectual content. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publications
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing interests
The author declare that they have no competing
interests.
References
|
1
|
Flaig TW, Spiess PE, Agarwal N, Bangs R,
Boorjian SA, Buyyounouski MK, Chang S, Downs TM, Efstathiou JA,
Friedlander T, et al: Bladder cancer, version 3.2020, NCCN clinical
practice guidelines in oncology. J Natl Compr Canc Netw.
18:329–354. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Babjuk M, Burger M, Capoun O, Cohen D,
Compérat EM, Dominguez Escrig JL, Gontero P, Liedberg F,
Masson-Lecomte A, Mostafid AH, et al: European association of
urology guidelines on non-muscle-invasive bladder cancer (Ta, T1,
and carcinoma in situ). Eur Urol. 81:75–94. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Green DB, Kawashima A, Menias CO, Tanaka
T, Redelman-Sidi G, Bhalla S, Shah R and King BF: Complications of
intravesical BCG immunotherapy for bladder cancer. Radiographics.
39:80–94. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Takenaka A, Yamada Y, Miyake H, Hara I and
Fujisawa M: Clinical outcomes of bacillus Calmette-Guérin
instillation therapy for carcinoma in situ of urinary bladder. Int
J Urol. 15:309–313. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sylvester RJ, van der Meijden AP, Witjes
JA and Kurth K: Bacillus calmette-guerin versus chemotherapy for
the intravesical treatment of patients with carcinoma in situ of
the bladder: A meta-analysis of the published results of randomized
clinical trials. J Urol. 174:86–92. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Malmström PU, Sylvester RJ, Crawford DE,
Friedrich M, Krege S, Rintala E, Solsona E, Di Stasi SM and Witjes
JA: An individual patient data meta-analysis of the long-term
outcome of randomised studies comparing intravesical mitomycin C
versus bacillus Calmette-Guérin for non-muscle-invasive bladder
cancer. Eur Urol. 56:247–256. 2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Böhle A and Bock PR: Intravesical bacille
Calmette-Guérin versus mitomycin C in superficial bladder cancer:
Formal meta-analysis of comparative studies on tumor progression.
Urology. 63:682–687. 2004.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sylvester RJ, van der Meijden AP and Lamm
DL: Intravesical bacillus Calmette-Guerin reduces the risk of
progression in patients with superficial bladder cancer: A
meta-analysis of the published results of randomized clinical
trials. J Urol. 168:1964–1970. 2002.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Larsen ES, Nordholm AC, Lillebaek T,
Holden IK and Johansen IS: The epidemiology of bacille
Calmette-Guérin infections after bladder instillation from 2002
through 2017: A nationwide retrospective cohort study. BJU Int.
124:910–916. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Muneer A, Macrae B, Krishnamoorthy S and
Zumla A: Urogenital tuberculosis-epidemiology, pathogenesis and
clinical features. Nat Rev Urol. 16:573–598. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liu Y, Lu J, Huang Y and Ma L: Clinical
spectrum of complications induced by intravesical immunotherapy of
bacillus Calmette-Guérin for bladder cancer. J Oncol.
2019(6230409)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
WHO: Treatment of Tuberculosis:
Guidelines. 4th edition. World Health Organization, Geneva,
pp95-99, 2010.
|
|
13
|
Kulchavenya E: Urogenital tuberculosis:
Definition and classification. Ther Adv Infect Dis. 2:117–122.
2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Handmer MM, Winter M, Lee WG and
Louie-Johnsun M: Unexpected tuberculosis causing ureteral
stricture. ANZ J Surg. 87:515–516. 2017.PubMed/NCBI View Article : Google Scholar
|