Introduction
Hypopharyngeal squamous cell carcinoma (HSCC) is one
of the most aggressive types of head and neck cancer (1-2).
Neck lymph node metastasis (LNM) is an important clinical
characteristic of HSCC. The incidence of neck LNM is 40-70%
(3), which influences the
prognosis and leads to poor survival of patients with HSCC
(2,4). Thus, in order to improve the survival
of patients with HSCC, neck lymph node dissection and irradiation
are routinely performed during hypopharyngeal cancer surgery and
radiotherapy, which are the two main treatment modalities for HSCC
(5). Since the neck lymphatic
drainage region in HSCC includes the whole neck region from the
skull base to the supraclavicular region, extensive lymph node
dissection and radiation are cumbersome. The difficulty of the
surgical procedure and the irradiation plan prolong the time to
recovery from these therapies, and at the same time increase the
incidence of surgical complications and radiation damage, such as
local dysfunction, pharyngeal fistula, neck edema, and so on
(6). This seriously affects the
quality of life of HSCC survivors (7). However, in clinical practice, there
is a great variation in neck LNM in HSCC among different patients
(8). Previous studies found that
~40-50% of patients who underwent neck lymph node dissection did
not exhibit tumor metastases in postoperative pathologic specimens
(9,10). Therefore, it is critical to
identify HSCC patients at high risk of neck LNM so that proper
lymph node dissection and irradiation can be performed only in
selected patients. This will be beneficial in reducing treatment
complications and improving the quality of life of HSCC
survivors.
Molecular mechanisms underlying HSCC determine tumor
development, progression, invasion and metastasis, and also
determine neck LNM in HSCC (11-13).
An improved understanding of the molecular mechanisms of neck LNM
in HSCC and identification of tumor-specific biomarkers for the
prediction of neck LNM are urgently needed to guide the treatment
of neck LNM, and to improve the prognosis and the quality of life
of patients with HSCC.
Stathmin1 (STMN1), also known as oncoprotein 18, is
a cytoplasmic protein that self-regulates through a phosphorylation
pathway, controlling the dynamic balance of the microtubule system,
influencing cell mitosis and regulating cell cycle progression.
This, in turn, affects tumor cell proliferation and motility
(14,15). It has been widely reported that
STMN1 is overexpressed in numerous different human cancers and is
closely associated with LNM (16,17).
Cao et al (16)
retrospectively analyzed eight studies and found that esophageal
cancer patients with high STMN1 expression had a significantly
higher risk of LNM than those with low STMN1 expression, further
proving that high STMN1 expression was a risk factor for
susceptibility to LNM in tumors. Chen et al (17) found that STMN1 was overexpressed in
HSCC, and promoted FaDu cell proliferation and migration. However,
whether STMN1 promotes neck LNM in HSCC and the underlying
molecular mechanisms remain to be elucidated. In the present study,
a correlation analysis was performed between neck LNM in HSCC and
STMN1 expression level in a large sample of clinical cases. The
molecular mechanisms underlying the promotion of neck LNM in HSCC
by STMN1 were explored, which could perhaps guide treatment of neck
LNM.
Materials and methods
Study case selection
To establish the association between STMN1 and neck
LNM in HSCC, clinical cases of HSCC were selected and analyzed.
Study inclusion criteria were as follows: Absence of distant
metastases; patient had undergone radical hypopharyngeal cancer
resection with neck lymph node dissection; pathological
confirmation as HSCC; neck LNM status was pathologically evaluated
after operation; patient had not undergone preoperative
chemotherapy or radiotherapy; preoperative clinical data and
paraffin-embedded specimens for immunohistochemical (IHC) staining
were available. Eligible cases were recruited from the Second
Hospital of Shandong University between January 2015 and December
2020 and from the Shandong Provincial Hospital between January 2018
and March 2021. A written informed consent was obtained from each
patient before surgery.
IHC staining and evaluation of
staining results
For eligible cases of HSCC, STMN1 expression and
lymphatic vessel invasion (LVI) status in tumor tissues were
evaluated with IHC staining. The detailed procedure of IHC was as
follows:
IHC staining was performed on 4-µm paraffin tissue
sections mounted on slides and dried for 8 h at 60˚C. The slides
were deparaffinized in xylene and dehydrated conventionally, then
pressure-cooked in sodium citrate buffer (pH 6.0) (LBP Med-Sci) to
facilitate antigen retrieval. After natural cooling, endogenous
peroxidase was blocked with 3% hydrogen peroxide. The sections were
subsequently incubated with rabbit anti-STMN1 polyclonal antibody
(1:75) (Wuhan Boster Biological Technology, Ltd.), or rabbit
anti-D2-40 polyclonal antibody (1:75) (Wuhan Boster Biological
Technology, Ltd.) (Anti-D2-40 antibody was used to stain lymphatic
vessels, and in stained lymphatic vessels, the presence of tumor
embolus represented LVI) overnight at 4˚C. After washing with PBS
(LBP Med-Sci), the sections were incubated for 30 min with the
two-step method followed by the poly-HRP anti-mouse/rabbit
detection system (LBP Med-Sci). A DAB detection kit (Talent-Bio)
was used for 5-10 min to show immunolabeling, resulting in a brown
precipitate. Finally, the sections were re-stained with hematoxylin
(Beijing Solarbio Science & Technology Co., Ltd.),
differentiated in hydrochloric acid alcohol, and sealed with
neutral balsam (Beijing Solarbio Science & Technology Co.,
Ltd.).
After IHC staining, the association between the
expression of STMN1 and neck LNM, and the association between the
expression of STMN1 and LVI status were both analyzed.
Cell culture and transfection
Human HSCC cell lines (FaDu cells) were purchased
from Procell Life Science & Technology Co., Ltd., and were
identified by short tandem repeat (STR) and free of mycoplasma
contamination. Subsequently, they were cultured in PMI150410-MEM
medium (Procell Life Science & Technology Co., Ltd.) with 10%
fetal bovine serum (FBS; Shanghai VivaCell Biosciences, Ltd.) and
1% penicillin/streptomycin (Shanghai Basal Media Technologies Co.,
Ltd.) in a humidified incubator containing 5% CO2 at
37˚C. Cells in favorable growth condition were collected for
subsequent experiments.
Human short hairpin RNA (shRNA) was packaged and
synthesized by Shanghai GeneChem Co., Ltd. The shRNA sequences
targeting STMN1 are shown in Table
I and different sequences were synthesized to inhibit STMN1.
The negative control (NC) shRNA was used as a blank control.
According to the infection multiplicity (MOI=10) of the FaDu cell
line provided in the pre-experiment, an aliquot of 2 ml FaDu cell
suspension at a cell concentration of 5x104 cells/ml was
seeded in a six-well plate (Corning, Inc.), when the cell density
roughly reached 30%, the culture medium was replaced, and then the
diluted 10 µl shRNA and 40 µl transfection enhancer P (GeneChem,
Inc.) were added and placed at 37˚C for 48 h for transfections.
After transfections, the transfection efficiencies were evaluated
with quantitative reverse transcription-polymerase chain reaction
(RT-qPCR) and western blot analyses.
 | Table ISequences of shRNAs targeting
STMN1. |
Table I
Sequences of shRNAs targeting
STMN1.
| Name | Sequence |
|---|
| NC shRNA | Blank sequence |
| STMN1-shRNA1 | PSC71180-1 |
| |
CCGGAACTGGAACGTTTGCGAGAGACTCGAGTCTCTCGCAAACGTTCCAGTTTTTTTG |
| STMN1-shRNA2 | PSC71181-1 |
| |
CCGGGAAGAGAAACTGACCCACAAACTCGAGTTTGTGGGTCAGTTTCTCTTCTTTTTG |
| STMN1-shRNA3 | PSC71182-1 |
| |
CCGGCCAGGTGAAAGAACTGGAGAACTCGAGTTCTCCAGTTCTTTCACCTGGTTTTTG |
After a week, the cell lines, which reached
satisfactory transfection efficiency and were readily cultured,
were selected for the following cell functional and mechanism
research experiments.
RNA extraction and RT-qPCR
RT-qPCR was used to test relative expression levels
of genes analyzed in FaDu cells. Total RNA was extracted from FaDu
cells using Esciece RNA Extraction Kit (www.esunbio.com), according to the manufacturer's
instructions. Evo M-MLV Mix Kit and SYBR Green Premix Pro Taq HS
qPCR Kit (Accurate; https://agbio.com.cn) were used for RT-PCR and qPCR,
according to the manufacturer's instructions. The first step of
RT-PCR was to remove genomic DNA under the reaction condition of
42˚C for 2 min, and then reverse transcription reaction was
performed at 37˚C for 15 min and 85˚C for 5 sec. The qPCR reaction
system included SYBR Green Pro Taq HS Premix, cDNA sample,
RNase-free water and primers. The primers were synthesized by
Shanghai GeneChem Co., Ltd and the sequences are presented in
Table II. Reaction steps were as
follows: 30 sec pre-denaturation at 95˚C followed by 40 cycles of
95˚C for 5 sec, and 60˚C for 30 sec, all of which were conducted on
the Quantstudio TM5 System (Thermo Fisher Scientific, Inc.). The
relative expression levels of the genes were calculated using the
comparative 2-ΔΔCq method (18) with GAPDH as the reference.
 | Table IIPrimer sequences of genes analyzed
for reverse transcription-quantitative PCR. |
Table II
Primer sequences of genes analyzed
for reverse transcription-quantitative PCR.
| Gene name | Primer sequences
(5'→3') | Product length
(bp) |
|---|
| STMN1 | F:
TGATTCTCAGCCCTCGGTCAA | 133 |
| | R:
GCTTCATGGGACTTGCGTCTT | |
| HIF-1α | F:
GGCAGCAACGACACAGAAAC | 86 |
| | R:
TTTTCGTTGGGTGAGGGGAG | |
| VEGF-A | F:
CTTGCAGATGTGACAAGCCG | 150 |
| | R:
GTCGATGGTGATGGTGTGGT | |
| MTA1 | F:
ACCGAGTCGCTCAAGTCCTA | 142 |
| | R:
ACAAGTCGGTGATGTCTGCC | |
| GAPDH | F:
GCACCGTCAAGGCTGAGAAC | 138 |
| | R:
TGGTGAAGACGCCAGTGGA | |
Cell functional experiments. Cell
proliferation assay
Cell Counting Kit-8 (CCK-8; Beyotime Institute of
Biotechnology) assay was performed to assess the proliferation
capacities of FaDu cells after transfections with different shRNA
sequences targeting STMN1. An aliquot of 100 µl of FaDu cell
suspension per well was seeded in 96-well culture plates (Corning,
Inc.) at a cell concentration of 3x104 cells/ml in an
incubator. After the cells adhered to the wall and showed evidence
of growth. Culture medium was replaced with 110 µl of fresh culture
medium containing 10 µl of CCK-8 and placed in the incubator at
37˚C for 1.5 h. The absorbance was measured at 450 nm with a
spectrophotometer (Tecan Group, Ltd.) and expressed as the optical
density (OD). The operation was repeated every 24 h for three
consecutive days.
Matrigel invasion assay
Matrigel invasion assay was performed to assess the
invasion capacities of FaDu cells after transfections with
different shRNA sequences targeting STMN1. During the procedures of
Matrigel invasion assay, an aliquot of 200 µl of serum-free FaDu
cell suspension that contains 5x104 cells was seeded in
the upper chamber lined with Matrigel (Corning, Inc.) in a 24-well
Transwell device (8-µm pore size; Jet Bio-Filtration,) which was
pretreated at 37˚C for 1 h, then 600 µl of 10% FBS culture medium
was added to the lower chamber, and placed in the incubator at 37˚C
for 36 h. The cells that invaded through the Matrigel to reach the
membrane of the chambers were fixed in 4% formaldehyde and
methanol, and subsequently, were stained with 0.1% crystal violet
(Beijing Solarbio Science & Technology Co., Ltd.) for 1 h.
Finally, images of the cells that invaded through the Matrigel to
reach the membrane of the chambers were captured with a DMI8
inverted microscope (Leica Microsystems GmbH), following which the
invasive cells were counted with ImageJ software (Java 1.8.0;
National Institutes of Health).
Cell scratching assay
Cell scratching assay was performed to assess the
migration capacities of FaDu cells after transfections with
different shRNA sequences targeting STMN1. During the procedures of
cell scratching assay, an aliquot of 2 ml of FaDu cell suspension
that contains 5x105 cells was seeded in a six-well plate
(Corning, Inc.), and after the cells covered the plates, a 200 µl
pipette tip was used to draw a straight line on the plates. Then, 2
ml of serum-free medium was added and the cells were placed in a 5%
CO2 incubator. Finally, images of the migration area
were captured with a DMI8 inverted microscope at 0, 24 and 48 h,
and densitometric analysis was performed using ImageJ software.
Bioinformatics analysis
Firstly, the expression levels of STMN1 in HSCC
tissues and normal tissues were analyzed. The data of the gene chip
GSE2379 were used for HSCC containing STMN1 from the Gene
Expression Omnibus (GEO; http://www.ncbi.nlm.nih.gov/geo/) for this.
Eventually, the gene chip data of four normal tissues and 14 HSCC
tissues were included in the present study. The expression
differences of STMN1 among the HSCC tissues, metastases tissues,
and normal tissues were analyzed using R4.2.0 software (http://www.R-project.org).
In order to explore the molecular mechanisms
underlying the promotion of neck LNM in HSCC by STMN1, a
bioinformatics analysis was performed to identify potential target
genes and pathways of STMN1. The gene sequencing data of HSCC are
unavailable in The Cancer Genome Atlas (TCGA). Since HSCC is a
representative cancer of head and neck SCC (HNSCC), HSCC exhibits
common biological feature with HNSCC; therefore, the gene
sequencing data of HNSCC were screened from TCGA. Eventually, a
total of 504 HNSCC gene sequencing data were obtained. The data
were divided into two groups (high and low expression groups)
according to the expression levels of STMN1, and an enrichment
analysis was performed using Molecular Signature Database v7.5.1 in
the GSEA software (https://www.gsea-msigdb.org/gsea). The pathways with
P<0.05 and false discovery rate (FDR) <0.25 were considered
as significant enrichment pathways. At the same time, in order to
obtain other potential target genes of STMN1, a target gene
prediction analysis was performed using the Rv4.0.3 package from
the Assistant for Clinical Bioinformatics website (www.aclbi.com).
After the bioinformatics analysis, the potential
target genes and pathways of STMN1 promoting neck LNM in HSCC were
identified. Subsequently, RT-qPCR and western blot analyses were
used to further validate these potential target genes and pathways
via a series of cell assays in vitro.
Western blot analysis
Western blot analysis was used to test the
transfection efficiency and validate the potential target genes and
pathways of STMN1. The FaDu cells of each group were lysed with
RIPA lysis solution (Beyotime Institute of Biotechnology) and
target proteins were extracted. Equal amounts of proteins (30 µg)
were added for 10% SDS-polyacrylamide gel electrophoresis and then
transferred to polyvinylidene difluoride membrane (Pall Life
Sciences), then blocked with 5% skimmed milk at room temperature
for 1.5 h. Subsequently, membranes were incubated with the
following primary antibodies against: STMN1 (1:1,000; cat. no.
PB9560; Wuhan Boster Biological Technology, Ltd.), hypoxia
inducible factor-1alpha (HIF-1α; 1:1,000; cat. no. A6265; ABclonal
Biotech Co., Ltd.), vascular endothelial growth factor (VEGF)-A
(1:1,000; cat. no. ab214424; Abcam), metastasis-associated protein
1 (MTA1; 1:1,000; cat. no. ab288765; Abcam) and β-actin (1:2,000;
cat. no. CPA9066; Cohesion Biosciences) overnight at 4˚C, and then
washed with Tris-buffered saline and Tween-20 (TBST, 0.01 M Tris,
0.15 M NaCl, 0.1% Tween-20, pH=7.4) for 30 min. The membranes were
incubated with the HRP-conjugated secondary antibody goat
anti-rabbit/mouse IgG (1:5,000; cat. nos. E-AB-1001/E-AB-1003;
Elabscience Biotechnology, Inc.) at room temperature for 1 h. After
washing again with TBST, ECL luminescent solution was added and
images were captured with Tanon chemiluminescence imager (Tanon
Science and Technology Co., Ltd.). Finally, gray values of protein
bands were quantitatively analyzed with ImageJ software, and
β-actin was used as an internal reference.
Statistical analysis
Statistical analyses were performed using SPSS 20.0
software (IBM Corp.) and GraphPad prism 8.0 software (GraphPad
Software, Inc.). All cell experiments were repeated three times.
The expression levels of genes, OD450 values, relative
number of invasive cells, and relative migratory ratios were
expressed as the mean ± standard deviation (SD). The differences in
numerical variables between two groups were compared using the
independent-samples t-test. The correlations between the expression
status of STMN1 and neck LNM and LVI status were analyzed using the
Spearman's rank correlation test. All P-values were two-sided, and
a value of P<0.05 was considered to indicate a statistically
significant difference.
Results
Clinicopathological features of the
included cases
A total of 117 HSCC cases from the two hospitals
were eligible, as per the inclusion criteria, and were included in
the present study. The expression levels of STMN1 and LVI status
for eligible cases were evaluated with IHC staining. The
clinicopathological features of the included cases are presented in
Table III.
 | Table IIIClinicopathological characteristics
of the included cases. |
Table III
Clinicopathological characteristics
of the included cases.
| Clinicopathological
characteristics | Number of
cases | Expression level of
stathmin1 |
|---|
| Sexa | | High (n=80) | Low (n=37) |
|
Male | 109 | 78 | 31 |
|
Female | 8 | 2 | 6 |
| Median age, years
(range) | 60 (40-76) | | |
|
>60 | 55 | 42 | 13 |
|
≤60 | 62 | 38 | 24 |
| Pathological
stageb | | | |
|
I-III | 41 | 24 | 17 |
|
IVc | 76 | 56 | 20 |
| Pathological
differentiation | | | |
|
Well | 66 | 39 | 27 |
|
Poor | 51 | 41 | 10 |
| Lymphatic vessel
invasion | | | |
|
Negative | 51 | 19 | 32 |
|
Positive | 66 | 61 | 5 |
| Lymph node
metastasis | | | |
|
Negative | 27 | 4 | 23 |
|
Positive | 90 | 76 | 14 |
STMN1 is highly expressed in HSCC
tissues and is associated with LNM
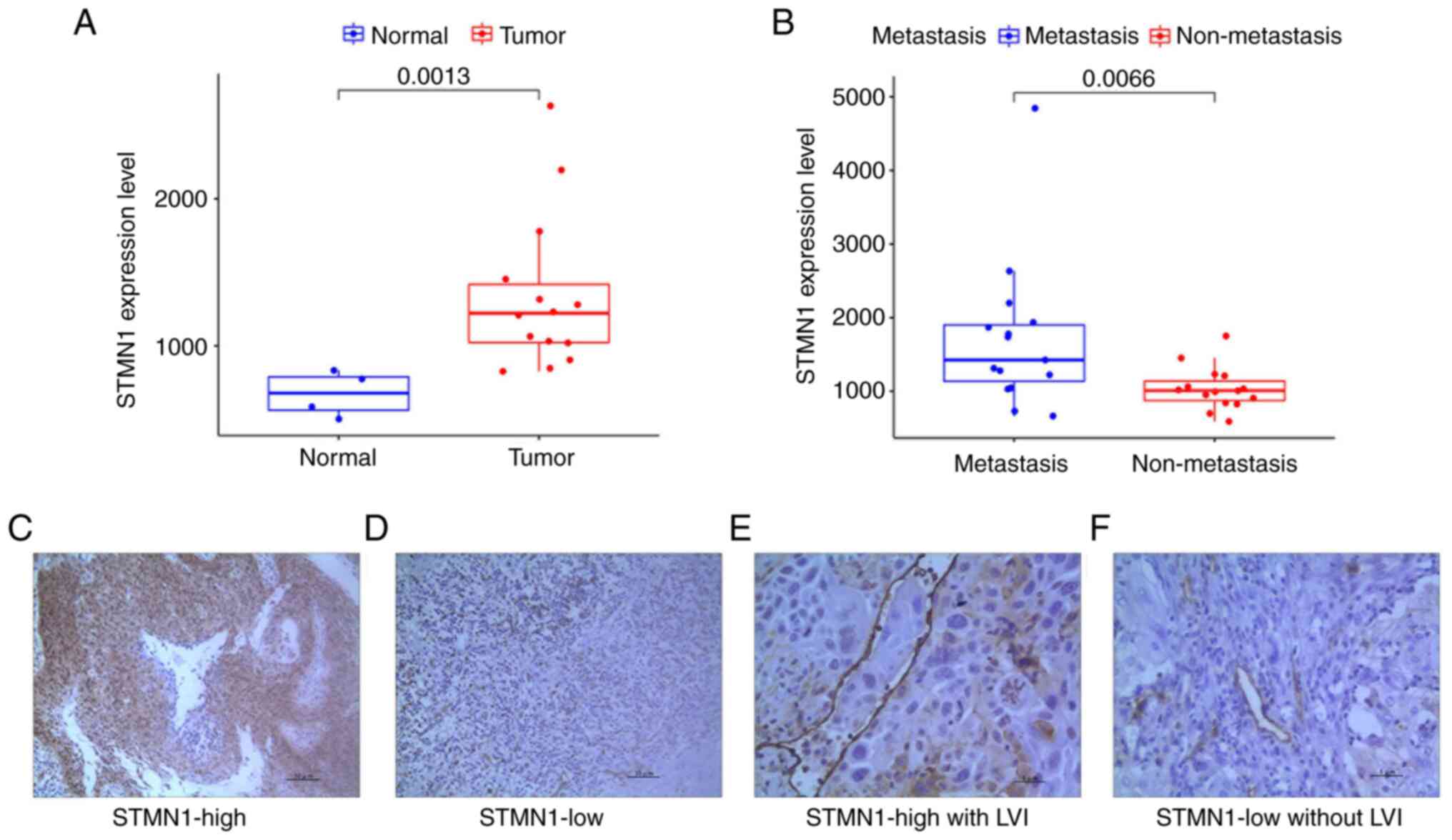
The analyses of included data from gene chips
GSE2379 revealed that STMN1 expression was evidently increased in
HSCC tissues compared with normal hypopharyngeal tissues, and
further increased in HSCC tissues of patients with metastases
(P<0.01, Fig. 1A and B).
Subsequently, IHC staining analysis of the 117
eligible cases in the present study demonstrated that STMN1 was
highly expressed in the majority of cases (Fig. 1C and D); moreover, high expression of STMN1 was
evidently associated with neck LNM in HSCC (Correlation
Coefficient: 0.631, P<0.001). Further analysis revealed that
high expression of STMN1 was also associated with LVI (Correlation
Coefficient: 0.588, P<0.001, Fig.
1E and F). These results
indicated that high expression of STMN1 in HSCC tissues promoted
neck LNM in HSCC and LVI.
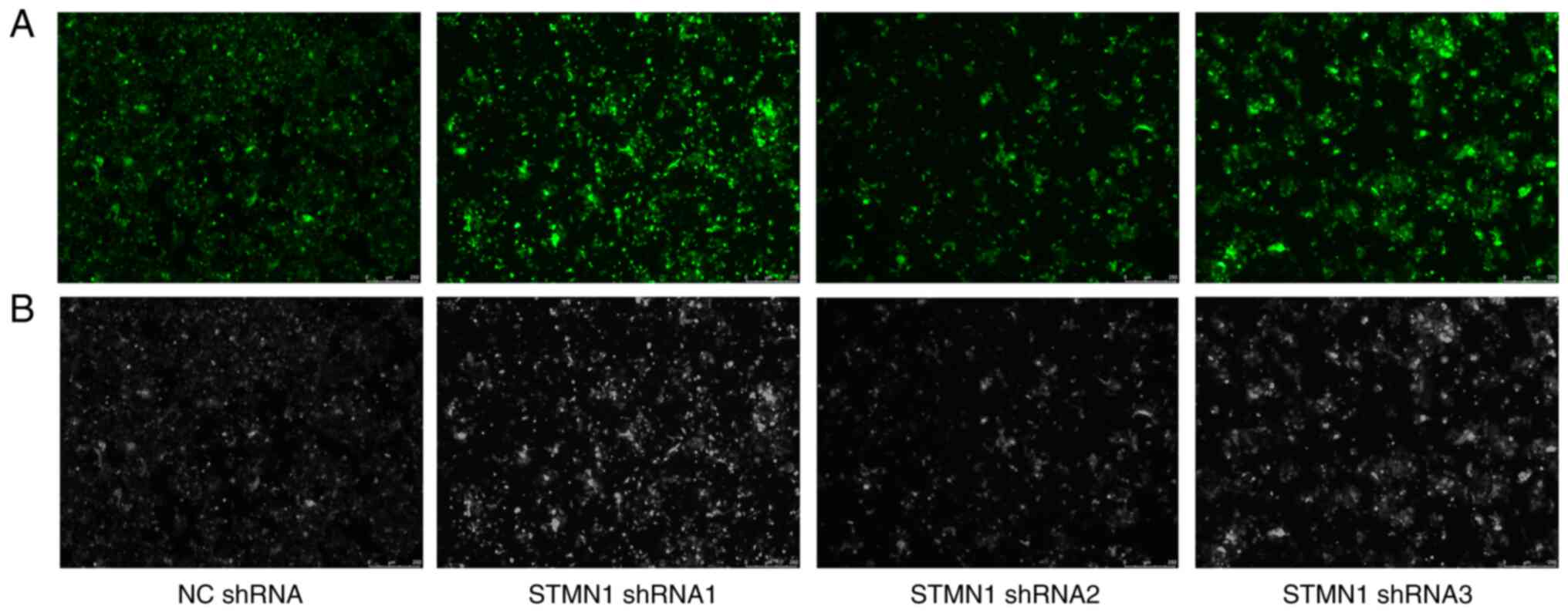
Knockdown of STMN1 in FaDu cell
lines
After performing the aforementioned clinical
analyses, the functions of STMN1 in HSCC were further verified in
FaDu cell lines. As STMN1 showed high expression in FaDu cell
lines, STMN1 was knocked down using different targeting sequences
of shRNA. After the transfections, the green fluorescent protein,
which was used to label the shRNA sequences, was observed under a
fluorescence microscope to confirm the success of the transfection
(Fig. 2). Then, RT-qPCR and
western blot analyses were performed to further verify the efficacy
of the STMN1 knockdown. The results showed that the shRNA1 and
shRNA2 sequences had improved efficacy in STMN1 knockdown than the
shRNA3 sequence, compared with the NC shRNA sequence (Fig. 3A and B). At the same time, the cell lines
transfected with the shRNA1 and shRNA2 sequences had improved
growth conditions than those transfected with the shRNA3 sequence.
Therefore, the FaDu cell lines of STMN1 knockdown with shRNA1 and
shRNA2 sequences were used in the following cell functional
experiments.
Knockdown of STMN1 reduces the
proliferation, invasion and migration of FaDu cells
In cell functional experiments, compared with the
cells in the NC shRNA group, the cells in the STMN1 shRNA groups
had lower OD450 value (P<0.01); the relative
migratory ratios were significantly reduced (P<0.05), and the
relative number of invasive cells in the lower chamber were
significantly decreased (P<0.05, Fig. 3C-E). These cell functional
experimental results revealed that knockdown of STMN1 significantly
reduced the abilities of cell proliferation, migration and
invasion.
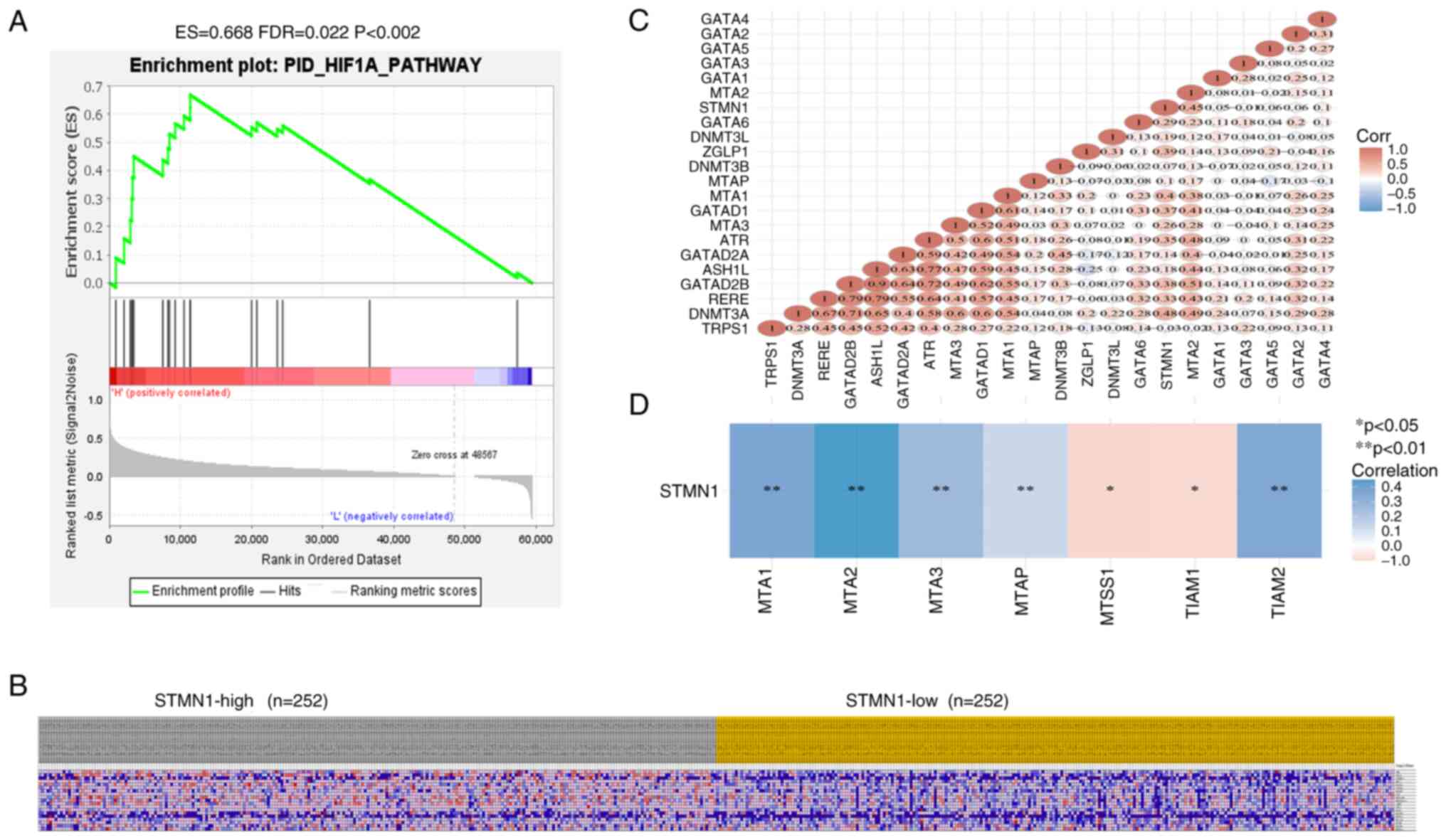
Potential target genes and pathways of
STMN1
To explore the potential mechanisms by which STMN1
promotes LNM in HSCC, evaluation of the potential target genes and
pathways of STMN1 based on a target gene prediction analysis from
the website https://www.aclbi.com and pathway
enrichment analysis from TCGA database were performed. The results
showed that the genes in the HIF-1α pathway were enriched in the
STMN1 high expression group (Fig.
4A and B). At the same time,
the expression level of tumor metastasis-associated protein 1
(MTA1) correlated well with that of STMN1 (Fig. 4C and D). These results indicated that STMN1
potentially promoted LNM in HSCC via regulation of MTA1 expression
and the HIF-1α pathway activation.
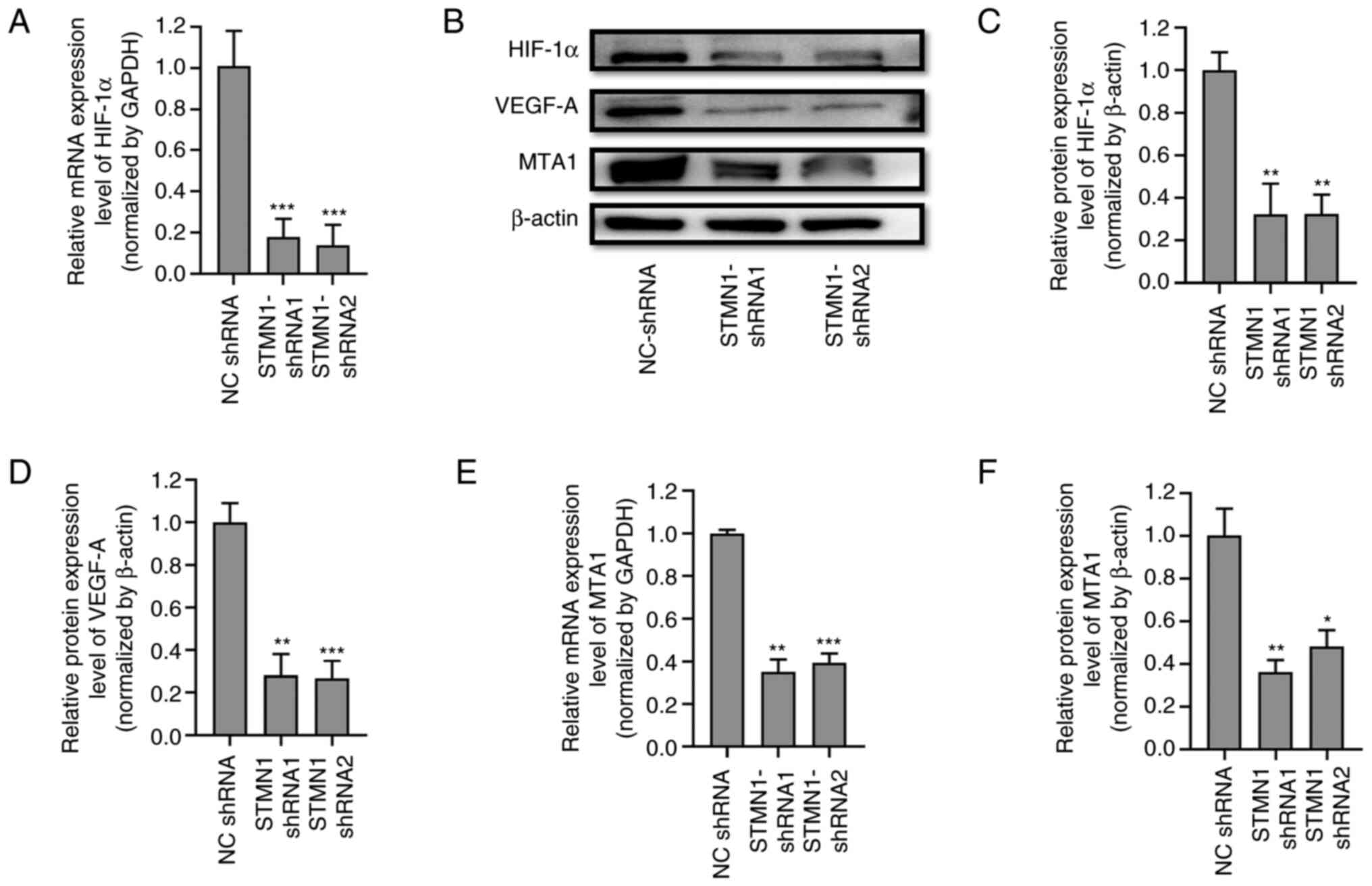
Knockdown of STMN1 inhibits the
activity of the HIF-1α/VGEF-A signal axis
After bioinformatics analysis, the mRNA and protein
levels of HIF-1α in FaDu cells with STMN1 knockdown were detected
by RT-qPCR and western blot analyses, respectively. It was
identified that the relative mRNA expression level and protein
expression level of HIF-1a were both significantly decreased after
STMN1 knockdown with different shRNA sequences (Fig. 5A-C). These findings indicated that
silencing of STMN1 played an important role in the HIF-1α pathway.
VEGF-A is one of the downstream target genes regulated by HIF-1α
and is associated with LNM. Therefore, at the protein level, the
relative expression level of VEGF-A in FaDu cells was also detected
by western blot analysis. The results revealed that the relative
expression level of VEGF-A was also significantly decreased along
with the decline in HIF-1α after STMN1 knockdown with different
shRNA sequences (Fig. 5B and
D). These results indicated that
STMN1 knockdown could inhibit the activity of the HIF-1α/VEGF-A
axis.
Knockdown of STMN1 inhibits the
expression of MTA1
After bioinformatics analysis, the relative mRNA and
protein expression levels of MTA1 in FaDu cells with STMN1
knockdown were also detected by RT-qPCR and western blot analyses.
Consistent with the authors' predictions, the relative expression
level of MTA1 in FaDu cells was significantly decreased after STMN1
knockdown with different shRNA sequences (Fig. 5B, E and F).
These results indicated that STMN1 knockdown could also inhibit the
expression of MTA1.
Discussion
HSCC is the dominant histological subtype in
hypopharyngeal carcinoma (HC), accounting for more than 95% of HC
cases, particularly in China. The tendency toward extensive neck
LNM is the most important clinical feature of HSCC, which
influences the prognosis and leads to poor survival in HSCC
(2,3). Strategies to control neck LNM in HSCC
treatment, including extensive neck lymph node dissection and
irradiation, cause immense pain to HSCC survivors (6,7).
Effective prediction of the possibility of neck LNM will reduce
unnecessary neck lymph node disposal, which will evidently improve
the quality of life of HSCC survivors. However, there is a paucity
of effective biomarkers for predicting neck LNM in HSCC in current
clinical practice. In the present study, for the first time to the
best of our knowledge, the association between STMN1 and neck LNM
in HSCC and the molecular mechanisms underlying the promotion of
neck LNM in HSCC by STMN1 were explored.
Firstly, in 117 postoperative samples and gene chip
data of HSCC, it was found that STMN1 expression was increased in
HSCC tissues; the high expression of STMN1 was associated with high
incidence of neck LNM. This result confirmed the authors'
hypothesis that high expression of STMN1 in HSCC promoted neck LNM,
providing the basis for further research, as also guaranteeing the
value of the present study. Afterwards, in the clinical cases, the
correlation between STMN1 expression and LVI in tumor tissues was
further analyzed; LVI is considered to be the initial step in LNM
and indicates the great possibility of LNM (19). Eventually it was revealed that high
expression of STMN1 was associated with high incidence of LVI,
which proved that high expression of STMN1 promoted LVI in HSCC.
This provided evidence that STMN1 promoted neck LNM in HSCC
possibly via promotion of LVI in HSCC.
In subsequent cell functional and mechanistic
experiments, different shRNA sequences targeting STMN1 were
synthesized to inhibit STMN1 expression in FaDu cell lines to
guarantee the reliability and repeatability of the experimental
results. Eventually, in the cell functional experiments, it was
found that high expression of STMN1 could actually promote FaDu
cell invasion and metastasis. These results of cell experiments
further verified the aforementioned clinical findings and confirmed
the reliability of the present study.
In the following cell mechanistic experiments, the
molecular mechanisms underlying promotion of neck LNM in HSCC by
STMN1 were investigated. A bioinformatics analysis was first
performed to identify potential target genes and pathways of STMN1,
and subsequently further validated these potential target genes and
pathways. After bioinformatics analysis, it was revealed that high
expression of STMN1 was associated with the activation of and gene
enrichment of the HIF-1α pathway. At the same time, it was also
revealed that the expression level of STMN1 was associated with
that of MTA1. These results indicated that STMN1 may influence neck
LNM in HSCC via regulation of the activity of the HIF-1α pathway
and the expression of MTA1.
HIF-1α is the most ubiquitously expressed protein
and functions as a key regulator of oxygen homeostasis in numerous
cell types, mediating transcriptional activation of
lymphangiogenesis and LNM under hypoxic conditions. It is a
critical feature of the tumor microenvironment that promotes
invasion and metastasis (20).
Promotion of LNM by HIF-1α has been widely reported in human
tumors. Zhao et al (21)
and Méndez-Blanco et al (22) found that HIF-1α was associated with
LNM in breast cancer and hepatocellular carcinoma in large samples
of clinical cases. Yang et al (23) reported that UBE2C mediated HIF-1α
activation to promote LNM in HNSCC. Further, the underlying
molecular mechanisms by which HIF-1α promotes LNM were considered
to be via regulation of signaling cascades, such as VEGF-A/-C/-D,
TGF-β, C/EBP-δ and Prox-1(20).
Among them, the HIF-1α/VEGF-A/-C/-D signaling axis has been
considered to be the most important molecular mechanism that
promotes LNM (20,24).
VEGFs stimulate lymphangiogenesis by activating VEGF
receptor (VEGFR) tyrosine kinases in endothelial cells.
Intratumoral hypoxia upregulates the expression of VEGFs, and
importantly, hypoxia selects a subpopulation of tumor cells with an
invasive and metastatic phenotype that have the capacity to escape
from the primary tumors (25,26).
The secreted glycoproteins VEGF-C or VEGF-D activate VEGFR-3, a
cell surface receptor tyrosine kinase on lymphatic endothelium,
leading to growth of lymphatic vessels at the periphery of and
occasionally inside the primary tumor, thereby promoting spread of
tumor cells to lymph nodes. At present, the VEGF-C/VEGF-D/VEGFR-3
pathway is the most well-understood pathway regulating
lymphangiogenesis and LNM (27).
VEGF-A, another VEGF family member, initially identified as an
important promoter of angiogenesis, primarily binds to VEGFR-1 and
VEGFR-2. VEGF-A is known to exert potent lymphangiogenic activity
by activating VEGFR-2, thereby facilitating metastatic spread
(28). In addition, VEGF-A
enhances the heterodimerization of VEGFR-3 with VEGFR-2 and the
phosphorylation of VEGFR-3. This, in turn, provides proliferative
stimuli to lymphatic endothelial cells (29), which are activated in lymphatic
metastasis of tumors (19). In the
present study, it was found that HIF-1α/VEGF-A was significantly
increased in FaDu cells with high expression of STMN1. Moreover,
after STMN1 knockdown with different interference sequences, the
expression levels of HIF-1α/VEGF-A were evidently decreased. These
results led to the conclusion that STMN1 promotes neck LNM in HSCC
via the HIF-1α/VEGF-A axis.
MTA1 has been considered as a transcriptional
regulator and was identified in a screen for genes expressed in
metastatic cells (30). MTA1 is
overexpressed in a variety of tumors and is closely related to LNM
and cancer cell invasion. Li et al (31) reported that the expression level of
MTA1 was strongly associated with the depth of invasion and
lymphatic metastasis in gastrointestinal cancer in a meta-analysis.
Liu et al (32) considered
MTA1 to be a novel marker predicting survival and LNM in cervical
cancer. In HNSCC, Roepman et al (33) found that MTA1 overexpression was
associated with invasion and neck LNM. In the bioinformatics
analysis performed in the present study, the expression of MTA1 was
considered to be associated with STMN1 expression. In the following
cell experiments, MTA1 was also found to be increased in FaDu cells
with high expression of STMN1; concurrently, with STMN1 knockdown
with different interference sequences, the expression levels of
MTA1 were evidently decreased. These results indicated that STMN1
may promote neck LNM in HSCC by affecting the expression of MTA1 in
some way. However, the mechanisms by which MTA1 promotes LNM were
unclear. Guo et al (34)
reported that MTA1 expression was correlated with HIF-1α expression
and lymphangiogenesis in esophageal cancer. In HSCC, whether MTA1
promotes neck LNM by regulating HIF-1α expression is worthy of
further research.
In summary, based on a clinical sample analysis, it
was identified that high expression of STMN1 promoted neck LNM in
HSCC and LVI. Subsequent cell experiments confirmed that high
expression of STMN1 could actually promote FaDu cell invasion and
metastasis. The studies on underlying molecular mechanisms revealed
that STMN1 promotes neck LNM in HSCC via the HIF-1α/VEGF-A axis and
by promoting the expression of MTA1. It would be worthwhile to
elucidate the detailed mechanisms further in future studies.
Acknowledgements
The authors appreciate the support and help from the
Pathology Department of the Shandong Provincial Hospital.
Funding
Funding: The present study was supported by the Natural Science
Foundation of Shandong Province (grant no. ZR2019MH017) and the
Development Foundation of the Second Hospital of Shandong
University for Postgraduate Supervisor (grant no. 6010220073).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
DS and YW contributed to the study concepts, study
design, and the manuscript editing and review. YW contributed to
the experimental studies, data acquisition and analysis. QL
contributed to the literature research. JT and CH contributed to
the data collection of eligible clinical cases and data analysis.
DS and YW confirm the authenticity of all the raw data. All authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study was approved (approval no.
KYLL-2022LW141) by the Ethics Committees of the Second Hospital of
Shandong University (Jinan, China). Written informed consent was
obtained from each patient before surgery.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Aupérin A: Epidemiology of head and neck
cancers: An update. Curr Opin Oncol. 32:178–186. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Newman JR, Connolly TM, Illing EA, Kilgore
ML, Locher JL and Carroll WR: Survival trends in hypopharyngeal
cancer: A population-based review. Laryngoscope. 125:624–629.
2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Buckley JG and MacLennan K: Cervical node
metastases in laryngeal and hypopharyngeal cancer: A prospective
analysis of prevalence and distribution. Head Neck. 2:380–385.
2000.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cooper JS, Porter K, Mallin K, Hoffman HT,
Weber RS, Ang KK, Gay EG and Langer CJ: National Cancer Database
report on cancer of the head and neck:10-year update. Head Neck.
31:748–758. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Eckel HE and Bradley PJ: Treatment options
for hypopharyngeal cancer. Adv Otorhinolaryngol. 83:47–53.
2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sewnaik A and Baatenburg de Jong RJ:
Sequelae and complications of treatment for hypopharyngeal cancer:
Minimising the risks. Adv Otorhinolaryngol. 83:109–117.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mahalingam S and Spielmann P: Quality of
life outcomes following treatment of hypopharyngeal cancer. Adv
Otorhinolaryngol. 83:126–134. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
van den Bosch S, Czerwinski M, Govers T,
Takes RP, de Bree R, Al-Mamgani A, Hannink G and Kaanders JHAM:
Diagnostic test accuracy of sentinel lymph node biopsy in squamous
cell carcinoma of the oropharynx, larynx, and hypopharynx: A
systematic review and meta-analysis. Head Neck. 44:2621–2632.
2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Horváth A, Prekopp P, Polony G, Székely E,
Tamás L and Dános K: Accuracy of the preoperative diagnostic workup
in patients with head and neck cancers undergoing neck dissection
in terms of nodal metastases. Eur Arch Otorhinolaryngol.
278:2041–2046. 2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Freiser ME, Ojo RB, Lo K, Saint-Victor S,
Bollig C, Nayak CS and Sargi ZB: Complications and oncologic
outcomes following elective neck dissection with salvage
laryngectomy for the N0 neck. Am J Otolaryngol. 37:186–194.
2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hardisson D: Molecular pathogenesis of
head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol.
260:502–508. 2003.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Rickman DS, Millon R, De Reynies A, Thomas
E, Wasylyk C, Muller D, Abecassis J and Wasylyk B: Prediction of
future metastasis and molecular characterization of head and neck
squamous-cell carcinoma based on transcriptome and genome analysis
by microarrays. Oncogene. 27:6607–6622. 2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Elsheikh MN, Rinaldo A, Hamakawa H,
Mahfouz ME, Rodrigo JP, Brennan J, Devaney KO, Grandis JR and
Ferlito A: Importance of molecular analysis in detecting cervical
lymph node metastasis in head and neck squamous cell carcinoma.
Head Neck. 28:842–849. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gupta KK, Li C, Duan A, Alberico EO, Kim
OV, Alber MS and Goodson HV: Mechanism for the
catastrophe-promoting activity of the microtubule destabilizer
Op18/stathmin. Proc Natl Acad Sci USA. 110:20449–20454.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hsieh SY, Huang SF, Yu MC, Yeh TS, Chen
TC, Lin YJ, Chang CJ, Sung CM, Lee YL and Hsu CY: Stathmin1
overexpression associated with polyploidy, tumor-cell invasion,
early recurrence, and poor prognosis in human hepatoma. Mol
Carcinog. 49:476–487. 2010.PubMed/NCBI View
Article : Google Scholar
|
|
16
|
Cao S, Zhang W, Shen P and Xu R: Low STMN1
is associated with better prognosis in Asian patients with
esophageal cancers: A meta-analysis. J Gastroenterol Hepatol.
35:1668–1675. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chen Y, Zhang Q, Ding C, Zhang X, Qiu X
and Zhang Z: Stathmin1 overexpression in hypopharyngeal squamous
cell carcinoma: A new promoter in FaDu cell proliferation and
migration. Int J Oncol. 50:31–40. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Zhang Z, Helman JI and Li LJ:
Lymphangiogenesis, lymphatic endothelial cells and lymphatic
metastasis in head and neck cancer-a review of mechanisms. Int J
Oral Sci. 2:5–14. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ji RC: Hypoxia and lymphangiogenesis in
tumor microenvironment and metastasis. Cancer Lett. 346:6–16.
2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhao Z, Mu H, Li Y, Liu Y, Zou J and Zhu
Y: Clinicopathological and prognostic value of hypoxia-inducible
factor-1α in breast cancer: A meta-analysis including 5177
patients. Clin Transl Oncol. 22:1892–1906. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Méndez-Blanco C, Fernández-Palanca P,
Fondevila F, González-Gallego J and Mauriz JL: Prognostic and
clinicopathological significance of hypoxia-inducible factors 1α
and 2α in hepatocellular carcinoma: A systematic review with
meta-analysis. Ther Adv Med Oncol.
13(1758835920987071)2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yang YF, Chang YC, Tsai KW, Hung MH and
Kang BH: UBE2C triggers HIF-1α-glycolytic flux in head and neck
squamous cell carcinoma. J Cell Mol Med. 26:3716–3725.
2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Hartiala P and Saarikko AM:
Lymphangiogenesis and lymphangiogenic growth factors. J Reconstr
Microsurg. 32:10–15. 2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Li S and Li Q: Cancer stem cells,
lymphangiogenesis, and lymphatic metastasis. Cancer Lett.
357:438–447. 2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Achen MG and Stacker SA: Molecular control
of lymphatic metastasis. Ann NY Acad Sci. 1131:225–234.
2008.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Gogineni A, Caunt M, Crow A, Lee CV, Fuh
G, van Bruggen N, Ye W and Weimer RM: Inhibition of VEGF-C
modulates distal lymphatic remodeling and secondary metastasis.
PLoS One. 8(e68755)2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Hirakawa S, Kodama S, Kunstfeld R, Kajiya
K, Brown LF and Detmar M: VEGF-A induces tumor and sentinel lymph
node lymphangiogenesis and promotes lymphatic metastasis. J Exp
Med. 201:1089–1099. 2005.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Alam A, Herault JP, Barron P, Favier B,
Fons P, Delesque-Touchard N, Senegas I, Laboudie P, Bonnin J,
Cassan C, et al: Heterodimerization with vascular endothelial
growth factor receptor-2 (VEGFR-2) is necessary for VEGFR-3
activity. Biochem Biophys Res Commun. 324:909–915. 2004.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Toh Y and Nicolson GL: Identification and
characterization of metastasis-associated gene/protein 1 (MTA1).
Cancer Metastasis Rev. 33:837–842. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Li P, Cao W, Ding R, Cheng M, Xu X, Chen
S, Chen B, Cao G and Xiong M: Expression and prognostic
significance of metastasis-associated protein 1 in gastrointestinal
cancer. Front Oncol. 10(542330)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Liu T, Yang M, Yang S, Ge T, Gu L and Lou
G: Metastasis-associated protein 1 is a novel marker predicting
survival and lymph nodes metastasis in cervical cancer. Hum Pathol.
44:2275–2281. 2013.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Roepman P, de Jager A, Groot Koerkamp MJ,
Kummer JA, Slootweg PJ and Holstege FC: Maintenance of head and
neck tumor gene expression profiles upon lymph node metastasis.
Cancer Res. 66:11110–11114. 2006.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Guo X, Chen Y, Fang W, Yang W, Shi L and
Zhu R: Metastasis associated protein 1 correlates with Hypoxia
inducible-factor 1 alpha expression and lymphangiogenesis in
esophageal cancer. Thorac Cancer. 4:312–317. 2013.PubMed/NCBI View Article : Google Scholar
|